Abstract
With the growing urbanization of China, which has changed older adults’ living conditions, lifestyle, and the source of support, coupled with rapid population aging, the health status of the elderly should be paid attention to. In addition to objective indicators such as the decline of function, specific factors, such as social support, health literacy, and productive aging, also have an impact on the health outcomes of the elderly. However, the interrelationships among these factors and their potential mechanisms in the context of urbanization remain unclear. Thus, this study was the first to explore the interrelationships among social support, health literacy, productive aging, and self-rated health in older adults living in a newly urbanized community in China.
We aimed to investigate the mediating effect of social support on the associations between health literacy, productive aging, and self-rated health among elderly Chinese adults in a newly urbanized community to provide reference data for future health interventions for the elderly.
This cross-sectional study was conducted between June and August 2013. Questionnaires on social support, health literacy, productive aging, and self-rated health were administered to 992 elderly residents. Structural equation models were used to examine the relationships among these 4 variables. Statistical analyses were performed using IBM SPSS Statistics 21.0 and Mplus 7.0.
The mean scores for social support, health literacy, productive aging, and self-rated health were 34.5 ± 5.8, 13.6 ± 4.4, 11.3 ± 3.0, and 3.4 ± 0.7, respectively. Social support was directly related to self-rated health (β=0.119, 95% confidence interval [CI]: 0.041–0.198), while productive aging and health literacy had indirect associations with self-rated health via social support (β=0.071, 95% CI: 0.054–0.216; β=0.049, 95% CI: 0.066–0.183). Both productive aging (β=0.214, 95% CI: 0.047–0.381) and health literacy had direct associations with social support (β=0.327, 95% CI: 0.175–0.479), while health literacy had a direct association with productive aging (β=0.676, 95% CI: 0.604–0.748). Productive aging mediated the relationship between health literacy and social support.
Overall, improving health outcomes among older adults requires enhancement of social support, along with consideration of productive aging and health literacy.
Keywords: health literacy, productive aging, self-rated health, social support, the elderly, urbanized community
1. Introduction
China has seen rapid urbanization over the years, which refers to a shift in the population from rural to urban residency, and from primarily agricultural to nonagricultural work. In 2011, the proportion of the population living in urban areas outnumbered that living in rural areas for the first time, reaching 51%.[1] Given the reduced family size that results from urbanization and the increased mobility of young people, especially from rural areas to cities, the traditional mode of family support has eroded. Where family was once the predominant provider of emotional, physical, and financial support to the elderly, the burden of care has now shifted to the state or other formal organizations.[2,3] However, China's current social security and health care systems are imperfect, and much work is needed to meet the demands of its aging residents.[4] Moreover, urbanization is a double-edged sword for the health of elderly people: urban areas have a relatively complete health infrastructure, and people living in such areas tend to have higher education and incomes, as well as better access to health services and health-related activities, all of which can promote health in the elderly. On the other hand, urbanization increases the population's risk of disease, particularly those related to changing lifestyles and challenging environmental and social conditions.[1] Therefore, the influences associated with Chinese older adults’ health status within the context of urbanization deserve further study.
With age-related declines in physiological function, social participation, and income, it is almost impossible for older adults to avoid poor health outcomes (both physical and mental). Nevertheless, there are numerous factors that can benefit their health outcomes. This study focused on 3 such factors: social support, health literacy, and productive aging.
1.1. Social support
Social support is defined as the “social resources that persons perceive to be available or that are provided to them.” These resources can be instrumental, emotional, or informational, all of which have unique associations with various physical and mental health outcomes.[5,6] Social support is considered a protective factor for maintaining good health and quality of life in old age.[7] Previous studies have demonstrated that people with better social support are less likely to suffer from noncommunicable chronic diseases and that satisfaction with social support is related to good self-rated health in older adults.[8,9] People with better social support were also more likely to develop more positive health behaviors, such as better adherence to medical treatment regimes, exercise, healthy diet, and smoking cessation.[9] It is worth noting that the effects of social support vary depending on a person's age, sex, socioeconomic status, cultural background, and social relationships.[10,11] Presently, we know little about how urbanization influences the relationship between social support and the health outcomes of older adults. Thus, we proposed Hypothesis 1: Social support has a direct positive effect on self-rated health.
1.2. Health literacy
The World Health Organization defines health literacy as the degree to which individuals have the necessary cognitive and social skills to access, understand, and apply basic health information and services to promote and maintain good health.[12] Low health literacy is a relatively universal phenomenon.[13,14] In China, only 3.81% of older adults aged 65 to 69 years have adequate health literacy.[15] Low health literacy is associated with numerous health problems and poor health outcomes[16]; people with low health literacy have a greater risk of developing chronic conditions and worse self-care ability than do persons with adequate health literacy.[17,18] Although research consistently reports that inadequate health literacy is associated with worse health outcomes, there is little information regarding the relationship between health literacy and health outcomes, specifically among elderly Chinese adults in a newly urbanized community. We therefore proposed Hypothesis 2: Health literacy has a direct positive effect on self-rated health.
