Abstract
Objectives
Violence is one of the leading causes of death among youth ages 14–24. Hospital- and ED-based violence prevention programs are increasingly becoming a critical part of public health efforts; however, evaluation of prevention efforts is needed to create evidence-based best practices. Retention of study participants is key to evaluations, though little literature exists regarding optimizing follow-up methods for violently-injured youth. This study aims to describe the methods for retention in youth violence studies and the characteristics of hard-to-reach participants.
Methods
The Flint Youth Injury (FYI) Study is a prospective study following a cohort of assault-injured, drug-using youth recruited in an urban ED, and a comparison population of drug-using youth seeking medical or non-violence-related injury care. Validated survey instruments were administered at baseline and four follow-up time points (6, 12, 18, 24 months). Follow-up contacts used a variety of strategies and all attempts were coded by type and level of success. Regression analysis was used to predict contact difficulty and follow-up interview completion at 24 months.
Results
599 patients (ages 14–24) were recruited from the ED (mean age=20.1 years, 41.2% female, 58.2% African American), with follow-up rates at 6, 12, 18, and 24 months of 85.3%, 83.7%, 84.2%, and 85.3%, respectively. Participant contact efforts ranged from 2 to 53 times per follow-up timeframe to complete a follow-up appointment, and more than 20% of appointments were completed off-site at community locations (e.g., participants’ homes, jail/prison). Participants who were younger (p<.05) and female (p<.01) were more likely to complete their 24-month follow-up interview. Participants who sought care in the ED for assault injury (p<.05) and had a substance use disorder (p<.01) at baseline required fewer contact attempts to complete their 24-month follow-up, while participants reporting a fight within the immediate 3 months before their 24-month follow-up (p<.01) required more intensive contact efforts.
Conclusions
The FYI study demonstrated that achieving high follow-up rates for a difficult-to-track, violently-injured ED population is feasible through the use of established contact strategies and a variety of interview locations. Results have implications for follow-up strategies planned as part of other violence prevention studies.
Keywords: Methods, Injury Prevention, Violence Prevention, Emergency Medicine
Introduction
Violence is an important public health issue in the United States. Homicide is currently the third leading cause of death for youth between the ages of 14–24 years, and results in over $8.9 billion in medical and work lost costs a year in the United States (not accounting for non-fatal assault injuries).1 In addition to fatal injuries, more than 400,000 youth (14–24 years old) seek emergency department (ED) care annually for non-fatal assault injuries.1 Many of these youth are not regularly attending school2 or accessing primary care clinicians,2,3 which often serve as traditional sites for violence prevention programs. As a result, EDs have become the primary setting for many violence prevention programs, especially those that provide behavioral counseling and wrap around care management intervenitons,4,5 aimed at reducing the risk of future violence, especially for the hardest to reach, most at-risk youth.
While several promising ED- and hospital-based interventions for reducing violence have been described in prior studies,6–11 their effectiveness has been limited by high attrition rates. Violently-injured patients are particularly difficult to retain in longitudinal research, often due to increased environmental (home/family) instability and co-occurring alcohol and drug use disorders.12–14 High attrition rates are associated with compromised internal study validity.15 While statistical techniques exist to compensate for the inevitability of attrition, such techniques are less preferable to achieving high follow-up rates that allow for complete understanding of the outcome data.12–14,16,17 Further, external validity is compromised by attrition rates that are unequal across patient populations.13–16,18,19 While the literature has identified a series of successful follow-up strategies for tracking and retention of hard-to-reach substance use populations,12–16,20–23 such techniques have not been fully examined among assault-injured youth populations.
The objective of this study is to describe effective approaches for tracking and retaining participants during a two-year longitudinal study of violently-injured and substance-using youth that achieved 85% follow-up. The techniques described here could aid future study design for interventions, especially in terms of retention of hard-to-reach participants, and support public health efforts that address the high rates of violence among youth.
Methods
Study Design
This study is part of a larger two-year prospective longitudinal cohort study measuring the prevalence of substance use and violent injury among a sample of youth (14–24 years old) seeking ED care for assault-injuries and reporting past six-month drug use (AIG) and a comparison group of youth (proportionally sampled by age/gender) who were seeking ED treatment for non-assault reasons, but also reporting past 6-month drug-use (CG).2,24,25 The study was approved by both the University of Michigan and Hurley Medical Center’s Institutional Review Boards, and an NIH Certificate of Confidentiality was obtained.
Study Setting and Population
Youth were recruited at a public urban Level 1 Trauma Center ED in Flint, MI. The ED provides care for ~75,000 adult and ~25,000 pediatric patients (<20 years-old) annually. Flint has high rates of violent crime (14.8/1000 population) that are comparable to other well-known de-industrialized urban centers, including Detroit, Michigan; Camden, New Jersey; and Oakland, California.26
Sample Recruitment
Patients 14–24 years-old seeking care for an assault injury, as well as a consecutively enrolled comparison group based on sex and age range (i.e. 14–17; 18–20; and 21–24), who reported past-six-month drug use on a private, self-administered computerized screening survey were eligible for inclusion in the longitudinal study. Youth were excluded if they were not able to provide informed consent (e.g., altered mental status, psychosis, non-English speaking), presented for child abuse, acute sexual assault, or suicidal ideation/attempt. Patients were recruited seven days per week, for 21 hours per day (5 am–2 am) on Tuesday and Wednesday and for 24-hours per day on Thursday through Monday between December 2009 and September 2011.
