Abstract
Background
Chronic peripheral joint pain due to osteoarthritis (OA) is extremely prevalent and a major cause of physical dysfunction and psychosocial distress. Exercise is recommended to reduce joint pain and improve physical function, but the effect of exercise on psychosocial function (health beliefs, depression, anxiety and quality of life) in this population is unknown.
Objectives
To improve our understanding of the complex inter‐relationship between pain, psychosocial effects, physical function and exercise.
Search methods
Review authors searched 23 clinical, public health, psychology and social care databases and 25 other relevant resources including trials registers up to March 2016. We checked reference lists of included studies for relevant studies. We contacted key experts about unpublished studies.
Selection criteria
To be included in the quantitative synthesis, studies had to be randomised controlled trials of land‐ or water‐based exercise programmes compared with a control group consisting of no treatment or non‐exercise intervention (such as medication, patient education) that measured either pain or function and at least one psychosocial outcome (self‐efficacy, depression, anxiety, quality of life). Participants had to be aged 45 years or older, with a clinical diagnosis of OA (as defined by the study) or self‐reported chronic hip or knee (or both) pain (defined as more than six months' duration).
To be included in the qualitative synthesis, studies had to have reported people's opinions and experiences of exercise‐based programmes (e.g. their views, understanding, experiences and beliefs about the utility of exercise in the management of chronic pain/OA).
Data collection and analysis
We used standard methodology recommended by Cochrane for the quantitative analysis. For the qualitative analysis, we extracted verbatim quotes from study participants and synthesised studies of patients' views using framework synthesis. We then conducted an integrative review, synthesising the quantitative and qualitative data together.
Main results
Twenty‐one trials (2372 participants) met the inclusion criteria for quantitative synthesis. There were large variations in the exercise programme's content, mode of delivery, frequency and duration, participant's symptoms, duration of symptoms, outcomes measured, methodological quality and reporting. Comparator groups were varied and included normal care; education; and attention controls such as home visits, sham gel and wait list controls. Risk of bias was high in one and unclear risk in five studies regarding the randomisation process, high for 11 studies regarding allocation concealment, high for all 21 studies regarding blinding, and high for three studies and unclear for five studies regarding attrition. Studies did not provide information on adverse effects.
There was moderate quality evidence that exercise reduced pain by an absolute percent reduction of 6% (95% confidence interval (CI) ‐9% to ‐4%, (9 studies, 1058 participants), equivalent to reducing (improving) pain by 1.25 points from 6.5 to 5.3 on a 0 to 20 scale and moderate quality evidence that exercise improved physical function by an absolute percent of 5.6% (95% CI ‐7.6% to 2.0%; standardised mean difference (SMD) ‐0.27, 95% CI ‐0.37 to ‐0.17, equivalent to reducing (improving) WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) function on a 0 to 100 scale from 49.9 to 44.3) (13 studies, 1599 participants)). Self‐efficacy was increased by an absolute percent of 1.66% (95% CI 1.08% to 2.20%), although evidence was low quality (SMD 0.46, 95% CI 0.34 to 0.58, equivalent to improving the ExBeliefs score on a 17 to 85 scale from 64.3 to 65.4), with small benefits for depression from moderate quality evidence indicating an absolute percent reduction of 2.4% (95% CI ‐0.47% to 0.5%) (SMD ‐0.16, 95% CI ‐0.29 to ‐0.02, equivalent to improving depression measured using HADS (Hospital Anxiety and Depression Scale) on a 0 to 21 scale from 3.5 to 3.0) but no clinically or statistically significant effect on anxiety (SMD ‐0.11, 95% CI ‐0.26 to 0.05, 2% absolute improvement, 95% CI ‐5% to 1% equivalent to improving HADS anxiety on a 0 to 21 scale from 5.8 to 5.4; moderate quality evidence). Five studies measured the effect of exercise on health‐related quality of life using the 36‐item Short Form (SF‐36) with statistically significant benefits for social function, increasing it by an absolute percent of 7.9% (95% CI 4.1% to 11.6%), equivalent to increasing SF‐36 social function on a 0 to 100 scale from 73.6 to 81.5, although the evidence was low quality. Evidence was downgraded due to heterogeneity of measures, limitations with blinding and lack of detail regarding interventions. For 20/21 studies, there was a high risk of bias with blinding as participants self‐reported and were not blinded to their participation in an exercise intervention.
Twelve studies (with 6 to 29 participants) met inclusion criteria for qualitative synthesis. Their methodological rigour and quality was generally good. From the patients' perspectives, ways to improve the delivery of exercise interventions included: provide better information and advice about the safety and value of exercise; provide exercise tailored to individual's preferences, abilities and needs; challenge inappropriate health beliefs and provide better support.
An integrative review, which compared the findings from quantitative trials with low risk of bias and the implications derived from the high‐quality studies in the qualitative synthesis, confirmed the importance of these implications.
Authors' conclusions
Chronic hip and knee pain affects all domains of people's lives. People's beliefs about chronic pain shape their attitudes and behaviours about how to manage their pain. People are confused about the cause of their pain, and bewildered by its variability and randomness. Without adequate information and advice from healthcare professionals, people do not know what they should and should not do, and, as a consequence, avoid activity for fear of causing harm. Participation in exercise programmes may slightly improve physical function, depression and pain. It may slightly improve self‐efficacy and social function, although there is probably little or no difference in anxiety. Providing reassurance and clear advice about the value of exercise in controlling symptoms, and opportunities to participate in exercise programmes that people regard as enjoyable and relevant, may encourage greater exercise participation, which brings a range of health benefits to a large population of people.
Keywords: Humans; Middle Aged; Health Knowledge, Attitudes, Practice; Anxiety; Anxiety/rehabilitation; Arthralgia; Arthralgia/rehabilitation; Chronic Pain; Chronic Pain/psychology; Chronic Pain/rehabilitation; Depression; Depression/rehabilitation; Exercise Therapy; Exercise Therapy/psychology; Osteoarthritis, Hip; Osteoarthritis, Hip/psychology; Osteoarthritis, Hip/rehabilitation; Osteoarthritis, Knee; Osteoarthritis, Knee/psychology; Osteoarthritis, Knee/rehabilitation; Qualitative Research; Quality of Life; Randomized Controlled Trials as Topic; Self Efficacy; Social Participation; Symptom Assessment
The health benefits of exercise for people with chronic hip and knee pain from osteoarthritis
Researchers conducted a review of the effect of exercise on physical, emotional and mental health for people with long lasting (chronic) knee or hip joint pain from osteoarthritis. The studies examined were from Europe, North America, Asia and Australasia, and included clinical settings, home exercise and sessions at leisure facilities. Studies included men and woman aged 45 years and over.
What is chronic joint pain and what is exercise?
Chronic knee and hip pain from osteoarthritis (breakdown of the bone and cartilage, causing pain and stiffness) is a common cause of physical disability, anxiety, depression, poor quality of life and social problems (such as feeling a burden). Exercise is recommended to reduce pain and disability, and improves people's health beliefs, depression, anxiety and quality of life. We wanted to improve understanding of the relationships between pain, movement ability, psychological issues such as depression and anxiety, how chronic pain affects social relationships, and exercise.
What happens to people with chronic knee or hip pain who take part in exercise programmes?
A search of medical databases up to March 2016 found 21 studies with 2372 people which considered pain, movement or both alongside psychological and social outcomes when people with pain and stiffness in their knee, hip, or both took part in exercise. Participation in exercise programmes probably slightly improves pain, physical function, depression, and ability to connect with others, and little or no difference in anxiety. It may improve belief in one's own abilities, and social function.
The studies confirmed that:
‐ people who exercised rated their pain to be 1.2 points lower on a scale of 0 to 20 after about 45 weeks (score: 5.3 with exercise compared with 6.5 with no exercise (control), an improvement of 6%).
‐ physical function improved by about 5% over 41 weeks (exercise group improved by 5.6 points on a scale of 0 to 100 (44.3 with exercise compared with 49.9 with control)).
‐ people's confidence in what they could do increased by 2% after 35 weeks (exercise group improved by 1.1 points on a scale of 17 to 85 (65.4 with exercise compared with 64.3 with control)).
‐ people who exercised were 2% less depressed, or half a point on a scale of 0 to 21, after 35 weeks (3.0 points with exercise compared with 3.5 with control).
‐ exercise made people feel less anxious about themselves by 2%, a 0.4 drop on a 0 to 21 scale, after 24 weeks (5.4 points with exercise compared with 5.8 with control).
‐ exercise resulted in social interaction improving by 7.9 points over 36 weeks on a scale of 0 to 100, giving a change of 8% (81.5 with exercise compared with 73.6 with control).
The quality of the evidence was generally moderate, but low for confidence in ability, mental health and social function. This is mainly due to varied measures, making comparison more difficult, and because people taking part knew they were exercising so may have been influenced by expectations of improvement. The studies did not report side effects. Studies lasted for different durations, so we do not know if changes occurred quickly and were maintained, or whether improvements were gradual throughout the studies. Some studies took measurements later after the programme than others.
Additionally, 12 studies investigated people's opinions, beliefs and experiences of exercise, and whether exercise changed these. The quality of evidence was high overall. Initially people were confused about the characteristics of their pain, which shaped their feelings, behaviours and decisions about relieving pain. People thought movement and exercise was good for joints, but movement caused pain and they worried this might cause them harm. Lack of information from medical professionals meant people avoided physical activity and exercise for fear of causing damage.
Overall, people who had taken part in exercise programmes had positive experiences, helping increase their beliefs that exercise could improve pain, physical and mental health, and general quality of life.
Providing reassurance and exercise advice, challenging poor health beliefs, and providing enjoyable exercise programmes may encourage participation and benefit the health of many people.
Summary of findings
Summary of findings for the main comparison.
Physical and psychosocial outcomes in people with hip, knee or hip and knee osteoarthritis
| Physical and psychosocial outcomes in people with hip, knee or hip and knee osteoarthritis | ||||||
| Patient or population: people with chronic hip, knee or hip and knee osteoarthritis Settings: outpatient and community Intervention: exercise Comparison: varied: included normal care, education, attention controls such as home visits, sham gel and wait list controls | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Exercise | |||||
| Pain. WOMAC normalised to 0‐20 pain scale based on largest study reporting the 0‐20 scale (Hurley 2007). Lower score indicated less pain. Mean duration of follow‐up: 45 weeks (range: 12 weeks to 30 months). | The mean WOMAC pain score was 6.5. | The mean pain in the intervention groups was 1.25 points lower (1.8 to 0.8 lower) | ‐ | 1058 (9 studies) | ⊕⊕⊕⊝ Moderate1 | 6% absolute pain reduction (95% CI ‐9% to ‐4%). 19% relative pain reduction (95% CI ‐27% to ‐11%). SMD ‐0.33 (95% CI ‐0.46 to ‐0.21). |
| Physical function. WOMAC function scales normalised to 0‐100. Lower score indicated improved physical function. Mean duration of follow‐up: 41 weeks (range: 9 weeks to 30 months). | The mean WOMAC function was 49.9. | The mean function in the intervention groups was 5.6 points lower (7.6 to 2.0 lower) | ‐ | 1599 (13 studies) | ⊕⊕⊕⊝ Moderate2 |
5.6% absolute function improvement (95% CI ‐7.6% to 2%). 11.2% relative function improvement (95% CI ‐15.2% to ‐4%). SMD ‐0.27 (95% CI ‐0.37 to ‐0.17). |
| Self‐efficacy. Self‐efficacy scores transformed to exercise beliefs score with score range from 17 to 85. Higher score indicated greater self‐efficacy. Mean duration of follow‐up: 35 weeks (range: 12 weeks to 18 months). | The mean self‐efficacy was 64.3. | The mean self‐efficacy in the intervention groups was 1.13 points higher (0.74 to 1.51 higher) | ‐ | 1138 (11 studies) | ⊕⊕⊝⊝ Low3 | 1.66% absolute increase in self‐efficacy (95% CI 1.08% to 2.20%). 1.76% relative increase (95% CI 1.14% to 2.23%). SMD 0.46 (95% CI 0.34 to 0.58). |
| Depression. Depression scores were transformed to the HADS depression scale with score range of 0‐21. Lower score indicated less depression. Mean duration of follow‐up: 35 weeks (range: 8 weeks to 30 months). | The mean depression was 3.5. | The mean depression in the intervention groups was 0.5 points lower (1.0 to 0.1 lower). | ‐ | 919 (7 studies) | ⊕⊕⊕⊝ Moderate4 | 2.4% absolute reduction in depression (95% CI ‐4.7% to ‐0.5%). The relative reduction was 14.3% (95% CI ‐2.8% to ‐28%). SMD ‐0.16 (95% CI‐0.29 to ‐0.02). |
| Anxiety. HADS scale of 0‐21. Lower score indicated lower anxiety levels. Mean duration of follow‐up: 24 weeks (range: 9 weeks to 12 months). | The mean anxiety was 5.8. | The mean anxiety in the intervention groups was 0.4 points lower (1.0 lower to 0.2 higher). | ‐ | 704 (4 studies) | ⊕⊕⊕⊝ Moderate5 | 2% absolute improvement in anxiety (95% CI ‐5% to 1%). The relative change was 6.9% (95% CI ‐17.2% to 3.4%). SMD ‐0.11 (95% CI ‐0.26 to 0.05). |
| SF‐36 social function. Domain of SF‐36 considered representative of quality of life: mental health domain largely covered by depression and anxiety above: scale of 0‐100. Higher score indicated improved social function. Mean duration of follow‐up: 36 weeks (range: 8 weeks to 18 months). | The mean social function was 73.6. | The mean SF‐36 social function in the intervention groups was 7.9 (4.1 to 11.6 higher). | ‐ | 576 (5 studies) | ⊕⊕⊝⊝ Low6 | 7.9% absolute improvement in social function (95% CI 4.1% to 11.6%). The relative improvement was 8.8% (95% CI 2.7% to 13.9%). |
| Adverse effects of treatment | ‐ | ‐ | ‐ | ‐ | ‐ | Studies did not provide information on adverse events. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HADS: Hospital Anxiety and Depression Scale; SF‐36: 36‐item Short Form Survey; SMD: standardised mean difference; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Pain downgraded one level due to high risk of bias for blinding of participants.
2Function downgraded one level due to high risk of bias for blinding of participants.
3Self‐efficacy downgraded two levels; one level due to moderate heterogeneity (I2 = 47%) probably due to different measures of self‐efficacy being used in each study, and one level due to high risk of blinding bias.
4Depression downgraded one level due to high risk of blinding bias.
5Anxiety downgraded one level due to high risk of blinding bias. 6SF‐36 social domain downgraded two levels due to high heterogeneity (I2 = 75%) and reduced confidence in the estimate of effect when the outlier Aglamis 2008 was included, and high risk of blinding bias.
Background
Description of the condition
Severe peripheral joint pain, often labelled as osteoarthritis (OA), is extremely prevalent worldwide (Bedson 2004; Woolf 2003), and a major cause of disability and healthcare expenditure (Gupta 2005; Leardini 2004; March 1997; Vos 2012). In the UK, nearly 20% of people aged over 50 years have severe disabling knee or hip pain (Jinks 2004; Peat 2001), also labelled as OA (Bedson 2004), which slowly worsens over time, compromising quality of life and independence (Dawson 2005). The economic burden of joint pain/OA is significant (Gupta 2005). Annually 15% of people aged over 50 years consult their general practitioners (GP) for knee pain (Jinks 2004). Estimated figures for 2010 indicated that OA totalled GBP16.8 billion in direct (formal medical care) and indirect (lost working days, informal care) costs (Arthritis Research UK 2017). The personal experiencing and psycho‐socioeconomic consequences of chronic joint pain will increase as people live longer, adopt sedentary lifestyles and obesity rises (Underwood 2004). By 2020, OA is projected to be the fourth leading cause of disability across the world (Woolf 2003).
Description of the intervention
Exercise is recommended to reduce joint pain and improve physical function (Fransen 2015; NICE 2008; Zhang 2008). In addition, successful completion of a challenging exercise programme can highlight to people their capabilities; challenge inappropriate health beliefs; disrupt detrimental behaviour (fear‐avoidance); and teach people that exercise is a safe, beneficial, and active coping strategy they can use to improve self‐efficacy (confidence in one's ability to perform a specific health behaviour or task) and self‐reliance, and reduce helplessness and disability (Hurley 2010; Keefe 1996a; Penninx 2002). Unfortunately, as there is no summary of the evidence describing the reciprocity between pain, physical and psychosocial function and the utility of exercise on addressing these problems, the importance of these inter‐relationships remains underappreciated, and potential treatment options underutilised.
Information and advice about the role of exercise in the management of joint pain form part of most self‐management (Miles 2011; Newman 2004) and physiotherapy programmes (Walsh 2009). The aim is to effect behavioural change, that is, encourage people to exercise regularly, but the most effective way to deliver exercise advice that will bring about this behavioural change and get people exercising regularly is unclear (Hurley 2009). Didactic programmes, explaining the benefits of exercise for joint pain management using verbal or written information, may enlighten people, but they do not detail how to start exercising, what (not) to do, when, how or how much, and fail to convince people who have experienced many years of activity‐related pain that moderate‐intensity exercise will not aggravate their condition (Larmer 2014a). Consequently, didactic programmes may have limited ability to improve health beliefs, self‐confidence, self‐efficacy, coping and affect behavioural change. To people with joint pain, exercise remains a burdensome, time‐consuming, effortful concept that causes pain.
Programmes that include a participatory exercise component may encourage regular exercise more effectively (Griffiths 2007). On these programmes, participants gain first‐hand experience of what exercises to do; how to do them; that exercise is not harmful; and how exercise can be used to reduce pain; and this improves their physical function, health beliefs, anxiety, depression and potentially their general quality of life (Hurley 2007; Hurley 2010). Again, without a systematic review of the evidence on the effectiveness of exercise education delivery, the best way to bring about participation in regular exercise is unclear; wasting time, effort and resources, and potentially missing effective treatment options.
It is important to consider a range of different exercise interventions: National Institute for Health and Care Excellence (NICE) guidelines recommend muscle strengthening in the area affected, and aerobic exercise, with stretching and manipulation, is also advocated, particularly for hip OA (NICE 2014). Interventions to consider might therefore be land‐based or water‐based, and may focus on a single aspect of fitness such as strength training, aerobic exercise or balance, for example, or a combination of these. A programme may be delivered to groups or one‐to‐one, and may be carried out at a specialised facility or at home, in classes or individually, and frequency and intensity demanded may vary from one study to another.
How the intervention might work
Conceptual framework
Relationship between chronic pain, physical function and psychosocial function
Chronic joint pain and disability are the most common symptoms of OA, and attract the most attention. Because OA and joint pain are often regarded as the benign, untreatable, inevitable consequences of ageing, the psychosocial sequelae (anxiety, depression, health beliefs, behaviours, quality of life, participation and dependency) are often underestimated by healthcare professionals and lay people. However, this overlooks the complex, reciprocal relationship between pain, physical functioning and psychosocial functioning where each affects and is affected by the others (Hurley 2003; Figure 1). For example, chronic joint pain is bewildering and distressing because it has no obvious cause, increases insidiously and is unaccountably episodic. People's reactions to pain are highly variable and influenced by the beliefs, meanings and explanations they attach to it.
Figure 1.

Complex reciprocal inter‐relationship between pain, physical and psychosocial function and exercise (Hurley 2003: permission for reproduction provided by the publishers, Wolters Kluwer).
Relationship between health beliefs and psychosocial outcomes
Beliefs about the cause, prognosis and effectiveness of treatment are key determinants of illness behaviour and response to treatment (Main 2002; Turk 1996). People commonly believe joint pain is the inevitable, incurable consequence of ageing, caused or exacerbated by activity, evoking feelings of helplessness, anxiety, depression and "fear‐avoidance" behaviour (Figure 2), when people avoid physical activity for fear of causing additional pain and damage (Keefe 1996a). However, avoiding activity results in greater muscle weakness, joint instability and stiffness, exacerbated pain, disability and dependency (Dekker 1992). Challenging these erroneous health beliefs is vital for successful pain management. Inappropriate health beliefs and behaviours can be altered by positive experiences that show people how active coping strategies such as exercise can reduce pain and improve physical functioning, self‐efficacy, anxiety, helplessness, catastrophising and depression (Keefe 1996b; Main 2002; Turk 1996). Appreciating the complex inter‐relationship between clinical symptoms and psychosocial effects of joint pain could provide additional strategies for better joint pain management.
Figure 2.

Effect of erroneous health beliefs (Hurley 2003: permission for reproduction provided by the publishers, Wolters Kluwer).
Better appreciation of the complex reciprocal relationship between pain, psychosocial effects and physical functioning would help us understand better the consequences of joint pain, identify the most effective ways of teaching the value of exercise, and develop more efficient models of care for people experiencing chronic joint pain. This is best achieved by a systematic review of the relevant literature to establish what interventions are most effective, and to quantify the size of the treatment effect produced. However, the complex reciprocity between joint pain, psychosocial impact, physical functioning and exercise will be influenced by many factors that are difficult to measure as they depend on nebulous, labile, personal beliefs, experiences, emotions, preferences and prejudices. A systematic review asking questions on effectiveness and synthesising outcome evaluations only would miss important facets and cannot accommodate information from qualitative studies better placed to assess pain, the psychosocial effects of pain and the benefits of exercise. These are best captured using methods that synthesise quantitative (systematic reviews) with qualitative studies of people's views and experiences (Lorenc 2008; Oliver 2008; Rees 2006; Thomas 2004). Appreciating the views, beliefs, experiences and preferences of target populations for an intervention provides greater insight into how an intervention achieves its effects, why it may not be as effective as anticipated and may expose gaps in our understanding. This enables us to adapt existing, or develop new, healthcare interventions that best address people's needs (Harden 2004; Oliver 2008; Rees 2006).
Why it is important to do this review
This review focused on exercise‐based rehabilitation programmes, defined as programmes that had an active participatory exercise component (for management of OA and the psychosocial variables affected by the condition). Establishing the effect of exercise‐based rehabilitation programmes on the psychosocial impact of chronic joint pain will increase our understanding about how and why these interventions are effective and identify the effective elements of exercise programmes.
To meet the aims, the review will answer the following questions.
What are the effects of exercise‐based rehabilitation programmes on physical and psychosocial functioning for people with chronic knee or hip (or both) pain?
What are people's experiences, opinions and preferences regarding exercise‐based rehabilitation programmes and the advice they receive about exercise?
What implications can be drawn from the qualitative synthesis of people's views to inform the appropriateness and acceptability of exercise‐based rehabilitation programmes for people living with OA?
Objectives
Overarching objective
To improve our understanding of the complex inter‐relationship between pain, psychosocial effects, physical function and exercise.
Specific aims and objectives
To systematically review the evidence on the impact of physical exercise on people's pain, physical and psychosocial functioning including:
identifying the most effective formats for delivering exercise advice;
explaining why some exercise interventions may be more effective than others;
recommending exercise formats and content by constructing a "toolbox" that describes the most effective exercise interventions for healthcare providers and patients to use.
These was achieved by conducting:
a synthesis of quantitative data on the benefits and harm of exercise interventions for improving pain, physical functioning and psychosocial functioning;
a synthesis of qualitative data on participant's experiences, opinions and preferences of physical exercise;
a synthesis integrating the quantitative and qualitative data (an integrative review) to assess the extent to which existing evaluated interventions address the needs and concerns of people living with OA.
Methods
Criteria for considering studies for this review
Types of studies
To be included in the review, quantitative clinical trials of exercise programmes had to have used individual or cluster randomised allocation. Qualitative studies reporting the views and opinions of participants of exercise‐based programmes had to have reported methods of data collection and data analysis, and people's perspectives, beliefs, feelings, understanding, experiences or behaviour about exercise or advice on exercise that were presented as data (e.g. direct quotes from participants or description of findings). There were no limits on location or language; however, quantitative clinical trials or qualitative studies had to be published after 1985 because of the paucity of well‐designed and well‐reported relevant studies prior to 1985.
Types of participants
We included studies with men, women, or both, aged 45 years or older, with a clinical diagnosis of OA (as defined by the study) or self‐reported chronic hip or knee (or both) pain (defined as more than six months' duration).
Types of interventions
Exercise‐based rehabilitation programmes could consist of any type of land‐based or aquatic‐based exercise programme aiming to improve OA symptoms delivered in hospitals or the community. Programmes could vary in content (e.g. range of motion, aerobics, Tai Chi) and their delivery mode (classes or individual therapy), length, frequency or intensity. The comparator (control group) could consist of no treatment, waiting list group or any non‐exercise intervention (e.g. medication, lifestyle/diet changes, information on OA).
Types of outcome measures
The major outcomes of interest were pain, physical function, self‐efficacy, depression, anxiety, quality of life and adverse effects of exercise.
For quantitative synthesis, randomised controlled trials (RCT) had to have measured either pain or function and at least one psychosocial outcome (self‐efficacy, depression, anxiety, quality of life). Quality of life related to a range of factors, which the World Health Organization (WHO) identifies as "physical health, psychological state, level of independence, social relationships, personal belief and their relationship to salient features of their environment" (WHO 1997).
The qualitative synthesis studies had to have reported people's opinions and experiences of exercise (e.g. their views and beliefs about the utility of exercise in the management of chronic pain, or barriers to adherence to exercise advice).
Search methods for identification of studies
Electronic searches
In July 2012, we searched electronic databases using comprehensive strings of thesaurus and free‐text terms for the key features:
condition: chronic knee and hip pain (e.g. 'osteoarthritis/chronic joint pain');
intervention: 'exercise,' physical activity, aerobic, walking, Tai Chi, physiotherapy.
The two strings were combined to identify reports that contained terms for both features (population AND topic). An example of the thesaurus and free‐text strings applied to PubMed is provided in Appendix 1.
These search strategies were applied to 23 clinical, public health, psychology and social care databases (Appendix 2), 25 other resources by handsearching (Appendix 2), and references of included studies. We contacted key experts/authors to identify any other potentially relevant studies.
We conducted follow‐up searches in March 2014 and March 2016 to ensure any further trials that had been published and which met criteria could be included in the review.
Searching other resources
We checked references of included studies by:
checking where included studies had been cited, using Google Scholar;
checking references of selected reviews in the topic area that the research team were aware of from a systematic review of reviews on adult social care; outcomes concurrently being undertaken at the EPPI‐Centre;
asking key experts/authors of included studies.
We engaged with experts from the research, advocacy and policy sectors in the field of OA rehabilitation. They informed key stages in the review including: advising on the scope, informing the search strategy, reviewing the final report and disseminating the research findings.
Data collection and analysis
Selection of studies
Review authors applied inclusion and exclusion criteria to titles and abstracts. We obtained full‐text reports for studies that appeared to meet the criteria. We extracted data and information from these studies and entered them into a database and reapplied the inclusion and exclusion criteria. We included studies that met the inclusion criteria in the review. All review authors involved in study screening (KD, HH, MH, NW) took part in a moderation exercise where results were discussed to ensure consistency in applying the review inclusion/exclusion criteria. For the initial title and abstract screening, we carried out a "double screening" of 200 papers before continuing with independent screening. For the screening of full reports, a second review author independently applied the criteria on 10% of the reports. A 90% agreement rate was required before proceeding to independent screening. Review authors (KD, HH, MH, NW) independently screened the remaining sample of potential studies. Where a review author (e.g. HH) was unable to reach a decision, consensus was reached through discussion with a second review author (e.g. KD) or, if required, a third review author (MH or NW). In two cases where there was doubt over whether a study should be included (Jenkinson 2009; Thomas 2002), we contacted authors but received no reply and the studies unfortunately had to be excluded as a result.
Data extraction and management
We used EPPI‐Reviewer software to manage the review (Thomas 2002). Four review authors (KD, HH, MH, NW) extracted descriptive details from the full reports using a prepiloted data collection form. If a review author was an author of one of the included studies, they were not involved in any decisions regarding data extraction from that study.
We extracted the following information from all studies:
aims and focus of the research;
study design;
-
details about the intervention including:
format: written, didactic, non‐participatory/participatory, lay/professional led, individual/group therapy, etc.;
content: type, frequency, intensity, etc.;
setting: hospital/outpatient/community/home‐based, etc.;
-
details about the study populations and settings as per the PROGRESS‐Plus framework (Kavanagh 2008):
broad social determinants of health and well‐being (e.g. ethnicity, occupation, gender, education, socioeconomic status);
characteristics that impinge on health and well‐being by attracting discrimination, such as age;
other contextual features pertinent to the experiences of living with knee and hip pain, such as housing.
Quantitative outcome data
For quantitative outcome measurements, whenever possible, we extracted raw scores. Where trials reported pain or function using more than one outcome measure tool, we extracted data according to the following hierarchy: Western Ontario McMaster Universities Osteoarthritis Index (WOMAC), Arthritis Impact Measurement Scale (AIMS), visual analogue scale (VAS) and other. Similarly, preference was given to standardised psychosocial outcomes. A summary of data collected for included studies is reported in the Characteristics of included studies table.
Qualitative "views" data
For qualitative studies that include "views" data, whenever possible, we extracted participant's quotes first, followed by and distinguished from authors' descriptions and analysis of participants' views. We followed the conceptual framework to support the identification of factors potentially impacting on participation in and experiences of exercise (Figure 2). A summary of data collected for included qualitative studies is reported in Appendix 3.
Assessment of risk of bias in included studies
In pairs, four review authors (HH, KD, MH, NW) independently assessed the risk of bias for all included studies using the Cochrane tool for assessing risk of bias addressing the following criteria (Higgins 2011a).
Sequence generation
The methods used to generate the allocation sequence were categorised as:
low risk of bias (risk of bias avoided or addressed (or both)) if a random component in the sequence generation process was described (e.g. referring to a random number table);
high risk of bias (risk of bias not adequately addressed) if the authors described a non‐random component in the sequence generation process (e.g. sequence was generated by hospital or clinic record number);
unclear risk of bias (uncertain risk) if the sequence generation process was not specified.
Allocation sequence concealment
The method used to conceal the allocation sequence in sufficient detail to determine whether intervention allocation could have been foreseen in advance of, or during, recruitment, or changed after assignment, categorised as:
low risk of bias if an appropriate method was used to conceal allocation (e.g. central allocation including telephone, web‐based and pharmacy‐controlled randomisation; sequentially numbered, opaque, sealed envelopes) from personnel enrolling participants;
high risk of bias if appropriate method to conceal allocation was not guaranteed;
unclear risk of bias if methods used to conceal allocation were not specified.
Blinding
As it is very difficult to blind providers and recipients to exercise programmes. We assessed the methods used to blind study participants and researchers to the intervention that participants received.
Blinding ofparticipants as:
low risk of bias if the authors described methods taken to blind study participants to the intervention;
high risk of bias if there were no attempts to blind study participants to the intervention;
unclear risk of bias if methods taken to blind study participants were not specified.
Blinding of outcome assessment as:
low risk of bias if the authors stated explicitly that the primary outcome variables were assessed blindly;
high risk of bias if the outcomes were not assessed blindly and this was likely to affect results;
unclear risk of bias if not specified in the paper.
Completeness of outcome data
The individual attrition rate for intervention and control groups, whether exclusions were reported and whether the authors conducted an in intention‐to‐treat analysis were categorised as:
low risk of bias if there were no missing data or missing outcome data were balanced in numbers across intervention groups, with similar reasons for those missing data and unlikely to alter the results of the study;
high risk of bias if missing outcome data were likely to bias the results;
unclear risk of bias if not specified in the paper.
Reporting bias
Outcome reporting was categorised as:
low risk of bias if evidence outcomes were selectively reported (e.g. all relevant outcomes in the methods section were reported in the results section);
high risk of bias if some important outcomes were omitted;
unclear risk of bias if not specified in the paper.
Other bias
Other potential sources of bias were categorised as:
low risk of bias if there was no evidence of other risk of biases, and
high risk of bias if there were concerns of other sources of bias affecting the results.
Any disagreements were resolved by discussion and, if necessary, by consulting a fifth review author.
Assessment of rigour in qualitative studies
We assessed the quality and methodological rigour of "views studies" using a tool developed at the EPPI‐Centre (Harden 2004), which considers whether the findings were grounded in the data and reflected people's views. The development of the criteria was informed by those engaged in ensuring increased transparency and explicit methods for assessing the quality of qualitative research (Boulton 1996; Cobb 1987; Mays 1995; Popay 1998), and was adapted in accordance with the Cochrane Qualitative Research Methods Group guidance on adopting a quality appraisal framework (Hannes 2011).
We assessed each study according to the extent to which they provide explicit description of:
aims and objectives;
methodology, including systematic data collection methods;
participants;
context, detailing factors important for interpreting the results;
data analysis to establish dependability and validity.
Two review authors (KD, HH) judged the quality of studies containing people's views based upon judgements about the 'dependability' and ‘credibility' of the study's findings. Any disagreements were resolved by discussion and, if necessary, by consulting a third review author.
Dependability
The sampling frame, methods of data collection and analysis were categorised as:
high quality (low risk of bias/error) if thorough attempts were made to increase rigour in the sampling, data collection and analysis;
medium quality if some steps were taken to increase rigour in the sampling, data collection and analysis;
low quality if minimal steps were taken or it was unclear what attempts study authors made to avoid methodological bias and error in conducting the study.
Credibility
Credibility was categorised as:
high quality (low risk of bias/error) if the findings were well grounded/supported by the data, contributed either depth or breadth of findings (in relation to their ability to answer the review question) and privileged the perspectives and experiences of people living with OA;
medium quality if studies met the same criteria as high‐quality studies, but were only fairly well grounded in the data;
low quality if studies were 'limited' on any of the above criteria.
Any disagreements were resolved by discussion and by consulting with a third review author (SO).
As one of the aims of the review was to synthesise people's experiences and preferences in relation to exercise to better understand the factors that might contribute to the success of exercise‐rehabilitation programmes, we did not exclude studies failing to meet a minimum quality threshold (i.e. those scoring low for both dependability and credibility). Instead, we used the quality assessment to assess the contribution of each study to the development of explanations and relationships.
Measures of treatment effect
Continuous data
For continuous data measured by the same scale or unit, we calculated mean differences (MD) with 95% confidence intervals (CI). For similar outcomes measured by a different scale or units, we used standardised mean differences (SMD) with 95% CIs.
We presented highly skewed continuous data in tables.
Where standard errors (SE) were reported instead of standard deviations (SD), we used Review Manager 5 to calculate the effect size estimate (RevMan 2014). In one study, the SD was calculated from the SE. Where there were no SDs or SEs reported, we estimated the mean SD from available studies, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
Dichotomous data
For dichotomous (binary) data, we calculated risk ratios (RR) with 95% CIs, or converted odds ratios (OR) to SMDs, using the Cox‐Snell formula, and where appropriate we combined results from different trials.
Unit of analysis issues
We identified the level at which randomisation occurred (e.g. individual participants, cluster‐randomised trials, repeated measures) at the data extraction stage and addressed the following issues if they arose:
cluster‐randomised trials: using intraclass correlation coefficient (ICC) estimates the design effect was calculated and the variance inflated accordingly;
multiple interventions per participant: we analysed studies that compared the effect of two or more types exercise‐based rehabilitation programmes with a control condition;
multiple follow‐up: for trials that measured outcomes at multiple time points, we selected the longest follow‐up.
Dealing with missing data
We recorded the amount of missing data, reasons, pattern (missing completely at random, missing at random, missing not at random) and how the missing data were handled (ignored, last observation carried forward, statistical modelling, etc.) (Carpenter 2008). We performed sensitivity analyses to assess the impact of the missing data on study findings and considered the implications to the review in the Discussion.
Assessment of heterogeneity
All pooled analyses used the I2 statistic to assess the percentage of total variation caused by heterogeneity of the trials (Higgins 2003). We assessed statistical heterogeneity across studies by visual inspection of the forest plot and using the Chi2 test with a significance level of P less than 0.10, and the I2 test and tentatively assign I2 statistic value of:
low heterogeneity: less than 49%;
moderate heterogeneity: 50% to 74%;
high heterogeneity: 75% to 100% (Higgins 2003).
We assessed clinical heterogeneity by analysing subgroups by type of OA (knee, hip, or a combination; age; gender and severity of symptoms; see Subgroup analysis and investigation of heterogeneity).
When there was moderate heterogeneity (Chi2 P less than 0.10 and I2 value 50% to 74%), we used a random‐effects model. When there was no clinical and no important statistical heterogeneity (I2 less than 49%), we combined results using a fixed‐effect model. We considered the potential cause of heterogeneity by conducting subgroup and sensitivity analyses as described below.
In the qualitative studies, differences in study setting and sample (e.g. gender, age, type and severity of OA/chronic pain) informed the qualitative synthesis and were used to explain variation in the study's findings.
Assessment of reporting biases
We constructed funnel plots (effect size versus SE) to assess publication bias, if a sufficient number of trials was found (about 10: Sterne 2004). Where possible, we compared the outcomes and comparisons reported in the papers against trial protocols to detect unreported results that may indicate reporting bias.
Assessment of reporting biases were not applied to qualitative studies.
Data synthesis
The methods used to synthesise data were driven by the research question, types of studies/data included, the detail and quality of reporting in these studies and their heterogeneity. The synthesis of study findings was informed by the conceptual framework and the type of interventions identified. If there was a wide variety of approaches and patient populations, we used a random‐effects model in the meta‐analyses.
Quantitative synthesis
Where possible, we used standard methods for statistical meta‐analysis to synthesise data using Review Manager 5 (RevMan 2014). We used an SMD approach, which scales each outcome at endpoint by its SD, due to the diversity of psychosocial measures. We conducted a fixed‐effect meta‐analysis for combining data where it was reasonable to assume studies had estimated the same underlying treatment effect (i.e. in trials examining the same intervention, and the trials' populations and methods were judged sufficiently similar). If there was substantial statistical heterogeneity, we used random‐effects models, presented as mean treatment effect with 95% CIs.
Subgroup analysis and investigation of heterogeneity
We investigated whether subpopulations responded differently to an exercise‐based rehabilitation programme by comparing the responses of different subgroups to the exercise programme. Theoretically, participants who only experience chronic hip pain may respond differently to exercise programmes than people who only experience knee pain, and both respond differently to people with hip and knee pain. Other a priori planned subgroup analyses included age, gender and severity of symptoms as defined by the studies included in the review.
For trials, we tested for heterogeneity across subgroup results and computed an I2 statistic. We used random‐effects models to analyse variation in the mean effects in the different subgroups using meta‐regression techniques to reduce false‐positive results when comparing subgroups in a fixed‐effect model (Higgins 2011b). Post‐hoc subgroups analyses were considered to be exploratory analyses.
Sensitivity analysis
If aspects of a trial (e.g. atypical intervention, methodology, missing information) appeared to unduly influence the review's findings, we conducted sensitivity analyses to assess the influence of that study and reported them in a summary table.
