Abstract
Strong evidence exists for the benefits of screening for hypertension to reduce the risk of cardiovascular disease and death. The aim of this study was to analyze the frequency and determinants of blood pressure (BP) measurement by a health professional in the general population and in individuals without hypertension in Germany.
Data from 17,431 participants 15+ years from the cross-sectional GEDA2014/2015-EHIS survey were used to calculate the percentage of the population who had no BP measurement within the last year and the last 3 years. In multivariate models, the determinants of no BP measurement were analyzed. The frequency of BP measurement was compared between 30 European countries.
In Germany, 27.5% of men and 16.6% of women had no BP measurement by a health professional within the last year and 10.9%, respectively 5.4% not within the last 3 years. In individuals without known hypertension, 34.1% of men and 23.6% of women aged 15 to 19 years had no BP measurement in the last 3 years compared to 5.2% of men and 4.8% of women 70+ years. Independent predictors of not receiving a BP measurement in the last 3 years besides age were male sex, good self-rated health, low health awareness, and no medical consultations but not educational level. Germany has low proportions of no BP measurement compared to other European countries.
Hypertension screening needs improvement in all age groups, especially in the young who have the lowest screening proportions but also in the elderly who have the highest hypertension risk.
Keywords: blood pressure measurement, blood pressure screening, hypertension, prevention
Key Points
The frequency of BP measurement by a health professional is high in Germany.
8.1% of the population had no BP measurement within the last 3 years.
Women, older people with bad self-rated health had more frequent measurements.
Educational level was not related to the frequency of BP measurement by a health professional.
1. Introduction
More than 60 years ago, the Framingham Heart Study played a key role in demonstrating that high blood pressure (BP) leads to increased mortality from stroke and myocardial infarction and physicians began to measure BP more systematically as part of their general medical examination.[1] Today, a continuous association between BP and cardiovascular events starting at a BP of 115/75 mmHg is well established.[2] High BP is widely recognized as a leading contributor to the global burden of disease and mortality, resulting in more than 10 million deaths each year for systolic BP of at least 110 to 115 mmHg.[3]
Strong evidence exists for the benefits of screening for high BP[4] and effectively treating hypertension, for example, a reduction in systolic BP by 10 mmHg reduced the risk of coronary heart disease by 17%, stroke by 27%, heart failure by 28%, and all-cause mortality by 13%.[5] Furthermore, regular BP measurement is an easy, not invasive, inexpensive and safe diagnostic procedure which can be done at home or in an office environment and effective hypertension treatment is available. Despite these facts, good hypertension management remains to be a global challenge. A recent multinational study reported that only 46.5% of participants with hypertension were aware of their diagnosis.[6] In Germany, the overall awareness rate was higher and ranged between 82.3% in men and 86.6% in women, but especially young, hypertensive men between 18 and 29 years had surprisingly low awareness rates with only 23.6%.[7]
Despite the well-established benefits of screening for hypertension,[4] there is surprisingly little data on the actual frequency of BP measurement on the population level not only in Germany but also in other countries. Therefore, the aim of this study is to analyze the frequency and determinants of BP measurement by a health professional in the German population on the basis of data from the cross-sectional nationwide “German Health Update 2014” (GEDA 2014/2015-EHIS) and to compare the results with other countries with data from the European Health Interview Survey (EHIS).
2. Methods
2.1. Study design and sample
In the cross-sectional “German Health Update 2014” (GEDA 2014/2015-EHIS), a 2-stage, clustered sampling design was used to select 301 communities and random samples of individuals ≥15 years with permanent residency in Germany were drawn from local population registries.[8] Between 2014 and 2015, a total of 24,824 people either completed a paper or online questionnaire (mixed-mode-design). The response rate was 27.6%. More detailed information is given elsewhere.[9,10] For our analysis, we excluded 109 (0.4%) participants with missing data on the last time their BP was measured, which left a final study sample of 24,705 participants.
The study was approved by The Federal Commissioner for Data Protection and Freedom of Information, and written informed consent was obtained from all participants before the interview.
2.2. BP measurement and other variables
The question “When was the last time that your BP was measured by a health professional?” had 5 answer options from:
-
1)
“less than 1 year”,
-
2)
“between 1 and 3 years”,
-
3)
“between 3 and 5 years”,
-
4)
“more than 5 years”, and
-
5)
to “never”.
We defined 3 outcomes:
-
1)
no BP measurement within the last year,
-
2)
no BP measurement within the last 3 years, and
-
3)
no BP measurement within the last 5 years.
Independent variables included sex, age, education, self-rated health, and health awareness. The last time a general practitioner (GP) or a medical specialist was consulted were dichotomized to “Within the last 12 months” compared to “More than 1 year ago”. Participants were classified as hypertensives if they reported that they had ever been diagnosed with hypertension by a physician and if they in addition either confirmed having hypertension within the last 12 month or currently taking anti-hypertensive medication.[11] For each of the independent variables, the number of missings was below 0.7%.
