Abstract
Background
Childbirth may cause the most severe pain some women experience in their lifetime. Epidural analgesia is an effective form of pain relief during labour and is considered to be the reference standard. Traditionally epidural analgesia has been delivered as a continuous infusion via a catheter in the epidural space, with or without the ability for the patient to supplement the analgesia received by activating a programmable pump to deliver additional top‐up doses, known as patient‐controlled epidural analgesia (PCEA). There has been interest in delivering maintenance analgesic medication via bolus dosing (automated mandatory bolus ‐ AMB) instead of the traditional continuous basal infusion (BI); recent randomized controlled trials (RCTs) have shown that the AMB technique leads to improved analgesia and maternal satisfaction.
Objectives
To assess the effects of automated mandatory bolus versus basal infusion for maintaining epidural analgesia in labour.
Search methods
We searched CENTRAL, MEDLINE, Embase, the World Health Organization International Clinial Trials Registry Platform (WHO‐ICTRP) and ClinicalTrials.gov on 16 January 2018. We screened the reference lists of all eligible trials and reviews. We also contacted authors of included studies in this field in order to identify unpublished research and trials still underway, and we screened the reference lists of the included articles for potentially relevant articles.
Selection criteria
We included all RCTs that compared the use of bolus dosing AMB with continuous BI for providing pain relief during epidural analgesia for labour in women.
Data collection and analysis
We used the standard methodological procedures expected by Cochrane. Our primary outcomes were: risk of breakthrough pain with the need for anaesthetic intervention; risk of caesarean delivery; risk of instrumental delivery. Secondary outcomes included: duration of labour; local anaesthetic consumption. We used GRADE to assess the certainty of evidence for each outcome.
Main results
We included 12 studies with a total of 1121 women. Ten studies enrolled healthy nulliparous women only and two studies enrolled healthy parous women at term as well. All studies excluded women with complicated pregnancies. There were variations in the technique of initiation of epidural analgesia. Seven studies utilized the combined spinal epidural (CSE) technique, and the other five studies only placed an epidural catheter without any intrathecal injection. Seven studies utilized ropivacaine: six with fentanyl and one with sufentanil. Two studies used levobupivacaine: one with sufentanil and one with fentanyl. Three used bupivacaine with or without fentanyl. The overall risk of bias of the studies was low.
AMB probably reduces the risk of breakthrough pain compared with BI for maintaining epidural analgesia for labour (from 33% to 20%; risk ratio (RR) 0.60; 95% confidence interval (CI) 0.39 to 0.92, 10 studies, 797 women, moderate‐certainty evidence). AMB may make little or no difference to the risk of caesarean delivery compared to BI (15% and 16% respectively; RR 0.92; 95% CI 0.70 to 1.21, 11 studies, 1079 women, low‐certainty evidence).
AMB may make little or no difference in the risk of instrumental delivery compared to BI (12% and 9% respectively; RR 0.75; 95% CI 0.54 to 1.06, 11 studies, 1079 women, low‐certainty evidence). There is probably little or no difference in the mean duration of labour with AMB compared to BI (mean difference (MD) −10.38 min; 95% CI −26.73 to 5.96, 11 studies, 1079 women, moderate‐certainty evidence). There is probably a reduction in the hourly consumption of local anaesthetic with AMB compared to BI for maintaining epidural analgesia during labour (MD −1.08 mg/h; 95% CI −1.78 to −0.38, 12 studies, 1121 women, moderate‐certainty evidence). Five out of seven studies reported an increase in maternal satisfaction with AMB compared to BI for maintaining epidural analgesia for labour; however, we did not pool these data due to their ordinal nature. Seven studies reported Apgar scores, though there was significant heterogeneity in reporting. None of the studies showed any significant difference between Apgar scores between groups.
Authors' conclusions
There is predominantly moderate‐certainty evidence that AMB is similar to BI for maintaining epidural analgesia for labour for all measured outcomes and may have the benefit of decreasing the risk of breakthrough pain and improving maternal satisfaction while decreasing the amount of local anaesthetic needed.
Plain language summary
Epidural with intermittent (automated mandatory bolus) versus constant delivery (basal infusion) for maintaining pain relief in childbirth
Background
Epidural analgesia involves the injection of pain relieving medication into the epidural space (area just outside the spinal column). It is an effective form of pain relief during childbirth. The medication is usually given via a programmable pump that injects the medication through a small tube positioned in the epidural space. Traditionally the medication was delivered at a constant rate known as a 'basal infusion'. Recently there has been interest in delivering the medication as an intermittent dose (every now and again) instead. This so‐called 'bolus dosing', or 'automated mandatory bolus', may be better for pain relief. This study reviewed the evidence regarding two interventions for maintaining epidural analgesia in childbirth: automated mandatory bolus and basal infusion.
Study characteristics
The evidence is current to January 2018. We found 12 studies involving 1121 women with uncomplicated pregnancies. We did not specifically assess the impact of the funding sources on the studies. The people taking part in the trials we looked for (known as randomized controlled trials) are randomly assigned to either the group receiving the treatment under investigation or to a group receiving standard treatment as the control. This is to reduce any bias that either the investigators or the participants of the trial may have.
Key results
We found that automated mandatory bolus decreases the risk of breakthrough pain (pain requiring medical intervention from an anaesthesiologist) compared with basal infusion during childbirth. It does this without increasing the risk of a caesarean section; the risk of instrumental delivery (whether the obstetrician intervenes to assist delivery using an obstetric forceps or vacuum device); or the duration of childbirth. It may also reduce the dose of medication required on a per hourly basis. In addition, five of seven studies found that mothers preferred the automated mandatory bolus over basal infusion.
Certainty of the evidence
The evidence was of moderate‐certainty for all the outcomes we measured, with the exception of the risk of caesarean delivery and risk of instrumental delivery, which had only low‐certainty evidence.
Summary of findings
Summary of findings for the main comparison. Automated mandatory bolus versus basal infusion for maintenance of epidural analgesia in labour.
| Automated mandatory bolus versus basal infusion for maintenance of epidural analgesia in labour | |||||
| Patient or population: maintenance of epidural analgesia in labour Setting: patients admitted into the labour ward Intervention: automated mandatory bolus Comparison: basal infusion | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with basal infusion | Risk with automated mandatory bolus | ||||
| Breakthrough pain assessed with: verbal patient reporting or need for rescue analgesia Follow‐up: range 242 min to 490 min | Study population | RR 0.60 (0.39 to 0.92) | 797 (10 RCTs) | ⊕⊕⊕⊝ Moderatea | |
| 333 per 1000 | 200 per 1000 (130 to 307) | ||||
| Caesarean delivery Follow‐up: range 242 min to 490 min | Study population | RR 0.92 (0.70 to 1.21) | 1079 (11 RCTs) | ⊕⊕⊝⊝ Lowb | |
| 160 per 1000 | 147 per 1000 (112 to 194) | ||||
| Instrumental delivery Follow‐up: range 242 min to 490 min | Study population | RR 0.75 (0.54 to 1.06) | 1079 (11 RCTs) | ⊕⊕⊝⊝ Lowb | |
| 123 per 1000 | 92 per 1000 (66 to 130) | ||||
| Duration of labour in min Follow‐up: range 242 min to 490 min | The mean duration of labour in min ranged from 186.3 to 690.0 min | MD 10.38 min lower (26.73 lower to 5.96 higher) | — | 1079 (11 RCTs) | ⊕⊕⊕⊝ Moderatec |
| LA consumption per hour Follow‐up: range 242 min to 490 min | The mean LA consumption per hour ranged from 3 mg to 21.4 mg | MD 1.08 mg/h lower (1.78 lower to 0.38 lower) | — | 1121 (12 RCTs) | ⊕⊕⊕⊝ Moderated |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aDowngraded one level due to considerable statistical heterogeneity for this outcome, i.e. I2 = 69%. bDowngraded two levels because the upper and lower confidence limit cross the effect size of 5% in either direction and there is inadequate information given the small numbers. cDowngraded one level because the upper and lower confidence limit cross the effect size of 0.5 in either direction. dDowngraded one level due to considerable statistical inconsistency for this outcome, i.e. I2 = 89%.
Background
Description of the condition
Labour is arguably one of the most painful experiences a woman can undergo in her lifetime. The pain experienced during labour is affected by psychosocial influences, pain experiences and obstetric interventions, such as oxytocin augmentation. Epidural analgesia is considered to be the reference standard for labour analgesia and is often preferable to other modes of pain relief such as systemic opioids, nitrous oxide and non‐pharmacological methods. It is a common anaesthetic technique whereby women receive injections of local anaesthetics or opioids in the epidural space to cause numbness and weakness in the lower part of the body, providing pain relief during labour. Women most commonly receive long‐acting local anaesthetics like bupivacaine and ropivacaine. Opioids such as fentanyl and sufentanil are routinely co‐administered to supplement the effects of the local anaesthetics.
Description of the intervention
Two techniques are used to maintain epidural analgesia during labour: automated mandatory boluses and basal infusion. The initial bolus is given as an epidural or combined spinal epidural dose administration. Automated mandatory bolus is a drug delivery technique in which the dose is delivered intermittently in a bolus. Basal infusion is a drug delivery technique in which the dose is delivered continuously. Drug delivery by automated mandatory bolus results in a higher injectate pressure (pressure when injecting the medication) compared to basal infusion; the difference in the delivery technique is believed to affect the spread and distribution of the drug in the epidural space after administration. A greater spread and distribution in the epidural space may provide effective pain relief and produce lower risk of motor blockade.
Patient‐controlled epidural analgesia (PCEA) has been established as a preferred mode of epidural drug delivery since its introduction by Gambling in 1988 (Gambling 1988). The PCEA technique allows patient‐initiated activation of a bolus of pain medication to treat labour pain. In comparison with continuous epidural infusion, studies have shown that PCEA decreases breakthrough pain requiring anaesthetic intervention, reduces local anaesthetic consumption without compromising analgesic efficacy and increases patient satisfaction by allowing the patient autonomy during labour. PCEA is commonly administered with a basal infusion in addition to boluses on patient demand.
How the intervention might work
Cadaveric and experimental models have suggested that epidural medications given as boluses may lead to wider and more uniform spread of the drugs in the epidural space (Hogan 2002; Kaynar 1999). Hogan found that the spread of liquids in the epidural space is highly non‐uniform, through multiple small channels, and suggested that the spread would be most uniform when using large volumes and a correspondingly high injectate pressure near the site of injection to engage the most channels (Hogan 2002). Kaynar and Shankar's experimental model used a multi‐orifice epidural catheter with bolus or continuous infusion delivery (Kaynar 1999). The bolus technique resulted in a wider and more uniform spread of contrast agent, whilst the continuous infusion resulted in smaller spread that was exclusively through the proximal port of the epidural catheter.
Several trials have shown that the automated mandatory bolus technique appears to reduce breakthrough pain and increase patient satisfaction during epidural labour analgesia, due to a more uniform spread in the epidural space (Fettes 2006; Lim 2005; Sia 2013; Wong 2006). The two modes of epidural drug delivery differ in the injectate pressure generated during drug delivery, although the total amount of drug may be similar (e.g. the amount of drug in one hour).
Why it is important to do this review
In the development of epidural analgesia, several trials have compared maintenance of epidural analgesia using automated mandatory boluses with basal infusion, but none have conclusively shown one technique to be superior to the other (Capogna 2011; Chua 2004; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006). Chua and Sia performed the first clinical trial that showed that the bolus technique increased the duration and quality of pain relief during epidural analgesia in 42 nulliparous labouring women (Chua 2004). Several studies have found that automated mandatory boluses may reduce breakthrough pain (having pain despite being on epidural medication that requires the anaesthetist to give additional pain medication) when compared with continuous infusion (Ferrer 2017; Fettes 2006; Lim 2005; Sia 2013; Wong 2006), whilst others have not observed any difference between the two techniques (Capogna 2011; Leo 2010; Lim 2010; Salim 2005; Sia 2007). There may also be the potential that automated mandatory bolus may decrease the risk and/or degree of motor block, which may lead to a decrease in instrumental vaginal delivery and increased maternal satisfaction (Capogna 2011).
Presently there is no clear evidence whether this new technology of delivery of anaesthetics is superior to the current practice. We considered the anaesthetic, obstetric and foetal outcomes relevant to women and side effects of the treatments, including risk of breakthrough pain, caesarean delivery, instrumental birth, local anaesthetic consumption and duration of labour. If one intervention was found to be more effective or safer, or resulted in a decrease in the total drug used, the practice of epidural drug delivery could be more standardized for epidural analgesia in labour.
Objectives
To assess the effects of automated mandatory bolus versus basal infusion for maintaining epidural analgesia in labour.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel‐group randomized controlled trials (RCTs) that compared the use of automated mandatory bolus with basal infusion for providing epidural analgesia pain relief during labour in women. We included studies irrespective of language and publication date and type. We included studies with and without a patient‐controlled epidural analgesia (PCEA) component.
We excluded non‐randomized studies such as cohort studies because of their increased risk of bias. We also excluded cross‐over trials, as this methodology is not appropriate for evaluating interventions that are administered at a specific time point. We excluded studies with combined automated mandatory boluses and basal infusion. We also excluded studies that did not use automated administration of bolus doses.
Types of participants
We included studies that recruited pregnant term women requesting epidural analgesia during labour.
We excluded studies that recruited women in preterm labour, with multiple pregnancy or malposition of fetus including breech presentations.
Types of interventions
We included studies that compared the use of automated intermittent mandatory boluses to basal infusion for maintaining epidural analgesia in labour. We included all local anaesthetics, with or without opioid maintenance regimens, administered during the epidural analgesia.
We excluded parturients (pregnant women who undergo labour) who received an intrathecal or spinal catheter for pain relief during labour. We excluded studies that utilized manually delivered boluses.
Types of outcome measures
Primary outcomes
Risk of breakthrough pain with the need for anaesthetic intervention (dichotomous)
Risk of caesarean delivery (dichotomous) (safety outcome)
Risk of instrumental delivery (dichotomous) (safety outcome)
Secondary outcomes
Duration of labour analgesia (continuous)
Local anaesthetic consumption per hour (continuous)
Maternal satisfaction (short ordinal scale)
Apgar scores (continuous): measured by Apgar score scale (safety outcome)
We considered the minimally important difference for risk of breakthrough pain, risk of caesarean delivery and risk of instrumental delivery when comparing automated mandatory bolus with basal infusion to be 5% for each outcome.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; 2018, Issue 1); MEDLINE (January 1966 to 16 January 2018) and Embase (January 1980 to 16 January 2018). We also searched the World Health Organization International Clinial Trials Registry Platform (WHO‐ICTRP) (August 2005 to 16 January 2018), and clinicaltrials.gov (February 2000 to 16 January 2018). Appendix 1 describes our search strategies for CENTRAL, MEDLINE, Embase, WHO‐ICTRP and clinicaltrials.gov.