For qualitative studies, we considered whether individual and contextual factors explained variation in the type of views identified.
Qualitative synthesis
We synthesised studies of people's views using the framework synthesis used in previous EPPI‐Centre reviews (Lorenc 2008; Oliver 2008). A framework synthesis accommodates a range of different types of studies and can be conducted relatively quickly by a team of review authors.
We extracted verbatim quotes from study participants and author description of findings from the result sections of included studies. We read the text reported in the discussions and conclusions during this data extraction process; however, these sections contained author's conclusions and implications but did not present any new data and, therefore, were not used to inform the synthesis.
Two review authors (KD, HH) independently read through reports and extracted data from the studies. Data were matched against the conceptual framework. As these were broad themes (Figure 1), we used a thematic analysis to identify subthemes. This enabled the existing conceptual framework to be used as the basis for the synthesis, which was then developed further by the introduction of themes from the studies (Figure 3). The themes' codes acted as an index to navigate the data and allowed the literature to be subdivided into manageable sections ready for indepth analysis. Each element of the framework was individually interrogated in turn, tabulating the data under key themes to present distilled summaries.
Figure 3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Both review authors then compared their individual coding. They considered the extent to which each subtheme was mutually exclusive and how they understood the data in relation to their individual coding, reflecting on the review questions' emphasis on participants' meanings and experiences ensuring that the coding did not go beyond the original context of the study. In some cases, both review authors went back to the original studies to check their understanding. Similar themes were then grouped and condensed until a smaller number of subthemes emerged. In some cases, themes originally coded under one broad theme (e.g. environmental factors) had a better fit with another broad theme (e.g. psychological factors). The discussion continued until a consensus was reached on which a priori themes were supported by the data, and whether new themes identified by the review authors did actually map to the pre‐existing broad theme. The result was a finalised list of themes. A diagram of these themes was generated to provide an illustration of the themes and subthemes in the synthesis (Figure 3). Overall drawing together what can be learnt from the tables and summaries and finding associations between themes and providing explanations for those findings across the included studies supported us to illuminate people's responses to aspects of arthritis and approaches to self‐management. This approach has provided a clear path from the original research data, to individual study authors' descriptions and analyses to the findings of the qualitative review synthesis (Appendix 4).
Synthesis integrating quantitative and qualitative findings (integrative review)
Two review authors (SO, KD) reread the qualitative synthesis and generated implications from people's views on what they considered important in supporting their engagement in exercise. After consulting with other review authors (MH, NW), we made refinements until consensus was reached on an agreed set of implications. The implications were generated into a coding tool and two review authors (KD, HH) critically re‐examined the intervention descriptions as reported in the 21 RCTs included in the quantitative synthesis to identify whether they addressed each of the implications.
Having identified which components were contained within each intervention, we aimed to assess the extent to which each component was present in the intervention by answering: 'yes,' 'no/not stated' or 'partially.' Two review authors independently conducted this assessment and then paired up to compare findings and check accuracy of extracted data. Decisions about the extent of a component's presence were based on the trial authors' descriptions and reporting. Detailed information to support 'yes' or 'partially' was required and decisions were recorded on EPPI‐Reviewer. Disagreements were discussed until consensus was reached with the option of referring to a third review author (SO) for resolution if agreement could not be made.
After coding agreements were finalised, the findings were mapped onto a matrix, as previously used in EPPI‐Centre systematic reviews, enabling the integration of controlled trials and view studies to be 'juxtaposed' (Candy 2011). The matrices in the integrative synthesis map the presence of components within the RCTs with the studies' effect sizes and contextual detail on recruitment and intervention description previously extracted as part of the quantitative synthesis. This enabled us to visibly illustrate and interrogate patterns in the findings, supporting the generation of a comparative descriptive narrative addressing the following questions.
Which components of (in)effective interventions correspond with views expressed by participants?
Does this match suggest why or how the intervention (does not) work?
What components appear in effective interventions but not in ineffective interventions?
Does the 'views' synthesis suggest these components are significant from a participant perspective?
Does addressing the psychosocial effects of joint pain improve pain and physical functioning?
Clinical relevance
The social science review authors (KD, HH, SO) conducted the synthesis of qualitative studies and drew implications from that for interventions and the final synthesis across the statistical meta‐analysis and qualitative study synthesis. In each case coreview authors, including two who were both clinicians and coauthors of a trial and two qualitative studies (MH, NW), checked the coherence of the emerging findings. Their responses prompted a reinspection of themes in terms of their roots in the primary studies, their language, their relationship to each other and to the conceptual framework, and the quotes chosen to support the themes. Inaccuracies were corrected, and language and interpretations refined.
Summary of evidence
We prepared a 'Summary of findings' table for the quantitative and qualitative syntheses. For quantitative trials, we used the methods and recommendations described in the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011), using GRADEpro software (GRADEpro 2008). Similarly, we created a 'Summary of qualitative evidence' to summarise the key findings and be informed by the assessment of rigour, detailing the extent to which the findings are trustworthy, based on their dependability and credibility, in answering the review question.
Results
Description of studies
Results of the search
Searches of bibliographic databases and websites, including the update searches to March 2016, yielded 26,455 potentially relevant citations. Figure 4 describes the flow of these records through the screening process. After removing 8266 duplicates, we screened 18,189 titles and abstracts using prespecified eligibility criteria of which 17,668 were excluded. Of the 521 potential reports, 24 were unobtainable and we obtained 497 for full‐text screening. Applying the same criteria used at the title and abstract screening stage, we excluded a further 464 studies. We included 33 studies in the data and analyses consisting of 21 in the quantitative synthesis and 12 in the qualitative synthesis.
Figure 4.
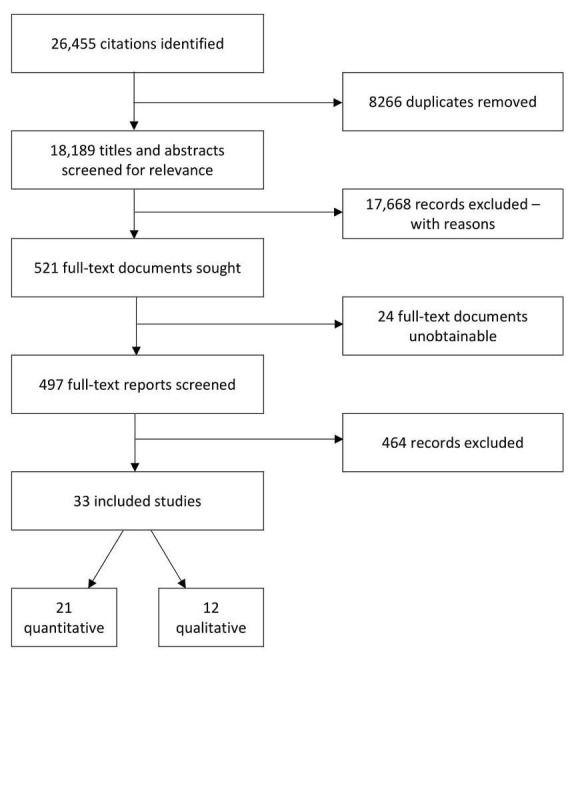
Flow chart of search and screening process.
Included studies
Twenty‐one trials (2372 participants) met the criteria for inclusion in the quantitative synthesis and 12 studies met the criteria for inclusion in the qualitative synthesis. Of the 21 studies identified for the quantitative synthesis, four had three treatment arms and so were split in the meta‐analyses (French 2013; Focht 2005; Hurley 2007; Keefe 2004), and were treated as 25 'comparisons' as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). The three‐arm studies had two entries for some outcomes in the Data and analyses table. Where this was the case, the first arm referred to intervention group and the second arm to intervention group, as outlined in the Characteristics of included studies table. Further details are provided in the Characteristics of included studies table.
Twelve qualitative studies of people's views, opinions and experiences were included (Appendix 3).
Setting
Studies were published between 1998 and 2016. All studies were conducted in high‐income countries. This included nine trials based in the US (Baker 2001; Cheung 2014; Focht 2005; Keefe 2004; Mikesky 2006; Park 2014; Schlenk 2011; Sullivan 1998; Wang 2009); three in Australia (Bennell 2014; Bennell 2016; Fransen 2007); and one each in Ireland (French 2013), the UK (Hurley 2007), the Netherlands (Hopman‐Rock 2000); South Korea (Kim 2012), Turkey (Aglamis 2008), Canada (Péloquin 1999), Taiwan (Kao 2012), Norway (Fernandes 2010), and Hong Kong (Yip 2007).
All the studies providing qualitative data were published from 2005 onwards. This date reflected the development of qualitative methodology and its widening uptake being relatively recent developments, and earlier studies found through the search were of insufficient quality to include. Four studies were based in the UK (Campbell 2001; Hendry 2006; Hurley 2010; Morden 2011), three in New Zealand (Fisken 2016; Larmer 2014b; Moody 2012); and one each in Australia (Hinman 2016), Canada (Stone 2015), Sweden (Thorstensson 2006), Iceland (Petursdottir 2010), and the Netherlands (Veenhof 2006).
All included papers were written in English.
Design
Twenty studies evaluating the effectiveness of exercise programmes used individual participant randomised controlled designs and one study used a cluster randomised control design (Hurley 2007). Seventeen trials had two arms (Aglamis 2008; Baker 2001; Bennell 2014; Bennell 2016; Cheung 2014; Fernandes 2010; Fransen 2007; Hopman‐Rock 2000; Kao 2012; Kim 2012; Mikesky 2006; Park 2014; Péloquin 1999; Schlenk 2011; Sullivan 1998; Wang 2009; Yip 2007), and four studies had three arms (Focht 2005; French 2013; Hurley 2007; Keefe 2004). Seven studies compared exercise with a usual care control arm (Hurley 2007; Kao 2012; Keefe 2004; Kim 2012; Péloquin 1999; Schlenk 2011; Yip 2007), nine trials with an attention control (Baker 2001; Bennell 2014; Bennell 2016; Fernandes 2010; Focht 2005; Mikesky 2006; Park 2014; Sullivan 1998; Wang 2009), and five studies with a 'wait list' control (Aglamis 2008; Cheung 2014; Fransen 2007; French 2013; Hopman‐Rock 2000).
All the studies included in the qualitative synthesis sought the views of people living with OA on aspects ranging from health beliefs to their experiences of exercise. Seven studies aimed to examine factors associated with exercise adherence, compliance and take up through the concepts of motivation and facilitators and barriers to participation in exercise (Campbell 2001; Fisken 2016; Hendry 2006; Petursdottir 2010; Stone 2015; Thorstensson 2006; Veenhof 2006). In the remaining five studies, the aims were to explore people's views of arthritis and exercise as a treatment (Hurley 2010), models of lay management (Morden 2011), and perceptions of an exercise intervention (Hinman 2016; Larmer 2014b; Moody 2012). Six studies included participants who had taken part in a formal evaluation of an exercise intervention, from which participants were drawn for indepth interviews; these participants were actively engaged in exercise (Campbell 2001; Hinman 2016; Hurley 2010; Moody 2012; Thorstensson 2006; Veenhof 2006). In the remaining six studies with no exercise intervention, participants' engagement in exercise ranged from sedentary to actively engaged in exercise and everyday activities (Fisken 2016; Hendry 2006; Larmer 2014b; Morden 2011; Petursdottir 2010; Stone 2015).
Study size
The sample size of studies varied; the largest study randomly assigned 418 people (Hurley 2007), while the smallest randomly assigned only 21 people (Schlenk 2011). Overall, 11 studies had a sample size of fewer than 100 participants (Aglamis 2008; Baker 2001; Cheung 2014; Fransen 2007; Hopman‐Rock 2000; Keefe 2004; Kim 2012; Park 2014; Schlenk 2011; Sullivan 1998; Wang 2009), and 10 studies had sample size between 102 and 418 participants (Bennell 2014; Bennell 2016; Fernandes 2010; Focht 2005; French 2013; Hurley 2007; Kao 2012; Mikesky 2006; Péloquin 1999; Yip 2007).
The largest qualitative views study had a sample size of 29 participants (Hurley 2010), and the smallest contained six participants (Hinman 2016), with remaining sample sizes ranging from 12 to 22 participants (Campbell 2001; Fisken 2016; Hendry 2006; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006; Veenhof 2006).
Outcomes
Pain
Of the 21 studies included in the review, only one did not measure pain (Schlenk 2011): it was still included because of its measurement of function. Nine studies used the WOMAC (Aglamis 2008; Baker 2001; Cheung 2014; Fernandes 2010; Focht 2005; Fransen 2007; Hurley 2007; Mikesky 2006; Wang 2009), five studies used the VAS Pain (Bennell 2014; Bennell 2016; Hopman‐Rock 2000; Kim 2012; Yip 2007), and two studies used the AIMS (Keefe 2004; Sullivan 1998). The study by French 2013 used a 'numerical rating scale' to measure pain severity during daytime activities and at night. In addition, Park 2014 used the McGill Pain Questionnaire, Péloquin 1999 used the Doyle's Joint Index and Kao 2012 used a health‐related quality of life measure for body pain.
Physical function
Eighteen studies measured function. Thirteen studies used the WOMAC (Aglamis 2008; Baker 2001; Bennell 2014; Bennell 2016; Cheung 2014; Fernandes 2010; Focht 2005; Fransen 2007; French 2013; Hurley 2007; Mikesky 2006; Schlenk 2011; Wang 2009); two used AIMS subscales (Péloquin 1999; Sullivan 1998); one used a health‐related quality of life measure (Kao 2012); one used gait speed tests, the six‐minute walk test and Berg Balance Scale (Park 2014); and one used a modified Health Assessment Questionnaire (HAQ) (Yip 2007).
Self‐efficacy
Eleven studies measured self‐efficacy (Bennell 2014; Bennell 2016; Focht 2005; Hopman‐Rock 2000; Hurley 2007; Keefe 2004; Kim 2012; Schlenk 2011; Sullivan 1998; Yip 2007; Wang 2009). Measures included those designed specifically for people living with OA (e.g. the Arthritis Self‐Efficacy Scale), or focused on beliefs about ability to exercise.
Depression and anxiety
Three studies measured anxiety and depression using the Hospital Anxiety and Depression Scale (HADS) (Fransen 2007; French 2013; Hurley 2007). Two studies measured depression, anxiety and stress using the 21‐item Depression, Anxiety, Stress Scales (Bennell 2014; Bennell 2016). Three studies measured depression only, two used the Center for Epidemiologic Studies Depression Scale (CES‐D) (Mikesky 2006; Wang 2009), and one study translated a "depression self‐rated measure for use in Korean" (Kim 2012).
Health‐related quality of life
Five studies used the 36‐item Short Form (SF‐36) measure of health‐related quality of life providing individual scores for four mental health‐related subscales (e.g. emotional role, vitality, social functioning and mental health) (Aglamis 2008; Baker 2001; Fernandes 2010; Focht 2005; Kao 2012).
Sleep quality
One study measured sleep quality using the Pittsburgh Sleep Quality Index (Cheung 2014).
Population characteristics
Symptoms
Fourteen studies recruited participants with knee OA only (Aglamis 2008; Baker 2001; Bennell 2016; Cheung 2014; Focht 2005; Hurley 2007; Kao 2012; Keefe 2004; Mikesky 2006; Péloquin 1999; Schlenk 2011; Sullivan 1998; Wang 2009; Yip 2007), three studies recruited participants with hip OA only (Bennell 2014; Fernandes 2010; French 2013), and four studies included participants with hip OA or knee OA (or both) (Fransen 2007; Hopman‐Rock 2000; Kim 2012; Park 2014).
Participants in six of the studies reporting people's views had a diagnosis or experienced chronic pain in the knee only (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Morden 2011; Thorstensson 2006), and six studies recruited participants living with OA of the lower limbs (Fisken 2016; Larmer 2014b; Moody 2012; Petursdottir 2010; Stone 2015; Veenhof 2006).
Gender
Three trials recruited only women (Aglamis 2008; Cheung 2014; Kim 2012), while the remaining were mixed samples.
In the qualitative studies, one study recruited only women (Fisken 2016). Eleven studies enrolled both men and women with women outnumbering men in all but two of the studies (Hinman 2016; Thorstensson 2006).
Ethnicity
Only one trial, conducted in the US, reported the ethnicity of participants (eight African‐American, three Hispanic/Latino and 91 Anglo‐American; Sullivan 1998). Cheung 2014 reported that 86% of participants were white and Park 2014 reported that 61.8% of participants were non‐Hispanic white, but neither study provided details of ethnicity of the remainders of their samples.
The majority of the qualitative studies did not explicitly state the ethnicity of participants. Of the three studies that reported ethnicity, participants were of black African, black Caribbean, Maori, Samoan, Indian or white ethnic backgrounds (Fisken 2016: six New Zealand European, two Maori, three others; Hurley 2010: three black African, five black Caribbean, one Indian and 20 Caucasian; Larmer 2014b: 14 New Zealand European, one Samoan).
Description of intervention
Types of exercise programmes
Of the 20 studies evaluating land‐based exercise programmes, seven studies combined strength training with different forms of aerobic exercise (Aglamis 2008; Focht 2005; Hurley 2007; Keefe 2004; Péloquin 1999; Schlenk 2011; Sullivan 1998), eight delivered strength‐based resistance training programmes (Baker 2001; Bennell 2014; Bennell 2016; Fernandes 2010; French 2013; Hopman‐Rock 2000; Kao 2012; Mikesky 2006), three provided Tai Chi (Fransen 2007; Wang 2009; Yip 2007), and two provided yoga (Cheung 2014; Park 2014). One study provided water‐based exercise (Kim 2012).
Thirteen studies had interventions with an educational component. Seven studies delivered educational interventions aimed at enhancing coping strategies and self‐efficacy (Bennell 2016; Fernandes 2010; Hurley 2007; Keefe 2004; Park 2014; Schlenk 2011; Yip 2007); five studies provided one‐off sessions on a range of topics such as types of OA, risk factors, pain management of OA, problem solving and self‐efficacy (Aglamis 2008; Hopman‐Rock 2000; Kao 2012; Kim 2012; Sullivan 1998); and one study provided patient information leaflets about OA (French 2013).
Activities carried out within the exercise programmes varied across the studies. More common interventions included walking or cycling (or both) for aerobic exercise, and isotonic exercises (i.e. incorporating movement) such as knee extensions and step‐ups for strength training. Combinations of different exercise protocols were widely utilised, and the attributes of these (exercises, sets and repetitions, location and frequency of exercise sessions) varied from study to study.
Format and setting
Twelve studies delivered exercise interventions in a group format (Cheung 2014; Fransen 2007; Hopman‐Rock 2000; Hurley 2007; Kao 2012; Keefe 2004; Kim 2012; Mikesky 2006; Park 2014; Sullivan 1998; Wang 2009; Yip 2007). Seven studies delivered exercise as one‐to‐one sessions either at home or at a facility (Baker 2001; Bennell 2014; Bennell 2016; Focht 2005; French 2013; Péloquin 1999; Schlenk 2011). Two studies comprised of group‐based sessions and an individual physical therapy (Fernandes 2010; Hurley 2007). It was unclear in one study in which format the exercise was delivered (Aglamis 2008). In six studies, the interventions contained elements of behaviour‐graded exercise with an individualised exercise programme for each participant (Aglamis 2008; Baker 2001; Fernandes 2010; French 2013; Hurley 2007; Kao 2012).
Only two of the qualitative studies involved a water‐based exercise intervention (Moody 2012; Larmer 2014b), four studies were land‐based exercise interventions (Campbell 2001; Hinman 2016; Hurley 2010; Veenhof 2006), two studies were home‐based (Campbell 2001; Hinman 2016), and two studies were in primary care/community settings (Hurley 2010; Veenhof 2006).
Intervention providers
Fifteen studies delivered the exercise interventions by trained professionals who were fitness/exercise instructors or physiotherapists (Aglamis 2008; Bennell 2014; Bennell 2016; Cheung 2014; Fernandes 2010; French 2013; Hopman‐Rock 2000; Hurley 2007; Kao 2012; Keefe 2004; Kim 2012; Mikesky 2006; Park 2014; Schlenk 2011; Sullivan 1998). In two studies involving Tai Chi used instructors who were qualified Tai Chi Masters (Fransen 2007; Wang 2009), and one study used a nurse specially trained to deliver Tai Chi (Yip 2007). The remaining three studies did not state who delivered the interventions (Baker 2001; Focht 2005; Péloquin 1999).
Excluded studies
A total of 395 studies did not meet the eligibility criteria and were excluded from the review. For brevity, a sample of 62 excluded studies and their reasons are shown in the Characteristics of excluded studies table.
Risk of bias in included studies
The risk of bias is summarised in Table 3 and also shown in the 'Risk of bias' graph in Figure 3 and the 'Risk of bias' summary in Figure 5.
Table 1.
Quality of evidence ‐ dependability and credibility ‐ of the qualitative studies
| No | Study | Quality of evidence | |||||
| Dependabilityof findings | Credibilityof findings | ||||||
| Author | Low | Medium | High | Low | Medium | High | |
| 1 | Campbell 2001 | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ |
| 2 | Fisken 2016 | ‐ | ✔ | ‐ | ‐ | ✔ | ‐ |
| 3 | Hendry 2006 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ |
| 4 | Hinman 2016 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ |
| 5 | Hurley 2010 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ |
| 6 | Larmer 2014b | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ |
| 7 | Moody 2012 | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ |
| 8 | Morden 2011 | ‐ | ‐ | ✔ | ‐ | ✔ | |
| 9 | Petursdottir 2010 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ |
| 10 | Stone 2015 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ |
| 11 | Thorstensson 2006 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ |
| 12 | Veenhof 2006 | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ |
Figure 5.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
The assessment of the quality of the design and risk of bias of the quantitative studies included in this review are presented in the Characteristics of included studies table and Table 3.
Allocation
Six studies had a high or unclear level of allocation bias. The methods used to generate the randomisation were unclear and therefore introduced a risk of bias in five of the 21 studies (Hopman‐Rock 2000; Kao 2012; Keefe 2004; Kim 2012; Schlenk 2011). Allocation in one study was partly based on people with more severe Alzheimer's being unsuited to the intervention thus introduced bias, and the procedure for allocation may have given some participants an increased chance of choosing a particular condition, creating high risk of bias (Park 2014).
Allocation concealment was poorly described, giving a high risk of bias in 11 studies (Focht 2005; Hopman‐Rock 2000; Kao 2012; Keefe 2004; Kim 2012; Mikesky 2006; Park 2014; Péloquin 1999; Schlenk 2011; Sullivan 1998; Yip 2007). The remaining studies were at low risk of allocation concealment.
Blinding
Twenty of the studies did not conduct blinding of participants due to the difficult nature of blinding to exercise interventions. However, one study used an innovative sham treatment design, with participants not identifying beyond numbers expected by chance whether their treatment was sham or genuine (James test), thus reducing risk of bias for participants (Bennell 2014), although exercise participants were not blinded to their intervention. Eight of the studies did not blind the outcome assessors and so had a high risk of bias (Baker 2001; French 2013; Kao 2012; Keefe 2004; Kim 2012; Schlenk 2011; Sullivan 1998; Yip 2007). All studies utilised participant self‐report scales, and since there were no attempts to blind participants in 20 of the 21 studies, this may have led to reporting bias.
Incomplete outcome data
Three studies had a high risk of bias for incomplete outcome data (Kao 2012; Park 2014; Yip 2007). Five studies were at unclear risk of bias (Aglamis 2008; Kim 2012; Mikesky 2006; Péloquin 1999; Sullivan 1998). The remaining studies were at low risk of attrition bias.
Selective reporting
All the studies reported all the outcomes mentioned in their methods sections giving them all a low risk of bias in selective reporting.
Other bias
One study was at unclear risk of other bias as the authors reported no statistically significant baseline differences between groups but did not report the values (Schlenk 2011). The remaining studies were at low risk of other bias.
Threats to rigour of qualitative studies
Rigour of qualitative studies
Table 2.
Quality appraisal of qualitative studies
| Quality appraisal question | Answer options | |||
| Not at all/not stated | Few steps | Several steps | A thorough attempt | |
| 1. Were steps taken to increase rigour in sampling? | 0 studies | 1 study Thorstensson 2006 |
7 studies Fisken 2016; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Stone 2015 |
4 studies Campbell 2001; Hendry 2006; Hinman 2016; Veenhof 2006 |
| 2. Were steps taken to increase rigour in data collection? | 0 studies | 0 studies | 7 studies Campbell 2001; Fisken 2016; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Veenhof 2006 |
5 studies Hendry 2006; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006 |
| 3. Were steps taken to increase rigour in data analysis? | 0 studies | 0 studies | 6 studies Campbell 2001; Fisken 2016; Hurley 2010; Larmer 2014b; Moody 2012; Stone 2015 |
6 studies Hendry 2006; Hinman 2016; Morden 2011; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 |
| Quality appraisal question | No grounding | Limited grounding/support | Fairly well grounded | Well grounded/supported |
| 4. Were the findings of the study grounded in/supported by data? | 0 studies | 0 studies | 4 studies Campbell 2001; Fisken 2016; Moody 2012; Veenhof 2006 |
8 studies Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006 |
| Quality appraisal question | Limited breadth and depth | Good/fair breadth, limited depth | Good/fair depth, limited breadth | Good/fair breadth and depth |
| 5. Breadth and depth of findings? | 0 studies | 3 studies Fisken 2016; Larmer 2014b; Petursdottir 2010 |
3 studies Moody 2012; Morden 2011; Veenhof 2006 |
6 studies Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Stone 2015; Thorstensson 2006 |
| Quality appraisal question | Not at all | A little | Somewhat | A lot |
| 6. To what extent did the study privilege the perspectives and experiences | 0 studies | 0 studies | 6 studies Fisken 2016; Hurley 2010; Moody 2012; Morden 2011; Thorstensson 2006; Veenhof 2006 |
6 studies Campbell 2001; Hendry 2006; Hinman 2016; Larmer 2014b; Petursdottir 2010; Stone 2015 |
Dependability of qualitative studies
See Table 3.
Sampling
Eleven of the 12 studies were judged to have made a thorough attempt (Campbell 2001; Hendry 2006; Hinman 2016; Veenhof 2006) or took several steps (Fisken 2016; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Stone 2015), to increase rigour in the sampling process (Table 4). Studies attempted to sample a diverse range of participants to represent geographic or socioeconomic diversity, or both. Participant recruitment strategies included sampling from the wider community, two or more GP surgeries or through existing evaluations of exercise programmes. Only one study was judged as making a 'few steps' because of lack of detail in their reporting (Thorstensson 2006).
Data collection
Five studies were judged to have made a thorough attempt to increase rigour in the collection of data (Hendry 2006; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006) (Table 4). These studies described how they put interviewees "at ease," such as offering people a choice of interview venue (e.g. at home or in the workplace). Two studies also attempted to enhance the validity of their study by using more than one method of data collection to triangulate their findings, for example by conducting indepth interviews and a focus group (Hendry 2006) or diary study (Morden 2011). The remaining seven studies had taken several steps to increase rigour of data collection (Campbell 2001; Fisken 2016; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Veenhof 2006). These studies also used indepth or semi‐structured interviews methods with the option of raising "off topic schedule" issues of relevance to participants (Table 4).
Data analysis
Six studies had made a thorough attempt (Hendry 2006; Hinman 2016; Morden 2011; Petursdottir 2010; Thorstensson 2006; Veenhof 2006), and a further six studies had made several attempts (Campbell 2001; Hurley 2010; Fisken 2016; Larmer 2014b; Moody 2012; Stone 2015) to increase rigour in the analysis (Table 4). All studies used an established method for analysing qualitative data (e.g. thematic analysis, constant comparative approach or grounded theory approaches) involving two or more researchers coding and comparing their analysis. Studies judged to have made a thorough attempt adopted additional strategies designed to increase validity and dependability such as presenting emerging findings to interviewees or peers to obtain further feedback and refine their analysis.
Supported by/grounded in the data
All studies were judged to have been at least well grounded (Hinman 2016; Hurley 2010; Hendry 2006; Larmer 2014b; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006) or fairly well grounded (Campbell 2001; Fisken 2016; Moody 2012; Veenhof 2006) with supporting data (Table 4). All studies provided a clear demarcation between participant's views and the author's description and interpretation of findings, with quotes from participant to show how the authors arrived at their findings.
Breadth and depth
Six studies provided both breadth and depth in their findings (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Stone 2015; Thorstensson 2006) (Table 4). Three reported indepth findings but did not cover a wide range of themes (i.e. depth but little breadth) (Moody 2012; Morden 2011; Veenhof 2006). The remaining three studies described a range of barriers and facilitators relevant to answering the review question, but did not report them indepth (Fisken 2016; Larmer 2014b; Petursdottir 2010).
Perspectives
The remaining quality criteria assessed the extent to which studies privileged the perspectives and experiences of older people living with knee or hip OA (or both) (Table 4). Studies were rated highly, being judged as privileging older people's perspectives "somewhat" (Fisken 2016; Hurley 2010; Moody 2012; Morden 2011; Thorstensson 2006; Veenhof 2006) or "a lot" (Campbell 2001; Hendry 2006; Hinman 2016; Larmer 2014b; Petursdottir 2010; Stone 2015).
Dependability and credibility of qualitative studies
None of the studies included in the qualitative synthesis were at low quality when assessing their dependability or credibility (Table 3). All studies took steps to ensure methodological reliability by reducing threats to rigour and were judged to be of high (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006) or medium (Fisken 2016; Moody 2012; Veenhof 2006) quality (dependability). All studies provided useful evidence to answer the review question on participant's experiences of exercise‐based rehabilitation programmes; nine studies were judged at high quality (Hendry 2006; Hinman 2016; Hurley 2010; Moody 2012; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006; Veenhof 2006), and three studies were judged at medium quality (Campbell 2001; Fisken 2016; Larmer 2014b) (Table 3).
Studies by review authors
One qualitative study (Hurley 2010) and three strands of a quantitative study (Hurley 2007) were authored by a member of the review team. Assessment of these papers was carried out by other members of the team. As any contributor would be a named author, it was not possible to achieve a completely independent review.
Effects of interventions
See: Table 1
1. Quantitative synthesis: effectiveness of exercise programmes
Extraction of statistics. In the meta‐analyses the four three‐arm studies that compared two active arms to a control had their control groups artificially regarded as being split in half (labelled (a) and (b)) to avoid double‐counting (Focht 2005; French 2013; Hurley 2007; Keefe 2004) (according to Higgins 2011b), giving 21 comparisons in the meta‐analyses ('Analysis 1.1' to 'Analysis 1.10').
Assumptions. One trial provided 95% CIs of various outcomes (WOMAC, global assessment, chair stand, CES‐D, SF‐36, six‐minute walk test, balance and self‐efficacy) over repeated measurements weekly to 12 weeks, then at 24 and 48 weeks' follow‐up (Wang 2009). There was no loss to follow‐up, so the stable CIs can be interpreted as stable SDs, and so we assumed this to be the case wherever SDs at endpoint were not provided, and substituted the baseline statistics. One trial reported baseline and change, which were suggestive of a mostly symptom‐free sample of participants with small mean changes, which led us to assume constant SDs (Mikesky 2006).
One trial provided outcomes in terms of mean change from baseline and t‐statistics, and to convert this to SDs at endpoint requires information on the baseline‐endpoint correlation, which is rarely given in RCT publications (Wang 2009). Testing different values with the statistics from the three studies suggested that the correlation was between 0.5 and 0.7, and so we assumed it to be 0.6 wherever required.
Subgroup analyses. We were unable to carry out subgroup analyses by age, gender and severity of symptoms due to the paucity of detail in the papers regarding these measures. However, we utilised subgroup analyses with respect to two trials with unusual characteristics. One trial used a depression scale in a long‐established Korean translation, and had an unusually large SMD, so we analysed it in its own subgroup (Kim 2012). One trial reporting SF‐36 quality of life using a validated Turkish translation reported unusually high improvements in the active group and unusually large deteriorations in the control group (Aglamis 2008). It was unclear why this study was so unlike the others reporting SF‐36 and so we analysed it in its own subgroup.
Major outcomes
Pain
Nine trials reported WOMAC pain (11 comparisons; 1058 participants), and their pooled effect showed exercise had a statistically significant effect on pain reduction and had low heterogeneity (SMD ‐0.33, 95% CI ‐0.46 to ‐0.21; I2 = 23%; Analysis 1.1). Other pain outcomes, reported by 10 trials (12 comparisons), also favoured exercise but their pooled effect was not statistically significant and had moderate heterogeneity (SMD ‐0.07, 95% CI ‐0.19 to 0.05; I2 = 69%). Pooling the pain results from all 19 trials (23 comparisons) showed exercise had a statistically significant effect on pain reduction with moderate heterogeneity (SMD ‐0.20, 95% CI ‐0.28 to ‐0.11, I2 = 62%).
Analysis 1.1.

Comparison 1 Exercise versus control, Outcome 1 Pain.
Physical function
The 13 trials (16 comparisons; 1599 participants) reporting WOMAC function had a statistically significant pooled effect favouring exercise (lower WOMAC function score represented greater function) with moderate heterogeneity (SMD ‐0.27, 95% CI ‐0.37 to ‐0.17; I2 = 45%; Analysis 1.2).
Analysis 1.2.

Comparison 1 Exercise versus control, Outcome 2 Physical function.
Self‐efficacy
Eleven trials (13 comparisons; 1138 participants) reported nine different outcome measures of self‐efficacy, so meta‐synthesis was challenging. The pooled effect showed exercise increased self‐efficacy and the trials had low heterogeneity (SMD 0.46, 95% CI 0.34 to 0.58; I2 = 54.9%; Analysis 1.3). Focht 2005 reported two different measures, six‐minute walk and stair climb. To avoid duplication from the same sample, we used the six‐minute walk data as this was the more common measure.
Analysis 1.3.

Comparison 1 Exercise versus control, Outcome 3 Self‐efficacy (SE).
Depression
Six trials (8 comparisons; 806 participants) indicated exercise had no effect on depression (SMD ‐0.09, 95% CI ‐0.24 to 0.05; I2 = 0%; Analysis 1.4). The inclusion of Kim 2012 (70 participants) resulted in an effect; heterogeneity increased markedly but remained low (SMD ‐0.16, 95% CI ‐0.29 to ‐0.02; I2 = 36%).
Analysis 1.4.

Comparison 1 Exercise versus control, Outcome 4 Depression.
Anxiety
Four trials (six comparisons; 704 participants) reported anxiety; their pooled effect suggested exercise did not affect anxiety (SMD ‐0.11, 95% CI ‐0.26 to 0.05, I2 = 0%; Analysis 1.5).
Analysis 1.5.
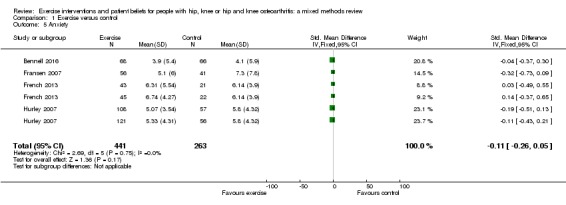
Comparison 1 Exercise versus control, Outcome 5 Anxiety.
Quality of life
SF‐36 social function
Four trials (five comparisons) showed exercise had a statistically significant benefit for social function (MD 6.58, 95% CI 2.78 to 10.38; I2 = 0%; Analysis 1.9). Aglamis 2008 had a large statistically significant effect (MD 58.30, 95% CI 34.58 to 82.02). The overall finding was not affected if Aglamis 2008 was included, but heterogeneity increased substantially (MD 7.87, 95% CI 4.12 to 11.62, I2 = 75%; 576 participants).
Analysis 1.9.

Comparison 1 Exercise versus control, Outcome 9 SF‐36 social function.
Adverse effects of exercise
None of the studies reported adverse effects of exercise.
Minor outcomes
Stress
Two trials (two comparisons; 206 participants) measured stress, which decreased following exercise (MD ‐4.76, 95% CI ‐7.57 to ‐1.95; Analysis 1.6).
Analysis 1.6.

Comparison 1 Exercise versus control, Outcome 6 Stress.
Quality of life
SF‐36 mental health
Although the pooled effect of four trials (five comparisons) appeared statistically significant (MD 2.90, 95% C 0.15 to 5.65, I2 = 36%; Analysis 1.7), the low heterogeneity of the studies except for one unusual outlier means this result should be treated with some caution. In one trial (25 participants), exercise improved SF‐36 mental health substantially alongside very small SDs; the reason for this was unclear (MD 32.90, 95% CI 23.07 to 42.73) (Aglamis 2008). Including Aglamis 2008 with the other trials raised the pooled effect, but heterogeneity increased substantially (MD 5.07, 95% CI 2.43 to 7.72, I2 = 87%; 576 participants).
Analysis 1.7.

Comparison 1 Exercise versus control, Outcome 7 SF‐36 mental health.
SF‐36 emotional role
There was a non‐significant, uncertain effect in four trials (five comparisons) that measured SF‐36 emotional role (MD 1.76, 95% CI ‐6.63 to 10.14, I2 = 54%; Analysis 1.8); heterogeneity was moderate. Aglamis 2008 had a large statistically significant effect (MD 72.80, 95% CI 47.14 to 98.46). Including Aglamis 2008 increased the estimate of the pooled effect but it remained uncertain, although heterogeneity increased substantially (MD 11.43, 95% CI ‐4.06 to 26.71, I2 = 87%; 576 participants).
Analysis 1.8.

Comparison 1 Exercise versus control, Outcome 8 SF‐36 emotional role.
SF‐36 vitality
Four trials (five comparisons) showed exercise had a statistically significant beneficial effect on SF‐36 vitality (MD 3.90, 95% CI 0.55 to 7.25, I2 = 15%; Analysis 1.10). Aglamis 2008 had a large improvement in vitality (MD 51.90, 95% CI 34.74 to 69.06), but the overall finding was not affected when this study was included, although heterogeneity increased substantially (MD 5.67, 95% CI 2.38 to 8.96, I2 = 85%; 607 participants).
Analysis 1.10.

Comparison 1 Exercise versus control, Outcome 10 SF‐36 vitality.
Sleep
One trial measured sleep (Cheung 2014; 36 participants) and there was no statistically significant difference in sleep quality (MD ‐1.10, 95% CI ‐2.54 to 0.34; Analysis 1.11).
Analysis 1.11.

Comparison 1 Exercise versus control, Outcome 11 Sleep.
2. Qualitative synthesis: people's views on exercise and exercise programmes
This section summarises the findings from 12 studies that reported the perspectives and experiences of older people living with knee or hip (or both) OA and exercise (Campbell 2001; Fisken 2016; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006; Veenhof 2006). The use of a framework synthesis enabled the findings from each of the studies to populate the main concepts outlined in the conceptual framework and supported the identification of additional themes and subthemes, enriching our understanding of the relationship between health beliefs, the psychosocial impact of arthritis and the role of exercise in mediating those impacts (Figure 6). The synthesis was organised according to the final, more detailed conceptual framework and presented themes related to older people's views within the four conceptual areas: (I) symptoms; (II) health beliefs and views on management; (III) psychological factors; and (IV) social and environmental factors influencing engagement in physical activity. CERQual assessments of the findings were carried out, and the findings and assessments are summarised in Table 5.
