Abstract
To investigate the relationship between depression and the self-reported prospective memory (SPM) problems in breast cancer survivors who have received chemotherapy.
Sixty-three breast cancer patients were administered with self-rating depression scale (SDS) and the prospective memory questionnaire as part of extensive neuropsychological assessments before and after chemotherapy. The performance of SDS and SPM were compared, with the level of significance set at P < .05.
Compared with the group before chemotherapy, there is a significant difference on the SPM score (t = 6.069, P = .000) in breast cancer patients after chemotherapy. Further, there is also a significant difference on the SPM score (t = −4.348, P = .000) between the patients with and without depression group after chemotherapy.
The present result indicated that the depression in breast cancer survivors after chemotherapy may be involved in their chemotherapy-induced SPM impairment.
Keywords: breast cancer, chemotherapy, depression, prospective memory
1. Introduction
Breast cancer is the most common cancer in women.[1] With the development of all kinds of cancer treatment, mortality rates of breast cancer patients had declined in recent years, but the side effects of chemotherapy are reported frequently. Chemotherapy-induced cognitive impairment (CICI) is the most frequent complication reported by breast cancer patients. CICI refers to the impairment of cognitive functions such as memory, attention, and information processing speed that occurs in cancer patients during or after chemotherapy.[2] Recently study suggested that most of breast cancer patients may experience CICI,[3] especially on all kinds of subjective and objective memory impairment.[4,5] The impact of CICI in long-term breast cancer survivor was even worse than the recurrence and metastasis of breast cancer itself. Recently, Wirkner et al[6] found that the levels of cognitive impairment in breast cancer patients were related to their anxiety level. Findings suggested that patients who scored lower on neuropsychological tests reported more symptoms of anxiety.
Recently studies have also suggested that the memory problem was prominent in breast cancer survivors after chemotherapy, and there is some heterogeneity on different memory components.[3] Prospective memory (PM) is the memory required for future plans or intentions and the memory component most closely related to human daily lives. Cheng et al[7] found that breast cancer survivors exhibited PM impairment after chemotherapy. Paquet et al[8] found that chemotherapy-induced PM impairment in breast cancer survivors was associated with symptoms of anxiety and depression.
There is also increasing evidence that subjective memory decline, even with normal performance on objective neuropsychological tests, is associated with an increased risk for developing cognitive decline. Complaints of memory dysfunction are commonly reported by breast cancer survivors after chemotherapy. Our previous study suggested that there was self-reported prospective memory (SPM) impairment in breast cancer survivors after chemotherapy.[9] However, the specific impacting factors are not clear yet. Previous studies have found that emotion is an important factor to affect memory,[10] and depression was one of the most common mental disorders in breast cancer patients,[11] and it may affect their cognitive functions.[12] But up to now, there is no report about whether the depression is related to chemotherapy-induced SPM impairment.
The objective of the present research is to identify whether the depression in breast cancer survivors after chemotherapy is involved in their chemotherapy-induced SPM impairment.
2. Methods
2.1. Participants
This is a case-control study in breast cancer patients. A total of 63 breast cancer patients who were hospitalized from October 2013 to August 2017 in the Department of Oncology, the Second Affiliated Hospital of Anhui Medical University, were recruited. There were 59 breast cancer patients were identified as those of invasive ductal carcinoma and 4 breast patients as invasive lobular carcinoma by postoperative pathology. All breast patients were right-handed and were selected according to the following criteria:
-
(1)
postoperative pathologic diagnosis of breast cancer;
-
(2)
chemotherapy with paclitaxel and doxorubicin;
-
(3)
mini-mental state examination (MMSE) score ≥24;
-
(4)
Karnofsky performance status score ≥80;
-
(5)
without impairment of vision or hearing and language.
Patients with breast cancer were excluded if the following conditions were present:
-
(1)
patients who have received other treatment such as radiotherapy or endocrine therapy before chemotherapy;
-
(2)
taking relevant drugs to affect cognitive function;
-
(3)
severe diseases of heart, liver, kidney, brain, and the hematopoietic system.
All subjects in the present study were investigated during 1 week before and after chemotherapy. The study was approved by the Research Ethics Committee of the Affiliated Second Hospital of Anhui Medical University, and all subjects provided their informed consent.
2.2. Depression assessment
Depression was assessed by self-rating depression scale (SDS), which is a self-rating scale to measure the severity of depression. The degrees of depression were divided into 3 different level: 53 to 62 points, mild depression; 63 to 72 points, moderate depression; and >72 points, severe depression.
2.3. Neuropsychological background tests
The MMSE was administered to assess the cognitive functions, including temporal and spatial orientation, short-term memory, calculation, language, and visuospatial skills. The verbal fluency test (VFT) was administered to the subjects, who were instructed to name as many animals as possible in 1 minute. The digit span test (DS) was used to measure short-term memory, in which the subjects were instructed to recall a series of numbers after hearing them in a randomized order.
