Abstract
Cough is a physiological defense reflex for protecting the airways from aspiration and irritation. Thus, roles of environmental triggers are postulated in the pathogenesis of chronic cough. There are several lines of epidemiological evidence demonstrating the relationships between environmental irritant and pollutant exposure and chronic cough. However, positive findings from cross-sectional studies just reflect the protective nature of cough but may not properly address the true impact of environmental triggers. If harmful inhalation is repeated, cough may be seen as chronic but indeed is protective in nature. Therefore, long-term residual outcomes would be the key for understanding the effects of environmental triggers on chronic cough. The present review aims to summarize the associations between chronic cough and environmental pollutants or irritant exposure, with a focus on the long-term residual effects of (1) chronic persistent exposure and (2) acute high-intensity exposure on chronic cough, and also to examine (3) whether childhood irritant/pollutant exposure may increase the risk of chronic cough in adulthood.
Keywords: Cough, Pollutant, Irritant, Hypersensitivity, Inflammation, Epidemiology
INTRODUCTION
Chronic cough is a multifactorial syndrome commonly presenting as cough hypersensitivity in adults [1,2]. Intrinsically, cough is a physiological defense reflex for protecting the airways from aspiration, infection or irritation. However, cough becomes a disease when the reflex is dysregulated. Indeed, chronic cough is a cause of significant morbidity, particularly in terms of the quality of life and daily activity [3].
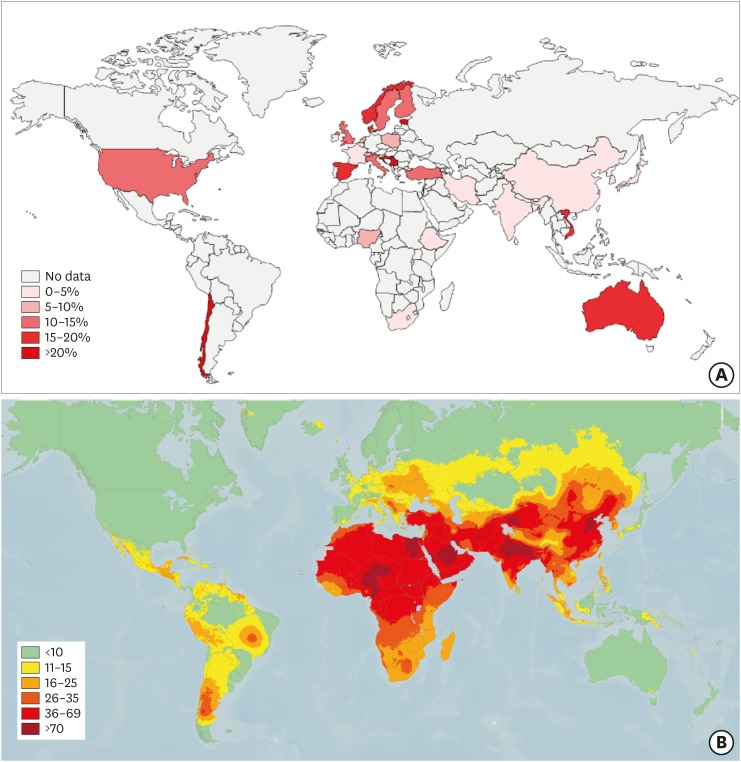
Given the intrinsic function of cough reflex, the roles of environmental triggers are postulated in the pathogenesis of chronic cough. However, there is an unexpectedly large gap between chronic cough prevalence and air pollutant level. While the air pollution level is higher in Asia [4], chronic cough is more prevalent in Europe and America [5]. The annual mean level of fine particulate matter with a diameter of 2.5 μg/m3 or less (PM2.5), an indicator for ambient air pollution, is high (≥25 μg/m3) in many parts of Asia [4], however, the prevalence of chronic cough is just less than half of that in Europe, America, and Oceania [5] (Fig. 1). This discrepancy is supposed to be attributed to a regional difference in comorbidity underlying chronic cough, such as reflux and asthma [6], and the roles of environmental triggers for chronic cough may be questioned.
Fig. 1. Maps showing (A) the prevalence of chronic cough in general adult populations (reproduced from Song et al., Eur Respir J 2015;45:1479-81, with permission of European Respiratory Society [5]) and (B) modeled annual mean PM2.5 (particulate matter with a diameter of 2.5 μg/m3 or less) for the year 2016 (reprinted from Global ambient air pollution [Internet]. World Health Organization [cited 2018 Mar 20]. Available from: http://maps.who.int/airpollution/).