We searched the Cochrane Pregnancy and Childbirth Group Trials Register with the Highly Sensitive Search Strategy (HSSS) found in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), with the help of their Trials Search Co‐ordinator. In addition, we screened the bibliography of included studies to identify potentially eligible records. We did not place any language restrictions on our searches.
Searching other resources
We used free‐text terms in all databases and subject headings in combination when thesauri were a component of a database.
We reviewed the 'Related articles' feature of PubMed for all eligible trials and reviews.
We screened the reference lists of all eligible trials and reviews.
We also contacted authors of included studies in this field in order to identify unpublished research and trials still underway on 8 July 2016. We screened the reference lists of the included articles for potentially relevant articles.
Data collection and analysis
Two authors (LWL, OTT) independently collected data on a standardized data collection form (see Appendix 2), and a third author (SBL) resolved any remaining disagreements through discussion.
Selection of studies
Two authors (LWL, OTT) independently assessed for inclusion all the potential studies we identified as a result of the search strategy (Criteria for considering studies for this review) and reviewed the titles and abstracts from the searches.
Data extraction and management
Two authors (LWL, OTT) independently extracted the data using a standardized form (see Appendix 2). We extracted information pertaining to the study design, method of randomization, use of allocation concealment, reporting of the study setting and participants, inclusion and exclusion criteria, sample size, interventions and outcomes. Two authors (SBL, FJS) entered and checked the data independently, and a third author (PNA) resolved disagreements.
Assessment of risk of bias in included studies
Two authors (LWL, OTT) independently assessed trial quality and risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and a third author (SBL) resolved any disagreements.
Based on the Cochrane 'Risk of bias' tool in Review Manager 5 (RevMan 5) (RevMan 2014), we considered the following domains (Higgins 2011): random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. Appendix 3 presents the details on the Cochrane 'Risk of bias' tool and criteria for judgment.
We graded each of the above dimensions of trial quality as being at low, high or unclear risk of bias. Given the low risk of bias for all studies and high quality of evidence for each outcome, we did not conduct a stratified analysis based on study quality.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio (RR) with 95% confidence intervals (CIs).
Continuous data
For continuous data, we used the mean difference (MD) if trials measured the outcomes in the same way. We planned to use the standardized mean difference (SMD) to obtain pooled estimates of an outcome measured on different scales.
Unit of analysis issues
The woman was the unit of analysis in all of the studies.
Dealing with missing data
We attempted to contact the study authors if key information was unavailable in the publications.
Assessment of heterogeneity
We evaluated clinical heterogeneity by qualitatively appraising differences in study characteristics such as participants, interventions, outcomes assessed and study methodology. Quantitative pooling of the data was first justified by a consensus clinical judgement of sufficient clinical homogeneity. We informally evaluated and investigated the degree of statistical heterogeneity by visual inspection of forest plots and more formally by using the Tau2, I2 and Chi2 statistics. We regarded heterogeneity as considerable if I2 was greater than 75%, substantial if I2 was between 50% and 90%, moderate if I2 was between 30% and 60%, and low if I2 was less than 40%.
Assessment of reporting biases
We checked the methodology and study protocols of the primary studies where available. We assessed publication bias and other small study effects in a qualitative manner using a funnel plot.
In future updates of this review, we will test for funnel plot asymmetry using weighted linear regression of effect estimates on their standard error if more than 10 trials are included (Egger 1997).
Data synthesis
We carried out statistical analyses using RevMan 2014. For data synthesis of dichotomous outcomes, we used the Mantel‐Haenszel method and reported the RRs and 95% CIs. For continuous outcomes we used the inverse variance method. We analysed maternal satisfaction as a continuous outcome, even if measured on ordinal scales. Some studies administered ropivacaine or levobupivacaine local anaesthesia in place of bupivacaine. For such studies we assumed 60% potency of bupivacaine based on a similar systematic review and meta‐analysis (George 2012). Hence we multiplied the means and standard deviations by 0.6. We used the RR to report pooled results for dichotomous outcomes. We used MDs to pool the results of the continuous outcomes. Where studies reported medians and interquartile ranges, we obtained the means and standard deviations (SD) from George 2012, we converted them using the formula by Hozo 2005, or we excluded them from the meta‐analysis and reported results qualitatively.
We expected both clinical and statistical heterogeneity, and therefore we used the random‐effects model to meta‐analyse all outcomes.
Subgroup analysis and investigation of heterogeneity
We performed the following subgroup analysis for all the outcomes.
Local anaesthetic alone versus local anaesthetic plus opioid regimens.
Epidural technique: epidural alone versus combined spinal‐epidural technique.
PCEA: regimens that used PCEA versus those that did not.
Sensitivity analysis
We did not perform sensitivity analyses because the quality of the studies was consistent across the different studies (Risk of bias in included studies).
We will consider performing sensitivity analysis in future updates of this review if required.
Sensitivity analysis for trial quality involves analysis based on rating of selection bias and attrition bias. We would exclude studies of poor quality from the analysis (those rated as unclear or high risk of bias) in order to assess for any substantive difference to the overall result. The sensitivity analysis for compliance would be based on trials where women did not receive their allocated treatment, combination therapy or intervention, or they received an additional form of analgesia to the one allocated. These sensitivity analyses will use only the primary outcomes.
'Summary of findings' table
We used the principles of the GRADE system in order to assess the certainty of the body of evidence associated with the following specific outcomes (Guyatt 2008).
Risk of breakthrough pain requiring anaesthetic intervention.
Risk of caesarean delivery.
Risk of instrumental delivery.
Duration of labour analgesia.
Total dose of local anaesthetic per hour.
We constructed a 'Summary of findings' table comparing automated mandatory bolus versus basal infusion therapy using GRADEpro software (GRADEpro GDT 2015). The GRADE approach assesses the certainty of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. Assessment of the certainty of a body of evidence involved considering the methodological quality of studies, the directness of the evidence, the heterogeneity of the data, the precision of the effect estimates and the risk of publication bias.
Results
Description of studies
Results of the search
See Figure 1.
1.
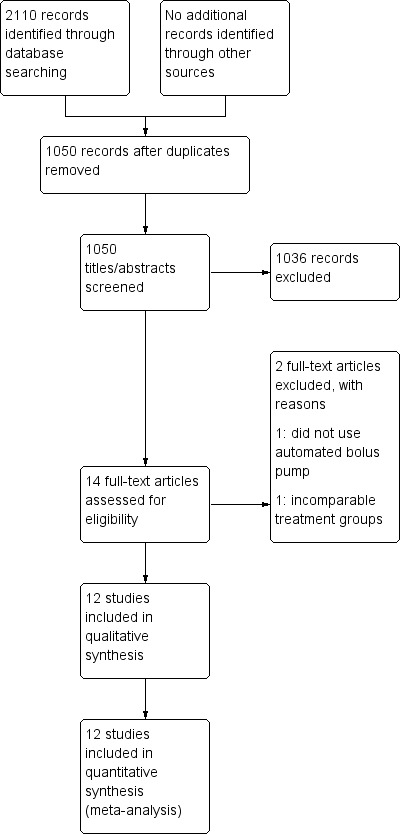
Study flow diagram.
We identified 2110 citations from the database searches. After screening by title and abstract, we obtained full text articles for 14 citations that we judged as potentially eligible for inclusion in the review. After excluding one study that did not use an automated bolus pump as their intervention and one study that utilized varying concentrations and volumes of local anaesthetic (rendering the different groups incomparable), we finally included 12 studies in our review.
Included studies
Characteristics of included studies
We included 12 studies involving 1121 women. Ten of the 12 studies enrolled healthy nulliparous women (Capogna 2011; Chua 2004; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013), while two studies enrolled healthy parous women at term (Ferrer 2017; Wong 2006). Ten studies involved women with singleton fetus in vertex presentation, while two studies did not specify the fetal position (Ferrer 2017; Lin 2016). All studies excluded women with complicated pregnancies.
All 12 studies reported the local anaesthetic consumption (either as total consumed or per hour consumption). The other outcomes included breakthrough pain, number of women who underwent caesarean delivery, number of women who underwent instrumental birth, duration of labour (total or first and second stage) and Apgar scores.
There were variations in the technique of initiation of epidural analgesia. Seven studies used the combined spinal epidural (CSE) technique (Chua 2004; Leo 2010; Lim 2005; Lim 2010; Sia 2007; Sia 2013; Wong 2006), with two of these studies giving only an opioid (fentanyl in both) without any local anaesthetic intrathecally (Chua 2004; Lim 2005). The other five studies only placed an epidural catheter without any intrathecal injection (Capogna 2011; Ferrer 2017; Fettes 2006; Lin 2016; Salim 2005).
There was also variation with the analgesic medications given in terms of the choice of drugs as well as the dosages. Six studies utilized ropivacaine with fentanyl (Chua 2004; Fettes 2006; Leo 2010; Lim 2010; Sia 2007; Sia 2013), one used ropivacaine with sufentanil (Lin 2016). Two studies utilized levobupivacaine: Capogna 2011 with sufentanil and Lim 2005 with fentanyl, and three studies utilized bupivacaine with or without fentanyl (Ferrer 2017; Salim 2005; Wong 2006).
In one study, the analgesic medication provided differed between the two groups, with the AMB group receiving bupivacaine only and the BI group receiving bupivacaine plus fentanyl (Salim 2005).
Excluded studies
We excluded two studies in total. One study did not use automated mandatory boluses but rather manual intermittent boluses (Patkar 2015). In the other, the interventions between the groups were not comparable: the continuous infusion group received half the volume of local anaesthetic as the AMB group, and there were two different concentrations of local anaesthetic administered to the two different AMB groups (Nunes 2014).
See Characteristics of excluded studies.
Studies awaiting classification
There are no studies awaiting classification.
Ongoing studies
We identified no ongoing studies.
Risk of bias in included studies
2.
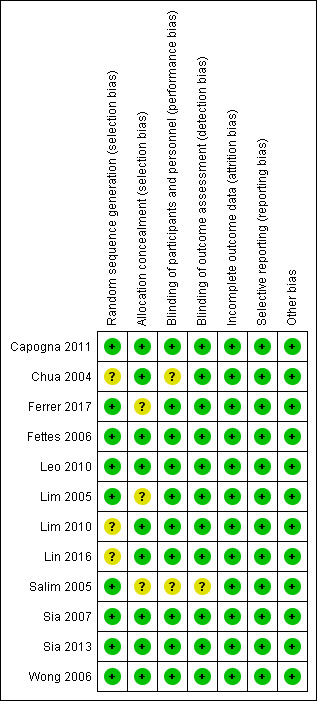
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
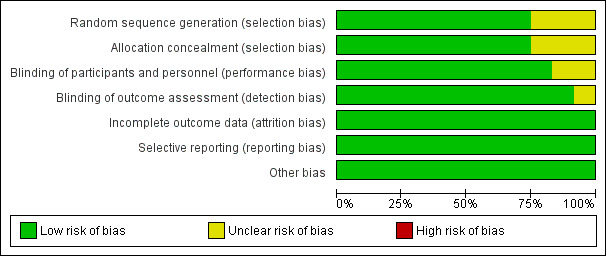
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Overall, there was low risk of selection, performance, detection, attrition and reporting bias, and no overt sources of other potential biases in the included studies. For allocation bias, 6 of the 12 studies reported the methods for both randomization and allocation (computer‐generated random numbers and sealed opaque envelopes respectively). Three studies reported using a computer‐generated randomization sequence but no allocation concealment (Ferrer 2017; Lim 2005; Salim 2005), and three studies reported using sealed opaque envelopes for allocation concealment but no randomization (Chua 2004; Lim 2010; Lin 2016). For performance and detection bias, 10 studies were double‐blinded and provided a description of the blinding, while one study did not report any blinding (Salim 2005), and one study was single‐blinded (Ferrer 2017). Apart from Lim 2005, no studies specifically mentioned performing an intention‐to‐treat analysis. All studies reported prespecified outcomes and had minimal missing data (< 10%). We therefore judged them to be at low risk of attrition and reporting bias.
Allocation
Nine studies utilized computer‐generated random numbers for randomization (Capogna 2011; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2010; Salim 2005; Sia 2007; Sia 2013; Wong 2006). We judged these studies to be at low risk for selection bias (random sequence generation). Three studies did not describe the method of randomization (Chua 2004; Lim 2010; Lin 2016). We judged these studies as being at unclear risk of selection bias (random sequence generation).
Nine studies utilized sealed opaque envelopes for allocation (Capogna 2011; Chua 2004; Fettes 2006; Leo 2010; Lim 2010; Lin 2016; Sia 2007; Sia 2013; Wong 2006). We judged these studies as being at low risk of selection bias (allocation concealment). Three studies did not describe the method of allocation concealment (Ferrer 2017; Lim 2005; Salim 2005). Although Ferrer 2017 and Salim 2005 did state that the allocation was concealed, we judged these studies to be at unclear risk of selection bias (allocation concealment) because the method of allocation concealment was not described.
Blinding
Ten studies were double‐blinded and provided a description of the blinding (Capogna 2011; Chua 2004; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Sia 2007; Sia 2013; Wong 2006). The principal investigator performed one of these blocks in one study, but a blinded anaesthetist handled subsequent data collection (Chua 2004). We judged these studies to be at low risk of performance bias except for Chua 2004, which we judged to be at unclear risk for performance bias.
One study described itself as single‐blinded, although the research assistant and the nurse staff in charge of drug administration were the only ones that knew the randomization sequence. Neither the participant nor the attending anaesthesiologist or the outcome assessor knew the randomization sequence (Ferrer 2017), so we judged it to be at low risk. One study did not describe blinding (Salim 2005), so we judged this study to be at unclear risk of performance and detection bias.
Incomplete outcome data
All 12 studies had a low risk of attrition bias, reporting all outcome data (recruitment and attrition data) with no missing data. We performed the analyses using the intention‐to‐treat principle (Capogna 2011; Chua 2004; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006). We judged all studies to be at low risk of attrition bias.
Selective reporting
All 12 studies reported all prespecified outcomes, and we judged them to be at low risk for reporting bias (Capogna 2011; Chua 2004; Fettes 2006; Ferrer 2017; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006). The funnel plot also suggested no reporting bias (Figure 4).
4.