Table 3.
Summary of qualitative findings and CERQual assessments
| # | Review finding | Relevant papers | CERQual assessment of confidence in the evidence | Explanation of CERQual assessment |
| I. Symptoms | ||||
| Pain, muscle weakness, physical function: the experience of living with pain and its impact dominated people's narratives because it affected most areas of their daily life and became worse over time. Pain levels varied, and were described as episodic and unpredictable. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Morden 2011; Petursdottir 2010; Stone 2015 | High confidence | Low methodological limitations across all studies, with high coherence and high relevance. 3 countries and 4 geographical regions represented by 6 studies. | |
| Capacity to exercise: pain, joint stiffness, fatigue, comorbidity and people's perceptions of their physical fitness, both before and after exercise, restricted the type and amount of exercise people felt able to engage in. Additional efforts required to shower and change exacerbated the difficulties, and people also reported difficulties with fatigue after exercise sessions. | Campbell 2001; Hendry 2006; Hurley 2010; Moody 2012; Petursdottir 2010; Thorstensson 2006 | High confidence | Low methodological limitations for 5 of the 6 studies, high relevance for 5 of the 6 studies, and high coherence. 4 countries and 2 geographical regions represented. | |
| Impact of exercise on the effects of OA: some participants reported dramatic improvements in symptoms as a result of exercising, while some felt there was little or no benefit. Some people believed other treatment routes were more effective. However, for those who did benefit from exercise, function was improved and pain reduced allowing a return to more normal day‐to‐day activities that had been avoided. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | Findings applied to 9 studies, 8 having low methodological limitations and 6 having high relevance. Moderate coherence across the studies. 6 countries and 2 geographical regions represented. | |
| II Health beliefs and views on the management of OA | ||||
| Aetiology and prognosis of OA: people considered OA to be an inevitable result of placing stress on their joints, the ageing process or a hereditary condition, with limited hope of improvement. Expectations that the condition would worsen over time made it difficult to convince people of the scope for improvement through appropriate treatment. | Campbell 2001; Hendry 2006; Hurley 2010; Morden 2011 | Low confidence | 4 studies representing 2 countries from 2 different geographical regions. Methodological limitations low across all studies, relevance high in 3 of the 4 but medium coherence. | |
| Non‐exercise management strategies: some people's understanding of how to manage their OA condition was limited to medication (analgesia) or surgery with little awareness of the role of exercise. Views on pain medication and surgery were mostly negative, with concerns of becoming addicted (to medication) and mixed views and hesitancy regarding surgery, with some people unsure it would work while others considered it a worthwhile option. There was a keenness to delay surgery as long as possible. | Campbell 2001; Hendry 2006; Hurley 2010 | Low confidence | Low methodological limitations, but only 3 studies with medium‐to‐high relevance and medium coherence, all from the same country. | |
| Advice and information from health professionals: participants described their experiences of receiving advice and information from health professionals. This was wide‐ranging in its usefulness and detail for people, and some formed negative beliefs due to limitations of the information they were provided with. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Thorstensson 2006 | Medium confidence | Low methodological limitations, high relevance in 5 of the 6 studies, 3 geographical regions represented by 4 countries. Medium coherence. | |
| Health beliefs and managing OA and exercise: attitudes towards exercise in OA were found to be closely linked to beliefs and perceptions regarding aetiology. Negative beliefs were widely held about the OA prognosis which in turn demotivated them from active management of the condition. Some were concerned about exacerbating the condition, and some felt they were too old for exercise to be of benefit. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Thorstensson 2006 | High confidence | Low methodological limitations across the 6 studies with high relevance for all except 1. Medium‐to‐high coherence. 4 countries and 2 geographical regions represented. | |
| Everyday activities (physical activity) versus structured exercise: this relates to whether people felt that general physical activities that took place in everyday life were sufficient to manage OA, or whether structured exercise sessions had additional benefits. Some people did not perceive a difference between the two, and did not see a need for structured exercise, while others felt normal daily activity was insufficient and needed to be supplemented with formal exercise. Some people worked to increase their general physical activity levels in the belief it would be helpful for their OA. | Hendry 2006; Moody 2012; Petursdottir 2010; Thorstensson 2006 | Low confidence | Low methodological limitations in 3 of only 4 studies, 2 regions and 4 countries represented, with high relevance but only medium coherence. | |
| III Psychological factors | ||||
| Impact of OA on people's sense of "self": the limitations of OA meant that activities that people had previously defined themselves by were now compromised. A new sense of self needed to be constructed to help overcome the negative psychological effects of this, taking on alternative social roles to ensure they maintained a sense of purpose and remained 'useful' despite incapacitation. Those who struggled to do so expressed negative emotions and the feeling of being a burden and frustrated with their limitations. | Hurley 2010; Morden 2011; Petursdottir 2010; Stone 2015 | High confidence | 4 studies with low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Individual disposition: high self‐efficacy and a positive outlook was seen as vital in ensuring people did not become defined by their OA. This involved the determination to find new ways to cope. Where self‐efficacy was low, there was an avoidance of physical activity because of the belief it would aggravate pain levels. | Petursdottir 2010; Stone 2015 | Low confidence | 2 studies, from 2 countries/regions with good methodological rigour and high relevance overall. However, medium coherence and lack of confidence in this review finding due to paucity of data. | |
| Psychological benefits of exercise: people reported favourable psychological benefits of exercise. They also appreciated the peer support and social opportunities that accompanied group forms of exercise. | Fisken 2016; Hendry 2006; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Thorstensson 2006 | High confidence | 8 studies with overall low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Influence of programme supervisors: people who undertook supervised exercise programmes valued programme providers who understood their condition and encouraged and facilitated their engagement in exercise. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | 9 studies with overall low methodological limitations. Highly relevant data from 5 countries and 2 geographical regions. High coherence. | |
| IV Social and environmental factors | ||||
| Impact of OA on people's sense of "self": the limitations of OA meant that activities that people had previously defined themselves by were now compromised. A new sense of self needed to be constructed to help overcome the negative psychological effects of this, taking on alternative social roles to ensure they maintained a sense of purpose and remained 'useful' despite incapacitation. Those who struggled to do so expressed negative emotions and the feeling of being a burden and frustrated with their limitations. | Hurley 2010; Morden 2011; Petursdottir 2010; Stone 2015 | High confidence | 4 studies with low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Individual disposition: high self‐efficacy and a positive outlook was seen as vital in ensuring people did not become defined by their OA. This involved the determination to find new ways to cope. Where self‐efficacy was low, there was an avoidance of physical activity because of the belief it would aggravate pain levels. | Petursdottir 2010; Stone 2015 | Low confidence | 2 studies, from 2 countries/regions with good methodological rigour and high relevance overall. However, medium coherence and lack of confidence in this review finding due to paucity of data. | |
| Psychological benefits of exercise: people reported favourable psychological benefits of exercise. They also appreciated the peer support and social opportunities that accompanied group forms of exercise. | Fisken 2016; Hendry 2006; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Thorstensson 2006 | High confidence | 8 studies with overall low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Influence of programme supervisors: people who undertook supervised exercise programmes valued programme providers who understood their condition and encouraged and facilitated their engagement in exercise. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | 9 studies with overall low methodological limitations. Highly relevant data from 5 countries and 2 geographical regions. High coherence. | |
CERQual: Confidence in the Evidence from Reviews of Qualitative Research; OA: osteoarthritis.
Figure 6.

Emergent themes from qualitative synthesis. OA: osteoarthritis.
Some of the exercise activities were clearly comparable with studies in the quantitative analysis: Hurley 2010, Moody 2012, and Veenhof 2006 all drew their samples from people taking part in studies included in the quantitative analysis. Participants in Hendry 2006 and Morden 2011 had not necessarily taken part in exercise, while participants in Campbell 2001, Petursdottir 2010, and Thorstensson 2006 had taken part in exercise programmes, but these were not described in sufficient detail to compare them with programmes in the quantitative studies.
I. Symptoms: pain, muscle weakness, physical function
In six studies, people's descriptions and experiences of pain and its impact dominated their narratives of living with OA because it affected most areas of their daily life, in a variety of ways (Campbell 2001; Hendry 2006; Hurley 2010; Morden 2011; Petursdottir 2010; Stone 2015). Although pain varied greatly within and between people, most described pain as being episodic, very unpredictable (Hurley 2010; Petursdottir 2010; Morden 2011) with its severity varying greatly from day to day (Campbell 2001; Hendry 2006; Hurley 2010; Petursdottir 2010; Morden 2011; Moody 2012; Morden 2011). For many people, the impact of pain on their physical function, mobility and wider aspects of their lives made arthritis a life‐changing condition, whose symptoms gradually increased over time (Campbell 2001; Hendry 2006; Hurley 2010): "…it got worse and worse and I started falling down…" (Campbell 2001, p.155). They talked about how this made even the most common activities of daily life difficult to perform; "I'm always in pain and agony, every movement is a chore. Sometimes, I just stare at my stairs, dreading what comes next" (Stone 2015). "…I can't walk as fast or as far as I used to because my knee hurts…" (Hendry 2006, p.560); "…getting out of bed, getting going, turning over in bed, waking up in the night…getting in and out of the car is a nightmare…" (Hurley 2010, p.5). People had adjusted their daily activities and routines to cope with their pain and reduced physical capabilities (Petursdottir 2010; Morden 2011): "…re‐arranging the order of kitchen shelving or altering walking routes to avoid hills if they found them problematic…" (Morden 2011, p.194).
Capacity to exercise
Six studies commented on how pain, joint stiffness, fatigue, comorbidity and people's perceptions of their physical fitness restricted the type and amount of exercise people could do (Campbell 2001; Hendry 2006; Hurley 2010; Moody 2012; Petursdottir 2010; Thorstensson 2006). People who reported feeling pain and fatigue afterwards felt less able to exercise (Hurley 2010); "…anything that would jog or jar my knee would really hurt…it's hard to get going on a bike and very painful…" (Hendry 2006, p.560). The severity of symptoms and their perceived physical capacity not only limited people's ability to exercise, but also affected their ability to carry out sustained and regular exercise (Campbell 2001; Moody 2012). The hope of reducing pain could be a motivating factor in increasing the likelihood of exercise. However, the variability of pain often meant people could not get into a regular exercise routine, but had to "adapt their exercise pattern to their levels of pain" (Petursdottir 2010, p.1020). Some people avoided exercise because of the additional time, effort and fatigue associated with exercise: "…the effort to get clean afterward is really hard…you just don't have the energy to take a shower…" (Petursdottir 2010, p.20); "…that's why I missed some of them. I couldn't go [to] more than one because I was just so tired the next day…" (Moody 2012, p.67). Some people also said old age limited what they could do and prevented exercise from helping them; "…I've reached an age where exercise doesn't help…I just get tired; I'm not fit and agile enough to do exercises…" (Hendry 2006, p.560). The physical and mental impact of comorbidity common in elderly people was also cited as a reason for impairing people's ability and desire to exercise (Campbell 2001; Hendry 2006).
Impact of exercise on the effects of osteoarthritis
Ten studies described the impact exercise could have on people's physical symptoms (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Stone 2015; Thorstensson 2006; Veenhof 2006). Some participants reported dramatic improvement in pain and physical function; "…the exercises we did at [centre]were helping and see I haven't had the pain…it was very helpful" (Hurley 2010, p.7), "the physiotherapist professionally guided me to feel less pain" (Stone 2015, p.14), "…exercise is the best thing for relieving pain…" (Hendry 2006), "at least 50% difference in the stiffness" (Larmer 2014b, p.91). However, other people found little or no benefit; "…exercise doesn't help my knees at all…" (Hendry 2006, p.561), or that exercise exacerbated pain; "In my case…the damage became worse, it only led to more pain instead of improvement'' (Thorstensson 2006, p.56). Some people considered other treatment options to be more relevant; "it [the exercise] was beneficial and it helped in the short term. However, had I not received injections I would never have been able to work for so long. It is thanks to them that I have been able to work for the past five or six years or since I got osteoarthritis. That is a fact" (Thorstensson 2006, p.56).
For people who found exercise beneficial, the reduced pain resulted in improved physical functioning enabling people to perform common daily or recreational activities they had previously avoided or given up to avoid aggravating their symptoms. Such improvements returned a degree of normality to people's lives, "…for example, walking longer distances, there are limits, but nevertheless longer walks without experiencing pain. It is a huge difference. So it was very positive…it makes it possible to work more and you can do more enjoyable things too…" (Thorstensson 2006, p.55); "…walking up stairs, I mean, at times I used to have to go up one step at a time, but then after the exercise I could just walk up the stairs and I was even beginning to try to walk normal…" (Hurley 2010, p.7); "The pain is different pain and I feel that I can do things easier now than I could a while back" (Hinman 2016, p.486).
Exercise was also perceived to have general health benefits including improvement in breathing, balance, sleeping and a reduction in falls (Campbell 2001; Moody 2012); "…since I started strengthening these muscles it seems I don't fall over so much which is good…it's so embarrassing…" (Campbell 2001, p.135); "…exercise has a good affect [effect] on everything including the heart" (Petursdottir 2010, p.1020). It was also possible for people to experience improved function and mobility but for pain to persist; "…exercise doesn't help pain but it gets it going, improves stiffness and mobility…" (Hurley 2010, p.562).
Many people stopped exercising after completing a programme (Campbell 2001; Hendry 2006; Hurley 2010; Thorstensson 2006 p.55), some because the perceived benefits were insufficient to warrant the time and effort invested; "…I was able to [exercise]pretty easily but it didn't appear to me to make a lot of difference…I carried them on during the time I was taking part in the programme although I've dropped them since…" (Campbell 2001, p.136).
II. Health beliefs and views on the management of osteoarthritis
Aetiology and prognosis of osteoarthritis
Four studies explored people's beliefs about the cause of OA (Campbell 2001; Hendry 2006; Hurley 2010; Morden 2011). Many people believed OA to be a normal part of the ageing process and a result of the 'wear and tear' on their joints incurred during occupational (Campbell 2001) and leisure activities or following injury (Hendry 2006; Hurley 2010; Morden 2011), "…I think it's just wear and tear. I think it's just accepted that you're going to get these things as you get older…" (Hurley 2010). Some people thought OA was hereditary and recalled relatives who had joint problems (Hurley 2010), others attributed it to excess bodyweight increasing the stress and strain on joints (Campbell 2001; Hendry 2006). Fatalistic views often made it difficult to convince people that things could be done to improve the prognosis of their symptoms; "…nothing will stop it getting worse I'm sure…" (Hurley 2010, p.5).
Non‐exercise management strategies
Three studies explored people's views of management strategies and found these were usually limited to medication (analgesia) and surgery (Campbell 2001; Hendry 2006; Hurley 2010), with little or no awareness of other management options, such as exercise (Hurley 2010). While many people believed medication could alleviate symptoms and used analgesia to manage severe pain, generally people disliked taking medication and often put up with pain; "I am not a one for taking a lot of tablets. I get a bit dubious, you know, so I just learnt to live with it for a bit" (Campbell 2001, p.134). People were reluctant to use medication because of concerns about the adverse effects, becoming "addicted" to medication and reduced effectiveness if taken regularly (pharmacological tolerance) (Campbell 2001; Hurley 2010); "…I do really try to keep off drugs because, you know, I mean I think that they all have side effects…" (Hurley 2010, p.5). People also avoided medication because they thought pain was a warning sign of further joint damage, and taking medication that suppressed this warning might make the problem worse; "…I'm not keen to take things because they're not going to cure it, and I mean to hide it is not strictly a good idea because you do things and it makes it worse…" (Hendry 2006, p.561).
One study described people's different attitudes towards surgery. Some people thought surgery the best way to correct the damaged caused by OA, eliminate pain, and restore mobility and function, others were more sceptical (Hurley 2010). People's views on surgery were influenced by the experiences of family and friends, reports in the media or the presence of comorbidities; "…I don't want knee surgery, I've seen it happen; I've seen people have it very successfully and I've seen it be a disaster" (Hurley 2010). Most people wanted to delay surgery for as long as possible; "…I'd have to be a lot worse than what I am now I think…well I mean if I've gone for thirty years I can go on for a few more…" (Hurley 2010, p.5).
People also reported using conservative, non‐pharmacological interventions such as acupuncture, osteopathy, herbal remedies and supplements, on the recommendations of family, friends, advertisements and media reports. While some people believed these to be helpful, others were unconvinced, but often continued taking them in the hope that they would slow the progression of the disease (Hurley 2010).
Advice and information from health professionals
Six studies reported the advice and information derived from health professionals (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Stone 2015). People often formed beliefs about OA in the early stages of the diagnosis process, sometimes with little or no advice or information from health professionals, leaving them ill‐informed about the aetiology of OA and appropriate management strategies (Campbell 2001; Hendry 2006; Hurley 2010; Petursdottir 2010; Stone 2015); "When I was first diagnosed, I didn't know what to think. I knew it wasn't good,… And no one warned me I didn't even know what to do…exercise was the farthest thing from my mind" (Stone 2015, p.6); "…[doctor] never said anything, that's why I have always thought it's not worth bothering about. He's not bothered so I am not bothered…" (Hurley 2010, p.5). Few people reported having received advice about exercise; "…I haven't had any advice about exercising and what exercises to do…" (Hendry 2006, p.561), or further guidance; "they [the physicians] are positive if you ask [for a referral to a physical therapist], but you have to ask" (Petursdottir 2010, p.1021).
Where information about exercise was provided, it was often vague, unclear and conflicting. Hendry and colleagues reported one participant had been advised to exercise; "…my doctor told me to keep exercising and not to stop…" (Hendry 2006, p.561), while another participant had been discouraged from exercising, "…they [doctor] said, ‘the walking's agitating you, your joints, so stop it'…" (Hendry 2006, p.561). Negative encounters with health professionals reinforced people's negative beliefs about exercise and their views that very little could be done; "So I go to the doctor and all he just simply done was put his hand on my knee, he said 'move your leg…you are getting old you've got rheumatism.' You see that was it I didn't take any more notice of it [the knee pain]" (Campbell 2001, p.135).
Conversely, provision of good advice and information positively influenced people's attitudes and behaviours towards exercise and its benefits (Campbell 2001; Hendry 2006; Hurley 2010; Petursdottir 2010; Stone 2015). Information was an important form of support that taught people about their condition and how to manage and cope with it (Hurley 2010); "…I learned so much from [the physiotherapist]…I learnt about pain management…it helped me understand arthritis much better…" (Hurley 2010, p.7). Many participants commented, "If my doctor tells me to [exercise], then I will" (Stone 2015). Information was viewed as invaluable when it came from someone people considered a knowledgeable healthcare professional who explained why the person was being asked to do something; tailored the advice to the recipient's individual context, experiences and condition; clearly specified what (not) to do; and that adhering to the advice brought benefits (Hendry 2006; Hurley 2010; Petursdottir 2010); "…I had to stick rigidly to what he had said, the weights that he had specified…the idea was to stretch it that little bit further than I normally would do in order to support the joint more…but too much would…cause more damage and not enough wouldn't do any good…I was quite impressed actually by his knowledge…and I did exactly what he said and I did notice an improvement, a definite improvement…" (Hendry 2006, p.563).
Improvement in people's symptoms and physical activity was often attributed to increased understanding and knowledge gained through information and practical advice delivered by healthcare professionals; "I was a bit sceptical at first and when the exercises came I thought 'hang on, this has got nothing to do with the knee as far I understand' being ignorant, you know. Now I sort of feel that 'hang on, yeah there is a difference' because the work has paid off" (Hinman 2016, p.486); "…now I think I handle it more wisely. I know better because I've been fortunate to get good instruction…" (Petursdottir 2010, p.1020).
Health beliefs and managing osteoarthritis and exercise
Six studies examined people's beliefs about the potential role of exercise in managing OA (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Thorstensson 2006). They suggested people's attitudes towards exercise in the management of OA were closely linked to their beliefs and perceptions about the aetiology of OA and symptoms. All six studies reported people holding some form of negative belief about the cause, prognosis and treatment of OA. People who believed OA was caused by immutable factors, such as ageing or hereditary, tended to be resigned to their problems, weakening their resolve to actively manage it (Campbell 2001); "…there is nothing that can be done about the OA; therefore, I do nothing…" (Petursdottir 2010, p.1021).
While some people considered exercise essential, others held doubts or anxieties about the benefits they might attain from exercise. "There's a basic level of exercise that I have to do to keep the joints flexible, so I can get up and move around" (Hendry 2006, p.562). In contrast, other people were anxious about the possible harm they could cause to themselves by exercising if the activity‐related pain was a signal of causing further damage (Hurley 2010; Thorstensson 2006); "…I'm questioning whether exercise might exacerbate or ease it. I really don't know…" (Hurley 2010, p.5). These doubts and anxieties often meant people avoided exercise (Hurley 2010; Thorstensson 2006). Some people thought they might be too old to benefit from exercise (Campbell 2001); "…[exercise] might not help me because I'm getting old…I just think I'm too old really to improve…" (Campbell 2001, p.135). People who believed excess bodyweight to be a contributing factor to OA thought any improvement would depend on them losing weight (Campbell 2001; Hurley 2010).
Four of the six studies found that after exposure to exercise (either independently or as part of a programme) participants held mostly positive beliefs about the benefits of exercise (Hendry 2006; Hinman 2016; Hurley 2010; Thorstensson 2006); "…I now know that it is beneficial. I know that simply going for a walk every day is very good for me. In that way I have changed. Previously I was not even aware that it was necessary" (Thorstensson 2006, p.53); "I know now it's going to be for my benefit. I keep on doing these exercises…if I stop, pain comes on again, and I can't do any activities" (Hinman 2016, p.485); "So your movement is important; this is why I want to get back into a regular exercise routine, so I can do more to help myself" (Hendry 2006, p.562). Hurley and colleagues was the only study that explored people's beliefs before and after participation in an education‐ and exercise‐based rehabilitation programme, and how and why their beliefs changed (Hurley 2010). Participants' initial fears about the danger of exercise were allayed after experiencing the benefits of exercise on their symptoms without exacerbating pain; "…I thought if I exercise I am going to make the pain worse…they have showed me that I can still exercise even though I have a bad knee…" (Hurley 2010, p.7). They retained their beliefs about the causes of OA, but prior pessimism that nothing could be done to help them was replaced by a more optimistic opinion about the role of exercise in helping them cope with and manage their problems; "…[exercise helps you understand] how to cope with pain…that exercise does help ease the pain and helps your mobility…but there is no cure for [arthritis], it's learning to live with it…" (Hurley 2010, p.7).
Everyday activities (physical activity) versus structured exercise
Four studies highlighted people's differing views about how best to increase physical activity and function, whether it required formal exercise or whether common activities of daily living, such as walking, would suffice (Hendry 2006; Moody 2012; Petursdottir 2010; Thorstensson 2006). Some people did not distinguish between structured physical activity and everyday activities and therefore saw no need to take part in formal exercise. "…I get enough exercise leading an active life…" (Hendry 2006, p.562); "…I really don't think that I need to take some exercise, but I just tell myself that I am going shopping and things like that…" (Thorstensson 2006, p.55), while others felt everyday activities were insufficient; "…day‐to‐day activity isn't enough to keep you mobile…" (Hendry 2006, p.562). People believed increased physical activity was beneficial and attempted to integrate more physical activity into their daily lives and activities; "…I try to walk more and more, to walk in the correct way and to climb stairs in the correct way and not to wear myself out…" (Thorstensson 2006, pp.53‐4).
III. Psychological factors
Impact of osteoarthritis on people's sense of "self"
Four studies contributed to an understanding of the impact of OA on people's sense of self (Hurley 2010; Morden 2011; Petursdottir 2010; Stone 2015). While some people acknowledged the importance of mental health and remaining positive and cheerful (Petursdottir 2010), OA could have a detrimental effect on people's sense of "self" (their view of themselves, their roles, etc.), caused 'biographical disruption' and necessitate them having to reconstruct a new narrative (purpose) for themselves (Morden 2011, p.194). Some people were able to adapt and keep a valued sense of self, other people found it challenging to accept the effects and limitations due to OA, and adapt their existing self‐image. For example, one participant's sense of self as a male provider and head of the family was challenged because of his diminished function, so he renegotiated his sense of self taking on a new "identity" as a carer looking after the home and his grandchildren. Examining how people maintain acceptable social roles, remain 'competent moral actors' and preserve a sense of self may be central to understanding and self‐managing in chronic illness (Morden 2011, p.194). People who felt they were incapacitated and in need of additional help evoked feelings of frustration, anger, depression, embarrassment and being a burden to others (Hurley 2010, p.3); "…I'm very upset with myself cos [because], you know, when you're used to being mobile and able to do things for yourself, now you have to depend on people to do it, it's not very nice is it?…" (Hurley 2010, p.5); "It definitely wears on you, on your mind because it stops you from doing what you want to do. Even if my body wanted to [exercise], my mind won't let me…I feel helpless and worthless" (Stone 2015, p.5). This caused unhappiness, particularly in younger people; "…I was extremely unhappy with myself. I couldn't work as hard as before, and I just could not understand why. It was one of the hardest things, to accept myself as what I had become…" (Petursdottir 2010, p.1019), but older people who attributed OA to ageing accepted its associated problems more readily; "…well, you have to face the fact that you are not young anymore, and you just have to slow down…" (Petursdottir 2010, p.1019).
Individual disposition
Two reports showed the strong influence personal adaptability and initiative had on exercise behaviour (Petursdottir 2010; Stone 2015). A positive outlook was seen as vital in not letting OA define and control people's lives or prevent them continuing with their everyday physical activities (Petursdottir 2010); "…I worked out new ways to cope, to keep my arthritis from getting in the way too much…" (Petursdottir 2010, p.1018). Low self‐efficacy was also a factor highlighted in Stone 2015 as many participants felt "demotivated from physical activity as they did not believe they could successfully perform a task without exacerbating their current pain levels" (p.9). As one participant expressed: "Not only does it hurt when you [move], but it would hurt the next day. The pain never lets you forget…and believe me, I don't. The only thing I can do is not do it again. Avoid exercise, avoid the pain" (Stone 2015, p.9).
Psychological benefits of exercise
Participants in eight studies reported psychological/psychosocial benefits of individual or group exercise (Fisken 2016; Hendry 2006; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Thorstensson 2006). People made notable claims about improvements in their mental state; "…overall I have improved…it's a feeling of general well being really…I feel a lot better in myself, I mean mentally, mostly mentally…" (Hurley 2010, p.1020); "you just feel great when you've done it…you know, they say exercise releases happy something in your brain and it certainly does…" (Hendry 2006, p.560). "Keeps the body moving, takes your mind off it, it's good to be outside. Yea, keeping active, or else if you've got osteo [osteoarthritis], it can get you right down, if you stay inside you just mope about it" (p.15); "…[W]hen I've been walking for a while, the pain goes away, which makes me happy…" (Thorstensson 2006, p.55). Participating in a formal exercise programme was also reported to reduce anxiety and increase confidence to exercise (Hurley 2010).
Programmes that involved group exercise meant people came into contact with other people with OA giving them the opportunity to make friends, share stories and gain peer support, "…I like the gym referral scheme because you're in a group of people who all have problems…" (Hendry 2006, p.562), "…we formed very tightly knit group…we were all trying to help one another, you know" (Hurley 2010, p.7). Being part of a group and having shared experiences made exercise more appealing, and more likely to be perceived as fun and enjoyable rather than a chore (Moody 2012). Choosing independent forms of exercise still provided opportunities for participants to benefit from the social experience of exercise "…when I've been swimming, that it does me good. Plus, I just love it. I enjoy it. It's a social thing as well and I just get so much out of it…I've made new friends and I just find that completely satisfying…" (Morden 2011). Observing improvements in other people participating in exercise programmes was a source of encouragement (Hurley 2010, p.8). Furthermore, group activities helped people realise they were not unique in their difficulties: "It's been an awful shock to get sick…It's been really really difficult, so coming and talking to other people, probably has been almost as beneficial as doing the exercise and realising that you're not the only one" (Larmer 2014b, p.91).
Influence of programme supervisors
In nine of the 12 studies, participants who undertook supervised exercise programmes commented on the importance of individual attributes of programme supervisors, usually physiotherapists (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006). The qualities people liked and derived value from included understanding, tolerance, friendliness, taking a genuine interest in them, encouragement, support and the guidance they received. Good communication skills and a sense of being listened to were also important to them.
Specific instruction on how to exercise alleviated people's anxiety and concern about doing it wrong; "…the gym instructors advise you and give you confidence that you're not going to make things worse…" (Hendry 2006, p.562) and they believed "…someone with a medical background is the best person to supervise exercise…" (Hendry 2006, p.562). Participants appreciated this needed the encouragement from instructors who could, "…jolly you along…" (Moody 2012, p.660) and "…I think it's really a lot, in fact an enormous amount, to do with the facilitator, she's both kind of encouraging and yielding and nurturing and understanding, but also was able to use a bit of steel and get us off our bums…" (Hurley 2010, p.7). Participants were more likely to adhere to an exercise programme if they were 'actively involved in the whole process' working alongside the physiotherapist (Veenhof 2006, p.275). Such partnerships were positive in that they led to feelings of accountability, of not wanting to let down who they were working with, "…I wasn't obligated to do it but I felt let's do my bit towards it, you know. I didn't want her to simply think that she was wasting her time…" (Campbell 2001, p.134). People were motivated by instructors: "The most important thing is listening to the physio [physiotherapist] and doing the exercises because he motivated me to do the exercises" (Hinman 2016, p.486). However, there was also the danger that people became reliant on the instructor to lead the exercise, losing this support when the programme was completed could '…undermine their motivation to exercise…' (Hurley 2010, p.9).
IV. Social and environmental factors
Prioritising exercise
In seven studies, participants commented on how difficult they found it to exercise regularly (Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Moody 2012; Morden 2011; Thorstensson 2006). Many people admitted they did not consider exercise to be a priority citing the demands of work and family life as impinging on their decision not to exercise; "…my job's very important, really important at the moment…" (Morden 2011, p.196), and they struggled to find time to incorporate exercise in their daily routine; "…one is so occupied that it is very easy not to find time for exercise. Everything else takes precedence…" (Thorstensson 2006, p.56). People were often aware their "reasons" for not exercising were often excuses to not exercise and that the real reason was the time and effort of exercising; "…its just excuses really when it comes down to the basics. I mean I could get up in the morning and do it between 6 or 7 or something like that…" (Campbell 2001, p.135). People who considered exercise an important and effective way of managing OA found ways to accommodate regular exercise/physical activity into their daily routines; "…I do the exercises upstairs when I get up in the morning…I find I might have a bit more time, because during the day you tend to let things slide…" (Hurley 2010, p.7); "It's part of life…I get up in the morning, I have a cup of coffee, I take my blood pressure medication, then I go and do my exercises…and I don't have to leave home!" (Hinman 2016, p.486).
The support of family and friends
Four studies looked at the role family and friends played in supporting participants' engagement with exercise (Campbell 2001; Fisken 2016; Petursdottir 2010; Stone 2015). Receiving emotional support, encouragement, approval and reassurance was seen as essential in motivating people to begin and maintain regular exercise. Programmes that allowed a friend or family member to exercise alongside the programme participants were appreciated and meant information provided by healthcare professionals could be reinforced (Hendry 2006). One participant, in the study by Stone 2015, explained, "One of my friends who knows about my arthritis asked me if I ever exercise."Exercise?!"I said, "What could I do with exercise?!"Then she said she would work out with me if I wanted to. That was the first time I ever seriously thought about exercising" pp.15‐6. While the participants in Fisken 2016 noted that when, "you're not stuck at home all the time, it's a way of getting out" finding that, "it's important to be with other people, how other people cope and that you're not alone and there are other people you know, in similar situations" (p.15).
Social characteristics
Two studies briefly explored the influence age on people's exercise behaviour (Fisken 2016; Hendry 2006). Age could act as barrier when participants considered exercise classes as unsuitable for older people: "It's got to be paced at our age range" (Fisken 2016, p.14). The expectation that other exercisers would be young and very fit was challenged: "I imagined…all these fit people you know, bodies like Adonis…I thought that I would be old, that I would show myself up, but in fact it wasn't like that at all…the people who were sort of totally 100% fit were very few and far between" (Hendry 2006 p.563).
Exercise facilities
Six studies investigated the acceptability and accessibility of exercise facilities (Fisken 2016; Hendry 2006; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006). For elderly people, on low incomes and without transport, the cost and location of accessible exercise facilities was important (Moody 2012; Thorstensson 2006), as was their experience of the facilities. The venues had to be convenient so that people "…did not have to travel long distances…" (Thorstensson 2006, p.55), and some people preferred to exercise at home while others found outdoors more convenient (Hendry 2006). Cost was mentioned as a barrier especially for older people on a low or fixed income; "…couldn't probably afford a big amount, twice a week…" (Moody 2012); "I mean some of them charge an awful lot to get in. When you go up to the pool it's $2 and then you get charged $5 to go into the aerobics, well that's really, sort of, you know, pay for the guys time, that person's time but when you're on a pension you haven't got that" (Fisken 2016, p.14), Thus, some people valued non‐paid‐for forms of exercise, such as walking, rather than travelling to attend expensive gyms (Petursdottir 2010, p.2021). However, inclement weather conditions, such as in Iceland, could be a barrier to exercising outside "…high winds and icy conditions prevented outdoor activities such as walking…" (Petursdottir 2010, p.1021).
Participants in two studies of water‐based exercise commented on their experience of the water itself (Fisken 2016; Larmer 2014b). In some cases they liked that the water kept them 'balanced' (p.14) and that the depth of the water "takes the impact off your joints…it gives you freedom" (p.14) (Fisken 2016). However, negative reactions to water could also be a barrier: "When I was in [name of pool] I stopped going because I got chlorine burns on my skin, from here (indicated chest level) right up" (Fisken 2016, p.14). Similarly in Larmer 2014b, when people exercised on their own initiative, attending local pools rather than the hydrotherapy pool, the cooler water temperatures meant that their symptoms were not alleviated to the same extent as they were in warmer water, and one person reported the colder water causing cramp. For ongoing effective relief, access to specialist hydrotherapy pools was therefore important.
Implications for effective exercise interventions derived from the qualitative synthesis
From the synthesis of the qualitative studies reporting the views and opinions of people with OA, nine implications were derived that are important when delivering exercise‐based interventions. Two review authors (MH and NW) who are physiotherapists grouped these into four main components:
Healthcare professionals with good interpersonal skills should provide clear, succinct, consistent and convincing advice and information for people with OA, and emphasise the improvements achieved in others.
Implication 1: provide accurate information about cause of OA, its likely prognosis and management options.
-
Implication 2: explain and demonstrate the benefits of exercise experienced by people with OA.
Provide opportunities to participate in physical activity/exercise people value, tailored to their individual abilities, needs and preferences.
Implication 3: provide opportunities to exercise, discuss and obtain personalised advice and encouragement from a skilled practitioner.
Implication 4: tailor exercise and advice to each person, taking into account severity of OA and under what circumstances exercise might improve, worsen or leave pain, physical (e.g. mobility, function) or psychosocial (self‐efficacy, confidence) symptoms unchanged.
-
Implication 5: offer opportunities for exercise that match personal preferences, as part of daily life or dedicated exercise classes delivered to individuals or groups.
Challenge, rather than reinforce, inappropriate health beliefs; in particular, explain and encourage the benefits of physical activity/exercise.
Implication 6: challenge beliefs about causes of OA that might discourage exercise (e.g. wear and tear).
-
Implication 7: explain value of pain relief in enabling people to perform controlled exercise/physical activity, and reassure people that exercising after taking 'regular' analgesia is not harmful.
Encourage family, friends and peer support, including value of shared learning/experiences from participation in group exercise classes.
Implication 8: encourage support from family, friends and peers.
Implication 9: provide practical support: use of equipment, teach correct exercises.
3. Synthesis integrating quantitative and qualitative findings
The final synthesis is in two parts.
First, we identified components of effective exercise programmes by comparing the implications derived from the qualitative synthesis with the exercise programmes evaluated by well‐designed RCTs with low risk of bias (Bennell 2014; Bennell 2016; Cheung 2014; Fernandes 2010; Fransen 2007; French 2013; Hurley 2007), all of which favoured exercise although not all were statistically significant (Table 6).
Table 4.