There are several lines of epidemiological evidence demonstrating the relationships between environmental trigger exposure and chronic cough. Exposure to various air pollutants and irritants, such as ambient particulate matter, cigarette smoke, biomass fuel or occupational dust and gas, has been associated with the chronic cough prevalence in different populations [6,7,8]. However, positive findings from cross-reactional studies may just reflect the protective nature of cough, but not properly address the true impact of environmental triggers on chronic cough. If harmful inhalation is repeated, cough may be seen as chronic but indeed is protective in nature. Characteristics of cough observed in patients seeking medical care for chronic cough are hypersensitivity, which is commonly triggered by trivial stimuli such as cold air, perfume, talking or eating [2]. Therefore, long-term residual outcomes would be the key for understanding the effects of an environmental pollutant or irritant on chronic cough.
In this review, we summarize the general evidence on the associations between chronic cough and environmental pollutants or irritant exposure, but with a particular focus on the long-term residual effects of (1) chronic persistent pollutant and irritant exposure and (2) acute high-intensity exposure on chronic cough, and we also reviewed (3) whether childhood irritant/pollutant exposure may increase the risk of chronic cough in adulthood.
LONG-TERM RESIDUAL EFFECTS OF CHRONIC REPEATED POLLUTANT/IRRITANT EXPOSURE ON CHRONIC COUGH
First, effects of chronic repeated occupational irritant exposure have been examined in several longitudinal studies. In a 13-year longitudinal study of 2,730 adults in Cracow, Poland (1968–1981), the prolonged occupational dust exposure during the five years of follow-up, defined by both positive exposures in 1968 and 1973, significantly increased the risk of chronic cough in females (vs. no exposure [defined by both negative exposure in 1968 and 1973]), with an odds ratio [OR] of 1.19 (95% confidence interval [95% CI], 1.2–3.0) [9]. In a 3-year follow-up of 8,967 adult cohort participants (aged 45–64 years) in the Atherosclerosis Risk in Communities study, compared to those in managerial and administrative support jobs, an increased risk of new-onset chronic cough was found for mechanics and repairers (relative risk [RR], 1.81; 95% CI, 1.02–3.21) and for cleaning and building service workers (RR, 1.85; 95% CI, 1.01–3.37) [10]. In a recent 20-year follow-up study of 8,794 adult participants in the European Community Respiratory Health Survey cohort, occupational metal exposure was particularly associated with an increased incidence of chronic cough (RR, 1.29; 95% CI, 1.02–1.64) and chronic bronchitis (defined by chronic cough and phlegm; RR, 1.70; 95% CI, 1.16–2.50) among 12 different categorized occupational chemical exposures [11]. The latter [11] was the largest-scale longitudinal study utilizing a common standardized tool, i.e., Job Exposure Matrix, to assess the level of occupational exposure. However, none of these studies specifically examined any long-term ‘residual’ effects of such exposure.
Practically, it is difficult to differentiate effects of a certain trigger from various irritants exposed over a long time period in a large population. Thus, effects of a specific exposure might be better seen in studies of a specific worker population. In a case-control study for effects of irritant fume exposure resulting from glass bottle manufacturing, the occupational exposure was associated with a higher prevalence of upper respiratory symptoms including cough and enhanced cough reflex sensitivity to citric acid and capsaicin inhalation challenge; however, it was not related to wheezing or methacholine airway hyper-responsiveness [12]. In a prospective cohort study of 694 copier toner handling workers, inhaled powdered toner exposure significantly increased the risk of chronic cough (OR, 2.26; 95% CI, 1.13–4.53), but not of chronic phlegm, breathlessness, pulmonary dysfunction or chest X-ray abnormality during the follow-up period (for up to 10 years) [13]. Long-term effects of certain occupational exposure on chronic cough were also reported in several working populations [14,15]. However, the long-term remnant effects are still unknown.
Second, chronic air pollutant exposure effects have been examined in a few longitudinal studies. In a United States (US) longitudinal study of women (mean, 5.7-year follow-up), the prevalence of chronic bronchitis was associated with PM10 level (OR per interquartile range difference [of 5.8 μg/m3], 1.07; 95% CI, 1.01–1.13) [16]. The 12-year longitudinal assessment of the Swiss Cohort Study on Air Pollution and Lung Diseases in Adults cohort study, which consisted of 7,019 adults in their communities (aged 18 to 60 years), demonstrated that a decline in PM10 over the period (mean decline: 6.2±3.9 μg/m3) accompanied the decrease in chronic cough (179 fewer patients with chronic cough per 10,000 persons [95% CI, 30–328]) [17].