1.3. Productive aging
“Productive aging” refers to the various activities performed by older people that contribute to the production of goods or services, or develop the capacity to produce such goods or services.[19] This includes employment, volunteering, and other forms of social participation, which were introduced to China in a series of conferences in Shandong and Beijing.[20] Previous research illustrated that productive aging among elderly people is associated with better self-rated health[21] and lower depressive symptoms.[22] Moreover, recent studies have shown that productive aging is also associated with a reduced risk of hypertension and mortality among older adults.[23,24] However, research on productive aging in China is still in its infancy; to date, few studies have examined the relationship between productive aging and health outcomes among older people in China. Thus, we proposed Hypothesis 3: Productive aging has a direct positive effect on self-rated health.
1.4. The present study
Most previous studies examined the relationships between one of the above factors and various health outcomes among the elderly, so comparatively little is known about the combined effects of these 3 factors or the underlying mechanisms of the relationships. Therefore, the primary aim of the present study was to examine the combined association of social support, health literacy, and productive aging with self-rated health and their respective mechanisms among older adults living in a newly urbanized community to identify key factors that benefit older adults’ self-rated health and provide reference for health promotion within the context of urbanization.
A previous study confirmed that lower health literacy was associated with lower social support and that lower social support significantly mediated the relationship between lower health literacy and elevated symptoms of depression.[25] Thus, we proposed Hypothesis 4: Health literacy has a direct positive effect on social support and Hypothesis 5: The relationship between health literacy and self-rated health is mediated by social support because depression is a part of self-rated health. As social support is likely to be the factor most affected by urbanization, and participation in productive aging can increase sources of social support, we speculated that social support would serve as a mediator of the relationship between productive aging and self-rated health among older adults. This led us to formulate Hypothesis 6: Productive aging has a direct positive effect on social support and Hypothesis 7: The relationship between productive aging and self-rated health is mediated by social support. In general, people's health literacy is related to their educational status. Furthermore, educational status has proven to be a strong predictor of productive aging.[26] Therefore, health literacy might also have a positive relationship with productive aging. To test this, we proposed Hypothesis 8: Health literacy has a direct positive effect on productive aging.
In sum, we examined the relationships between social support, health literacy, productive aging, and self-rated health in older adults in a newly urbanized community in China. The hypothesized model is shown in Figure 1.
Figure 1.
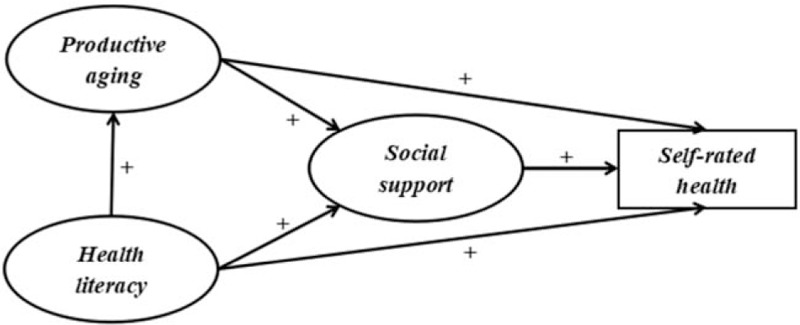
Theoretical model and hypotheses.
2. Materials and methods
2.1. Ethics
The study was approved by the ethics committee of Sichuan University. Ethical issues were taken into consideration in designing the project. All included participants provided written informed consent and voluntarily participated in our study. Their information was kept anonymous.
2.2. Participants and sampling
This cross-sectional study was conducted between June and August 2013. The survey was administered in a newly urbanized district in the suburbs of Chengdu, which began the rural-to-urban conversion process in 2006. The majority of elderly residents in the urbanizing region had shifted from the agricultural to the nonagricultural sector, and the conversion process is still ongoing. All older residents aged 65 years and older who had been living continuously in that community for more than 6 months were eligible to participate.
We calculated the sample size using the following formula:  ; here, π = 9.94% (which was the overall health literacy rate of urban residents in China's first health literacy survey in 200915), δ = 2%, ɑ=0.05, Zα/2 = 1.96. Based on this formula, the minimum effective sample size was calculated as 818. Considering possible dropout, the sample size was increased by 20%, so that the final selected sample was 1000.
; here, π = 9.94% (which was the overall health literacy rate of urban residents in China's first health literacy survey in 200915), δ = 2%, ɑ=0.05, Zα/2 = 1.96. Based on this formula, the minimum effective sample size was calculated as 818. Considering possible dropout, the sample size was increased by 20%, so that the final selected sample was 1000.