Integrative review
| Integrative review | Implications for exercise programmes derived from the qualitative synthesis | Mean and 95% CI | ||||||||||||||
| Information/demonstrate improvement | Individually tailored interventions | Challenge beliefs | Practical support | |||||||||||||
| Trial (meta‐analysis comparison) | Recruitment | Intervention | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Pain | Function | Self‐efficacy | Depression | Anxiety |
| Studies with a low risk of bias | ||||||||||||||||
| Bennell 2014 | Local community. | 10 individual sessions of semi‐standardised exercises over 12 weeks plus exercises to perform 4 times a week at home. | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | √ | 0.21 ‐0.19 to 0.61 |
0.09 ‐0.31 to 0.49 |
0.05 ‐0.35 to 0.45 |
‐ | ‐ |
| Bennell 2016 | Community participants. | 10 treatments over 12 weeks of exercise or exercise and education. | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.33 ‐0.67 to 0.01 |
‐0.81 ‐1.17 to ‐0.46 |
0.61 0.26 to 0.96 |
‐ | ‐0.04 ‐0.37 to 0.30 |
| Cheung 2014 | Community through flyers, press releases and mailings via local physician practice. | Hatha yoga, once a week in a class + 4 shorter sessions a week at home. | ‐ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.86 ‐1.55 to ‐0.17 |
‐0.42 ‐1.08 to 0.24 |
‐ | ‐ | ‐ |
| Fernandes 2010 | University hospital, local hospital, rehabilitation centre, general practitioners, and local newspaper advert. | 3 group‐based sessions and 1 individual physical therapy visit, 2 months after completing the group sessions. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.30 ‐0.75 to 0.15 |
‐0.47 ‐0.92 to ‐0.02 |
‐ | ‐ | |
| Fransen 2007 | Local newspapers & social clubs, general practitioners and rheumatologists. | Tai Chi, twice a week, 12 weeks. | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.52 ‐0.93 to ‐0.11 |
‐0.66 ‐1.07 to ‐0.24 |
‐ | ‐0.21 ‐0.61 to 0.20 |
‐0.32 ‐0.73 to 0.09 |
| French 2013a | General practitioners, rheumatologists, orthopaedic surgeons, and hospital consultants. | 6‐8 individual 30‐minute physiotherapy sessions over 8 weeks. Strength/resistance training and manual therapy + patient information. | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.43 ‐0.96 to 0.10 |
‐0.40 ‐0.83 to 0.03 |
‐ | ‐0.18 ‐0.61 to 0.24 |
0.04 ‐0.39 to 0.46 |
| French 2013b | General practitioners, rheumatologists, orthopaedic surgeons, and hospital consultants. | 6‐8 individual 30‐minute physiotherapy sessions over 8 weeks. Strength/resistance training + patient information (no manual therapy). | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.55 ‐1.07 to ‐0.03 |
‐0.49 ‐0.92 to ‐0.07 |
‐ | ‐0.16 ‐0.58 to 0.26 |
0.15 ‐0.27 to 0.56 |
| Hurley 2007a | Inner‐city primary care practices. | Physiotherapist, twice a week, 6 weeks; individual exercise. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.25 ‐0.56 to 0.07 |
‐0.15 ‐0.41 to 0.10 |
0.44 0.12 to 0.76 |
‐0.19 ‐0.50 to 0.13 |
‐0.19 ‐0.51 to 0.13 |
| Hurley 2007b | Inner‐city primary care practices. | Physiotherapist, twice a week, 6 weeks; group exercise. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.13 ‐0.45 to 0.19 |
0.06 ‐0.19 to 0.19 |
0.42 0.09 to 0.75 |
‐0.09 ‐0.42 to 0.23 |
‐0.11 ‐0.43 to 0.21 |
| Studies with a high risk of bias | ||||||||||||||||
| Aglamis 2008 | ‐ | ‐ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.54 ‐1.37 to 0.30 |
‐0.64 ‐1.48 to 0.20 |
‐ | ‐ | ‐ |
| Baker 2001 | ‐ | ‐ | ‐ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.56 ‐1.16 to 0.05 |
‐0.48 ‐1.08 to 0.12 |
‐ | ‐ | ‐ |
| Focht 2005 | ‐ | ‐ | ‐ | ‐ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐0.23 ‐0.62 to 0.16 |
‐0.17 ‐0.22 to 0.56 |
0.44* 0.05 to 0.83 |
‐ | ‐ |
| Focht 2005 | ‐ | ‐ | ‐ | ‐ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐0.05 ‐0.33 to 0.44 |
‐0.3 ‐0.42 to 0.36 |
‐ | ‐ | ‐ |
| Hopman‐Rock 2000 | ‐ | ‐ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.15 ‐0.55 to 0.24 |
‐ | 0.89* 0.47 to 1.30 |
‐ | ‐ |
| Kao 2012 | ‐ | ‐ | √ | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.54 0.26 to 0.82 |
‐ | ‐ | ‐ | ‐ |
| Keefe 2004 | ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.13 ‐0.51 to 0.76 |
‐ | 0.36 ‐0.44 to 1.15 |
‐ | ‐ |
| Keefe 2004 | ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.42 ‐1.10 to 0.27 |
‐ | ‐0.07 ‐0.89 to 0.74 |
‐ | ‐ |
| Kim 2012 | ‐ | ‐ | √ | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.60 ‐1.07 to 0.12 |
‐ | 1.04 0.05 to 1.54 |
‐0.88 ‐0.37 to 0.39 |
‐ |
| Mikesky 2006 | ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.56 ‐0.88 to ‐0.25 |
0.10 ‐0.21 to 0.41 |
‐ | 0.05 ‐0.26 to 0.36 |
‐ |
| Park 2014 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.35 ‐0.33 to 1.03 |
‐ |
| Péloquin 1999 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.04 ‐0.32 to 0.39 |
‐ | ‐ | ‐ | ‐ |
| Schlenk 2011 | ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.22 ‐0.52 to 0.08 |
‐0.95* 0.04 to 1.87 |
‐ | ‐ |
| Sullivan 1998 | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.40 ‐0.95 to 0.16 |
‐ | ‐0.16 ‐0.70 to 0.39 |
‐ | ‐ |
| Wang 2009 | ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.68 ‐1.32 to ‐0.04 |
‐0.17 ‐0.31 to ‐0.03 |
0.71 0.07 to 1.35 |
‐ | ‐ |
| Yip 2007 | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.17 ‐0.53 to 0.19 |
‐ | 0.32 ‐0.04 to 0.69 |
‐ | ‐ |
CI: confidence interval.
This showed that:
six of these seven exercise programmes provided tailored advice about exercise (Implication 4) (Bennell 2014; Cheung 2014; Fernandes 2010; Fransen 2007; French 2013; Hurley 2007);
the exercise programmes in five trials provided people with accurate information about cause, prognosis and management options, including exercise (Implication 1) (Bennell 2014; Bennell 2016; Fernandes 2010; French 2013; Hurley 2007), and opportunities to experience exercise with personalised advice and encouragement from a skilled practitioner (Implication 3: also provided by Cheung 2014);
the programmes in two trials challenged health beliefs that might discourage exercise (Implication 6) (Fernandes 2010; Hurley 2007);
programmes in three trials provided practical support for use of exercise equipment (Bennell 2014; Bennell 2016; Cheung 2014);
none of the exercise programmes explicitly reported highlighting improvements experienced by people (Implication 2), offer participants personal preferences in the exercise undertaken (Implication 5), explaining to participants the value of pain relief in enabling people to perform controlled exercise (Implication 7), or encouraged support from other people (Implication 8).
Second, we compared exercise programmes evaluated by less well‐designed RCTs, that is, with a medium/high risk of bias (Aglamis 2008; Baker 2001; Focht 2005; Hopman‐Rock 2000; Kao 2012; Keefe 2004; Kim 2012; Mikesky 2006; Park 2014; Péloquin 1999; Schlenk 2011; Sullivan 1998; Wang 2009; Yip 2007), with the implications from the qualitative synthesis to identify components that have been incorporated into exercise programmes.
This showed that some exercise programmes:
provided activities that matched personal preferences (Implication 5). Focht 2005 allowed participants to choose whether they exercised at home, at a community facility, or combination of the two;
incorporated peer or family support (Implication 8). Three trials reported supporting people to exercise (Keefe 2004; Kim 2012; Mikesky 2006). One trial used an aquatic exercise programme to provide peer support by including social time as part of the intervention when participants could become better acquainted (Kim 2012). One trial distributed a newsletter and T‐shirts identifying the subject as a participant in the study, arranged group training sessions and an "exercise buddy" system to help people find training partners, and co‐ordinated social gatherings (Mikesky 2006). One trial incorporated a "couples' skills training" component which provided training to patients and their spouses in a wide range of skills including communication, behavioural rehearsal and mutual goal setting (Keefe 2004).
This comparison shows how implications derived from the qualitative synthesis can be incorporated into interventions, but weaknesses in study designs mean that evidence of the effects is lacking.
Discussion
Summary of main results
This review highlighted the impact chronic joint pain associated with OA has on a wide range of physical and psychosocial variables of older people. In addition, we looked at whether, how and why exercise alleviated some of the impact of chronic pain/OA, and if exercise could help people to manage their condition better.
Meta‐analyses of the quantitative studies provided moderate to low quality evidence that exercise slightly improved pain and function, and also offered a range of benefits on self‐efficacy, depression and other psychosocial traits when the outcomes were measured using quantitative scales. These benefits may arise indirectly from a reduction in pain and improvement in function, or directly as a result of attending a rehabilitation programme that developed positive attitudes toward living with OA, support from clinicians and sharing experiences with people who have similar problems.
The qualitative synthesis provided an insight into people's experiences and beliefs about OA; how these beliefs were constructed; and how they shaped people's attitudes, behaviours and decisions about how to engage with and manage OA. The experience and impact of pain dominated the lives of people with OA because it affected most areas of their daily life in a variety of ways (Figure 1; Figure 2). Pain, joint stiffness, fatigue, comorbidity and people's perceptions of their physical fitness restricted the type and amount of exercise they could do. The consequences of OA evoked anxiety and depression, undermined people's self‐confidence, their social role and their sense of self. With little or no information or advice forthcoming from healthcare professionals, people attributed their condition to "wear and tear" on their joints, ageing processes, familial disposition or a combination of these. Moreover, the onset of pain with physical activity was often interpreted as causing additional joint damage, so people avoided activity for fear of causing additional harm.
Healthcare professionals were an important source of information, advice, reassurance and motivation. Clear instructions and advice from a trusted healthcare professional were important in allaying people's fears and anxieties about exercise, and convincing them exercise is safe and beneficial. The instructions and advice needed to be contextualised so that each person knew unequivocally what exercises to do, the correct way to do them, when and where to do them, what they should avoid doing, and what they might expect to experience and feel. Although some people did not find exercise helpful, most thought rehabilitation programmes that included an active participatory exercise regimen produced physical, emotional and psychosocial benefits.
The qualitative analysis revealed that people reported receiving support from family, friends and their peer group. In particular, exercise classes provided a sense of community, camaraderie and working together. Unfortunately, sustaining regular exercise was difficult. People exercised regularly if they perceived exercise to be important, fun and enjoyable. However, family and work commitments, time pressure and other health issues were often prioritised over exercise, and exercise was sometimes regarded as a burdensome chore. If the benefits derived from exercise were not considered a 'good return' for the time and effort people invested, exercise was discontinued.
The support and conditions required for each person to exercise varied greatly. Some people liked to exercise in groups, others preferred to exercise alone. Some people needed access to exercise facilities, special equipment and relied on supervisors to lead them. Others were intimidated by these and preferred exercising at home, particularly elderly women self‐conscious about their age and body image, and considered activities such as walking sufficient exercise. Cost of exercise facilities or equipment was a barrier to exercise for people on low and fixed incomes.
Overall completeness and applicability of evidence
Better understanding of the complex reciprocity of symptoms, health beliefs and behaviours of people with chronic joint pain (Figure 1; Figure 2), and greater appreciation of how exercise can positively affect people's symptoms, beliefs and behaviours, might enable us to maximise the effectiveness of exercise programmes and encourage uptake so that more people might benefit. Although many studies demonstrate that exercise programmes improve pain and physical functioning in older people with OA, the effect of exercise on psychosocial outcomes has been less well investigated. In addition, little is known about the effect pain, disability and psychosocial dysfunction have on people's ability and willingness to participate in exercise programmes. These gaps in our understanding are evident from the large number of studies that we had to exclude from this review because they had not measured psychosocial outcomes. Of the studies that were included, although many were small studies, they were generally well designed and reported. However, the exercise programmes varied greatly in their content and focus (strength, endurance, balance/co‐ordination, functional performance), 'dose' (exercise intensity, frequency, etc.), mode of delivery (classes, individual treatment, facility‐based, home programme), duration of intervention, time to follow‐up after completion of the programme, study design and outcome measures. We considered using meta‐regression to explain some of the heterogeneity (Juhl 2014), but the wide variety of outcome measures across the studies prevented this. Consequently, there were insufficient data to determine which aspects and features of exercise programmes are most effective at producing beneficial effects in specific outcome measures.
One of the most valuable aspects of qualitative research is to provide explanations and enhance our understanding. The views, opinions and beliefs reported in the studies in this review were consistent with other qualitative studies of people with OA, but which did not look specifically at exercise: perceptions of conservative treatment programmes for OA (Smith 2014a), the experience of living with OA (Smith 2014b), recognising and addressing emergent knee problems (Maly 2009), personal models of OA (Hampson 1994), and lay‐beliefs regarding rheumatoid arthritis (Donovan 1989). The qualitative studies in this review were conducted in five high‐income countries. Studies, and therefore understanding of people's views and behaviour, in low‐ and middle‐income countries are lacking. Therefore, the opinions and beliefs of the participants in these included studies were shaped by the context of high‐income countries, and may not be valid for other populations.
Quality of the evidence
Overall the risk of bias of the RCTs comprising the quantitative synthesis was low, apart from blinding and allocation concealment, both of which are particularly challenging with exercise interventions. The descriptions of the trial design were generally clear, though some were complex and difficult to understand. We also found levels of ambiguity, particularly with regard to the success of blinding and provision of sufficient details about interventions. Many of the trials were relatively small (fewer than 50 participants per group) and had low power to detect medium effect sizes. Outcome measures were heterogeneous and often self‐reported which are subject to recall bias and socially desirable biases. Most of the trials only reported changes immediately after completing an exercise programme, or had a short follow‐up period (less than six months) after completion, so whether there were sustained benefits on chronic joint pain was unknown. Attrition rates were usually reported, but how many people withdrew because of adverse effects of exercise was rarely reported. This is important in understanding the acceptability of burdensome interventions that require investment of time and effort and could potentially cause discomfort, pain or harm. Intention‐to‐treat analyses were usually reported, but the handling of missing data was less well described, and exposed very small trials' attrition bias.
Most of the exercise programmes reported tailoring their exercise programmes to meet individual patients' capabilities and needs, which reflects current clinical practice (Holden 2008; Walsh 2009), and suggests the programmes that informed our synthesis were clinically applicable.
In the first part of the integrative review, none of the exercise programmes explicitly reported highlighting improvements experienced by people (Implication 2), offered participants personal preferences in the exercise undertaken (Implication 5), explained to participants the value of pain relief (Implication 7), encouraged support from other people (Implication 8) or provided practical support for use of gym equipment (Implication 9). However, such advice and information is usually considered such an integral part of exercise programmes that the authors may have not consider it worth reporting, or editorial limitations often restrict what is included in the description of an intervention, or both. Such omissions will have influenced this finding of the integrative review.
Two trials with ostensibly high‐quality designs had unusually large effect sizes and small sample sizes (Aglamis 2008; Kim 2012). These studies showed large benefits of exercise on depression (SMD ‐0.88) (Kim 2012), SF‐36 social function (MD 58.30), SF‐36 mental health (MD 32.90) and SF‐36 vitality (MD 51.90) (Aglamis 2008). As there was no obvious reason to exclude these studies, we conducted sensitivity analyses with these studies included and excluded. In general including the studies had little material effect on the overall conclusions, but borderline changes become more statistically significant, and an uncertain effect on depression attained statistical significance when Kim was included. Therefore, the magnitude of effect size should be treated with caution when these studies are included.
Similar to most other reviews of exercise interventions, none of the trials made an attempt to blind participants to their intervention. Devising placebo exercise requires considerable effort; the placebo itself may have an effect and people usually know what group (active or placebo) they are in. Moreover, in many complex health interventions that aim to affect behavioural change, the participant‐supervisor interaction is integral to the success of the intervention. Our qualitative synthesis highlighted the close partnership formed between participants and supervisor which was very important in getting people with chronic joint pain to undertake activities they might consider harmful. Removing this important contextual component by blinding participants (or supervisors) would create a 'clinically inappropriate' intervention. All the trials attempted to blind the outcome assessors to each participant's treatment allocation. Whether these attempts were successful were not reported.
The quality of design and reporting of the qualitative studies included in this review was good. Researchers gave clear descriptions of their methodology and findings, and took measures to minimise bias such as ensuring they purposively recruited a representative cross‐section of participants and prevented their values and opinions biasing their report and interpretation. Unfortunately, qualitative research is vulnerable to specific sources of bias: 'recall bias' is a particular problem for studies of older populations; 'volunteer bias' may lead to the recruitment of people who are enthusiastic about exercise and their opinions reflect their enthusiasm; 'socially desirable reporting' can affect interventions that require participants to invest a great deal of time and effort, and they may want to convince themselves this investment has been worthwhile or where strong bonds formed between participants and supervisors, participants may try to reflect well on the supervisor (or a combination of these). Despite the efforts made to minimise these sources of bias, it is unlikely they will have been eliminated completely. However, the study findings are generally consistent across several studies; they reported the views of people who did not find exercise beneficial, who were not enthusiastic about exercise and who admitted not sustaining regular exercise after the end of an exercise programme. Thus, in general, the studies recruited and reflected the varied views and opinions of people with OA about exercise, increasing our confidence in their validity of the findings of the qualitative synthesis.
Potential biases in the review process
We conducted a thorough search of the literature which was designed by the review authors with experience in this field, patient representatives, systematic reviewers and information scientists skilled in constructing and conducting searches. This maximised the chances of identifying relevant data from pertinent databases and other sources of relevant information, and resulted in a large number of potential sources of information (research papers, theses, reports, etc.) being identified. The search will have been affected by publication and selective reporting bias because psychosocial variables were usually secondary outcome measures, or if the intervention produced no change in the outcome, these outcomes may not have been reported in the abstract, as a keyword or in the final publication. Where this was suspected. we sourced and appraised the full‐text paper to decide on its inclusion/exclusion in the review. This substantially increased the number of papers that had to be obtained and appraised before inclusion/exclusion, and resulted in the large number of papers screened and excluded (399 papers), which was necessary to ensure the thoroughness of the review process. Brief details of a representative sample (62 studies) of the excluded studies are provided.
We tried to contact the authors of two relatively large studies with 289 (Jenkinson 2009) and 600 (Thomas 2002) completing participants, but received no response and so they had to be excluded from the review. The absence of their information on anxiety and depression is unfortunate, since they could have contributed data to important outcomes that might have affected the uncertain findings of these outcomes.
Although we did not stipulate that papers had to be written in English to be included, all those meeting the criteria were in the English language. It is possible that research written up in other languages was not identified via searches, and it should be recognised that findings may not apply across all social and cultural contexts.
Our patient representative (JC) was involved at each stage of the review process to ensure our review question, process, data capture, processing, report and its conclusions are relevant to this patient population.
Two of the authors of the review, MH and NW, had been involved in work in this area, and coauthored papers included in the review (Hurley 2007; Hurley 2010). To prevent bias, they did not evaluate their own quantitative paper (Hurley 2007), and neither were involved in any part of the data extraction and synthesis of the qualitative synthesis.
Agreements and disagreements with other studies or reviews
Our quantitative synthesis (pain improvement SMD ‐0.33, 95% CI ‐0.46 to ‐0.21, I2 = 23%; function improvement SMD ‐0.27, 95% CI ‐0.37 to ‐0.17, I2 = 45%) corroborates other systematic reviews and meta‐analyses that showed evidence that exercise improved pain and physical function for people with knee OA, although the quality of evidence for pain was compromised due particularly to risk of bias arising from lack of blinding in most studies. For knee OA, there was a 6% absolute reduction in pain and a 5.6% absolute improvement in function (Fransen 2015: pain reduction: SMD ‐0.49, 95% CI ‐0.39 to 0.59; function improvement: SMD ‐0.52, 95% CI ‐0.39 to ‐0.64; Juhl 2014: pain reduction: SMD 0.50, 95% CI ‐0.39 to 0.52, P = 0.001; disability: SMD 0.49, 95% CI 0.35 to 0.63, P = 0.001; Uthman 2013: pain: SMD ‐0.69, 95% CI ‐1.04 to 0.35; function: SMD ‐0.63, 95% CI ‐1.16 to ‐0.10) and for hip OA (Fransen 2014: pain reduction: SMD ‐0.38, 95% CI ‐0.55 to ‐0.20; function improvement: SMD ‐0.38, 95% CI ‐0.54 to ‐0.05). Evidence‐based clinical guidelines that recommend exercise as a core intervention in the management of OA (EULAR 2013; Hochberg 2012; McAlindon 2014; NICE 2014), although there is evidence that self‐management interventions in OA are of little or no benefit (Kroon 2014). Heterogeneity of the interventions prevents us drawing conclusions about the type, duration, frequency, intensity or delivery mode of the most effective exercise programmes. Other reviews concluded that optimal exercise programmes consist of 12 sessions, delivered two or three sessions a week; that individual sessions, classes, facility‐based or home‐based programmes are all equally effective; and that a combination of exercises to increase strength, control, endurance, aerobic capacity and functional performance can address sensorimotor, physical and psychosocial dysfunction and deficits (Fransen 2015; Juhl 2014; Roddy 2005; Uthman 2013). Our review included only one quantitative (Kim 2012) and two qualitative (Larmer 2014b; Moody 2012) studies of aquatic exercise: this compared with six studies identified in a previous Cochrane Review of aquatic interventions for OA (Bartels 2007), published prior to both the studies we included. None of those six papers qualified for inclusion in this study, and it should be noted that Bartels 2007 found studies to be of a low standard.
Although the quantitative synthesis demonstrated exercise was effective in producing a benefit and the meta‐analysis estimated the magnitude of improvement, it did not inform us about the underlying mechanisms whereby exercise brings about improvement. It is very unlikely to occur by physiological increases in muscle function (i.e. strength, control, endurance, or a combination of these), as physiological changes require a greater stimulus than provided by relatively brief exercise programmes. Hurley and colleagues suggested that improvements in self‐reported pain, physical functioning and psychosocial functioning are more likely due to alteration in the complex, inter‐relationships between pain, physical functioning and psychosocial functioning, following the positive experiences of exercise influencing people's perception of health beliefs and their behavioural response to pain (Hurley 2003; Figure 1; Figure 2).
Knee pain is strongly associated with greater depression and anxiety (Hawker 2011; Phyomaung 2014), and disability is related to perceptions about OA. Bijsterbosch 2009 found that higher perceived negative consequences and lack of control of OA at baseline were associated with higher levels of disability at six years. Greater disability was also associated with the number of symptoms attributed to OA (which may simply indicate more severe cases), poor understanding of the condition, holding strong beliefs about its adverse impact and chronicity, and experiencing more negative emotions. If people interpret knee pain as causing harm and damage, they will avoid physical activity for fear of causing additional pain and damage (fear‐avoidance; Figure 2) (Keefe 1996a; Leeuwa 2007; Maly 2009). Over time, reduced activity will result in greater muscle weakness, pain and disability, and disrupt participation in meaningful activities, induce feelings of depression, anxiety, helplessness and loss of independence, and reduced quality of life, which will have a negative impact on clinical outcomes, physical functioning and psychosocial functioning (Dekker 1992; Hurley 1999; van Baar 1998a).
Lack of advice and information was associated with unhelpful perceptions and beliefs about the causes, consequences and prognosis of OA, and this was evident in study participants included in our qualitative synthesis. Challenging these unhelpful perceptions is vital for successful management. Inappropriate health beliefs and behaviours can be altered by positive experiences that show people how active coping strategies such as exercise can reduce pain and improve physical functioning, self‐efficacy, anxiety, helplessness, catastrophising and depression (Keefe 1996b; Main 2002; Turk 1996).
Self‐efficacy, a person's confidence in their ability to perform a specific health behaviour, is an important psychological trait for self‐management of health (Bandura 1977; McAuley 2006; Stretton 2005; Taylor 2004), although it does not necessarily lead to the behaviour in question. People with high self‐efficacy are more active, less depressed and anxious, and report less pain than people with low self‐efficacy. "Exercise self‐efficacy" is a person's confidence in their ability to perform exercise, and plays an important role in the adoption of activities they may be unfamiliar with, and that they may be concerned might cause discomfort or pain. It builds their confidence in their ability to overcome barriers (McAuley 1992; McAuley 1993; Rejeski 1998), although the term is not without controversy (Kroon 2014). Exercise self‐efficacy might be enhanced by informing people about the value of exercise in the management of OA (verbal persuasion), and through the positive experience of successfully completing a challenging exercise programme (master experiences): these are both mechanisms identified by Bandura 1977 as ways in which self‐efficacy can be increased, although he suggests verbal persuasion alone may have relatively little effect; it is better as a method to increase self‐efficacy through use alongside another strategy. Combining verbal persuasion with other interventions is common. Rehabilitation programmes that integrate exercise and patient education improve people's understanding of the condition, its effects and prognosis, and the beneficial role of exercise as a treatment and self‐management strategy in OA that can restore a sense of control, construct positive illness perceptions and hence improve clinical outcome (Hurley 2009).
Meta‐analysis showed exercise statistically significantly improved self‐efficacy (Analysis 1.3), which is reflected in participants' opinions of their ability to perform exercise and change their health beliefs that was evident in the qualitative synthesis. This may result from people coming to appreciate the benefits of exercise, their ability to perform exercise and understanding how they can use exercise to control their condition as a result of their positive experiences following participation on the exercise programmes.
Most of the trials included in the review reported short‐term outcomes. One cohort followed for two and a half years showed initial benefits declined over time (Hurley 2012), which confirms other findings (Pisters 2007). Sustaining regular exercise does not appear to be motivated by the type of exercise involved, but rather is influenced by providing supervised, graded activity programmes that include self‐management strategies, cognitive behavioural techniques, individualised exercise programmes and booster sessions after completing a programme (Jordan 2010; Pisters 2007), and the important influence health beliefs have on people's participation in exercise (Campbell 2001). Our qualitative synthesis emphasised the importance people attach to the continued support and encouragement for the continued engagement with regular physical activity.
Authors' conclusions
Chronic hip and knee pain affects all domains of people's lives. Beliefs about chronic pain shaped people's attitudes and behaviours about how to manage their pain. With little or no information or advice from healthcare professionals, people attributed their condition to "wear and tear" on their joints, ageing processes, familial disposition, or a combination of these. Moreover, the onset of pain with physical activity was often interpreted as causing additional joint damage, so people avoided activity for fear of causing additional harm. People's views about their symptoms, health beliefs and psychosocial experiences revealed implications for practice which covered providing information and demonstrating improvement, tailoring interventions to individuals, challenging unhelpful health beliefs and providing practical support. These findings have implications for clinical practice and topics and design of future research studies in this area.
From the meta‐analysis of randomised controlled trial, which was rated as low‐to‐moderate quality using GRADE:
older people with chronic knee or hip pain should be encouraged to participate in regular exercise since evidence indicates this slightly improves physical function, depression, pain and health‐related quality of life. It may improve self‐efficacy, stress, social function and mental health.
From the qualitative studies it is clear these programmes should:
provide information about cause, prognosis and management options, including exercise;
challenge beliefs that might discourage efforts to exercise;
tailor advice about exercise taking into account severity of the arthritis and under what circumstances might exercise improve, worsen or leave symptoms and function unchanged;
provide opportunities to exercise with personalised advice and encouragement from an experienced practitioner.
Relying on patients' views and experiences alone, the following components may be added:
highlight the improvements exercise can bring to people with chronic joint pain/osteoarthritis;
offer exercise that people prefer and enjoy, performed in exercise classes (individual or group) and encourage incorporation into daily life;
explain the value of pain relief and reassure that masking pain with analgesics is not harmful;
encourage support from peers, family and friends;
provide practical support for use of equipment.
Despite a relatively large number of studies of exercise, few studies have included psychosocial outcomes. Moreover, only a handful of studies were well designed, with low risk of biases, which allow us to be confident in drawing conclusions from their findings. Adverse effects were not reported, leaving us unable to draw conclusions about these. The syntheses, and in particular the integrative review, highlight the information that is missing about effectiveness from programmes that contain the elements of the implications from the qualitative synthesis but which still need rigorous evaluation from well‐designed clinical trials. These are needed to produce robust conclusions about what are the most effective exercise programmes. This research could be categorised as needing to establish effectiveness, mechanisms of action and methodology, although there may be overlap in certain areas:
investigate which components, combinations and settings within interventions are most effective (effectiveness);
investigate how moderate treatment effects can be enhanced (effectiveness);
determine how to sustain short‐term benefits (effectiveness);
confirm the effect of exercise on psychosocial effects including health beliefs, depression, anxiety, quality of life, etc., as primary outcomes (effectiveness/mechanisms of action);
ensure better reporting of pertinent aspects of studies, such as populations, recruitment strategies and interventions (methodology);
determine whether using advanced methods of data analysis (Bayesian structural equation modelling) could elucidate associations or causal relationships between pain, function and physical and psychosocial outcomes (methodology).
Acknowledgements
The authors thank Arthritis Research UK for their financial support of this work.
Appendices
Appendix 1. Example of search strategy
CONCEPT 1 OSTEOARTHRITIS TERMS
Controlled vocabulary:
| Arthralgia Osteoarthritis Arthritis Osteoarthritis, Hip Osteoarthritis, Knee Osteoarthritis |
OR
Free text, title and abstract:
| Gonarthros* Coxarthros* Osteoarthr* Arthralgia* Arthrosis "degenerative joint" |
OR
Terms used in conjunction – both columns ANDed:
| Controlled vocabulary · Musculoskeletal Diseases · Chronic Pain · Pain · Joint Diseases OR freetext in title and abstract · "joint pain" · "chronic joint" · arthriti* · "Chronic pain" |
Controlled vocabulary · Knee Joint · hip joint · knee · hip OR freetext in title and abstract · Knee · Knees · Hip · hips |
Exclusion of surgery terms.
| Exclude in title: · Arthroplasty · Surgery · Surgical · "hip replacement" · "knee replacement" · osteotomy · arthroscopic · postoperative · "post operative" |
CONCEPT 2 ‐ EXERCISE
Controlled vocabulary
Exercise therapy
Exercise
Muscle Stretching Exercises
Physiotherapy
Rehabilitation
"Tai Ji"
Walking
Yoga
OR
Free text – title and abstract
Aerobic OR Aerobics OR aquarobics OR balneotherapy OR classes OR exercise OR exercises OR hydrotherapy OR "muscle strength" OR "muscle strengthening" OR "Muscle training" OR "nonpharmacological" OR "non‐pharmacological" OR "nonsurgical" OR "non‐surgical" OR "physical activity" OR "physical therapy" OR "physical training" OR "pool therapy" OR physiotherap* OR pilates OR "resistance training" OR "strength training" OR "T ai Chi" OR "Tai Chi" OR "taichi" OR Walk OR walking OR walks OR yoga OR manipulative therap* OR stretch OR stretches OR stretching
Example of PubMed search
Where mh = MeSH terms, and tiab = title and abstract terms
| #25 | Search #23 AND #24 |
| #24 | Search ("1985"[Date ‐ Publication] : "3000"[Date ‐ Publication]) |
| #23 | Search #19 NOT #22 |
| #22 | Search #21 NOT #20 |
| #21 | Search animals[mh] |
| #20 | Search humans[mh] AND animals[mh] |
| #19 | Search #18 AND #14 |
| #18 | Search #15 OR #16 OR #17 |
| #17 | Search "Exercise therapy"[mh] OR Exercise[mh] OR "Muscle Stretching Exercises"[mh] OR Rehabilitation[mh:noexp] OR "Tai Ji"[mh] OR Walking[mh] OR Yoga[mh] |
| #16 | Search (stretch[tiab] OR stretches[tiab] OR stretching[tiab]) AND (muscle[tiab] OR muscles[tiab] OR physical[tiab] OR physically[tiab]) |
| #15 | Search Aerobic[tiab] OR aerobics[tiab] OR aquarobics[tiab] OR balneotherapy[tiab] OR classes[tiab] OR exercise[tiab] OR exercises[tiab] OR hydrotherapy[tiab] OR "muscle strength"[tiab] OR "muscle strengthening"[tiab] OR "Muscle training"[tiab] OR "nonpharmacological"[tiab] OR "non‐pharmacological"[tiab] OR "nonsurgical"[tiab] OR "non‐surgical"[tiab] OR "physical activity"[tiab] OR "physical activities"[tiab] OR "physical therapy"[tiab] OR "physical therapies"[tiab] OR "physical training"[tiab] OR "pool therapy"[tiab] OR physiotherap*[tiab] OR pilates[tiab] OR "resistance training"[tiab] OR "strength training"[tiab] OR "T ai Chi"[tiab] OR "Tai Chi"[tiab] OR "taichi"[tiab] OR Walk[tiab] OR walking[tiab] OR walks[tiab] OR yoga[tiab] OR "manipulative therapy"[tiab] OR "manipulative therapies"[tiab] OR "water therapy"[tiab] OR "water therapies"[tiab] |
| #14 | Search #13 NOT #12 |
| #13 | Search #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #11 |
| #12 | Search arthroplasty[ti] OR surgery[ti] OR surgical[ti] OR "hip replacement"[ti] OR "knee replacement"[ti] OR osteotomy[ti] OR arthroscopic[ti] OR postoperative[ti] OR "post operative"[ti] |
| #11 | Search #9 AND #10 |
| #10 | Search Knee Joint[mh] OR hip joint[mh] OR knee[mh] OR hip[mh] OR knee[tiab] OR knees[tiab] OR hip[tiab] OR hips[tiab] |
| #9 | Search Musculoskeletal Diseases[mh:noexp] OR "joint pain"[tiab] OR "chronic joint"[tiab] OR arthriti*[tiab] OR "Chronic pain"[tiab] OR "Chronic Pain"[mh] OR Pain[mh:noexp] OR Joint Diseases[mh:noexp] |
| #7 | Search Osteoarthr*[tiab] OR Arthralgia*[tiab] OR Arthrosis[tiab] OR "degenerative joint"[tiab] |
| #6 | Search Arthralgia[mh:noexp] NOT Arthralgia/surgery[mh:noexp] |
| #5 | Search Osteoarthritis[mh:noexp] NOT Osteoarthritis/surgery[mh:noexp] |
| #4 | Search Arthritis[mh:noexp] NOT Arthritis/surgery[mh:noexp] |
| #3 | Search Coxarthros*[tiab] OR Gonarthros*[tiab] |
| #2 | Search Osteoarthritis, Hip[mh] NOT Osteoarthritis, Hip/surgery[mh] |
| #1 | Search Osteoarthritis, Knee[mh] NOT Osteoarthritis, Knee/surgery[mh] |
Appendix 2. Electronic databases and other resources searched
We applied these search strategies for a comprehensive search of the following clinical, public health, psychology, social care databases:
Allied and Complementary Medicine (AMED);
Applied Social Sciences Index and Abstracts (ASSIA);
BiblioMap (EPPI‐Centre database of health promotion research);
British Nursing Index (BNI);
Cochrane Database of Systematic Reviews (CDSR);
Cochrane Central Register of Controlled Trials (CENTRAL);
Cumulative Index to Nursing and Allied Health Literature (CINAHL);
Database of Abstracts of Reviews of Effects (DARE);
Database of Promoting Health Effectiveness Reviews (DoPHER);
EMBASE;
Health Management Information Consortium (HMIC);
Health Technology Assessment (HTA);
International Bibliography of the Social Sciences (IBSS);
Medline
NHS Economic Evaluation Database (NHS EED);
Physiotherapy Evidence Database (PEDro) (systematic reviews and appraised randomised trials in physiotherapy);
PsycINFO;
PubMed;
Sociological Abstracts (SOCABS);
Social policy and Practice (SPP);
Social Services Abstracts;
Trials Register of Promoting Health Interventions (TRoPHI);
Web of Knowledge.
We handsearched the following resources:
Arthritis Australia;
Arthritis Foundation (USA);
Arthritis New Zealand;
Arthritis Society (Canada);
Cochrane Collaboration Behavioral Medicine Field Register archive;
British library Integrated Catalogue (BLIC);
British Index to Theses;
Dart Europe;
British Library Electronic Theses Online Service (ETHOS);
Economic and Social Research Council (ESRC);
Evidence Database on Ageing Care;
Fade: The North West Grey Literature Service (UK);
Google;
Google Scholar;
New York Academy of Medicine Library Catalogue;
Arthritis Care UK;
Healthtalkonline.org;
NHS Evidence;
NHS Health Scotland Library;
Opengrey.eu;
Rehabdata;
Social Science Research Network;
Alerts from Rehab database;
Northern Ireland Qualitative Archive on Ageism;
Arthritis Research Centre of Canada.
