Abstract
Background
The prevalence of allergy among Surabaya school children is currently unknown.
Objective
To identify the prevalence of the common allergic sensitization and allergic diseases among school children and undergraduate students in suburban of Surabaya by epidemiologic data collection.
Methods
A multistage simple random sampling was done to select 5 primary schools, 8 secondary schools (4 of junior high schools and senior high schools, respectively), and 1 university from 5 districts in Surabaya city. Out of 550 invited respondents, 499 (128 primary school, 221 secondary school, and 150 undergraduate) respondents gave their consent. A complete personal history, allergic symptoms, environmental exposure of common allergens was obtained from interview and the physical examinations were performed. Skin prick test (SPT) was done using 45 different allergen extracts. Total serum IgE and specific IgE radioallergosorbent test levels were measured for respondents with allergic manifestations.
Results
There was an increasing SPT positivity among study respondents, from primary school, secondary school, to undergraduate students (21.90%, 28.95%, to 45.30% respectively). Cockroach (42.85%) and fungi/mold spore (42.85%) were the most common allergens in primary school children. House dust mites was the most common allergen in secondary school (63.16%) and undergraduate students (58.82%). Urticaria and rhinitis were the commonest allergic diseases manifestation. History of atopy was positive in 60.79% of the allergic respondents.
Conclusion
The prevalence of allergic sensitization among school children and undergraduate students in Surabaya suburb areas were increased compared to previous estimates in 1998. While house dust mites are known as important allergens, surprisingly cockroach was the common allergen among the younger school children.
Keywords: Allergy, Schoolchildren, Skin prick test, Epidemiologic studies, Fungi/mold spore
INTRODUCTION
The prevalence of allergic diseases is dramatically increased in the last decades. Some factors are believed to contribute to that phenomenon i.e., more affluent and urbanized society, increased outdoor and indoor pollution, changes in life style and dietary habits, climate change and reduced biodiversity [1]. Allergies now affect up to 30% to 40% of the population worldwide with the children and young adults bear the greatest burden of these diseases as the escalation of the prevalence of the diseases is mostly seen in these populations [2]. But there is a wide variation in the prevalence of allergic diseases between developed and developing countries, being lowest in the later [3]. Allergy which includes asthma among the urban population is considered to be related to westernized life style [4]. While rural population in the developing countries are more exposed to environmental microorganisms which protect them from allergy and atopy [5,6].
Indonesia has the lowest prevalence of asthma, allergic rhinitis, and eczema symptoms as showed by the results of The International Study of Asthma and Allergies in Childhood (ISAAC) in 2007 [3,7,8]. Surabaya is the second biggest city in Indonesia, but unfortunately was not involved in the ISAAC study. The fast economic growth in Surabaya give rise to the increasing number of city inhabitants which in turn contributes to growing numbers of cars, motorcycles, and creates high levels of air pollution. Many areas in the city can no longer support the requirements of the people and become slump areas. This condition presents a unique situation where air pollution and the low hygiene and sanitation have an opposing influence on the pathogenesis of allergic diseases [9,10]. To date, the prevalence of allergic sensitizations and diseases among Surabaya's school children and undergraduate students are unknown. A cross-sectional epidemiologic study was conducted to respond to the following questions: (1) what is the prevalence of allergen sensitization (defined as skin prick test [SPT] positivity) and allergic diseases among school children and undergraduate students in Surabaya, and (2) what are the common types of allergen sensitizations and allergic diseases in these populations.
MATERIALS AND METHODS
Subject recruitment
Surabaya city consisted of 5 districts. A complete data of primary schools, secondary schools, university was obtained from the Surabaya city Education Office. By using a multistage simple random sampling, 5 primary schools, 8 secondary schools (4 of each junior high school and senior high schools), and 1 university were chosen to represent school children and undergraduate students of Surabaya city. Out of 550 invited students, 499 agreed to be involved in this study on voluntary basis. They were 128 primary school students, 221 secondary school students (112 of junior high schools and 109 of senior high schools), and 150 of undergraduate university students. Data of children from junior and senior high schools were combined under one category i.e., secondary school children. All respondent below 18 years old was briefed on the patient information and signed the informed consent together with their parent(s). While undergraduate students signed the consent on their own will.