We used simple random sampling to recruit the study population. The SAS 9.3 proc plan program (SAS Institute Inc., Cary, NC) was used to randomly select respondents from a database of older adults established by the Community Health Service Centers. A total of 1000 older residents were surveyed face-to-face by trained investigators; of these, we obtained and analyzed 992 (99.2%) valid responses.
2.3. Measuring instruments
The questionnaire survey included the following 5 domains: socio-demographics; social support; health literacy; productive aging; and self-rated health.
2.3.1. Socio-demographics
Socio-demographics included sex, age, education, marital status, pre-retirement occupation, personal monthly income, and living arrangements. Age was categorized as 65–69, 70–74, 75–79, and ≥80 years. Educational level was classified as “no formal education,” “primary school,” “middle school,” and “above.” Marital status was defined as a binary variable: “divorced, widowed, or unmarried” and “married.” Living arrangements were divided into 4 types: “living with spouse only,” “living with child only,” “living with spouse and child,” and “living alone.” Preretirement occupation included white-collar workers (e.g., professional and technical personnel as well as governmental, institutional, or managerial staff), blue-collar workers (business service workers, factory workers), and farmers. Personal monthly income was divided into 4 categories: 0–999, 1000–1999, 2000–2999, and ≥3000 yuan.
2.3.2. Social support
Social support was measured by The Social Support Rating Scale, designed by Xiao.[27] This scale contains 3 subscales (support utilization, objective support, and subjective support) and was developed for use in a Chinese context. Support utilization (3 items) measured the degree to which available support was used and had a total score range of 3 to 12. Objective support (3 items) measured people's actual or visible support and had a total score of 1 to 20. Finally, subjective support (4 items) measured the level of support felt or experienced (e.g., feelings of being understood and respected); it had a total score of 8 to 32. The total score of the full scale, which is the sum of all items, ranged from 12 to 64. Higher scores indicated higher social support. This scale is considered reliable, with a Cronbach's α coefficient of 0.89 and a test–retest reliability of 0.92.[27]
2.3.3. Health literacy
The Chinese Citizen Health Literacy Questionnaire, developed by the National Health and Family Planning Commission of the People's Republic of China, was referenced for this study questionnaire.[28] Representative questions related to health literacy for older adults were selected from this questionnaire by experts, to which we added further questions assessing older adults’ knowledge of common chronic disease prevention to improve the questionnaire. The questionnaire contained 3 subscales: knowledge and belief literacy (19 items), behavior literacy (8 items), and skill literacy (2 items). The full scale contained 29 items, with a total possible score of 29. The scale had a Cronbach's α coefficient of .89.[29]
2.3.4. Productive aging
In line with the research by Ng and others,[19,30] we focused on 5 productive aging activities: paid work, doing chores, caregiving, volunteering, and learning. We measured paid work by asking respondents whether they had maintained paid work after retirement (1 = no, 2 = yes). For the other 4 activities, we assessed the frequency on a scale of 1 (never) to 4 (frequently). The sum of these 5 items (which ranged from 5 to 18) served as an indicator of productive aging, with higher scores indicating a higher level of productive aging. This scale had a Cronbach's α coefficient of 0.73.
2.3.5. Self-rated health
Self-rated health was measured by asking participants “Would you rate your health as very good, good, fair, poor, or very poor?” Responses were assigned scores of 5, 4, 3, 2, and 1, respectively. Higher scores indicated better self-rated health.
2.4. Statistical analysis
We first calculated descriptive statistics (frequencies, percentages, means, and standard deviations) to describe the sample. Subsequently, we performed structural equation modeling (SEM) using the maximum likelihood estimation method to test the hypotheses. We used the subscale scores of social support, health literacy, and productive aging as measurement variables and the total scores of these measures as latent variables. The self-rated health score was also included as a measurement variable. To examine whether the estimated model fit the data, we employed 4-fit indices with their respective cutoffs:[31] root mean square error of approximation (RMSEA) <0.05; Tucker–Lewis index (TLI) and comparative fit index (CFI) values >0.90; a standardized root mean square residual (SRMR) of <0.05; and a χ2/df of < 3. If all indices demonstrate values close to or higher than these cutoff values, the model is considered to have a good fit to the data. All statistical analyses were performed using IBM SPSS Statistics 21.0 (IBM, Inc., Chicago IL) and Mplus 7.0 (Los Angeles, CA). Statistical significance was set at P < .05.
