Abstract
Exposure to total hydrocarbons (THC) and volatile organic compounds from air pollution is associated with risk of coronary heart disease. THC exposure from oil spills might be similarly associated, but no research has examined this. We assessed the relationship between THC exposure during the response and cleanup of the Deepwater Horizon oil spill (Gulf of Mexico) and heart attack risk among 24,375 oil spill workers enrolled in the Gulf Long-Term Follow-up Study. There were 312 first heart attacks (self-reported physician-diagnosed myocardial infarction, or fatal coronary heart disease) ascertained during the study period (2010–2016). THC exposures were estimated using a job-exposure matrix incorporating self-reported activities and personal air measurements. We used Cox proportional hazards regression to estimate hazard ratios, with inverse-probability weights to account for confounding and censoring. Maximum THC levels of ≥0.30 parts per million (ppm) were associated with heart attack risk, with a 1.8-fold risk for exposure of ≥3.00 ppm versus <0.30 ppm (hazard ratio = 1.81, 95% confidence interval: 1.11, 2.95). The risk difference for highest versus lowest THC level was 10 excess cases per 1,000 workers. This is the first study of the persistent health impacts of THC exposure during oil spill work, and results support increased protection against oil exposure during cleanup of future spills.
Keywords: coronary disease, myocardial infarction, occupational exposure, occupational health, petroleum pollution
Workers involved in the response and cleanup for the 2010 Deepwater Horizon oil spill faced exposures to a number of chemicals generated by crude oil, burning oil, and cleanup activities. Some of these pollutants, including particulate matter, polycyclic aromatic hydrocarbons, and some volatile organic compounds, have been associated with risk of coronary heart disease (CHD) (1–4). Working in proximity to chemical stressors and air pollutants might affect the risk of CHD among oil spill response and cleanup workers, but to our knowledge no previous study of oil spills has addressed this question.
Exposure to particulate matter and organic chemicals has been shown to be associated with cardiovascular disease risk (4–8). Short-term, 24-hour average increases in ambient particulate matter are associated with incidence of myocardial infarction (2, 9). Air concentrations of particulates, polycyclic aromatic hydrocarbons, and total hydrocarbons (THC) varied spatially and temporally over the course of the Deepwater Horizon oil spill (10). Particulate matter concentrations might have exceeded typical ambient levels (11), which range from 0.02 to 1.00 μg/m3 in the Southern United States (12). It is unknown whether these exposures, at levels present during the spill, could have affected cardiovascular health and whether any such effects would be acute or persistent.
Several studies have examined acute health outcomes associated with oil spills, but there has been relatively little research into longer-term health impacts following these events. Respiratory symptoms persisted among fishermen involved in the cleanup of the Prestige oil spill 5 years after the spill (13). In a study of the Tasman Spirit oil spill, cleanup workers had reduced lung function 5 months after the spill, compared with community members not involved with cleanup (14). Although these studies did not examine any specific spill-related chemical exposures, results are consistent with the hypothesis that short-term exposures might elicit persistent biological changes.
The Gulf Long-Term Follow-up (GuLF) Study is the largest study of the health impacts of oil spills and is, to our knowledge, the first to assess heart disease among individuals exposed to oil spills (15). We hypothesized that THC exposures occurring during the Deepwater Horizon oil spill response and cleanup increased the risk of coronary heart disease and assessed whether these associations, if present, persisted over time. We used information from 2 sequential GuLF Study interviews and mortality data from the National Death Index to examine relationships between THC exposure and risk of first heart attack up to 5 years after the oil spill.
METHODS
Study population
Participants included individuals who completed mandatory worker safety training in order to take part in the oil spill response and cleanup, as well as government workers and oil industry professionals (15). Study enrollment began 11 months after the start of the oil spill and occurred from March 2011 to May 2013. A total of 32,608 individuals enrolled in the cohort; this report includes the 24,375 English- and Spanish-speaking participants who worked on the oil spill for at least 1 day. Among these, 16,814 (69%) completed a second telephone interview in 2014–2016, 2–3 years after enrollment.
Exposure measures
We evaluated maximum and median levels of estimated THC exposure as a general marker of total petroleum hydrocarbon exposure during oil spill work. A job-exposure matrix was developed using personal air measurements taken by passive dosimeters during the spill to assign estimated ordinal THC exposure levels to exposure groups reflecting the study participants’ self-reported activities, locations, and dates of work (16). Participants reported complex work patterns (e.g., performing multiple activities, sometimes at the same time) and were assigned to multiple exposure groups.
We defined maximum THC exposure as workers’ highest intensity exposure at any time during their oil spill work, across all of his/her exposure groups. Maximum THC exposures were categorized based on the distribution of the maximum exposure group estimates as <0.30 parts per million (ppm), 0.30–0.99 ppm, 1.00–2.99 ppm, and ≥3.00 ppm. Median THC exposure was defined as the median exposure level across all exposure groups before the oil well was capped on July 15, 2010, the period when oil exposures were generally highest (16). Categories for median THC exposure were: <0.10 ppm, 0.10–0.29 ppm, 0.30–0.99 ppm, and ≥1.00 ppm, based on the distribution of the median exposure group estimates. Maximum THC was estimated for all 24,375 workers; median exposures were estimated for the 22,550 workers who initiated oil spill work on or before July 15, 2010.
Outcome measure
The outcome of interest was the first occurrence of an incident heart attack, defined as either a self-reported physician-diagnosed myocardial infarction (MI) or a fatal CHD event. During the study interviews, participants were asked whether they had ever received a diagnosis of a heart attack or MI and, if so, the month and year of their first MI diagnosis. Deaths due to CHD were ascertained from the National Death Index, from the date of enrollment through December 31, 2014, the latest date for which National Death Index data were available. Deaths with International Classification of Diseases, Tenth Revision, codes in any position indicating ischemic heart disease as a cause of death (codes I20–I25) were included.
Risk period for heart attack
To reduce potential bias due to left truncation, the risk period for a nonfatal MI began at the initiation of oil spill work and ended at the first of either the date of diagnosis of a first MI or the date of the last GuLF Study interview that the participant completed. The risk period for a fatal CHD event began at the date of the enrollment interview, given that participants had to be alive to enroll in the study, and continued until December 31, 2014. Fatal CHD events occurring after the initiation of oil spill work but before study enrollment were therefore truncated. Participants were followed until they had a CHD event, died, or reached the end of follow-up. Only a participant’s first reported MI or CHD event was counted. Participants who reported a first MI prior to initiation of oil spill work (n = 452) were excluded.