Physical examinations and SPTs
A complete personal and family histories of allergy, allergic symptoms or diseases, environmental or home exposure of various common allergens were obtained, followed by the physical examinations. Allergen sensitizations, defined as SPTs positivity, were evaluated using 45 different inhalant and ingested allergen extracts (Inmunotek, Madrid, Spain). The list of allergen extracts used in this study as in Table 1. The diameters of the resulting wheals were measured in 2 dimensions and compared to a positive (histamine 10 mg/mL) and negative (diluent) controls. The perimeter of the wheals were marked using a felt tipped pen. Using a transparent tape over the marked wheals, results were transferred to a result sheet. Total serum IgE and specific IgE radioallergosorbent test (RAST) for selected allergens were also measured by a reference laboratory in Surabaya (Prodia Laboratory). The levels of serum total IgE were measured using standard enzyme-linked immunosorbent assay method on VIDAS equipment. Serum specific IgE levels were measured using radioallergosorbent technique on UniCAP equipment (Pharmacia, Uppsala, Sweden). Normal reference value for serum total IgE in adolescent/adult is <150 IU/L [11,12,13], while cutoff value for normal serum specific IgE (RAST) level is <0.35 kU/L [13,14,15].
Table 1. Allergen extracts used in this study and the results of skin prick test.
| No. | Allergen extracts* | Positive skin prict test | ||
|---|---|---|---|---|
| Primary school children (n = 128) | Secondary school children (n = 221) | Undergraduate students (n = 150) | ||
| 1 | Cat epithelium (catalog # E801) | 4 (3.13) | 6 (2.71) | 1 (0.67) |
| 2 | Dog dander (catalog # E802) | - | - | - |
| 3 | Chicken feather (catalog # E806) | - | 1 (0.45) | 1 (0.67) |
| 4 | Cow's dander (catalog # E808) | - | 1 (0.45) | 1 (0.67) |
| 5 | Horse's dander (catalog # E807) | - | - | - |
| 6 | House dust mite (catalog # S005) | 9 (7.03) | 43 (19.46) | 40 (26.67) |
| 7 | Dermatophagoides farinae (catalog # M602) | 11 (8.59) | 37 (16.74) | 35 (23.33) |
| 8 | Dermatophagoides pteronyssinus (catalog # M601) | 12 (9.38) | 25 (11.31) | 32 (21.33) |
| 9 | Grass pollen mix (catalog # TP27) | 2 (1.56) | 2 (0.90) | 3 (2.00) |
| 10 | Timothy grass pollen (catalog # G110) | 4 (3.13) | 6 (2.71) | 1 (0.67) |
| 11 | Mucor mucedo (catalog # P907) | 13 (10.16) | 19 (8.60) | 25 (16.67) |
| 12 | Rhizopus oryzae (catalog # P909) | 3 (2.34) | 1 (0.45) | - |
| 13 | Aspergilus niger (catalog # P903) | - | 1 (0.45) | - |
| 14 | Penicillium notatum (catalog # P908) | 1 (0.78) | - | - |
| 15 | Triticum aestivum (catalog # F235) | - | 1 (0.45) | - |
| 16 | Alternaria alternata (catalog # P901) | - | - | - |
| 17 | Periplaneta americana (catalog # I703) | 12 (9.38) | 25 (11.31) | 32 (21.33) |