Study Protocol
Assault-injured youth were identified through electronic medical records, and approached by trained research assistants (RAs) in treatment spaces or waiting rooms. Assaults were defined as any injury intentionally caused by another person and included gunshot wounds, being struck by/against (punching), and stab wounds. RAs assessed whether the injury complaint fit the definition of assault when they approached potential participants. Youth agreeing to study participation completed written consent (written assent with parental consent if they were <18 years-old), and self-administered a private computerized screening survey to assess eligibility (i.e., past 6-month drug use).24 Participants who completed the screen were compensated with a dollar store gift worth $1.00. The CG was enrolled consecutively with the AIG to limit seasonal and temporal variation, and was proportionally balanced by age range (as above) and sex. For example, after identifying a 20-year old female with an acute assault-related injury and past six-month drug use on the screening survey, the RA would recruit sequentially, by time of triage, the next 18–20-year-old female seeking ED care for a medical complaint or unintentional injury (e.g., motor vehicle crash); those screening positive for any past six-month drug use would be consented for inclusion in the longitudinal study. After consenting for the longitudinal study, eligible participants completed a second written assent/consent (and parental consent < 18), and completed a ~90-minute baseline survey, including both an RA-administered structured interview and a computerized self-administered survey portion. This consent process included a consent for the study team to review the patient’s medical record. Remuneration was $20 cash. Additionally, any patient who was unstable while in the ED could be recruited on the hospital floors if they stabilized within 72 hours from triage.
Follow-up assessments were conducted at 6, 12, 18, and 24 months at a location convenient for the participant, including the study ED, community locations (e.g., library, restaurant, their homes), via telephone, or in jail/state prison (process described below) if the participant was incarcerated during the follow-up period. If needed, transportation to follow-up appointments was provided. Remuneration included $30 for the 6-month interview, $35 for the 12-month interview, $35 for the 18-month interview, and $45 for the 24-month interview. Cash payments were provided at each follow-up. Participants were also provided with a toll-free phone number to contact study offices and were remunerated $5 per interview if they telephoned the study office within 2 weeks of their scheduled interview date and confirmed or rescheduled their appointment. Incarcerated participants were not allowed compensation. Participants who turned 18 during the follow-up timeframe were consented as adults at their next appointment. Family and friends accompanying the patient were not allowed to observe or participate during survey administration.25
Participant Tracking Protocol
At the index ED visit, participants completed a locator form providing information for study personnel to contact them for follow-up interviews. Specific data collected included: 1) date of birth; 2) social security number; 3) telephone numbers (e.g., cellular, home, others; including optimal contact number and times of day); 4) living and mailing address, including any plans to move; 5) email address; 6) social media account information (e.g., Facebook); 7) work address/phone number with associated permission to contact; 8) school information (if relevant); 9) organized extracurricular activity involvement; and, 10) information regarding legal status (i.e., whether the participant anticipates being in jail or state prison at the time of follow-up). Study RAs also gathered contact information (e.g., names, telephone number, addresses) for at least two people (e.g., a spouse, family member, or friend) who would know the patient’s whereabouts during the study period. Participants were also asked to provide the names for locations they frequented (e.g., churches, shelters).
Participant Follow-up and Contact Protocol
See Table 1, for a timetable of contacts. At the time of their ED visit, participants were given business cards with the project logo, phone numbers to the study office, date of next interview, and potential payment amounts. Additionally, participants were given small gifts (e.g., pens) that contained both the project logo and contact information. The project business card and gifts were given to participants at each follow-up interview and at every home visit attempt.
Table 1.
Tracking Techniques used to Locate and Interview Participants and Timeline of Contact Efforts
| Tracking Strategy | Examples | Timeframe Used |
|---|---|---|
| Participant Information Collected |
|
At each successful contact or follow-up interview this information was updated |
| Standard Tracking Procedures/Effort |
|
Given at time of initial contact, follow-up interview, and each letter and home visit effort. |
|
48 hours after ED visit | |
|
3 months before interview | |
|
4 weeks before interview | |
|
2 weeks before due date | |
|
After each interview | |
|
Mid-end of December | |
|
24 hours before appointment | |
| Tracking Procedures/Effort for Hard-to-Reach participants |
|
As needed, repeated letters to all known addresses 2 weeks before due date-if participant is non-compliant. |
|
As needed, repeated calls to working numbers 2 weeks before due date-if participant is non-compliant. | |
|
As needed-if participant is non-compliant or in jail | |
| Participant Incentives |
|
At each interview |
Participants were called 48 hours after their index ED visit to confirm their contact information and that their 6-month appointment had been scheduled. Between each longitudinal follow-up time point, RAs contacted participants a minimum of four times. First, approximately 3 months prior to each scheduled 6-, 12-, 18-, and 24-month follow-up appointment, a post card was sent to the participant, which included information on their scheduled date, time, and location of the appointment. The postcard also contained information on the remuneration for participation in the follow-up, and provided study contact information for the participant to reschedule their appointment if necessary. Next, a “reminder” letter was sent to each participant 4 weeks before their intended appointment. This letter included the same information as the postcard that was sent prior, if information had not been updated. Third, two weeks prior to each follow-up appointment, a reminder post card was sent to the participant. Finally, RAs contacted participants by phone the day prior to their appointment to confirm the date/time.