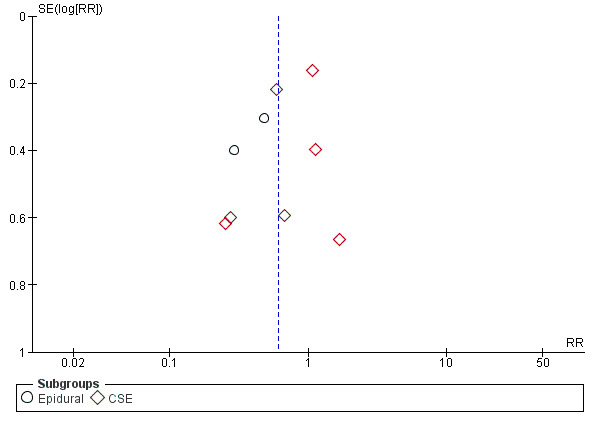
Funnel plot of comparison: 1 Automated mandatory bolus vs basal infusion, outcome: 1.2 Breakthrough pain (epidural vs CSE).
Other potential sources of bias
We judged all 12 studies to be at low risk for other bias (Capogna 2011; Chua 2004; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006).
Effects of interventions
See: Table 1
See Table 1.
Primary outcomes
1. Risk of breakthrough pain
Ten studies in 797 women reported the incidence of breakthrough pain (Capogna 2011; Chua 2004; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Sia 2007; Sia 2013; Wong 2006). The pooled results showed automated mandatory bolus probably reduces the risk of breakthrough pain (RR 0.60 95%, CI −0.39 to 0.92; Analysis 1.1) compared to continuous infusion for maintaining epidural analgesia.
1.1. Analysis.
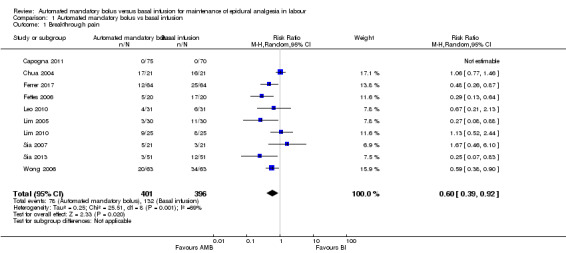
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 1 Breakthrough pain.
There was substantial heterogeneity (I2 = 69%). The overall certainty of evidence based on GRADE was moderate.
We grouped studies on the basis of the method of initiation of the epidural (epidural versus combined spinal‐epidural). For the subgroup of CSE, the automated mandatory bolus probably reduces the risk of breakthrough pain (RR 0.71, 95% CI 0.44 to 1.13, random‐effects, 7 studies, 484 participants; moderate‐certainty evidence; Analysis 1.2) compared to continuous infusion for maintenance of epidural analgesia. There was substantial heterogeneity (I2 = 64%).
1.2. Analysis.
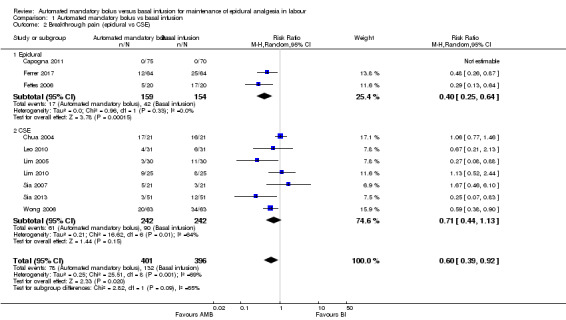
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 2 Breakthrough pain (epidural vs CSE).
2. Risk of caesarean delivery (safety outcome)
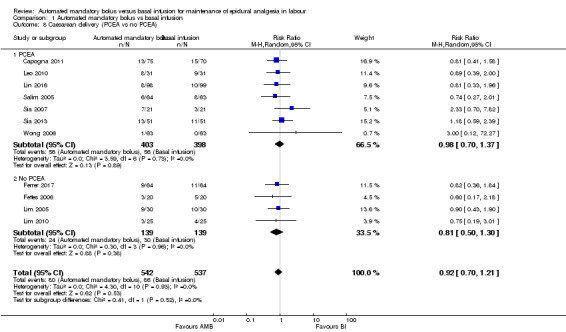
Eleven studies in 1079 women reported the incidence of caesarean delivery (Capogna 2011; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006). The pooled results showed that automated mandatory bolus may make little or no difference in the risk of caesarean delivery (RR 0.92, 95% CI 0.70 to 1.21, random‐effects; Analysis 1.5) compared with continuous infusion for maintenance of epidural analgesia. This difference was also not clinically meaningful as the risk difference did not exceed 5% (RD 0.00, 95% CI −0.03 to 0.03).
1.5. Analysis.
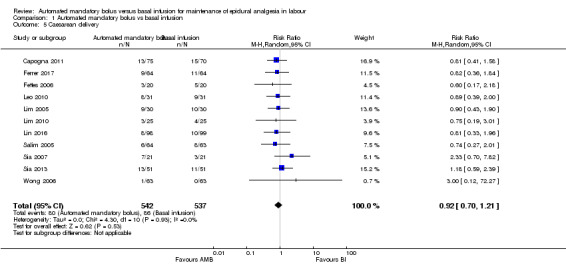
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 5 Caesarean delivery.
There was low heterogeneity (I2 = 0%). The overall certainty of the evidence based on GRADE was low.
3. Risk of instrumental delivery (safety outcome)
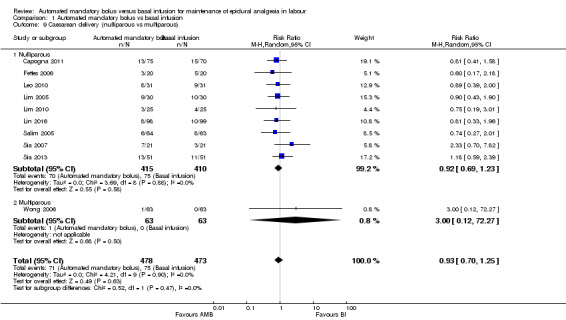
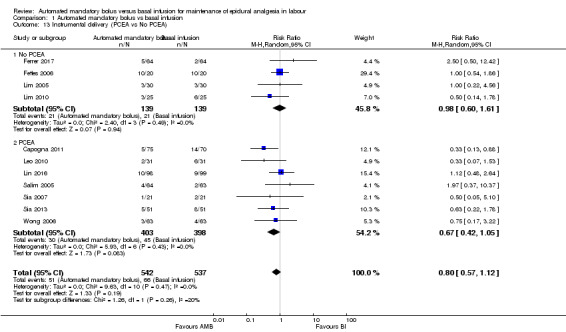
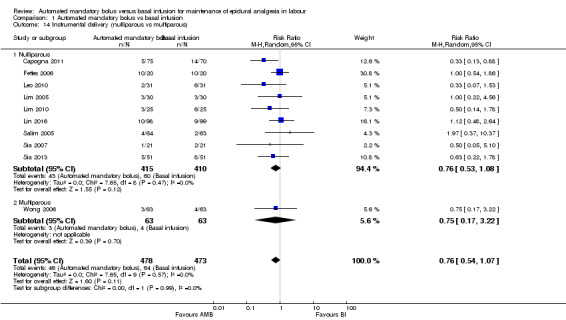
Eleven studies in 1079 women reported the incidence of instrumental delivery (Capogna 2011; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006). The pooled results showed that automated mandatory bolus may make little or no difference in the risk of instrumental delivery (RR 0.75, 95% CI 0.54 to 1.06, random‐effects; Analysis 1.10) compared with continuous infusion. The difference was also not clinically meaningful, as the risk difference did not exceed 5% difference (RD −0.03, 95% CI −0.06 to −0.01).
1.10. Analysis.
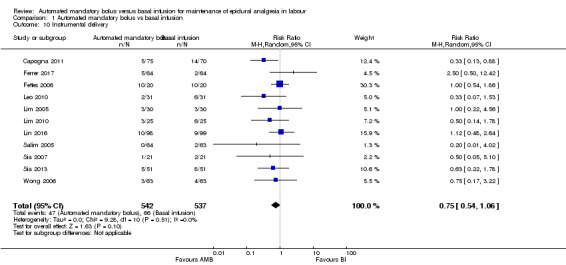
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 10 Instrumental delivery.
There was low heterogeneity (I2 = 0%). The overall certainty of the evidence based on GRADE was low .
Secondary outcomes
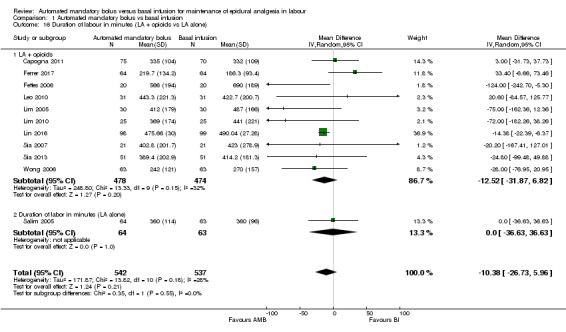
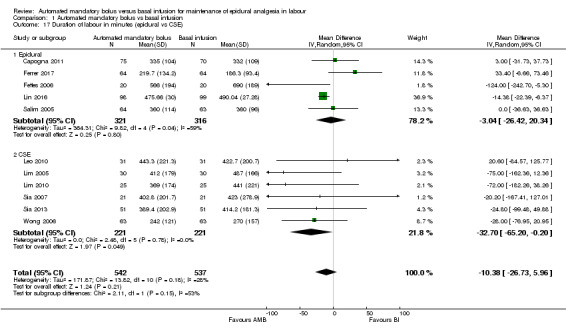
1. Duration of labour analgesia in minutes
Eleven studies in 1079 women reported the duration of labour analgesia (Capogna 2011; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006). The pooled results showed that automated mandatory bolus probably makes little or no difference in the duration of labour analgesia (MD −10.38 min, 95% CI −26.73 to 5.96, random‐effects; Analysis 1.15) compared with continuous infusion. There was low heterogeneity (I2 = 28%), and the overall certainty of the evidence based on GRADE was moderate.
1.15. Analysis.
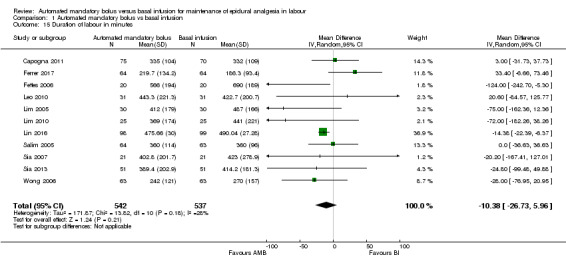
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 15 Duration of labour in minutes.
We grouped studies based on the regimen used to maintain epidural analgesia (PCEA versus no PCEA). For the subgroup that utilized PCEA, the results showed that automated mandatory bolus probably reduces the duration of labour analgesia (MD −13.24 min, 95% CI −20.71 to −5.76, random‐effects; 7 studies, 801 participants; Analysis 1.18) compared with continuous infusion for maintenance of epidural analgesia. There was low heterogeneity (I2 = 0%). For the subgroup that did not utilize PCEA, the results showed that automated mandatory bolus probably makes little or no difference in the duration of labour analgesia (MD −48.65 min, 95% CI −129.92 to 32.62, random‐effects; 4 studies, 278 participants; Analysis 1.18) compared with continuous infusion. There was substantial heterogeneity (I2 = 73%).
1.18. Analysis.
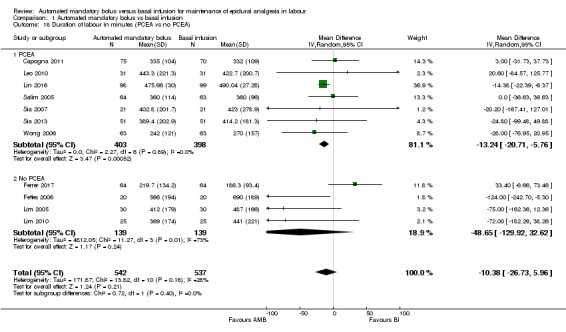
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 18 Duration of labour in minutes (PCEA vs no PCEA).
2. Local anaesthetic consumption per hour
Twelve studies in 1121 women reported the local anaesthetic consumption per hour (Capogna 2011; Chua 2004; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013; Wong 2006). We accounted for differing LAs used by various studies by converting them to bupivacaine equivalents as described in a previous study (George 2012). The pooled results showed that automated mandatory bolus probably reduces local anaesthetic consumption per hour in parturients admitted into the labour ward (MD −1.08 mg/h, 95% CI −1.78, −0.38; random‐effects; Analysis 1.20) compared to continuous infusion for maintenance of epidural analgesia. There was considerable heterogeneity (I2 = 89%). The overall certainty of the evidence based on GRADE was moderate.
1.20. Analysis.
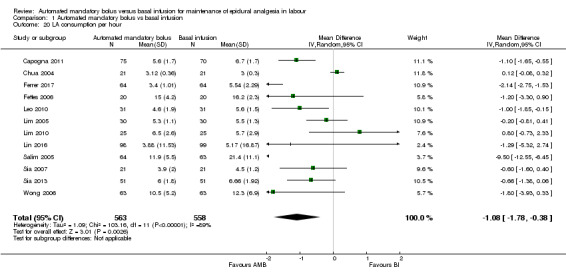
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 20 LA consumption per hour.
We grouped studies based on the regimen used to maintain epidural analgesia (PCEA versus no PCEA). For the subgroup that utilized PCEA, the results showed that automated mandatory bolus probably reduces local anaesthetic consumption per hour in parturients admitted into the labour ward (MD −1.59 mg/h, 95% CI −2.58 to −0.60, random‐effects; 7 studies, 801 participants; Analysis 1.23) as compared to continuous infusion. There was considerable heterogeneity (I2 = 81%). For the subgroup that did not utilize PCEA, the results showed that automated mandatory bolus may make little or no difference in the amount of local anaesthetic consumed per hour (MD −0.53 mg/h, 95% CI −1.58, 0.52, random‐effects; 4 studies, 278 participants; Analysis 1.23) as compared with continuous infusion for maintenance of epidural analgesia. There was high heterogeneity (I2 = 92%).
1.23. Analysis.
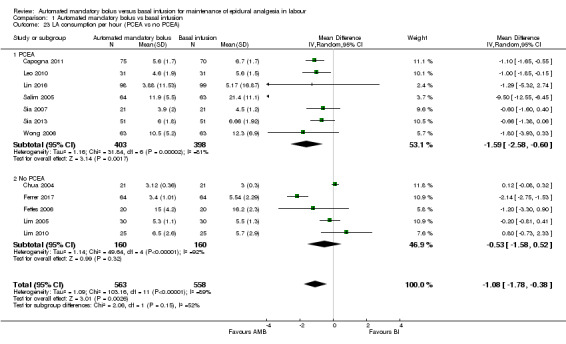
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 23 LA consumption per hour (PCEA vs no PCEA).