| 18 | Peanut (catalog # F13) | 1 (0.78) | - | 1 (0.67) |
| 19 | Pea (catalog # F12) | 1 (0.78) | - | - |
| 20 | Chocolate (catalog # F93) | - | - | - |
| 21 | Chicken egg yolk (catalog # F75) | 1 (0.78) | - | 3 (2.00) |
| 22 | Chicken egg white (catalog # F1) | - | 2 (0.90) | 2 (1.33) |
| 23 | Chicken egg whole (catalog # F245) | 1 (0.78) | 2 (0.90) | 3 (2.00) |
| 24 | Rye flour (catalog # F5) | - | - | - |
| 25 | Wheat flour (catalog # F4) | - | 1 (0.45) | - |
| 26 | Crab (catalog # F23) | 3 (2.34) | 14 (6.33) | 28 (18.67) |
| 27 | Prawn (catalog # F24) | 1 (0.78) | 2 (0.90) | 8 (5.33) |
| 28 | Mussel (catalog # F37) | 1 (0.78) | - | 3 (2.00) |
| 29 | Fish mix 1 (catalog # MF10) | - | 1 (0.45) | 2 (1.33) |
| 30 | Fish mix 2 (catalog # MF11) | - | 1 (0.45) | 2 (1.33) |
| 31 | Mackerel (catalog # F206) | 1 (0.78) | 2 (0.90) | 3 (2.00) |
| 32 | Scallop (catalog # F32) | - | - | - |
| 33 | Chicken meat (catalog # F83) | - | - | 1 (0.67) |
| 34 | Meat mix - mamalians (catalog # MF01) | - | 1 (0.45) | 3 (2.00) |
| 35 | Meat mix - birds (catalog # MF02) | 1 (0.78) | 2 (0.90) | 4 (2.67) |
| 36 | Orange (catalog # F33) | 1 (0.78) | 1 (0.45) | 1 (0.67) |
| 37 | Melon (catalog # F87) | - | - | - |
| 38 | Watermelon (catalog # F329) | - | 2 (0.90) | 1 (0.67) |
| 39 | Banana (catalog # F92) | 3 (2.34) | - | - |
| 40 | Potato (catalog # F35) | 1 (0.78) | - | - |
| 41 | Cow's milk (catalog # F231) | - | 2 (0.90) | - |
| 42 | Latex (Hevea brasiliensis) (catalog # L001) | 1 (0.78) | 2 (0.90) | - |
| 43 | Bee venom (Apis mellifera) (catalog # HX2) | 1 (0.78) | 1 (0.45) | - |
| 44 | Clam (Mercenaria spp.) (catalog # F10) | 1 (0.78) | - | - |
| 45 | Juniperus oxicedrus (catalog # T521) | - | 1 (0.45) | - |
Values are presented as number (%).
*All allergen extracts were purchased from Inmunotek (Madrid, Spain).
Statistical analysis
All statistical analyses were performed using the SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA).
Ethics
Ethical approval for this study project was obtained from Health Research Ethics Committee of Dr. Soetomo General Hospital, Surabaya, Indonesia with certificate number: 44/Panke.KKE/2006.
RESULTS
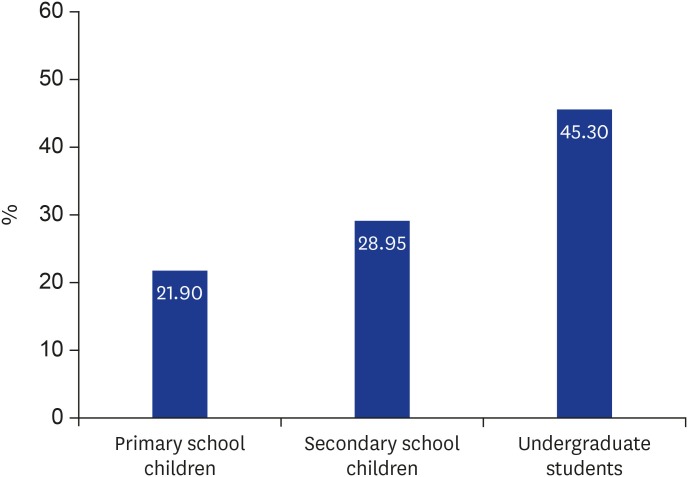
There was a trend of increasing allergic sensitization among school children and undergraduate students, being 21.9% among primary school children (aged 7 to 12 years), to 28.9% among secondary school children (aged 13 to 18 years), and to 45.3% among undergraduate students (aged >19 years) as in Fig. 1.
Fig. 1. The prevalence of allergic sensitization in Surabaya school children. There was a trend of increasing allergic sensitization among school children and undergraduate students. Allergic sensitization was defined as positive skin prick test result to one or more of 45 allergen extracts tested.