2.3. Statistical analyses
All analyses were stratified for men and women and we calculated the prevalence of no BP measurement within the last year and the last 3 years with 95% confidence interval (CI) (Figs. 1 and 2). We used logistic regression analyses to estimate multivariate-adjusted odds ratios (OR) with 95%-CI for factors associated with no BP management within the last 3 years.
Figure 1.
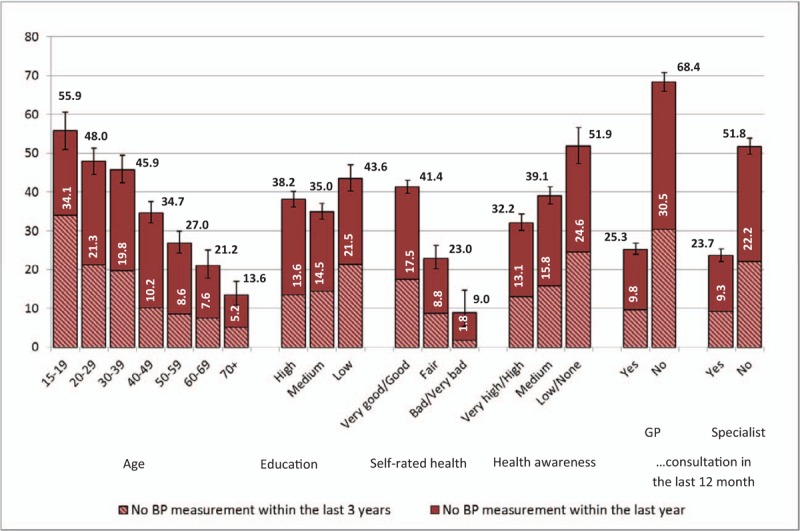
Percentage (% with 95%-CI) of men 15 + years without hypertension (n = 7446) who had no blood pressure measurement by a health professional within the last year or within the last 3 years (GEDA 2014/2015-EHIS data). CI = confidence interval, EHIS = European Health Interview Survey.
Figure 2.
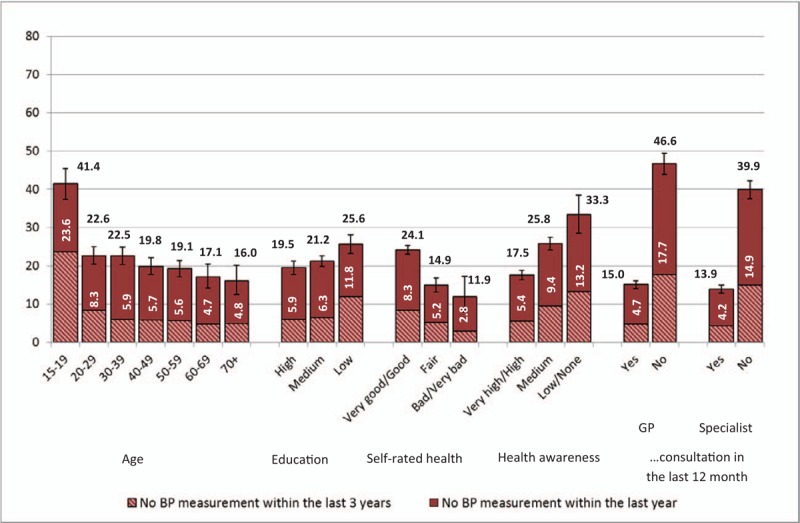
Percentage (% with 95%-CI) of women 15 + years without hypertension (n = 9895) who had no blood pressure measurement by a health professional within the last year or within the last 3 years (GEDA 2014/2015-EHIS data). CI = confidence interval, EHIS = European Health Interview Survey.
For international comparison, we analyzed data from the EHIS to show the percentage of the population with no BP management within the last year and the 3 years in 30 European countries. The data can be openly accessed under http://ec.europa.eu/eurostat/de/data/database.
All analyses were performed using STATA SE14 (StataCorp LP, Texas, US). Weights and survey commands were used to adjust the sample to the German standard population from 31. December 2011 with respect to age, sex, education and regional distribution of the population.[10]
3. Results
In the study population aged 15+ with complete data on hypertension prevalence and BP measurement (n = 24,075), 27.5% of men and 16.6% of women had no BP measurement by a health professional within the last year and 10.9%, respectively 5.4% not within the last 3 years. 7.3% of men and 3.4% of women in the general population had no BP measurement within the last 5 years. The prevalence of known hypertension in the last 12 months was 31.5% in men and 29.9% in women.
The first part of the analysis focused on 17,341 participants without hypertension. The sample characteristics are described in Table 1.