3. Maternal satisfaction
Seven studies in 570 women reported maternal satisfaction scores (Ferrer 2017; Leo 2010; Lim 2005; Lim 2010; Sia 2007; Sia 2013; Wong 2006). The common definition of maternal satisfaction is using a score of 0 (very dissatisfied) to 100 (very satisfied) using patient verbal reporting or a visual analogue scale (VAS) for pain as a proxy for satisfaction. As maternal satisfaction scores are ordinal in nature, we have decided to review the data qualitatively. Five studies reported increased maternal satisfaction with AMB as compared to BI (Leo 2010; Lim 2005; Lim 2010; Sia 2013; Wong 2006), while two studies found no difference in maternal satisfaction between AMB and BI (Ferrer 2017; Sia 2007).
4. Apgar scores: measured by Apgar score scale (safety outcome)
Nine studies reported Apgar scores, with one study reporting Apgar scores at 1, 5 and 10 minutes (Ferrer 2017), four studies reporting Apgar scores at 5 minutes (Leo 2010; Lim 2005; Lim 2010; Sia 2013), three studies reporting Apgar scores at both 1 and 5 minutes (Fettes 2006; Lin 2016; Salim 2005), and one study reporting Apgar scores greater than seven at 5 minutes (Sia 2007). In view of heterogeneity of reporting we have decided to review the data qualitatively. None of the studies showed any significant difference between Apgar scores between groups.
Discussion
Summary of main results
Moderate‐certainty evidence from 12 studies (1121 women) contributing data to the outcomes of this review showed a significant reduction in the risk of breakthrough pain with automated mandatory bolus (AMB) as compared with basal infusion (BI). There was high‐certainty evidence that showed no difference in the risk of caesarean delivery between groups, while moderate‐certainty evidence showed no difference in the risk of instrumental delivery. There was moderate‐certainty evidence that showed no difference in the duration of labour analgesia. Of note, four studies reported the duration from epidural initiation to time of breakthrough pain (Lim 2005; Leo 2010; Lim 2010; Sia 2013), but there was no difference between groups. Few participants in each study had breakthrough pain, which led to a small number of events. There was moderate‐certainty evidence of a statistically significant reduction in local anaesthetic consumption per hour with AMB. Qualitatively, there was increased maternal satisfaction with AMB compared to BI and no difference in Apgar scores between AMB and BI.
The 12 studies identified and addressed most of the objectives of the review. However, only 7 of the 12 studies reported maternal satisfaction. The results of this review are relevant to current practice as AMBs are increasingly used internationally.
Overall completeness and applicability of evidence
Ten of the 12 included studies enrolled healthy nulliparous women (Capogna 2011; Chua 2004; Fettes 2006; Leo 2010; Lim 2005; Lim 2010; Lin 2016; Salim 2005; Sia 2007; Sia 2013), while one study enrolled healthy parous women at term (Wong 2006), and one study enrolled both nulliparous and multiparous women (Ferrer 2017). Ten studies involved women with a singleton fetus in vertex presentation, while two studies did not specify the fetal lie (Ferrer 2017; Lin 2016); all 12 studies excluded women with complicated pregnancies. The studies were of sufficient scope to address the objectives of the review, investigating most relevant participants, interventions and outcomes; however, only two studies included multiparous women.
Quality of the evidence
All 12 studies with 1121 women reported random allocation, but only 9 described the method of randomization, all used computer‐generated random numbers (Capogna 2011; Ferrer 2017; Fettes 2006; Leo 2010; Lim 2005; Salim 2005; Sia 2007; Sia 2013; Wong 2006). Nine studies reported the method for allocation concealment, which consisted of sealed opaque envelopes in all cases (Capogna 2011; Chua 2004; Fettes 2006; Leo 2010; Lim 2010; Lin 2016; Sia 2007; Sia 2013; Wong 2006). There was overall low risk of selection bias.
There was a overall low risk of performance bias, detection bias, attrition bias, reporting bias and other potential bias. The overall certainty of evidence was moderate for incidence of breakthrough pain, instrumental delivery, duration of labour and hourly local anaesthesia consumption. This was mostly due to imprecision resulting from wide 95% confidence intervals. The quality of evidence for the risk of caesarean delivery was high.
Potential biases in the review process
Potential biases in the review process can arise from clinical heterogeneity due to the following factors: differing types and concentrations of local anaesthesia (details provided in Data synthesis), usage of adjuvants (e.g. opioids), technique of initiation of epidural analgesia (epidural alone versus combined spinal‐epidural) and methods of reporting Apgar scores. Women could receive epidural analgesia at various stages of labour and would have different pain thresholds. Hence, the different onset of epidural analgesia could influence the duration of epidural use, local anaesthetic consumption and the likelihood of developing motor blockade. The use of oxytocin augmentation should also be considered as a confounder.
Potential bias may also arise from statistical heterogeneity, even after stratifying into the pre‐planned subgroups. However, we did not select the subgroups based on anticipated statistical heterogeneity, but after careful consideration of clinically meaningful sub‐populations that may be generalizable to other similar populations.
With regard to the search, potential publication bias may arise due to varied search terms used for each database and the fact that we were unable to identify unpublished studies through author contacts. WIth this in mind, we have developed a highly sensitive search strategy and extended our search beyond CENTRAL, Embase and Pubmed to include trial registries (clinicaltrials.gov and www.who.int/ictrp/en) and a discipline‐specific database (Cochrane Pregnancy and Childbirth Group Trials Register).
Alex Sia is the author of six of the studies included in this review (Chua 2004; Leo 2010; Lim 2005; Lim 2010; Sia 2007; Sia 2013). He was not involved in the process of appraising quality of papers or abstracting data from papers.
Agreements and disagreements with other studies or reviews
We compared this review with the systematic review performed by George 2012. Our data is consistent with theirs, and we utilized the same method of conversion for studies with different local anaesthetics to bupivacaine equivalents. We also included two additional studies in this review (Lin 2016; Sia 2013).
Our results show good agreement with George and colleagues' review in the pooled results (George 2012). We found similar results for the risk of caesarean delivery (no difference), instrumental delivery (no difference), local anaesthetic consumption (decreased with AMB) and maternal satisfaction (increased with AMB). We also found a decrease in duration of labour with AMB, while George 2012 found a decrease in the duration of second stage of labour with AMB (we did not separately analyse the duration of first and second stages of labour). However, we found a decrease in the risk of breakthrough pain with AMB, whereas George 2012 did not.
Authors' conclusions
Implications for practice.
This systematic review found moderate‐certainty evidence that automated mandatory bolus (AMB) for maintenance of epidural analgesia in labour, confers a decrease in risk of breakthrough pain requiring anaesthetic intervention as compared with basal infusion (BI). There was low‐certainty evidence of no difference in risk of caesarean delivery, and low‐ to moderate‐certainty evidence of similar effects on the risk of instrumental delivery and duration of labour. There is evidence that AMB decreased local anaesthetic consumption per hour and increased maternal satisfaction. There appears to be no difference with Apgar scores.
Implications for research.
In our review, our results showed a reduced risk in breakthrough pain with AMB compared to BI. However, due to the limited number of events, the certainty of evidence was moderate. Future studies with a larger sample could provide more precision to our results. There remain unanswered questions regarding the clinical significance of reduced local anaesthetic consumption with AMB compared to BI. Furthermore most studies, with the exception of Capogna 2011, did not examine the difference in motor block between AMB and BI, and additional well‐designed and adequately powered RCTs are required to better delineate this area. The use of standardized definitions for motor block (such as using the modified Bromage score) would be useful in future trials. Future trials should consider the timing of breakthrough pain to enable investigation of the duration of analgesia between epidural initiation to time of breakthrough pain. Patient‐centric outcomes, such as maternal satisfaction or cost‐effectiveness analysis, could also be considered with advancement in new pump technology.
History
Protocol first published: Issue 10, 2014 Review first published: Issue 5, 2018
| Date | Event | Description |
|---|---|---|
| 17 October 2014 | Amended | Acknowledgement section updated |
Acknowledgements
We would like to thank Rodrigo Cavallazzi (content editor), Jing Xie (statistical editor), Stephen Halpern, Argyro Fassoulaki, Sui Cheung Yu (peer reviewers) and Wendy Free (consumer referee) for their help and editorial advice during the preparation of this systematic review.
We thank Dr Cynthia Wong for providing and analysing the data for Wong 2006, Dr Giorgio Capogna for providing and analysing the data for Capogna 2011, and Dr Leopoldo Ferrer for providing and analysing the data for Ferrer 2017.
We would also like to thank Rodrigo Cavallazzi (content editor), Cathal Walsh (statistical editor), Sui Cheung Yu, Stephen Halpern and Giorgio Capogna (peer‐referees) for their help and editorial advice during the preparation of the protocol for the systematic review (Sng 2014).
Appendices
Appendix 1. Search strategies
CENTRAL (the Cochrane Library) search strategy
#1 MeSH descriptor: [labour, Obstetric] explode all trees #2 MeSH descriptor: [labour Pain] explode all trees #3 MeSH descriptor: [Delivery, Obstetric] explode all trees #4 MeSH descriptor: [Parturition] explode all trees #5 (labo?r near (obstetric or pain* or vaginal)) or (labo?r or parturient* or child?birth or obstet* or deliver*):ti,ab #6 #1 or #2 or #3 or #4 or #5 #7 MeSH descriptor: [Analgesia, Epidural] explode all trees #8 MeSH descriptor: [Anesthesia, Epidural] explode all trees #9 MeSH descriptor: [Infusions, Spinal] explode all trees #10 MeSH descriptor: [Injections, Spinal] explode all trees #11 epidural*:ti,ab or (spinal near (infusion* or injection*)):ti,ab or (pain near relief) or (bupivacaine or ropivacaine or mepivacaine or fentanyl or sufentanil) #12 #7 or #8 or #9 or #10 or #11 #13 bolus* or AMB or basal infusion* or BCI or (intermittent or variable?frequency or patient?controlled):ti,ab #14 #6 and #12 and #13
OVID MEDLINE search strategy
1 bolus*.mp. or AMB.ti,ab. or basal infusion*.mp. or BCI.ti,ab. or (intermittent or variable?frequency or patient?controlled).ti,ab. 2 exp Analgesia, Epidural/ or exp Anesthesia, Epidural/ or exp Infusions, Spinal/ or exp Injections, Spinal/ or epidural*.ti,ab. or (spinal adj3 (infusion* or injection*)).ti,ab. or (pain adj3 relief).mp. or (bupivacaine or ropivacaine or mepivacaine or fentanyl or sufentanil).mp. 3 exp labour, Obstetric/ or exp labour Pain/ or exp Delivery, Obstetric/ or Parturition/ or (labo?r adj3 (obstetric or pain* or vaginal)).mp. or (labo?r or parturient* or child?birth or obstet* or deliver*).ti,ab. 4 ((randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or placebo.ab. or clinical trials as topic.sh. or randomly.ab. or trial.ti.) not (animals not (humans and animals)).sh. 5 1 and 2 and 3 and 4
OVID Embase search strategy
1 bolus*.mp. or AMB.ti,ab. or basal infusion*.mp. or BCI.ti,ab. or (intermittent or variable?frequency or patient?controlled).ti,ab. 2 exp epidural anesthesia/ or exp epidural anesthesia/ or exp intraspinal drug administration/ or epidural*.ti,ab. or (spinal adj3 (infusion* or injection*)).ti,ab. or (pain adj3 relief).mp. or (bupivacaine or ropivacaine or mepivacaine or fentanyl or sufentanil).mp. 3 exp labour/ or exp labour pain/ or exp delivery/ or birth/ or (labo?r adj3 (obstetric or pain* or vaginal)).mp. or (labo?r or parturient* or child?birth or obstet* or deliver*).ti,ab. 4 (randomized‐controlled‐trial/ or randomization/ or controlled‐study/ or multicenter‐study/ or phase‐3‐clinical‐trial/ or phase‐4‐clinical‐trial/ or double‐blind‐procedure/ or single‐blind‐procedure/ or (random* or cross?over* or multicenter* or factorial* or placebo* or volunteer*).mp. or ((singl* or doubl* or trebl* or tripl*) adj3 (blind* or mask*)).ti,ab. or (latin adj square).mp.) not (animals not (humans and animals)).sh. 5 1 and 2 and 3 and 4
WHO‐ICTRP
1 (basal infusion OR analgesia OR bolus) AND labor
ClinTrials.gov
1 labor [DISEASE] AND ( "basal infusion" OR bolus ) [TREATMENT] AND EXACT NOT "Male" [GENDER]
Appendix 2. Data collection form
Data collection form
| Review title or ID |
| Automated mandatory bolus versus basal infusion for maintenance of epidural analgesia in labour |
| Study ID(surname of first author and year first full report of study was published e.g. Smith 2001) |
| Report IDs of other reports of this study(e.g. duplicate publications, follow‐up studies) |
| Notes: |
1. General information
| Date form completed(dd/mm/yyyy) | |
| Name/ID of person extracting data | |
|
Report title (title of paper/abstract/report that data are extracted from) |
|
|
Report ID (ID for this paper/abstract/report) |
|
| Reference details | |
| Report author contact details | |
|
Publication type (e.g. full report, abstract, letter) |
|
|
Study funding sources (including role of funders) |
|
|
Possible conflicts of interest (for study authors) |
|
| Notes: | |
2. Study eligibility
| Study characteristics |
Eligibility criteria (Insert eligibility criteria for each characteristic as defined in the protocol) |
Yes | No | Unclear |
Location in text (pg & ¶/fig/table) |
|
| Type of study | Randomized controlled trial | |||||
| Controlled clinical trial (quasi‐randomized trial) |
||||||
| Participants | Healthy parturients requesting for epidural analgesia during labour | |||||
| Types of intervention | Automated mandatory bolus Basal infusion |
|||||
| Types of outcome measures | 1. Risk of breakthrough pain with need for anaesthetic intervention (dichotomous) 2. Risk of caesarean delivery (dichotomous) 3. Risk of instrumental delivery (dichotomous) 4. Duration of labour (continuous) 5. Total dose of local anaesthetic per hour (continuous) 6. Maternal satisfaction (continuous) 7. Apgar scores (continuous) |
|||||
| INCLUDE | EXCLUDE | |||||
| Reason for exclusion | ||||||
| Notes: | ||||||
DO NOT PROCEED IF STUDY EXCLUDED FROM REVIEW
3. Population and setting
|
Description Include comparative information for each group (i.e. intervention and controls) if available |
Location in text (pg & ¶/fig/table) |
||
|
Population description (from which study participants are drawn) |
|||
|
Setting (including location and social context) |
|||
| Inclusion criteria | |||
| Exclusion criteria | |||
| Method/s of recruitment of participants | |||
| Informed consent obtained | Yes No Unclear | ||
| Notes: | |||
4. Methods
| Descriptions as stated in report/paper |
Location in text (pg & ¶/fig/table) |
||
| Aim of study | |||
| Design(e.g. parallel, cross‐over, cluster) | |||
|
Unit of allocation (by individuals, cluster/groups or body parts) |
|||
| Start date | |||
| End date | |||
| Total study duration | |||
| Ethical approval needed/obtained for study | Yes No Unclear | ||
| Notes: | |||
5. 'Risk of bias' assessment
See Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions
| Domain | Risk of bias | Support for judgement |
Location in text (pg & ¶/fig/table) |
||
| Low risk | High risk | Unclear | |||
|
Random sequence generation (selection bias) |
|||||
|
Allocation concealment (selection bias) |
|||||
|
Blinding of participants and personnel (performance bias) |
Outcome group: All/ | ||||
| (if required) | Outcome group: | ||||
|
Blinding of outcome assessment (detection bias) |
Outcome group: All/ | ||||
| (if required) | Outcome group: | ||||
|
Incomplete outcome data (attrition bias) |
|||||
|
Selective outcome reporting? (reporting bias) |
|||||
| Other bias | |||||
| Notes: | |||||
6. Participants
Provide overall data and, if available, comparative data for each intervention or comparison group.