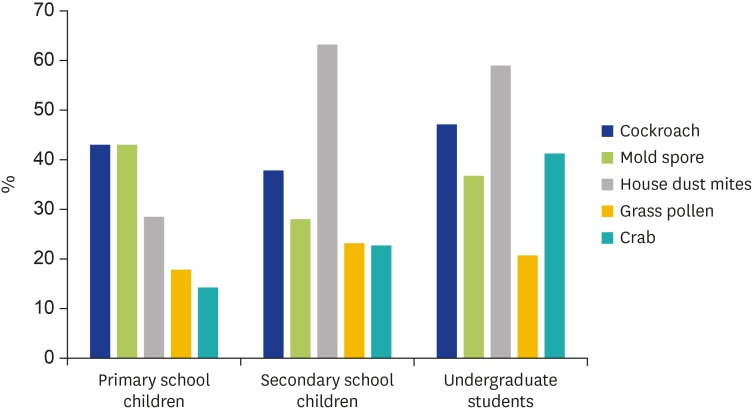
The distribution of skin test positivity for all allergens tested on the respondent is shown in Table 1. Among 28 primary school children with positive skin test, the most common sensitization was against cockroach, fungi/mold spore (both at 42.8%), house dust mites (28.6%), grass pollen (17.9%), and crab (14.3%). Among 64 secondary school children with positive skin test, the most common sensitization was against house dust mites (62.5%), followed by cockroach (37.5%), fungi/mold spore (28.1%), grass pollen (23.4%), and crab (21.9%). While among 68 undergraduate students with positive skin test, the most common sensitization was against house dust mites (58.8%), followed by cockroach (47.1%), crab (41.2%), fungi/mold spore (36.7%), and grass pollen (20.6%) (Fig. 2).
Fig. 2. The most common allergens in sensitized Surabaya school children. The coloured bar diagram showed the percentage of sensitization in a particular group of children. House dust mites were the most common allergens in secondary school children and undergraduate student. Cockroach and mold spore were quite dominant in all of the groups, and being the most common allergen in primary school children.
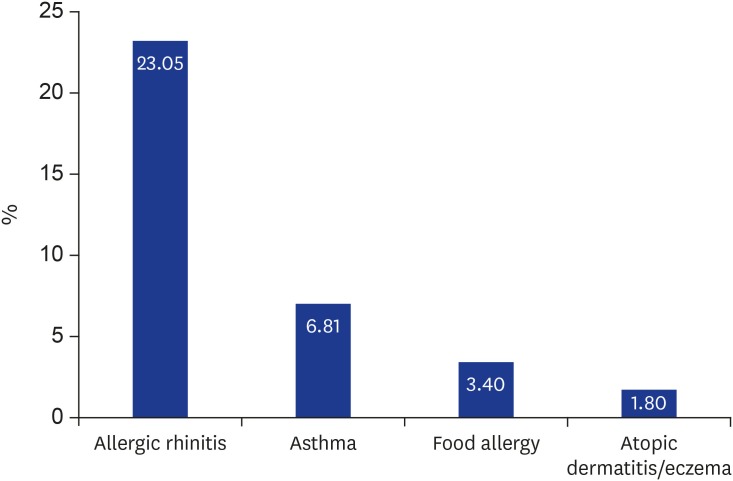
The information from the personal history prevails 278 respondents suffered from at least one allergic disease manifestations. The most common allergic disease found was allergic rhinitis (23.0%), followed by asthma (6.8%), food allergy (3.4%), and atopic dermatitis/eczema (1.8%) (Fig. 3). A substantial number of respondents actually suffered from urticaria (20.6%) but this data was not shown in Fig. 3 because this diagnosis category was not assessed in the ISAAC study.
Fig. 3. The common allergic diseases in Surabaya school children. Diagnosis of allergic disease was determined based on history of allergic symptoms, physical examination, and skin prick test or IgE examination result. Allergic rhinitis was the most common allergic disease manifestation in Surabaya school children.
Table 2 shows some factors (allergic disease inheritance, home and environmental allergen exposure) that may predispose the study respondent to allergic diseases. Out of 278 respondents with allergic disease manifestation, 169 (60.8%) had at least one of the parents (father, mother, or both) suffered from any allergic disease.
Table 2. Predisposing factors for allergic diseases in Surabaya school children.