2.4. PM Questionnaires
PM questionnaire (PMQ) were performed individually for each patient before and after chemotherapy. The PMQ is used to test the performance of SPM, and it consists of 8 items for testing PM disorders. The patients were required to rate the degree of their memory failure on a 4-point, Likert scale for each item: (4: very often, 3: sometimes, 2: rarely, 1: never). The total score for PM ranged from 8 to 32, with higher scores indicating greater PM impairment.
2.5. Statistical analysis
All data were expressed as mean ± standard deviation. Statistical analysis was performed with SPSS 17.0 software. Scores between before and after chemotherapy were analyzed by means of paired-samples t tests. Scores between the depression and nondepression groups were compared using 2 independent samples t tests. All statistical tests were 2-tailed, with the level of significance set at P < .05.
3. Results
3.1. The basic clinical information in breast cancer patients
Sixty-three BC patients were evaluated after chemotherapy, out of which, 29 patients were found to have depression, while 34 patients were not. There was no significant difference in age (50.66 ± 7.76 vs 47.35 ± 8.56; t = 1.593, P = .116) and years of education (7.90 ± 3.36 vs 9.44 ± 3.57; t = −1.758, P = .084), and other general characteristics between the depression and nondepression groups.
3.2. The performance of SDS, MMSE, VFT, DS, and SPM in breast cancer patients before and after chemotherapy
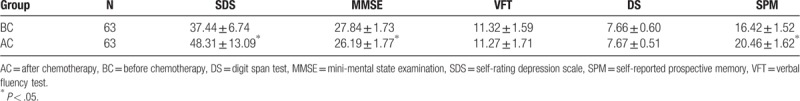
There were a statistically significant difference on SDS (t = −5.860, P = .000), MMSE scores (t = 5.292, P = .000) and SPM score (t = 6.069, P = .000), while no statistically significant differences on VFT and DS in breast cancer patients between before and after chemotherapy group (Table 1).
Table 1.
Comparison of performance of SDS, MMSE, VFT, DS, SPM before and after chemotherapy.
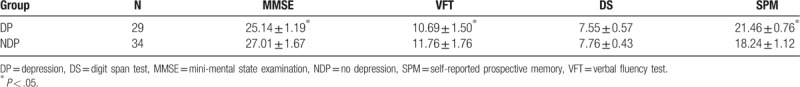
3.3. Performance of neuropsychological tests and SPM between depression and no depression groups
There were significantly lower on MMSE (t = −5.202, P = .000) and VFT scores (t = −2.591, P = .012) of the depression group when compared to nondepression group. Further, as compared with the depression group, the SPM score of the nondepression group was significantly different (t = −4.348, P = .000) (Table 2).
Table 2.
Comparison performance of depression, MMSE, VFR, DS, SPM, between the depression group and the nondepression group after chemotherapy.
4. Discussion
As we know, the present research is the first time to evaluate the relationship between depression and the SPM problems in breast cancer survivors after chemotherapy. Previous evidence[13–15] suggested that CICI in breast cancer survivors were mainly related to attention, information processing speed, executive function, language function, visuospatial function, and memory. The present result suggests that depression may contribute to the SPM impairment in breast cancer survivors after chemotherapy.
Memory is one of the important cognitive functions for human, which could be divided into retrospective memory (RM) and PM,[16] and different types of memory involve different region of the brain.[17] Complaints of memory decline are perhaps the most frequently reported cognitive difficulties in breast cancer survivors, which historically has been the exclusive focus of objective memory. PM is one of the most important forms of human memory. PM complaints were significantly more frequent than RM complaints, and were more frequent on self-perceptions regarding day-to-day memory functioning, which required self-initiated intention monitoring, maintenance, and retrieval strategies. Volle et al[18] found that the spontaneous extraction of PM information was related to the functions of the prefrontal cortex. Our previous studies found that there was significant PM impairment in patients with frontal lobe impairment.[19] The present result indicated that breast cancer survivors with depression had significant SPM impairment following chemotherapy, which might be related to insufficient function in the prefrontal structures.