| Description as stated in report/paper |
Location in text (pg & ¶/fig/table) |
|
|
Total no. randomized (or total pop. at start of study for NRCTs) |
||
|
Clusters (if applicable, no., type, no. people per cluster) |
||
| Baseline imbalances | ||
|
Withdrawals and exclusions (if not provided below by outcome) |
||
| Age | ||
| Sex | ||
| Race/ethnicity | ||
| Severity of illness | ||
| Co‐morbidities | ||
| Other treatment received(additional to study intervention) | ||
| Other relevant sociodemographics | ||
| Subgroups measured | ||
| Subgroups reported | ||
| Notes: | ||
7. Intervention groups
Copy and paste table for each intervention and comparison group
Intervention Group 1
| Description as stated in report/paper |
Location in text (pg & ¶/fig/table) |
|
| Group name | ||
|
No. randomized to group (specify whether no. people or clusters) |
||
| Theoretical basis(include key references) | ||
| Description(include sufficient detail for replication, e.g. content, dose, components) | ||
| Duration of treatment period | ||
| Timing(e.g. frequency, duration of each episode) | ||
| Delivery(e.g. mechanism, medium, intensity, fidelity) | ||
|
Providers (e.g. no., profession, training, ethnicity etc. if relevant) |
||
| Co‐interventions | ||
| Economic variables (i.e. intervention cost, changes in other costs as result of intervention) | ||
|
Resource requirements to replicate intervention (e.g. staff numbers, cold chain, equipment) |
||
| Notes: | ||
8. Outcomes
Copy and paste table for each outcome.
Outcome 1
| Description as stated in report/paper |
Location in text (pg & ¶/fig/table) |
||
| Outcome name | |||
| Time points measured | |||
| Time points reported | |||
| Outcome definition(with diagnostic criteria if relevant) | |||
| Person measuring/reporting | |||
|
Unit of measurement (if relevant) |
|||
| Scales: upper and lower limits(indicate whether high or low score is good) | |||
| Is outcome/tool validated? | Yes No Unclear | ||
| Imputation of missing data (e.g. assumptions made for ITT analysis) | |||
|
Assumed risk estimate (e.g. baseline or population risk noted in Background) |
|||
| Power | |||
| Notes: | |||
9. Results
Copy and paste the appropriate table for each outcome, including additional tables for each time point and subgroup as required.
Dichotomous outcome
| Description as stated in report/paper |
Location in text (pg & ¶/fig/table) |
|||||
| Comparison | ||||||
| Outcome | ||||||
| Subgroup | ||||||
| Time point (specify whether from start or end of intervention) | ||||||
| Results | Intervention | Comparison | ||||
| No. events | No. participants | No. events | No. participants | |||
| No. missing participants and reasons | ||||||
| No. participants moved from other group and reasons | ||||||
| Any other results reported | ||||||
| Unit of analysis(by individuals, cluster/groups or body parts) | ||||||
| Statistical methods used and appropriateness of these methods(e.g. adjustment for correlation) | ||||||
| Reanalysis required?(specify) | Yes No Unclear | |||||
| Reanalysis possible? | Yes No Unclear | |||||
| Reanalysed results | ||||||
| Notes: | ||||||
Continuous outcome
| Description as stated in report/paper |
Location in text (pg & ¶/fig/table) |
|||||||||
| Comparison | ||||||||||
| Outcome | ||||||||||
| Subgroup | ||||||||||
| Time point (specify whether from start or end of intervention) | ||||||||||
| Post‐intervention or change from baseline? | ||||||||||
| Results | Intervention | Comparison | ||||||||
| Mean | SD (or other variance) | No. participants | Mean | SD (or other variance) | No. participants | |||||
| No. missing participants and reasons | ||||||||||
| No. participants moved from other group and reasons | ||||||||||
| Any other results reported | ||||||||||
|
Unit of analysis (individuals, cluster/groups or body parts) |
||||||||||
| Statistical methods used and appropriateness of these methods(e.g. adjustment for correlation) | ||||||||||
| Reanalysis required?(specify) | Yes No Unclear | |||||||||
| Reanalysis possible? | Yes No Unclear | |||||||||
| Reanalysed results | ||||||||||
| Notes: | ||||||||||
Other outcome
| Description as stated in report/paper |
Location in text (pg & ¶/fig/table) |
|||||
| Comparison | ||||||
| Outcome | ||||||
| Subgroup | ||||||
| Time point (specify whether from start or end of intervention) | ||||||
| Results | Intervention result | SD (or other variance) | Control result | SD (or other variance) | ||
| Overall results | SE (or other variance) | |||||
| No. participants | Intervention | Control | ||||
| No. missing participants and reasons | ||||||
| No. participants moved from other group and reasons | ||||||
| Any other results reported | ||||||
| Unit of analysis(by individuals, cluster/groups or body parts) | ||||||
| Statistical methods used and appropriateness of these methods | ||||||
| Reanalysis required?(specify) | Yes No Unclear | |||||
| Reanalysis possible? | Yes No Unclear | |||||
| Reanalysed results | ||||||
| Notes: | ||||||
10. Applicability
| Have important populations been excluded from the study?(consider disadvantaged populations, and possible differences in the intervention effect) | Yes No Unclear | |
| Is the intervention likely to be aimed at disadvantaged groups?(e.g. lower socioeconomic groups) | Yes No Unclear | |
|
Does the study directly address the review question? (any issues of partial or indirect applicability) |
Yes No Unclear | |
| Notes: | ||
11. Other information
| Description as stated in report/paper |
Location in text (pg & ¶/fig/table) |
|
| Key conclusions of study authors | ||
| References to other relevant studies | ||
| Correspondence required for further study information(from whom, what and when) | ||
| Notes: | ||
Appendix 3. Cochrane 'Risk of bias' tool and criteria for judgment
1. Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as being at:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
2. Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and will assess whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as being at:
low risk of bias (e.g. telephone or central randomization; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
3. Blinding
3.1 Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding would be unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as being at:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
3.2 Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as being at:
low, high or unclear risk of bias.
4. Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomized participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information is reported, or could be supplied by the trial authors, we re‐included missing data in the analyses which we undertook.
We assessed methods as being at:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; 'as treated' analysis done with substantial departure of intervention received from that assigned at randomization);
unclear risk of bias.
5. Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as being at:
low risk of bias (where it is clear that all of the study's pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study's pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
6. Other bias (checking for bias due to problems not covered by 1 to 5 above)
We described for each included study any important concerns we had about other possible sources of bias.
7. Overall risk of bias
We made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to items 1 to 6 above, we assessed the likely magnitude and direction of the bias and whether we considered it likely to impact on the findings. We planned to explore the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Data and analyses
Comparison 1. Automated mandatory bolus vs basal infusion.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Breakthrough pain | 10 | 797 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.39, 0.92] |
| 2 Breakthrough pain (epidural vs CSE) | 10 | 797 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.39, 0.92] |
| 2.1 Epidural | 3 | 313 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.25, 0.64] |
| 2.2 CSE | 7 | 484 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.44, 1.13] |
| 3 Breakthrough pain (PCEA vs no PCEA) | 10 | 797 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.39, 0.92] |
| 3.1 PCEA | 5 | 477 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.35, 1.07] |
| 3.2 No PCEA | 5 | 320 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.30, 1.12] |
| 4 Breakthrough pain (nulliparous vs multiparous) | 9 | 669 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.39, 1.00] |
| 4.1 Nulliparous | 8 | 543 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.33, 1.15] |
| 4.2 Multiparous | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.38, 0.90] |
| 5 Caesarean delivery | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.70, 1.21] |
| 6 Caesarean delivery (LA + opioids vs LA alone) | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.70, 1.21] |
| 6.1 LA + opioids | 10 | 952 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.70, 1.24] |
| 6.2 LA alone | 1 | 127 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.27, 2.01] |
| 7 Caesarean delivery (epidural vs CSE) | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.70, 1.21] |
| 7.1 Epidural | 5 | 637 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.53, 1.15] |
| 7.2 CSE | 6 | 442 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.73, 1.59] |
| 8 Caesarean delivery (PCEA vs no PCEA) | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.70, 1.21] |
| 8.1 PCEA | 7 | 801 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.70, 1.37] |
| 8.2 No PCEA | 4 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.50, 1.30] |
| 9 Caesarean delivery (nulliparous vs multiparous) | 10 | 951 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.70, 1.25] |
| 9.1 Nulliparous | 9 | 825 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.69, 1.23] |
| 9.2 Multiparous | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.12, 72.27] |
| 10 Instrumental delivery | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.54, 1.06] |
| 11 Instrumental delivery (LA + opioids vs LA alone) | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.57, 1.12] |
| 11.1 LA + opioids | 10 | 952 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.54, 1.08] |
| 11.2 LA alone | 1 | 127 | Risk Ratio (M‐H, Random, 95% CI) | 1.97 [0.37, 10.37] |
| 12 Instrumental delivery (epidural vs CSE) | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.57, 1.12] |
| 12.1 Epidural | 5 | 637 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.53, 1.74] |
| 12.2 CSE | 6 | 442 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.33, 1.05] |
| 13 Instrumental delivery (PCEA vs No PCEA) | 11 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.57, 1.12] |
| 13.1 No PCEA | 4 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.60, 1.61] |
| 13.2 PCEA | 7 | 801 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.42, 1.05] |
| 14 Instrumental delivery (nulliparous vs multiparous) | 10 | 951 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.54, 1.07] |
| 14.1 Nulliparous | 9 | 825 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.53, 1.08] |
| 14.2 Multiparous | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.17, 3.22] |
| 15 Duration of labour in minutes | 11 | 1079 | Mean Difference (IV, Random, 95% CI) | ‐10.38 [‐26.73, 5.96] |
| 16 Duration of labour in minutes (LA + opioids vs LA alone) | 11 | 1079 | Mean Difference (IV, Random, 95% CI) | ‐10.38 [‐26.73, 5.96] |
| 16.1 LA + opioids | 10 | 952 | Mean Difference (IV, Random, 95% CI) | ‐12.52 [‐31.87, 6.82] |
| 16.2 Duration of labor in minutes (LA alone) | 1 | 127 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐36.63, 36.63] |
| 17 Duration of labour in minutes (epidural vs CSE) | 11 | 1079 | Mean Difference (IV, Random, 95% CI) | ‐10.38 [‐26.73, 5.96] |
| 17.1 Epidural | 5 | 637 | Mean Difference (IV, Random, 95% CI) | ‐3.04 [‐26.42, 20.34] |
| 17.2 CSE | 6 | 442 | Mean Difference (IV, Random, 95% CI) | ‐32.70 [‐65.20, ‐0.20] |
| 18 Duration of labour in minutes (PCEA vs no PCEA) | 11 | 1079 | Mean Difference (IV, Random, 95% CI) | ‐10.38 [‐26.73, 5.96] |
| 18.1 PCEA | 7 | 801 | Mean Difference (IV, Random, 95% CI) | ‐13.24 [‐20.71, ‐5.76] |
| 18.2 No PCEA | 4 | 278 | Mean Difference (IV, Random, 95% CI) | ‐48.65 [‐129.92, 32.62] |
| 19 Duration of labour in minutes (nulliparous vs multiparous) | 10 | 951 | Mean Difference (IV, Random, 95% CI) | ‐14.38 [‐21.80, ‐6.96] |
| 19.1 Nulliparous | 9 | 825 | Mean Difference (IV, Random, 95% CI) | ‐13.92 [‐23.75, ‐4.10] |
| 19.2 Multiparous | 1 | 126 | Mean Difference (IV, Random, 95% CI) | ‐28.0 [‐76.95, 20.95] |
| 20 LA consumption per hour | 12 | 1121 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.78, ‐0.38] |
| 21 LA consumption per hour (LA + opioids vs LA alone) | 12 | 1121 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.78, ‐0.38] |
| 21.1 LA + opioids | 11 | 994 | Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.35, ‐0.15] |
| 21.2 LA alone | 1 | 127 | Mean Difference (IV, Random, 95% CI) | ‐9.50 [‐12.55, ‐6.45] |
| 22 LA consumption per hour (epidural vs CSE) | 12 | 1121 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.78, ‐0.38] |
| 22.1 Epidural | 5 | 637 | Mean Difference (IV, Random, 95% CI) | ‐2.59 [‐4.13, ‐1.05] |
| 22.2 CSE | 7 | 484 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.80, 0.11] |
| 23 LA consumption per hour (PCEA vs no PCEA) | 12 | 1121 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.78, ‐0.38] |
| 23.1 PCEA | 7 | 801 | Mean Difference (IV, Random, 95% CI) | ‐1.59 [‐2.58, ‐0.60] |
| 23.2 No PCEA | 5 | 320 | Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.58, 0.52] |
| 24 LA consumption per hour (nulliparous vs multiparous) | 11 | 993 | Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.55, ‐0.23] |
| 24.1 Nulliparous | 10 | 867 | Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.51, ‐0.15] |
| 24.2 Multiparous | 1 | 126 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐3.93, 0.33] |
1.3. Analysis.
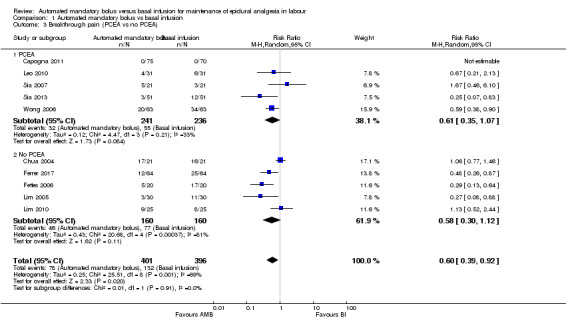
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 3 Breakthrough pain (PCEA vs no PCEA).
