Supplemental Digital Content is available in the text
Keywords: factor analysis, postmenopause, randomized controlled trials, statistical, stress, urinary incontinence, women
Abstract
Postmenopausal women are at a higher risk of stress urinary incontinence (SUI). In a previous trial, electroacupuncture (EA) was shown to be an effective treatment for women with SUI. Here we present a secondary analysis to investigate the specific factors associated with response to acupuncture therapy among postmenopausal women with SUI.
We conducted secondary analysis of data from a multicenter randomized controlled trial. This trial included a baseline period of 1 week and a treatment period of 6 weeks with electroacupuncture (EA) or sham electroacupuncture (SA). The patients were randomly assigned to 2 groups (EA group or SA group). Participants who showed a decrease in urine leakage by at least 50% from baseline level, as measured by 1-hour pad at week 6, were defined as responders. Baseline characteristics associated with response to acupuncture therapy (e.g., demographic, comorbidities, and lifestyle-related factors) were identified by logistic regression analysis and the interactions between treatment assignment and baseline characteristics assessed.
This analysis included a total of 349 postmenopausal women, of whom 137 (39.3%) were classified as responders. Response rate in the EA group was significantly higher than that in the SA group (60.9% vs 18.9%, respectively; P < .001). On multivariable logistic regression analysis, only “mean number of urine pads used before treatment” remained a significant predictor of response to therapy (EA or SA). Greater weekly mean number of urine pads used before treatment showed a correlation with non-response to therapy, as the likelihood of clinical response reduced by 5.26% with increase in the weekly mean number of urine pads used (odds ratio 0.947, 95% confidence interval 0.902–0.993; P = .020). The interaction terms were not statistically significant.
Postmenopausal women with SUI who used fewer number of pads per week before treatment were more likely to respond to therapy. This study provides valuable insights for pretreatment selection of women with SUI. Specific factors related to the therapeutic effects of acupuncture were not identified and need to be explored in future studies.
Trial registration: Clinical Trials.gov: NCT01784172.
1. Introduction
Stress urinary incontinence (SUI) is characterized by involuntary loss of urine on effort, exertion, sneezing, or cough.[1] SUI adversely affects the quality of life of the afflicted individual. According to the American College of Obstetricians and Gynecologists, more than 25% young women and 44% to 57% of middle-aged and postmenopausal women experience symptoms of SUI.[2] Estrogen deficiency has been implicated in the causation of SUI in postmenopausal women; in addition, urinary incontinence was shown to be one of the main pelvic floor diseases in postmenopausal women.[3] Therefore, there is a close connection between SUI and postmenopausal women.[4] Moreover, several factors such as age, body mass index (BMI), and the manner of child delivery are known to affect the development and progression of SUI.[5]
Acupuncture has recently been shown to be an effective therapy for pelvic floor dysfunction.[6] In our previous study, postmenopausal women (n = 349) were administered 28 sessions of acupuncture or sham acupuncture treatment over a period of 8 weeks;[7] the results demonstrated the efficacy of acupuncture for treatment of SUI in women. Since the study primarily focused on the efficacy of acupuncture, the correlation between patient characteristics and therapeutic effects of acupuncture was not specifically examined in the primary study. Some recent studies have sought to identify patients that are more likely to benefit from acupuncture by investigating specific factors that influence the response to acupuncture therapy.[8] Therefore, it is worthwhile to identify the factors that influence the response of postmenopausal women with SUI to acupuncture therapy.
In the present study, we performed a post-hoc secondary analysis of data pertaining to 349 post-menopausal women in the study cohort. The objective was to identify factors that may affect the response to acupuncture therapy in postmenopausal women with SUI.