In addition to these four scheduled contacts, RAs also sent a “thank you” letter or post card after each follow-up appointment to remind participants of their next scheduled appointment, and would send holiday cards to participants mid-December to keep them engaged with the study.
For participants who had letters returned due to wrong mailing address, RAs would attempt phone contact with the participant and/or complete appropriate searches through the medical record (consent granted in initial consent document) or public search databases to obtain new contact information. For appointments where the participant missed their scheduled date and time, RAs would attempt to contact participants within 15–30 minutes to assess if they were planning to arrive late or needed to reschedule. If participants failed to arrive for their appointment, RAs would send a missed appointment letter encouraging them to reschedule.
For participants who missed their scheduled follow-up, multiple additional attempts at contact were made. In addition to the contact attempts detailed above, participants that did not show up for appointments were sent texts, emails, and Facebook messages. These methods of contact were noted as part of the consent signed at time of study enrollment. If participants were unable to be reached via the contact information provided at the time of the ED visit, a search of their medical record and public databases was conducted, and more intensive contact attempts were made. First, a review of the participant’s medical record, which included confirming information provided by the participant and adding new contact information, was conducted. Then, public databases, such as Department of Public Health death records, internet people finder databases (e.g., Alumnifinder, Yahoo people search), and offender and prison websites were reviewed. If contact information was still not found, a visit to the participant’s home was scheduled. A letter informing the participant of the home visit was sent out at least 1 week before the scheduled visit. Home visits were conducted with two interviewers (for safety) and took place during daylight hours. If the participant was not home, interviewers left friendly, handwritten notes on index cards, similar to the ones given to the participant at baseline. During visits to the participant’s residence, study personnel would attempt to contact neighbors (without revealing that the study was related to substance use or violence) to confirm if the participant resided at that address or if they knew a more current address. During winter months, letters were left at local shelters or soup kitchens where homeless participants were known to have previously stayed or visited.
For participants incarcerated at the time of follow-up, the study received permission from both the MDOC (Michigan Department of Corrections), both (U-M and Hurley) IRBs, and from participants themselves to contact them while in jail/state prison. If participants were known to be in jail or state prison during their follow-up appointment (either through a search of publically available offender websites, or family members or participants themselves notifying the study team), a letter was sent to the warden of the jail or state prison introducing the study, as well as providing a copy of the MDOC approval letter granting the study permission to conduct the interview while the participant was incarcerated (which was obtained at the outset of the study). After the warden provided written permission for the study to conduct the follow-up interview, the written permission was submitted to the IRB and appointments were made with the jail/state prison and the participant to set up a time to conduct the follow-up interview. Interviews were conducted over the phone or in-person within interview rooms. Response cards were used to preserve confidentiality; data from participants were not shared with the warden or prison staff.
For all contact attempts, participants were called during the times they indicated during the initial study interview were most convient for them. Typically, interviewers would call throughout the day (9am–8pm), leaving only a single message per day. During subsequent participant interactions, their contact information was verified and/or updated. In compliance with IRB requirements, if at any time participant asked not to be contacted, they were thanked for their participation in the study and no further contact efforts were attempted. Participants were allowed a total of 3 months to complete a follow-up after their exact follow-up date (i.e., for the 6 month follow-up interview, participants had 90 days to complete their appointment from their 6 month post ED date before they would time out for that follow-up appointment). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies, and the funding agencies had no role in the conduct or reporting of the study.
Measures
Outcome Measures
Completion of study follow-up at 6, 12,18 and 24 months was examined. Completion was not necessarily consecutive (i.e., the few who did not complete the 6 month follow-up could complete the 12, 18 or 24 month follow up interviews). Subsequently, contact difficulty at the 24 month time point was examined. Difficulty was measured by the number of contacts required to complete follow-up or determine the patient would not complete the interview (i.e. patient declined or the study was completed). Contact difficulty was defined as needing more contact attempts. Contact attempts include both attempts made by staff and by participants. Study team initiated and participant initiated contact attempts were combined into a single metric in order to fully capture the resources and scope of work needed to successfully complete follow ups among a high risk population
Tracking Measures
Every contact attempt made by a staff member to reach a participant or from a participant to the study team was recorded in their unique follow-up file folder. Information collected on contacts included date, time, type of contact (mail, email, call, home visit), who was involved (e.g., participant, family member, unknown), and the main focus of the contact (e.g., change of address).