3. Results
3.1. Descriptive results
The socio-demographic characteristics of the sample are displayed in Table 1. The sample consisted of slightly more women than men (52.4% vs 47.6%), and the largest number (n = 430) were aged 65 to 69 years. The largest proportion (n = 452, 45.6%) had a primary school education, and most were married (n = 748, 75.4%) and lived with family members (n = 947, 95.5%). The majority of the sample (n = 657, 66.2%) were farmers, followed by blue-collar workers (n = 209, 21.1%), and white-collar workers (n = 126, 12.7%). The vast majority of participants had personal monthly incomes in the ¥1000–1999 range (n = 733, 73.9%).
Table 1.
Socio-demographic characteristics of the study sample.

Table 2 shows the mean scores of the key variables for the entire sample. The mean scores for social support, health literacy, and productive aging were 34.5 ± 5.8, 13.6 ± 4.4, and 11.3 ± 3.0, respectively. The mean score for self-rated health was 3.4 ± 0.7.
Table 2.
Mean scores of key variables for the total sample.

3.2. Hypothesis testing
We used SEM to test the fitness of the hypothetical model in Figure 1. The analyses revealed that model-fit indices did not achieve acceptable levels if we kept the direct paths between productive aging and self-rated health, and between health literacy and self-rated health. Thus, we revised the model by removing these paths. With the addition of socio-demographics as covariates, the arrow direction among the core variables in the SEM remained unchanged and the corresponding coefficients did not change significantly, so the socio-demographics were not confounding factors. Figure 2 shows the final model where all paths were statistically significant and the model had an adequate fit: RMSEA=0.045, TLI=0.912, CFI=0.944, SRMR=0.038, and χ2/df=3.190.
Figure 2.
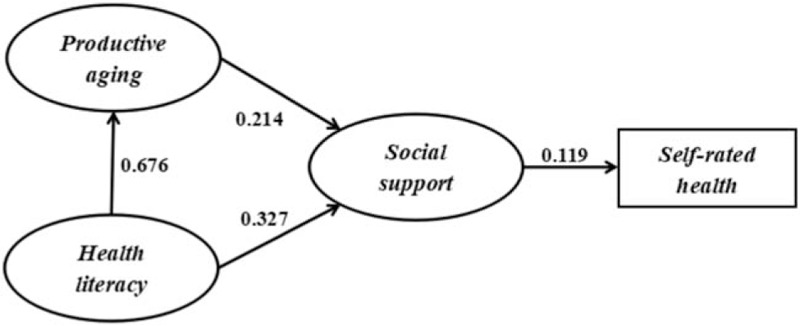
Structural equation analysis of social support, health literacy, productive aging, and self-rated health. All coefficients are significant.
Tables 3 and 4 show the results of hypothesis testing. As expected, social support had a direct association with self-rated health (β=0.119, 95% confidence interval [CI]: 0.041–0.198), thus supporting Hypothesis 1. However, productive aging and health literacy had only indirect associations with self-rated health (β=0.071, 95% CI: 0.054–0.216; β=0.049, 95% CI: 0.066–0.183), rather than direct associations, leading us to reject Hypotheses 2 and 3. Productive aging had a direct association with social support (β=0.214, 95% CI: 0.047–0.381). Health literacy had a direct association with social support (β=0.327, 95% CI: 0.175–0.479) and productive aging (β=0.676, 95% CI: 0.604–0.748). Taken together, these results supported Hypotheses 4, 5, and 7.
Table 3.
Direct, indirect, and total effects of key study variables.

Table 4.
Significance tests of mediating pathways.

Table 4 shows the significance testing of the mediating pathways. In these analyses, if the 95% CI does not include 0, the mediating effect is statistically significant. The results indicated that the relationships of productive aging and health literacy with self-rated health were both mediated by social support (95% CI: 0.004–0.057, 0.011–0.076), thus supporting Hypotheses 6 and 8. In addition, productive aging mediated the relationship between health literacy and social support (95% CI: 0.031–0.268).
4. Discussion
The purpose of the present study was to explore the relationships among social support, health literacy, productive aging, and self-rated health among older adults living in a newly urbanized community, thereby providing theoretical support for future health interventions for elderly people.