Third, cigarette smoking may have long-term consequences on cough. In the Scottish Heart Health Study, former heavy smokers (≥20 cigarettes/day) still had a higher rate of chronic cough than former light/moderate smokers (<20/day) and never smokers after 10 or more years of quitting cigarette smoking [18]. In a 13-year longitudinal study of adults in Cracow, Poland and Tucson, US, the incidence rate of chronic cough was reduced to approximately 73% in those who quit smoking compared to those who continued to smoke; however, the beneficial effects of smoking cessation was lower in patients with a heavy smoking history than in former light or moderate smokers [19], and thus suggesting possible cumulative dose effects.
LONG-TERM RESIDUAL EFFECTS OF ACUTE HIGH-LEVEL EXPOSURE ON CHRONIC COUGH
Effects of acute high-level irritant exposure have been reported in studies regarding patients exposed to high respiratory irritants during disasters. During the World Trade Center (WTC) collapse caused by a terrorists' attack in 2001, many citizens and rescue workers were exposed to various inhaled irritants and pollutants. In the first 6 months after the WTC collapse exposure, many firefighters developed persistent cough, called as “WTC cough syndrome,” and with a dose relationship to the exposure level [20]. This syndrome was found in 29.1% of the firefighters at baseline, but in 22.1% at follow-up (3–4 years later) [21]. During the first year, the most common lower respiratory symptom was frequent cough, reported by 54.2% of the firefighters, but the rate decreased to 15.7% during the fourth year [22]. In a 9-year, longitudinal follow-up study of 10,999 firefighters exposed to the WTC collapse, a serial pattern of symptom prevalence was examined and showed stabilization of the prevalence between years 5 and 9; approximately 9.5% of the exposed firefighters had a cough at year 9 [23]. The WTC cough syndrome differed, however, from common phenotypes of chronic cough. The majority of firefighters with WTC cough syndrome had upper airway symptoms such as nasal congestion, nasal drip and sore throat, gastroesophageal reflux disease (GERD), and lower airway symptoms such as dyspnea, wheeze, and chest discomfort [20]. Notably, 87% of these firefighters also had GERD. GERD may have resulted from dust-induced irritation of the gastroesophageal tract or from stress related to the terrorist attack and their diet, all of which facilitated the persistence of the airway irritation or inflammation. Other features were a reduction in lung function, i.e. reductions in forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1), but no change from the FEV1/FVC ratio determined before exposure, and air-trapping or bronchial wall thickening seen on chest radiography. Despite the normal FEV1/FVC ratios, airway obstruction was the predominant physiological abnormality. Bronchodilator response testing was positive in 63% of them and methacholine challenge testing in 24%. Radiographic evidence of parenchymal lung disease was uncommon, but air trapping was confirmed in many cases, suggesting that obstructive ventilator disturbances may be associated with WTC cough syndrome.
After a 6.4-magnitude earthquake in southern Taiwan in 2016, a survey was conducted for the incidence of respiratory symptoms in 519 firefighters who participated in the search and rescue during the 9-day field operation. Approximately 37% reported new or worsened respiratory symptoms even 3 weeks after the earthquake, and cough was the most frequent symptom (23%), followed by rhinorrhea or nasal congestion (22%) and chest tightness (6%) [24]. The mean duration of the exposure on site was 5.6 days, and the prevalence of symptoms was significantly associated with the self-reported degree of exposure to dust [24].
These observations suggest a potential that acute, high-level exposure to irritants may increase the risk of persistent cough. The mechanisms by which acute, high-level exposure leads to chronic cough are not clear, but they may be similar to those of reactive airway dysfunction syndrome. Inhalation of irritants is likely to induce the release of reactive oxygen species by airway epithelium, and oxidative stress can cause epithelial damage following increased releases of neuropeptides from the neuronal terminals and leading to neurogenic inflammation with release of substance P and neurokinins [25].
COULD CHILDHOOD EXPOSURE PREDISPOSE THE DEVELOPMENT OF CHRONIC COUGH IN ADULTHOOD?
Young children are supposed to be more vulnerable to environmental triggers due to the immaturity of their biological systems and higher air-intake per body weight compared to that of adults [26]. Therefore, it is postulated that exposure to an irritant/pollutant during early childhood may further increase the future risk of respiratory problems, including chronic cough.