Table 1.
Overview on the GEDA2014–2015-EHIS study population 15+ years without hypertension∗ stratified for men and women (weighted percentages).
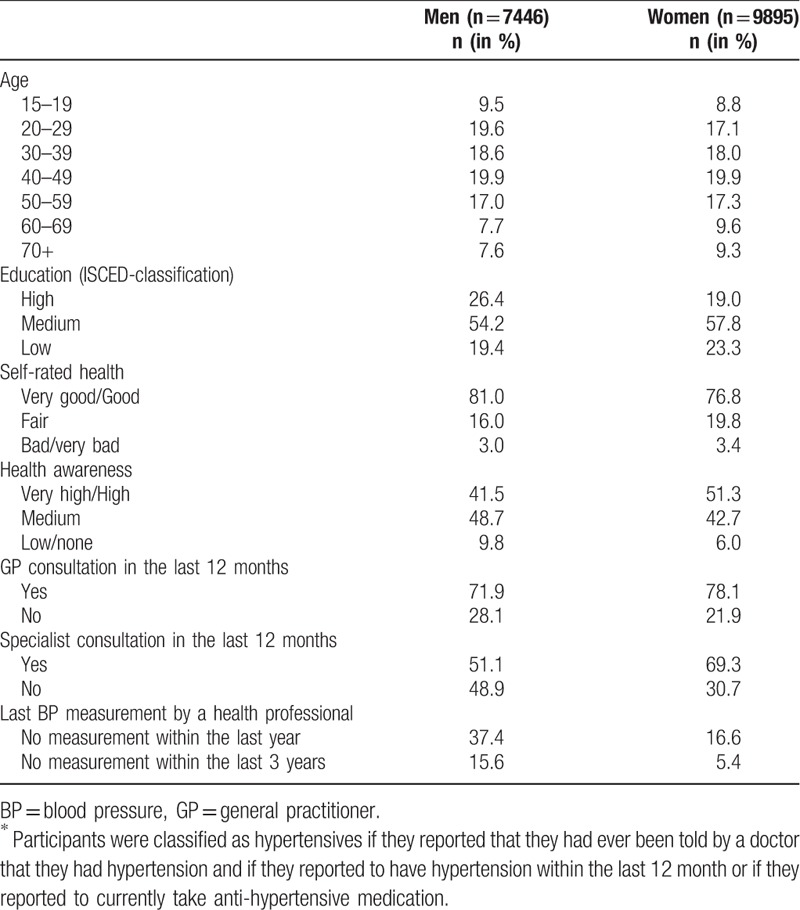
The 37.5% of men and 21.9% of women without hypertension had no BP measurement by a health professional within the last year, and 15.6% of men and 7.6% of women no BP measurement within the last 3 years and 10.6%, respectively 4.8% not within the last 5 years. For all 3 time intervals, the percentage of men with no BP measurement was about 2 times higher compared to women (P <.001).
Figures 1 and 2 show that the percentage of men and women with no BP measurement within the last 3 years was especially high in young individuals between 15 and 19 years (34.1% of men and 23.6% of women) and in individuals who had not visited a GP (30.5% and 17.7%) or a specialist (22.2% and 14.9%) within the last 12 months. No BP measurement within the last 3 years was also common in men (17.5%) with very good or good self-rated health and in men (24.6%) and women (13.2%) who reported low or no health awareness. In contrast, only 1.8% of men and 2.8% women with a bad or very bad self-rated health status and 5.2% of men and 4.8% of women aged 70+ years had no PB measurement within the last 3 years.
The age distribution no BP measurement within the last 5 years resembles the other 2 measurement periods and is not shown in order to maintain the readability of Figure 1 and Figure 2. In the youngest age group from 15 to 19 years, 28.0% of men and 17.4% of women had no BP measurement within the last 5 years. These numbers decreased to 1.3% of men and 0.9% of women aged 70 years and older.
The multivariate model (Fig. 3) showed that age was the strongest predictor for not having a BP measurement in the past 3 years. Compared to older people (70+ years), young individuals had the highest chance not to have their BP measured within the last 3 years (OR for 15–19 years: 6.1; OR for 20–29 years: 2.4 and OR for 30–39 years: 1.9). Furthermore, individuals who had not seen a GP (OR: 3.5) or specialist (OR: 2.1) within the last 12 months were more likely not to have their BP measured. The chance for no BP measurement within the last 3 years was also higher in men (OR: 1.8) and individuals with very good or good self-rated health (OR: 2.9) and those reporting low or no health awareness (OR: 1.9).
Figure 3.