| Variable | Primary school children with allergy (n = 45) | Secondary school children with allergy (n = 139) | Undergraduate students with allergy (n = 94) | Total (n = 278) | |
|---|---|---|---|---|---|
| Parental atopy | |||||
| Father | 24 (53.3) | 78 (56.1) | 49 (52.1) | 151 (54.3) | |
| Mother | 27 (60.0) | 84 (60.4) | 58 (61.7) | 169 (60.8) | |
| None | 18 (40.0) | 55 (39.6) | 36 (38.3) | 109 (39.2) | |
| Birth order | |||||
| First | 30 (66.7) | 97 (69.8) | 65 (69.1) | 192 (69.1) | |
| Second | 9 (20.0) | 32 (23.0) | 29 (30.9) | 70 (25.2) | |
| Third | 2 (4.4) | 9 (6.5) | - | 11 (3.9) | |
| Fourth | 2 (4.4) | 1 (0.7) | - | 3 (1.1) | |
| Fifth | 2 (4.4) | - | - | 2 (0.7) | |
| House dust mite exposure | |||||
| Yes | 28 (62.2) | 85 (61.2) | 74 (78.7) | 187 (67.3) | |
| No | 17 (37.8) | 54 (38.8) | 20 (21.3) | 91 (32.7) | |
| Clean, hygienic home and environment | |||||
| Yes | 30 (66.7) | 94 (67.6) | 63 (67) | 187 (67.3) | |
| No | 15 (33.3) | 45 (32.4) | 31 (33) | 91 (32.7) | |
| Pet ownership | |||||
| Yes | 28 (62.2) | 54 (38.8) | 28 (29.8) | 110 (39.6) | |
| No | 17 (37.8) | 85 (61.2) | 66 (70.2) | 168 (60.4) | |
Values are presented as number (%).
DISCUSSION
This study showed a trend of increasing prevalence of skin test positivity among school children and students with the increasing age (from primary school children to undergraduate students). It gives an indication that although Indonesia belongs to the developing countries, the prevalence of allergic diseases in school children and undergraduate students of metropolitan cities such as Surabaya shows a pattern more similar to that of the developed countries [16,17,18,19].
The most common allergic disease in this study was allergic rhinitis, as prevailed at 23% is within the estimation for the worldwide (10%–30% of the population) but lower as compared to that of similar population-based study in the Netherlands [16], Finland [17], Australia [18], or United States [19]. Compared to other cities in the South East Asian region, the rates in Surabaya were found to be higher than in Kota Bahru (Malaysia) [20] or Taoyuan (Taiwan) [21], but similar to metropolitan cities as Bangkok (Thailand) [22], or Metro Manila (Republic of The Philippines) [23]. Consistent to the results from those big cities and that of developed countries, the prevalence of asthma and atopic dermatitis/eczema in this study was also lower than the allergic rhinitis [16,17,18,19,20,21,22,23].
The present results were apparently higher than the previous reported prevalence for Indonesia in ISAAC study in 1998 [3]. According to the survey held in Bandung at that time, the estimate prevalence of allergic rhinitis in Indonesia was around 5% [3]. There are several factors that may explain the increasing prevalence of allergic diseases in Surabaya. Genetic factors within populations, such as atopy (history of allergic disease inheritance in the family), usually do not change in a decade, so researchers have postulated other causes from the environment for the increased prevalence of allergic diseases [24]. These include the so-called 'hygiene hypothesis,' which refers to a lack of immunological shift from Th2-dominant, infantile states to Th1-dominant, adult type responses during the early period of life as a result of decreased exposure to microbial antigens [1,9,25]. Other researchers also mentioned the important role of extrinsic antigens, including air pollution [26,27,28].
In accordance with the current concepts of the immunopathogenesis of allergic disorders [10], the majority of our study respondent with allergic disease manifestations had parental atopy. Most of them were also born as first child, and admitted the exposure of house dust mites allergens in their home or environment. There was a decreasing percentage of allergic disease from the first child to second child, to third child and so on. Pet ownership does not seem to have an effect. Most of the respondent claimed that they lived in clean and hygienic house and environment (data was obtained as a self-testimony from the interview and the exact conditions were not verified), but from the facts that cockroach and fungi/mold spore were found to be the common allergens among these children, we suspected that they live in damp houses with many food leftovers that might attract cockroach into their house.