Appendix 3. Characteristics of included qualitative studies
Campbell 2001
| Methods | Sampling frame: purposely selected from list of participants in RCT intervention arm of study. Data collection: in depth interviews. Data analysis: constant comparative/thematic analysis. |
|
| Stated aim of study | To understand reasons for compliance and non‐compliance with a home‐based exercise regimen by people with osteoarthritis of the knee. | |
| Details of participants | Country: UK. Sample number: 20. Age: ≥ 45 years. Gender: mixed. SES: not stated. Occupation/employment: not stated. |
|
| Details of exercise programme | Provider(s): physiotherapists Training: not stated Setting: home‐based Content: strengthening of the vastus medialis component of the quadriceps muscle, medial taping of the patella; advice and information leaflets. Length/intensity: 8 weeks; 9 sessions; 30‐minute duration; and encouraged to continue with the exercises and taping at home. Comparator: general advice about weight reduction and exercise at a single visit. |
|
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | A thorough attempt. | |
| Were steps taken to increase rigour in data collection? | Several steps. | |
| Were steps taken to increase rigour in data analysis? | Several steps. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth, but limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | Medium. | |
Fisken 2016
| Methods | Sampling frame: advertising within community to find participants with OA who had discontinued aqua‐based exercise. Data collection: focus groups. Data analysis: general Inductive Thematic Analysis. |
|
| Stated aim of study | To provide insight into the factors contributing to older adults with OA ceasing participation in an aqua‐based exercise programme. | |
| Details of participants | Country: New Zealand. Sample number: 11. Age: ≥ 60 years. Gender: female. SES: Not stated Ethnicity: 6 New Zealand European, 2 Maori, 3 others. Occupation/employment: Not stated |
|
| Details of exercise programme | Name of programme: Not stated Provider(s): Not stated Training: Not stated Setting: Aqua facilities Content: aqua‐fitness or aqua‐jogging classes attended previously, but no longer attended. |
|
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, several attempts. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth, but little depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | Medium. | |
| Credibility of findings | Medium. | |
Hendry 2006
| Methods | Sampling frame: purposely selected from GPs' disease registers and gyms representing geographic and socioeconomic diversity. Data collection: semi‐structured interviews. Data analysis: Framework 'thematic' analysis. |
|
| Stated aim of study | To examine the views of primary care patients with OA knee towards exercise, explore factors that determine the acceptability and motivation to exercise, and to identify barriers that limit its use. To examine the views of primary care patients with OA of the knee towards exercise, to explore factors that determine the acceptability and motivation to exercise and to identify barriers that limit its use that could be addressed in primary care consultations. | |
| Details of participants | Country: UK. Sample number: 22. Age: ≥ 50 years. Gender: 16 women. SES: not stated. Ethnicity: not stated. Occupation/employment: not stated. |
|
| Details of exercise programme | Not applicable. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, a (fairly) thorough attempt was made. | |
| Were steps taken to increase rigour in data collection? | Yes, a (fairly) thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a (fairly) thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Hinman 2016
| Methods | Sampling frame: sequential purposive sampling to recruit from RCT that recruited from the community. Data collection: semi‐structured individual interviews. Data analysis: thematic analysis guided by grounded theory method: systematic and structured engagement, and interplay and constant comparison. |
|
| Stated aim of study | To explore how key stakeholders (physical therapists, telephone coaches and patients) experienced, and made sense of, being involved in delivering or receiving an integrated physical therapy and telephone coaching intervention. | |
| Details of participants | Country: Australia. Sample number: 6 participants (10 physical therapists, 4 telephone coaches). Age: ≥ 50 years. Gender: mixed. SES: Not stated Ethnicity: Not stated Occupation/employment: Not stated |
|
| Details of exercise programme | Name of programme: Not stated Provider(s): physiotherapists and telephone coaches. Training: physical therapists: at least 2 years of postgraduate musculoskeletal experience. Coaches completed training programme by HealthChange Australia. Setting: private practice and at home. Content: exercise and physical activity programme with telephone coaching, plus a booklet explaining the benefits of exercise. Coaching component: assistance with behaviour change through effective information exchange, assistance to form behavioural goal intention, and helping to convert intention into action. Exercise component: 4‐6 individualised lower limb exercises performed 3 times a week and advice to increase general physical activity. Coaching component: mean 28 minutes per call, with 6‐12 calls over the 6‐month intervention. Exercise component: 30‐minute consultations in weeks 1, 3, 7, 12 and 20 of a 6‐month period, with exercises carried out 3 times a week. |
|
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, fairly thorough attempt. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, fairly thorough attempt. | |
| Were the findings of the study grounded/supported by data? | Well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Hurley 2010
| Methods | Sampling frame: from RCT that recruited from primary care surgery databases. Data collection: semi‐structured interviews. Data analysis: constant comparative/thematic analysis. |
|
| Stated aim of study | To explore the health beliefs, experiences, treatment and expectations of people with chronic knee pain, and investigate if, how and why these change after taking part in an integrated exercise‐based rehabilitation programme‐Enabling Self‐management and Coping with Arthritis knee Pain through Exercise. | |
| Details of participants | Country: UK. Sample number: 29 (6 interviewed before the intervention only, 23 interviewed before and after the intervention). Age: ≥ 50 years. Gender: mixed. SES: Not stated Ethnicity: 3 black African, 5 black Caribbean, 1 Indian, 20 Caucasian (White). Occupation/employment: Not stated |
|
| Details of exercise programme | Name of programme: ESCAPE. Provider(s): physiotherapists. Training: Not stated Setting: Community, gym of a physiotherapy outpatient department. Content: rehabilitation programme comprising of education component and exercise component. Education component: themed, informal discussion led by a physiotherapist designed to enhance patients understanding of condition, its causes, consequences, prognosis and promote simple self‐management strategies. Exercise component: designed to increase strength, balance and co‐ordination and confidence. Length/intensity: Overall rehabilitation programme: 12 sessions twice weekly for 6 weeks. Education component: 10‐15 minutes. Exercise component: 30‐45 minutes. |
|
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Several steps. | |
| Were steps taken to increase rigour in data collection? | Several steps. | |
| Were steps taken to increase rigour in data analysis? | Several steps. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Larmer 2014
| Methods | Sampling frame: via 3 hydrotherapy services in Auckland, with potential participants given information packs by clinicians. Data collection: focus groups, with an option provided for individual interview. Data analysis: content analysis framework with constant comparative methods. |
|
| Stated aim of study | To explore the perceived benefits of hydrotherapy from a patient's perspective. | |
| Details of participants | Country: New Zealand. Sample number: 15. Age: ≥ 56 years. Gender: mixed. SES: Not stated Ethnicity: 14 New Zealand European, 1 Samoan. Occupation/employment: Not stated |
|
| Details of exercise programme | Name of programme: Not stated Provider(s): Hydrotherapy services. Training: Not stated Setting: hydrotherapy pool. Content: hydrotherapy exercise programme. |
|
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, several attempts. | |
| Were the findings of the study grounded/supported by data? | Well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth, but little depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | Medium. | |
Moody 2010
| Methods | Sampling frame: from RCT (no other details reported). Data collection: focus groups. Data analysis: The General Inductive Approach. |
|
| Stated aim of study | To investigate the effects of a 12‐week aqua‐aerobics programme on falls risk and physical function in older adults with lower extremity osteoarthritis in New Zealand. | |
| Details of participants | Country: New Zealand. Sample number: 17. Age: ≥ 65 years. Gender: 13 women. SES: not stated. Ethnicity: not stated Occupation/employment: not stated. |
|
| Details of exercise programme | Provider(s): water exercise instructor. Training: yes. Setting: community; local municipal swimming pool. Content: group water‐based exercise programme that included warm‐up and warm‐down exercises and a series of progressively more challenging balance exercises. Length/intensity: twice weekly for 12 weeks. |
|
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, several steps were taken. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth but limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | Medium. | |
| Credibility of findings | High. | |
Morden 2011
| Methods | Sampling frame: from longitudinal survey of people aged > 50 years. Data collection: indepth interviews, semi‐structured interviews and diary. Data analysis: constant comparative/thematic analysis. |
|
| Stated aim of study | To explore the ‘lay' model of self‐management for knee pain within a populace of people with knee pain who have not recently consulted with their GP for their condition. It can be argued that this allows specific exploration of how people manage without professional advice and support, and whether they distinguish between professional and lay approaches to self‐management. | |
| Details of participants | Country: UK. Sample number: 22. Age: > 50 years. Gender: 9 male, 13 female SES: not stated. Ethnicity: not stated. Occupation/employment: 2 professional; 3 unskilled; 15 retired/pensioner; 1 semi‐retired. |
|
| Details of exercise programme | Not applicable. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, a fairly thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Petursdottir 2011
| Methods | Sampling frame: advertisements in clinics and newsletter. Data collection: indepth interviews. Data analysis: Phenomenological Analysis. |
|
| Stated aim of study | To increase knowledge and understanding of the experience of exercising among people with OA and to determine what they perceive as facilitators and barriers to exercising. | |
| Details of participants | Country: Iceland. Sample number: 12. Age: ≥ 50 years. Gender: 44 men; 72 women. SES: not stated. Ethnicity: not stated. Occupation/employment: 6 retired/pensioner; 1 full‐time; 2 part‐time; 3 disability pension/allowance. |
|
| Details of exercise programme | Not applicable | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, a fairly thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/Fair breadth, but limited depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Stone 2015
| Methods | Sampling frame: advertising through posters in physician's surgery, with snowball recruitment used to extend sample beyond initial volunteers. Data collection: demographic survey and semi‐structured individual interviews. Data analysis: interpretational analysis: coding, categorisation and forming themes based on verbal trends. |
|
| Stated aim of study | To develop a broader understanding of patients' perspectives and experiences with physician‐recommended treatments and interventions for OA symptoms, with an emphasis on exploring facilitators and barriers toward regular physical activity participation. | |
| Details of participants | Country: Canada. Sample number: 15. Age: 30‐85 years (3 participants under 45 years, whose quotations are excluded). Gender: mixed. SES: Not stated Ethnicity: Not stated Occupation/employment: 3 retired, 12 working. |
|
| Details of exercise programme | Study was an exploration of attitudes to exercise and physical activity, and details of exercise participated in are limited. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data collection? | Yes, fairly thorough attempt. | |
| Were steps taken to increase rigour in data analysis? | Yes, several attempts. | |
| Were the findings of the study grounded/supported by data? | Well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Thorstensson 2006
| Methods | Sampling frame: exercise intervention. Data collection: interviews. Data analysis: Phenomenological Analysis. |
|
| Stated aim of study | To describe how middle‐aged people conceive exercise as a treatment for knee osteoarthritis. | |
| Details of participants | Country: Sweden. Sample number: 16. Age: ≥ 45 years. Gender: 10 male, 6 female SES: not stated. Ethnicity: not stated. Occupation/employment: not stated |
|
| Details of exercise programme | Part of an intervention; details not provided. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, minimal few steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, a fairly thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Veenhof 2006
| Methods | Sampling frame: from RCT investigating behavioural graded activity. Data collection: indepth interviews. Data analysis: grounded theory approach. |
|
| Stated aim of study | To investigate which factors explain the difference, after a behavioural graded activity programme, between people who successfully integrate activities in their daily lives and those who do not succeed in integrating activities in their daily lives. | |
| Details of participants | Country: Netherlands. Sample number: 12. Age: ≥ 55 years. Gender: 4 male, 8 female SES: not stated. Ethnicity: not stated. Occupation/employment: Not stated |
|
| Details of exercise programme | Provider(s): physiotherapists. Training: yes. Setting: primary care. Content: behavioural graded activity delivered individually according to strict protocols directed at increasing the level of activities in a time‐contingent way, with the goal being to integrate these activities into daily living; included written materials such as education messages, activity diaries, and performance charts. Length/intensity: maximum of 18 sessions delivered over a 12‐week period, followed by 5 preset booster sessions in week 18. |
|
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, a (fairly) thorough attempt was made. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth but limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | Medium. | |
| Credibility of findings | High. | |
GP: general practitioner; OA: oestioarthritis; RCT: randomised controlled trial; SES: socioeconomic status.
Appendix 4. Themes: people's views of living with arthritis and exercise
Themes: people's views of living with arthritis and exercise
Symptoms
| Subtheme | Study | Direct participant data | Author description of data |
| Pain, muscle weakness, physical function | Campbell 2001 | "It [severity of knee symptoms] got worse and worse and I started falling down." p.135. "I was having trouble with my knees every so often it did hurt you know with one thing and another." p.135. "Because when you've got knees like this, you like to do other things, you think I'm gonna go ‐ I'd like to get back to how I was before, but I don't think that's ever going to happen now." p.136. |
None reported. |
| Hendry 2006 | "I can't walk as fast or as far as I used to because my knee hurts." p.560. "My knee is stiff, especially first thing in the morning or after resting." p.560. "Going downhill or downstairs is particularly painful." p.560. "It's absolute agony in spite of painkillers, so any activity is very limited." p.560. |
None reported. | |
| Hurley 2010 | Pain described as: "a niggle", "not too bad", "murder" or "agony." p.3. "…Getting out of bed, getting going, turning over in bed, waking up in the night…getting in and out of the car is a nightmare…" p.5. "…I'm limited now, I can't go out as often as before, you know." p.5. "…It alters your life…it swings your life right round, it restricts you…" p.5. |
Typically, people described episodic pain that increased gradually over several years. Pain varied greatly within and between participants, described variously. Often weight‐bearing activities brought on pain, but people with advanced disease also had pain while sitting or in bed. The unpredictability of pain bewildered people. p.3. | |
| Morden 2011 | "I mean, I now work at (Supermarket X) shelf filling and I've actually bought a set of knee‐pads. The tilers use them. Yeah, I put them on, it's a source of amusement for most other people, but they are not 'with it' ‐ the kneeling on a cold floor, for eight hours a day. Young people don't realise what they're doing to their knees. I tried it for the first week and I couldn't walk. I've got my kneepads, now. I can do the job with no problem at all, no problem at all. My knees are as good as they were before I went to (Supermarket X)" p.194. | Frequently participants discussed how they make adaptations and adjust routines to enable them to continue in their daily tasks in the face of painful symptoms. This could include bursts of activity followed by rest and using heat rubs, making adaptations to the household such as rearranging the order of kitchen shelving or altering walking routes to avoid hills if they found them problematic. For example, Michael had experienced knee pain for several years. He was a keen keep fit fanatic and engaged in regular exercise. The pain from his knee caused him difficulties when bending and also prevented him from placing his knee on hard surfaces for too long. Michael works as a manual labourer for a large supermarket chain. In his account, he discussed the importance of having to work to help keep the family home, arguably part of a moral need to maintain a sense of competency in his social role which, in turn, was related to his sense of self. He outlined a particular self‐initiated strategy that helped to maintain his role as a contributor to the family home. Michael discovered this particular strategy after going on a tiling course when he was unemployed. This particular knowledge helped him to plan and ensure his knee pain was manageable while working. pp.193‐4. | |
| Petursdottir 2010 | "It was like my body was made of lead." p.1020. | A few of the women mentioned "paralyzing fatigue" as a major barrier for getting anything done and felt it might be related more to mental fatigue than to physical fatigue. | |
| Stone 2015 | "I'm always in pain and agony, every movement is a chore. Sometimes, I just stare at my stairs, dreading what comes next." p.8. "I can't bend down. I can't get on the floor, if I do, it is a chore for me to get up. Bending my knees hurts all the time. Walking now seems to be hurting me as well. (P5)." p.9. "If someone called to play ball or something I would say, "I'm busy, I can't, and pretty soon I realized that I couldn't do it, not that I didn't want to, I just couldn't anymore. It wasn't worth the pain." p.9. |
Multiple participants expressed being in a constant state of pain, in which any movement, let alone "stressful" exercise, was overwhelming. This statement exemplifies the difficulties many participants expressed when attempting to accomplish functional tasks, such as ascending and descending staircases. Other functional difficulties included pain during walking, showering and bending. These activities of daily living were frequently described as "chores." p.8. In addition to these limitations, participants spoke of fatiguing rapidly, which made considering physical activity as more of a challenge. Some participants elaborated on this "fatigue," explaining how OA pain caused them to feel "broken" or "100 years old," and often motivated them in avoiding social interactions that involved some sort of physical activity. p.9. |
| Subtheme | Study | Direct participant data | Author description of data |
| Capacity to exercise | Campbell 2001 | "When I did the exercises in the beginning, it wasn't painful with the tape on, so I think that was how I was able to get on with them so well…whereas if the tape came off and I didn't put it on it was more painful." p.135. "I see people come in with arthritis and I think oh…god they are in terrible trouble and absolute agony and I think well I've got nothing to complain about." p.135. |
The perceived severity of knee symptoms was an important factor in motivation, with those experiencing severe pain or loss of mobility (or both) being most likely to continue to exercise. p.135. The existence of other comorbidities, comparison with other people with more limiting disease or a stoic attitude to knee symptoms all seemed to be associated with an attenuation of the motivation to comply. p.135. |
| Hendry 2006 | "Anything that would jog or jar my knee would really hurt." p.560. "I can't swim anymore because breaststroke is bad for my knee." p.560. "It's hard to get going on a bike and very painful." p.560. "I've reached an age where exercise doesn't help, I just get tired." p.560 "I'm not fit and agile enough to do exercises." p.560. |
Participants' ability to exercise was limited by the pain and stiffness in their knees, which restricted the type and amount of exercise that was possible. Ability was also limited by a perceived general lack of physical fitness, sometimes attributed to old age, as well as comorbidity including angina, lymphoedema, congenitally malformed hip and osteoporosis. p.560. | |
| Hurley 2010 | "…Well there's hardly a good day you know. I mean I just make the best of it. I don't try to you know, let it get me down. Although I have pain, I'll try and do what I can do you know rather than to just say' I am in pain I can't do that'…" p.5. "…I'm good at going up stairs, it's the coming down I have difficulty with." p.5. "…It's very tiring walking round shops…Some days I just sit here most of the time because it's too painful to move…" p.5. "…my daughter has to be with me to have a bath…I can't move, I can't push my legs down from my knees, they won't function…I can't do shopping…my daughter does it all, yeah. You know, I mean she's ever so good to me…She does things, she does this of a morning before she goes to work…" p.5. "…I don't have a bath. I can't get up and down…I stand in the bath and wash down." p.5. |
Pain, muscle weakness and fatigue after common activities of daily living impaired people's physical functioning and mobility. They stoically tried to carry out their normal activities, but often had to adjust or avoid activities (e.g. showering instead of bathing) to cope with their limitations and maximise their independence, and depended on family and friends for help with essential domestic and social activities (e.g. shopping, housework, gardening, transport, bathing). | |
| Moody 2012 | "Umm, I suppose the things that sort of do prevent you are if you get ill. One thing, that's probably the only thing would be if I got ill…I probably wouldn't be able to go, but only that would keep me away." p.67. "Well for me, at first that's why I missed some of them. I couldn't go more than one because I was just so tired the next day and would sleep so sound, you know at the night‐time, that I couldn't always wake up early enough to get myself organized to get the bus." p.67. |
1 barrier to ongoing participation was that of illness. For some participants, fatigue was an issue. | |
| Petursdottir 2010 | "The effort to get clean afterward is really hard…You just don't have the energy to take a shower." p.1020. | Pain was a crucial issue in the interviews, being a barrier in itself, but the hope of decreasing the pain by exercising turned out to be a major facilitator to encourage regular exercise. The participants described the difficulty of having to constantly adapt their exercise pattern to pain that could vary from day to day and even be too intense to be able to exercise at all. p.1020. 1 woman expressed her deep concern regarding how pain and fatigue led to difficulties with personal hygiene. She believed that people with chronic pain hesitate to exercise because they do not feel up to taking a shower afterward. p.1020. |
|
| Thorstensson 2006 | "You need to have the will to do it…when you are well you don't do it, and when you need to do it, then it hurts and therefore you don't do it (laughter)." p.55. "And even if it hurts a bit, one should not give in but of course sometimes you can feel sore or aching joints afterwards, if it hurts when doing certain movements…of course it hurts, even when exercising." p.55. |
‐ |
| Subtheme | Study | Direct participant data | Author description of data |
| Impact of exercise on the effects of OA | Campbell 2001 | "Since I started strengthening these muscles it seems I don't fall over so much which is good…" p.135. "I still do [the exercises] and I remember to stand the correct way without even thinking about it now…[The pain] has been a lot better, much better, and I can do things better. Dressing ‐ I don't have to hold on to anything, I can balance now and in fact, you know, I find it a great improvement." p.136. "I was able to do [the exercises] pretty easily but it didn't appear to me to make a lot of difference…I carried them on during the time I was taking part in the programme although I've dropped them since." p.136. |
High levels of continued compliance were closely related to the perception that the physiotherapy intervention was effective. Those who noticed an improvement in their knee symptoms were much more likely to comply than those who did not. However, if the benefits of the physiotherapy were not perceived as sufficient, or there was an allergic reaction to the tape, non‐compliance was a rational outcome. p.136. |
| Hendry 2006 | "Exercise is the best thing for relieving the pain." p.561. "Exercise doesn't help pain but it gets it going, improves stiffness and mobility." p.561. "Exercise doesn't help my knees at all." p.561. |
Some people found that exercise was helpful for relieving pain; other people found that pain persisted, but stiffness and mobility improved; other people found no improvement in knee symptoms. p.560. | |
| Hinman 2016 | "The pain is different pain and I feel that I can do things easier now than I could a while back." p.486. | None reported. | |
| Hurley 2010 | "…the exercises we did at (centre) were helping. and see I haven't had the pain…it was very helpful." p.7 "…I felt generally strong, you know. Walking up stairs, I mean, at times I used to have to go up one step at a time, but then after the exercise I could just walk up the stairs and I was even beginning to try to walk normal…" p.7. "…I was disappointed, because I hoped, I just hoped…but it didn't sort of do what I wanted it to do for my knees and I don't think anything will…I think your age, as you get older, you know, you get a bit dodgy." p.7. "…If I can get myself back to a little bit of [line dancing] then I kind of umm, my life is kind of coming back to normality, you know, cause it can take over your life a bit as I say, you are scared of what to do and what not to do…" p.7. |
Most participants found the programme "interesting" and "informative," bringing "small" to "life‐changing" improvements in pain and function (i.e. walking, domestic and social activities, getting on and off buses, driving). They felt less tired and had a general sense of better physical well‐being. p.6. The physical and psychological improvements returned a degree of normality to people's lives. Some returned to previous activities they had begun to avoid for fear of harm, or take up activities to increase their level of physical activity. p.6. 2 participants were "disappointed" in the programme, experiencing little or no benefit from. This may have been a factor in the participants who withdrew from the study. The small number of people who found the programme ineffective makes it difficult to explore the reasons for ineffectiveness, but the 2 participants believed themselves too old or their symptoms too severe to enable them to benefit from exercise, and were sceptical and pessimistic about all interventions. p.6. |
|
| Larmer 2014b; Larmer 2014a | "It's just a relief to get into the water to get out of pain." p.91. "It takes your mind off, my pain. It's there all the time but when I get into the water, it lifts away from me." p.91. |
Pain relief was described as a benefit from hydrotherapy and was ascribed to warmth and buoyancy…Not only did the pain itself ease, but hydrotherapy helped participants shift the focus from the constant pain that they were experiencing. p.91. | |
| Moody 2012 | None reported | Participants described the perceived health benefits they received from attending the programme, such as an increase in movement or mobility, an improvement in breathing, a decrease in their pain levels, balance had improved and a reduction in falls. p.66. | |
| Petursdottir 2010 | "Exercising has a good effect on everything, including the heart." p.1020 | Many benefits of exercising concerning the OA symptoms were mentioned. Other general effects were also mentioned, such as increased fitness and a better heart condition. p.1020. | |
| Stone 2015 | "Sometimes, after a long day, I'll throw some ice on my knees, take a hot bath after. It feels great…Using the heat was my favorite part of my physiotherapy…That is probably the only way I could handle exercising." p.14. "The physiotherapist professionally guided me to feel less pain. It made me want to do exercises on my own." p.14. |
Pain relief. When participants were able to moderate their pain effectively, they were motivated toward contemplating physical activity adoption. Participants commonly found heat and hydrotherapy helpful for pain management. p.14. Participants also noted that positive experiences with physiotherapy inspired them toward physical activity. |
|
| Thorstensson 2006 | "…exercise hurts. The pain was almost unbearable but I still carried on. Yes, it was very strenuous, but that's how it is, the pain becomes increasingly worse, I think…it just becomes more and more painful." p.55. "…for example, walking longer distances, there are limits, but nevertheless longer walks without experiencing pain. It is a huge difference. So it was very positive…it makes it possible to work more and you can do more enjoyable things too…Go fishing and hunting, walking the dog. All those things, like simply going for a walk." p.55. "…when I have been walking for a while, the pain goes away, which makes me happy." p.55. "…exercise can help, I am convinced about that, although it did not work for me…the damage was too great when I started. It had gone too far. If one had started to exercise five or six years earlier, it might have helped." "In my case…the damage became worse, it only led to more pain instead of improvement." p.56. "it [the exercise] was beneficial and it helped in the short term. However, had I not received injections I would never have been able to work for so long. It is thanks to them that I have been able to work for the past five or six years or since I got osteoarthritis. That is a fact." p.56. |
To experience symptom relief. This conception contained experiences of the effects of exercise on pain and other symptoms. Statements ranged from total pain relief to a worsening of symptoms. p.55. To deprecate; the belief that exercise could cause harm or be unnecessary in that the informants considered other treatments to be more effective. p.56. |
|
| Veenhof 2006 | "I continue with my exercises, they are integrated in my daily living. I really know these exercises have beneficial effects and that motivates me to continue with my exercises. The main motivation to do all this is to prevent an operation to get a new hip." p.275. "Although I experience the same level of pain, I have learned to continue with my activities and I realise that I achieve more because of that." p.275. |
First, the initial motivation of the participants played an important role. Some participants were motivated to reach short‐term goals, e.g. to decrease pain, while other people were motivated to reach long‐term goals, e.g. to postpone an operation or to live independently for as long as possible. It appeared that all adherent participants were initially motivated to reach long‐term goals, while all non‐adherent participants reported a short‐term initial goal or had no specific goal. These participants tended to stop performing their activities as soon as the short‐term goal was obtained. Therefore, there seems to be a relationship between the initial motivation in visiting a physiotherapist and exercise adherence. p.275. |
Health beliefs and views on the management of OA
| Subtheme | Study | Direct participant data | Author description of data |
| Aetiology and prognosis of OA | Campbell 2001 | "I was having trouble with my knees every so often it did hurt you know with one thing and another. Working in the construction industry there is a lot of lifting and a lot kneeling you see and I felt well I wonder if that's got anything to do with it…" p.135. | ‐ |
| Hendry 2006 | "It's caused by heavy work, always being on your feet or doing a lot of sport when young." p.56. "Being overweight has made my knee problem worse." p.56. "It's a vicious circle; you put on weight because you don't want to exercise when your knees hurt and then they hurt more because of the extra weight." p.56. |
Some believed that their joint problems were a direct result of excessive sport or heavy manual work when younger. p.561. | |
| Hurley 2010 | "I think it's just wear and tear. I think it's just accepted that you're going to get these things as you get older." p.5. "…I was very athletic when I was young, and you know yourself with the athletes the injuries they get affects them later in life." p.5. "…My daughters have trouble with their knee now as well, don't know if it's inheritance…my granddad suffered with it, my mother's troubled with it." p.5. "…Well as I say, I need to lose weight…Well I mean there must be a lot of pressure on my knees as well, because I am overweight." p.5 "…I hope not permanent." p.5. "…I think probably it might get worse because it has been getting worse over the years." p.5. "…I think, having to sit in one of those [wheelchairs]…I wouldn't want to do it, I don't want to get to that stage…" p.5. "…nothing will stop it getting worse I'm sure…if you have a replacement thing well alright that'll be alright but I mean otherwise they [his knees] just go on getting older…" p.5. |
People were uncertain and bewildered about how, why and when their knee pain started. Most attributed knee pain to mechanical "wear and tear" of occupational, sporting and leisure physical activities, which led them to believe knee pain was an inevitable consequence of normal ageing. Some people tried to identify a specific incident as the start of their pain, but their recollection of the incident was often vague and they struggled to convince even themselves that this was the start of their problems. Frequently a familial predisposition for joint pain was mentioned with reference to a close relative, often female, who had "arthritis" or "rheumatism." p.3. People hoped rather than believed their symptoms would improve. They reasoned that joint damage was irreversible and likely to deteriorate without surgical correction. These beliefs arose from people linking the cause of joint pain to their biography, and the influence of other people's experiences and beliefs. p.6. |
|
| Morden 2011 | None reported. | A large number of participants described their knee pain as something unremarkable or related to ageing. p.193. |
| Subtheme | Study | Direct participant data | Author description of data |
| Non‐exercise management strategies | Campbell 2001 | "I am not a one for taking a lot of tablets. I get a bit dubious, you know, so I just learnt to live with it for a bit and then I had the chance of [the trial]." p.134. "I'm a great believer in physiotherapy anyway I think. I don't agree with drugs quite as much as, I think, if you can have it naturally." p.134. |
A dislike of taking prescription drugs and a positive view or experience of physiotherapy also provided an initial motivation to comply. p.134. |
| Hendry 2006 | "I'm not keen to take things because they're not going to cure it, and I mean to hide it is not strictly a good idea because you do things and it makes it worse." p.561. | Analgesics were used warily, as there was concern that they might disguise the warning function of pain. p.561. | |
| Hurley 2010 | "…I don't want too many tablets in me…I can try and bear pain myself." p.5. "…I do really try to keep off drugs because, you know, I mean I think that they all have side effects." p.5. "I'm waiting for a knee replacement, cos I find it very difficult to get around, you know…I'm hoping the operation will correct it." p.5. "…I'd have to be a lot worse than what I am now I think…well I mean if I've gone for thirty years I can go on for a few more." p.5 (about surgery). "…I don't want knee surgery, I've seen it happen; I've seen people have it very successfully and I've seen it be a disaster." p.5. |
People used analgesia reluctantly, usually when pain was severe or before/after activities that exacerbated pain (e.g. shopping, gardening). They were concerned about adverse effects, becoming addicted and worried that taking it regularly would reduce its effectiveness. People taking medication for common comorbidities (e.g. diabetes, cardiovascular, respiratory disease) wanted to limit the medications they were taking, preferring to omit analgesia and cope with pain rather than omit medication for comorbidities seen as more serious, over which they had little control. pp.3‐4. People reasoned that while medication might alleviate symptoms, surgery was the only way to correct structural joint damage, eliminate pain and restore mobility, function and independence, but they wanted to delay surgery as long as possible. Other people were more sceptical and frightened of surgery. Whether people held positive or negative expectations of surgery was strongly influenced by the experiences of family, friends, media reports or presence of comorbidities that contraindicated surgery. p.4. Awareness of treatment options other than medication and surgery was poor. Many people were using alternative remedies (e.g. fish oils, glucosamine, herbal remedies, acupuncture, osteopathy, copper bracelets, etc.) on the recommendation of family, friends, media reports and advertisements. Some people found these helpful, other people were sceptical but often continued to use them in the hope they would prevent or delay progression." p.5. |
| Subtheme | Study | Direct participant data | Author description of data |
| Advice and information from health professionals | Campbell 2001 | "So I go to the doctor and all he just simply done was put his hand on my knee, he said "move your leg…you are getting old you've got rheumatism." You see that was it I didn't take any more notice of it [the knee pain]." p.135. "She [the physiotherapist] said the kneecap is out, so she taped it up and pushed it back…So now if it starts aching, that's what I do. I tape it up and push it back to where it should be." p.136. |
As the model described in fig 1 of Campbell 2001 suggests, these ideas (about exercise interventions) were sometimes shaped by people's previous experiences of health care. p.135. |
| Hendry 2006 | "My doctor told me to keep exercising and not to stop." p.561. "…they [hospital doctors] said, 'the walking's agitating you, your joints, so stop it'." "The physiotherapist told me to exercise." p.561. "My doctor showed me how to do quads exercises to strengthen the muscles." "My doctor gave me a referral to the gym." p.561. "I was given advice about exercise at the gym." p.561. "At the hospital they told me I shouldn't overdo exercise, I should look after my knees." p.561. "He told me to take painkillers and keep my knees moving but he didn't advise any particular kind of exercise." p.561. "I haven't had any advice about exercising and what exercises to do." p.561. "Doctors could give you more encouragement to exercise; I had to get the referral form from the gym myself and ask him to sign it." p.561. "I think they would have told me in the clinic if I should be exercising and what exercises to do." p.561. This could be more relevant in/similar to 'influence of program supervisors in terms of individual instruction and the 'knowledge' is a secondary part of this; currently quoted in text for this themes: "…I had to stick rigidly to what he had said, the weights that he had specified…the idea was to stretch it that little bit further than I normally would do in order to support the joint more…but too much would…cause more damage and not enough wouldn't do any good…I was quite impressed actually by his knowledge…and I did exactly what he said and I did notice an improvement, a definite improvement." p.563. |
Advice from health professionals was mainly in favour of exercise and consisted of encouragement to exercise, advice about specific exercises and referral to a gym. Sometimes the advice was vague or absent. p.561. Occasionally exercise was discouraged. p.561. The expert advice and supervision available in gyms or from physiotherapists was valued. p.563. |
|
| Hinman 2016 | "I was a bit sceptical at first and when the exercises came I thought 'hang on, this has got nothing to do with the knee as far as I understand' being ignorant, you know. Now I sort of feel that 'hang on, yeah there is a difference' because the work has paid off." p.486. | All 3 groups of participants referred to the importance of giving and receiving information. p.483. | |
| Hurley 2010 |
"…[participants GP] never said anything, that's why I have always thought it's not worth bothering about. He's not bothered so I am not bothered…" p.5. "…I learned so much from [the physiotherapist]…I learnt about pain management…" p.7. "…It helped me understand arthritis much better…" p.7. "…I class it as spring cleaning my mind…" p.7. "…[helped understand] how to cope with pain…that exercise does help ease the pain and helps your mobility…" p.7. |
Our inclusion criteria meant all participants had consulted their GP about knee pain. People were often told the problem was due to wear and tear and getting old. Few could remember receiving information or advice, and they perceived knee pain was considered a benign condition that did not have a high priority, which confirmed their own beliefs and attitudes. No‐one had been offered a self‐management programme. Management was seen as ineffectual, and consequently few were regularly consulting their GP despite ongoing problems. p.3. Management usually involved people being offered palliative medication. p.3. Receiving information and practical advice about what (not) to do, and the opportunity to discuss things that concerned and confused them with a healthcare professional, helped people appreciate their problems and what they could do to address these. In particular, they learned about the role of inactivity and excess bodyweight in development of knee pain, and how exercise and losing weight could control symptoms. p.8. |
|
| Petursdottir 2010 | "He encourages me in every way." p.1021. "They have not done it [encouraged exercising]." p.1021. "They [the physicians] are positive if you ask [for a referral to a physical therapist], but you have to ask." p.1021. "Now I think I handle it more wisely. I know better because I've been fortunate to get good instruction." p.1021. "There are many 60 year‐olds who don't use computers to get information. And these are the people with arthritis! I think it is much easier to get information to the younger people. We use the Internet." p.1020. |
The encouragement of physicians to exercise was very important to some of the participants. However, this encouragement (i.e. whether physicians emphasised exercise) varied. Whether physicians referred their patients to physical therapists also varied. p.1021. Participants' knowledge of both general health and OA was of high importance. Most of the participants had experienced being educated by their physical therapists. Some participants wondered how to get such information to the public. p.1020. |
|
| Stone 2015 | "My doctor told me to go on a [recumbent] bicycle for 20 minutes a day, or whatever was easiest for me. So she tells me to pick up my hands [to the sky], which I can't do because of arthritis in my back. So then she tells me to pick up my legs or do sit ups…But I can't do those either! I'm so confused. I just find it easier to do nothing. (P3)." p.12. "I was never prescribed exercise. My family doctor and rheumatologist have never even mentioned it. If my doctors don't think it's important, why should I? (P1)." p.12. "When I was first diagnosed, I didn't know what to think. I knew it wasn't good, but I didn't know how bad it was going to be. After a couple of years, the pain was too much to bear and I thought, that's it…my life is over. And no one warned me…I didn't even know what to do…exercise was the farthest thing from my mind." p.6. Many participants echoed, "If my doctor tells me to [exercise], then I will" (P1, P4, P5, P6, P7, P8, P10, P11, P12). p.14. 1 participant noted, "If [my doctor] told me what to do and how to do it, I'd be at the gym right now" (P6). p.14. |
Participants were knowledgeable of the benefits that physical activity can have for the general population; however, many were unaware of specific OA‐related benefits and unsure of what activities would provide optimal self‐management. Furthermore, participants noted that physicians often provided them with counteradvice or did not offer any recommendations. This created further confusion about physical activity and the potential benefits for OA. p.12. Much like the quotations above, many participants held the perspective of being inadequately educated about exercise by their healthcare providers, and rarely having an open dialogue regarding prescribing exercise or physiotherapies (or both). This lack of communication regarding exercise and physical activity was compounded with a participant perspective of having inadequate knowledge/communication regarding their OA diagnosis in general. This increased confusion often related to their disease and alternative treatment options. p.12. All participants spoke about the instrumental role of healthcare providers in influencing and encouraging physical activity. Participants expressed that if their physician advocated exercise, they would be eager to adopt it. p.14. In addition, participants desired more knowledge and specific guidance related to physical activity. p.14. |
| Subtheme | Study | Direct participant data | Author description of data |
| Health beliefs and managing OA and exercise | Campbell 2001 | "[the exercise and taping]might not help me because I'm getting old but it might help somebody else…I just think I'm too old really to improve." p.136. | Ideas about the cause of arthritis also played a part. Those who thought that arthritis was caused by immutable factors such as age, obesity and "wear and tear," tended to have a resigned attitude towards their arthritis. As a consequence, they found it hard to believe that the intervention could be effective and this weakened the resolve to comply. In contrast, those most likely to be continued compliers tended to believe that although there was no cure for arthritis, there were things they could do to minimise its impact, including the physiotherapy. p.136. |
| Hendry 2006 | "If it's wear and tear on the bone, is it helping to do all this exercising, walking and that?" p.561. "So your movement is important; this is why I want to get back into a regular exercise routine, so I can do more to help myself." p.562. "You should do moderate exercise; overdoing it could make things worse." p.562. You can't do too much exercise; take painkillers, if you need to, and keep going. |
Many participants were worried that exercise was wearing out their joints. They reasoned that if OA is caused by wear and tear, then exercise would exacerbate the disease process. p.561. Some participants were determined to take control of their disability and used exercise as a means of actively maintaining or improving their mobility. In some cases, this determination was such that they continued to exercise in spite of a belief that OA was caused by 'wear and tear.' p.562. 1 participant felt that it was impossible to do too much exercise, but people felt that excessive exercise would make the knee problem worse. However, other people had become resigned to their physical limitations. p.563. |
|