In a study of 1,756 infants from the German part of the Traffic-Related Air Pollution on Childhood Asthma birth cohort study, the exposure to air pollutants during the first year of life was associated with cough without infection (at the age of 1 year) and dry cough at night (at ages of 1 and 2 years) [27]. In a survey of 11,860 children (aged 3 to 12 years) in Liaoning, a heavy industrial province in China, three air pollutant levels including total suspended particulates (TSP), sulfur dioxide (SO2), and NO2 were positively associated with risks of persistent cough (21%–28%), but not with persistent phlegm or current wheeze [28]. In a cohort study of children living in 6 cities in the US, the cough frequency was significantly correlated with the 24-hour mean concentrations of all 3 air pollutants, i.e., TSP, the sulfate fraction of TSP, and SO2, during the year preceding the examination [29]; and in subgroup analyses restricted to lifetime residents in the cities, the respiratory outcomes were also significantly associated with the lifetime mean TSP concentration [29]. A study of 9,881 adolescents (aged 11 to 20 years) in Hong Kong reported a 4.7% increase in the prevalence of cough when the average 30-day exposure to PM10 increased by 10 μg/m3 [30]; and the associations were also significant in nonsmokers and nonasthmatics [30]. In the Cincinnati Childhood Allergy and Air Pollution Study, a birth cohort study, traffic exhaust exposure showed a dose response with the risk of recurrent dry night cough during early childhood (at ages of 1, 2, and 3) [31]. Also, persistent cough was more common when these children were exposed to environmental tobacco smoke (ETS) at home and also when their home or classroom was close to the main road or a factory [28].
However, there are very few studies regarding the long-term remnant effects of childhood airway irritant exposure on chronic cough during adulthood. In the Singapore Chinese Health Study, approximately 35,000 ‘never smokers’ were followed up for a period of mean 5.8 years, and it was determined that living with a smoker before the age of 18 was significantly associated with a future risk of chronic dry cough (vs. no ETS exposure; OR, 2.1; 95% CI, 1.4–3.3) [32]. Notably, the OR was higher for those exposed during childhood only (OR, 4.03; 95% CI, 1.96–8.29) than for those exposed during adulthood only (OR, 1.57; 95% CI, 0.80–3.08) [32]. In a longitudinal follow-up study of 985 children in the WTC Health Registry who were exposed to the WTC collapse environment (aged 0 to 12 years at the exposure in 2001), respiratory symptoms, i.e., cough plus shortness of breath and/or wheeze, were present in 14.4% of them, as seen in 2007–2008. However, the prevalence of symptoms was greater in younger children aged 5–10 years at the time of exposure (OR, 2.2; 95% CI, 1.2–3.9) than in adolescents aged 11–17 years at the time of their exposure (OR, 1.7; 95% CI, 0.9–3.2) [33].
EXPERIMENTAL EVIDENCE FOR ENVIRONMENTAL TRIGGERS FOR CHRONIC COUGH
Mechanisms by which environmental factors trigger chronic cough are not fully understood but may be partly inferred from experimental studies. Transient receptor potential channels are widely present in sensory nerve endings and may be relevant to environmental trigger effects. In particular, the transient receptor potential ankyrin-1 (TRPA1) channel may be important in irritant-induced cough, as it is activated by a wide range of irritants, including isothiocyanate, acrolein or cinnamaldehyde, all of which are preset in air pollutants and cigarette smoke and may sense cellular oxidative stress [34,35]. Robinson et al. [36] have recently demonstrated a direct interaction between diesel exhaust particles and chemo-sensitive C-fivers in anesthetized guinea pigs and isolated human vagus nerve and which was mediated by TRPA1 and oxidative stress pathways.
Airway nerve density and sensory neuron functional or phenotypic profiles may change by interaction with allergens or viral infection [37,38], but the neural plasticity may also occur in response to air pollutants and irritant exposure. Exposure to cigarette smoke during the prenatal and early postnasal critical period induced airway hyper-reactivity and hyper-innervation of the airway sensory nerve in mice [39]. In guinea pigs exposed to cigarette smoke, the number of coughs evoked by capsaicin inhalation was significantly increased compared with those of the air-exposed controls [40]. ETS exposure over a period of time equivalent to human childhood in young guinea pigs induced recruiting substance P in vagal sensory afferent fibers and resulted in an augmentation of evoked synaptic transmission between the primary sensory fibers and second-order neurons in the nucleus tractus solitaries [41]. In a guinea pig experiment performed by Lv et al. [42] using PM2.5 as the stimulant, a 3-week exposure to PM2.5 upregulated the expression of TRPV1 in sensory neurons and enhanced cough reflex sensitivity to citric acid and which was dependent on the TRPV1 pathway.