Among the 23,923 workers without MI prior to the oil spill, there were 253 deaths during the study period, including 36 CHD-related deaths. Incident nonfatal MI was reported by 282 participants. Of the 36 CHD-related deaths, 6 were among individuals who had already reported an incident first MI diagnosis. Thus, a total of 312 first heart attack cases were included in this report.
Censoring and predictors of censoring
Self-reported MI might have been censored among participants who did not complete the second interview but were at risk for a first MI. We compared distributions of factors plausibly related with the outcome and nonresponse to the second interview, including demographic factors, lifestyle and socioeconomic characteristics, factors related to health at enrollment, and cleanup work characteristics. We compared crude proportions of censoring across levels of each predictor variable to assess the ability of each variable to predict nonresponse.
To reduce the impact of potential selection bias, we weighted the population that completed the second interview with respect to predictors of censoring; this approach allowed us to estimate associations that would be observed in the absence of censoring (17). Inverse probability (IP)-of-censoring weights were estimated from models conditional on predictors of censoring. The variables (derived from information collected at the first interview) included in the censoring weights model were determined from a causal diagram (18): age at enrollment (in years: 20–29, 30–39, 40–49, 50–59, 60–64, ≥65); maximum educational attainment (less than high school, high-school diploma/General Educational Development certificate, some college/2-year degree, ≥4-year college graduate); cigarette smoking (current, former, never); maximum THC exposure during cleanup work (<0.30 ppm, 0.30–0.99 ppm, 1.00–2.99 ppm, ≥3.00 ppm); and residential proximity to the oil spill (“direct/indirect” defined as living in or adjacent to a county with coastline oiled during the spill vs. “away from the spill”). We grouped participants living in and adjacent to counties that were oiled during the spill because these areas were most likely to have faced the socioeconomic impacts of the oil spill; living in these areas was also associated with adverse mental health symptoms (19). We calculated stabilized IP-censoring weights by dividing the marginal probability of being observed at the second interview by the conditional probabilities of being observed that were output from the censoring weights model.
Time-to-heart-attack analyses
We assessed the associations between THC exposure and time-to–incident first heart attack using Cox proportional hazards models (20). Person-time was accrued from the start of an individual’s oil spill work until the earlier of first MI event, leaving the study, or administrative censoring at the end of National Death Index follow-up.
We controlled for confounders using IP-exposure weights (21). The adjustment set was determined using a directed acyclic graph (18) and included all variables from the censoring weights models, with the addition of sex (male, female). We did not adjust for body mass index or self-reported hypertension because these were not associated with THC exposure. Stabilized IP-exposure weights were obtained by fitting a multinomial logistic regression model for the exposure with confounders as independent variables; the denominator of the weights was based on the probability output from the model, and the numerator was based on the marginal probability of exposure (17). In sensitivity analyses, we controlled for confounders conditionally in the Cox models and adjusted for body mass index at enrollment (calculated as height (m)/weight (kg)2, with categories of <25.0, 25.0–29.9, ≥30.0).
Cox proportional hazards models (20) with a robust variance estimator were fitted to estimate hazard ratios and 95% confidence intervals (21). We assessed whether each covariate met the proportional hazards assumption by modeling a term for interaction between the natural log of time and each covariate (20). Tests of the proportional hazards assumption did not indicate any departures from proportional hazards (P > 0.10 for all; results not shown).
The National Death Index mortality data were censored on December 31, 2014, before some participants had completed their second interviews. Thus, fatal events after December 31, 2014, were missed. To account for this, we performed an analysis excluding the 2,092 participants who gave their second interview after December 31, 2014. We also assessed associations for nonfatal MI only; this analysis included the 282 incident nonfatal heart attacks reported during the interviews. In separate analyses, we controlled for oil spill work duration to assess confounding due to healthy-worker survivor bias, given that healthier workers might have worked longer on the spill. To assess the possible impact of heat stress during cleanup work, we adjusted for whether a participant reported ever stopping cleanup work activities due to the heat. In another analysis, we excluded US Coast Guard and other federal employees (n = 4,619), because these workers might have been more physically fit and/or had more access to health-care services compared with workers who were not federal employees.
Cumulative incidence of heart attack
To assess whether associations with heart attack changed across the study period, we estimated cumulative risks of heart attack at yearly intervals throughout follow-up. We generated weighted, cumulative conditional risk plots based on our proportional hazards regression using the approach of Cole and Hernán (22). This approach requires an estimate of the baseline hazard, which we obtained using the Nelson-Aalen estimator (23), with months since initiation of cleanup work as the time scale. We accounted for confounders and predictors of censoring using the same IP weights as were included in the Cox regression models (22). Analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
Participants who completed both study interviews, compared with those who only completed the first, were more likely to be older, white, or nonsmokers; to have attended or graduated from college; and to have a 2010 household income over $50,000 (Table 1). Distributions of demographic, health, and oil-spill exposure characteristics according to heart attack status among the 23,923 workers with no prevalent MI diagnosis are shown in Table 2.
Table 1.