Socio-demographics
Demographics and socio-economic measures (i.e., age, gender, race, public assistance) were collected using validated measures from the Drug Abuse Treatment Outcome Studies (DATOS)27 and the National Longitudinal Study of Adolescent Health.28 For analysis, race was dichotomized as African American vs. Other given that African-Americans comprise 57% of the Flint community.29
Baseline Substance Use Disorder
The RA-administered Mini International Neuropsychiatric Interview (MINI, version 6.0, 1/1/10) was used to assess whether participants met diagnostic criteria for an alcohol or drug use disorder (i.e. abuse or dependence) at the time of the baseline assessment.30
Past 3-month Violence
The Time Line Follow Back (TLFB)-Aggression Module (TLFB-AM), developed to be used with the TLFB, assessed detailed characteristics of incidents of physical violence in the past 90 days and was administered at baseline and during each of the subsequent follow-up appointments.31–33 Using monthly calendars, beginning on the day of assessment, and working backwards, participants were asked to identify specific dates in which they experienced interpersonal conflict (whether victimization or aggression) with partners or others.31
Data Analysis
All analyses were conducted using SAS 9.4. To define different participants and the number of contact attempts needed to reach them, those that were easy to reach were defined as those in the lower three quartiles of contact attempts made or received at each time point; the hard-to-reach was defined as the top quartile of number of contact attempts made or received. A phi coefficient was calculated to determine the relationship between where a participant completed their follow-up at 6-months and at 24-months. Chi-square analyses and t-tests were used to evaluate bivariate associations with the outcome of interest (i.e., follow-up completion). We used a significance level of α=.05 for all hypothesis tests. A logistic regression was used to identify variables associated with 24-month follow-up completion (completed 24-month follow-up versus not completed). Predictors in the model were chosen to account for the sampling scheme (i.e., age, sex), theoretical considerations (i.e., race, public assistance), and significance in bivariate comparisons (i.e., substance use disorder, AIG). A separate analysis was conducted to determine the variables associated with contact difficulty. Due to overdispersion in the outcome variable of contact difficulty (total number of contact attempts), a negative binomial regression was used to predict contact difficulty at 24-month among the entire sample. Again, background characteristics were included in the model based on prior literature, or based on significance in bivariate analyses.
Results
Sample Characteristics
The baseline and longitudinal FYI sample has been described in prior publications.2,24,25 The longitudinal sample included 349 youth in the assault-injury group (AIG) and 250 youth in the comparison group (CG). Differences in group sample size was due to oversampling the AIG to meet the aims of the original grant.25 At baseline, participants were mostly Black (58%), male (59%), and in receipt of public assistance (73%). No baseline differences were observed between the two groups (AIG vs. CG) with respect to age, sex, race, or receipt of public assistance.
Follow-up Rates and Characteristics
The longitudinal sample was followed for 24 months at 6-month intervals. Follow-up completion rates were 85.3%, 83.7%, 84.2%, and 85.3% at 6, 12, 18, and 24 months, respectively. There were no significant differences in completion rates by time point. The majority of follow-up interviews (78.9%) were completed at the study site where the initial ED encounter took place. The study site was easy for participants to find, with relatively good access to transportation, and was considered a safe place in the community. The next most common location for completion of follow-up interviews was the participant’s home (9.5% of follow-up interviews), although this was noted to decrease over time. At the 6-month follow-up, 14% of follow-up appointments occurred at the participant’s home, while at 24 months only 7% were completed at a participant’s home. In total, 2% of follow-up appointments were completed at community locations (e.g., at a fast food restaurant, public library) other than the hospital or participant’s home. Participants completed their follow-up appointment in jail/state prison 3.4% of the time (by time point: 2.9% at 6-months, 3.0% at 12-months, 4.4% at 18-months, and 3.5% at 24-months). Participants were also given the option to complete their follow-up appointment over the phone if it was not possible to meet in person. At 6 months, 4% of appointments were completed over the phone, while at 24 months, 10% were completed over the phone. Participant completing the 6-month follow-up at the study site more likely to complete their 24-month follow-up interview at the study site (phi coefficient= .5508, p<.001). However, participants completed more home visit interviews at 6 months than at 24 months, and more phone interviews at 24 months than 6 months (p<.001).
Follow-Up Contact Attempts
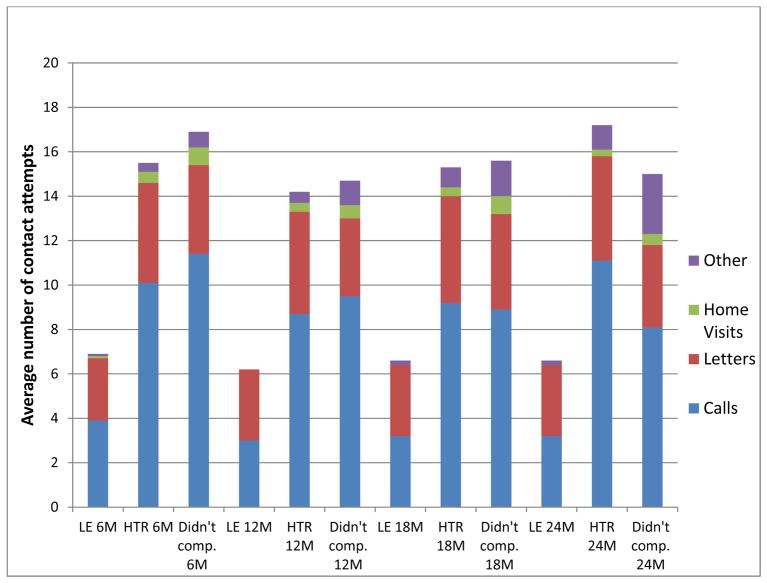
Figure 1 shows the average number of contact attempts per participant by contact type and appointment time point. Contact attempts include both attempts made by staff and by participants, and included both a standard contact protocol and hard-to-reach contact protocol (see table 1). Each time point shows the average number of contacts required to reach someone who needed the “least effort” (among the lower 3 quartiles of contact attempts but completed the appointment) as well as the average for those who were “hard-to-reach” (among the upper quartile of contact attempts but completed the appointment), and the contact attempts for participants who did not complete the appointment. Easy-to-reach participants (those requiring the least effort) initiated/recieved an average of 6.2 (standard deviation (SD)=1.5) contact attempts, 97–100% of which were phone calls and letters. Hard-to-reach participantsinitiated/recieved 14.1 (SD=6.0) contact attempts, with only 92–94% of contact attempts by phone and 6–8% contact attempts requiring more intensive contact methods beyond the standard calls and letters, such as home visits, text messages, and public database searches. Participants who did not complete appointments initiated/recieved 15.7 (SD=9.3) contact attempts, and required 9–21% of these attempts to be more intensive (e.g., home visits, text messages, public database searches).