2. Methods
2.1. Summary of original research
We provide a brief outline of the protocol of our published clinical trial[7] (See Supplemental Digital Content 1). The multicenter, randomized, controlled trial was performed at 12 Chinese hospitals from October 2013 to May 2015. The trial consisted of a baseline period of 1 week, a treatment period of 6 weeks with electroacupuncture (EA) or sham electroacupuncture (SA), and 2 follow-up visits (without any treatment) at 12 weeks and 24 weeks. A block randomization scheme (block size: six per site based on a random table) stratified by center was used to randomly assign patients to the EA group or the SA group. The details of group identity of the participants were signed and placed in a sealed cover by the researcher who performed group allocation and kept by other staff who did not participate in this trial. Acupuncturists at each center obtained the random numbers by inputting the participant's sex and date of birth in the central randomization system through a phone or web-based interface. A total of 504 women were enrolled in this RCT until May 2015: the EA group included 252 women and the SE group included 252 women. A total of 482 women continued till week 6 while 22 women dropped out during the trial. Out of the 504 women, 349 had attained menopause. Menopause is defined as a retrospective concept and refers to the period starting 12 months after a woman's last menstruation; the average age at menopause is 51.3 years.[9] The primary outcome of this trial was the change in the amount of urine leakage from baseline levels, as measured by the 1-hour pad test at week 6. The secondary outcomes were: change from baseline in the amount of urine leakage at week 2; 72-hour incontinence episode frequency measured during weeks 1 to 6, 15 to 18, and 27 to 30; proportion of participants with at least 50% decrease in the amount of urine leakage from baseline level as measured by 1-hour pad at week 6 and the mean 72-hour incontinence episodes during weeks 1 to 6, 15 to 18, and 27 to 30; severity of SUI in postmenopausal women during weeks 1 to 6, 15 to18, and 27 to 30; change from baseline in the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF, Chinese version) scores and the participants’ self-evaluation of therapeutic effects at weeks 6, 18, and 30; the number of urine pads used; and other treatments for SUI during weeks 1 to 6, 7 to 18, and 19 to 30. Adverse events were also monitored throughout the trial.
The trial was performed in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. This trial was approved by the Ethics Committee (See Supplemental Digital Content 2); written informed consent was obtained from all patients after detailed counseling. The Clinical Trials Government Identifier number is NCT01784172.
2.2. Secondary analysis design
We compared the response rate of postmenopausal women with SUI in the EA and SA groups. Participants who showed at least 50% decrease in the amount of urine leakage from baseline level, as measured by 1-hour pad at week 6 were defined as responders.[10–12] The amount of urine leakage during the 1-week screening period, as measured by1-hour pad, was defined as the baseline level.
We also assessed the association between baseline characteristics and the response to acupuncture therapy. Baseline demographic characteristics and some clinical indicators related to postmenopausal women were collected using a questionnaire and also included in the analysis. The baseline demographic characteristics included age, gender, race, educational level, manner of child delivery, and BMI. Clinical indicators included the duration of SUI, coexisting diseases other than SUI (including cardiovascular and cerebrovascular diseases, osteoarthritis, respiratory diseases, metabolic disorders, or other diseases), severity of SUI (classified based on the amount of urine leakage, as measured by the 1-hour pad test: mild, 1.1–9.9 g; moderate, 10–49.9 g; severe, ≥50 g), amount of urine leakage as measured by the 1-hour pad test, 72-hour incontinence episode frequency (IEF), ICIQ-SF score, previous treatment for SUI within 2-weeks (including pelvic floor muscle training, medicine, acupuncture, lifestyle interventions), weekly mean number of urine pads used, and 24-hour liquid intake.
2.3. Statistical analysis
Descriptive statistics were used for demographic and other baseline characteristics. Variables that showed a significant association with therapeutic response on univariate analysis (P < .25)[13] were included in the multivariable logistic regression model to assess their interaction with treatment assignment. Using 1000 bootstrap samples, backward elimination as variable selection strategy was used to retain independent variables in the final model.[14] To counter the problem of overfitting associated with automated modeling, we applied bootstrapping technique to adjust for overfitting with respect to the measures in the prediction model. In addition, the area under the ROC curve (AUC) was used to assess predictive discrimination; the higher the AUC value, the better is the prediction power of the model. Bootstrapping is a powerful approach that involves repeated sampling from the original dataset to form many bootstrap datasets that are of the same size as the original dataset. Prior to the regression analyses, variance inflation factor (VIF) was used to detect multicollinearity among the independent variables. Multicollinearity was considered if the VIFs for one of the variables were greater than 5.
Since the analyses were exploratory, 2-sided P values were assessed at a significance level of.05 without adjustment for multiplicity. All statistical tests were performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and R 3.4.1 (R Project for Statistical Computing, Vienna, Austria).