| Hinman 2016 | "I know now it's going to be for my benefit. I keep on doing these exercises…if I stop, pain comes on again, and I can't do any activities." p.485. | No direct description. | |
| Hurley 2010 | (Before intervention): "…I get the pain and there is nothing that can be done about it…" p.5. "…I'm questioning whether exercise might exacerbate or ease it. I really don't know." p.5. "…I got a little bit frightened of doing exercise because I don't know what exercises will be detrimental to the knee or advantageous to it." p.5. (After intervention): "…I thought if I exercise I am going to make the pain worse…they have showed me that I can still exercise even though I have a bad knee…" p.7. "…I feel that I am not thinking about my knee pain anymore as a pain, I think about it more as preventing it by doing the exercises." p.7. "…[arthritis]can ease…but there is no cure for it, so it's learning to live with it…" p.7. "…I'll go on as much as I can doing the exercises…" p.7. "…I thought it was good, very good. To my mind I was helping to do something to help my knee pain…" "…This [exercise] is much better because like I said I found is helpful, because I don't take any medicine…" "…If you don't exercise you're never going to be able to manage the pain…Gentle exercise actually relieves the pain, and it means that you should be able to cut down [analgesia] and that the answer is not necessarily knee replacement…" p.7. "…I mean exercise might stop it from getting worse any sooner that it would have done…before it deteriorates to the point where an operation might be needed…" p.7. |
As a result of this confusion, and in the absence of any advice about what they should (not) be doing, few people were exercising and most were refraining from or avoiding activities. p.5. Participation in the exercise regimen allayed people's fears, confusion and anxiety about the safety of exercise and showed them it was beneficial. Its successful completion convinced participants that exercise was an effective self‐management strategy they were capable of implementing and a viable alternative to medication that might slow deterioration and delay or avoid surgery. p.8. |
|
| Petursdottir 2010 | "There is nothing that can be done about the OA; therefore, I do nothing." p.1021. | Only 1 woman did not exercise. She worked part‐time and believed that was quite enough activity. p.1021. | |
| Thorstensson 2006 | "Well, I am worried, I sometimes think that if it hurts when I do something it will cause even more damage." p.56. "…I now know that it is beneficial. I know that simply going for a walk every day is very good for me. In that way I have changed. Previously I was not even aware that it was necessary." p.53. "It can't have improved just like that. It [exercise] must have helped. So that's why I've found it beneficial in all sorts of ways, and it has changed my attitude to this kind of exercise. It must have done it." p.53. "Well, it is different now because, as I've already said, previously you exercised to maintain your level of fitness whereas now you exercise in order to regain your physical condition." p.55. |
To hesitate. This conception contained doubts about the benefits of exercise. Experiencing pain while exercising made it difficult to decide whether it was beneficial or counterproductive. p.53. To experience coherence. This conception contained statements about connecting knowledge about OA with knowledge and experiences of exercise. The informants expressed satisfaction and were convinced of the effectiveness of exercise. p.56. |
| Subtheme | Study | Direct participant data | Author description of data |
| Everyday activities versus structured exercise programs | Hendry 2006 | "Day‐to‐day activity isn't enough to keep you mobile." p.562. "There's a basic level of exercise that I have to do to keep the joints flexible, so I can get up and move around." p.562. "I get enough exercise leading an active life." p.562. |
There was a broad range of opinion as to the appropriate level of exercise. Some people felt that keeping active was sufficient; other people that this was insufficient. p.563. |
| Moody 2012 | "Exercise in water, it's not like walking or running…you're not jarring any limbs or bones…And for old people I'm, I'm not sure (land‐based exercise) is the best sort of exercise that you could do." (p.66). | Participants were of the opinion that exercise in water was superior to other forms of exercise for them. They talked of other types of exercise they had tried and how land‐based exercise caused pain whereas water‐based exercise did not. p.66. | |
| Petursdottir 2010 | "And I think that it is important when people choose which exercises to do, that you enjoy it, that you feel it is rewarding…these positive factors have to be present." p.1020. | The participants described the importance of suitable exercise…the importance of finding an enjoyable training mode. p.1020. | |
| Thorstensson 2006 | "I really don't think that I need to take some exercise but I just tell myself that I am going shopping and things like that." p.55. "I try to walk more and more, to walk in the correct way and to climb stairs in the correct way and not to wear myself out." p.54. "Well, with respect to time, I try to be out for at least half an hour and then I try to go for a longer walk at the weekend, perhaps for up to an hour." p.55. |
The informants described their need to exercise. The statements ranged from conceptions about the importance of exercise in order to maintain physical functioning, to the fact that daily living demands movement. p.55. |
Psychological
| Subtheme | Study | Direct participant data | Author description of data |
| Impact of OA on people's sense of "self" | Hurley 2010 | "…[inability to do gardening] makes me mad at times, cos I feel frustrated about it. I know there's masses of things that want to be done out there, I just haven't got the energy to do them…It makes you feel older." p.5 "…I'm very upset with myself cos, you know, when you're used to being mobile and able to do things for yourself, now you have to depend on people to do it, it's not very nice is it?…It's embarrassing. Like [at a dinner and dance] I sat down and had the dinner, and when I was to get up I couldn't move. I was so embarrassed and people looking at me." p.5. |
Limitations in functioning and the need for help made people feel frustrated, angry, depressed, embarrassed, incapacitated and a burden to other people, and increased worries that the ultimate outcome would be severe disability, immobility and dependency. p.3. |
| Morden 2011 | "Today I am very tired and in quite a lot of pain, I went fishing with my grandson for the full day yesterday. Even though I enjoy the sport and have warm gear and wet gear, it still knocks me about. With having back pain and knee pain anyway, I can't stand for long. I was given a folding chair for Christmas, and very useful it turned out to be. With being able to adjust the chair to several positions and also the height I can usually find a position that suits me. One of the problems about not being able to walk very far is that if we want to go somewhere that we haven't been before we have to do lots of research into the place. We have to check to see if the terrain is reasonably flat, and if not, how far I will have to walk." p.194. | In James' account, his biography became disrupted due to a combination of back and knee pain. As a result, his physical capacity to work declined forcing him to retire early. His sense of self as male provider and head of the family was challenged. His account highlights the process of changing his role and renegotiating his sense of self as a family man. By taking on more of a carer role in the sense of looking after grandchildren and doing more work around the house, he was able to engage in what Gareth Williams calls 'narrative reconstruction.' As part of this process, James is constantly engaged in activities, strategies and treatments to enable him to carry on in a social role within the context of family life that was important to him. James' position as a 'good grandparent' sees him constantly negotiating ways to maintain physical and psychological well‐being. Spending time with his grandson both aided and threatened. For example, by taking regular shared fishing trips, he not only gained pleasure and psychological well‐being, but also incurred pain and suffering. Embedded in James' account are a number of strategies that he has to utilise to ensure continuity that he can continue valued activities: James, Diary 2 entry 18th January 2009. Here, we can see how James negotiates the negative part of 'being a good grandparent' (pain) to maintain a valued identity. This requires the application of aids (chair) and planning (research into place) p.193. A broader perspective of self‐management is witnessed in the accounts. Examining how people maintain acceptable social roles, remain competent moral actors and preserve a sense of self is central to understanding self‐managing in chronic illness. Taking such an approach acknowledges the essential part that making adaptations in daily life plays, so that people are able to continue valued activities, fulfil obligations and roles. p.194. | |
| Petursdottir 2010 | "I was extremely unhappy with myself…I couldn't work as hard as before, and I just could not understand why. It was one of the hardest things, to accept myself as what I had become." "Well, you have to face the fact that you are not young anymore, and you just have to slow down." p.1019. "I worked out new ways to cope, to keep my arthritis from getting in the way too much." "I think that general positivism is part of your health; if you think constantly about pain and aches, then you get really sick." p.1018. |
Many of the participants described how they had to fit their OA into their self‐image and adapt their lives to it. Some of the younger participants seemed frustrated. The older participants expressed greater acceptance. The personality traits of adaptability and initiative had a strong influence on the exercise behaviour of the participants. They described the importance of not letting the OA control their lives, although its existence should be recognised and respected. Many participants talked about the importance of mental health and the importance of being positive, cheerful and not lingering on negative circumstances. | |
| Stone 2015 | It definitely wears on you, on your mind because it stops you from doing what you want to do. Even if my body wanted to [exercise], my mind won't let me…I feel helpless and worthless." p.5. | Participants expressed depressing thoughts, referring to OA as "mentally agonising." Many participants felt betrayed by their bodies and felt helpless regarding their functional limitations. 1 participant specifically mentioned, "Mentally, it's so depressing. I can't tell you how I just want to sit down and cry sometimes because I can't move." p.13. Other participants echoed this "helplessness," noting the effects of OA‐related psychological distress on their functionality. p.10. |
| Subtheme | Study | Direct participant data | Author description of data |
| Self‐efficacy | Petursdottir 2010 | "I worked out new ways to cope, to keep my arthritis from getting in the way too much." p.1018. | The personality traits of adaptability and initiative had a strong influence on the exercise behaviour of the participants. They described the importance of not letting the OA control their lives, although its existence should be recognized and respected. p.1018. |
| Stone 2015 | "Not only does it hurt when you [move], but it would hurt the next day. The pain never lets you forget…and believe me, I don't. The only thing I can do is not do it again. Avoid exercise, avoid the pain." p.9. | Low exercise self‐efficacy was consistently mentioned by other participants. Low levels of self‐efficacy demotivated participants from physical activity as they did not believe they could successfully perform a task without exacerbating their current pain levels. In addition to fear of pain on a daily basis (pre‐exercise) and fear of exacerbating pain during exercise, participants also expressed fear of experiencing pain after exercise of which they were determined to avoid. This fear avoidance of physical pain seemed to provide participants with a "logical" rationale for avoiding activity. p.9. |
| Subtheme | Study | Direct participant data | Author description of data |
| Psychological benefits of exercise | Fisken 2016 | "Strengthening your muscles…keeping your weight down…keeps you in shape." "Keeps the body moving, takes your mind off it, it's good to be outside. Yea, keeping active, or else if you've got osteo, it can get you right down, if you stay inside you just mope about it." p.14. | ‐ |
| Hendry 2006 | "You just feel great when you've done it…you know, they say exercise releases happy something in your brain and it certainly does…" p.560. "You feel great when you exercise, it gives you a buzz." p.561. "Exercise is part of a healthy lifestyle, it improves fitness and I feel better for it." p.561. |
Some commented on an improvement in general well‐being. p.560. | |
| Hurley 2010 | "…Overall I have improved…. it's a feeling of general well being really…I feel a lot better in myself, I mean mentally, mostly mentally…" p.7. "…If I can get myself back to a little bit of [line dancing] then I kind of umm, my life is kind of coming back to normality, you know, cause it can take over your life a bit as I say, you are scared of what to do and what not to do…" p.7. "…I didn't do no exercise, I didn't know I should do, I was frightened…but since I knew of the exercise, I have been doing it…" p.7. "…you are all in there with similar problems, and it's the friendliness, like on a, personal level." p.7. "…we formed very tightly knit group…we were all trying to help one another, you know." p.7. |
The programme reduced anxiety and fear of activities people previously thought might increase pain, increased confidence in their ability to exercise safely and effectively, and generated a sense of self‐achievement. p.6. The physical and psychological improvements returned a degree of normality to people's lives. Some returned to previous activities they had begun to avoid for fear of harm, or take up activities to increase their level of physical activity. p.6. Participants who received group‐rehabilitation thought meeting, sharing experiences and the support derived from fellow group members was beneficial, and that observing improvements in other people was a source of encouragement. p.8. |
|
| Larmer 2014b; Larmer 2014a | "It's been an awful shock to get sick…It's been really really difficult, so coming and talking to other people, probably has been almost as beneficial as doing the exercise and realising that you're not the only one." p.91. | Participants described psychological benefits from going to hydrotherapy…sharing and comparing their health condition with people who also had OA was also identified as beneficial. The sessions helped participants gain a better perspective on their condition, through comparing to other people and talking with other people in similar situations. p. 91. | |
| Morden 2011 | "So, you tended to be concentrating more on the dogs than on what you were doing. So you then noticed that you've been walking and you were getting more comfortable purely because your mind was distracted from the circumstances of the pain in the knee and the hip. So that was what we used the dogs for, but that was an incidental. It just happened that it was when you took the dogs out, you were distracted from the pain. So, you got your Physio." pp.194‐195. "I think swimming is one of the best exercises that you can get and I do feel when I've been swimming, that it does me good. Plus, I just love it. I enjoy it. It's a social thing as well and I just get so much out of it. I pay a fee at the gym and I only swim; I don't do anything else but I just love the place I go to. It's only just over the way and I just go every Monday, Wednesday and Friday morning so it's not just the exercise. The exercise is very important to me but it's everything that goes along with it. I've made new friends since I retired and I just find that completely satisfying; I enjoy it and I don't want to give that up." p. 195. |
One participant outlined the unintended beneficial consequence of walking his dogs, in particular, the fact that this was not just physical ('you got your physio') but also psychological in terms of distracting his thoughts away from pain. p.195. Another participant recognised the psychological, social and physical benefits of exercise and the combination of these factors provide the motivation to continue. p.195. Participants had some worries about the potential for damaging the joint, but their main concern was maintaining their social contacts, preferred leisure activities or sense of self as a 'fit and active' person. p.195. |
|
| Moody 2012 | "the social side of things is really, really good." p.66. "all in the same boat." p.66. "…sometimes being actually on your own to be motivated uh it's harder. It's harder: A lot harder." p.66. |
Participants spoke of the good social atmosphere of camaraderie created by the group and the instructor and the friendships that were forged. Exercising with other people made it more fun and enjoyable and participants found they helped one another. As they were "all in the same boat" they felt more comfortable and could empathisse with and relate to each other. Many people stated they would not have gone to water‐based exercise or similar exercise on their own. Some participants expressed frustration that they could not motivate themselves to go alone, but that there was no problem with motivation if they went with the group. Being part of a group contributed to motivation both for getting to the classes and also once they were there. p.66. | |
| Petursdottir 2010 | "I am more vivacious, both physically and mentally." | Most of the participants agreed that physical exercise improved their mental well‐being. | |
| Thorstensson 2006 | "…it has a beneficial effect on the whole body. It gives you a sense of well‐being, not just because you have done it and feel good about it, but your muscles feel as if they have benefited too." p.53. "…yes, I definitely feel better, apart from my knees that is…I'm more alert…. Perhaps not immediately afterwards but I feel more alert after a shower." |
To experience well‐being. In this conception, the informants described experiences of mental and physical relaxation, satisfaction and well‐being connected to the moments immediately following the exercise sessions. p.53. |
| Subtheme | Study | Direct participant data | Author description of data |
| Influence of programme supervisors | Campbell 2001 | "Well I felt because [physiotherapist] took the trouble of explaining it all to me I couldn't turn around and say, "well blow it, why bother sort of thing? you know?" And when I first turned round and said that I would do it, I felt well alright I wasn't obligated to do it but I felt let's do my bit towards it, you know. I didn't want her. p.134. ME: "So would you say that some weeks you do them [the exercises] two or three times?" Eileen: "Some weeks I can't…" ME: "Sometimes you can't make it at all?" Participant: "Yeah. Latterly. I think this is my own fault. I mean when I was going [to see the physiotherapist] every week you make yourself sort of do it don't you…I must admit I am not so good now I am not going." p.135. MT "Since you have stopped seeing [the physiotherapist] have you stopped doing the exercises?" Participant: "Yes I'm sorry I have yes. But as I said I haven't had no pain…I wondered whether it was temperature or dampness or something like that you see. Now there is nothing wrong with them." MT: "So you feel if there is nothing wrong with it you feel there is not much point in a…" Participant: "Well that's it. It's the wrong attitude I know." |
The complex reciprocity that surrounds the relationship between therapist and patient and the obligation patients felt towards the physiotherapist, particularly the desire not to let her down, were important reasons for high levels of initial compliance. One participant explained how difficult it was to continue the exercises programme since she stopped seeing the physiotherapist. p.135. |
| Hendry 2006 | "The gym instructors advise you and give you confidence that you're not going to make things worse." p.562. "I think the physiotherapist or someone with a medical background is the best person to supervise exercise." p.562. "At the gym they give you one‐to‐one attention and an individual programme that's right for your body." "The supervision at the gym is very good; they monitor what you do." p.562. "…I had to stick rigidly to what he had said, the weights that he had specified…the idea was to stretch it that little bit further than I normally would do in order to support the joint more…but too much would…cause more damage and not enough wouldn't do any good…I was quite impressed actually by his knowledge…and I did exactly what he said and I did notice an improvement, a definite improvement." p.563. |
The expert advice and supervision available in gyms or from physiotherapists was valued. p.563. | |
| Hinman 2016 | "The most important thing is listening to the physio and doing the exercises because he motivated me to do the exercises." p.486 | The impact of this feeling of accountability was to increase their motivation to exercise. People with knee OA described feeling accountable to their physical therapists and not wanting to let down the therapist. p.483. | |
| Hurley 2010 | "…I think it's really a lot, in fact an enormous amount, to do with the facilitator, she's both kind of encouraging and yielding and nurturing and understanding, but also was able to use a bit of steel and get us off our bums, you know, so she's got those kind of qualities naturally…" p.7. "…[Physiotherapist] gave us enormous confidence because she is such a, she is very very confident, obviously highly qualified, so it was good to have some body for an hour giving you good advice, which was sound…" p.7. |
The care, support and guidance participants received during the informal discussions helped build a trusting, collaborative partnership between patient and physiotherapist. This increased participant's confidence and trust in the physiotherapist and belief in the rehabilitation programme. The interpersonal qualities and professional skills of the supervising therapist were considered as important to the success of the programme as the content of the programme itself. p.7. However, their greatest concern was losing the ongoing support of the physiotherapist would undermine their motivation to exercise, and they expressed a desire for ongoing support. pp.8‐9. |
|
| Larmer 2014b; Larmer 2014a | "She's so enthusiastic and she's pleased to see us every day, whether she feels like she is or not. She's always very welcoming and um yeah, very encouraging and you can ask her things all the time." p. 91. | The importance of good 'therapist/instructor' interaction was noted. The instructor helped create an enjoyable and supportive atmosphere, which appeared crucial for many participants. p.91. | |
| Moody 2012 | "…umm the instructor we had was very, very good and ah I think it was just so good. And I think the motivation was there which is the big thing is to get you motivated you know?" p.66. "jolly you along." p.66. "Yes, I think the instructor was sort of aware of our capabilities and kept the challenge up. And it made it more interesting that way, because if you did the same thing over and over at the same level, it would be boring." p.66. "Yeah, so it's just funny little things that keep you thinking you have a responsibility to attend 'cause someone's gonna miss you." p.66. "No, I'd sooner have a leader." p.66. |
The instructor was important and group members considered essential attributes of an instructor were: being understanding, tolerant, friendly and someone who will "jolly you along." The participants valued their relationship with a challenging instructor with whom they could establish a connection. It emerged that accountability was an important factor in motivation. Participants felt if they missed a class the instructor or group would notice, and this helped keep them motivated to go. The fact that there was a record of attendance being kept also contributed towards this. Participants were cognisant of the instructor watching them and noticing if they were doing exercises incorrectly, that he/she would playfully encourage them to challenge themselves and they wanted to do well for the instructor. All these factors contributed to the feeling of accountability, and were strong motivators to attend the classes. A number of questions as to how a water‐based exercise programme could continue to run, especially if funding for it was limited, were discussed. One question was the use of a 'buddy' system, where people would be paired up and go to the pool with their friend to do the exercises together. However, most participants were unenthusiastic about this idea as they would rather attend in a group with an instructor and did not want to rely on one person to go with. It was asked if groups could run with a short‐term instructor for a few weeks to demonstrate the exercises, with the groups then becoming self‐sufficient. Reactions to this idea were mixed. Some felt this would work, as long as it was a structured group with a set time and place to meet. However, most participants felt that an instructor was essential and that a class without an instructor would fall apart; that they were too forgetful to remember the exercises without an instructor there to tell them or that there would not be sufficient motivation. It was considered embarrassing to go without an instructor and some felt it would not be safe exercising without an instructor to guide them. A few participants had continued with the water exercises on their own since the classes had finished, and had found it difficult to maintain. Nominating a leader from the group to be the instructor was suggested and some participants liked this idea but other people felt this would not be fair on the nominated instructor. The instructor was important and group members. |
|
| Petursdottir 2010 | "I think that physical therapists are the best to help those who have a physical dilemma to start exercising…and start carefully, and under supervision. I think that is very important." p.1020. "Well, I always say that my physical therapist is as good as any psychologist." p.1021. "What keeps me going now is attending physical therapy sessions." p.1021. |
The participants described the importance of suitable exercise and their experience of how exercise should progress gradually under the supervision of a qualified person. p.1020. All participants had some experience with physical therapists, most of it positive, and many participants placed emphasis on the fact that the encouragement and understanding they received from their physical therapists were very important. The importance of listening and good communication was highlighted and seemed to play a big role in the perceived benefits of physical therapy. p.1021. 4 participants exercised under the supervision of a physical therapist at the time of the interviews. These participants described how the physical therapists kept them going and that the therapists were sometimes the key to going on. p.1021. |
|
| Thorstensson 2006 | "It is something you notice when you give it up, since it [the exercise] was very difficult to do on your own…As there was nobody to supervise me it was easy to deteriorate again…Then there was nobody to urge you on." "I think that [an instructor] is good because then you learn what to do so that you do not do it in the wrong way. Otherwise you might do certain movements incorrectly and put too much pressure on your knees." p.55. |
To receive guidance: this conception concerned the perceived need for moral support, encouragement and instructions on how to exercise. The statements were about compliance and the anxiety of doing something wrong. | |
| Larmer 2014b; Larmer 2014a | "The physiotherapist determined the gradual increase of the exercises; he told me, for example, to increase the exercises by five minutes. I liked it that he told me what to do, nevertheless, he was my physiotherapist." p.275. The approach of the physiotherapist was very democratic, which I appreciated. Together, we discussed the activities and the increase of the activities. I could indicate to what extent I wanted to increase the activities, to what extent I could maintain the exercises. p.276. |
Some participants reported that they were actively involved in choosing the activities, in gradually increasing these activities, and in using the performance charts. In contrast, other participants reported that the main decisions were taken by the physiotherapist and that they performed the activities as instructed by the physiotherapist. It appeared that all adherent participants reported that they were actively involved in the whole process and that the physiotherapists had a coaching role during intervention. However, most non‐adherent participants reported that the physiotherapist made all decisions (which was sometimes a deliberate choice of the participants). Therefore, it seems that active involvement of the participant facilitates adherence to exercises and activities. p.275. |
Social and environmental
| Subtheme | Study | Direct participant data | Author description of data |
| Prioritising exercise | Campbell 2001 | Alan: "It wasn't so much at home I am able to do it, it's more at work…Perhaps not as often as I would really like to, but I can do it quite freely then, because I'm totally on my own." Kenneth: "So many things happening…The boys used to come in from school or work…people come and see [wife] and ugh…I'm out twice at least a week to band practice and I have two engagements as well." p.134. Eileen: "Weekends I try to do [the exercises] but I am very busy on the weekend really it is the only chance I get to do sort of any cleaning. Then my family usually come up in the afternoon, my sister and her husband, because on the way to Mum's they always come in. Sunday's I have Mum on Sunday see, then I have her two sisters because they are older." p.134. Kenneth: "It's just excuses when it comes down to basics. I mean you know you could get up in the morning and do it between 6 or 7 or something like that." p.134. Geoffrey: "There was a time when I missed one [session with the physiotherapist]. I don't know why…I think it was taking the wife somewhere I don't know and I must honestly admit that her needs come as a priority as far as I am concerned." p.135. |
While a positive disposition towards exercise could increase motivation, more important was the willingness and ability to accommodate the exercises into everyday life. People who ceased exercising often cited conflict with regular routines to explain why continuing with exercises was not possible. By giving these explanations, 2 participants could have been trying to portray themselves in a favourable light by indicating that their non‐compliance was due to family commitments and obligations. Nevertheless, later in their interviews, both went on to admit some personal responsibility for their lack of compliance. For example, 1 participant indicated that non‐compliance resulted from a combination of a busy life and a reduced commitment to the physiotherapy. 1 participant, who was only partially compliant even during the time he was seeing the physiotherapist, recalled in his interview that he had missed 1 of the sessions with the physiotherapist because, not unreasonably, he always put the needs of his wife, who had a progressive and debilitating disease, before his own needs. p.135. |
| Hendry 2006 | "…I try and say, 'OK well I'll go there [gym], have a shower and go shopping'. I also work in a charity shop on a Saturday so I can go before I go there you know…I try to fit it in." p.563. I try to fit exercise into my weekly routine. (25) I'm on a gym referral scheme, so I have a set time to go and that helps. p.562. I do my exercises when I remember but when I'm busy I forget. (15, 11) I don't have enough self‐discipline to make me exercise regularly. (11) Finding the time to go to the gym is a problem. p.562. |
Prioritising exercise and making it part of a weekly routine helped some people to maintain their exercise habit. For other people finding time to exercise was a low priority; some because they did not consider exercise to be important or appropriate, while other people freely admitted to being lazy or lacking motivation. | |
| Hinman 2016 | "It's part of life…I get up in the morning, I have a cup of coffee, I take my blood pressure medication, then I go and do my exercises…and I don't have to leave home!" p.486. | The structured programme enabled people with knee OA to incorporate the prescribed exercises into their daily schedules. p. 483. | |
| Hurley 2010 | "…I do the exercises upstairs when I get up in the morning…I find I might have a bit more time, because during the day you tend to let things slide." | ‐ | |
| Moody 2012 | No data reported. | There was much discussion surrounding all aspects around the timing of the classes (time of day, frequency, regularity, which days of the week, how many days a week, duration of class, duration of programme, continuity, time of year/season) and no consensus was reached. This discussion mostly hinged around tiredness, illness and business. Some people felt they could not manage twice a week as they got tired or were too busy, while other people would prefer the classes to be more frequent, for example, 3 times a week or more to derive more health benefits. p.67. | |
| Morden 2011 | "My job's very important, really important at the moment. Not only for the money but for myself as well because when my husband died, I just had to get busy. I just like being busy." p.196. | Some people had ceased to exercise and this was due to differing priorities. In some cases, they worked or had familial obligations like child minding or carer duties to fulfil. The way that participants made priorities in their life was not a linear process. For example, spending a lot of time working was not just related to needing money. Rather, making priorities of how time was spent formed part of the ongoing 'back story' of participant's lives. 1 woman who had talked about her longstanding love of walking and the benefits of it for easing her knee pain outlined how she had chosen to do more hours at work to help her cope with the loss of her husband. The amount of time she spent in work then impacted upon the amount of time available to go walking. Knee pain was not the main priority. Often, the activities that people engaged in are related to psychological and social well‐being. It is not to say that some participants had lost the motivation to exercise in some cases. 1 participant had access to gym facilities as part of his job, but when he left that position he lost that benefit. As a result, he described how he had fallen out of the 'habit.' pp.195‐196. | |
| Thorstensson 2006 | "One is so occupied that it is very easy not to find time for exercise. Everything else takes precedence." | To devote time. This conception included different aspects of time as essential for the effectiveness of the exercise. The statements concerned time as the most appropriate time point during disease course when first starting to exercise, and having adequate time to exercise. pp.55‐6. |
| Subtheme | Study | Direct participant data | Author description of data |
| Support of friends and family | Campbell 2001 | Stanley: "If perhaps my wife would work with me and you had a bit of competition, but I feel such a fool standing on one leg and going up and down on my own and I tends to drop it I do. I'm not very strong disciplined on that, no. I know some people can be so, but not me. I suppose if there was a really good reason I would." | 1 participant stopped the exercises because it was difficult to do them alone and, as he had not noticed much improvement in his symptoms, there did not seem to be a strong rationale for continuing. |
| Fisken 2016 | "You know, you're not stuck at home all the time, it's a way of getting out." "It's nice to be out in a group and not feel so isolated so it was a good, psychological it was, really good." "I think it's important to be with other people, how other people cope and that you're not alone and there are other people you know, in similar situations." p.15. |
‐ | |
| Petursdottir 2010 | "Yes, my wife, naturally, she encourages me." "It [the experience of lack of support] was, just, what should I say, totally pathetic…. I guess men are not all equally understanding." p.2020. |
The support, caring and encouragement of other people were among important external factors influencing how much the participants exercised. Most of the participants seemed to feel the need for such encouragement. Yet, when talking about the family's attitudes toward the disease and the importance of exercise, some of the women expressed having a hard time justifying to themselves and their families their need to spend time exercising. | |
| Stone 2015 | "One of my friends who knows about my arthritis asked me if I ever exercise." "Exercise?!" I said, "What could I do with exercise?!" Then she said she would work out with me if I wanted to. That was the first time I ever seriously thought about exercising." pp.15‐16. "I know [my husband] supports being active, but I never really felt overly supported until my youngest asked if she could come with me on walks. The shocking interest in my exercise habits motivated me to want to exercise more, and be a great role model." p.16. |
Participants expressed feeling facilitated toward physical activity adoption with high levels of social support stemming from their family and friends. p.15. Other participants contemplated physical activity if they had support from their family members. More specifically, spouses and children were cited as being the most important family members in facilitating physical activity adoption. p.16. |
| Subtheme | Study | Direct participant data | Author description of data |
| Social identity | Hendry 2006 | "They're (gyms) mostly young people that go to those aren't they? I think I'd feel out of place…They don't want to be dragged down by somebody that's not up to their standard I would think." p.563. "I imagined…all these fit people you know, bodies like Adonis…I thought that I would be old, that I would show myself up, but in fact it wasn't like that at all…the people who were sort of totally 100% fit were very few and far between." p.563. "I imagined the people at the gym would all be young and fit and that I would feel out of place but it wasn't like that at all." "The gym is safer for women than going out walking alone." |
Data not reported. |
| Fisken 2016 | "I would love to see something for the elderly people, to be active and keep reasonably fit. There's very little around for the older people. They don't want to know the older people." "It's got to be paced at our age range." "They need to have something for the older people, keep the younger ones different." "Well I think it's important that you go, even if it's on land, that you go with people relative to your own age and that you're all at the same level 'cause I mean if you go with a 30‐year old…we can't keep up with that, as much as we'd like to. Whereas if you go and you're all this age, you encourage each other." p.14. |
1 of the primary reasons given for discontinuing an aqua‐based exercise programme was that participants felt the class they had attended was not suitable for their age…Participants in the study felt strongly that they should be attending classes suitable for their age. p.14. Training with people of a comparable age was also considered important in the study. Similarly, older adults who performed land‐based resistance training identified this as an important facilitator for exercise. Attending age or ability (or both) appropriate classes may have increased adherence to aqua‐based exercise among participants in the study. p.15. |
| Subtheme | Study | Direct participant data | Author description of data |
| Exercise facilities | Hendry 2006 | "I'm happy to go to the gym." "I'd be too embarrassed to go to a gym." "I would go to a gym if my doctor referred me." "The bikes at the gym are easier to use and safer than cycling in traffic." p.562. "I prefer to do outdoor exercise like cycling or walking." p.562. "I would rather do exercises at home." p.562. "I wasn't keen on doing things on the machines 'cause I think that they're so boring." p.562. |
The location of exercise was important. Some people preferred exercising at home; other people preferred outdoors. Some people who had tried exercising at a gym did not enjoy it. Gyms were sometimes viewed as inappropriate places. Other people found by experience that this was not the case. pp.563‐4. |
| Larmer 2014b; Larmer 2014a | "In the break in the summer time, I've gone to the normal pool…and tried to do my exercises there…you're less stiff after you come out, shall we say, than before you went in, but you don't get the same kind of pain relief as from the heated water." p.91. "After about 20 minutes in that temperature of the normal public pools, you tend to get cramp…So the water there, isn't warm enough really for arthritic people." p.91. |
Participants also discussed the importance of the warm water to exercise in, helping to relax muscles and easing pain, a benefit they did not gain from public pools…And importantly for some people, being in a normal (cooler) pool gave them extra symptoms. p.91. | |
| Fisken 2016 | "I suppose one of the reasons why I did stop is because it's coming up to winter and it's outside…and it's cold…I would like to go to a class in a hotter pool." "Very cold, I found that a real downside." "At [the pool I attended] that was the worst…coming out you were freezing cold and you have to get changed back again." "The water wasn't warm enough for me, this was a class at about 5 o'clock, the other thing was where I went you parked your car and you had to take quite a big walk to the actual pool and then after a few weeks when it was getting towards winter it would be dark when you came out and I didn't feel it was very safe. I'm not sure about the security round there." "Then I ran out of money basically…it's very expensive, to belong to a gym club." "I mean some of them charge an awful lot to get in. When you go up to the pool it's $2 and then you get charged $5 to go into the aerobics, well that's really, sort of, you know, pay for the guys time, that person's time but when you're on a pension you haven't got that." "The cost, when you're on a limited budget." "When I was in [name of pool] I stopped going because I got chlorine burns on my skin, from here (indicated chest level) right up." "That's right, it was like weeping eczema and the arthritis society was so worried because I was going to one of their classes at the beginning and they said that they wanted to take it further and of course I became allergic to a lot of the minerals that are added to the [name of pool]." p.14. |
2 weaker environmental themes that emerged were cost and skin reaction to the pool water. Several participants in the study felt that cost was a barrier to continued participation in aqua‐based exercise and this applied regardless of whether they had attended a private or public facility. Not surprisingly, socioeconomic status would appear to be a major factor in whether or not cost is perceived as a barrier to activities like aqua‐based exercise. Skin reaction to the pool water was described by 2 participants in the study. p.15. |
|
| Moody 2012 | "…couldn't probably afford a big amount, twice a week." | The location of the water‐based exercise classes (a large indoor aquatic centre pool) was discussed, as well as other potential locations (the warm therapeutic community pool, local school pools, the community salt water pool and other smaller community pools). Participants weighed up the pros and cons of the various pools and opinion differed on the ideal location for the classes. p.67. The next discussion centred on which community pool to use. While a few people thought that using local smaller community or school pools would increase accessibility and reduce transportation issues, the suitability of these pools, particularly the depth and width, was questioned. Furthermore, these pools did not regularly have lifeguards in attendance and thus there were safety concerns. Most people liked the large, centrally located medium‐depth pool the classes were held in even though it was "very public" and busy. An added bonus to the latter pool was the spa pool which some participants used at the end of each class. p.67. Money (e.g. cost, funding, payment, expense, price, discounts) and who pays or contributes was discussed extensively. While grateful for the free classes, participants were realistic in understanding that this could not continue. The majority of participants said they would not mind contributing a small amount of money towards pool entry or the cost of the classes. Some participants were confident that alternative funding could be sourced, and thought that personal contributions may not be necessary allowing the classes to continue to be run free of charge. Ideas of how the classes could continue were discussed. Alternative sources of funding was discussed, such as from local charitable organisations concerned with assisting older adults or perhaps the pool itself would provide discounted or free entry for these classes. The majority of participants said they would not mind contributing a small amount toward pool entry or to the running of the classes. However, some participants stated they were on their pension and that it was a great motivation to have the classes for free. p.68. |
|
| Petursdottir 2010 | If I was a boy or a man, I would kick those machines; I hate adjusting them, it takes half the time." "And this costs money. Walking, however, is free. Such things matter when you only have your pension." p.2021. |
Sometimes, the accessibility of training facilities was poor and the equipment not user‐friendly. When walking outside, the lack of benches was mentioned as a barrier. The cost of exercising indoors (e.g. using a gym) was a barrier for those participants with low income. p.2021. |
|
| Thorstensson 2006 | "It has to be close at hand, one should not have to travel long distances. It would never work for me, if I had to travel to a rehabilitation centre every day. I don't think so." p.55. "But it [the exercise] should be done in an appropriate manner." p.55. |
To have structure. This conception contained statements about accessibility as a prerequisite for exercise, and the importance of quality of exercise, concerning both purpose with and type of exercise. p.55. | |
| GP: general practitioner; OA: osteoarthritis. | |||
Appendix 5. Contribution of each study to the themes arising from the qualitative synthesis
| Themes from the qualitative synthesis (number of studies) | Campbell 2001 | Fisken 2016 | Hendry 2006 | Hinman 2016 | Hurley 2010 | Larmer 2014b; Larmer 2014a | Moody 2012 | Morden 2011 | Petursdottir 2010 | Stone 2015 | Thorstensson 2006 | Veenhof 2006 |
| Symptoms | ||||||||||||
| Pain and physical function (6) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ‐ | ✔ | ✔ | ✔ | ‐ | ‐ |
| Capacity to exercise (6) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ |
| Impact of exercise on the effects of OA (10) | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ |
| Health beliefs and views on the management of OA | ||||||||||||
| Aetiology and prognosis of OA (4) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Non‐exercise management strategies (3) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Advice and information from health professionals (6) | ✔ | ‐ | ✔ | ✔ | ✔ | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ |
| Health beliefs and managing OA and exercise (6) | ✔ | ‐ | ✔ | ✔ | ✔ | ‐ | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ |
| Everyday activities (physical activity) versus structured exercise (4) | ‐ | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ |
| Psychological factors | ||||||||||||
| Impact of OA on people's sense of "self" (4) | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ | ‐ |
| Individual disposition (2) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ |
| Psychological benefits of exercise (8) | ‐ | ✔ | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ | ✔ | ‐ | ✔ | ‐ |
| Influence of programme supervisors (9) | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ | ✔ | ‐ | ✔ | ‐ | ✔ | ✔ |
| Social and environmental factors | ||||||||||||
| Prioritising exercise (7) | ✔ | ‐ | ✔ | ✔ | ✔ | ‐ | ✔ | ✔ | ‐ | ‐ | ✔ | ‐ |
| The support of family and friends (4) | ✔ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ |
| Social identity (2) | ‐ | ✔ | ‐ | ‐ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Exercise facilities (6) | ‐ | ✔ | ✔ | ‐ | ‐ | ✔ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ |
| OA: osteoarthritis. | ||||||||||||
Data and analyses
Comparison 1.