Figure 1. Average Number of Contact Attempts per participant by Contact Type and Follow-Up Interview.
LE= least effort, lower 3 quartiles
HTR = Hard to reach, upper quartile
M=Month
Other= any methods used other than calls, letters or home visits (i.e., texts, Facebook messages, emails, letters and/or emails to the warden of a jail/state prison, etc.)
Factors Associated with 24 months Appointment Completion
Younger (p<.05) and female (p<.01) participants were more likely to complete their 24-month follow-up interview. Race, receiving public assistance, a baseline diagnosis of a substance use disorder and belonging to the AIG did not affect 24-month follow-up completion (Table 2). There was no evidence for severe lack of model fit based on the Hosmer and Lemeshow test (p=0.39).
Table 2.
MultivariableLogistic Regression of Participant Completion of the 24 Month Follow-Up Appointment (n=599)
| Baseline Characteristics | AOR (95% CI) |
|---|---|
| Age | 0.86 (0.77–0.97)* |
| Female | 2.28 (1.24–4.18)** |
| African-American | 1.44 (0.85–2.43) |
| Public Assistance | 1.17 (0.66–2.07) |
| Substance Use Disorder | 0.79 (0.45–1.37) |
| Assault-injury Group (AIG) | 0.94 (0.55–1.60) |
Note: CI= Confidence Interval, AOR: adjusted odds ratio.
p< 0.05;
p< 0.01;
p< 0.001
Factors Associated with Contact Difficulty at 24 Months Post-ED Visit
At 24 months, AIG participants (p<.05) and those who met diagnostic criteria for a substance use disorder at baseline (p<.01) required fewer contact attempts, while participants reporting a violent fight within the 3 months prior to their 24-month follow-up (p<.01) required a greater number of contact attempts to complete their 24-month follow-up. Contact difficulty was defined as needing more contact attempts. Age, sex, race, and receiving public assistance did not affect contact difficulty (Table 3). The deviance to degrees of freedom ratio was 1.01, indicating good model fit. The largest variance inflation factor was 1.06 indicating that collinearity was not a concern in either model.
Table 3.
Negative Binomial Regression of Contact Difficulty at 24-Month Follow-Up Appointment (n=599)
| Participant Characteristic | IRR | 95% CI |
|---|---|---|
| Age | 1.004 | (0.983–1.025) |
| Female | 0.992 | (0.897–1.097) |
| African American | 1.038 | (0.964–1.117) |
| Receive Public Assistance | 0.953 | (0.852–1.067) |
| Assault Injury at Baseline* | 0.906 | (0.821–1.000) |
| Substance Use Disorder at Baseline** | 0.861 | (0.779–0.952) |
| Have Fights in 3 months leading up to 24 month follow-up ** | 1.060 | (1.023–1.098) |
Note: CI= Confidence Interval, IRR: incident rate ratio
p< 0.05;
p< 0.01;
p< 0.001
Discussion
Following violently-injured research study participants requires extensive effort and dedication. This is particularly challenging in emergency department-based studies where patients have an episodic connection to care rather than a longitudinal relationship. To our knowledge this is the first study to describe methodological best practices for successful retention of high-risk youth populations recruited from emergency department (ED) settings. Previous research on substance-using populations has demonstrated effective strategies for minimizing attrition which informed the strategies employed with our violently-injured youth population to achieve a greater than 85% follow-up rate.12–16,20–23
We also describe the characteristics of the hardest-to-reach sample. Importantly, this paper demonstrates both the feasibility of following this hard-to-reach sample, and the significant effort and resources required to do so successfully. Understanding this population and the contact efforts necessary are crucial to successfully completing valid studies in injury research. Although some degree of attrition is inevitable, without the inclusion of the hard-to-reach sample, biased results are more likely.15 Quantifying the effort required to achieve the follow-up necessary for validity allows for better targeting of limited resources in future studies. This effort was uniquely designed to create the greatest accessibility to the study population. To that end we have provided detail regarding methods and resources used for the successful follow-up protocols.