Demographic and Oil-Spill Work Characteristics at Enrollment (Except Where Noted) Among Those Who Completed (n = 16,814) and Did Not Complete (n = 7,561) the Second Study Interview, Gulf Long-Term Follow-up Study, United States, 2010–2016
| Characteristic | Completed Interview 2 (n = 16,814) | Did Not Complete Interview 2 (n = 7,561) | RD | 95% CI | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Sex | ||||||
| Male | 13,747 | 81.8 | 6,335 | 83.8 | 0 | Referent |
| Female | 3,067 | 18.2 | 1,226 | 16.2 | 0.0299 | 0.0149, 0.0448 |
| Missing | 0 | 0.0 | 0 | 0.0 | ||
| Age category, years | ||||||
| 20–29 | 2,936 | 17.5 | 2,063 | 27.4 | −0.0489 | −0.0673, −0.0306 |
| 30–39 | 3,745 | 22.3 | 2,141 | 28.4 | 0 | Referent |
| 40–49 | 4,245 | 16.8 | 1,726 | 7.6 | 0.0747 | 0.0579, 0.0915 |
| 50–59 | 4,018 | 16.8 | 1,188 | 5.5 | 0.1355 | 0.1188, 0.1523 |
| 60–65 | 1,071 | 4.6 | 256 | 1.3 | 0.1708 | 0.1463, 0.1954 |
| ≥65 | 753 | 3.4 | 153 | 0.9 | 0.1949 | 0.1676, 0.2222 |
| Missing | 46 | 0.3 | 34 | 0.4 | ||
| Ethnicity | ||||||
| White | 11,270 | 67.4 | 4,827 | 64.2 | 0 | Referent |
| Black | 3,767 | 22.5 | 1,859 | 24.7 | −0.0306 | −0.0447, −0.0164 |
| Asian | 132 | 0.8 | 87 | 1.2 | −0.0974 | −0.1626, −0.0322 |
| Other/multiracial | 1,554 | 9.3 | 743 | 9.9 | −0.0236 | −0.044, −0.0032 |
| Missing | 91 | 0.5 | 45 | 0.6 | ||
| Hispanic | ||||||
| Yes | 1,112 | 6.6 | 599 | 7.9 | −0.0431 | −0.0664, −0.0197 |
| No | 15,659 | 93.4 | 6,938 | 92.1 | 0 | Referent |
| Missing | 43 | 0.3 | 24 | 0.3 | ||
| Education completed | ||||||
| Less than high school | 2,446 | 14.6 | 1,376 | 18.3 | −0.0129 | −0.0317, 0.0059 |
| High-school diploma/GED | 4,673 | 27.9 | 2,485 | 33.0 | 0 | Referent |
| Some college/2-year degree | 5,032 | 30.0 | 2,269 | 30.1 | 0.0364 | 0.0211, 0.0517 |
| ≥4-year college graduate | 4,618 | 27.5 | 1,408 | 18.7 | 0.1135 | 0.0982, 0.1289 |
| Missing | 45 | 0.3 | 23 | 0.3 | ||
| 2010 household income, $ | ||||||
| ≤20,000 | 3,960 | 25.9 | 2,114 | 31.3 | −0.0208 | −0.0370, −0.0045 |
| 20,001–50,000 | 4,748 | 31.1 | 2,310 | 34.2 | 0 | Referent |
| >50,000 | 6,581 | 43.0 | 2,330 | 34.5 | 0.0658 | 0.0516, 0.0801 |
| Missing | 1,525 | 9.1 | 807 | 10.7 | ||
| Residential proximity to the spilla | ||||||
| Direct/indirect | 9,688 | 57.6 | 4,723 | 62.5 | −0.0429 | −0.0546, −0.0312 |
| Away from the spill | 7,126 | 42.4 | 2,838 | 37.5 | 0 | Referent |
| Missing | 0 | 0.0 | 0 | 0.0 | ||
| Cleanup work duration, days | ||||||
| 1–30 | 2,063 | 12.3 | 935 | 12.4 | 0 | Referent |
| 31–90 | 5,293 | 31.5 | 2,376 | 31.4 | 0.0021 | −0.0175, 0.0216 |
| 91–180 | 5,735 | 43.8 | 2,628 | 44.2 | −0.0024 | −0.0217, 0.0170 |
| >180 | 3,723 | 22.1 | 1,622 | 21.5 | 0.0084 | −0.0122, 0.0291 |
| Missing | 0 | 0.0 | 0 | 0.0 | ||
| Worked before the well was capped | ||||||
| Yes | 15,453 | 94.0 | 7,097 | 94.8 | −0.0321 | −0.0567, −0.0076 |
| No | 985 | 6.0 | 388 | 5.2 | 0 | Referent |
| Missing | 0 | 0.0 | 0 | 0.0 | ||
| Maximum total hydrocarbon exposure, ppm | ||||||
| <0.30 | 3,864 | 23.0 | 1,579 | 20.9 | 0 | Referent |
| 0.30–0.99 | 5,519 | 32.9 | 2,465 | 32.6 | −0.0186 | −0.0344, −0.0029 |
| 1.00–2.99 | 5,094 | 30.3 | 2,382 | 31.5 | −0.0285 | −0.0446, −0.0125 |
| ≥3.00 | 2,313 | 13.8 | 1,132 | 15.0 | −0.0385 | −0.0583, −0.0187 |
| Missing | 24 | 0.1 | 3 | 0.0 | ||
| Reported ever having had a nonfatal MI | ||||||
| Yes | 416 | 2.5 | 126 | 1.7 | 0.0795 | 0.0434, 0.1155 |
| No | 16,350 | 97.5 | 7,413 | 98.3 | 0 | Referent |
| Missing | 48 | 0.3 | 22 | 0.3 | ||
| First nonfatal MI/fatal CHD occurring after initiation of oil spill work | ||||||
| Yes | 250 | 1.5 | 62 | 0.8 | 0.1156 | 0.0710, 0.1603 |
| No | 16,125 | 98.5 | 7,392 | 99.2 | 0 | Referent |
| Missing | 439 | 2.6 | 107 | 1.4 | ||
| Self-reported physician-diagnosed hypertension before study enrollment | ||||||
| Yes | 4,716 | 28.1 | 1,701 | 22.6 | 0.0613 | 0.0485, 0.0741 |
| No | 12,053 | 71.9 | 5,839 | 77.4 | 0 | Referent |
| Missing | 45 | 0.3 | 21 | 0.3 | ||
| Perceived health | ||||||
| Excellent | 2,689 | 16.1 | 1,279 | 17.0 | −0.0130 | −0.0308, 0.0048 |
| Very good | 5,383 | 32.2 | 2,350 | 31.3 | 0.0054 | −0.0091, 0.0200 |
| Good | 5,352 | 32.0 | 2,397 | 31.9 | 0 | Referent |
| Fair | 2,471 | 14.8 | 1,132 | 15.1 | −0.0049 | −0.0232, 0.0135 |
| Poor | 841 | 5.0 | 360 | 4.8 | 0.0096 | −0.0183, 0.0375 |
| Missing | 78 | 0.5 | 43 | 0.6 | ||
| Tobacco smoking | ||||||
| Current | 4,710 | 28.2 | 2,635 | 35.2 | −0.0681 | −0.0818, −0.0544 |
| Former | 3,713 | 22.2 | 1,452 | 19.4 | 0.0095 | −0.0052, 0.0243 |
| Never | 8,300 | 49.6 | 3,401 | 45.4 | 0 | Referent |
| Missing | 91 | 0.5 | 73 | 1.0 | ||
| Current alcohol use | ||||||
| Yes | 12,852 | 76.9 | 5,677 | 75.7 | 0.0135 | −0.0003, 0.0274 |
| No | 3,871 | 23.1 | 1,821 | 24.3 | 0 | Referent |
| Missing | 91 | 0.5 | 63 | 0.8 | ||
| BMIb at enrollment | ||||||
| <25.0 | 4,365 | 26.2 | 2,140 | 28.7 | 0 | Referent |
| 25.0–29.9 | 6,911 | 41.5 | 3,078 | 41.3 | 0.0208 | 0.0063, 0.0354 |
| ≥30.0 | 5,365 | 32.2 | 2,236 | 30.0 | 0.0348 | 0.0195, 0.0501 |
| Missing | 173 | 1.0 | 107 | 1.4 | ||
Abbreviations: BMI, body mass index; CHD, coronary heart disease; CI, confidence interval; GED, General Educational Development; MI, myocardial infarction; ppm, parts per million; RD, risk difference.
a Residential proximity to the spill is defined as living in, or adjacent to, a county with coastline that was oiled during the spill.
b BMI defined as weight (kg)/height (m)2.