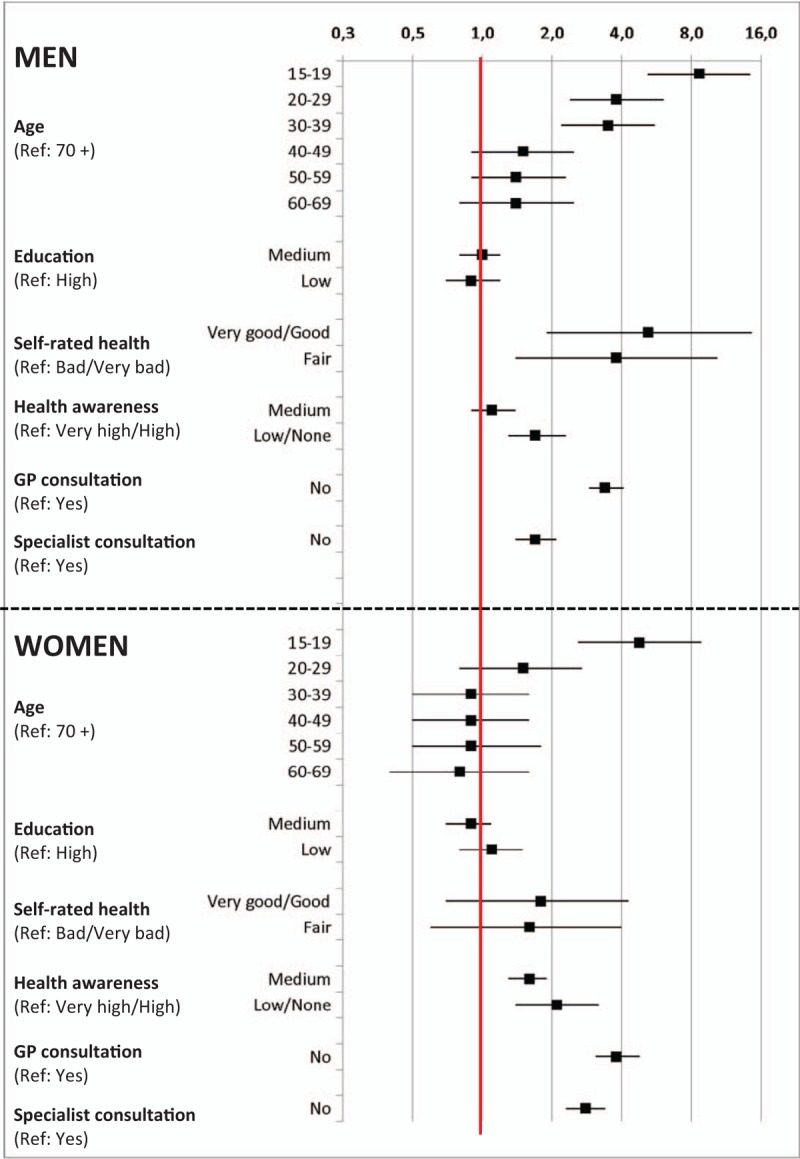
Factors associated with no blood pressure measurement within the last 3 years in individuals 15+ without hypertension (adjusted OR with 95%-CI) on the basis of GEDA 2014/2015-EHIS data. CI = confidence interval, EHIS = European Health Interview Survey, OR = odds ratio.
The second part of the analysis used EHIS data from 30 European countries and refers to the whole population aged 15 years and older, not only to those without hypertension (Figs. 4 and 5). Romania had the highest percentage of individuals with no BP measurement within the last 3 years (66.1% of men and 55.1% of women) and Luxembourg the lowest percentage (24.2% of men and 16.6% of women). Germany ranked third after Luxembourg and France for men and second after Luxembourg for women.
Figure 4.