Exercise versus control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 19 | 2144 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.28, ‐0.11] |
| 1.1 WOMAC pain | 9 | 1058 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.46, ‐0.21] |
| 1.2 Other pain outcomes | 10 | 1086 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.19, 0.05] |
| 2 Physical function | 13 | 1599 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.37, ‐0.17] |
| 3 Self‐efficacy (SE) | 11 | 1138 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.46 [0.34, 0.58] |
| 3.1 Six‐minute walk SE | 1 | 115 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.05, 0.83] |
| 3.2 Lorig SE exercise scale | 2 | 168 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.63, 1.27] |
| 3.3 ExBeliefs SE | 1 | 338 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [0.20, 0.66] |
| 3.4 Arthritis SE scale | 1 | 54 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.42, 0.72] |
| 3.5 McAuley SE exercise scale | 1 | 21 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.04, 1.87] |
| 3.6 VAP SE | 1 | 52 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.70, 0.39] |
| 3.7 Arthritis SE scale ‐ pain | 1 | 120 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.04, 0.69] |
| 3.8 SE Score | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.71 [0.07, 1.35] |
| 3.9 ASES pain | 2 | 230 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.11, 0.63] |
| 4 Depression | 7 | 876 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.29, ‐0.02] |
| 4.1 Kim | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.88 [‐1.37, ‐0.39] |
| 4.2 Other studies | 6 | 806 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.24, 0.05] |
| 5 Anxiety | 4 | 704 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.26, 0.05] |
| 6 Stress | 2 | 206 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐7.57, ‐1.95] |
| 7 SF‐36 mental health | 5 | 576 | Mean Difference (IV, Fixed, 95% CI) | 5.07 [2.43, 7.72] |
| 7.1 Aglamis study | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 32.9 [23.07, 42.73] |
| 7.2 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 2.90 [0.15, 5.65] |
| 8 SF‐36 emotional role | 5 | 576 | Mean Difference (IV, Random, 95% CI) | 11.43 [‐4.06, 26.91] |
| 8.1 Aglamis | 1 | 25 | Mean Difference (IV, Random, 95% CI) | 72.8 [47.14, 98.46] |
| 8.2 Other studies | 4 | 551 | Mean Difference (IV, Random, 95% CI) | 1.76 [‐6.63, 10.14] |
| 9 SF‐36 social function | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| 9.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| 10 SF‐36 vitality | 5 | 1158 | Mean Difference (IV, Fixed, 95% CI) | 6.06 [3.57, 8.54] |
| 10.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 51.9 [34.74, 69.06] |
| 10.2 Other studies | 4 | 582 | Mean Difference (IV, Fixed, 95% CI) | 3.90 [0.55, 7.25] |
| 10.3 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 6.58 [2.78, 10.38] |
| 11 Sleep | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐2.54, 0.34] |
Differences between protocol and review
The original protocol differed from the review with regard to the variables in the inclusion criteria. In the protocol, quantitative criteria were that studies must have measured pain, function, self‐efficacy or depression (major outcomes) with anxiety, quality of life and adverse effects of exercise listed as minor outcomes. In the review, it was stipulated that studies should either have measured pain or function and at least one psychosocial outcome (self‐efficacy, depression, anxiety or quality of life): therefore, pain and function were major outcomes in the review. Five trials used the 36‐item Short Form (SF‐36) measure of health‐related quality of life and the SF‐36 social function and mental health outcomes have been incorporated to reflect changes to quality of life. Insufficient information on adverse effects was provided in the studies to include it as a measure in the review.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: OA of knee meeting ACR radiographic grade II, III or IV criteria; aged 50‐69 years; judged to be engaged in independent in daily activity. Exclusion criteria: use of intra‐articular injections in the last 6 months; involved in regular physical activity and physiotherapy, using assistive equipment, unable to exercise, diagnosed with a chronic condition, or a combination of these. Country: Turkey. Sample number: IG: 16; CG: 9. Mean age: 57 years. 100% women. |
|
| Interventions |
Provider(s): fitness trainer and health technician. Training: yes. Setting: not stated. Content: multicomponent: strength/resistance + aerobic + patient information. Length/intensity: 3 sessions a week for 12 weeks. Control: waiting list. |
|
| Outcomes | At 12 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | Low risk | Managed externally to the project. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported. However, participants and providers unlikely to be blinded to exercise intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessments. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition: IG: 5.8% (1/17); CG: 35.7% (5/14). Lost to follow‐up: IG: 1 reactive arthritis; CG: 2 change of city; 1 low back pain; 1 intra‐articular injection; 1 no contact. ITT/intervention received not reported. Note that there was a higher rate of attrition in the CG, increasing risk, and that some instances may relate to lack of intervention. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: radiographic evidence of knee OA (defined as the presence of osteophytes in the tibiofemoral compartment or the patellofemoral compartment (or both), as assessed on standing anterior/posterior and lateral views), aged 55+ years, BMI ≤ 40 kg/m2; pain on more than half the days of the past month during at least 1 of the following activities; walking, going up or down stairs, standing upright or in bed at night. Exclusion criteria: medical condition that prohibited people from participating safely in an exercise programme, diagnosed with inflammatory arthritis, experience of an exercise programme in the past 6 months (e.g. strength training or > 20 minutes of aerobic activity twice a week, or both). Country: US. Sample number: IG: 22; CG: 22. Mean age: 68 years. Progress Plus: 83% women. |
|
| Interventions |
Provider(s): not stated. Training: yes. Setting: home. Content: progressive strength training programme Length/intensity: 3 times a week for 16 weeks. Control: attention control; home visits, nutrition education. |
|
| Outcomes | At 16 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment by biostatistician. |
| Allocation concealment (selection bias) | Low risk | Allocation concealed from the technician and physician collecting the data. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Authors reported that participants were blinded to the 'active' intervention. However, no further details provided regarding how this was achieved. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessor not blinded to participant's group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IG: 17% (4/22); CG: 13.6% (3/22). Lost to follow‐up reported: IG: 1 severe neck arthritis; 1 prior back injury; 2 lack of time; CG: 2 severe intercurrent illness; 1 diagnostic of psoriatic arthritis. No differences in baseline characteristics of the 8 participants who withdrew when compared to participants who completed trial. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised, placebo‐controlled, participant‐ and assessor‐blinded trial. | |
| Participants |
Inclusion criteria: aged ≥ 50 years, hip OA fulfilling ACR classification criteria, pain in groin/hip for > 3 months, mean pain intensity in past week of ≥ 40 on 100 mm VAS, at least moderate difficulty with daily activities. Exclusion criteria: hip or knee joint replacements or both; planned lower limb surgery, physical therapy, chiropractic treatment or prescribed exercises for hip, lumbar spine or both in the past 6 months; walking continuously > 30 minutes daily; regular structured exercise more than once weekly. Sample size: 102; 96 completed intervention, 83 completed follow‐up. IG (n = 49): mean age 64.5 years; CG (n = 53): mean age 62.7 years. Country: Australia. |
|
| Interventions |
Providers: 8 physical therapists with ≥ 5 years of clinical experience and postgraduate qualifications. Training: yes. Setting: private clinic. Content: semi‐standardised exercises with core components and exercises depending on assessment. Participants given manual therapy techniques and 4‐6 home exercises to perform 4 times a week including strengthening, flexibility and balance exercises. Length/intensity: 10 individual treatment sessions over 12 weeks: 2 sessions in week 1, then once weekly for 6 weeks, then approximately once per fortnight. First 2 sessions were 45‐60 minutes, subsequent sessions were 30 minutes. Control: sham intervention of inactive ultrasound and inert gel applied to hip. No exercise or manual therapy instructions. During follow‐up phases, participants asked to apply gel for 5 minutes 3 times a week. |
|
| Outcomes |
Musculoskeletal impairments and functional performance tests at baseline and week 13:
Outcomes at 13 and 36 weeks: Primary:
Secondary:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table, results placed in sealed envelopes by independent person. |
| Allocation concealment (selection bias) | Low risk | Opened by another independent person 1 by 1, shortly before the next participant attended, and allocation result emailed to non‐blinded therapist. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | IG delivered by non‐blinded therapist: authors acknowledged non‐blinding of therapists was a weakness. Blinding of participants was low risk: checked with James test. Participants informed that the comparison was between physical intervention and sham physical therapy intervention but not what either consisted of. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor and biostatistician blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: 6 (5.9%) completed did not complete the intervention in both groups and 19 (18.6%) did not complete follow‐up. |
| Selective reporting (reporting bias) | Low risk | Results reported for all measures. |
| Other bias | Low risk | |
| Methods | Assessor‐blinded, 3‐arm randomised controlled trial. | |
| Participants |
Inclusion criteria: aged > 50 years, knee OA fulfilling ACR criteria, and at least moderate difficulty with daily activities (WOMAC). Exclusion criteria: "systemic arthritic conditions such as rheumatoid arthritis; medical condition precluding safe exercise such as uncontrolled hypertension or heart condition; self‐reported history of serious mental illness, such as schizophrenia, or self‐reported diagnosis of current clinical depression; neurological condition such as Parkinson's disease, multiple sclerosis or stroke; knee surgery including arthroscopy within the past 6 months or total joint replacement; awaiting or planning any back or lower limb surgery within the next 12 months; current or past (within 3 months) oral or intra‐articular corticosteroid use; physiotherapy, chiropractic or acupuncture treatment or exercises specifically for the knee within the past 6 months; walking exercise for >30 minutes continuously daily; participating in a regular (more than twice a week) structured or supervised (or both) exercise programme such as attending exercise classes in a gym or use of a personal trainer; participating in or previous participation in a formal PCST programme; inability to walk unaided; inadequate written and spoken English; inability to comply with the study protocol such as inability to attend physical therapy sessions or attend assessment appointments at the University." Sample size: 222. Exercise group: 75; mean age: 62.7 years (SD 7.9); 44 women; median symptom duration 6 years. Education group: 74; mean age: 63.0 years (SD 7.9); 45 women; median symptom duration 5.5 years. Combined intervention: 73; mean age 64.6 years (SD 8.3); 44 women; median symptom duration 5.5 years. Country: Australia. |
|
| Interventions |
Providers: physical therapists, with 11 therapists delivering education and education/exercise treatments and 11 therapists delivering exercise treatments. Training: yes. Setting: private practice. Content: CG: education only (pain education and cognitive and behavioural pain coping skills; exercise only group: 6 exercises to strengthen quadriceps, hamstrings, and hip abductor muscles; exercise + education group. Length/intensity: 10 treatments over 12 weeks + home programme. |
|
| Outcomes | Outcomes at 12, 32 and 52 weeks: Primary outcomes:
Secondary outcomes:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table used for allocations, which were sealed in an envelope by an independent person. |
| Allocation concealment (selection bias) | Low risk | Envelopes opened by another independent person who emailed the therapist shortly before the next participant attended. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists not blinded. Participants blinded to study hypotheses but not to intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up from 222 participants: 21 at 12 weeks (9.5%), 41 (27.9%) at 32 weeks and 36 (44.1%) at 52 weeks. |
| Selective reporting (reporting bias) | Low risk | Results reported for all variables. |
| Other bias | Low risk | |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: symptomatic knee OA for ≥ 6 months, no previous yoga training, no current participation in a supervised exercise programme. Exclusion criteria: score < 8 on Short Portable Mental Status Questionnaire; symptoms of joint locking; use of knee brace, walking stick, walker or wheelchair; corticosteroid injection in symptomatic joint within 3 months or hyaluronic acid injection within 6 months of study entry; knee surgery in previous 2 years; joint replacement; self‐reported hypertension; heart condition or other condition with symptoms overlapping with OA. Sample: 36 community‐dwelling women, mean age 72 years, 18 allocated to IG and 18 to CG, 1 participant withdrew from each group. Country: US. |
|
| Interventions |
Providers: programme developed by 5 certified/registered yoga teachers specifically for older adults with knee OA. All classes taught by same yoga teacher. Training: no specific training, but teacher had 10 years' experience. Setting: small classes (9 participants per class). Content: Hatha yoga. Length/intensity: 1 × 60‐minute class a week for 8 weeks, and instructed to practice for 30 minutes 4 times a week at home using printed instructions. Control: wait‐list control. |
|
| Outcomes | Outcomes at baseline; 4, 8 and 20 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random list of numbers from 1 to 36, allocated in the order of enrolment. An even computer‐generated number denoted allocation to the CG and an odd number to the IG. |
| Allocation concealment (selection bias) | Low risk | Allocation carried out blinded. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants in wait list control, so no blinding. Low risk for personnel: research assistant enrolling participants and collecting outcome data blinded to group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research assistant enrolling participants and collecting outcome data blinded to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IG: 1 (5.6%); CG: 1 (5.6%). |
| Selective reporting (reporting bias) | Low risk | Results for all variables measured reported. |
| Other bias | Low risk | |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: aged 40‐80 years, with radiographically verified minimum joint space (< 4 mm for participants aged < 70 years and < 3 mm for participants aged > 70 years), and a Harris Hip Score 60‐95 points. Exclusion criteria: total hip replacement in the index joint, diagnosed with knee OA or had knee or lower back pain, rheumatoid arthritis, osteoporosis, cancer, cardiovascular disease, dysfunction in lower extremities due to accident or disease, were pregnant, could not participate in exercise, who could not communicate in Norwegian. Sample number: IG: 54; CG: 54. Country: Norway. Mean age: 58 years. Progress‐plus: 56% women; 78.2% > 12 years; 63.6% employed, 20% retired, 14.5%sick‐leave. |
|
| Interventions |
Provider(s): physical therapist. Training: yes. Setting: healthcare site. Content: strength/resistance + participant education. Length/intensity: 2‐3 times a week for 12 weeks. Control: attention control: patient education. |
|
| Outcomes | At 16 months:
|
|
| Notes | Included participant education a 'Hip school' comprising of 3 group‐based sessions and 1 individual physical therapy visit, 2 months after completing the group sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using computer‐generated, blocked schedule, administered through numbered, opaque, sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants or providers were blind to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors blinded to group allocation throughout trial and analysis period. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | IG=23.6% attrition (13/55) CG=33% attrition (18/54) Lost to follow‐up: IG: 6 'total hip replacement' surgery; 7 did not respond; CG: 1 'total hip replacement' surgery; 7 did not respond. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed randomised controlled trial. | |
| Participants |
Inclusion criteria: radiographic evidence of tibiofemoral OA as determined by a single observer on the basis of weight‐bearing anteroposterior radiographs; aged > 60 years,; BMI > 28; engaging in < 20 minutes formal exercise a week; difficulty with ≥ 1 of the following activities due to knee pain: walking 0.25 miles, climbing stairs, bending, stooping, kneeling, shopping, house cleaning, getting in or out of bed, standing up from a chair, lifting and carrying groceries, or getting in or out of a bathtub; willingness to undergo testing and intervention procedures. Exclusion criteria: medical condition that precluded safe participation in an exercise programme, mental score < 28; inability to complete the 18‐month study or unlikely to be compliant; inability to walk without a walking stick or other assistive device; participation in another research study; excessive alcohol consumption; or inability to complete the trial protocol, in the opinion of the clinical staff, because of frailty, illness or other reasons. Country: USA. Sample number: IGa: 76; IGb: 80; CG: 78. Mean age: 69 years Progress Plus: 74% women, 22% non‐white, 88% post 16 or higher education (e.g. vocational/college); Income: 19% < USD15,000; 33% USD15,000‐USD35,000; 23% USD35,000‐USD50,000; 26% > USD50,000. |
|
| Interventions |
Provider(s): not stated. Training: yes. Setting: facility and home. Length/intensity: 3 times a week for 18 months. Intervention content: IGa: exercise (strength/resistance/aerobic) and diet; IGb: exercise (strength/resistance/aerobic). Control: attention control; healthy lifestyle education. |
|
| Outcomes | At 18 months:
|
|
| Notes | There are 2 Focht 2005 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation stratified by race. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not clear and unlikely that participants or providers were aware of group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of staff to the treatment assignment of the participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IGa: 23.7% (18/76); IGb: 20% (16/80); CG: 14% (11/78). Reasons for withdrawal not specified. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: aged 59‐85 years, diagnosed with hip or knee OA using the ACR criteria and living current and chronic (>1 year) hip or knee pain hip or knee pain. Exclusion criteria: involved in recreational physical activity more than twice a week; inability to walk indoors without a walking aide; unstable cardiac conditions or severe pulmonary disease; incontinence, fear of water or uncontrolled epilepsy; low back pain referred to the lower limbs; joint replacement surgery in previous year; arthroscopic surgery or intra‐articular injections within previous 3 months; and current participation in Tai Chi or hydrotherapy. Country: Australia. Sample number: IG: 56; CG: 41. Mean age: 70 years. Progress Plus: 68% women. |
|
| Interventions |
Provider(s): qualified Tai Chi Master. Training: yes. Setting: not stated. Content: 24 forms from the Sun style of Tai Chi and 10‐minute warm‐up session. Length/intensity: 1 session a week for 12 weeks. Control: waiting list. |
|
| Outcomes | At 12 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule, in blocks of 30. |
| Allocation concealment (selection bias) | Low risk | Concealed in an offsite location. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Authors stated that trial involved a physical intervention, therefore participants were not blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IG: 7.1% (4/56); CG: 0% (0/43). Lost to follow‐up: IG: 3 withdrew and 1 had knee surgery. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed randomised controlled trial. | |
| Participants |
Inclusion criteria: subjective complaint of hip pain with either 1. (a) hip internal rotation < 15° and hip flexion < 115° or (b) > 15° hip internal rotation and pain on hip internal rotation, morning stiffness ≤ 60 minutes, aged > 50 years. 2. Aged 40‐80 years except in (b) above (aged > 50 years). 3. Radiological evidence of OA (2 of the following 3 criteria): osteophytes, joint space narrowing, ESR < 20 mm/hour (ACR Criteria for the Classification and Reporting of Osteoarthritis of the Hip) (Altman 1991). Exclusion criteria: previous hip arthroplasty, history of congenital/adolescent hip disease; clinical signs of lumbar spine disease; physiotherapy in previous 6 months; pregnancy; hip fracture; contraindications to exercise therapy (unstable angina/blood pressure, myocardial infarction in past 3 months, cardiomyopathy, uncontrolled metabolic disease, recent ECG changes, advanced respiratory disease, third‐degree heart block) (AGS 2001); on waiting list for joint replacement within the next 27 weeks; rheumatic diseases (e.g. rheumatoid arthritis, ankylosing spondylitis); intra‐articular hip corticosteroid injection in previous 30 days; insufficient English language to complete questionnaires. Country: Ireland. Sample number: IGa: 43; IGb: 45; CG: 43. Mean age: 61 years. Progress Plus: 61% women, 24% retired, 30% homemaker, 35% employed, 9% other. |
|
| Interventions |
Provider(s): senior grade or clinical specialist physiotherapists. Training: yes. Setting: hospital and home. Intervention content: IGa: multicomponent: strength/resistance and manual therapy + patient information; IGb: strength/resistance + patient information no manual therapy. Length/intensity: 8 sessions over 8 weeks. Control: wait list. |
|
| Outcomes | At 9 weeks:
|
|
| Notes | There are 2 French 2013 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomisation number table devised in Microsoft Excel 2003. |
| Allocation concealment (selection bias) | Low risk | Group allocation by external research. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Authors stated that blinding not viable in a non‐pharmacological trial. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding undertaken. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IGa: 7% (3/43); IGb: 7% (3/45); CG: 0% (43/43). Lost to follow‐up: IGa: 2 declined, 1 family reasons; IGb: 1 unable to contact, 1 cardiac symptoms, 2 declined, 1 surgery. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: self‐reported OA, aged 50‐75 years. Exclusion criteria: on waiting list for knee/hip replacement. Country: Netherlands. Sample number: IG: 35; CG: 35. Mean age: 65 years. Progress Plus: 80% women; 68% living as married; 29% living alone; primary education 17%, secondary education 54%, college/university 27%. |
|
| Interventions |
Provider(s): physical therapist. Training: yes. Setting: not stated. Content: stretch/balance + patient information. Length/intensity: 1 session a week for 6 weeks. Control: wait list. |
|
| Outcomes | At 12 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Limited information. Participants described as ‘randomised.' |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Likely that participants and providers were aware of treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcomes assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IG: 0% (0/35); CG: 2.8% (1/35). ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed cluster‐randomised controlled trial. | |
| Participants |
Inclusion criteria: aged ≥ 50 years; mild, moderate or severe knee pain of > 6 months' duration. Exclusion criteria: lower limb arthroplasty, physiotherapy for knee pain in the preceding 12 months, intra‐articular injections in the preceding 6 months, unstable medical conditions, inability/unwillingness to exercise, wheelchair dependence and inability to understand English. Participants were not excluded if they used assistive walking devices; had stable comorbidities common in this age group (e.g. type II diabetes, cardiovascular or respiratory disorders); or had back, lower limb pain or upper limb pain. Country: UK. Sample number: IGa: 132 (108 with no missing data points); IGb: 146 (121 with no missing data points); CG: 140 (113 with no missing data points). Mean age: IGa: 66 years; IGb 68 years; CG 67 years. Progress Plus: women:men: IGa 94:38; IGb: 104:42; CG 96:44. |
|
| Interventions |
Provider(s): physiotherapists. Training: yes. Setting: clinical setting, hospital. Intervention content: intervention: combined discussion on specific topics regarding self‐management and coping, etc., with a progressive exercise regimen delivered to IGa (small groups of participants) and IGb (individual participants). Length/intensity: twice weekly for 6 weeks. Control: usual primary care. |
|
| Outcomes | At 24 weeks:
|
|
| Notes | There are 2 Hurley 2007 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Primary care practices randomly allocated in blocks of 3. 2 centres were randomly assigned as intervention sites (usual primary care and individual rehabilitation or group rehabilitation) and 1 clinic assigned as control site. |
| Allocation concealment (selection bias) | Low risk | Central allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blinded to allocation groups. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors blinded to a participant's allocation. Success of blinding evaluated by asking assessors to identify each participant's allocation at each assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: CG: 27/140 (9%); IGa: 24/132 (18%); IGb: 25/146 (17%). Reasons reported. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Cluster randomised controlled trial. | |
| Participants |
Inclusion criteria: adults verbally complaining of knee pain or muscle weakness in lower extremity or when they were confirmed by a clinical examination as having OA affecting their knees. Diagnosis of OA of the knee confirmed by medical history and a physical examination. Consisted of having at least 1 of 3 conditions: aged > 50 years; having morning stiffness lasting for < 30 minutes or existing crepitus when moving the legs; or an X‐ray showing osteophytes. Exclusion criteria: previous knee replacement or surgery, unable to maintain balance while standing independently, comorbidity with any medical conditions that could be exacerbated by the protocol, such as unstable heart disease. Country: Taiwan. Sample number: IG: 114; CG: 91. Mean age: 67 years. Progress Plus: gender: mixed; marital status: single/widow: 34.2%, married: 65.8%; elementary/primary school education: 41.2%, high school education: 28.1%, above college education: 30.7%. |
|
| Interventions |
Provider(s): physical therapist. Training: yes. Setting: community. Content: education; stretching and strengthening exercises and discussion. Length/intensity: 80‐minute sessions 1 × week for 4 weeks. Control: Normal routine care. |
|
| Outcomes | At 8 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Lack of information regarding cluster randomisation process. |
| Allocation concealment (selection bias) | High risk | No information. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported, but unlikely that providers and participants were blind to treatment condition. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded outcomes assessors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition: IG: 14.9% (20/134); CG: 27.2% (34/125). Details of how missing data were handled not reported. No ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed randomised controlled trial. | |
| Participants |
Inclusion criteria: married adults with persistent knee pain due to OA and who were diagnosed as having OA of the knees and their respective spouses. Exclusion criteria: comorbid medical conditions that could affect health status over course of trial, abnormal cardiac response to exercise or other known organic disease that would contraindicate safe participation in the study. Country: US. Sample number: IGa: 20; IGb: 16; CG: 18. Mean age: 59 years. Progress Plus: 50% women. |
|
| Interventions |
Provider(s): exercise physiologist and psychologist. Training: yes. Setting: not stated. Intervention content: IGa: spouse‐assisted coping skills training + exercise training (strength/resistance + aerobic) + patient information; IGb: exercise training (strength/resistance + aerobic) + patient information. Length/intensity: 3 × 60‐minute sessions a week for 12 weeks total 50 hours. Control: usual treatment/care with assignment. |
|
| Outcomes | At 12 weeks:
|
|
| Notes | There are 2 Keefe 2004 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Limited information. |
| Allocation concealment (selection bias) | High risk | No information given. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No information given. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IGa: 5% (1/20); IGb: 0% (0/16); CG: 11% (2/18). Reasons for lost to follow‐up not reported. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: women aged ≥ 60 years with OA capable of understanding the information in the questionnaires and the objectives of the study; gave consent to participate; able to detect and record their pain levels (over 3 points on VAS); able to walk and move. Exclusion criteria: none reported. Country: South Korea. Sample number: IG: 35; CG: 35. Mean age: IG: 55‐59 0 (0.0%); 60‐64 11 (31.4%); 65‐69 15 (42.9%); ≥70 9 (25.7%) CG: 55‐59 2 (5.7%); 60‐64 9 (25.7%); 65‐69 17 (48.6%); ≥70 7 (20.0%) Progress Plus: 100% women; education: none 11.4, elementary 14.3, middle school 42.9, high school 14.3, ≥ college 17.1; marital status: married 62.9, bereavement 31.4, other 5.7; income: yes 11.4, none 88.6. |
|
| Interventions |
Provider(s): certified exercise instructor. Training: yes. Setting: recreational/leisure facilities. Content: patient education; stretching; strengthening exercises; cardiovascular\range of motion, flexibility, muscle strength and endurance. Length/intensity: 3 sessions a week for 12 weeks. Control: usual care. |
|
| Outcomes | At 12 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as "simple randomization" of people recruited from a public health centre located in G city, South Korea. |
| Allocation concealment (selection bias) | High risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition: IG: 12.5% (5/40); CG: 12.5% (5/40). Lost to follow‐up: IG: 1 accident on the pool deck, 2 domestic problems, 2 physical problems; CG: 2 domestic problems; 3 physical problems. Details of how missing data was handled not reported. No ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: adults aged > 55 years with knee OA, considered to be present if 1 or both knees exhibited grade 2 or higher OA by Kellgren and Lawrence (K/L) criteria. Knee pain was considered to be present if participants reported moderate or greater knee pain in the past month (i.e. a rating of ≥3 on a 5‐point Likert scale) for any of the 5 items of the WOMAC pain scale. Exclusion criteria: inability to walk without assistance; amputation of either lower extremity; knee or hip replacement; history of stroke, myocardial infarction, congestive heart failure, uncontrollable hypertension, fibromyalgia, rheumatoid arthritis or other systemic connective tissue disease; lower‐extremity neuropathy; severe cognitive impairment. Country: US. Sample number: IG: 82; CG: 80. Mean age: 69 years. Progress Plus: 84% women. |
|
| Interventions |
Provider(s): fitness trainer. Training: yes. Setting: National Institute for Fitness and Sport and home based. Content: strength training. Length/intensity: exercise 3 times a week (twice at a fitness facility, once at home) for 12 weeks, followed by transition to home‐based exercise after 12 months. Comparator: attention placebo/alternative intervention; range of motion exercises. |
|
| Outcomes | At 30 months:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation scheme allocated participants into 8 groups on the basis of sex and the presence of radiographic evidence of knee OA and knee pain. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blind to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Breakdown of attrition by group for each follow‐up period not provided. Attrition: entire sample: 30% (66/221); IG: 36%; CG: 24%. Reasons for dropout not reported in full. However, authors described that primary reason was time and travel involved in participating. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Quasi‐experimental partially randomised controlled trial. | |
| Participants |
Inclusion criteria: aged > 65 years; living in the community/non‐institutionalised; self‐reported joint pain attributed to OA and in 1 or more of hip, knee, foot or ankle; chronic pain ≥ 15 days a month for > 3 months, pain level ≥ 4 on a 10‐point scale (1 = no pain, 10 = excruciating pain); inability to participate in standing exercise; ability to speak English. Sample size: 34; IG: 23; CG: 11. Mean age: 79 years (SD 6.42). Country: US. Progress Plus: 26 women (76.5%); 21 non‐Hispanic white (61.8%); 19 widowed (55.8%); 27 (79.4%) reported chronic pain for > 3 years; 11 (73.5%) reported highest pain level ≥ 5; 27 (79.4%) taking medication for pain. |
|
| Interventions |
Providers: Yoga Alliance certified instructors with cardiopulmonary resuscitation certification and ≥ 1 year of yoga teaching experience. Setting: group sessions at a senior centre. Content: chair yoga. Length/intensity: both groups had 45 minutes twice a week for 8 weeks. Control: general health education information and specific facts related to effects of OA. |
|
| Outcomes |
Outcomes: at 4 and 8 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sealed envelopes; unclear if these were selected 1 by 1 removed from box: this could have made subsequent participants have an increased chance of picking an envelope for a particular condition. |
| Allocation concealment (selection bias) | High risk | 9 participants with more severe Alzheimer's disease were assigned to the intervention condition as the control condition was not suitable for them. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding apparent, and CG participants appeared to have been aware of what the IG entailed (contamination reported by authors). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition: uneven and some uncertainty in reporting. 1 IG (due to unrelated hospitalisation) and 5 CG withdrew (1 due to scheduling and preference for IG, others unspecified. Some inconsistency in reporting: the final reported sample size is "29 participants after 5 participants withdrew" but other reporting suggested 6 withdrawals. |
| Selective reporting (reporting bias) | Low risk | All measured variables had results reported. |
| Other bias | Low risk | No other bias identified. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: aged > 50 years with knee OA. Exclusion criteria: not expecting to be absent from the city for > 2 weeks; having independent non‐institutional lifestyle, not having intra‐articular steroid or visco‐elastic device injections within 2 months preceding intervention period; stable regimen using analgesics or non‐steroidal anti‐inflammatory drugs ≥ 2 weeks before beginning of intervention. Country: Canada. Sample number: IG: 59; CG: 65. Mean age: 66 years. Progress Plus: 70% women; married or living as married 61%; divorced separated 5%; never married: 15%. |
|
| Interventions |
Provider(s): not stated. Training: yes. Setting: not stated. Content: aerobic strength, stretching and strengthening exercises. Length/intensity: 3 × 1‐hour session a week for 12 weeks. Control: usual treatment/care, with assignment, continued usual activities and attended 1‐hour education/information session twice a month. |
|
| Outcomes | At 12 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Blocked random number tables, stratified according to disease severity. |
| Allocation concealment (selection bias) | High risk | No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants and providers were unaware of treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition: IG: 14.4% (10/69); CG: 4.4% (3/68). Breakdown of participants lost to follow‐up by group not reported. Authors described medical conditions and lack of time as most common reason for dropout. 1 person withdrew after knee inflammation. Reported difference included dropouts: having a lower educational level, more difficulty performing household tasks, fewer social activities and more joint pain and were more likely to be separated or divorced. No ITT analysis reported. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial, feasibility study. | |
| Participants |
Inclusion criteria: aged ≥ 50 years, physician‐confirmed diagnosis of OA of knee, overweight or obese, and written permission to participate from a physician. Exclusion criteria: self‐reported currently doing lower‐extremity exercise ≥ 2 times a week; self‐reported currently fitness walking ≥ 90 minutes a week; unable to read and write English at a level necessary to complete a physical activity diary and questionnaires; did not have, or could not use, a telephone or was unwilling to provide home telephone number; incapable of managing own treatment regimen or scored ≤ 23 on the Mini‐Mental Status Examination (Folstein 1975); self‐reported OA of hip that prohibited participation in fitness walking or inflammatory arthritis; self‐reported current knee conditions such as meniscus tears, knee ligament ruptures or previous unilateral knee replacement surgery; scheduled to undergo major surgical procedure in the next 6 months; currently participating in a drug or psychoeducational trial that may confound, or be confounded by, participation in this study; and contraindications for exercise testing based on American College of Sports Medicine (ACSM 2006) criteria or has resting or exercise responses during baseline maximum‐graded exercise testing that are consistent with the ACSM guidelines suggesting that exercise is contraindicated. Country: US. Sample number: IG: 11; CG: 10. Mean age: 63 years. Progress Plus: 96% women; 54% married; 71% unemployed. |
|
| Interventions |
Provider(s): physical therapist and nurse. Training: yes. Setting: medical centre and home. Content: multicomponent lower‐extremity flexibility and strengthening exercise and adherence counselling using self‐efficacy strategies. Length/intensity: 15 sessions over 24 weeks; 6 weekly physical activity sessions and 9 biweekly telephone counselling sessions. Control: usual care. |
|
| Outcomes | At 12 months:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Limited information provided. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants could not be blinded to group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IG: 15.3% (2/13); CG: 23% (3/13). Reasons for dropout not reported; however, authors report no differences between groups. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | Authors reported no statistically significant baseline differences between intervention and control groups but did not report values. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: aged ≥ 40 years; documented diagnosis of chronic, stable, primary OA of 1 or both knee joints in association with ≥ 4‐month history of symptomatic knee pain occurring during weight‐bearing activities (people with multiple joint involvement, who had undergone major joint surgery, or had a lower joint prosthesis were also eligible); radiographic evidence of primary OA of 1 or both knee joints, as demonstrated by joint‐space narrowing, marginal spur formation or subchondral cyst formation; use of any of the various common, non‐prescription non‐steroidal anti‐inflammatory drugs ≥ 2 days a week; and non‐participation in a regular programme of physical activity at time of enrolment. Exclusion criteria: serious medical conditions for which exercise would be contraindicated, such as unstable angina, significant aortic stenosis, myocardial infarction within the last 3 months or advanced chronic obstructive pulmonary disease; asymptomatic primary OA of 1 or both knees; dementia or inability to give informed consent; non‐ambulation due to amputation, stroke or incapacitating arthritis; or involvement in another treatment programme or study protocol. Country: US. Sample number: IG: 47; CG: 45. Mean age: 72 years. Progress Plus: 75% women; 27% married, 72% unmarried; 96% white American, 3% Hispanic Latino. |
|
| Interventions |
Provider(s): not stated. Training: yes. Setting: hospital, group based. Content: multicomponent: aerobic + patient education. Length/intensity: 3 sessions a week for 8 weeks. Control: weekly telephone call. |
|
| Outcomes | At 12 months:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | High risk | Randomisation conducted by the study co‐ordinator; no mention of concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers not blind to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unblinded outcomes assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition: IG: 38.2% (18/47); CG: 48.8% (22/45). Lost to follow‐up: IG: 3 refused to be interviewed, 2 sick in the hospital and unable to complete an interview, 1 death 1, 12 could not be contacted; CG: 3 refused to be interviewed, 2 death, 17 could not be contacted. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: aged > 55 years, body mass index ≤40 kg/m2, WOMAC pain subscale score (VAS version) >40 (range 0‐500), and fulfilment of the ACR criteria for knee OA with radiographic Kellgren/Lawrence scale knee OA grade ≥ 2. Exclusion criteria: none specified. Country: US. Sample number: IG: 20; CG: 20. Mean age: 72 years. Progress Plus: gender: mixed; high school education: 100%. |
|
| Interventions |
Provider(s): qualified Tai Chi Master/instructor. Training: yes. Setting: hospital. Content: warm up and review of Tai Chi principles and techniques; Tai Chi exercises; breathing techniques and relaxation methods. Length/intensity: twice weekly for 12 weeks. Control: attention placebo/alternative intervention; wellness education and stretching programme. |
|
| Outcomes | At 48 weeks:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment by statistician using computer‐generated numbers to randomise permuted blocks of sizes 2 and 4. |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers unblended to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded outcomes assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition: IG 0% (0/20); CG 0% (0/20). ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants |
Inclusion criteria: capable of completing questionnaire verbally and either had OA affecting the knee according to self‐report or screening of outpatient medical records. Diagnosis of OA of the knee confirmed by medical history and physical examination based on the clinical criteria of the ACR criteria 1991 (Altman 1986, Altman 1991, Hopkins 2002). Clinical criteria for OA of knee consisted of pain in knee and any 3 of: aged ≥ 50 years; < 30 minutes of morning stiffness; crepitus on active motion; bony tenderness; bony enlargement; or no palpable joint warmth. Exclusion criteria: bed bound, wheelchair bound or loss of balance while standing; knee replacement; currently undergoing active physiotherapy such as hydrotherapy or strengthening exercises; currently receiving acupuncture treatments, since they could over‐exert efforts for exercise compliance and could influence the outcome results masking the results from the intervention itself. Country: Hong Kong. Sample number: IG: 67; CG: 54. Mean age: 64 years. Progress Plus: 88% women; 53% married/living together. |
|
| Interventions |
Provider(s): nurse. Training: yes. Setting: not stated. Content: multicomponent: stretching/walking/Tai Chi + patient education self‐management programme. Length/intensity: 1 session a week for 16 weeks. Control: usual care. |
|
| Outcomes | At 8 months:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition: IG: 23.9% (21/88); CG: 43.6% (41/94). Missing data between groups not accounted for; no ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
ACR: American College of Rheumatology; AIMS: Arthritis Impact Measurement Scale; AQoL‐6D: Assessment of Quality of Life‐6D; BMI: body mass index; CES‐D: Center for Epidemiologic Studies Depression Scale; CG: control group; ECG: electrocardiogram; ESR: erythrocyte sedimentation rate; HADS: Hospital Anxiety and Depression Scale; HRQoL: health‐related quality of life; IG: intervention group; ITT: intention to treat; m: metre; m/s: metres/second; n: number of participants; NRS: numerical rating scale; OA: osteoarthritis; PCST: Pain Coping Skills Training; SD: standard deviation; SF‐12: 12‐item Short Form; SF‐36: 36‐item Short Form; VAS: visual analogue scale; VAP: Visual Analogue Pain Scale; WOMAC: Western Ontario McMaster Universities Osteoarthritis Index.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Arnold 2010 | Intervention: no non‐exercise control group. |
| Bautch 1997 | Outcome: pain only. |
| Bennell 2010 | Outcome: pain only. |
| Bezalel 2010 | Outcome: pain only. |
| Brismee 2007 | Outcome: pain only. |
| Bruce‐Brand 2012 | Outcome: mental health component score. |
| Cadmus 2010 | Intervention: no non‐exercise control group. |
| Callaghan 1995 | Outcome: pain only. |
| Deyle 2000 | Outcome: pain only. |
| Dias 2003 | Outcome: pain only. |
| Ebnezar 2012 | Outcome: pain only. |
| Ettinger 1997 | Outcome: pain only |
| Eyigor 2004 | Intervention: no non‐exercise control group. |
| Foley 2003 | Outcome: data not available as mean scores and standard deviations. |
| Fransen 2001 | Outcome: mental component score given as a total not individual. |
| Gomes 2012 | Outcome: pain only. |
| Gur 2002 | Outcome: pain only. |
| Halbert 2001 | Outcome: pain only. |
| Hart 2000 | Outcome: pain only. |
| Hasegawa 2013 | Outcome: pain only. |
| Hay 2006 | Outcome: data not available as mean scores and standard deviations. |
| Hinman 2007 | Outcome: pain only. |
| Hiyama 2012 | Outcome: pain only. |
| Hoeksma 2005 | Outcome: pain only. |
| Huang 2003 | Outcome: pain only. |
| Huang 2005 | Outcome: pain only. |
| Hughes 2004 | Outcome: data not available as mean scores and standard deviations. |
| Jenkinson 2009 | Outcome: data not available as mean scores and standard deviations. |
| Juhakoski 2011 | Outcome: pain only. |
| Kawasaki 2009 | Outcome: pain only. |
| Kostopoulos 2000 | Intervention: no non‐exercise control group. |
| Kovar 1992 | Outcome: pain only. |
| Lee 2009 | Outcome: mental health component score. |
| Lim 2010 | Intervention: no non‐exercise control group. |
| Mangione 1999 | Outcome: pain only. |
| McCarthy 2003 | Intervention: no non‐exercise control group. |
| Messier 2004 | Outcome: pain only; additional analysis reported in Focht 2005. |
| Murphy 2010 | Intervention: no non‐exercise control group. |
| O'Reilly 1999 | Outcome: pain only. |
| Petrella 2000 | Outcome: pain only. |
| Pisters 2010 | Outcome: pain only. |
| Pollard 2008 | Outcome: pain only. |
| Quilty 2003 | Outcome: pain only. |
| Ravaud 2004 | Outcome: pain only. |
| Røgind 1998 | Outcome: pain only. |
| Salli 2010 | Outcome: mental health component score. |
| Schilke 1996 | Outcome: pain only. |
| Sekir 2005 | Outcome: pain only. |
| Shakoor 2007 | Outcome: pain only. |
| Silva 2008 | Outcome: pain only. |
| Simao 2012 | Outcome: pain only. |
| Song 2003 | Outcome: pain only. |
| Stoneman 2001 | Outcome: pain only. |
| Tak 2005 | Outcome: pain only. |
| Talbot 2003 | Outcome: pain only. |
| Thomas 2002 | Outcome: data not available as mean scores and standard deviations. |
| Thorstensson 2005 | Outcome: mental health component score. |
| Topp 2002 | Outcome: pain only. |
| van Baar 1998b | Outcome: pain only. |
| Veenhof 2006 | Outcome: pain only. |
Contributions of authors
| Roles and responsibilities | |
| Draft the protocol | MH, KD, NW, SO |
| Develop a search strategy | CS, KD |
| Search for trials | CS, KD, RH |
| Obtain copies of trials | HH, KD, RH |
| Select which trials to include | KD, HH, MH, NW, RH |
| Extract data from trials | KD, HH, NW, MH, RH, RG |
| Enter data into RevMan | KD, MH, HH, RH, RG |
| Carry out the analysis | KD, HH, RG |
| Interpret the analysis | KD, HH, RG, MH, NW, SO, RH |
| Draft the final review | KD, HH, MH, SO, NW, RG |
| Update the review | KD, MH, NW, RH, RG |
| CERQual | KD, RH |
Sources of support
Internal sources
No sources of support supplied
External sources
-
Arthritis Research UK, UK.
Educational Grant, Number 20163
Declarations of interest
MH: no conflicting interests to declare.
KD: no conflicting interests to declare.
RH: no conflicting interests to declare.
RG: no conflicting interests to declare.
HH: no conflicting interests to declare.
NW: no conflicting interests to declare.
CS: no conflicting interests to declare.
SO: no conflicting interests to declare.