Fang et al. [43] recently investigated the effects of traffic-related air pollution (TRAP) on cough response and airway inflammation. In nonallergic guinea pigs, the TRAP exposure (for 7 or 14 days) increased the cough frequency (measured in citric acid and allyl isothiocyanate challenge) and induced nonatopic but eosinophilic airway inflammation. Epithelial cytokine release such as interleukin-33 and thymic stromal lymphopoietin and subsequent induction of type 2 innate lymphoid cells were suggested as the potential mechanism. These findings also suggest the potential roles of air pollutant in the pathogenesis of eosinophilic bronchitis which is frequently nonatopic [43].
CLINICAL IMPLICATIONS
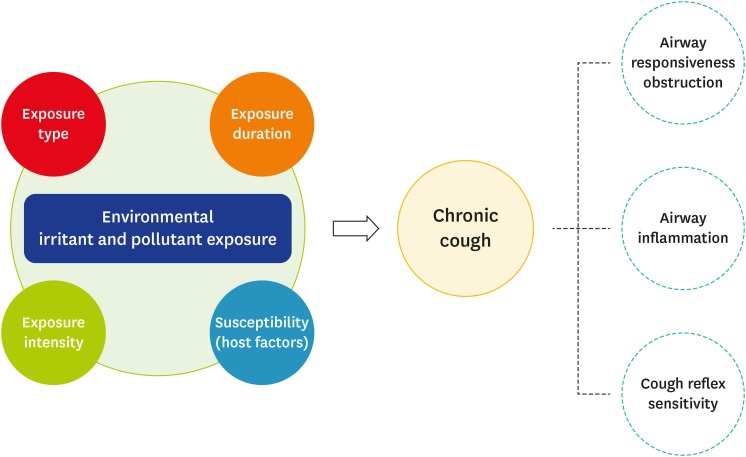
As reviewed above, current epidemiological and experimental evidence indicates that environmental irritant or pollutant exposure may potentially trigger chronic cough. Thus, it is recommended to assess the type, intensity and duration of a specific exposure and also consider host factors such as patient age at the exposure or the comorbidity (Fig. 2). Recent clinical practice guidelines recommend routine history taking of occupational and environmental triggers in adult patients presenting with chronic cough [7]. Associated clinical phenotypes are still unclear but likely to be dependent on the type and intensity of such exposure, which may include chronic bronchitis, eosinophilic bronchitis or hyper-reactive airway obstructive diseases.
Fig. 2. Environmental triggers for chronic cough. Several components – such as type, intensity and duration of exposure and host susceptibility (e.g., age at exposure and comorbidity) may be determinants for the incidence and phenotypes of chronic cough.
CONCLUSION
In this paper, we reviewed possible long-term or residual effects of environmental trigger exposure on chronic cough. There are significant associations between environmental pollutants, irritant exposure and chronic cough seen in cross-sectional studies. However, there are still few longitudinal studies to confirm the long-term residual effects. Available evidence suggests that both chronic persistent and acute high-intensity exposures may trigger chronic cough. It is still unclear whether early-life exposure to an environmental pollutant and irritant leads to chronic cough in adulthood, but a few longitudinal studies have suggested that this is also likely. Effects and mechanisms of airway irritant or pollutant exposure may be dependent on types and intensity of exposure, but may include neuronal changes, airway inflammation or airway hyper-reactivity. Given the major significance, further research is warranted in order to understand the long-term effects and mechanisms and prevent the adverse effects of environmental irritant and pollutant exposure on chronic cough.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Morice AH, Millqvist E, Belvisi MG, Bieksiene K, Birring SS, Chung KF, Dal Negro RW, Dicpinigaitis P, Kantar A, McGarvey LP, Pacheco A, Sakalauskas R, Smith JA. Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J. 2014;44:1132–1148. doi: 10.1183/09031936.00218613. [DOI] [PubMed] [Google Scholar]
- 2.Song WJ, Morice AH. Cough hypersensitivity syndrome: a few more steps forward. Allergy Asthma Immunol Res. 2017;9:394–402. doi: 10.4168/aair.2017.9.5.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.French CL, Irwin RS, Curley FJ, Krikorian CJ. Impact of chronic cough on quality of life. Arch Intern Med. 1998;158:1657–1661. doi: 10.1001/archinte.158.15.1657. [DOI] [PubMed] [Google Scholar]
- 4.Song WJ, Wong GWK. Changing trends and challenges in the management of asthma in Asia. J Allergy Clin Immunol. 2017;140:1272–1274. doi: 10.1016/j.jaci.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, Kim S, Jo EJ, Kim MH, Plevkova J, Park HW, Cho SH, Morice AH. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J. 2015;45:1479–1481. doi: 10.1183/09031936.00218714. [DOI] [PubMed] [Google Scholar]