3. Results
3.1. Response rate among postmenopausal women with SUI
A total of 349 postmenopausal women were randomly allocated to the EA group or SA group; of these 137 (39.3%) were classified as responders. Figure 1 shows the response rates of postmenopausal women with SUI at week 2 and week 6. The between-group difference with respect to response rate was statistically significant at week 2 and week 6 (P < .01). Importantly, the response rates in the EA group were approximately 1.70 and 3.05 times higher than that in the SA group at weeks 2 and 6, respectively.
Figure 1.
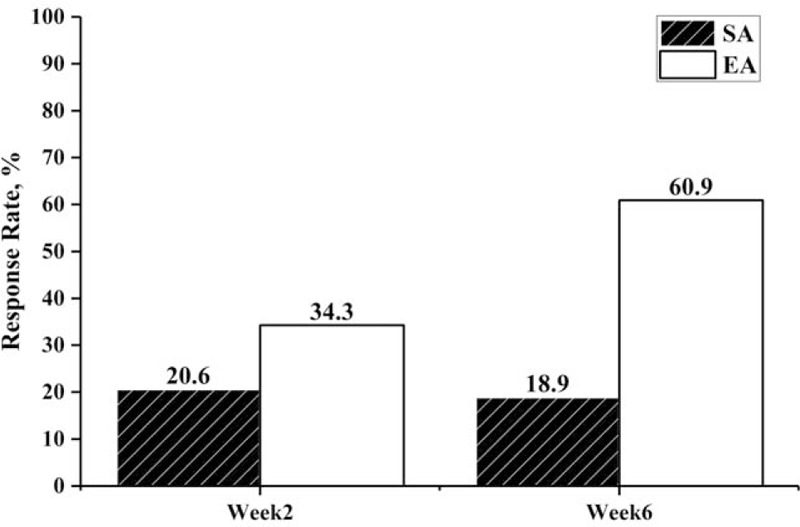
Response rate in EA and SA groups at week 2 and week 6.
3.2. Results of logistic regression analysis
Table 1 shows the baseline characteristics of the responders. Seventeen factors (9 candidate variables and 8 interactions between the candidate variables and treatment assignment) were included in the logistic regression model. In the logistic regression analysis, no significant between-group differences were observed except those with respect to the assigned treatment and the weekly mean number of urine pads used before treatment (Table 2). The odds of responders among postmenopausal women with SUI in the EA group was 6.28 times higher than that in the SA group [odds ratio (OR) 6.280, 95% confidence interval (CI) 5.752 to 6.808; P < .001]. Patients who used more urine pads per week were approximately 5.26% less likely to respond to therapy (EA or SA) as compared to patients who used fewer number of urine pads per week (OR 0.947, 95% CI 0.902 to 0.993; P = .020). Therefore, postmenopausal women with SUI who used fewer urine pads in a week showed better response to therapy (EA or SA) when compared with those who used more urine pads in a week. Moreover, the interaction terms between treatment assignment and the key baseline factors did not make it to the final model.
Table 1.
Demographic and clinical characteristics of responders∗.
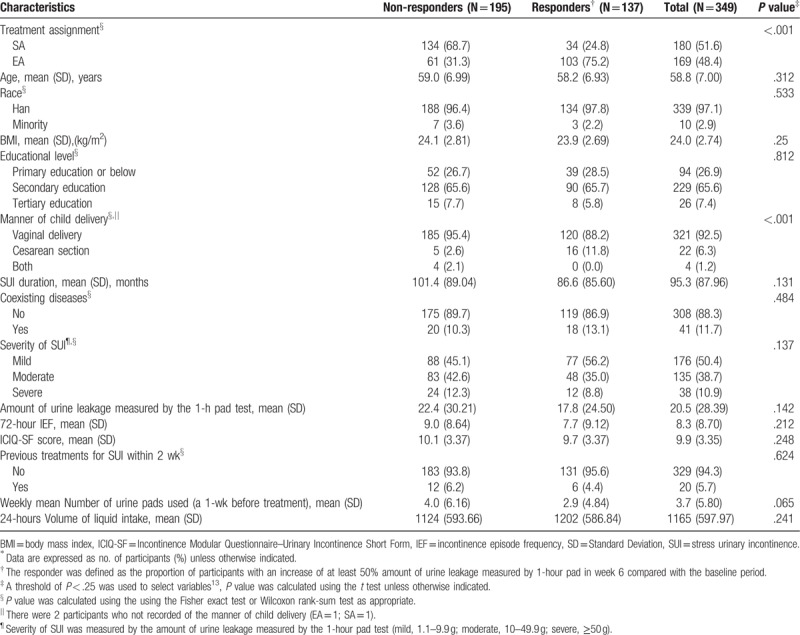
Table 2.