New
References
References to studies included in this review
- Aglamis B, Toraman NF, Yamanc H. The effect of a 12‐week supervised multi‐component exercise program on knee OA in Turkish women. Journal of Back and Musculoskeletal Rehabilitation 2008;21:121‐8. [Google Scholar]
- Baker KR, Nelson ME, Felson DT, Layne J, Sarno R, Roubenoff R. The efficacy of home based progressive strength training in older adults with knee osteoarthritis: a randomized controlled trial. Journal of Rheumatology 2001;28:1655‐65. [PubMed] [Google Scholar]
- Bennell KL, Egerton T, Martin J, Abbott JH, Metcalf B, McManus F, et al. Effect of physical therapy on pain and function in patients with hip osteoarthritis: a randomized clinical trial. JAMA 2014;311(19):1987‐97. [DOI] [PubMed] [Google Scholar]
- Bennell KL, Ahamed Y, Jull G, Bryant C, Hunt MA, Forbes AB, et al. Physical therapist‐delivered pain coping skills training and exercise for knee osteoarthritis: randomized controlled trial. Arthritis Care & Research 2016;68(5):590‐602. [DOI] [PubMed] [Google Scholar]
- Cheung C, Wyman JF, Resnick B, Savik K. Yoga for managing knee osteoarthritis in older women: a pilot randomized controlled trial. BMC Complementary and Alternative Medicine 2014;14:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes L, Storheimyz K, Sandvik L, Nordsletten L, Risberg MA. Efficacy of patient education and supervised exercise vs patient education alone in patients with hip osteoarthritis: a single blind randomized clinical trial. Osteoarthritis and Cartilage 2010;18:1237‐43. [DOI] [PubMed] [Google Scholar]
- Focht BA, Rejeski WJ, Ambrosius WT, Katula JA, Messier SP. Exercise, self‐efficacy, and mobility performance in overweight and obese older adults with knee osteoarthritis. Arthritis Care & Research 2005;53(5):659‐65. [DOI] [PubMed] [Google Scholar]
- Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Care & Research 2007;57:407‐14. [DOI] [PubMed] [Google Scholar]
- French H, Cusack T, Brennan A, Caffrey A, Conroy R, Cuddy V, et al. Exercise and Manual Physiotherapy Arthritis Research Trial (EMPART) for osteoarthritis of the hip: a multicenter randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2013;94:302‐14. [DOI] [PubMed] [Google Scholar]
- Hopman‐Rock M, Westhoff MH. The effects of a health educational and exercise program for older adults with osteoarthritis for the hip or knee. Journal of Rheumatology 2000;27:1947‐54. [PubMed] [Google Scholar]
- Hurley MV, Walsh NE, Mitchell HL, Pimm TJ, Patel A, Williamson E, et al. Clinical effectiveness of a rehabilitation program integrating exercise, self‐management, and active coping strategies for chronic knee pain: a cluster randomized trial. Arthritis Research 2007;57:1211‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kao MJ, Wu MP, Tsai MW, Chang WW, Wu SF. The effectiveness of a self‐management program on quality of life for knee osteoarthritis (OA) patients. Archives of Gerontology and Geriatrics 2012;54:317‐24. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Blumenthal J, Baucom D, Affleck G, Waugh R, Caldwell DS, et al. Effects of spouse‐assisted coping skills training and exercise training in patients with osteoarthritic knee pain: a randomized controlled study. Pain 2004;110:539‐49. [DOI] [PubMed] [Google Scholar]
- Kim IS, Chung HS, Park YJ, Kang HY. The effectiveness of an aquarobic exercise program for patients with osteoarthritis. Applied Nursing Research 2012;25:181‐9. [DOI] [PubMed] [Google Scholar]
- Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Care & Research 2006;55(5):690‐9. [DOI] [PubMed] [Google Scholar]
- Park J, McCaffrey R, Newman D, Cheung C, Hagen D. The effect of sit 'n' fit chair yoga among community‐dwelling older adults with osteoarthritis. Holistic Nursing Practice 2014;28(4):247‐57. [DOI] [PubMed] [Google Scholar]
- Péloquin L, Bravo G, Gauthier P, Lacombe G, Billiard JS. Effects of a cross‐training exercise program in persons with osteoarthritis of the knee a randomized controlled trial. Journal of Clinical Rheumatology 1999;5:126‐36. [DOI] [PubMed] [Google Scholar]
- Schlenk EA, Lias JL, Sereika SM, Dunbar‐Jacob J, Kwoh CK. Improving physical activity and function in overweight and obese older adults with osteoarthritis of the knee: a feasibility study. Rehabilitation Nursing 2011;36(1):32‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan T, Allegrante JP, Peterson MG, Kovar PA, MacKenzie CR. One‐year followup of patients with osteoarthritis of the knee who participated in a program of supervised fitness walking and supportive patient education. Arthritis and Rheumatism 1998;11:228‐33. [DOI] [PubMed] [Google Scholar]
- Wang C, Schmid CH, Hibberd PL, Kalish R, Roubenoff R, Rones R, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Care & Research 2009;61(11):1545‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip YB, Sit JW, Fung KK, Wong DY, Chong SY, Chung LH, et al. Effects of a self‐management arthritis programme with an added exercise component for osteoarthritic knee: randomized controlled trial. Journal of Advanced Nursing 2007;59:20‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Arnold CM, Faulkner RA. The effect of aquatic exercise and education on lowering fall risk in older adults with hip osteoarthritis [corrected] [published erratum appears in Journal of Aging & Physical Activity 2010;18(4):477‐9]. Journal of Aging & Physical Activity 2010;18:245‐60. [DOI] [PubMed] [Google Scholar]
- Bautch JC, Malone DG, Vailas AC. Effects of exercise on knee joints with osteoarthritis: a pilot study of biologic markers. Arthritis Care & Research 1997;10(1):48‐55. [DOI] [PubMed] [Google Scholar]
- Bennell KL, Hunt MA, Wrigley TV, Hunter DJ, McManus FJ, Hodges PW. Hip strengthening reduces symptoms but not knee load in people with medial knee osteoarthritis and varus malalignment: a randomised controlled trial. Osteoarthritis and Cartilage 2010;18:621‐8. [DOI] [PubMed] [Google Scholar]
- Bezalel T, Carmeli E, Katz‐Leurer M. The effect of a group education programme on pain and function through knowledge acquisition and home‐based exercise among patients with knee osteoarthritis: a parallel randomised single‐blind clinical trial. Physiotherapy 2010;96:137‐43. [DOI] [PubMed] [Google Scholar]
- Brismee JM, Paige RL, Chyu MC, Boatright JD, Hagar JM. Group and home‐based Tai Chi in elderly subjects with knee osteoarthritis: a randomized controlled trial [with consumer summary]. Clinical Rehabilitation 2007;21:99‐111. [DOI] [PubMed] [Google Scholar]
- Bruce‐Brand RA, Walls RJ, Ong JC, Emerson BS, O'Byrne JM, Moyna NM. Effects of home‐based resistance training and neuromuscular electrical stimulation in knee osteoarthritis: a randomized controlled trial. BMC Musculoskeletal Disorders 2012;13:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadmus L, Patrick MB, Maciejewski ML, Topolski T, Belza B, Patrick DL. Community‐based aquatic exercise and quality of life in persons with osteoarthritis. Medicine and Science in Sports and Exercise 2010;42:8‐15. [DOI] [PubMed] [Google Scholar]
- Callaghan MJ, Oldham JA, Hunt J. An evaluation of exercise regimes for patients with osteoarthritis of the knee: a single‐blind randomized controlled trial. Clinical Rehabilitation 1995;9:213‐8. [Google Scholar]
- Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Annals of Internal Medicine 2000;132:173‐81. [DOI] [PubMed] [Google Scholar]
- Dias RC, Dias JM, Ramos LR. Impact of an exercise and walking protocol on quality of life for elderly people with OA of the knee. Physiotherapy Research International 2003;8:121‐30. [DOI] [PubMed] [Google Scholar]
- Ebnezar J, Nagarathna R, Yogitha B, Nagendra HR. Effects of an integrated approach of hatha yoga therapy on functional disability, pain, and flexibility in osteoarthritis of the knee joint: a randomized controlled study. Journal of Alternative and Complementary Medicine 2012;18:463‐72. [DOI] [PubMed] [Google Scholar]
- Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA 1997;277:25‐31. [PubMed] [Google Scholar]
- Eyigor S. A comparison of muscle training methods in patients with knee osteoarthritis. Clinical Rheumatology 2004;23:109‐15. [DOI] [PubMed] [Google Scholar]
- Foley A, Halbert J, Hewitt T, Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis ‐ a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Annals of the Rheumatic Diseases 2003;62:1162‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. Journal of Rheumatology 2001;28:156‐64. [PubMed] [Google Scholar]
- Gomes WF, Lacerda AC, Mendonca VA, Arrieiro AN, Fonseca SF, Amorim MR, et al. Effect of aerobic training on plasma cytokines and soluble receptors in elderly women with knee osteoarthritis, in response to acute exercise. Clinical Rheumatology 2012;31:759‐66. [DOI] [PubMed] [Google Scholar]
- Gur H, Cakin N, Akova B, Okay E, Kucukoglu S. Concentric versus combined concentric‐eccentric isokinetic training: effects on functional capacity and symptoms in patients with osteoarthrosis of the knee. Archives of Physical Medicine and Rehabilitation 2002;83:308‐16. [DOI] [PubMed] [Google Scholar]
- Halbert J, Crotty M, Weller D, Ahern M, Silagy C. Primary care‐based physical activity programs: effectiveness in sedentary older patients with osteoarthritis symptoms. Arthritis and Rheumatism 2001;45:228‐34. [DOI] [PubMed] [Google Scholar]
- Hart LE. Combination of manual physical therapy and exercises for osteoarthritis of the knee. Clinical Journal of Sport Medicine 2000;10:305. [DOI] [PubMed] [Google Scholar]
- Hasegawa M, Yamazaki S, Kimura M, Nakano K, Yasumura S. Community‐based exercise program reduces chronic knee pain in elderly Japanese women at high risk of requiring long‐term care: a non‐randomized controlled trial. Geriatrics & Gerontology International 2013;13:167‐74. [DOI] [PubMed] [Google Scholar]
- Hay EM, Foster NE, Thomas E, Peat G, Phelan M, Yates HE. Effectiveness of community physiotherapy and enhanced pharmacy review for knee pain in people aged over 55 presenting to primary care: pragmatic randomised trial. BMJ 2006;333:995‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinman RS, Heywood SE, Day AR. Aquatic physical therapy for hip and knee osteoarthritis: results of a single‐blind randomized controlled trial. Physical Therapy 2007;87:32‐43. [DOI] [PubMed] [Google Scholar]
- Hiyama Y, Yamada M, Kitagawa A, Tei N, Okada S. A four‐week walking exercise programme in patients with knee osteoarthritis improves the ability of dual‐task performance: a randomized controlled trial. Clinical Rehabilitation 2012;26:403‐12. [DOI] [PubMed] [Google Scholar]
- Hoeksma HL, Dekker J, Ronday HK, Breedveld FC, Ende CH. Manual therapy in osteoarthritis of the hip: outcome in subgroups of patients. Rheumatology 2005;44:461‐4. [DOI] [PubMed] [Google Scholar]
- Huang MH, Lin YS, Yang RC, Lee CL. A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis. Seminars in Arthritis and Rheumatism 2003;32:398‐406. [DOI] [PubMed] [Google Scholar]
- Huang MH, Yang RC, Lee CL, Chen TW, Wang MC. Preliminary results of integrated therapy for patients with knee osteoarthritis. Arthritis and Rheumatism 2005;53:812‐20. [DOI] [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell R, Pollak N, Huber G, Sharma L. Impact of the fit and strong intervention on older adults with osteoarthritis. Gerontologist 2004;44:217‐28. [DOI] [PubMed] [Google Scholar]
- Jenkinson CM, Doherty M, Avery AJ, Read A, Taylor MA, Sach TH. Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial [with consumer summary]. BMJ 2009;339:b3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juhakoski R, Tenhonen S, Malmivaara A, Kiviniemi V, Anttonen T, Arokoski JP. A pragmatic randomized controlled study of the effectiveness and cost consequences of exercise therapy in hip osteoarthritis. Clinical Rehabilitation 2011;25:370‐83. [DOI] [PubMed] [Google Scholar]
- Kawasaki T, Kurosawa H, Ikeda H, Takazawa Y, Ishijima M, Kubota M, et al. Therapeutic home exercise versus intraarticular hyaluronate injection for osteoarthritis of the knee: 6‐month prospective randomized open‐labeled trial. Journal of Orthopaedic Science 2009;14:182‐91. [DOI] [PubMed] [Google Scholar]
- Kostopoulos D. Comparative Effects of Aquatic Recreational and Aquatic Exercise Programs on Mobility, Pain Perception, and Treatment Satisfaction Among Elderly Persons with Osteoarthritis of the Knee. Dissertation2000.
- Kovar PA, Allegrante JP, MacKenzie CR, Peterson MG, Gutin B, Charlson ME. Supervised fitness walking in patients with osteoarthritis of the knee. A randomized, controlled trial. Annals of Internal Medicine 1992;116:529‐34. [DOI] [PubMed] [Google Scholar]
- Lee HJ, Park HJ, Chae Y, Kim SY, Kim SN, Kim ST. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: a pilot, randomized, waiting list controlled trial. Clinical Rehabilitation 2009;23:504‐11. [DOI] [PubMed] [Google Scholar]
- Lim JY, Tchai E, Jang SN. Effectiveness of aquatic exercise for obese patients with knee osteoarthritis: a randomized controlled trial. PM & R : the Journal of Injury, Function, and Rehabilitation 2010;2:723‐31. [DOI] [PubMed] [Google Scholar]
- Mangione KK, McCully K, Gloviak A, Lefebvre I, Hofmann M, Craik R. The effects of high‐intensity and low‐intensity cycle ergometry in older adults with knee osteoarthritis. Journals of Gerontology: Series A: Biological Sciences and Medical Sciences 1999;54A:M184‐90. [DOI] [PubMed] [Google Scholar]
- McCarthy C, Pullen R, Mills P, Roberts C, Silman A, Oldham J. Supplementing home exercise with class‐based exercise leads to reductions in pain in knee osteoarthritis, but no greater muscle strength or compliance with home exercise at long term follow‐up. Rheumatology 2003;42:17‐8. [Google Scholar]
- Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the arthritis, diet, and activity promotion trial. Arthritis and Rheumatism 2004;50:1501‐10. [DOI] [PubMed] [Google Scholar]
- Murphy SL, Lyden AK, Smith DM, Dong Q, Koliba JF. Effects of a tailored activity pacing intervention on pain and fatigue for adults with osteoarthritis. American Journal of Occupational Therapy 2010;64:869‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reilly SC, Muir KR, Doherty M. Effectiveness of home exercise on pain and disability from osteoarthritis of the knee. Annals of Rheumatic Diseases 1999;58:15‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrella R J, Bartha C. Home based exercise therapy for older patients with knee osteoarthritis: a randomized clinical trial. Journal of Rheumatology 2000;27:2215‐21. [PubMed] [Google Scholar]
- Pisters MF, Veenhof C, Schellevis FG, De Bakker, DH, Dekker J. Long‐term effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized controlled trial comparing two different physical therapy interventions. Osteoarthritis and Cartilage 2010;18:1019‐26. [DOI] [PubMed] [Google Scholar]
- Pollard H, Ward G, Hoskins W, Hardy K. The effect of a manual therapy knee protocol on osteoarthritic knee pain: a randomised controlled trial. Journal of the Canadian Chiropractic Association 2008;52:229‐42. [PMC free article] [PubMed] [Google Scholar]
- Quilty B, Tucker M, Campbell R, Dieppe P. Physiotherapy, including quadriceps exercises and patellar taping, for knee osteoarthritis with predominant patello‐femoral joint involvement: randomized controlled trial. Journal of Rheumatology 2003;30:1311‐7. [PubMed] [Google Scholar]
- Ravaud P, Giraudeau B, Logeart I, Larguier JS, Rolland D, Treves R, et al. Management of osteoarthritis (OA) with an unsupervised home based exercise programme and/or patient administered assessment tools. A cluster randomised controlled trial with a 2x2 factorial design. Annals of the Rheumatic Diseases 2004;63:703‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Røgind H, Bibow‐Nielsen B, Jensen B, Møller HC, Frimodt‐Møller H, Bliddal H. The effects of a physical training program on patients with osteoarthritis of the knees. Archives of Physical Medicine and Rehabilitation 1998;79:1421‐7. [DOI] [PubMed] [Google Scholar]
- Salli A, Sahin N, Baskent A, Ugurlu H. The effect of two exercise programs on various functional outcome measures in patients with osteoarthritis of the knee: a randomized controlled clinical trial. Isokinetics and Exercise Science 2010;18:201‐9. [Google Scholar]
- Schilke JM, Johnson GO, Housh TJ, O'Dell JR. Effects of muscle‐strength training on the functional status of patients with osteoarthritis of the knee joint. Nursing Research 1996;45:68‐72. [DOI] [PubMed] [Google Scholar]
- Sekir U, Gur H. A multi‐station proprioceptive exercise program in patients with bilateral knee osteoarthrosis: functional capacity, pain and sensoriomotor function. A randomized controlled trial. Journal of Sports Science and Medicine 2005;4:590‐603. [PMC free article] [PubMed] [Google Scholar]
- Shakoor MA, Taslim MA, Hossain MS. Effects of activity modification on the patients with osteoarthritis of the knee. Bangladesh Medical Research Council Bulletin 2007;33:55‐9. [DOI] [PubMed] [Google Scholar]
- Silva LE, Valim V, Pessanha AP, Oliveira LM, Myamoto S, Jones A. Hydrotherapy versus conventional land‐based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Physical Therapy 2008;88:12‐21. [DOI] [PubMed] [Google Scholar]
- Simao AP, Avelar NC, Tossige‐Gomes R, Neves CD, Mendonca VA, Miranda AS. Functional performance and inflammatory cytokines after squat exercises and whole‐body vibration in elderly individuals with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation 2012;93:1692‐700. [DOI] [PubMed] [Google Scholar]
- Song R, Lee EO, Lam P, Bae SC. Effects of Tai Chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. Journal of Rheumatology 2003;30:2039‐44. [PubMed] [Google Scholar]
- Stoneman PD. Effect of Manual Therapy and Exercise on Pain, Stiffness and Function in Persons with Knee Osteoarthritis. Dissertation2001.
- Tak E, Staats P, Van Hespen, A, Hopman‐Rock M. The effects of an exercise program for older adults with osteoarthritis of the hip. Journal of Rheumatology 2005;32:1106‐13. [PubMed] [Google Scholar]
- Talbot LA, Gaines JM, Huynh TN, Metter EJ. A home‐based pedometer‐driven walking program to increase physical activity in older adults with osteoarthritis of the knee: a preliminary study. Journal of the American Geriatrics Society 2003;51:387‐92. [DOI] [PubMed] [Google Scholar]
- Thomas KS, Muir KR, Doherty M, Jones AC, O'Reilly SC, Bassey EJ, et al. Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ 2002;325:752‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorstensson CA, Roos EM, Petersson IF, Ekdahl C. Six‐week high‐intensity exercise program for middle‐aged patients with knee osteoarthritis: a randomized controlled trial. BMC Musculoskeletal Disorders 2005;6:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp R, Woolley S, Hornyak J, Khuder S, Kahaleh B. The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Archives of Physical Medicine and Rehabilitation 2002;83:1187‐95. [DOI] [PubMed] [Google Scholar]
- Baar ME, Dekker J, Oostendorp R, Bijl D, Voorn T. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. Journal of Rheumatology 1998;25:2432‐9. [PubMed] [Google Scholar]
- Veenhof C, Koke AJ, Dekker J, Oostendorp RA, Bijlsma JW, van Tulder, et al. Effectiveness of behavioral graded activity in patients with osteoarthritis of the hip and/or knee: a randomized clinical trial. Arthritis and Rheumatism 2006;55:925‐34. [DOI] [PubMed] [Google Scholar]
Additional references
- American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. Vol. 7, Philadelphia: Lippincott Williams and Wilkins, 2006. [Google Scholar]
- AGS. Exercise Prescription for Older Adults with Osteoarthritis Pain: Consensus Practice Recommendations. Journal of the American Geriatrics Society 2001;49:808‐823. [DOI] [PubMed] [Google Scholar]
- Altman RD, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development criteria for the classification and reporting of osteoarthritis – classification of osteoarthritis of the knee. Arthritis and Rheumatism 1986;29:1039–1049. [DOI] [PubMed] [Google Scholar]
- Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505‐514. [DOI] [PubMed] [Google Scholar]
- Arthritis Research UK. Musculoskeletal health, 2017. www.arthritisresearchuk.org/arthritis‐information/data‐and‐statistics/state‐of‐musculoskeletal‐health.aspx (accessed prior to 12 March 2018).
- Bandura A. Self‐efficacy: towards a unifying theory of behaviour change. Psychological Review 1977;84:191‐215. [DOI] [PubMed] [Google Scholar]
- Bartels Em, Lund H, Hagen KB, Dagfinrud H, Christensen R, Danneskiold‐Samsøe B. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD005523.pub2; CD005523] [DOI] [PubMed] [Google Scholar]
- Bedson J, McCarney R, Croft P. Labelling chronic illness in primary care: a good or a bad thing?. British Journal of General Practice 2004;54:932‐8. [PMC free article] [PubMed] [Google Scholar]
- Bijsterbosch J, Sharloo M, Visser AW, Watt I, Meulenbelt I, Huizinga TW, et al. Illness perceptions in patients with osteoarthritis: change over time and association with disability. Arthritis Care & Research 2009;61:1054‐61. [DOI] [PubMed] [Google Scholar]
- Boulton MR, Fitzpatrick R, Swinburn C. Qualitative research in health care II: a structured review and evaluation of studies. Journal of Evaluation of Clinical Practice 1996;2:171‐9. [DOI] [PubMed] [Google Scholar]
- Campbell R, Evans M, Tucker M, Quilty B, Dieppe P, Donovan JL. Why don't patients do their exercises? Understanding non‐compliance with physiotherapy in patients with osteoarthritis of the knee. Journal of Epidemiology and Community Health 2001;55:132‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candy B, King M, Jones L, Oliver S. Using qualitative synthesis to explore heterogeneity of complex interventions. BMC Medical Research Methodology 2011;11:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter J, Kenward M. Missing Data in Randomised Controlled Trials ‐ a Practical Guide. Birmingham (UK): National Institute for Health Research, 2008. [Google Scholar]
- Cobb AK, Hagemaster JN. Ten criteria for evaluating qualitative research proposals. Journal of Nursing Education 1987;26:138‐43. [DOI] [PubMed] [Google Scholar]
- Dawson J, Linsell L, Zondervan Z, Rose P, Carr A, Randall T, et al. Impact of persistent hip or knee pain on overall health status in elderly people: a longitudinal population study. Arthritis Care & Research 2005;53:368‐74. [DOI] [PubMed] [Google Scholar]
- Dekker J, Bott B, Woude LH, Bijlsma JW. Pain and disability in osteoarthritis: a review of biobehavioral mechanisms. Journal of Behavioral Medicine 1992;15:189‐214. [DOI] [PubMed] [Google Scholar]
- Donovan J, Blake D, Fleming W. The patient is not a blank sheet: lay beliefs and their relevance to patient education. British Journal of Rheumatology 1989;28:58‐61. [DOI] [PubMed] [Google Scholar]
- Fernandes L, Hagen KB, Bijlsma JW, Andreassen O, Christensen P, Conaghan PG, et al. EULAR recommendations for the non‐pharmacological core management of hip and knee osteoarthritis. Annals of the Rheumatic Diseases 2013;72:1125‐35. [DOI] [PubMed] [Google Scholar]
- Fisken AL, Waters DL, Hing WA, Keogh JW. Perceptions towards aqua‐based exercise among older adults with osteoarthritis who have discontinued participation in this exercise mode. Australasian Journal on Ageing 2016;35(1):12‐7. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini‐mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- Fransen M, McConnell S, Hernandez‐Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database of Systematic Reviews 2014, Issue 4. [DOI: 10.1002/14651858.CD007912.pub2; Art. No. CD007912] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fransen M, McConnell S, Harmer AR, Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2015, Issue 1. [DOI: 10.1002/14651858.CD004376.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- GRADE Working Group, McMaster University. GRADEpro. Version 3.2 for Windows. Hamilton (ON): GRADE Working Group, McMaster University, 2008.
- Griffiths C, Foster G, Ramsay J, Eldridge S, Taylor S. How effective are expert patient (lay led) education programmes for chronic disease?. BMJ 2007;334:1254‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Hawker GA, Laporte A, Croxford R, Coyte PC. The economic burden of disabling hip and knee osteoarthritis (OA) from the perspective of individuals living with this condition. Rheumatology 2005;44:1531‐7. [DOI] [PubMed] [Google Scholar]
- Hampson SE, Glasgow RE, Zeiss AM. Personal models of osteoarthritis and their relation to self‐management activities and quality of life. Journal of Behavioural Medicine 1994;17:143‐58. [DOI] [PubMed] [Google Scholar]
- Hannes K. Chapter 4: critical appraisal of qualitative research, 2011. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. Version 1 (updated August 2011). cqrmg.cochrane.org/supplemental‐handbook‐guidance (last accessed prior to 12 March 2018).
- Harden A, Garcia J, Oliver S, Rees R, Shepherd J, Brunton G, et al. Applying systematic review methods to studies of people's views: an example from public health research. Journal of Epidemiology and Community Health 2004;58:794‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawker G, Gignac M, Badley E, Davis A, French M, Li Y, et al. A longitudinal study to explain the pain‐depression link in older adults with osteoarthritis. Arthritis Care & Research 2011;63:1382‐90. [DOI] [PubMed] [Google Scholar]
- Hendry M, Williams NH, Markland D, Wilkinson C, Maddison P. Why should we exercise when our knees hurt? A qualitative study of primary care patients with osteoarthritis of the knee. Family Practice 2006;23:558‐67. [DOI] [PubMed] [Google Scholar]
- Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Sterne JA. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Hinman RS, Delany CM, Campbell PK, Gale J, Bennell KL. Physical therapists, telephone coaches, and patients with knee osteoarthritis: qualitative study about working together to promote exercise adherence. Physical Therapy 2016;96(4):479‐93. [DOI] [PubMed] [Google Scholar]
- Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt GH, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care & Research 2012;64:465‐74. [DOI] [PubMed] [Google Scholar]
- Holden MA, Nicholls EE, Hay EM, Foster NE. Physical therapists’ use of therapeutic exercise for patients with clinical knee osteoarthritis in the United Kingdom: in line with current recommendations?. Physical Therapy 2008;88:1109‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins J. 2002. Arthritis provides clinical classification criteria and management guidelines. www.hopkinsarthritis.som.jhmi.edu (accessed on May 21 2002 by Yip et al. Webpage no longer available at time of review).
- Hurley MV. The role of muscle weakness in the pathogenesis of osteoarthritis. Rheumatic Diseases Clinics of North America 1999;25:283‐98. [DOI] [PubMed] [Google Scholar]
- Hurley MV, Mitchell HL, Walsh N. In osteoarthritis, the psychosocial benefits of exercise are as important as physiological improvements. Exercise and Sports Science Review 2003;31:138‐43. [DOI] [PubMed] [Google Scholar]
- Hurley MV, Walsh NE. Effectiveness and clinical applicability of integrated rehabilitation programs for knee osteoarthritis. Current Opinion in Rheumatology 2009;21:171‐6. [DOI] [PubMed] [Google Scholar]
- Hurley M, Walsh N, Bhavnani V, Britten N, Stevenson F. Health beliefs before and after participation on an exercised‐based rehabilitation programme for chronic knee pain: doing is believing. BMC Musculoskeletal Disorders 2010;11:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley MV, Walsh NE, Mitchell H, Nicholas J, Patel A. Long‐term outcomes and costs of an integrated rehabilitation program for chronic knee pain: a pragmatic, cluster randomized, controlled trial. Arthritis Care & Research 2012;64:238‐47. [DOI] [PubMed] [Google Scholar]
- Jinks C, Jordan K, Ong BN, Croft P. A brief screening tool for knee pain in primary care (KNEST). 2. Results from a survey in the general population aged 50 and over. Rheumatology 2004;43:55‐61. [DOI] [PubMed] [Google Scholar]
- Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD005956.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta‐regression analysis of randomized controlled trials. Arthritis and Rheumatology 2014;66:622‐36. [DOI] [PubMed] [Google Scholar]
- Kavanagh J, Oliver S, Lorenc T. Reflections on developing and using PROGRESSPlus. Cochrane Health Equity Field and Campbell Equity Methods Group Equity Update. March 2008. Equity Update2008; Vol. 2, issue 1:1‐3.
- Keefe FJ, Beaupre PM, Gil KN. Group therapy for patients with chronic pain. In: Gatchel RJ, Turk DC editor(s). Psychological Approaches to Pain Management: a Practitioner's Handbook. New York (NY): Guildford Press, 1996. [Google Scholar]
- Keefe FJ, Kashikar‐Zuck S, Opiteck J, Hage E, Dalrymple L, Blumenthal JA. Pain in arthritis and musculoskeletal disorders: the role of coping skills training and exercise interventions. Journal of Orthopedics & Sports Physical Therapy 1996;24:278‐90. [DOI] [PubMed] [Google Scholar]
- Kroon FP, Burg LR, Buchbinder R, Osborne R, Johnston R, Pitt V. Self‐management education programmes for osteoarthritis. Cochrane Database of Systematic Reviews 2014, Issue 1. [DOI: 10.1002/14651858.CD008963.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larmer PJ, Reay ND, Aubert ER, Kersten P. Systematic review of guidelines for the physical management of osteoarthritis. Archives of Physical Medicine and Rehabilitation 2014;95:375‐89. [DOI] [PubMed] [Google Scholar]
- Larmer P, Kersten P, Dangan J. Patient reported benefits of hydrotherapy for arthritis. New Zealand Journal of Physiotherapy 2014;42(2):89‐93. [Google Scholar]
- Leardini G, Salaffi F, Caporali R, Canesi B, Rovati L, Montanelli R, et al. Direct and indirect costs of osteoarthritis of the knee. Clinical and Experimental Rheumatology 2004;22:699‐706. [PubMed] [Google Scholar]
- Leeuwa M, Houben RM, Severeijns R, Picavet HS, Schouten EG, Vlaeyena JW. Pain‐related fear in low back pain: a prospective study in the general population. European Journal of Pain 2007;11:256‐66. [DOI] [PubMed] [Google Scholar]
- Lorenc T, Brunton G, Oliver S, Oliver K, Oakley A. Attitudes to walking and cycling among children, young people and parents: a systematic review. Journal of Epidemiology and Community Health 2008;62:852‐7. [DOI] [PubMed] [Google Scholar]
- Main C, Watson P. Psychological aspects of pain. Manual Therapy 2002;4:203‐15. [DOI] [PubMed] [Google Scholar]
- Maly MR, Cott CA. Being careful: a grounded theory of emergent chronic knee problems. Arthritis Care & Research 2009;61:937‐43. [DOI] [PubMed] [Google Scholar]
- March LM, Bachmeier CJ. Economics of osteoarthritis: a global perspective. Bailliere's Clinical Rheumatology 1997;11:817‐34. [DOI] [PubMed] [Google Scholar]
- Mays N, Pope C. Rigor and qualitative research. BMJ 1995;311:109‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma‐Zeinstra SM, et al. OARSI guidelines for the non‐surgical management of knee osteoarthritis. Osteoarthritis and Cartilage 2014;22:363‐88. [DOI] [PubMed] [Google Scholar]
- McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle‐aged adults. Journal of Behavioral Medicine 1992;15:65‐88. [DOI] [PubMed] [Google Scholar]
- McAuley E, Lox C, Duncan TE. Long‐term maintenance of exercise, self‐efficacy, and physiological change in older adults. Journal of Gerontology (Psychological Sciences) 1993;48:218‐24. [DOI] [PubMed] [Google Scholar]
- McAuley E, Konopack JF, Morris KS, Motl RW, Hu L, Doerksen SE, et al. Physical activity and functional limitations in older women: influence of self‐efficacy. Journal of Gerontology 2006;61B:270‐7. [DOI] [PubMed] [Google Scholar]
- Miles CL, Pincus T, Carnes D, Homer KE, Taylor SJ, Bremner SA, et al. Can we identify how programmes aimed at promoting self‐management in musculoskeletal pain work and who benefits? A systematic review of sub‐group analysis within RCTs. European Journal of Pain 2011;15:775.e1‐11. [DOI] [PubMed] [Google Scholar]
- Moody J, Hale L, Waters D. Perceptions of a water‐based exercise programme to improve physical function and falls risk in older adults with lower extremity osteoarthritis: barriers, motivators and sustainability. New Zealand Journal of Physiotherapy 2012;40(2):64‐70. [Google Scholar]
- Morden A, Jinks C, Ong BN. Lay models of self‐management: how do people manage knee osteoarthritis in context?. Chronic Illness 2011;7(3):185‐200. [DOI] [PubMed] [Google Scholar]
- Newman PS, Steed L, Mulligan K. Self‐management interventions for chronic illness. Lancet 2004;364:1523‐37. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. Osteoarthritis: the care and management of osteoarthritis in adults. NICE clinical guideline 59. www.nice.org.uk/nicemedia/pdf/cg59niceguideline.pdf. Accessed prior to 12 March 2018.
- National Institute for Health and Care Excellence. Osteoarthritis: care and management in adults. NICE clinical guideline 177. www.nice.org.uk/guidance/cg177. Accessed prior to 12 March 2018.
- Oliver S, Harden A, Rees R, Shepherd J, Brunton G, Oakley A. Young people and mental health: novel methods for systematic review of research on barriers and facilitators. Health Education Research 2008;23:770‐90. [DOI] [PubMed] [Google Scholar]
- Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Annals of the Rheumatic Diseases 2001;60:91‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx BW, Rejeski WJ, Pandya J, Miller ME, Bari M, Applegate WB, et al. Exercise and depressive symptoms: a comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. Journals of Gerontology Series B: Psychological Sciences & Social Sciences 2002;57:124‐32. [DOI] [PubMed] [Google Scholar]
- Petursdottir U, Arnadottir SA, Halldorsdottir S. Facilitators and barriers to exercising among people with osteoarthritis: a phenomenological study. Physical Therapy 2010;90:1014‐25. [DOI] [PubMed] [Google Scholar]
- Phyomaung PP, Dubowitz J, Cicuttini FM, Fernando S, Wluka AE, Raaijmaakers P, et al. Are depression, anxiety and poor mental health risk factors for knee pain? A systematic review. BMC Musculoskeletal Disorders 2014;15:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisters MF, Veenhof C, Meeteren NL, Ostelo RW, Bakker DH, Schellevis FG, et al. Long‐Term effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review. Arthritis Care & Research 2007;57:1245‐53. [DOI] [PubMed] [Google Scholar]
- Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qualitative Health Research 1998;8:341‐51. [DOI] [PubMed] [Google Scholar]
- Rees R, Kavanagh J, Harden A, Shepherd J, Brunton G, Oliver S, et al. Young people and physical activity: a systematic review matching their views to effective interventions. Health Education Research 2006;21:806‐25. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Ettigner WH, Martin K, Morgan T. Treating disability in knee osteoarthritis with exercise: a central role for self‐efficacy and pain. Arthritis Care & Research 1998;11:94‐101. [DOI] [PubMed] [Google Scholar]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- Roddy E, Zhang W, Doherty M, Arden NK, Barlow J, Birrell F, et al. Evidence‐based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee ‐ the MOVE consensus. Rheumatology 2005;44:67‐73. [DOI] [PubMed] [Google Scholar]
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JP, Green S, editor(s), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Smith TO, Purdy R, Lister S, Salter C, Fleetcroft R, Conaghan PG. Attitudes of people with osteoarthritis towards their conservative management: a systematic review and meta‐ethnography. Rheumatology International 2014;34:299‐313. [DOI] [PubMed] [Google Scholar]
- Smith TO, Purdy R, Lister S, Salter C, Fleetcroft R, Conaghan P. Living with osteoarthritis: a systematic review and meta‐ethnography. Scandinavian Journal of Rheumatology 2014;43:441‐52. [DOI] [PubMed] [Google Scholar]
- Sterne JA, Harbord RM. Funnel plots in meta‐analysis. Stata Journal 2004;4(2):127‐41. [Google Scholar]
- Stone RC, Baker J. Painful choices: a qualitative exploration of facilitators and barriers to active lifestyles among adults with osteoarthritis. Journal of Applied Gerontology 2015;36(9):1091‐116. [DOI: 10.1177/0733464815602114] [DOI] [PubMed] [Google Scholar]
- Stretton CM, Latham NK, Carter KN, Lee AC, Anderson CS. Determinants of physical health in frail older people: the importance of self efficacy. Clinical Rehabilitation 2005;20:357‐66. [DOI] [PubMed] [Google Scholar]
- Taylor AH, Cable NT, Faulkner G, Hillsdon M, Narici M, Bij AK. Physical activity and older adults: a review of health benefits and the effectiveness of interventions. Journal of Sports Science 2004;22:703‐25. [DOI] [PubMed] [Google Scholar]
- Thomas J, Harden A, Oakley A, Oliver S, Sutcliffe K, Rees R, et al. Integrating qualitative research with trials in systematic reviews. BMJ 2004;328:1010‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorstensson CA, Roos EM, Petersson IF, Arvidsson B. How do middle‐aged patients conceive exercise as a form of treatment for knee osteoarthritis?. Disability and Rehabilitation 2006;28(1):51‐9. [DOI] [PubMed] [Google Scholar]
- Turk DC. Biopsychosocial perspectives on chronic pain. Psychological Approaches to Pain Management: a Practitioner's Handbook. New York (NY): Guildford Press, 1996. [Google Scholar]
- Underwood M. Community management of knee pain in older people: is knee pain the new back pain?. Rheumatology 2004;43:2‐3. [DOI] [PubMed] [Google Scholar]
- Uthman OA, Windt DA, Jordan JL, Dziedzic KS, Healey EL, Peat GM, et al. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta‐analysis. BMJ 2013;347:f5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baar ME, Dekker J, Lemmens JA, Oostendorp RA, Bijlsma JW. Pain and disability in patients with osteoarthritis of hip or knee: the relationship with articular, kinesiological, and psychological characteristics. Journal of Rheumatology 1998;25:125‐33. [PubMed] [Google Scholar]
- Veenhof C, Hasselt TJ, Koke AJ, Dekker J, Bijlsma JW, Ende CH. Active involvement and long‐term goals influence long‐term adherence to behavioural graded activity in patients with osteoarthritis: a qualitative study. Australian Journal of Physiotherapy 2006;52(4):273‐8. [DOI] [PubMed] [Google Scholar]
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990‐2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh NE, Hurley MV. Evidence based guidelines and current practice for physiotherapy management of knee osteoarthritis. Musculoskeletal Care 2009;7:45‐56. [DOI] [PubMed] [Google Scholar]
- Division of Mental Health and Prevention of Substance Abuse, World Health Organization. WHOQOL measuring quality of life. www.who.int/mental_health/media/68.pdf (accessed prior to 12 March 2018).
- Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bulletin of the World Health Organization 2003;81:646‐56. [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis. Part II: OARSI evidence‐based, expert consensus guidelines. Osteoarthritis and Cartilage 2008;16:137‐62. [DOI] [PubMed] [Google Scholar]