Previous studies investigated the relationship between psychological variable and CICI in breast cancer survivors.[20,21] Depression is a common mental state in breast cancer survivors, and affective distress appears to be a primary contributor to their PM impairment. Higher self-reported levels of depression were significantly associated with increased frequency of SPM complaints. Regression analyses revealed that depression was the predictor of memory complaints.[22] The incidence of depressive symptoms in patients with newly diagnosed breast cancer was up to 32.1%, and in 19.4% of them the depression was moderate or mild, while in 12.7% patients it was moderate or severe.[23]
Chemotherapy is one of the important treatment for breast cancer patients; however, most breast cancer survivors worried about chemotherapy. Additionally, the incidence of depression in breast cancer survivors has been reported to be even higher than patients before chemotherapy. Studies have also found that not all breast cancer survivors suffer from depression, and that those with depression have also exhibited differences in the manifestation, degree, and duration of depression.[22,23] Lekovich et al[24] found that the incidence of depression in 95 breast cancer survivors within 1 to 6 months after chemotherapy, and reported it to be up to 67%. Recently studies have found that depression in breast cancer survivors was not temporary, and some patients have even exhibited high levels of depressive symptoms after the treatment.[25,26]
The main causes of depression in breast cancer survivors have been reported as follows: shock from the breast cancer diagnosis; special importance of breasts to females, and as most breast cancer patients prefer surgical treatment, the physical change would result in a double whammy physically and mentally; socio-demographic factors such as age, educational level, employment status, household income, obesity, and marital status (all these have been reported to affect patient's depression); the side effects of chemotherapy on fertility, sexual function, perimenopausal period, and related health problems, which have been reported to cause significant anxiety and pain in breast cancer survivors.[27]
The present result found that depression caused by various factors might be involved in the occurrence of CICI in breast cancer survivors, especially on SPM impairment. The mechanisms of CICI in breast cancer survivors are not clear yet. However, recently there has been active research in this field. Several studies have found that CICI is manifested differently in breast cancer survivors, with many impacting factors and complex pathogeneses. Therefore, several multidisciplinary studies, such as those on mechanisms of CICI in breast cancer survivors studies have been conducted.[28,29,30] The present result provided evidence for the incidence of SPM impairment in breast cancer survivors after chemotherapy from the perspective of the effect of depression on memory.
5. Conclusion
To summarize, the present result suggested that there was a significant decline on general cognitive function and SPM in the breast cancer survivors with depression after chemotherapy. It indicated that depression might be associated with chemotherapy-induced SPM impairment in breast cancer survivors.
Author contributions
Conceptualization: Huaidong Cheng, Jingjing Zhao.
Data curation: Zhonglian Huang, Jingjing Zhao, Ke Ding.
Formal analysis: Huaidong Cheng, Congjun Zhang, Chiang Shan Li.
Funding acquisition: Huaidong Cheng, Yue Lv.
Investigation: Jingjing Zhao, Ke Ding, Yue Lv, Huaidong Cheng.
Methodology: Huaidong Cheng, Jingjing Zhao, Ke Ding, Herta H. Chao.
Project administration: Huaidong Cheng, Congjun Zhang.
Supervision: Huaidong Cheng, Congjun Zhang, Herta H. Chao, Chiang Shan Li.
Writing – original draft: Zhonglian Huang, Jingjing Zhao, Ke Ding, Yue Lv.
Footnotes
Abbreviations: CICI = chemotherapy induced cognitive impairment, DS = digit span test, MMSE = mini-mental state examination, PM = prospective memory, PMQ = prospective memory questionnaire, RM = retrospective memory, SDS = self-rating depression scale, SPM = self-reported prospective memory, VFT = verbal fluency test.
ZH, JZ, and KD contributed equally to this study.
The present study was funded by the National Natural Science Foundation of China (No. 81872504; 81372487).
The authors declare no conflict of interest.
References
- [1].Fan L, Strasser-Weippl K, Li JJ, et al. Breast cancer in China. Lancet Oncol 2014;15:e279–89. [DOI] [PubMed] [Google Scholar]
- [2].Winocur G, Berman H, Nguyen M, et al. Neurobiological mechanisms of chemotherapy-induced cognitive impairment in a transgenic model of breast cancer. Neuroscience 2018;369:51–65. [DOI] [PubMed] [Google Scholar]
- [3].Jim HS, Phillips KM, Chait S, et al. Meta-analysis of cognitive functioning in breast cancer survivors previously treated with standard-dose chemotherapy. J Clin Oncol 2012;30:3578–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ahles TA, Root JC, Ryan EL. Cancer-and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol 2012;30:3675–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wefel JS, Saleeba AK, Buzdar AU, et al. Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer 2010;116:3348–56. [DOI] [PubMed] [Google Scholar]