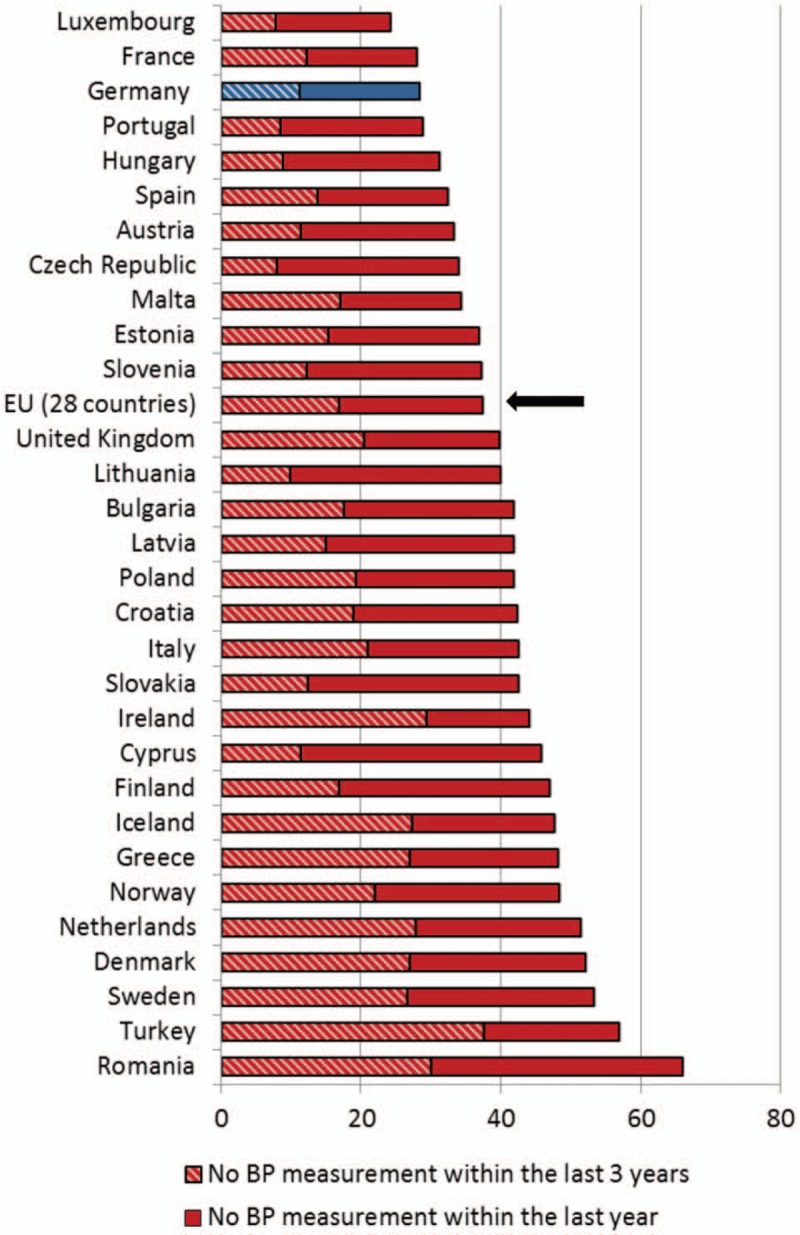
Percentage (%) of men 15+ years who had no blood pressure measurement by a health professional within the last year and the last 3 years in different European countries (EHIS data). EHIS = European Health Interview Survey.
Figure 5.
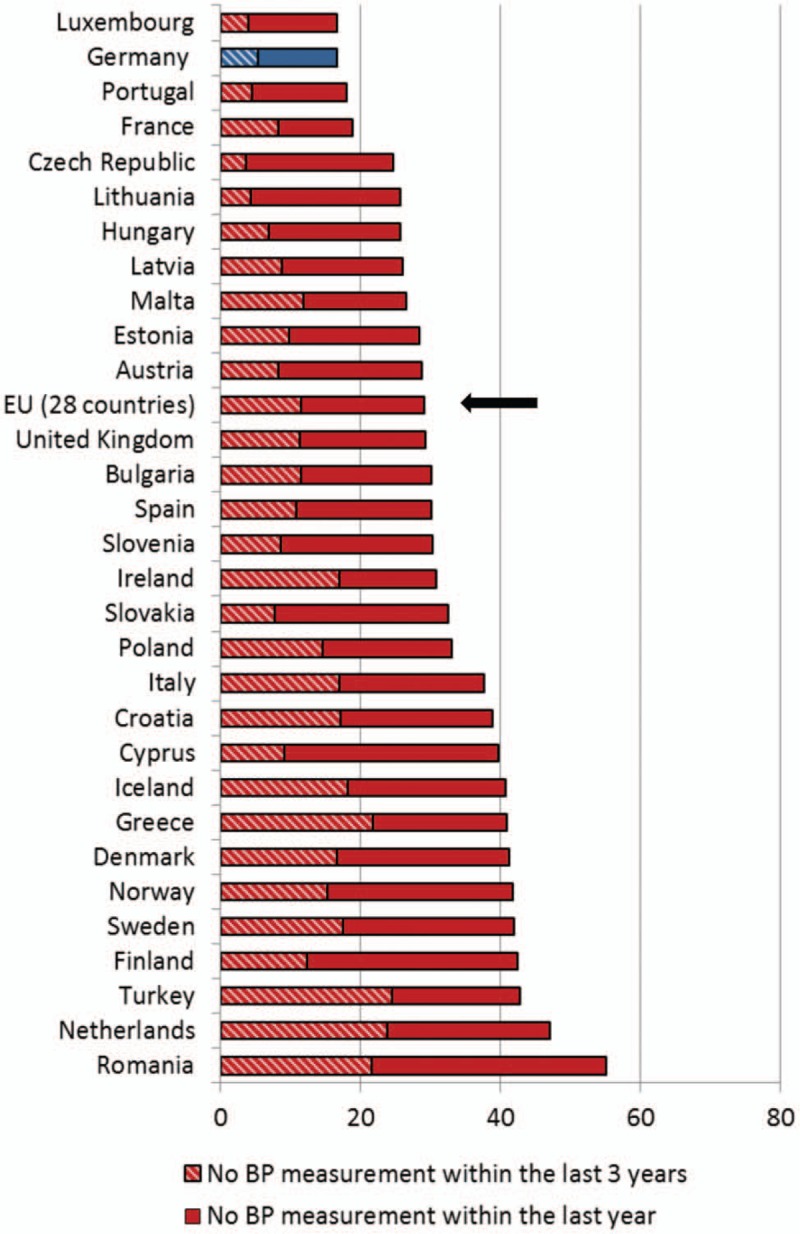
Percentage (%) of women 15+ years who had no blood pressure measurement by a health professional within the last year and the last 3 years in different European countries (EHIS data). EHIS = European Health Interview Survey.