Completion of the 24-month follow-up interview was associated with being younger and of female gender, without any significant differences for self-reported race, receipt of public assistance, substance use disorder, or having sustained an assault injury. The association of younger participants may reflect a difference in housing stability, as early adulthood is characterized by major transitions in housing.34 Younger participants would be more likely to continue to live with their parents or guardians for the duration of the study versus living independently. The latter would be expected to result in greater mobility, less stability, and thus a greater difficulty reaching or locating such participants. Additionally, although transportation was aided with taxi/bus vouchers, participants who were younger and lived with other family members likely had access to family modes of transportation that our older participants did not. Lastly, the association of female gender could be due to the known trend for females to seek care more often than males,35 and thus be more likely to be connected to the medical system and more likely to complete their follow-up appointment.
Participants in the assault-injured group required less contact effort than the comparison group to complete the 24-month follow-up appointment. The finding that the acutely violently injured patient that seek care in the ED is easier to track, likely reflects that people in the AIG who sustained a violent injury may have more frequent contacts with the medical system in the months after an injury (e.g., follow-up visits to orthopedics/trauma surgery, etc.). These contacts may promote a stronger connection with the medical system, making such patients more likely to complete follow-up visits. For a visit for a more minor medical issue such as strep throat, young, otherwise healthy participants may not have the same degree of linkage with the medical system.
Conversely, participants with recent violence (fighting within 3 months preceding 24-month follow-up visit), required greater effort to complete the follow-up interview. It may be the contemporaneous violence occurring at their time in their life made scheduling more difficult, or that an ongoing conflict may cause participants to “lay low” or avoid encounters with unfamiliar individuals or locations out of fear of recurrence of fighting, retribution, or exposure to the police/authorities, thereby making them much more difficult to contact through regular channels.
Participants with a substance use disorder at baseline also required fewer contact attempts to complete the 24-month follow-up interview. Although this may reflect a greater motivation to obtain compensation, measures of low socioeconomic status such as receiving public assistance were not significantly associated with contact difficulty. Alternatively, those with a substance use disorder may also be more highly connected to nearby substance abuse treatment clinics and community resources that improved their access to the interview sites and reliable points of contact. Similar findings have been observed in previous studies.13
We did note a trend requiring greater flexibility in location of follow-up appointment and types of contact attempts to complete the follow-up interview over time. Initially, more interviews were completed at the participant’s home, but at 24 months a greater number of interviews required phone completion. This may reflect the transient nature of our sample, which made home visits impossible in later follow-up appointments due to movement outside of the study city and state. Future studies will need to ensure a robust process for conducting phone or web-based interviews and delivering the participation stipend in order to adequately capture such samples accurately.
The resources required to complete follow-up assessments with the hard-to-reach population were significantly greater than those required for the general study sample. In order to plan for adequate follow-up rates to support acceptable internal and external study validity, future studies should plan to invest follow-up resources accordingly in order to reach their hard-to-reach sample. Staffing on the follow-up portion of this study included a masters-level coordinator, two full-time bachelors level research assistants, and one part-time research assistant.
In this study, use of technology such as text messaging, email, and social media did not play a major role in contact attempts, for many reasons. First, many of our participants did not have active email accounts (based on self-report). Next, at the time of the study 2009–2013, many participants did not have access to unlimited text/SMS message services and many used phone plans purchased by minutes of use (minute phones), and asked the study team not to text them. Third, access to Wi-Fi and 3G/4G/LTE service within this community is limited, making it difficult to connect with participants through the internet. Lastly, per our IRB protocol, we were only allowed to private message participants on Facebook. We did not “friend” participants or “write on their walls”. These private non-friend messages would automatically arrive in an alternative message inbox (due to not being friends), which most participants were not aware of or checked often. Current studies in this population have been able to utilize SMS messaging more frequently and successfully, and the use of apps to aid in research has promising contact potential.
This study analyzes data from a 24-month ED-based prospective cohort study of assault-injured, drug-using youth to describe methodological best practices for successful retention of high-risk youth populations recruited from emergency department (ED) settings. It should be noted that other analyses from this study have examined trajectories of the study population over the 24-month time period. These analyses include joint trajectories of alcohol use and anxiety/depression symptoms over time,36 prediction of future firearm violence,37 trajectories of marijuana use,38 and predictors of assault re-injury.25
Limitations
Study limitations should be recognized. First, this study was conducted at a single ED in a deindustrialized Midwestern city, potentially limiting generalizability. However, the profile of this ED is similar to those of other urban level-1 trauma centers. Further, our sample reflects the racial composition of Flint. Future studies may want to explore samples with broader ranges of ethnicities and races, particularly Hispanic youth. This study still adds to the literature, however, given that few prior investigations have provided this granular level of information on follow-up with hard-to-reach populations. These data relied on staff to record every contact attempt made with a participant; for most incidences, we did not have a way to independently verify that every attempt was recorded. However, staff were trained to log all contact attempts and the study coordinator conducted monthly supervision and quality assurance on contact notes.