- [6].Wirkner J, Weymar M, Löw A, et al. Cognitive functioning and emotion processing in breast cancer survivors and controls: an ERP pilot study. Psychophysiology 2017;54:1209–22. [DOI] [PubMed] [Google Scholar]
- [7].Cheng H, Yang Z, Dong B, et al. Chemotherapy-induced prospective memory impairment in patients with breast cancer. Psychooncology 2013;22:2391–5. [DOI] [PubMed] [Google Scholar]
- [8].Paquet L, Collins B, Song X, et al. A pilot study of prospective memory functioning in early breast cancer survivors. Breast 2013;22:455–61. [DOI] [PubMed] [Google Scholar]
- [9].Cheng H, Li W, Gan C, et al. The COMT (rs165599) gene polymorphism contributes to chemotherapy-induced cognitive impairment in breast cancer patients. Am J Transl Res 2016;8:5087–97. [PMC free article] [PubMed] [Google Scholar]
- [10].Lindquist KA, Gendron M, Barrett LF, et al. Emotion perception, but not affect perception, is impaired with semantic memory loss. Emotion 2014;14:375–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Suppli NP, Johansen C, Christensen J, et al. Increased risk for depression after breast cancer: a nationwide population-based cohort study of associated factors in Denmark, 1998-2011. J Clin Oncol 2014;32:3831–9. [DOI] [PubMed] [Google Scholar]
- [12].Kalender ME, Buyukhatipoglu H, Balakan O, et al. Depression, anxiety and quality of life through the use of complementary and alternative medicine among breast cancer patients in Turkey. J Cancer Res Ther 2014;10:962–6. [DOI] [PubMed] [Google Scholar]
- [13].Duijts SF, Faber MM, Oldenburg HS, et al. Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors-a meta-analysis. Psychooncology 2011;20:115–26. [DOI] [PubMed] [Google Scholar]
- [14].Phillips KA, Ribi K, Fisher R. Do aromatase inhibitors have adverse effects on cognitive function? Breast Cancer Res 2011;13:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Shaffer VA, Merkle EC, Fagerlin A, et al. Chemotherapy was not associated with cognitive decline in older adults with breast and colorectal cancer: findings from a prospective cohort study. Med Care 2012;50:849–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].McDaniel MA, Einstein GO. The neuropsychology of prospective memory in normal aging: a componential approach. Neuropsychologia 2011;49:2147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Shen H. How to see a memory. Nature 2018;553:146–8. [DOI] [PubMed] [Google Scholar]
- [18].Volle E, Gonen-Yaacovi G, Costello Ade L, et al. The role of rostral prefrontal cortex in prospective memory: a voxel-based lesion study. Neuropsychologia 2011;49:2185–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cheng HD, Wang K, Xi CH, et al. Prefrontal cortex involvement in the event-based prospective memory: evidence from patients with lesions to prefrontal cortex. Brain Inj 2008;22:697–704. [DOI] [PubMed] [Google Scholar]
- [20].Schilder CM, Seynaeve C, Linn SC, et al. Self-reported cognitive functioning in postmenopausal breast cancer patients before and during endocrine treatment: findings from the neuropsychological TEAM side-study. Psychooncology 2012;21:479–87. [DOI] [PubMed] [Google Scholar]
- [21].Jung MS, Zhang M, Askren MK, et al. Cognitive dysfunction and symptom burden in women treated for breast cancer: a prospective behavioral and fMRI analysis. Brain Imaging Behav 2017;11:86–97. [DOI] [PubMed] [Google Scholar]
- [22].Fann JR, Thomas-Rich AM, Katon WJ, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 2008;30:112–26. [DOI] [PubMed] [Google Scholar]
- [23].Luutonen S, Vahlberg T, Eloranta S, et al. Breast cancer patients receiving postoperative radiotherapy: distress, depressive symptoms and unmet needs of psychosocial support. Radiother Oncol 2011;100:299–303. [DOI] [PubMed] [Google Scholar]
- [24].Levkovich I, Cohen M, Pollack S, et al. Cancer-related fatigue and depression in breast cancer patients post chemotherapy: different associations with optimism and stress appraisals. Palliat Support Care 2014;9:1–1. [DOI] [PubMed] [Google Scholar]
- [25].Seliktar N, Polek C, Brooks A, et al. Cognition in breast cancer survivors: hormones versus depression. Psychooncology 2015;24:402–7. [DOI] [PubMed] [Google Scholar]
- [26].Pullens MJ, De Vries J, Van Warmerdam LJ, et al. Chemotherapy and cognitive complaints in women with breast cancer. Psychooncology 2013;22:1783–9. [DOI] [PubMed] [Google Scholar]
- [27].Andrykowski MA, Burris JL, Walsh E, et al. Attitudes toward information about genetic risk for cognitive impairment after cancer chemotherapy: breast cancer survivors compared with healthy controls. J Clin Oncol 2010;28:3442–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Andreotti C, Root JC, Ahles TA, et al. Coping, and cognition: a model for the role of stress reactivity in cancer-related cognitive decline. Psychooncology 2015;24:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Menning S, de Ruiter MB, Veltman DJ, et al. Multimodal MRI and cognitive function in patients with breast cancer prior to adjuvant treatment – the role of fatigue. Neuroimage Clin 2015;7:547–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hermelink K, Bühner M, Sckopke P, et al. Chemotherapy and post-traumatic stress in the causation of cognitive dysfunction in breast cancer patients. J Natl Cancer Inst 2017;109:dxj057. [DOI] [PubMed] [Google Scholar]