- 6.Song WJ, Faruqi S, Klaewsongkram J, Lee SE, Chang YS. Chronic cough: an Asian perspective. Part 1: epidemiology. Asia Pac Allergy. 2015;5:136–144. doi: 10.5415/apallergy.2015.5.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tarlo SM, Altman KW, Oppenheimer J, Lim K, Vertigan A, Prezant D, Irwin RS, Adams TM, Altman KW, Azoulay E, Barker AF, Birring SS, Blackhall F, Bolser DC, Boulet LP, Braman SS, Brightling C, Callahan-Lyon P, Chang AB, Ebihara S, El Solh AA, Escalante P, Feinstein A, Field SK, Fisher D, French CT, Gibson P, Gold P, Gould MK, Grant C, Harding SM, Harnden A, Hill AT, Irwin RS CHEST Expert Cough Panel. Occupational and environmental contributions to chronic cough in adults: Chest Expert Panel Report. Chest. 2016;150:894–907. doi: 10.1016/j.chest.2016.07.029. [DOI] [PubMed] [Google Scholar]
- 8.Szram J, Schofield SJ, Cosgrove MP, Cullinan P. Welding, longitudinal lung function decline and chronic respiratory symptoms: a systematic review of cohort studies. Eur Respir J. 2013;42:1186–1193. doi: 10.1183/09031936.00206011. [DOI] [PubMed] [Google Scholar]
- 9.Krzyzanowski M, Jedrychowski W. Occupational exposure and incidence of chronic respiratory symptoms among residents of Cracow followed for 13 years. Int Arch Occup Environ Health. 1990;62:311–317. doi: 10.1007/BF00640839. [DOI] [PubMed] [Google Scholar]
- 10.Mirabelli MC, London SJ, Charles LE, Pompeii LA, Wagenknecht LE. Occupation and three-year incidence of respiratory symptoms and lung function decline: the ARIC Study. Respir Res. 2012;13:24. doi: 10.1186/1465-9921-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lytras T, Kogevinas M, Kromhout H, Carsin AE, Antó JM, Bentouhami H, Weyler J, Heinrich J, Nowak D, Urrutia I, Martínez-Moratalla J, Gullón JA, Vega AP, Raherison Semjen C, Pin I, Demoly P, Leynaert B, Villani S, Gíslason T, Svanes Ø, Holm M, Forsberg B, Norbäck D, Mehta AJ, Probst-Hensch N, Benke G, Jogi R, Torén K, Sigsgaard T, Schlünssen V, Olivieri M, Blanc PD, Watkins J, Bono R, Buist AS, Vermeulen R, Jarvis D, Zock JP. Occupational exposures and incidence of chronic bronchitis and related symptoms over two decades: the European Community Respiratory Health Survey. Occup Environ Med. 2019;76:222–229. doi: 10.1136/oemed-2018-105274. [DOI] [PubMed] [Google Scholar]
- 12.Gordon SB, Curran AD, Turley A, Wong CH, Rahman SN, Wiley K, Morice AH. Glass bottle workers exposed to low-dose irritant fumes cough but do not wheeze. Am J Respir Crit Care Med. 1997;156:206–210. doi: 10.1164/ajrccm.156.1.9610042. [DOI] [PubMed] [Google Scholar]
- 13.Nakadate T, Yamano Y, Yamauchi T, Okubo S, Nagashima D. Assessing the chronic respiratory health risk associated with inhalation exposure to powdered toner for printing in actual working conditions: a cohort study on occupationally exposed workers over 10 years. BMJ Open. 2018;8:e022049. doi: 10.1136/bmjopen-2018-022049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Kampen V, Hoffmeyer F, Deckert A, Kendzia B, Casjens S, Neumann HD, Buxtrup M, Willer E, Felten C, Schöneich R, Brüning T, Raulf M, Bünger J. Effects of bioaerosol exposure on respiratory health in compost workers: a 13-year follow-up study. Occup Environ Med. 2016;73:829–837. doi: 10.1136/oemed-2016-103692. [DOI] [PubMed] [Google Scholar]
- 15.Hedmer M, Karlsson JE, Andersson U, Jacobsson H, Nielsen J, Tinnerberg H. Exposure to respirable dust and manganese and prevalence of airways symptoms, among Swedish mild steel welders in the manufacturing industry. Int Arch Occup Environ Health. 2014;87:623–634. doi: 10.1007/s00420-013-0896-3. [DOI] [PubMed] [Google Scholar]