Conclusions
The FYI study demonstrated that achieving high follow-up rates for a difficult-to-track violently-injured ED population is feasible. This was achieved by employing established contact strategies and flexible interview locations which were important for interview completion in this hard-to-reach group. Future studies focusing on hard-to-reach populations should take into account the time needed to achieve successful follow-up retention, and the number and types of contacts needed to ensure the continued involvement of as many participants as possible. Further, newer developing methods of contacting participants through advancements in technology should be explored. Using these methods to reduce attrition should improve the quality of hospital- and ED-based violence prevention programs, and help promote evidence-based best practices.
Acknowledgments
Funding Support: This work was funded by NIDA R01 024646 and in part, by CDCP 1R49CE002099, NIH/NIDA K23DA039341, NIAAA K23AA022641, The National Center for Advancing Translational Sciences of the NIH (2UL1TR000433), and NICHD R03HD087520.
The authors wish to acknowledge project staff, including Kaneesha Wallace, MBA, Lynn Massey, LMSW, Linping Duan, MS, and Sonia Kamat for their assistance in data and manuscript preparation. Finally, special thanks are owed to the patients and medical staff of the Hurley Medical Center (HMC) for their support of this project.
Abbreviations
- ED
Emergency Department
- HMC
Hurley Medical Center
- UM
University of Michigan
- IRB
Institutional Review Board
Footnotes
Prior Presentations: Clery SAEM 2016: Michael Clery, Jessica Roche MPH, Maureen Walton MPH PhD, Patrick Carter MD, Rebecca Cunningham MD. (May 2016). Violence prevention efforts - Methods to retain participants in youth violence research. Society for Academic Emergency Medicine. New Orleans, LA.
No conflict of interest
JR, MC, ADL, PC, MW, RC, QN report no conflict of interest.
Author contributions: MW and RC were responsible for the original study concept and design, JR, MW, PC and RC were responsible for the the manuscript concept and data acquisition. JR, MW, PC, and RC were responsible for the analysis and interpretation of the data. JR was responsible for drafting of the manuscript. All authors were responsible for critical revision of the manuscript for important intellectual content. PC, RC, MW, QN and JR were responsible for statistical expertise, and MW and RC were responsible for the acquisition of funding
Contributor Information
Jessica S. Roche, Email: jroche@med.umich.edu.
Michael J. Clery, Email: clery@med.umich.edu.
Patrick M. Carter, Email: cartpatr@med.umich.edu.
Aaron Dora-Laskey, Email: doralask@med.umich.edu.
Maureen A. Walton, Email: waltonma@med.umich.edu.
Quyen M. Ngo, Email: qen@med.umich.edu.
Rebecca M. Cunningham, Email: stroh@med.umich.edu.
References
- 1.Web-based Injury Statistics Query and Reporting System (WISQARS) 2017 doi: 10.1016/j.jsr.2017.01.001. at www.cdc.gov/ncipc/wisqars. [DOI] [PMC free article] [PubMed]
- 2.Bohnert KM, Walton MA, Ranney M, et al. Understanding the service needs of assault-injured, drug-using youth presenting for care in an urban Emergency Department. Addictive behaviors. 2015;41:97–105. doi: 10.1016/j.addbeh.2014.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grove DD, Lazebnik R, Petrack EM. Urban emergency department utilization by adolescents. Clinical pediatrics. 2000;39:479–83. doi: 10.1177/000992280003900806. [DOI] [PubMed] [Google Scholar]
- 4.Shibru D, Zahnd E, Becker M, Bekaert N, Calhoun D, Victorino GP. Benefits of a hospital-based peer intervention program for violently injured youth. Journal of the American College of Surgeons. 2007;205:684–9. doi: 10.1016/j.jamcollsurg.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 5.Carter P, Roche J, Walton M, Cunningham R. 29 Open-pilot of an ed-based multi-session remote therapy intervention (rti) for violence. Injury Prevention. 2017;23:A11-A. [Google Scholar]
- 6.Becker MG, Hall JS, Ursic CM, Jain S, Calhoun D. Caught in the crossfire: the effects of a peer-based intervention program for violently injured youth. Journal of Adolescent Health. 2004;34:177–83. doi: 10.1016/j.jadohealth.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. Journal of Trauma and Acute Care Surgery. 2006;61:534–40. doi: 10.1097/01.ta.0000236576.81860.8c. [DOI] [PubMed] [Google Scholar]
- 8.Cheng TL, Wright JL, Markakis D, Copeland-Linder N, Menvielle E. Randomized trial of a case management program for assault-injured youth: impact on service utilization and risk for reinjury. Pediatric emergency care. 2008;24:130–6. doi: 10.1097/PEC.0b013e3181666f72. [DOI] [PubMed] [Google Scholar]
- 9.Karraker N, Cunningham RM, Becker MG, Fein JA, Knox LM. Violence is preventable: a best practices guide for launching & sustaining a hospital-based program to break the cycle of violence. Office of Victims of Crime, Office of Justice Programs, US Department of Justice; Washington, DC: 2011. [Google Scholar]