4. Discussion
High BP is a major global risk factor and measurement of BP in all adults for screening purposes is consistently recommended[12,13] as a prerequisite for the detection, treatment, and control of high BP.
Despite the importance of regular PB measurement, the recommended time intervals for BP measurement in the general population are inconsistent and range between at “least every 5 years” in individuals without hypertension in the UK,[14] and “annual screening for adults aged 40 years or older and for those who are at increased risk for high BP” in the US[4] and an assessment of “BP at all appropriate clinical visits” in Canadian adults.[15] The new European Guidelines for the treatment of high BP, which were presented on the European Society of Hypertension meeting in June 2018 and will be soon be published,[13] recommend PB screening every 5 years for individuals with optimal BP (<120/80 mmHg) and at least every year for individuals with high-normal BP (130–139/85–89 mmHg). In addition, resting BP measurement is part of preventive care examinations in Germany covered by the statutory health insurance every 2 years for individuals aged 35+, with an intended lowering of this age limit to 18 years in the recent national Prevention Act.[16]
This analysis shows that in the general population 15+ years in Germany, the majority of men (89.1%) and women (94.6%) had their BP measured by a health professional at least once within the last 3 years. As expected, in individuals without hypertension the frequency of BP measurement was slightly lower (84.4% of men and 92.4% of women within the last 3 years). The comparison with other European countries confirmed the generally high frequency of BP measurement in the office in Germany.
Furthermore, this analysis highlights that in certain population groups the frequency of BP measurement was relatively low. Around 1 in 4 (21.3%–19.8%) young men between 20 to 39 years without a prior diagnose of hypertension had no BP measurement within the last 3 years. In a Canadian study, no BP measurement within the last 2 years was also more common in young individuals between 20 to 39 years (12.3%) and men (12.4%), compared to women (5.9%) and individuals aged 60+ (0.6%).[17] Although the prevalence of hypertension in young men in Germany is relatively low and ranged between 8.5% (18–29 years) and 15.8% (30–44 years), these 2 groups had the highest proportion (76.4%, respectively 37.2%) of undetected raised BP.[7]
Not surprisingly, a GP or specialist consultation within the last 12 months was one of the most important independent predictors for BP measurement (adjusted for age, self-rated health status, and health awareness). Similar results were observed in Canada, where only 6.2% of adults with a regular doctor did not have their BP assessed in the last 2 years, compared to 23.9% without a regular doctor.[17] However, our analysis showed that still 25.3% of men and 15.0% of women had no BP measurement within the last year, although they had seen a GP at least once within this time period. The time to obtain a reliable resting BP in the office, which includes a resting time of 5 to 10 minutes and several measurements[18,19] possibly makes it difficult to always integrate it in routine clinical practice.[20] In the US, BP was measured in 68.4% of all clinic visits in patients aged 18 years or older in 2015.[21]
Furthermore, we found that men with a very good or good self-rated health were less likely to have their BP measured. A similar association was observed in Canada where only 3.3% individuals with a fair or poor health status had no BP measurement within the last 2 years compared to 9.9% with an excellent, very good or good health status.[17]
In summary, especially young men with very good or good self-rated health and who reported low health awareness were most likely not to have a BP measurement. The planned extension of statutory check-ups to all insured persons from the age of 18, which are offered independently of the need to see a GP or specialist, targets this specific population group.[22] However, only 1 quarter of statutory health insurance members aged 35+ (25.9% of women and 23.1% of men) attended the existing medical check-up in 2016[23] and the evidence for the benefits of general health checks to reduce morbidity and mortality from disease[24] are scarce.