Table 2.
Demographic and Oil Spill Work Characteristics at Enrollment Among Cleanup Workers Without Prevalent Heart Attack (n = 23,923), According to Incident Self-Reported Myocardial Infarction/Fatal Coronary Heart Disease, Gulf Long-Term Follow-up Study, United States, 2010–2016
| Characteristic | No. of Cases (n = 312) | % | Total No. (n = 23,923) | % |
|---|---|---|---|---|
| Sex | ||||
| Male | 284 | 91.0 | 19,667 | 82.2 |
| Female | 28 | 9.0 | 4,256 | 17.8 |
| Missing | 0 | 0.0 | ||
| Age, years | ||||
| 20–29 | 6 | 1.9 | 4,985 | 21.0 |
| 30–39 | 30 | 9.6 | 5,850 | 24.6 |
| 40–49 | 94 | 30.1 | 5,865 | 24.7 |
| 50–59 | 118 | 37.8 | 5,012 | 21.1 |
| 60–64 | 37 | 11.9 | 1,245 | 5.2 |
| ≥65 | 27 | 8.7 | 793 | 3.3 |
| Missing | 173 | 0.7 | ||
| Ethnicity | ||||
| White | 199 | 63.8 | 15,708 | 66.3 |
| Black | 77 | 24.7 | 5,543 | 23.4 |
| Asian | 5 | 1.6 | 213 | 0.9 |
| Other/multiracial | 31 | 9.9 | 2,232 | 9.4 |
| Missing | 227 | 0.9 | ||
| Education | ||||
| Less than high school | 78 | 25.0 | 3,702 | 15.6 |
| High-school diploma/GED | 108 | 34.6 | 6,987 | 29.4 |
| Some college/2-year degree | 83 | 26.6 | 7,149 | 30.1 |
| ≥4-year college graduate | 43 | 13.8 | 5,925 | 24.9 |
| Missing | 160 | 0.7 | ||
| Household income, $ | ||||
| ≤20,000 | 102 | 34.9 | 5,917 | 27.4 |
| 20,001–50,000 | 102 | 34.9 | 6,905 | 32.0 |
| >50,000 | 88 | 30.1 | 8,748 | 40.6 |
| Missing | 2,353 | 9.8 | ||
| Residential proximity to the oil spilla | ||||
| Direct/indirect | 231 | 74.0 | 14,019 | 58.8 |
| Away from the spill | 81 | 26.0 | 9,810 | 41.2 |
| Missing | 94 | 0.4 | ||
| Duration of cleanup work, days | ||||
| ≤30 | 29 | 9.3 | 2,920 | 12.3 |
| 31–90 | 88 | 28.2 | 7,488 | 31.4 |
| 91–180 | 122 | 39.1 | 8,178 | 34.3 |
| >180 | 73 | 23.4 | 5,243 | 22.0 |
| Missing | 94 | 0.4 | ||
| Maximum THC exposure, ppm | ||||
| <0.30 | 42 | 13.5 | 5,342 | 22.4 |
| 0.30–0.99 | 106 | 34.2 | 7,801 | 32.8 |
| 1.00–2.99 | 114 | 36.8 | 7,283 | 30.6 |
| ≥3.00 | 48 | 15.5 | 3,377 | 14.2 |
| Missing | 120 | 0.5 | ||
| Median THC exposure, ppm | ||||
| <0.10 | 41 | 14.0 | 4,460 | 19.9 |
| 0.10–0.29 | 106 | 36.3 | 7,792 | 34.7 |
| 0.30–0.99 | 128 | 43.8 | 9,035 | 40.2 |
| ≥1.00 | 17 | 5.8 | 1,173 | 5.2 |
| Missing | 1,463 | 6.1 | ||
| Self-reported prevalent hypertension | ||||
| Yes | 199 | 64.4 | 6,092 | 25.6 |
| No | 110 | 35.6 | 17,689 | 74.4 |
| Missing | 142 | 0.6 | ||
| Cigarette smoking | ||||
| Current | 120 | 38.8 | 7,140 | 30.2 |
| Former | 88 | 28.5 | 4,989 | 21.1 |
| Never | 101 | 32.7 | 11,547 | 48.8 |
| Missing | 247 | 1.0 | ||
| BMIb at enrollment | ||||
| <25 | 63 | 20.2 | 6,401 | 27.2 |
| 25–29.9 | 110 | 35.3 | 9,785 | 41.5 |
| ≥30 | 139 | 44.6 | 7,376 | 31.3 |
| Missing | 361 | 1.5 |
Abbreviations: BMI, body mass index; GED, General Educational Development; ppm, parts per million; THC, total hydrocarbon.
a Residential proximity to the spill is defined as living in, or adjacent to, a county with coastline that was oiled during the spill.
b BMI defined as weight (kg)/height (m)2.
IP censoring and exposure weights
After excluding workers with prevalent MI, censoring weights were determined separately for the full cohort (n = 23,923) and for those who began cleanup work before July 15, 2010 (n = 22,550). For the full cohort, the mean, range, and standard deviation of the stabilized censoring weights, exposure weights, and final weights (exposure weight multiplied by censoring weight) were as follows: 1.00 (range, 0.52–2.61; standard deviation (SD), 0.21), 1.00 (range, 0.32–7.05; SD, 0.48), and 1.00 (range, 0.25–13.40; SD, 0.55), respectively. For the 22,550 workers who started cleanup work by July 15, 2010, the means, ranges, and standard deviations of the stabilized censoring weights, exposure weights, and final weights were as follows: 1.00 (range, 0.55–2.68; SD, 0.21), 1.00 (range, 0.31–4.47; SD, 0.39), and 1.00 (range, 0.25–6.33; SD, 0.47), respectively.