1.4. Analysis.
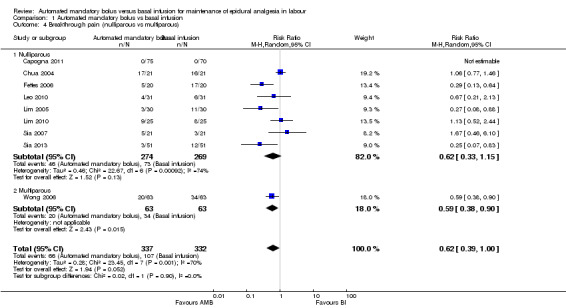
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 4 Breakthrough pain (nulliparous vs multiparous).
1.6. Analysis.
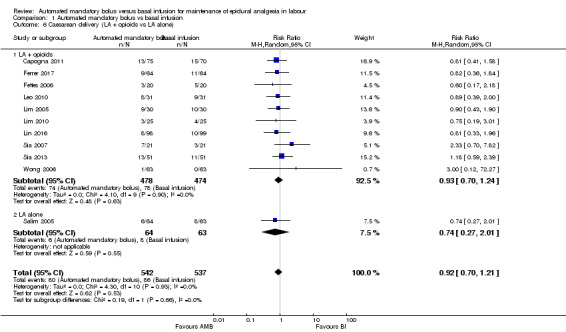
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 6 Caesarean delivery (LA + opioids vs LA alone).
1.7. Analysis.
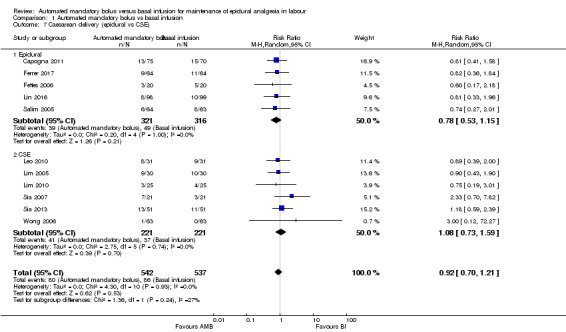
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 7 Caesarean delivery (epidural vs CSE).
1.8. Analysis.
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 8 Caesarean delivery (PCEA vs no PCEA).
1.9. Analysis.
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 9 Caesarean delivery (nulliparous vs multiparous).
1.11. Analysis.
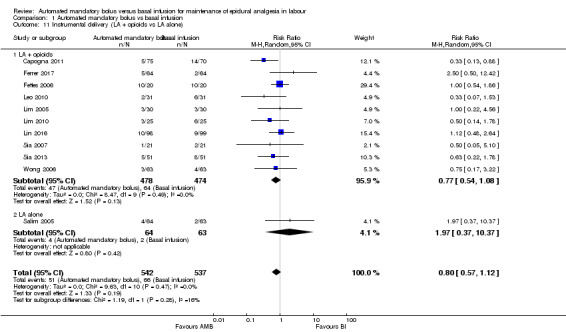
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 11 Instrumental delivery (LA + opioids vs LA alone).
1.12. Analysis.
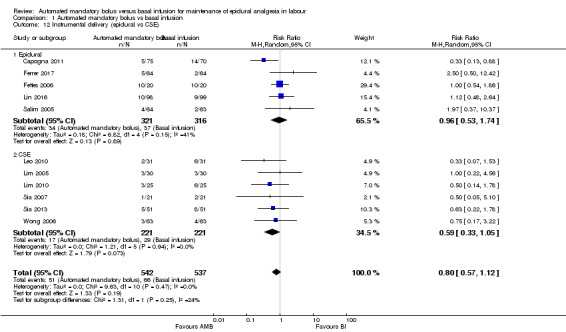
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 12 Instrumental delivery (epidural vs CSE).
1.13. Analysis.
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 13 Instrumental delivery (PCEA vs No PCEA).
1.14. Analysis.
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 14 Instrumental delivery (nulliparous vs multiparous).
1.16. Analysis.
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 16 Duration of labour in minutes (LA + opioids vs LA alone).
1.17. Analysis.
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 17 Duration of labour in minutes (epidural vs CSE).
1.19. Analysis.
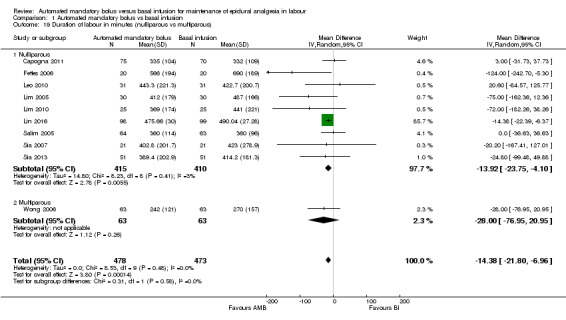
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 19 Duration of labour in minutes (nulliparous vs multiparous).
1.21. Analysis.
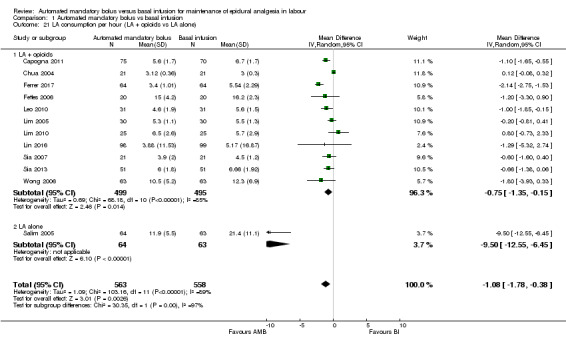
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 21 LA consumption per hour (LA + opioids vs LA alone).
1.22. Analysis.

Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 22 LA consumption per hour (epidural vs CSE).
1.24. Analysis.
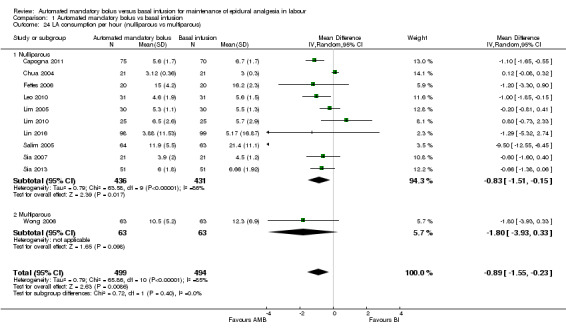
Comparison 1 Automated mandatory bolus vs basal infusion, Outcome 24 LA consumption per hour (nulliparous vs multiparous).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Capogna 2011.
| Methods | Prospective randomized double‐blind controlled study | |
| Participants | Setting: recruited from Citta di Roma Hospital, Roma, Italy Sample size: N = 150 (N completers = 145) Participants: age 27 ± 5 years (BI) and 29 ± 5 years (AMB) Inclusion criteria: healthy, nulliparous, term women with singleton, vertex pregnancies in spontaneous labour if cervical dilation was < 4 cm and if her baseline pain score, assessed at the peak of the contraction, was > 50 mm on a 100 mm visual analogue pain scale (VAPS) 5 women in the continuous epidural infusion group excluded: 4 reported VAPS > 10 mm 30 min after the epidural injection and one unintentional epidural catheter dislodgement during labour |
|
| Interventions | AMB (n = 75): 0.0625% levobupivacaine with sufentanil 0.5 µg/mL, 10 mL every hour, beginning 60 min after the administration of the initial epidural loading dose. PCEA pump was programmed to deliver 5 mL patient‐activated boluses of levobupivacaine 0.125% with a lockout interval of 10 min and a per hour maximum volume of 15 mL BI (n = 70): 0.0625% levobupivacaine with sufentanil 0.5 µg/mL, 10 mL/h, beginning immediately after the administration of the initial epidural loading dose. PCEA pump was programmed to deliver 5 mL patient‐activated boluses of levobupivacaine 0.125% with a lockout interval of 10 min, and a per hour maximum volume of 15 mL |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour Total dose of LA (levobupivacaine) |
|
| Notes | Study dates: April 2009 to July 2010 Funding sources not declared No conflict of interests declared References to other studies in this review: Fettes 2006; Leo 2010; Lim 2005 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random‐number sequence |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Unblinded researcher set up the 2 epidural pumps according to group allocation. The participants and other study personnel were blinded to group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All the observations and assessments were performed by a researcher blinded to the mode of drug administration. The infusion pumps were inserted into an opaque, portable bag. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition and exclusions reported; 5 out of 150 participants dropped out; however, this dropout rate is not significant (3%). |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size of 70 subjects in each group had a power of at least 80% for a 2‐sided Chi2 test of association between maintenance technique and incidence of motor block, with a significance level set to 0.05. |
Chua 2004.
| Methods | Parallel, randomized controlled trial | |
| Participants | Setting: recruited from Singapore General Hospital, Singapore Sample size: N = 42 Participants: age not provided Inclusion criteria: ASA physical status I nulliparous women in early spontaneous labour pain with at least one contraction every 5 min who had requested neuraxial block |
|
| Interventions | AMB (n = 21): ropivacaine 0.1% plus fentanyl 2 µg/mL for maintaining epidural analgesia The initial 5 mL bolus was administered 30 min after time 0, followed by 5 mL boluses every hour thereafter. As the highest rate of delivery afforded by the pump was 100 mL/h, each epidural bolus was delivered over 3 min. BI (n = 21): ropivacaine 0.1% plus fentanyl 2 µg/mL for maintaining epidural analgesia. A rate of 5 mL/h was initiated 1 min after time 0 by using a Terumo syringe pump |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention LA consumption per hour |
|
| Notes | Study dates not stated Funding sources not declared No conflict of interests declared References to other studies in this review: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Low risk | Randomly assigned by the blind opaque envelope technique |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | All blocks performed by the principal investigator |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All data was collected by an anaesthesiologist who was not involved in instituting the block |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Sample size was computed to detect a 30‐min difference (α = 0.05, ß = 0.2) in the duration of analgesia |
Ferrer 2017.
| Methods | Prospective, randomized, controlled, single‐blind, parallel study | |
| Participants | Setting: recruited from Hospital Universitario Fundación Santa Fe de Bogotá (Colombia) Sample size: N = 132 (N completers = 128) Participants: age 32.3 ± 3.8 years (BI) and 31.6 ± 5.1 years (AMB) Inclusion criteria: labouring term women aged between 18 and 45 years requiring epidural analgesia Two women in each group were excluded from analysis as they delivered within 60 min of epidural initiation |
|
| Interventions | AMB (n = 64): initial loading dose of 10 mL of 0.1% bupivacaine (2 mL of 0.5% bupivacaine plus 50 μg/mL of fentanyl in 7 mL of 0.9% normal saline), then a 10 mL bolus of a mixture of 0.1% bupivacaine plus 2 μg/mL of fentanyl in 0.9% normal saline every hour starting 1 hour after the initial loading dose BI (n = 64): initial loading dose of 10 mL of 0.1% bupivacaine (2 mL of 0.5% bupivacaine plus 50 μg/mL of fentanyl in 7 mL of 0.9% normal saline) then a 10 mL/hh infusion of a mixture of 0.1% bupivacaine plus 2 μg/mL of fentanyl in 0.9% normal saline every hour starting immediately after the loading dose |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour analgesia Total LA dose Maternal satisfaction Apgar scores |
|
| Notes | Study dates not stated No funding sources No conflict of interests declared References to other studies in this review: Capogna 2011; Chua 2004; Leo 2010; Lim 2005; Salim 2005; Wong 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Unclear risk | Participants, caregivers and outcome assessors were not aware of the next treatment allocation. Under Materials and Methods: Quote: "neither the patient nor the attending anesthesiologist nor the outcome assessor knew the randomization sequence." However, the method of allocation concealment was not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | This is a single blind trial. The outcomes are objective and the outcome assessors were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition and exclusions reported |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size of 132 participants (66 per group) with 10% attrition would give the study a power of > 0.8 to detect a 10% reduction in the difference of means of breakthrough pain between the 2 groups |
Fettes 2006.
| Methods | Parallel, randomized controlled trial | |
| Participants | Setting: recruited from Ninewells Hospital and Medical School, Dundee, UK Sample size: N = 47 (N completers = 40) Participants: age 25.8 ± 6.3 years (AMB) and 27.1 ± 4.5 years (BI) Inclusion criteria: ASA I–II primigravid participants with uncomplicated, full‐term (> 37 weeks) pregnancy 7 women were excluded after epidural catheter placement: 3 because of inadequate analgesia at 45 min; and 1 each because of patchy block, epidural filter disconnection, catheter occlusion and study protocol violation |
|
| Interventions | AMB (n = 20): ropivacaine 2 mg/mL with fentanyl 2 mg/mL. Hourly boluses, delivered at 2 mL/min, were started 30 min after time zero BI (n = 20): ropivacaine 2 mg/mL with fentanyl 2 mg/mL. Infusion was started immediately at a constant rate of 10 mL/h |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour Total LA dose Apgar scores |
|
| Notes | Study dates not stated Funding sources not declared No conflict of interests declared References to other studies in this review: Chua 2004; Lim 2005 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated numbers |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were nursed in the sitting position by staff that were unaware of the treatment used. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Observations were made by an assessor 'blind' (the pump was covered) to the mode of drug administration |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition and exclusions reported; under Results section p. 361, Quote: "dropouts were divided equally into the two groups" |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size of 40 participants (20 per group) would give the study a power of > 0.9 to detect a statistically significant difference in visual analogue pain scores |
Leo 2010.
| Methods | Randomized controlled trial | |
| Participants | Setting: recruited from KK Women's and Children's Hospital, Singapore Sample size: N = 62 Participants: age not provided Inclusion criteria: healthy ASA I nulliparous parturients with term (> 36 weeks of gestation), singleton fetuses in the vertex presentation, who were in early labour (cervical dilation < 5 cm) and requested labour epidural analgesia |
|
| Interventions | AMB (n = 31): 0.1% ropivacaine + fentanyl 2 µg/mL. PCEA algorithm initiated immediately after completion of CSE. Participants in this group received automated mandatory boluses (AMB) of 5 mL every hour instead of a basal infusion. The first AMB dose was delivered 30 min from CSE and epidural catheter placement and every hour subsequently if no PCEA demands were made. If the participant had made a successful PCEA self‐bolus, the next AMB bolus would be delivered 30 min after the last successful PCEA self‐bolus and every hour thereafter. The lockout period for both PCEA and AMB boluses was 10 min. If a PCEA demand was made within 10 min of an AMB dose, no further bolus would be given. This would be recorded as an unsuccessful PCEA attempt. PCEA bolus was set at 5 mL and maximal hourly limit at 20 mL/h (inclusive of basal infusion and automated boluses) BI (n = 31): 0.1% ropivacaine + fentanyl 2 μg/mL. PCEA with basal infusion 5 mL/h initiated immediately after intrathecal drug administration and epidural catheter placement. PCEA bolus was set at 5 mL, lockout interval at 10 min and maximal dose at 20 mL/h |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour Total LA/hour (time weighted hourly consumption of ropivacaine) Maternal satisfaction Apgar scores |
|
| Notes | Study dates not stated Funding sources not declared No conflict of interests declared References to other studies in this review: Chua 2004; Fettes 2006; Lim 2005; Sia 2007; Wong 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number tables |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Independent assistant programmed the epidural drug delivery system according to group assignment. Parturients were subsequently monitored by a second anaesthesiologist not involved in performing the block. Neither the parturients nor the anaesthesiologists who monitored and collected post‐block data were aware of group assignments |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Neither the parturients nor the anaesthesiologists who monitored and collected post‐block data were aware of group assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size of 30 participants in each group was calculated to detect a 30% reduction in the incidence of breakthrough pain requiring physician top‐up for participants in the PCEA + AMB arm compared with those in the PCEA + BI arm (α = 0.05, ß = 0.2) |
Lim 2005.