One interesting result of our analysis was that education was not associated with BP measurement in our data. This result is in line with results from the US[25] and with a recent German study showing that the utilization of statutory check-ups was not influenced by education.[26] However, it is questionable whether the underlying mechanisms and motives which determine BP measurement in the office, which are rather driven by office procedures or physicians‘ recommendations and can, therefore, be described as “opportunistic”,[27] and the participation in check-ups, where patients have to actively request an appointment, can be compared at all.
4.1. Strengths and weaknesses
A major strength of this analysis is the use of national survey data with a large sample size and standardized questions. Weights were applied to adjust the sample to the German standard population which increased the representativeness of the results. Furthermore, the use of EHIS data made an international comparison possible. However, there are several limitations. The response rates were only moderate and although this has become a common problem in epidemiological studies,[28] this might reduce the generalizability of our findings. In addition, our results do not distinguish between accurate and standardized resting BP taken for preventive screening purposes and quick measurement of BP as a vital sign in acute care situations. Therefore, the high proportion of adults with BP measurements may overestimate BP screening in the sense of long-term cardiovascular prevention. Although the measurements were done by a health professional, we do not know whether and how the BP values were discussed and managed. Unfortunately, we did not have any information about the actual BP level, which is likely to have a major influence of the frequency of PB measurement in the office. However, we excluded persons with a self-reported, physician-diagnosed hypertension and therefore tried to minimize this confounding factor. Other factors that might influence the frequency of BP measurement in certain population groups, such as comorbidities or family history of hypertension, could not be considered in our analysis.
Finally, a general shortcoming of the questionnaire is that it fails to include information on BP measurement at home. A recent American study showed that 87.4% of 18 to 39-year-old individuals had never engaged in home BP measurement[29] and therefore we assume that only a minority of young men without recent BP measurement by a health professional alternatively use home devices. In addition, the term “measured by a health professional” is not further specified and therefore it is not clear whether the study participants considered PB measurement in a pharmacy, or in any other setting, for example, preventive check-ups for athletes, as “done by a health professional”. Although it is not the focus of this research article, it is important to mention that the reliability of BP measurement outside a standardized procedure can be critically questioned.
5. Conclusion
BP screening needs improvement at all ages, in the young who have the lowest screening proportions but also in the elderly who have the highest prevalence of hypertension and overall cardiovascular risk. However, further research is needed to better understand age- and sex-specific barriers to BP screening and to determine the best setting for BP screening.
Acknowledgments
The authors are most thankful to all those who have contributed and worked hard on planning and conducting the study as well as on administration and data management. The authors particularly thank as well the participants of the GEDA2014/2015-EHIS survey, whose participation made this work possible.
Author contributions
Conceptualization: Hannelore Neuhauser.
Formal analysis: Claudia Diederichs.
Methodology: Claudia Diederichs, Hannelore Neuhauser.
Project administration: Hannelore Neuhauser.
Resources: Hannelore Neuhauser.
Writing – original draft: Claudia Diederichs.
Writing – review & editing: Hannelore Neuhauser.
Footnotes
Abbreviations: BP = blood pressure, EHIS = European Health Interview Survey, GP = general practitioner, OR = odds ratio.
The study was approved by The Federal Commissioner for Data Protection and Freedom of Information, and written informed consent was obtained from all participants before the interview.
The study has been financed by the German Ministry of Health (BMG) and by the Robert Koch Institute. The GEDA2014/2015-EHIS survey is part of the health monitoring system of the Robert Koch Institute.
The authors declare no conflicts of interest.
References
- [1].Barnett R. Case histories—hypertension. Lancet 2017;389:2365. [DOI] [PubMed] [Google Scholar]
- [2].Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual BP to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–13. [DOI] [PubMed] [Google Scholar]
- [3].Forounzafar MH, Liu P, Roth GA. Global Burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA 2016;317:165–82. [DOI] [PubMed] [Google Scholar]
- [4].Siu A on behalf of the US preventive services task force. Screening for high BP in adults: U.S. Preventive services task force recommendation statement. Ann Intern Med 2015;163:778–86. [DOI] [PubMed] [Google Scholar]
- [5].Ettehad D, Emdin CA, Kiran A, et al. BP lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957–67. [DOI] [PubMed] [Google Scholar]