Hazard ratios for THC exposure and heart attack
Hazard of heart attack was elevated for maximum THC exposures of ≥0.30 ppm (Table 3). Maximum THC exposure of ≥3.00 ppm (vs. <0.30 ppm) showed the strongest association with heart attack (hazard ratio (HR) = 1.81, 95% confidence interval (CI): 1.11, 2.95), although hazard ratios were also significantly higher for exposure levels 0.30–0.99 ppm (HR = 1.66, 95% CI: 1.09, 2.53) and 1.00–2.99 ppm (HR = 1.62, 95% CI: 1.06, 2.47). There was no clear monotonic exposure-response relationship across exposure groups. Results were robust to factors associated with nonresponse to the second interview—hazard ratios without IP-censoring weights were not meaningfully changed (for maximum THC exposure of ≥3.00 ppm, HR = 1.70 (95% CI: 1.05, 2.74) vs. HR = 1.81). Hazard ratios for the associations of median THC exposure before the oil well was capped and heart attack were attenuated compared with the associations with maximum THC exposure (Table 4). Associations were similar using the Cox models conditional on confounders (Web Table 1, available at https://academic.oup.com/aje) and after adjusting for body mass index (Web Table 2).
Table 3.
Marginal Hazard Ratios of the Association of Maximum Total Hydrocarbon Exposure and Self-Reported Myocardial Infarction/Fatal Coronary Heart Disease, Gulf Long-Term Follow-up Study, United States, 2010–2016
| Max THC Exposure, ppm | Total Cases (n = 307) | Total No.a (n = 23,520) | HRb | 95% CI |
|---|---|---|---|---|
| No censoring weights | ||||
| <0.30 | 41 | 5,246 | 1.00 | Referent |
| 0.30–0.99 | 105 | 7,719 | 1.60 | 1.07, 2.41 |
| 1.00–2.99 | 114 | 7,209 | 1.45 | 0.96, 2.18 |
| ≥3.00 | 47 | 3,346 | 1.70 | 1.05, 2.74 |
| IP-censoring weightedc | ||||
| <0.30 | 41 | 5,215 | 1.00 | Referent |
| 0.30–0.99 | 105 | 7,682 | 1.66 | 1.09, 2.53 |
| 1.00–2.99 | 114 | 7,178 | 1.62 | 1.06, 2.47 |
| ≥3.00 | 47 | 3,334 | 1.81 | 1.11, 2.95 |
Abbreviations: CI, confidence interval; HR, hazard ratio; IP, inverse probability; ppm, parts per million; THC, total hydrocarbons.
a Total n for models without censoring weights is where maximum THC exposure, sex, age, smoking, education, and residential proximity to the spill are nonmissing; total n for models with censoring weights is where ethnicity is also nonmissing.
b Models controlled for sex, age, smoking, education, and residential proximity to the oil spill using IP-exposure weights.
c Censoring weights accounted for age, ethnicity, education, residential proximity to the oil spill, smoking, and maximum total hydrocarbon exposure.
Table 4.
Marginal Hazard Ratios of the Association of Median Total Hydrocarbon Exposure Before the Oil Well Was Capped and Self-Reported Myocardial Infarction/Fatal Coronary Heart Disease, Gulf Long-Term Follow-up Study, United States, 2010–2016
| Median THC Exposure, ppm | Total Cases (n = 289) | Total No.a (n = 22,200) | HRb | 95% CI |
|---|---|---|---|---|
| No censoring weights | ||||
| <0.10 | 40 | 4,386 | 1.00 | Referent |
| 0.10–0.29 | 106 | 7,715 | 1.44 | 1.01, 2.06 |
| 0.30–0.99 | 126 | 8,940 | 1.27 | 0.89, 1.80 |
| ≥1.00 | 17 | 1,159 | 1.35 | 0.75, 2.43 |
| IP-censoring weightedc | ||||
| <0.10 | 40 | 4,363 | 1.00 | Referent |
| 0.10–0.29 | 106 | 7,682 | 1.58 | 1.04, 2.40 |
| 0.30–0.99 | 126 | 8,904 | 1.32 | 0.88, 2.00 |
| ≥1.00 | 17 | 1,154 | 1.47 | 0.78, 2.78 |
Abbreviations: CI, confidence interval; HR, hazard ratio; IP, inverse probability; ppm, parts per million; THC, total hydrocarbons.
a Total n for models without censoring weights is where median THC exposure, sex, age, smoking, education, and residential proximity to the spill are nonmissing; total n for models with censoring weights is where ethnicity is also nonmissing.
b Models controlled for sex, age, smoking, education, and residential proximity to the oil spill using inverse probability of exposure weights.
c Censoring weights accounted for age, ethnicity, education, residential proximity to the oil spill, smoking, and maximum total hydrocarbon exposure.
Sensitivity analyses that censored all participants on December 31, 2014—the last date of available National Death Index data—showed slightly strengthened results across all levels of maximum THC exposure; the hazard ratio for maximum THC exposure of ≥3.00 ppm (vs. <0.30 ppm) was 2.01 (95% CI: 1.21, 3.34) (Web Table 3). Analyses that did not count fatal events, but censored at date of CHD death, were slightly weakened in magnitude but were overall not meaningfully different from the results in Table 3 (Web Table 4). Hazard ratios adjusting for self-reported heat stress during cleanup work were also similar (results not shown).