Other factors may also play a role, such as decreased microbial exposure and the increased air pollution. With regards to the decreased exposure to microbial antigens, recent data on the use of antibiotics by doctors in Indonesia gave a strong supporting evidence [29,30,31,32]. Irrational use of antibiotics has become a common practice in developing countries, where the prevalence of infectious disease burden is aggravated by uncontrolled access to antibiotics. Twenty years ago, a survey in Jakarta revealed that doctors prescribed antibiotics to 94% of young children although they admit that the infection was of viral origin [29,30]. This practice did not change much to the present days as was shown by the results of The Antimicrobial Resistance in Indonesia ‘Prevalence and Prevention’ study held in Surabaya and Semarang [31]. Being less than 18 years of age and uninsured were independent determinants of antibiotic use. Furthermore, antibiotics without prescription can even be obtained over the counter in pharmacies and drug stores, although this has been prohibited by law [31,32]. Urban provenances, being adult, male sex, and having no health insurance were independent determinants of antibiotic self-medication [31,32]. This practice seemed so overwhelming in all areas of the city, and in that way might undo the protective effects of living in slump areas with unhygienic sanitation.
The role of air pollution in the rising trends in allergic respiratory diseases had been emphasized by the results of both epidemiological and laboratory studies [26,27,28]. Pollutants of particular interest include nitrogen dioxide, diesel exhaust particles, as well as particulate matter [33]. Two major mechanisms that may explain the phenomenon is allergic sensitization and airway hyper-responsiveness induced by increased fossil fuel combustion. Airway hyper-responsiveness to environmental allergens may subsequently aggravate symptoms of allergic rhinitis [33]. A longitudinal birth cohort study reports that children living near major roads have increased odds of runny nose and sneezing during the first year of life as well as increased odds of sensitization during the first 8 years of life [26,34]. Stronger associations appeared between traffic-dense areas and respiratory symptoms among children living in poverty [35]. These arguments fit to the current condition in Surabaya where people (including children and students) are trapped in heavy traffic at morning and evening rush hours every day.
The major limitations of this study were the cross-sectional design and the use of questionnaires to obtain information on risk factors. The cross-sectional design does not allow us to identify the temporal sequence between the risk factors and allergic diseases or atopy, although reverse causality is not a possibility for many of the exposures measured. The use of questionnaires makes the study open to information bias. Misperception of allergen and microbial antigens exposure is likely to be a problem with this study as we did not observe directly the housing and the surrounding environmental condition of the study respondent. However, due to this study was population based, the findings can likely be generalized to the population of school children and undergraduate students living in metropolitan cities like Surabaya in Indonesia or to similar areas elsewhere in the region.
In conclusion, the present study has shown the prevalence of allergen sensitizations and allergic diseases in school children and undergraduate students in Surabaya are markedly higher than the previous estimates. This information provides a suitable baseline for the analysis and the anticipation of potential health problems among children and young adults in the future, which hopefully lead to a proper health care and health intervention planning to deal with the increasing prevalence of allergic diseases. There is also an urgent need for an in-depth study to define epidemiological factors that responsible for this increase.
ACKNOWLEDGEMENTS
The authors would thank Prof. Dr. Nasuruddin Abdullah (International Islamic University, Malaysia) for his generous support and advice in conducting this study. We would also thank Prof. Peterhans Jan van den Broek, MD, PhD (LUMC, Leiden, the Netherlands) for reviewing and giving his helpful advice to refine the manuscript.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Gatot Soegiarto, Mai Shihah Abdullah, Chaerul Effendi.
- Data curation: Gatot Soegiarto, Mai Shihah Abdullah, Luki Agustina Damayanti, Arief Suseno, Chaerul Effendi.
- Investigation: Gatot Soegiarto, Mai Shihah Abdullah, Luki Agustina Damayanti, Arief Suseno, Chaerul Effendi.
- Supervision: Chaerul Effendi.
- Validation: Gatot Soegiarto.
- Writing - original draft: Gatot Soegiarto.
- Writing - review & editing: Mai Shihah Abdullah, Luki Agustina Damayanti, Arief Suseno, Chaerul Effendi.