The mean score for self-rated health was 3.4, and only 35% of participating older adults rated their health as “very good” or “good.” This suggests that the self-rated health status among the elderly in this newly urbanized community was generally low. This is not surprising given our focus on elderly respondents and the special social characteristics of the urbanized community. By virtue of their age, older adults often show deteriorating physical function, which means that many are in a relatively weak state of health and have a high risk of health insecurity. Furthermore, in a newly urbanized area, older adults might experience physical and psychological discomfort resulting from their efforts to cope with such social changes. In addition, urban health hazards such as water and air pollution, crowded living conditions, and traffic injuries might cause older adults to develop a negative subjective perception of their own health.[32]
Regarding the 3 dimensions of social support in our sample, objective support and support utilization were relatively poor, with mean scores of 6.8 ± 1.7 and 6.7 ± 2.4, respectively. Objective support refers to an individual's social networks, and the instrumental and emotional support they have actually received in the past, particularly in times of distress and crisis. Previous studies have shown that older adults tend to report higher levels of enjoyment and better self-esteem when interacting with friends and neighbors than family members.[33,34] However, in China, older adults tend to interact more frequently with family members and less frequently with neighbors and friends. This presents a challenge in that urbanization has increasingly caused more elderly to live apart from their children, which weakens older adults’ dependence on their family members in all aspects of life. This weakening of family support, coupled with older adults’ isolation from friends and neighbors, is bound to lead to poor objective support. Moreover, the influence of Chinese culture may cause older adults to feel ashamed about seeking help from friends because they feel that it will hurt their relationship.[35] As these individuals grow older, conservative and inflexible personality traits may become increasingly difficult to change. Consequently, older adults might not utilize social support effectively, even when possessing sufficient resources. Therefore, increasing support utilization is the key to alleviating the health effects of limited social support on the elderly.
Social support had a direct positive effect on the self-rated health of older adults, which is consistent with previous studies’ results[36,37] showing that lack of social support was associated with poorer self-assessed mental and physical health.[38,39] Lima-Costa et al[40] verified that older adults who were dissatisfied with their social network had 2 to 4 times greater odds of rating their health as poor, while results from a household survey in the Shunyi district of Beijing suggested that self-rated health was an accurate reflection of social support.[41] Social support can provide older adults with a source of health information. Furthermore, social participation may enhance communication and interpersonal skills to promote the utilization of health information. The spiritual comfort and improved medical and sanitary conditions afforded by good social support may also contribute to the maintenance and promotion of health among older adults. Moreover, social support has been shown to slow down the deterioration of older adults’ health,[42] including cognitive function, making it easier for the elderly to cope with the incapacitating effects of illness.
We also explored productive aging among older adults in a newly urbanized community. Of the 5 dimensions of productive aging, doing chores and caregiving had relatively high scores, at 3.3 ± 1.0 and 2.9 ± 1.1, respectively. The cultural expectations of caring for grandchildren and doing housework are a well-known phenomenon in China.[43] Reciprocity among family members and across generations is often practiced in this family-oriented, collectivistic society.[44] In newly urbanized communities, most older adults no longer engage in farm work. Accordingly, they may spend more time doing chores and assisting families. However, paid work and volunteering had relatively poor scores, at 1.0 ± 0.2 and 1.5 ± 0.9. In China, retirement is mandated at age 60 for men and 55 for women (age 50 for blue-collar jobs). This policy has limited the careers of older adults, even while they remain in their productive years. Formal volunteering is a rather new phenomenon in China. Nongovernmental organizations are restricted, and government-led volunteer programs were only recently developed,[45] leaving few opportunities for older adults to volunteer; consequently, they have not formed habits for volunteering. Previous studies have shown that younger elderly participants with better education and financial status are more likely to engage in productive activities.[4] In our study, the older adults were all over 65 years, and most had low education levels and economic status. Thus, it is not surprising that older adults were at a low level of productive aging in the newly urbanized community.
Prior research has suggested that individuals with low levels of productive aging are more likely to experience symptoms of depression, have poorer self-rated health, and face increased incidence of chronic disease.[46–48] In the current study, we found that the relationship between productive aging and self-rated health was indirect rather than direct, with social support functioning as the mediator. These findings are a meaningful addition to the existing literature and suggest that productive activities such as working and volunteering provide individuals with more opportunities to accept social support. Working and volunteering are known to expand older people's social networks, which grants them more opportunities to receive support from others. In China, assisting the family and doing housework are considered examples of receiving support from others while helping them. Thus, older adults who prefer productive activities experience better social support, which in turn increases their self-reported physical and mental health.
In this study, the mean score for health literacy was 13.6 ± 4.4, indicating that the sample had rather low health literacy. This is congruent with the literature, which shows that low health literacy is a widespread phenomenon.[49,50] For example, in Canada, people aged 65 years or older have the lowest health literacy,[51] and health literacy declines rapidly after the age of 55 years.[52] Populations that are particularly vulnerable to low health literacy are older adults with low education and income levels.[53] In our sample, 86.5% of older adults had a primary school level of education or below, while 80.2% of participants had incomes below ¥2000 per month. People with a low education level might not understand or use medical information in their daily life, while those with a low income are less likely to seek health knowledge, and so are less likely to obtain beneficial health information.[49] In newly urbanized communities, individuals with low education and income levels may receive little health information despite its wide availability via electronic and online sources because they lack internet access.