Backward logistic regression with bootstrap method.
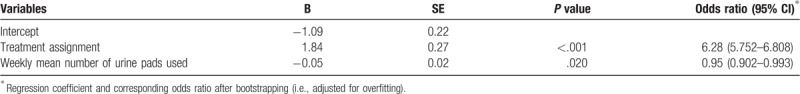
No multicollinearity was observed among these predictor variables and the dependent variables (VIFs < 1.5). After adjustment for overfitting using bootstrap techniques, the area under the ROC curve of the final model was 0.71 (overfitting 0.0726). Table 2 (columns 2 and 5) shows the regression coefficients and odds ratios per predictor adjusted for overfitting (i.e., after bootstrapping).
4. Discussion
This secondary analysis of a RCT showed that the mean number of urine pads used per week was the underlying factor associated with response to therapy (EA or SA) for postmenopausal women with SUI. There were no specific factors related to the response to acupuncture among postmenopausal women with SUI. Postmenopausal women with SUI who used fewer urine pads per week had higher response rates. Factors such as age, gender, race, educational level, manner of child delivery, BMI, duration of SUI, coexisting diseases apart from SUI, severity of SUI, amount of urine leakage measured by the 1-hour pad test, 72-hour IEF, ICIQ-SF score, previous treatment for SUI within 2 weeks, weekly mean number of urine pads used, and 24-hour liquid intake showed no significant association with acupuncture response.
In a study by Aksac et al, at least 50% decrease in wet weight of leaked urine from the baseline level, as measured by the 1-hour pad test, was considered indicative of improvement.[10] In another RCT that compared 3 different non-operative techniques for treatment of SUI using objective means, >50% decrease in pad weights was considered indicative of a significant improvement.[11] Moreover, a decrease in urine leakage by a minimum of 50% from baseline level, measured by 1-hour pad test, was used as the criterion for improvement in our previous study;[12] the study showed that EA may effectively and safely relieve urinary incontinence symptoms and improve the quality of life of postmenopausal women with SUI. Based on these previous studies, we used the same criteria in the present study to determine clinically meaningful response among women with SUI. In our trial, the response rate in the EA and SE groups were different at week 6 (60.9% and 18.9%, respectively, P = .02). In a clinical trial conducted in 2003, the response rate of treatment with PFMT and PFMT plus biofeedback was 20% and 25%, respectively, as compared to 20% in the control group (no intervention).[10] In our trial, we used a blunt-tipped placebo needle which is similar in appearance to the conventional needles.[8] In addition, this placebo needle did not penetrate the skin and it was connected with a broken inner cord; However, some systemic selection bias cannot be ruled out as this analysis is based on data extracted from a RCT. These results suggest that postmenopausal women with SUI were more likely to show a favorable response to EA than SA during the treatment period. However, another study conducted in 2003 found no difference between the acupuncture and placebo arms.[15] So some specific factors may influence the response to acupuncture therapy. It is necessary to further explore additional correlates of the response to acupuncture and to identify patients who are more likely to benefit from acupuncture.
A few trials have employed the weekly number of urine pads as a primary outcome. Some trials suggest that the number of urine pads used is not an objective measure to assess the risk and severity of urinary incontinence.[16] However, our analysis suggests that participants who used fewer urine pads per week were more likely to be responders than participants who used more number of urine pads. A study reported that older patients have higher per-pad leakage.[17] It can be inferred that the more the weekly number of urine pads used, the worse is the severity of SUI among postmenopausal women. This explains the better response to therapy among postmenopausal women with SUI who used fewer number of urine pads per week. Another potential explanation is that more frequent change of urine pads may be attributable to other medical and non-medical reasons unrelated to the severity of incontinence.[18] Additionally, many trials have used 24-hour pad tests to explore the correlation between the count of urine pads and the severity of urinary incontinence while we used the 1-hour pad test in our trial. We need to use 1-hour pad test to explore the correlation between the count of urine pads and the severity of urinary continence and to better explore the correlation between the counts of urine pads and postmenopausal women with SUI in further analysis.