- 16.Hooper LG, Young MT, Keller JP, Szpiro AA, O'Brien KM, Sandler DP, Vedal S, Kaufman JD, London SJ. Ambient air pollution and chronic bronchitis in a cohort of U.S. women. Environ Health Perspect. 2018;126:027005. doi: 10.1289/EHP2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schindler C, Keidel D, Gerbase MW, Zemp E, Bettschart R, Brändli O, Brutsche MH, Burdet L, Karrer W, Knöpfli B, Pons M, Rapp R, Bayer-Oglesby L, Künzli N, Schwartz J, Liu LJ, Ackermann-Liebrich U, Rochat T SAPALDIA Team. Improvements in PM10 exposure and reduced rates of respiratory symptoms in a cohort of Swiss adults (SAPALDIA) Am J Respir Crit Care Med. 2009;179:579–587. doi: 10.1164/rccm.200803-388OC. [DOI] [PubMed] [Google Scholar]
- 18.Brown CA, Crombie IK, Smith WC, Tunstall-Pedoe H. The impact of quitting smoking on symptoms of chronic bronchitis: results of the Scottish Heart Health Study. Thorax. 1991;46:112–116. doi: 10.1136/thx.46.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krzyzanowski M, Robbins DR, Lebowitz MD. Smoking cessation and changes in respiratory symptoms in two populations followed for 13 years. Int J Epidemiol. 1993;22:666–673. doi: 10.1093/ije/22.4.666. [DOI] [PubMed] [Google Scholar]
- 20.Prezant DJ, Weiden M, Banauch GI, McGuinness G, Rom WN, Aldrich TK, Kelly KJ. Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med. 2002;347:806–815. doi: 10.1056/NEJMoa021300. [DOI] [PubMed] [Google Scholar]
- 21.Niles JK, Webber MP, Gustave J, Cohen HW, Zeig-Owens R, Kelly KJ, Glass L, Prezant DJ. Comorbid trends in World Trade Center cough syndrome and probable posttraumatic stress disorder in firefighters. Chest. 2011;140:1146–1154. doi: 10.1378/chest.10-2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Webber MP, Gustave J, Lee R, Niles JK, Kelly K, Cohen HW, Prezant DJ. Trends in respiratory symptoms of firefighters exposed to the world trade center disaster: 2001-2005. Environ Health Perspect. 2009;117:975–980. doi: 10.1289/ehp.0800291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weakley J, Webber MP, Gustave J, Kelly K, Cohen HW, Hall CB, Prezant DJ. Trends in respiratory diagnoses and symptoms of firefighters exposed to the World Trade Center disaster: 2005-2010. Prev Med. 2011;53:364–369. doi: 10.1016/j.ypmed.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Wu CL, Lan FY, Chen BL, Chang RH, Chang WH, Pan ST, Fang PH, Lu CH, Lin CH. Respiratory symptoms among search and rescue workers who responded to the 2016 Taiwan earthquake. Occup Environ Med. 2018;75:639–646. doi: 10.1136/oemed-2018-105027. [DOI] [PubMed] [Google Scholar]
- 25.Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med. 2014;370:640–649. doi: 10.1056/NEJMra1301758. [DOI] [PubMed] [Google Scholar]
- 26.Bell ML, Zanobetti A, Dominici F. Evidence on vulnerability and susceptibility to health risks associated with short-term exposure to particulate matter: a systematic review and meta-analysis. Am J Epidemiol. 2013;178:865–876. doi: 10.1093/aje/kwt090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gehring U, Cyrys J, Sedlmeir G, Brunekreef B, Bellander T, Fischer P, Bauer CP, Reinhardt D, Wichmann HE, Heinrich J. Traffic-related air pollution and respiratory health during the first 2 yrs of life. Eur Respir J. 2002;19:690–698. doi: 10.1183/09031936.02.01182001. [DOI] [PubMed] [Google Scholar]
- 28.Pan G, Zhang S, Feng Y, Takahashi K, Kagawa J, Yu L, Wang P, Liu M, Liu Q, Hou S, Pan B, Li J. Air pollution and children's respiratory symptoms in six cities of Northern China. Respir Med. 2010;104:1903–1911. doi: 10.1016/j.rmed.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Ware JH, Ferris BG, Jr, Dockery DW, Spengler JD, Stram DO, Speizer FE. Effects of ambient sulfur oxides and suspended particles on respiratory health of preadolescent children. Am Rev Respir Dis. 1986;133:834–842. [PubMed] [Google Scholar]
- 30.Lai HK, Ho SY, Wong CM, Mak KK, Lo WS, Lam TH. Exposure to particulate air pollution at different living locations and respiratory symptoms in Hong Kong--an application of satellite information. Int J Environ Health Res. 2010;20:219–230. doi: 10.1080/09603120903511119. [DOI] [PubMed] [Google Scholar]