In other studies on older adults’ health, limited health literacy has been linked to poor health outcomes;[16,54] however, these studies were unable to clarify the mediating factors in this relationship. The current study showed that there was an indirect effect of health literacy on self-rated health, but no direct effect. Adequate health literacy appears to be associated with increased productive aging and social support, both of which were related to better self-rated health. Prior research has shown that individuals with poor health literacy often hide their difficulties from family, friends, and others due to feelings of shame or guilt.[55,56] Thus, people with lower health literacy might isolate themselves, not communicate with those around them, and participate in fewer productive aging activities. As a result, their social networks may weaken, causing them to lose necessary social support. Individuals with adequate health literacy may frequently obtain health information through multiple channels and thus are more willing to be part of a collective to share their knowledge with neighbors and others. Consequently, they may receive greater social support and enjoy increased self-rated physical and mental health.
5. Limitations
The cross-sectional design of this study is its main limitation, as it precludes conjecture on the long-term effects of social support, health literacy, and productive aging on self-rated health among older adults. Furthermore, we cannot draw conclusions on the causal relationships between social support, health literacy, productive aging, and self-rated health. Our results only provide information on the direct and indirect influences on self-rated health among these older adults.
Another limitation is our measure of self-rated health. Although self-rated health is shown to be a comprehensive reflection of the physical and mental health of older adults and is useful for assessing the health of the population, other indicators (e.g., illness within 2 weeks, chronic disease, and well-being) should be incorporated into future studies to more fully capture the health outcomes of older adults.
6. Conclusions
The survey showed that the self-rated health of the elderly in the newly urbanized community was not positive. In the process of urbanization, the elderly may experience poor health outcomes due to their inadaptability to the changes in the environment and lifestyle and the increase in urban health hazards. Professionals should be aware of the impact of urbanization on the health outcomes of the elderly, and future interventions should focus on mitigating its negative effects.
Our findings indicate that social support has a direct positive relationship with self-rated health and mediates the influence of health literacy and productive aging on the self-rated health of older adults. Therefore, priority should be given to interventions that target social support, of which objective support and support utilization are the 2 key components. More collective activities and communication opportunities should be provided for the elderly to strengthen their contact with neighbors and friends and to rebuild their social network, thereby compensating for the lack of family support as a result of urbanization. In addition, the elderly should be encouraged to express how they feel and seek help when necessary, in order to improve the utilization of social support.
In addition, health literacy and productive aging should also be considered seriously. Adequate health literacy is a necessary requirement for older adults’ adherence to healthy habits and positive self-health management. Moreover, productive aging is the basis of older adults’ self-identity and social identity. Thus, paying more attention to improving the health literacy of the older adults through community health education and making use of activity opportunities can improve their self-rated health and have positive effects of urbanization on the health outcomes of the elderly.
Acknowledgments
We wish to acknowledge the research support of HelpAge International and Community Health Foundation of Chengdu. We would also like to thank all the investigators for their assistance with data collection and all the respondents for their cooperation.
Author contributions
DL conceived the idea. BZ and YY performed the statistical analyses and wrote the first draft of the manuscript. DL and MS played a major role in the field survey. DL and HM critically revised the manuscript. All the authors have checked and approved the final manuscript.
Conceptualization: Danping Liu.
Data curation: Danping Liu, Min Sun.
Formal analysis: Yikai Yang, Baiyang Zhang.
Funding acquisition: Danping Liu, Min Sun.
Investigation: Danping Liu, Min Sun.
Methodology: Yikai Yang, Baiyang Zhang, Hongdao Meng, Danping Liu.
Software: Yikai Yang, Baiyang Zhang.
Supervision: Hongdao Meng, Danping Liu.
Writing – original draft: Yikai Yang, Baiyang Zhang.
Writing – review & editing: Hongdao Meng, Danping Liu.
Footnotes
Abbreviations: 95% CI = 95% confidence interval, CFI = comparative fit index, RMSEA = root mean square error of approximation, SEM = structural equation modelling, SRMR = standardized root mean square residual, TLI = Tucker–Lewis index.