Luber et al reported that sex, race, childbirth, obesity, constipation, age, or other variables may be potential risk factors related to SUI.[19] Some recent studies also found that age, manner of child delivery, BMI, and other clinical factors may influence the therapeutic response among women with SUI.[20] According to a study, women who had undergone vaginal deliveries are at a higher risk of urinary incontinence.[21] This is likely attributable to direct injury to vaginal wall, pelvic floor muscles and nerves during vaginal delivery.[18] Also, obesity is commonly reported as a risk factor for development and recurrence of SUI in women. Obesity may increase the intra-abdominal pressure in women with SUI.[22] Some coexisting diseases such as constipation and respiratory diseases which are associated with increased abdominal pressure have also been shown to cause SUI.[5,23,24] With the exception of weekly number of urine pads used, none of the other factors showed a significant difference between the responders and non-responders. In other words, our study did not identify other specific factors that may have influenced the efficacy of acupuncture therapy. These clinical factors were also significantly different between responders and non-responders before logistic regression analysis. The lack of statistical significance observed on logistic regression analysis may be explained by the relatively small sample size in this analysis, which was based on data extracted from a RCT. Based on our findings, future studies are required to confirm the factors associated with response to acupuncture therapy among postmenopausal women with SUI.
Since only postmenopausal women with SUI were included in this analysis, it led to a relatively small sample size. For the same reason, we only employed the weekly number of urine pads as a parameter of response to therapy (EA or SA) and did not explore other factors related to response. Therefore, further studies should explore specific factors related to response to acupuncture therapy and include more factors to facilitate better patient selection for acupuncture therapy among postmenopausal women with SUI.
There are some limitations of this secondary analysis. This data was extracted from a RCT; therefore, the sample size in this study was relatively small, which is the main limitation. In addition, owing to the limited demographic factors or use of only 1 threshold of responder, some potential risk factors may not have been captured in this analysis. Further, the use of fixed block randomization may have introduced an element of selection bias where in the patients are able to predict the next allocation. Second, according to the data of our previous trial, other factors such as psychologic factors were not reported.[18] Final, since the study population comprised of Chinese patients, these conclusions may not entirely be applicable to postmenopausal women with SUI in other countries.
5. Conclusion
In this study, postmenopausal women with SUI showed a superior response to EA as compared to SA during the treatment period of 6 weeks. Postmenopausal women with SUI who used a fewer number of pads per week before treatment might be more responsive to therapy (EA or SA). However, the specific factors related to response to acupuncture therapy among postmenopausal women with SUI were not found and need to be explored in future studies.
Acknowledgments
We thank the doctors, subjects, and other researchers participating in the original clinical trial for use of the data.
Author contributions
ZL and YL contributed to the conception of this study. ZL and BL contributed the data of this study. RJ and YL drafted the manuscript. Data synthesis was completed by YL. ZL revised this manuscript. All authors approved the final manuscript.
Conceptualization: Yan Liu, Zhishun Liu.
Data curation: Ruimin Jiao, Yan Liu.
Formal analysis: Ruimin Jiao.
Investigation: Baoyan Liu, Zhishun Liu.
Software: Yan Liu.
Supervision: Baoyan Liu, Zhishun Liu.
Validation: Baoyan Liu, Zhishun Liu.
Writing – original draft: Ruimin Jiao, Yan Liu.
Writing – review & editing: Ruimin Jiao, Yan Liu, Zhishun Liu.
Zhishun Liu orcid: 0000-0001-7570-8917.
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: BMI = body mass index, EA = electroacupuncture, ICIQ-SF = Incontinence Modular Questionnaire–Urinary Incontinence Short Form, IEF = incontinence episode frequency, RCT = Randomized controlled trial, SA = sham electroacupuncture, SUI = stress urinary incontinence, SUI = stress urinary incontinence.
Ruimin Jiao and Yan Liu are the cofirst authors of this study.
Owing to patient privacy, the data acquired is available from the Committee of Data management of acupuncture of Twelfth Five-Year National Science and Technology Pillar Program (via email: amreg@ndctcm.cn).