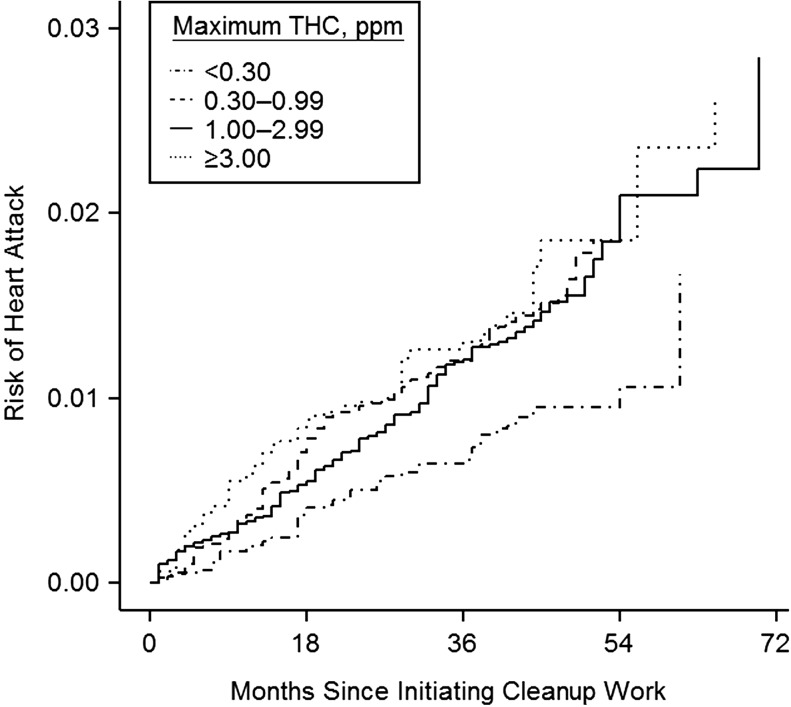
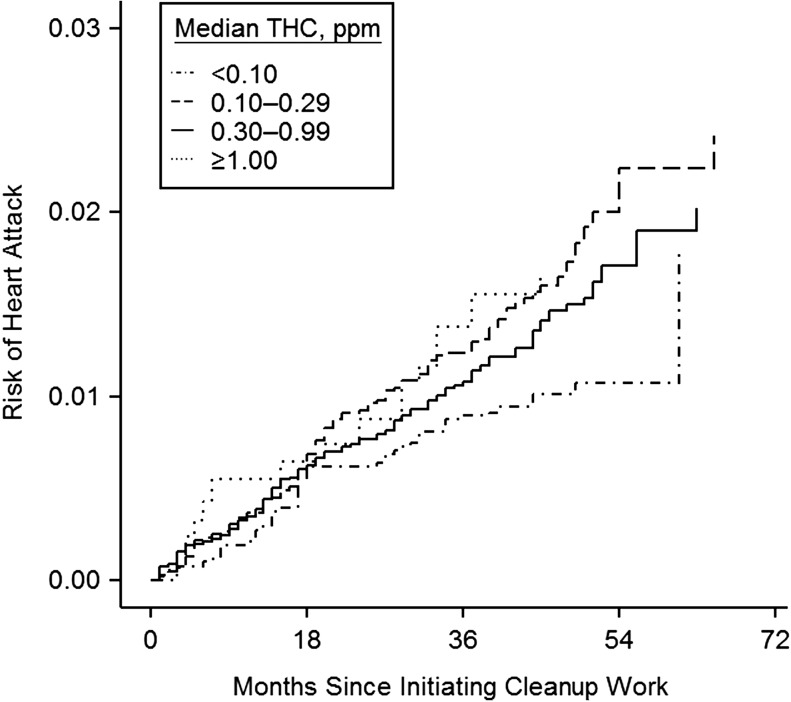
Workers with maximum THC exposure <0.30 ppm had the lowest cumulative risk of heart attack across follow-up (Table 5; Figure 1). The risk differences for maximum THC exposure of ≥3.00 ppm (vs. <0.30 ppm) and heart attack showed elevated risks from 4 excess cases per 1,000 workers at 12 months of follow-up to 10 excess cases per 1,000 workers at 48 months of follow-up (Table 5). The sensitivity analyses that censored all participants on December 31, 2014, also yielded similar risk differences (Web Table 5). The risk differences for median THC exposure of ≥1.00 ppm (vs. <0.10 ppm) ranged from 3 excess cases per 1,000 workers to 6 excess cases per 1,000 workers (Table 6; Figure 2).
Table 5.
Risk of Self-Reported Myocardial Infarction/Fatal Coronary Heart Disease According to Maximum Total Hydrocarbon Exposure and Time Since Initiating Oil Spill Work (n = 23,923), Gulf Long-Term Follow-up Study, United States, 2010–2016
| Max THC Exposure, ppm | Time Since Initiating Oil Spill Work | |||||||
|---|---|---|---|---|---|---|---|---|
| 12 Months | 24 Months | 36 Months | 48 Months | |||||
| Riska | RD | Riska | RD | Riska | RD | Riska | RD | |
| <0.30 | 0.002 | Referent | 0.005 | Referent | 0.007 | Referent | 0.009 | Referent |
| 0.30–0.99 | 0.004 | 0.002 | 0.010 | 0.005 | 0.012 | 0.005 | 0.016 | 0.007 |
| 1.00–2.99 | 0.004 | 0.002 | 0.008 | 0.003 | 0.012 | 0.005 | 0.016 | 0.007 |
| ≥3.00 | 0.006 | 0.004 | 0.010 | 0.005 | 0.013 | 0.006 | 0.019 | 0.010 |
Abbreviations: ppm, parts per million; RD, risk difference; THC, total hydrocarbons.
a Risk estimates accounted for confounders (age, sex, education, smoking, and residential proximity to the spill) and predictors of censoring (age, education, ethnicity, smoking, cleanup work duration, and residential proximity to the spill) using inverse-probability weights.
Figure 1.
Cumulative risk of self-reported myocardial infarction/fatal coronary heart disease according to maximum total hydrocarbon (THC) exposure (parts per million (ppm)) during cleanup work (n = 23,923), Gulf Long-Term Follow-up Study, United States, 2010–2016. Risk estimates accounted for confounders (age, sex, education, smoking, and residential proximity to the spill) and predictors of censoring (age, education, ethnicity, smoking, cleanup work duration, and residential proximity to the spill) using inverse probability weights.
Table 6.
Risk of Self-Reported Myocardial Infarction/Fatal Coronary Heart Disease According to Median Total Hydrocarbon Exposure and Time Since Initiating Oil Spill Work (n = 22,550), Gulf Long-Term Follow-up Study, United States, 2010–2016
| Median THC Exposure, ppm | Time Since Initiating Oil Spill Work | |||||||
|---|---|---|---|---|---|---|---|---|
| 12 Months | 24 Months | 36 Months | 48 Months | |||||
| Riska | RD | Riska | RD | Riska | RD | Riska | RD | |
| <0.10 | 0.003 | Referent | 0.006 | Referent | 0.009 | Referent | 0.010 | Referent |
| 0.10–0.29 | 0.004 | 0.001 | 0.009 | 0.003 | 0.012 | 0.003 | 0.017 | 0.007 |
| 0.30–0.99 | 0.004 | 0.001 | 0.008 | 0.002 | 0.011 | 0.002 | 0.015 | 0.005 |
| ≥1.00 | 0.006 | 0.003 | 0.009 | 0.003 | 0.014 | 0.005 | 0.017 | 0.006 |
Abbreviations: ppm, parts per million; RD, risk difference; THC, total hydrocarbons.
a Risk estimates accounted for confounders (age, sex, education, smoking, and residential proximity to the spill) and predictors of censoring (age, education, ethnicity, smoking, cleanup work duration, and residential proximity to the spill) using inverse-probability weights.
Figure 2.
Cumulative risk of self-reported myocardial infarction/fatal coronary heart disease according to median total hydrocarbon (THC) exposure (parts per million (ppm)) before the oil well was capped on July 15, 2010 (n = 22,550), Gulf Long-Term Follow-up Study, United States, 2010–2016. Risk estimates accounted for confounders (age, sex, education, smoking, and residential proximity to the spill) and predictors of censoring (age, education, ethnicity, smoking, cleanup work duration, and residential proximity to the spill) using inverse probability weights.