- [6].Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-Income countries. JAMA 2013;310:959–68. [DOI] [PubMed] [Google Scholar]
- [7].Neuhauser HK, Adler, Rosario AS, et al. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008-11. J Hum Hypertens 2015;29:1–7. [DOI] [PubMed] [Google Scholar]
- [8].Kurth BM, Lange C, Kamtsiuris P, et al. Gesundheitsmonitoring am Robert Koch-Institut: Sachstand und Perspektiven. Bundesgesundheitsbl 2009;52:557–70. [DOI] [PubMed] [Google Scholar]
- [9].Lange C, Finger JD, Allen J, et al. German Health Update (GEDA) 2014/2015: design, objectives and implementation of the European Health Interview Survey (EHIS) in Germany. Arch Publ Health 2017;75:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Saß AC, Lange C, Finger JD, et al. German health update: new data for Germany and Europe. The background to and methodology applied in GEDA 2014/2015-EHIS. JoHM 2017;2:75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Neuhauser H, Kuhnert R, Born S. 12-Monats-Prävalenz von Bluthochdruck in Deutschland. JoHM 2017;2:57–63. [Google Scholar]
- [12].Sheridan S, Pignone M, Donahue K. Screening for high blood pressure: a review of the evidence for the U.S. Preventive Services Task Force. Am J Prev Med 2003;25:151–8. [DOI] [PubMed] [Google Scholar]
- [13].Williams B, Mancia G, Spiering W, et al. 2018 European Society of Cardiology (ESC) and European Society of Hypertension (ESH) joint guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021–104. [DOI] [PubMed] [Google Scholar]
- [14].National Institute for Health and Care Excellence (NICE). Hypertension in adults: diagnosis and management. Clinical Guideline 127. NICE 2011. Available at: https://www.nice.org.uk/guidance/cg127 Accessed June 5, 2018. [Google Scholar]
- [15].Leung A, Daskalolpoulou SS, Dasqupta L, et al. Hypertension Canada's 2017 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults. CJC 2017;33:557–76. [DOI] [PubMed] [Google Scholar]
- [16].Bundesministerium für Gesundheit 2017. Gesundheits-Check-up. Available at: https://www.bundesgesundheitsministerium.de/themen/krankenversicherung/online-ratgeber-krankenversicherung/medizinische-versorgung-und-leistungen-der-krankenversicherung/gesundheits-check-up.html Accessed December 21, 2017. [Google Scholar]
- [17].Amankwah E, Campbell NRC, Maxwell C, et al. Why some adult Canadians do not have BP measured. J Clin Hypertens 2007;9:944–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sala C, Santin A, Rescaldani M, et al. How long shall the patient rest before clinic BP measurement. Am J Hypertens 2006;19:713–7. [DOI] [PubMed] [Google Scholar]
- [19].Nikolic SB, Abhayaratna WP, Leano R, et al. Waiting a few extra minutes before measuring blood pressure has potentially important clinical and research ramifications. J Hum Hypertens 2014;28:56–61. [DOI] [PubMed] [Google Scholar]
- [20].Myers M, Godwin M, Dawes M, et al. Measurement of BP in the office recognizing the problem and proposing the solution. Hypertens 2010;55:195–200. [DOI] [PubMed] [Google Scholar]
- [21].National Center for Health Statistics. National Ambulatory Medical Care Survey: 2015 State and National Summary Tables. Available at: https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2015_namcs_web_tables.pdf Accessed January 5, 2017. [Google Scholar]
- [22].Bundestag, 2017. Gesetz zur Stärkung der Gesundheitsförderung und Prävention (PrävG). Available at: http://www.nakos.de/data/Andere/2015/PraevG-Bundesgesetzblatt.pdf Accessed December 21, 2017. [Google Scholar]
- [23].Gesundheitsberichterstattung des Bundes. Indikator 7.17 des Indikatorensatzes der GBE der Länder: Teilnahme am gesetzlichen Gesundheits-Check-up (Anzahl der Anspruchsberechtigten und Inanspruchnahme in %) nach Geschlecht (ab 35 Jahre), Deutschland, ab 2007/2008. Available at: http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=26544573&nummer=779&p_sprache=E&p_indsp=28681124&p_aid=61950116 Accessed June 5, 2018. [Google Scholar]
- [24].Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, et al. General health checks in adults for reducing morbidity and mortality from disease. BMJ 2012;345:e7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Robbins CL, Dietz PM, Bombard JM, et al. Blood pressure and cholesterol screening prevalence among U.S. women of reproductive age opportunities to improve screening. Am J Prev Med 2011;41:588–659. [DOI] [PubMed] [Google Scholar]
- [26].Hoebel J, Starker A, Jordan S, et al. Determinants of health check attendance in adults: findings from the cross-sectional German Health Update (GEDA) study. BMC Publ Health 2014;14:913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Piper MA, Evans CV, Burda BU, et al. Screening for high BP in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Evidence Synthesis. 2014, Number 121. AHRQ Publication No. 13-05194-EF-1. [PubMed] [Google Scholar]
- [28].Galea S, Tracy M. Participation rates in epidemiological studies. Ann Epidemiol 2007;17:643–53. [DOI] [PubMed] [Google Scholar]
- [29].Ostchega Y, Zhang G, Kit BK, et al. Factors associated with home blood pressure monitoring among US adults: national health and nutrition examination survey, 2011–2014. Am J Hypertens 2017;30:1126–32. [DOI] [PMC free article] [PubMed] [Google Scholar]