| Methods | Randomized controlled trial | |
| Participants | Setting: recruited from KK Women's and Children's Hospital, Singapore Participants: age 30 ± 6 years (AMB) and 31 ± 5 years (BI) Sample size: N = 60 Inclusion criteria: ASA I nulliparous labouring parturients at term who requested neuraxial analgesia in established labour with cervical dilatation less than or equal to 5 cm and with baseline pain scores more than or equal to 50 (on a 0–100 visual analogue scale (VAS): 0 = no pain, 100 = worst pain imaginable) |
|
| Interventions | AMB (n = 30): 5 mL epidural boluses of levobupivacaine 0.1% with fentanyl 2 µg/mL every 30 min. This was initiated 15 min after the intrathecal component was given BI (n = 30): levobupivacaine 0.1% with fentanyl 2 µg/mL at a rate of 10 mL/h as a continuous infusion delivered by a syringe pump. The epidural infusion was initiated in the next minute after the intrathecal component was given |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour Total LA/hour Maternal satisfaction Apgar scores |
|
| Notes | Study dates not stated Funding sources not declared No conflict of interests declared References to other studies in this review: Chua 2004 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized using a computer‐generated table |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | An anaesthetist, who was not involved in performing the block and blinded to the mode of drug delivery, collected the data |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size was computed to detect a 40% reduction of incidence of breakthrough pain |
Lim 2010.
| Methods | Randomized double‐blinded controlled clinical trial | |
| Participants | Setting: recruited from KK Women's and Children's Hospital, Singapore Sample size: N = 51 (N completers = 50) Participants: age not provided Inclusion criteria: healthy nulliparous parturients with cephalic presentation at > 36 weeks gestation in early, spontaneous labour (cervical dilation < 5 cm) 1 woman from CEI group excluded as epidural catheter was blocked and resited 2 hours after initiation of CSE |
|
| Interventions | AMB (n = 25): 2.5 mL epidural boluses of 0.1% ropivacaine with fentanyl 2 µg/mL, infused over a 2‐minute period, every 15 min. The first bolus was given 7.5 min after the intrathecal injection BI (n = 25): 0.1% ropivacaine with fentanyl 2 µg/mL at 10 mL/hour, delivered by syringe pump and initiated immediately after the intrathecal injection |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour Time‐weighted consumption of LA Maternal satisfaction Apgar scores |
|
| Notes | Study dates: 18 February to 19 March 2007 Funding sources not declared No conflict of interests declared References to other studies in this review: Chua 2004; Fettes 2006; Lim 2005; Wong 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not explained |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelope, which was opened after recruitment by the anaesthetist who was to perform the epidural |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Parturient was blinded to the group allocation. Nurse/midwife was also blinded to participant study group allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome data were gathered by a blinded observer |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition and exclusions reported. Intention‐to‐treat analysis conducted |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size was computed to detect a 30% difference in the incidence of breakthrough pain |
Lin 2016.
| Methods | Randomized double blinded controlled clinical trial | |
| Participants | Setting: recruited from First Affiliated Hospital of Guangxi Medical University, Nanning, People's Republic of China Sample size: N = 200 (N completers = 197) Participants: age 27.45 ± 4.61 (AMB) and 28.16 ± 4.679 (CI) Inclusion criteria: healthy nulliparous women in early spontaneous labor (> 37 weeks' gestation) having at least one uterine contraction every 5 min and who had requested neuraxial block 3 women were excluded because of unplanned epidural catheter removal |
|
| Interventions | AMB (n = 98): test dose of 4 mL of 1% lignocaine then 10 mL of 0.15% ropivacaine loading dose, then maintenance with 0.1% ropivacaine with sufentanil 0.3 µg/mL at 5 mL bolus per hour plus PCEA of 5 mL with 20 min lockout period, maximum 15 mL/h BI (n = 99): test dose of 4 mL of 1% lignocaine then 10 mL of 0.15% ropivacaine loading dose, then maintenance with 0.1% ropivacaine with sufentanil 0.3 µg/mL at 5 mL/h infusion plus PCEA of 5 mL with 20 min lockout period, maximum 15 mL/h |
|
| Outcomes | Rate of caesarean delivery Rate of instrumental delivery Duration of labour LA used Apgar scores at 1 and 5 min |
|
| Notes | Study dates: not provided Funding sources not declared No conflict of interests declared References to other studies in this review: Capogna 2011; Lim 2005; Wong 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization not explained |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Unblinded researcher programmed the epidural drug delivery system according to group assignment. Parturients were subsequently monitored by a second blinded researcher. Neither the parturients nor the researchers who monitored and collected postblock data were aware of group assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Neither the parturients nor the researchers who monitored and collected postblock data were aware of group assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition and exclusions reported; 3 out of 200 participants were excluded from the analysis; however, this dropout rate is minimal (1.5%). |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation not explained |
Salim 2005.
| Methods | Parallel 3‐group, randomized controlled trial | |
| Participants | Setting: recruited from Ha'Emek Medical Center, Afula, Israel Sample size: N = 190 Participants: age 25.7 ± 4.2 years (AMB), 25.6 ± 3.8 years (BI) and 23.7 ± 4.4 years (control) Inclusion criteria: all nulliparous women at term (37 weeks or more) who requested epidural analgesia during labour |
|
| Interventions | AMB (n = 64): intermittent bolus infusions of 10 mL of 0.25% bupivacaine on demand with minimal intervals of 60 min BI (n = 63): basal continuous infusion of 0.125% bupivacaine with 2 µg/mL fentanyl at a rate of 8 mL/h with patient‐controlled epidural analgesia doses of 3 mL of this solution with a lockout time of 20 min Control (n = 63): control group without epidural who received a mixture of oxygen/nitrous oxide and/or pethidine |
|
| Outcomes | Rate of caesarean delivery Rate of instrumental delivery Duration of labour LA used Maternal satisfaction Apgar scores |
|
| Notes | Study dates: 6 January to 22 July 2004 Funding sources not declared No conflict of interests declared References to other studies in this review: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization of group A and B was performed using Microsoft Excel XP Professional (Microsoft, Redmond, WA). The allocation sequence was generated by the primary author Attending physicians enrolled and assigned participants to their groups |
| Allocation concealment (selection bias) | Unclear risk | The sequence was concealed until intervention was assigned however the method of allocation concealment was not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size of 63 subjects in each group was needed to demonstrate a difference of 30 min, considered clinically significant, in duration of the second stage of labor (60 min) between groups A and B with an alpha of 0.05 and power of 80% |
Sia 2007.
| Methods | Parallel, randomized controlled trial | |
| Participants | Setting: recruited from KK Women's and Children's Hospital, Singapore Sample size: n = 42 Participants: age not provided Inclusion criteria: healthy (ASA I), nulliparous parturients with cephalic presentation at ≥ 36 weeks of gestation who were in early spontaneous labour (cervical dilation ≤ 5 cm) and who had requested neuraxial blocks for analgesia and had a VAPS of > 3 cm |
|
| Interventions | AMB (n = 21): 0.1% ropivacaine + fentanyl 2 µg/mL. PCEA + automated mandatory boluses (based on an empirical algorithm, maximal dose per hour = 20 mL), initiated the minute after time 0. In this group, apart from PCEA boluses of 5 mL per demand, the parturients received mandatory boluses of 5 mL/h with the first AMB dose delivered 30 min after the initiation of the pump and every hour after that if no PCEA demands were made. The lockout period for both PCEA and AMB boluses was 10 min. If a PCEA demand was made within 10 min of an AMB dose, no further bolus would be given. This would be recorded as an unsuccessful PCEA attempt. Provided that no further PCEA demands were made, the next AMB bolus would then be delivered 1 h after the last AMB. If there had been a successful PCEA bolus, the next AMB bolus would be delivered one hour after the last successful PCEA bolus BI (n = 21): 0.1% ropivacaine + fentanyl 2 µg/mL. PCEA + basal continuous infusion (BCI 5 mL/h, PCEA bolus of 5 mL, lockout interval = 10 min, maximal dose per hour = 20 mL), initiated the minute after time 0 |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour Time weighted ropivacaine consumed per hour Maternal satisfaction Apgar scores |
|
| Notes | Study dates not stated Funding sources not declared No conflict of interests declared References to other studies in this review: Chua 2004; Lim 2005; Wong 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The assignment of parturients to group was done by another investigator (ATS) not involved in performing the block or subsequent monitoring of the parturients |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Neither the parturients nor the investigators who monitored and collected data were aware of the participant group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size determined (α = 0.05, ß = 0.2) to detect a 20% reduction in the time weighted epidural ropivacaine consumption for PCEA‐AMB compared with PCEA‐BCI |
Sia 2013.
| Methods | Parallel randomized controlled trial | |
| Participants | Setting: recruited from KK Women's and Children's Hospital, Singapore Sample size: N = 102 Participants: age not provided Inclusion criteria: healthy (ASA 1) nulliparous parturients at term (> 36 weeks gestation) with a singleton fetus, who were in early labour (cervical dilation < 5 cm) and who had requested labour epidural analgesia with VAS > 3 cm |
|
| Interventions | AMB (n = 51): 0.1% ropivacaine + fentanyl 2 µg/mL. Automated bolus group: a PCEA algorithm was used, initiated immediately after the completion of CSE. The pump was designed to administer automated boluses of 5 mL in addition to the patient‐controlled boluses. The frequency of such automated boluses was dependent on the history of the participant's analgesic requirement over the past hour. The first automated bolus was programmed to be delivered 60 min from time 0 and every hour thereafter if no PCEA patient‐bolus was made (1 automated bolus of 5 mL every hour). At the first activation of a PCEA patient‐bolus, the timer would be reset with the subsequent automated bolus delivered 30 min following the PCEA patient‐bolus, and every hour thereafter if no further PCEA patient bolus was made (1 automated bolus of 5 mL every hour). If there was a second PCEA patient bolus in that same hour after the initial bolus, the time interval between 2 automated boluses would be shortened to 30 min (2 automated boluses of 5 mL every hour). If there was a third PCEA patient‐bolus within that hour, the automated bolus would be delivered at 20‐min intervals (3 automated boluses of 5 mL every hour). A fourth PCEA patient‐bolus within the same hour would further shorten the time interval between 2 automated boluses to 15 min (4 automated boluses of 5 mL every hour). On the other hand, if there were no patient‐bolus for 60 min, the frequency of automated boluses would step down in the reverse fashion. The lockout period for both PCEA and automated boluses was 10 min. If a PCEA demand was made within 10 min of an automated bolus, no patient bolus would be given and this would be recorded as an unsuccessful PCEA attempt. The PCEA demand bolus was set at 5 mL with a maximum hourly limit of 20 mL/h (inclusive of automated boluses). BI (n = 51): 0.1% ropivacaine + fentanyl 2 µg/mL. Infusion group: PCEA with basal infusion 5 mL/h initiated immediately following intrathecal drug administration (noted as time 0). The PCEA demand bolus was set at 5 mL, lockout interval at 10 min and maximum dose at 20 mL/h (inclusive of background infusion) |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour Total LA/hour (time‐weighted mean hourly consumption of ropivacaine) Maternal satisfaction Apgar scores |
|
| Notes | Study dates not stated Funding sources: no external funding No conflict of interests declared References to other studies in this review: Chua 2004; Fettes 2006; Lim 2005; Sia 2007; Wong 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number tables by a different investigator |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The parturients were subsequently monitored by a second anaesthetist who was not involved in performing the block |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Neither the parturient nor the anaesthetist who recorded the post‐block data was aware of the group assignment Post‐block parameters were monitored by a separate blinded anaesthetist after the procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size of 49 participants in each group was required to detect an 80% reduction in the incidence of breakthrough pain requiring physician top‐up (α = 0.05, ß = 0.2) |
Wong 2006.
| Methods | Parallel, randomized controlled trial | |
| Participants | Setting: recruited from Northwestern University, Chicago, Ilinois, USA Sample size: N = 158 (N completers = 126) Participants' age not provided Inclusion criteria: healthy, parous (at least one previous vaginal delivery), term women with singleton, vertex pregnancies, scheduled for induction of labour 11 women from the PIEB group and 9 women from the CEI group were excluded for having delivered within 90 min of intrathecal analgesia. 10 women from the PIEB group were excluded for exceeded pump occlusion limits. 2 women were excluded for VAS > 10 mm 10 min after intrathecal injection |
|
| Interventions | AMB (n = 63): PIEB pump delivered a 6‐mL bolus at a rate of 400 mL/h every 30 min beginning 45 min after administration of the intrathecal dose The PCEA pump was programmed to deliver 5 mL patient‐activated boluses with a lockout interval of 10 min and a per hour maximum of 15 mL. The participant was instructed on the use of the PCEA pump and was told to push the button whenever she felt uncomfortable. If the parturient felt she had inadequate analgesia after having activated the PCEA bolus twice in a 20‐min period an anaesthesiologist administered manual boluses of bupivacaine 1.25 mg/mL (5 mL to 15 mL) until the VAS was < 10 mm BI (n = 63): the CEI pump delivered a continuous infusion at 12 mL/h beginning 15 min after the intrathecal dose The PCEA pump was programmed to deliver 5 mL patient‐activated boluses with a lockout interval of 10 min and a per hour maximum of 15 mL. The subject was instructed on the use of the PCEA pump and was told to push the button whenever she felt uncomfortable. If the parturient felt she had inadequate analgesia after having activated the PCEA bolus twice in a 20‐min period an anaesthesiologist administered manual boluses of bupivacaine 1.25 mg/mL (5 to 15 mL) until the VAS was < 10 mm |
|
| Outcomes | Rate of breakthrough pain with need for anaesthetic intervention Rate of caesarean delivery Rate of instrumental delivery Duration of labour LA per hour Maternal satisfaction |
|
| Notes | Study dates: June 2003 to April 2005 Funding sources not declared No conflict of interests declared References to other studies in this review: Chua 2004 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | One unblinded anaesthesia researcher who opens the envelope. Subject and other study personnel were blinded as to group assignment. An unblinded researcher set up two epidural pumps for each participant. One pump administered either the PIEB or CEI while the second pump administered PCEA |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participant and other study personnel were blinded to group assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All a priori outcomes reported based on published protocol |
| Other bias | Low risk | Appears to be free of other sources of bias. Sample size calculation: sample size would be required to avoid a type II error at 0.05 and power of 0.80. 30 additional participants were included in the randomization to allow for anticipated exclusion of participants from data analysis |
AMB: automated mandatory bolus; ASA: American Society of Anesthesiologists; BCI: basal continuous infusion; BI: basal infusion; CEI: continuous epidural infusion; CSE: combined spinal‐epidural; LA: local anaesthetic; PCEA: patient controlled epidural analgesia; PIEB: programmed intermittent epidural boluses; VAPS: visual analogue pain scale; VAS: visual analogue scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Nunes 2014 | Intervention groups not comparable in study as given different volumes and concentrations of LA |
| Patkar 2015 | Study did not use automated bolus, instead manual bolus was administered |
LA: local anaesthetic.