The sensitivity analyses excluding 4,619 federally employed workers showed slightly increased hazard ratios for maximum THC exposure of ≥0.30 ppm. The hazard ratio for maximum THC exposure of ≥3.00 ppm (vs. <0.30 ppm) was 1.92 (95% CI: 1.14, 3.23) (Web Table 6). In analyses that controlled for work duration, we also observed slightly strengthened associations between THC exposure and heart attack (Web Table 7).
DISCUSSION
This study of Deepwater Horizon oil spill workers showed 62%–81% higher hazards for heart attack 5 years after the spill among those with estimated maximum THC exposure levels of ≥0.30 ppm. Risk differences comparing those with the highest to the lowest level of exposure were small in magnitude but showed persistent associations across follow-up. Accounting for differences in characteristics of those who completed the second interview using IP-censoring weights showed that results were generally robust to censoring, although the magnitudes of the observed associations were slightly attenuated when the weights were not applied.
Associations between median THC exposures and heart attack were weaker than associations with maximum exposure levels. Maximum exposures were meant to capture highest daily THC exposure while median exposure groups represented the typical exposures a worker experienced. Workers reported multiple jobs representing a wide range of exposures, and the ordinal exposure categories did not capture the full range of exposures workers might have experienced, because workers within an exposure category were all assigned the same value. Thus, the range of exposures was narrower and the distribution of median exposures was less variable than the distribution of maximum exposures, making it more difficult to detect an association with heart attack. We were unable to assess cumulative or continuous THC exposures because the ordinal job-exposure matrix-based estimates did not account for duration of oil-spill work tasks.
We observed persistence of the association between maximum THC exposure and heart attack risk across the follow-up period. Most studies of air pollutant exposures and heart disease have focused on short temporal periods between exposure and outcome (4, 24), and we are unaware of any studies that assessed persistent effects of short-term pollution exposures. Our results are consistent with studies that identified persistent respiratory symptoms 5 years after oil spill work (13), although our study is the first, to our knowledge, to consider persistence of heart disease risk among oil spill workers.
We evaluated the extent to which other factors, such as heat stress associated with cleanup work, explained the observed associations. Heat stress was common among workers (25), and heat stress or other physical stress can increase risk of heart attack (26, 27). Adjusting for self-reported heat stress did not meaningfully change the associations between THC exposure and heart attack. We were unable to account for any heat stress–related fatalities occurring during the oil spill cleanup or prior to the enrollment interviews, because participants had to be alive at the time of enrollment. Truncation of deaths prior to enrollment might have resulted in underestimation of heart attack risk and underestimation of the associations between spill-related exposures and heart attack, given that events were not observable among workers who died before study enrollment.
Healthier or more physically fit workers might have been less predisposed to heart attack compared with less fit workers and might have worked longer durations or worked on higher-skilled tasks with greater THC exposures, such as cleanup work on a vessel. Although the majority of oil spill work was completed in less than 1 year, these differences might have resulted in healthy-worker survivor bias (28, 29). When we controlled for work duration, we saw only a slight strengthening in the associations between THC exposure and heart attack, which is consistent with no appreciable healthy-worker survivor bias but might not have captured this bias if exposure strongly predicted retention in cleanup activities. If exposure resulted in higher rates of leaving employment or caused workers to alter their work tasks or behaviors to reduce exposure, then controlling for work duration to account for healthy-worker survivor bias might result in residual bias (29, 30). However, we do not think the THC exposures (or correlates) at the levels observed would have a strong effect on employment or work behaviors, and therefore the residual bias from adjusting for work duration would likely be very small (31).
In an analysis excluding the 4,619 federally employed workers, the hazard ratios for maximum THC exposure were slightly stronger compared with results in the full cohort. Federal workers had lower prevalence of self-reported physician-diagnosed hypertension compared with the remainder of the cohort (16% vs. 29%) and generally had lower THC exposures compared with other workers. These differences likely explain why associations strengthened when federal workers were excluded. Unmeasured differences among workers regarding physical fitness, diet, socioeconomic status, or underlying health might have otherwise attenuated associations if healthier workers were more likely to have higher THC exposures.
This study relied on self-reported information on nonfatal MI, which is subject to errors in reporting. Self-reported MI has shown moderate sensitivity (61%) when compared against adjudicator diagnosis (32). Recall of MI is also dependent on the time period for which disease was ascertained, but the 5-year period of this study is a relatively short period to recall a serious event such as an MI. There is also the possibility for competing risks (non-CHD death) to introduce bias in our conditional risk estimates. The Cox model assumes that censoring due to competing risks is noninformative, given the covariates considered in the model. Non-CHD death was rare during the study period (0.82% prevalence) and was not associated with THC exposure, and therefore bias due to competing risks is unlikely. Bias might occur if our models do not include confounders of the relationship between exposure and the competing events (33), but we do not anticipate such bias would be strong, given our adjustment set and our use of weights to account for informative censoring.
In summary, the GuLF Study is the largest study of the health impact of oil spills and is the first, to our knowledge, to investigate the association between THC exposure and heart attack risk among oil spill workers. Our study improves on exposure assessment methods used in past studies of oil spills by utilizing job-exposure matrix–based estimates of THC exposure derived from personal air measurements and detailed data on oil spill–work activities. Our study showed positive associations between the estimated maximum THC exposure during oil spill work and risk of heart attack 5 years after the spill. Future studies can make use of planned subsequent follow-up interviews to assess longitudinal changes in these associations and cumulative exposure measures for THC that are currently being developed.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (Jean Strelitz, Alexander P. Keil, David B. Richardson, Gerardo Heiss, Marilie D. Gammon, Lawrence S. Engel); Epidemiology Branch, National Institute of Environmental Health Sciences, National Institutes of Health, Department of Health and Human Services, Research Triangle Park, North Carolina (Dale P. Sandler, Richard K. Kwok, Lawrence S. Engel); Stewart Exposure Assessments, LLC, Arlington, Virginia (Patricia A. Stewart); and Exposure Assessment Applications, LLC, Arlington, Virginia (Mark Stenzel).
This study was supported by the National Institutes of Health Common Fund and the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences (grant Z01 ES102945). J.S. was supported by a training grant from the National Institute of Environmental Health Sciences (grant T32 ES007018).
We thank the study team at Social & Scientific Systems.
Conflict of interest: P.S. reports personal fees from Stewart Exposure Assessments, LLC, during the conduct of this study. M.S. reports personal fees from Exposure Assessment Applications, LLC, during the conduct of the study. No other authors report any competing financial interests.