- 31.Sucharew H, Ryan PH, Bernstein D, Succop P, Khurana Hershey GK, Lockey J, Villareal M, Reponen T, Grinshpun S, LeMasters G. Exposure to traffic exhaust and night cough during early childhood: the CCAAPS birth cohort. Pediatr Allergy Immunol. 2010;21(2 Pt 1):253–259. doi: 10.1111/j.1399-3038.2009.00952.x. [DOI] [PubMed] [Google Scholar]
- 32.David GL, Koh WP, Lee HP, Yu MC, London SJ. Childhood exposure to environmental tobacco smoke and chronic respiratory symptoms in non-smoking adults: the Singapore Chinese Health Study. Thorax. 2005;60:1052–1058. doi: 10.1136/thx.2005.042960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stellman SD, Thomas PA, S Osahan S, Brackbill RM, Farfel MR. Respiratory health of 985 children exposed to the World Trade Center disaster: report on world trade center health registry wave 2 follow-up, 2007-2008. J Asthma. 2013;50:354–363. doi: 10.3109/02770903.2013.776073. [DOI] [PubMed] [Google Scholar]
- 34.Birrell MA, Belvisi MG, Grace M, Sadofsky L, Faruqi S, Hele DJ, Maher SA, Freund-Michel V, Morice AH. TRPA1 agonists evoke coughing in guinea pig and human volunteers. Am J Respir Crit Care Med. 2009;180:1042–1047. doi: 10.1164/rccm.200905-0665OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morice AH. TRPA1 receptors in chronic cough. Pulm Pharmacol Ther. 2017;47:42–44. doi: 10.1016/j.pupt.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 36.Robinson RK, Birrell MA, Adcock JJ, Wortley MA, Dubuis ED, Chen S, McGilvery CM, Hu S, Shaffer MSP, Bonvini SJ, Maher SA, Mudway IS, Porter AE, Carlsten C, Tetley TD, Belvisi MG. Mechanistic link between diesel exhaust particles and respiratory reflexes. J Allergy Clin Immunol. 2018;141:1074–84.e9. doi: 10.1016/j.jaci.2017.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Undem BJ, Taylor-Clark T. Mechanisms underlying the neuronal-based symptoms of allergy. J Allergy Clin Immunol. 2014;133:1521–1534. doi: 10.1016/j.jaci.2013.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song WJ, Chang YS. Cough hypersensitivity as a neuro-immune interaction. Clin Transl Allergy. 2015;5:24. doi: 10.1186/s13601-015-0069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu ZX, Hunter DD, Kish VL, Benders KM, Batchelor TP, Dey RD. Prenatal and early, but not late, postnatal exposure of mice to sidestream tobacco smoke increases airway hyperresponsiveness later in life. Environ Health Perspect. 2009;117:1434–1440. doi: 10.1289/ehp.0800511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Belvisi MG, Birrell MA, Khalid S, Wortley MA, Dockry R, Coote J, Holt K, Dubuis E, Kelsall A, Maher SA, Bonvini S, Woodcock A, Smith JA. Neurophenotypes in airway diseases. Insights from translational cough studies. Am J Respir Crit Care Med. 2016;193:1364–1372. doi: 10.1164/rccm.201508-1602OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sekizawa S, Chen CY, Bechtold AG, Tabor JM, Bric JM, Pinkerton KE, Joad JP, Bonham AC. Extended secondhand tobacco smoke exposure induces plasticity in nucleus tractus solitarius second-order lung afferent neurons in young guinea pigs. Eur J Neurosci. 2008;28:771–781. doi: 10.1111/j.1460-9568.2008.06378.x. [DOI] [PubMed] [Google Scholar]
- 42.Lv H, Yue J, Chen Z, Chai S, Cao X, Zhan J, Ji Z, Zhang H, Dong R, Lai K. Effect of transient receptor potential vanilloid-1 on cough hypersensitivity induced by particulate matter 2.5. Life Sci. 2016;151:157–166. doi: 10.1016/j.lfs.2016.02.064. [DOI] [PubMed] [Google Scholar]
- 43.Fang Z, Huang C, Zhang JJ, Xie J, Dai S, Ge E, Xiang J, Yao H, Huang R, Bi X, Wang B, Zhong N, Lai K. Traffic-related air pollution induces non-allergic eosinophilic airway inflammation and cough hypersensitivity in guinea-pigs. Clin Exp Allergy. 2019;49:366–377. doi: 10.1111/cea.13308. [DOI] [PubMed] [Google Scholar]