Differences between protocol and review
We made the following changes to the protocol (Sng 2014).
Nurun Nisa Amatullah de Souza and Nian‐Lin R Han joined the review team in 2016.
We did not search the metaRegister of Controlled Trials (mRCT). This was because the service was under review and was not accessible.
We have edited the wording of our Objectives section to conform with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The underlying aims remain the same.
-
We have edited the criteria for considering studies for this review, to be more concise and relevant. This has not, however, led to any study being included or excluded on this basis.
Under types of studies, we stated that we would exclude studies that did not use automated administration of bolus doses. This is to clarify that we would not include studies that involved clinician administration of bolus doses or automated administration of varying continuous infusions (non‐boluses).
Under types of participants, we have only included studies that recruited pregnant term women and excluded studies that recruited women with complicated pregnancies including preterm labour, multiple pregnancy, and malposition of the fetus.
Under types of interventions, we have added criteria that were previously written under the heading 'Type of participants'. This is because the information is more suited to this section. There has been no overall change to either the inclusion or exclusion criteria.
Under measures of treatment effects, we did not calculate the numbers needed to treat to benefit/harm as it was not indicated. We otherwise separated the data as dichotomous/categorical and continuous and presented them as planned.
Under 'Dealing with missing data', we chose to contact the authors for missing data. The other methods discussed in the protocol such as worst‐case scenario analysis and imputation were not possible due to lack of the raw data of the studies.
Under 'Summary of findings table', we did not construct separate tables for the two interventions but placed them under one unified table.
We did not perform subgroup analyses for nulliparous versus multiparous women as only one study, Wong 2006, included parous women, and examination of our results showed removing or including this study as a subgroup would not have affected any of the outcomes in a meaningful way.
-
We did not include subgroup analyses for the following outcomes, as after dividing the data by subgroups led to no meaningful difference between subgroups (low heterogeneity).
Risk of caesarean delivery.
Risk of instrumental delivery.
Maternal satisfaction.
-
We included subgroup analyses for the following outcomes where relevant when comparison between subgroups showed a meaningful difference.
Risk of breakthrough pain ‐ epidural technique: epidural alone versus combined spinal‐epidural technique.
Duration of labour ‐ PCEA: regimens that used PCEA versus those that did not.
Local anaesthetic consumption per hour ‐ PCEA: regimens that used PCEA versus those that did not.
-
We also did not include subgroups for data in which no subgroups were present.
Risk of breakthrough pain ‐ all studies used local anaesthetic plus opioids; there was no study that utilized local anaesthetic alone.
Maternal satisfaction ‐ all included studies utilized local anaesthetic with opioids; there was no study that utilized local anaesthetic alone. All included studies utilized CSE; there was no study that utilized epidural alone.
We changed the reporting of Apgar scores from ordinal (in the protocol) to continuous (in the review) based on how studies reported the outcome. In addition we reviewed the data qualitatively due to heterogeneity in reporting by the various studies. We therefore did not include it in the 'Summary of findings' table.
We ended up reporting maternal satisfaction qualitatively due to the ordinal nature of the data, so we did not include it in the 'Summary of findings' table.
We went on to perform subgroup analyses for outcomes that had considerable heterogeneity (i.e. I2 > 75%) because the analyses were pre‐planned; however, we interpreted the results of only the clinically meaningful subgroups in the 'Results' section.
We used the Mantel‐Haenszel risk ratio method for dichotomous outcomes and did not use the Peto method because the events were not rare, i.e. the highest study event rate is more than 10%. We did not pool the Apgar score and instead interpreted the outcome qualitatively because of the lack of data for this outcome. Where there was moderate to high heterogeneity, we used random‐effects estimates to interpret the results. Otherwise, we interpreted the fixed‐effect estimate.
We regarded heterogeneity as considerable if I2 was greater than 75%, substantial if I2 was between 50% and 90%, moderate if I2 was between 30% and 60%, and low if I2 was less than 40%.
Contributions of authors
Conceiving the review: Ban Leong Sng (SBL), Fahad Javaid Siddiqui (FJS), Pryseley N Assam (PNA), Alex T Sia (AS), Edwin SY Chan (EC), Wan Ling Leong (LWL), Ting Ting Oh (OTT), Yanzhi Zeng (ZYZ), Nurun Nisa Amatullah de Souza (NNAdS), Nian‐Lin R Han (NLRH).
Co‐ordinating the review: SBL, FJS, ZYZ, NNAdS.
Undertaking manual searches: FJS, PNA.
Screening search results: SBL, FJS, PNA, ZYZ, NNAdS.
Organizing retrieval of papers: SBL, LWL, OTT.
Screening retrieved papers against inclusion criteria: SBL, LWL, OTT.
Appraising quality of papers: SBL, LWL, OTT.
Abstracting data from papers: SBL, LWL, OTT.
Writing to authors of papers for additional information: SBL, LWL, OTT.
Providing additional data about papers: SBL, LWL, OTT.
Obtaining and screening data on unpublished studies: SBL, LWL, OTT.
Data management for the review: SBL, FJS, PNA, AS, EC, LWL, OTT, ZYZ, NNAdS, NLRH.
Entering data into Review Manager 5 (RevMan 5): SBL, FJS, PNA, OTT, ZYZ, NNAdS, NLRH.
RevMan 5 statistical data: SBL, FJS, PNA, EC, ZYZ, NNAdS, NLRH.
Other statistical analysis not using RevMan: SBL, FJS, PNA, EC, NNAdS, NLRH.
Interpretation of data: SBL, FJS, PNA, AS, EC, LWL, OTT, ZYZ, NNAdS, NLRH.
Statistical inferences: SBL, FJS, PNA, EC, NNAdS.
Writing the review: SBL, FJS, PNA, AS, EC, LWL, OTT, ZYZ, NNAdS, NLRH.
Securing funding for the review: SBL.
Performing previous work that was the foundation of the present study: SBL, AS.
Guarantor for the review (one author): SBL.
Person responsible for reading and checking review before submission: SBL.
Sources of support
Internal sources
-
KK Women's and Children's Hospital, Singapore.
Research time utilised
External sources
-
Duke‐NUS Graduate Medical School, Singapore.
Research time utilised
-
Singapore Clinical Research Institute, Singapore.
Research time utilised
Declarations of interest
Ban Leong Sng: none known.
Yanzhi Zeng: none known.
Fahad Javaid Siddiqui: none known.
Pryseley N Assam: none known.
Edwin SY Chan: none known.
Wan Ling Leong: none known.
Ting Ting Oh: none known.
Alex T Sia is an author of six of the studies that are included in this review: Chua 2004; Leo 2010; Lim 2005; Lim 2010; Sia 2007; Sia 2013. The variable frequency automated mandatory bolus technique described in Sia 2013 prompted the filing of a patent for the technique.
Nurun Nisa Amatullah de Souza: none known.
Nian‐Lin R Han: none known.
New
References
References to studies included in this review
Capogna 2011 {published data only}
- Capogna G, Camorcia M, Stirparo S, Farcomeni A. Programmed intermittent epidural bolus versus continuous epidural infusion for labor analgesia: the effects on maternal motor function and labor outcome. A randomized double‐blind study in nulliparous women. Anesthesia and Analgesia 2011;113(4):826‐31. [DOI: 10.1213/ANE.0b013e31822827b8; PUBMED: 21788309] [DOI] [PubMed] [Google Scholar]
Chua 2004 {published data only}
- Chua SM, Sia AT. Automated intermittent epidural boluses improve analgesia induced by intrathecal fentanyl during labour. Canadian Journal of Anaesthesia 2004;51(6):581‐5. [PUBMED: 15197122] [DOI] [PubMed] [Google Scholar]
Ferrer 2017 {published data only}
- Ferrer LE, Romemro DJ, Vásquez OI, Matute EC, Velde M. Effect of programmed intermittent epidural boluses and continuous epidural infusion on labor analgesia and obstetric outcomes: a randomized controlled trial. Archives of Gynecology and Obstetrics 2017;296(5):915‐922. [DOI] [PubMed] [Google Scholar]
Fettes 2006 {published data only}
- Fettes PD, Moore CS, Whiteside JB, McLeod GA, Wildsmith JA. Intermittent vs continuous administration of epidural ropivacaine with fentanyl for analgesia during labour. British Journal of Anaesthesia 2006;97(3):359‐64. [PUBMED: 16849382] [DOI] [PubMed] [Google Scholar]
Leo 2010 {published data only}
- Leo S, Ocampo CE, Lim Y, Sia AT. A randomized comparison of automated intermittent mandatory boluses with a basal infusion in combination with patient‐controlled epidural analgesia for labor and delivery. International Journal of Obstetric Anaesthesia 2010;19(4):357‐64. [DOI: 10.1016/j.ijoa.2010.07.006; PUBMED: 20832282] [DOI] [PubMed] [Google Scholar]
Lim 2005 {published data only}
- Lim Y, Sia AT, Ocampo C. Automated regular boluses for epidural analgesia: a comparison with continuous infusion. International Journal of Obstetric Anaesthesia 2005;14(4):305‐9. [PUBMED: 16154735] [DOI] [PubMed] [Google Scholar]
Lim 2010 {published data only}
- Lim Y, Chakravarty S, Ocampo CE, Sia AT. Comparison of automated intermittent low volume bolus with continuous infusion for labour epidural analgesia. Anaesthesia and Intensive Care 2010;38(5):894‐9. [PUBMED: 20865875] [DOI] [PubMed] [Google Scholar]
Lin 2016 {published data only}
- Lin Y, Li Q, Liu J, Yang R, Liu J. Comparison of continuous epidural infusion and programmed intermittent epidural bolus in labor analgesia. Therapeutics and Clinical Risk Management 2016;12:1107‐12. [PUBMED: 27471390] [DOI] [PMC free article] [PubMed] [Google Scholar]
Salim 2005 {published data only}
- Salim R, Nachum Z, Moscovici R, Lavee M, Shalev E. Continuous compared with intermittent epidural infusion on progress of labor and patient satisfaction. Obstetrics and Gynaecology 2005;106(2):301‐6. [PUBMED: 16055579] [DOI] [PubMed] [Google Scholar]
Sia 2007 {published data only}
- Sia AT, Lim Y, Ocampo C. A comparison of a basal infusion with automated mandatory boluses in parturient‐controlled epidural analgesia during labor. Anesthesia and Analgesia 2007;104(3):673‐8. [PUBMED: 17312228] [DOI] [PubMed] [Google Scholar]
Sia 2013 {published data only}
- Sia AT, Leo S, Ocampo CE. A randomised comparison of variable‐frequency automated mandatory boluses with a basal infusion for patient‐controlled epidural analgesia during labour and delivery. Anaesthesia 2013;68(3):267‐75. [DOI: 10.1111/anae.12093; PUBMED: 23278328] [DOI] [PubMed] [Google Scholar]
Wong 2006 {published data only}
- Wong CA, Ratliff JT, Sullivan JT, Scavone BM, Toledo P, McCarthy RJ. A randomized comparison of programmed intermittent epidural bolus with continuous epidural infusion for labor analgesia. Anesthesia and Analgesia 2006;102(3):904‐9. [PUBMED: 16492849] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Nunes 2014 {published data only}
- Nunes J, Nunes S, Veiga M, Rodrigues R, Seifert I. Programmed intermittent boluses: are we improving epidural labour analgesia?. European Journal of Anaesthesiology 2014;31:182‐83. [Google Scholar]
Patkar 2015 {published data only}
- Patkar CS, Vora K, Patel H, Shah V, Modi MP, Parikh G. A comparison of continuous infusion and intermittent bolus administration of 0.1% ropivacaine with 0.0002% fentanyl for epidural labor analgesia. Journal of Anaesthesiology Clinical Pharmacology 2015;31(2):234‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [PUBMED: 9310563] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gambling 1988
- Gambling DR, Yu P, Cole C, McMorland GH, Palmer L. A comparative study of patient controlled epidural analgesia (PCEA) and continuous infusion epidural analgesia (CIEA) during labour. Canadian Journal of Anaesthesia 1988;35(3):249‐54. [PUBMED: 3289769] [DOI] [PubMed] [Google Scholar]
George 2012
- Geroge RB, Allen TK, Habib AS. Intermittent epidural bolus compared with continuous epidural infusions for labor analgesia: a systematic review and meta‐analysis. Anesthesia and Analgesia 2013;116(1):133‐44. [PUBMED: 23223119 ] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed prior to 31 August 2017. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ. What is "quality of evidence" and why is it important to clinicians?. BMJ 2008;336(7651):995‐8. [PUBMED: 18456631] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hogan 2002
- Hogan Q. Distribution of solution in the epidural space: examination by cryomicrotome section. Regional Anaesthesia and Pain Medicine 2002;27(2):150‐6. [PUBMED: 11915061] [DOI] [PubMed] [Google Scholar]
Hozo 2005
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology 20 April 2005;5(13):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaynar 1999
- Kaynar AM, Shankar KB. Epidural infusion: continuous or bolus?. Anesthesia and Analgesia 1999;89(2):534. [PUBMED: 10439786] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
References to other published versions of this review
Sng 2014
- Sng BL, Zeng Y, Leong WL, Oh TT, Siddiqui FJ, Assam PN, et al. Automated mandatory bolus versus basal infusion for maintenance of epidural analgesia in labour. Cochrane Database of Systematic Reviews 2014, Issue 10. [DOI: 10.1002/14651858.CD011344] [DOI] [PMC free article] [PubMed] [Google Scholar]