Abbreviations
- CHD
coronary heart disease
- CI
confidence interval
- GuLF Study
Gulf Long-Term Follow-up Study
- HR
hazard ratio
- IP
inverse probability
- MI
myocardial infarction
- ppm
parts per million
- SD
standard deviation
- THC
total hydrocarbons
REFERENCES
- 1. Bard D, Kihal W, Schillinger C, et al. Traffic-related air pollution and the onset of myocardial infarction: disclosing benzene as a trigger? A small-area case-crossover study. PLoS One. 2014;9(6):e100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Peters A. Particulate matter and heart disease: evidence from epidemiological studies. Toxicol Appl Pharmacol. 2005;207(2 suppl):477–482. [DOI] [PubMed] [Google Scholar]
- 3. Pope CA 3rd, Muhlestein JB, May HT, et al. Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation. 2006;114(23):2443–2448. [DOI] [PubMed] [Google Scholar]
- 4. Brook RD, Rajagopalan S, Pope CA 3rd, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–2378. [DOI] [PubMed] [Google Scholar]
- 5. Kotseva K, Popov T. Study of the cardiovascular effects of occupational exposure to organic solvents. Int Arch Occup Environ Health. 1998;71(suppl):S87–S91. [PubMed] [Google Scholar]
- 6. Matanoski GM, Tao XG. Styrene exposure and ischemic heart disease: a case-cohort study. Am J Epidemiol. 2003;158(10):988–995. [PubMed] [Google Scholar]
- 7. Pope CA 3rd, Burnett RT, Thurston GD, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109(1):71–77. [DOI] [PubMed] [Google Scholar]
- 8. Xu X, Freeman NC, Dailey AB, et al. Association between exposure to alkylbenzenes and cardiovascular disease among National Health and Nutrition Examination Survey (NHANES) participants. Int J Occup Environ Health. 2009;15(4):385–391. [DOI] [PubMed] [Google Scholar]
- 9. Peters A, Dockery DW, Muller JE, et al. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001;103(23):2810–2815. [DOI] [PubMed] [Google Scholar]
- 10. Middlebrook AM, Murphy DM, Ahmadov R, et al. Air quality implications of the Deepwater Horizon oil spill. Proc Natl Acad Sci U S A. 2012;109(50):20280–20285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nance E, King D, Wright B, et al. Ambient air concentrations exceeded health-based standards for fine particulate matter and benzene during the Deepwater Horizon oil spill. J Air Waste Manag Assoc. 2016;66(2):224–236. [DOI] [PubMed] [Google Scholar]
- 12. Solomon GM, Janssen S. Health effects of the Gulf oil spill. JAMA. 2010;304(10):1118–1119. [DOI] [PubMed] [Google Scholar]
- 13. Zock JP, Rodríguez-Trigo G, Rodríguez-Rodríguez E, et al. Persistent respiratory symptoms in clean-up workers 5 years after the Prestige oil spill. Occup Environ Med. 2012;69(7):508–513. [DOI] [PubMed] [Google Scholar]
- 14. Meo SA, Al-Drees AM, Rasheed S, et al. Effect of duration of exposure to polluted air environment on lung function in subjects exposed to crude oil spill into sea water. Int J Occup Med Environ Health. 2009;22(1):35–41. [DOI] [PubMed] [Google Scholar]
- 15. Kwok RK, Engel LS, Miller AK, et al. The GuLF STUDY: a prospective study of persons involved in the Deepwater Horizon oil spill response and clean-up. Environ Health Perspect. 2017;125(4):570–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stewart PA, Stenzel MR, Ramachandran G, et al. Development of a total hydrocarbon ordinal job-exposure matrix for workers responding to the Deepwater Horizon disaster: The GuLF STUDY. J Expo Sci Environ Epidemiol. 2018;28(3):223–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. [PubMed] [Google Scholar]
- 19. Kwok RK, McGrath JA, Lowe SR, et al. Mental health indicators associated with oil spill response and clean-up: cross-sectional analysis of the GuLF STUDY cohort. Lancet Public Health. 2017;2(12):e560–e567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34(2):187–202. [Google Scholar]
- 21. Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. [DOI] [PubMed] [Google Scholar]
- 22. Cole SR, Hernán MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed. 2004;75(1):45–49. [DOI] [PubMed] [Google Scholar]
- 23. Fleming TR, Harrington DP. Counting Processes and Survival Analysis. Hoboken, NJ: John Wiley & Sons; 1991. [Google Scholar]
- 24. Abplanalp W, DeJarnett N, Riggs DW, et al. Benzene exposure is associated with cardiovascular disease risk. PLoS One. 2017;12(9):e0183602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. King BS, Gibbins JD Health Hazard Evaluation of Deepwater Horizon Response Workers. Centers for Disease Control and Prevention. National Institute for Occupational Safety and Health, 2011. https://www.cdc.gov/niosh/hhe/reports/pdfs/2010-0115-0129-3138.pdf. Accessed January 16, 2019.
- 26. Culić V. Acute risk factors for myocardial infarction. Int J Cardiol. 2007;117(2):260–269. [DOI] [PubMed] [Google Scholar]
- 27. Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9(6):360–370. [DOI] [PubMed] [Google Scholar]
- 28. Arrighi HM, Hertz-Picciotto I. The evolving concept of the healthy worker survivor effect. Epidemiology. 1994;5(2):189–196. [DOI] [PubMed] [Google Scholar]
- 29. Buckley JP, Keil AP, McGrath LJ, et al. Evolving methods for inference in the presence of healthy worker survivor bias. Epidemiology. 2015;26(2):204–212. [DOI] [PubMed] [Google Scholar]
- 30. Chevrier J, Picciotto S, Eisen EA. A comparison of standard methods with g-estimation of accelerated failure-time models to address the healthy-worker survivor effect: application in a cohort of autoworkers exposed to metalworking fluids. Epidemiology. 2012;23(2):212–219. [DOI] [PubMed] [Google Scholar]
- 31. Keil AP, Richardson DB, Westreich D, et al. Estimating the impact of changes to occupational standards for silica exposure on lung cancer mortality. Epidemiology. 2018;29(5):658–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Heckbert SR, Kooperberg C, Safford MM, et al. Comparison of self-report, hospital discharge codes, and adjudication of cardiovascular events in the Women’s Health Initiative. Am J Epidemiol. 2004;160(12):1152–1158. [DOI] [PubMed] [Google Scholar]
- 33. Lesko CR, Lau B. Bias due to confounders for the exposure-competing risk relationship. Epidemiology. 2017;28(1):20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.