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Kobashi KC, Albo ME, Dmochowski RR, et al. Surgical treatment of female stress urinary incontinence: AUA/SUFU guideline. J Urol 2017;198. [DOI] [PubMed] [Google Scholar]
- [2].Morantz CA. ACOG guidelines on urinary incontinence in women. Eur Urol 2005;37:1118–29. 1129. [Google Scholar]
- [3].Perrotta C, Aznar M, Mejia R, et al. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Obstet Gynecol 2008;112:689–90. [DOI] [PubMed] [Google Scholar]
- [4].Fritel X, Ringa V, Quiboeuf E, et al. Female urinary incontinence, from pregnancy to menopause: a review of epidemiological and pathophysiological findings. Acta Obstet Gynecol Scand 2012;91:901–10. [DOI] [PubMed] [Google Scholar]
- [5].Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Rev Urol 2004;6Suppl 3:S3–13. [PMC free article] [PubMed] [Google Scholar]
- [6].Frank LP. Acupuncture for pelvic floor dysfunction. Springer London 2008;263–5. [Google Scholar]
- [7].Liu Z, Liu Y, Xu H, et al. Effect of electroacupuncture on urinary leakage among women with stress urinary incontinence: a randomized clinical trial. JAMA 2017;317:2493–12493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Shi GX, Yang XM, Liu CZ, et al. Factors contributing to therapeutic effects evaluated in acupuncture clinical trials. Trials 2012;13:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Grossman DC, Curry SJ, Owens DK, et al. Hormone therapy for the primary prevention of chronic conditions in postmenopausal women: US preventive services task force recommendation statement. JAMA 2017;318:2224. [DOI] [PubMed] [Google Scholar]
- [10].Aksac B, Aki S, Karan A, et al. Biofeedback and pelvic floor exercises for the rehabilitation of urinary stress incontinence. Gynecol Obstet Invest 2003;56:23–7. [DOI] [PubMed] [Google Scholar]
- [11].Hou JC, Lemack GE. Non-operative methods in the treatment of female genuine stress incontinence of urine. J Obstet Gynaecol 2009;9:222–5. [Google Scholar]
- [12].Wang W, Liu Y, Sun S, et al. Electroacupuncture for postmenopausal women with stress urinary incontinence: secondary analysis of a randomized controlled trial. World J Urol 2018;1–7. [DOI] [PubMed] [Google Scholar]
- [13].Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989;130:125–37. [DOI] [PubMed] [Google Scholar]
- [14].Helmreich JE. Regression modeling strategies with applications to linear models, logistic and ordinal regression and survival analysis (2nd edition). J Stat Softw 2016;070. [Google Scholar]
- [15].Colquhoun D, Novella SP. Acupuncture is theatrical placebo. Anesth Analg 2013;116:1360–3. [DOI] [PubMed] [Google Scholar]
- [16].Jackson RA, Vittinghoff E, Kanaya AM, et al. Urinary incontinence in elderly women: findings from the Health, Aging, and Body Composition Study. Obstet Gynecol 2004;104:301–7. [DOI] [PubMed] [Google Scholar]
- [17].Dylewski DA, Jamison MG, Borawski KM, et al. A statistical comparison of pad numbers versus pad weights in the quantification of urinary incontinence. Neurourol Urodyn 2007;26:3–7. [DOI] [PubMed] [Google Scholar]
- [18].Ghanaat M, Tsui J, Blaivas J, et al. 1156 does pad usage reflect the severity of urinary incontinence. J Urol 2011;185:e464–1464. e464-464. [Google Scholar]
- [19].Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Rev Urol 2004;6Suppl 3:S3. [PMC free article] [PubMed] [Google Scholar]
- [20].Oh SJ, Hong SK, Son H, et al. Quality of life and disease severity in Korean women with stress urinary incontinence. Urology 2005;66:69–73. [DOI] [PubMed] [Google Scholar]
- [21].Viktrup L. Female stress and urge incontinence in family practice: insight into the lower urinary tract. Int J Clin Pract 2002;56:694–700. [PubMed] [Google Scholar]
- [22].Cummings JM, Rodning CB. Urinary stress incontinence among obese women: review of pathophysiology therapy. Int Urogynecol J Pelvic Floor Dysfunct 2000;11:41–4. [DOI] [PubMed] [Google Scholar]
- [23].Karantanis E, Fynes M, Moore KH, et al. Comparison of the ICIQ-SF and 24-hour pad test with other measures for evaluating the severity of urodynamic stress incontinence. Int Urogynecol J 2004;15:111–6. [DOI] [PubMed] [Google Scholar]
- [24].Yalcin I, Peng G, Viktrup L, et al. Reductions in stress urinary incontinence episodes: what is clinically important for women. Neurourol Urodyn 2010;29:344–7. 347. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