References
- 1.Haahtela T, Holgate S, Pawankar R, Akdis CA, Benjaponpitak S, Caraballo L, Demain J, Portnoy J, von Hertzen L WAO Special Committee on Climate Change and Biodiversity. The biodiversity hypothesis and allergic disease: world allergy organization position statement. World Allergy Organ J. 2013;6:3. doi: 10.1186/1939-4551-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pawankar R, Canonica GW, Holgate ST, Lockey RF, editors. WAO white book on allergy. Milwaukee (WI): World Allergy Organization; 2011. [Google Scholar]
- 3.Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet. 1998;351:1225–1232. [PubMed] [Google Scholar]
- 4.Douwes J, Pearce N. Asthma and the westernization ‘package’. Int J Epidemiol. 2002;31:1098–1102. doi: 10.1093/ije/31.6.1098. [DOI] [PubMed] [Google Scholar]
- 5.Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrländer C, Heederik D, Piarroux R, von Mutius E GABRIELA Transregio 22 Study Group. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011;364:701–709. doi: 10.1056/NEJMoa1007302. [DOI] [PubMed] [Google Scholar]
- 6.Obihara CC, Beyers N, Gie RP, Potter PC, Marais BJ, Lombard CJ, Enarson DA, Kimpen JL. Inverse association between Mycobacterium tuberculosis infection and atopic rhinitis in children. Allergy. 2005;60:1121–1125. doi: 10.1111/j.1398-9995.2005.00834.x. [DOI] [PubMed] [Google Scholar]
- 7.Pearce N, Aït-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, Robertson C ISAAC Phase Three Study Group. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC) Thorax. 2007;62:758–766. doi: 10.1136/thx.2006.070169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mallol J, Crane J, von Mutius E, Odhiambo J, Keil U, Stewart A ISAAC Phase Three Study Group. The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three: a global synthesis. Allergol Immunopathol (Madr) 2013;41:73–85. doi: 10.1016/j.aller.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Ring J, Krämer U, Behrendt H. A critical approach to the hygiene hypothesis. Clin Exp Allergy Rev. 2004;4:40–44. [Google Scholar]
- 10.Kumar Y, Bhatia A. Immunopathogenesis of allergic disorders: current concepts. Expert Rev Clin Immunol. 2013;9:211–226. doi: 10.1586/eci.12.104. [DOI] [PubMed] [Google Scholar]
- 11.Beeh KM, Ksoll M, Buhl R. Elevation of total serum immunoglobulin E is associated with asthma in nonallergic individuals. Eur Respir J. 2000;16:609–614. doi: 10.1034/j.1399-3003.2000.16d07.x. [DOI] [PubMed] [Google Scholar]
- 12.Kerkhof M, Dubois AE, Postma DS, Schouten JP, de Monchy JG. Role and interpretation of total serum IgE measurements in the diagnosis of allergic airway disease in adults. Allergy. 2003;58:905–911. doi: 10.1034/j.1398-9995.2003.00230.x. [DOI] [PubMed] [Google Scholar]
- 13.Platts-Mills TA. The role of immunoglobulin E in allergy and asthma. Am J Respir Crit Care Med. 2001;164(8 Pt 2):S1–5. doi: 10.1164/ajrccm.164.supplement_1.2103024. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton RG, Franklin Adkinson N., Jr In vitro assays for the diagnosis of IgE-mediated disorders. J Allergy Clin Immunol. 2004;114:213–225. doi: 10.1016/j.jaci.2004.06.046. [DOI] [PubMed] [Google Scholar]
- 15.Choo-Kang LR. Specific IgE testing: Objective laboratory evidence supports allergy diagnosis and treatment. MLO Med Lab Obs. 2006;38:10–12. 14, 17. [PubMed] [Google Scholar]
- 16.van de Ven MO, van den Eijnden RJ, Engels RC. Atopic diseases and related risk factors among Dutch adolescents. Eur J Public Health. 2006;16:549–558. doi: 10.1093/eurpub/ckl022. [DOI] [PubMed] [Google Scholar]
- 17.Huurre TM, Aro HM, Jaakkola JJ. Incidence and prevalence of asthma and allergic rhinitis: a cohort study of Finnish adolescents. J Asthma. 2004;41:311–317. doi: 10.1081/jas-120026088. [DOI] [PubMed] [Google Scholar]
- 18.Robertson CF, Dalton MF, Peat JK, Haby MM, Bauman A, Kennedy JD, Landau LI. Asthma and other atopic diseases in Australian children. Australian arm of the International Study of Asthma and Allergy in Childhood. Med J Aust. 1998;168:434–438. [PubMed] [Google Scholar]