YY and BZ are contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Gong P, Liang S, Carlton EJ, et al. Urbanisation and health in China. Lancet 2012;379:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Feng Z, Wang WW, Jones K. A multilevel analysis of the role of the family and the state in self-rated health of elderly Chinese. Health Place 2013;23(23C):148–56. [DOI] [PubMed] [Google Scholar]
- [3].Ergin I, Mandiracioglu A. Demographic and socioeconomic inequalities for self-rated health and happiness in elderly: the situation for Turkey regarding World Values Survey between 1990 and 2013. Arch Gerontol Geriatr 2015;61:224–30. [DOI] [PubMed] [Google Scholar]
- [4].Li Y, Xu L, Chi I, et al. Participation in productive activities and health outcomes among older adults in urban China. Gerontologist 2014;54:784–96. [DOI] [PubMed] [Google Scholar]
- [5].Ashida S, Heaney CA. Differential associations of social support and social connectedness with structural features of social networks and the health status of older adults. J Aging Health 2008;20:872–93. [DOI] [PubMed] [Google Scholar]
- [6].Gottlieb BH, Bergen AE. Social support concepts and measures. J Psychosom Res 2010;69:511–20. [DOI] [PubMed] [Google Scholar]
- [7].Newsom JT, Schulz R. Social support as a mediator in the relation between functional status and quality of life in older adults. Psychol Aging 1996;11:34–44. [DOI] [PubMed] [Google Scholar]
- [8].White AM, Philogene GS, Fine L, et al. Social support and self-reported health status of older adults in the United States. Am J Public Health 2009;99:1872–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med 2006;29:377–87. [DOI] [PubMed] [Google Scholar]
- [10].Uchino BN. Social Support and Physical Health: Understanding the Health Consequences of Relationships. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- [11].Craigs CL, Twiddy M, Parker SG, et al. Understanding causal associations between self-rated health and personal relationships in older adults: a review of evidence from longitudinal studies. Arch Gerontol Geriatr 2014;59:211–26. [DOI] [PubMed] [Google Scholar]
- [12].Kickbusch I, Pelikan JM, Tsouros, et al. Health Literacy: The Solid Facts. Copenhagen: World Health Organization Regional Office for Europe; 2013. [Google Scholar]
- [13].Kutner M, Greenburg E, Jin Y, et al. The health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006-483. Washington, DC: National Center for Education Statistics; 2006. [Google Scholar]
- [14].Eichler K, Weiser S, Brügger U. The costs of limited health literacy: a systematic review. Int J Public Health 2009;54:313–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Xiao L, Yu MA, Ying Hua LI, et al. Study on the health literacy status and its influencing factors of urban and rural residents in China. Chinese J Health Educ 2009;25:323–6. [Google Scholar]
- [16].Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. [DOI] [PubMed] [Google Scholar]
- [17].Zimmerman T, Shenenberger DW. Health literacy and diabetic control. JAMA 2002;288:2687–8. [DOI] [PubMed] [Google Scholar]
- [18].Murray MD, Tu W, Wu J, et al. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Therap 2009;85:651–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Morrow-Howell N, Hinterlong J, Sherraden M. The John Hopkins University Press, Productive Aging: Concepts and Challenges. Baltimore, MD: 2001. [Google Scholar]
- [20].Lum YS. Advancing research on productive aging activities in greater Chinese societies. Ageing Int 2013;38:171–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hinterlong JE, Morrow-Howell N, Rozario PA. Productive engagement and late life physical and mental health findings from a nationally representative panel Study. Res Aging 2007;29:348–70. [Google Scholar]
- [22].Thoits PA, Hewitt LN. Volunteer work and well-being. J Health Soc Behav 2001;42:115–31. [PubMed] [Google Scholar]
- [23].Pynnönen K, Törmäkangas T, Heikkinen RL, et al. Does social activity decrease risk for institutionalization and mortality in older people? J Gerontol B Psychol Sci Soc Sci 2012;67:765–74. [DOI] [PubMed] [Google Scholar]
- [24].Tavares JL, Burr JA, Mutchler JE. Race differences in the relationship between formal volunteering and hypertension. J Gerontol B Psychol Sci Soc Sci 2013;68:310–9. [DOI] [PubMed] [Google Scholar]
- [25].Stewart DW, Reitzel LR, Correa-Fernández V, et al. Social support mediates the association of health literacy and depression among racially/ethnically diverse smokers with low socioeconomic status. J Behav Med 2014;37:1169–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Burr JA, Caro FG, Moorhead J. Productive aging and civic participation. J Aging Stud 2002;16:87–105. [Google Scholar]
- [27].SY X. The theoretical basis and application of social support questionnaire. J Clin Psychol Med 1994;4:98–100. [Google Scholar]
- [28].Xiaoping W. The first survey results of Chinese residents’ health literacy. Chin J Reprod Health 2010;21:120–120. [Google Scholar]