- 19.Jackson KD, Howie LD, Akinbami LJ. Trends in allergic conditions among children: United States, 1997-2011. NCHS Data Brief. 2013;(121):1–8. [PubMed] [Google Scholar]
- 20.Quah BS, Wan-Pauzi I, Ariffin N, Mazidah AR. Prevalence of asthma, eczema and allergic rhinitis: two surveys, 6 years apart, in Kota Bharu, Malaysia. Respirology. 2005;10:244–249. doi: 10.1111/j.1440-1843.2005.00645.x. [DOI] [PubMed] [Google Scholar]
- 21.Kao CC, Huang JL, Ou LS, See LC. The prevalence, severity and seasonal variations of asthma, rhinitis and eczema in Taiwanese schoolchildren. Pediatr Allergy Immunol. 2005;16:408–415. doi: 10.1111/j.1399-3038.2005.00268.x. [DOI] [PubMed] [Google Scholar]
- 22.Vichyanond P, Jirapongsananuruk O, Visitsuntorn N, Tuchinda M. Prevalence of asthma, rhinitis and eczema in children from the Bangkok area using the ISAAC (International Study for Asthma and Allergy in Children) questionnaires. J Med Assoc Thai. 1998;81:175–184. [PubMed] [Google Scholar]
- 23.Cua-Lim F, Roa C, Jr, Ferreria M, Sumpaico M, Tuazon A, Amores JP, Cue PE, Cruzat L, Castillo-Carandang N. Prevalence of asthma in Metro Manila, Philippines. Philipp J Allergy Immunol. 1997;4:9–20. [Google Scholar]
- 24.Ho SM. Environmental epigenetics of asthma: an update. J Allergy Clin Immunol. 2010;126:453–465. doi: 10.1016/j.jaci.2010.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thornton CA, Macfarlane TV, Holt PG. The hygiene hypothesis revisited: role of materno-fetal interactions. Curr Allergy Asthma Rep. 2010;10:444–452. doi: 10.1007/s11882-010-0148-5. [DOI] [PubMed] [Google Scholar]
- 26.Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Krämer U, Behrendt H, Herbarth O, von Berg A, Bauer CP, Wichmann HE, Heinrich J GINI Study Group; LISA Study Group. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008;177:1331–1337. doi: 10.1164/rccm.200701-036OC. [DOI] [PubMed] [Google Scholar]
- 27.D'Amato G. Environmental urban factors (air pollution and allergens) and the rising trends in allergic respiratory diseases. Allergy. 2002;57(Suppl 72):30–33. doi: 10.1034/j.1398-9995.57.s72.5.x. [DOI] [PubMed] [Google Scholar]
- 28.Modig L, Torén K, Janson C, Jarvholm B, Forsberg B. Vehicle exhaust outside the home and onset of asthma among adults. Eur Respir J. 2009;33:1261–1267. doi: 10.1183/09031936.00101108. [DOI] [PubMed] [Google Scholar]
- 29.Abdulah R. Antibiotic abuse in developing countries. Pharmaceut Reg Affairs. 2012;1:e106 [Google Scholar]
- 30.Gani L, Arif H, Widjaja SK, Adi R, Prasadja H, Tampubolon LH, Lukito E, Jauri R. Physicians' prescribing practice for treatment of acute diarrhoea in young children in Jakarta. J Diarrhoeal Dis Res. 1991;9:194–199. [PubMed] [Google Scholar]
- 31.Hadi U, Duerink DO, Lestari ES, Nagelkerke NJ, Werter S, Keuter M, Suwandojo E, Rahardjo E, van den Broek P, Gyssens IC Antimicrobial Resistance in Indonesia ‘Prevalence and Prevention’ study group. Survey of antibiotic use of individuals visiting public healthcare facilities in Indonesia. Int J Infect Dis. 2008;12:622–629. doi: 10.1016/j.ijid.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Res Notes. 2011;4:491. doi: 10.1186/1756-0500-4-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takizawa H. Impact of air pollution on allergic diseases. Korean J Intern Med. 2011;26:262–273. doi: 10.3904/kjim.2011.26.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim HH, Kim CS, Lim YW, Suh MA, Shin DC. Indoor and outdoor air quality and its relation to allergic diseases among children: a case study at a primary school in Korea. Asian J Atmos Environ. 2010;4:157–165. [Google Scholar]
- 35.Meng YY, Wilhelm M, Rull RP, English P, Nathan S, Ritz B. Are frequent asthma symptoms among low-income individuals related to heavy traffic near homes, vulnerabilities, or both? Ann Epidemiol. 2008;18:343–350. doi: 10.1016/j.annepidem.2008.01.006. [DOI] [PubMed] [Google Scholar]