- [29].Lei LI, Shi FF, Liu DP, et al. Research on the status and influencing factors of health literacy among urban community elderly residents. Mod Prev Med 2014;41:3931–5. [Google Scholar]
- [30].Ng SH, Cheung CK, Chong AM, et al. Aging well socially through engagement with life: adapting Rowe and Kahn's model of successful aging to Chinese cultural context. Int J Aging Hum Dev 2011;73:313–30. [DOI] [PubMed] [Google Scholar]
- [31].Weston R, Gore PA., Jr A brief guide to structural equation modeling. Couns Psychol 2006;34:719–51. [Google Scholar]
- [32].Moore M, Gould P, Keary BS. Global urbanization and impact on health. Int J Hyg Environ Health 2003;206:269–78. [DOI] [PubMed] [Google Scholar]
- [33].Adams RG, Blieszner R. Aging well with friends and family. Am Behav Sci 1995;39:209–24. [Google Scholar]
- [34].Lee GR, Shehan CL. Social relations and the self-esteem of older persons. Res Aging 1989;11:427–42. [DOI] [PubMed] [Google Scholar]
- [35].Dai Y, Zhang CY, Zhang BQ, et al. Social support and the self-rated health of older people: a comparative study in Tainan Taiwan and Fuzhou Fujian province. Medicine (Baltimore) 2016;95:e3881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Song L, Li S, Zhang W, et al. Intergenerational Support and Self-rated Health of the Elderly in Rural China: An Investigation in Chaohu, Anhui Province. Dordrecht, Netherlands: Springer; 2008. [Google Scholar]
- [37].Berkman LF. The role of social relations in health promotion. Psychosom Med 1995;57:245–54. [DOI] [PubMed] [Google Scholar]
- [38].Sun W, Watanabe M, Tanimoto Y, et al. Factors associated with good self-rated health of non-disabled elderly living alone in Japan: a cross-sectional study. BMC Public Health 2007;7:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav 2009;50:31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lima-Costa MF, Firmo JO, Uchôa E. Differences in self-rated health among older adults according to socioeconomic circumstances: the Bambuí Health and Aging Study. Cad Saúde Pública 2005;21:830–9. [DOI] [PubMed] [Google Scholar]
- [41].Meng Q. Social support, self-care status and self-rated health in elderly. J Med Res 2010;39:86–9. [Google Scholar]
- [42].Choi NG, Wodarski JS. The relationship between social support and health status of elderly people: does social support slow down physical and functional deterioration? Social Work Res 1996;20:52–63. [PubMed] [Google Scholar]
- [43].Chen F, Liu G. The health implications of grandparents caring for grandchildren in China. J Gerontol B Psychol Sci Soc Sci 2012;67:99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Hwang K. Face and favor: the Chinese power game. Am J Sociol 1987;92:944–74. [Google Scholar]
- [45].Mui AC. Productive ageing in China: a human capital perspective. China J Soc Work 2010;3:111–23. [Google Scholar]
- [46].Choi NG, Bohman TM. Predicting the changes in depressive symptomatology in later life: how much do changes in health status, marital and caregiving status, work and volunteering, and health-related behaviors contribute? J Aging Health 2007;19:152–77. [DOI] [PubMed] [Google Scholar]
- [47].Menec VH. The relation between everyday activities and successful aging: a 6-year longitudinal study. J Gerontol B Psychol Sci Soc Sci 2003;58:S74–82. [DOI] [PubMed] [Google Scholar]
- [48].Chiao C, Weng LJ, Botticello AL. Social participation reduces depressive symptoms among older adults: an 18-year longitudinal analysis in Taiwan. BMC Public Health 2011;11:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Liu YB, Wang YR, Liang F, et al. The health literacy status and influencing factors of older population in Xinjiang. Iran J Public Health 2015;44:913–9. [PMC free article] [PubMed] [Google Scholar]
- [50].Gazmararian JA, Williams MV, Peel J, et al. Health literacy and knowledge of chronic disease. Patient Educ Couns 2003;51:267–75. [DOI] [PubMed] [Google Scholar]
- [51].Murray TS, Hagey J, Willms D, et al. Health Literacy in Canada: A Healthy Understanding. Ottawa: Canadian Council on Learning; 2008. [Google Scholar]
- [52].Kutner M, Greenberg E, Jin Y, et al. Literacy in Everyday Life: Results from the 2003 National Assessment of Adult Literacy. NCES 2007-490. Washington, DC: National Center for Education Statistics; 2007. [Google Scholar]
- [53].Abdellatif M, Saad SY. Health literacy among Saudi population: a cross-sectional study. Health Promot Int 2019;34:60–70. [DOI] [PubMed] [Google Scholar]
- [54].Serper M, Patzer RE, Curtis LM, et al. Health literacy, cognitive ability, and functional health status among older adults. Health Serv Res 2014;49:1249–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Johnson VR, Jacobson KL, Gazmararian JA, et al. Does social support help limited-literacy patients with medication adherence? A mixed methods study of patients in the Pharmacy Intervention for Limited Literacy (PILL) Study. Patient Educ Couns 2010;79:14–24. [DOI] [PubMed] [Google Scholar]
- [56].Nurss JR. Shame and health literacy: the unspoken connection. Patient Educ Couns 1996;27:33–9. [DOI] [PubMed] [Google Scholar]