- 10.Zun LS, Downey L, Rosen J. The effectiveness of an ED-based violence prevention program. The American journal of emergency medicine. 2006;24:8–13. doi: 10.1016/j.ajem.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 11.De Vos E, Stone DA, Goetz MA, Dahlberg LL. Evaluation of a hospital-based youth violence intervention. American journal of preventive medicine. 1995;12:101–8. [PubMed] [Google Scholar]
- 12.Scott CK. A replicable model for achieving over 90% follow-up rates in longitudinal studies of substance abusers. Drug and alcohol dependence. 2004;74:21–36. doi: 10.1016/j.drugalcdep.2003.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cunningham R, Walton MA, Tripathi SP, Outman R, Murray R, Booth BM. Tracking inner city substance users from the emergency department: how many contacts does it take? Academic emergency medicine. 2008;15:136–43. doi: 10.1111/j.1553-2712.2008.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bootsmiller BJ, Ribisl KM, Mowbray CT, Davidson WS, Walton MA, Herman SE. Methods of ensuring high follow-up rates: lessons from a longitudinal study of dual diagnosed participants. Substance Use & Misuse. 1998;33:2665–85. doi: 10.3109/10826089809059344. [DOI] [PubMed] [Google Scholar]
- 15.Ribisl KM, Walton MA, Mowbray CT, Luke DA, Davidson WS, Bootsmiller BJ. Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: Review and recommendations. Evaluation and Program Planning. 1996;19:1–25. [Google Scholar]
- 16.Cotter RB, Burke JD, Loeber R, Navratil JL. Innovative retention methods in longitudinal research: A case study of the developmental trends study. Journal of Child and Family Studies. 2002;11:485–98. [Google Scholar]
- 17.Claus RE, Kindleberger LR, Dugan MC. Predictors of attrition in a longitudinal study of substance abusers. Journal of psychoactive drugs. 2002;34:69–74. doi: 10.1080/02791072.2002.10399938. [DOI] [PubMed] [Google Scholar]
- 18.Prinz RJ, Smith EP, Dumas JE, Laughlin JE, White DW, Barrón R. Recruitment and retention of participants in prevention trials involving family-based interventions. American journal of preventive medicine. 2001;20:31–7. doi: 10.1016/s0749-3797(00)00271-3. [DOI] [PubMed] [Google Scholar]
- 19.Hansen WB, Collins LM, Malotte CK, Johnson CA, Fielding JE. Attrition in prevention research. Journal of behavioral medicine. 1985;8:261–75. doi: 10.1007/BF00870313. [DOI] [PubMed] [Google Scholar]
- 20.Hobden K, Curtis Forney J, Wyszacki Durham K, Toro P. Limiting attrition in longitudinal research on homeless adolescents: What works best? Journal of Community Psychology. 2011;39:443–51. [Google Scholar]
- 21.Desmond DP, Maddux JF, Johnson TH, Confer BA. Obtaining follow-up interviews for treatment evaluation. Journal of substance abuse treatment. 1995;12:95–102. doi: 10.1016/0740-5472(94)00076-4. [DOI] [PubMed] [Google Scholar]
- 22.Twitchell GR, Hertzog CA, Klein JL, Schuckit MA. The anatomy of a follow-up. British Journal of Addiction. 1992;87:1327–33. doi: 10.1111/j.1360-0443.1992.tb02741.x. [DOI] [PubMed] [Google Scholar]
- 23.Marmor JK, Oliveria SA, Donahue RP, et al. Factors encouraging cohort maintenance in a longitudinal study. Journal of clinical epidemiology. 1991;44:531–5. doi: 10.1016/0895-4356(91)90216-v. [DOI] [PubMed] [Google Scholar]
- 24.Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, Walton MA. Characteristics of youth seeking emergency care for assault injuries. Pediatrics. 2014;133:e96–e105. doi: 10.1542/peds.2013-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cunningham RM, Carter PM, Ranney M, et al. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA pediatrics. 2015;169:63–70. doi: 10.1001/jamapediatrics.2014.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Federal Bureau of Investigation. Uniform Crime Reports: Table 8 - Offenses Known to Law Enforcement by State by City. 2017. [Google Scholar]
- 27.Handelsman L, Stein JA, Grella CE. Contrasting predictors of readiness for substance abuse treatment in adults and adolescents: A latent variable analysis of DATOS and DATOS-A participants. Drug and alcohol dependence. 2005;80:63–81. doi: 10.1016/j.drugalcdep.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 28.Sieving RE, Beuhring T, Resnick MD, et al. Development of adolescent self-report measures from the National Longitudinal Study of Adolescent Health. Journal of adolescent health. 2001;28:73–81. doi: 10.1016/s1054-139x(00)00155-5. [DOI] [PubMed] [Google Scholar]
- 29.US Census Bureau. American Factfinder. 2010. Profile of general population and housing characteristics: 2010 demographic profile data. [Google Scholar]
- 30.Sheehan DV, Sheehan KH, Shytle RD, et al. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID) The Journal of clinical psychiatry. 2010;71:313–26. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- 31.Chermack ST, Grogan-Kaylor A, Perron BE, Murray RL, De Chavez P, Walton MA. Violence among men and women in substance use disorder treatment: A multi-level event-based analysis. Drug and alcohol dependence. 2010;112:194–200. doi: 10.1016/j.drugalcdep.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chermack ST, Blow FC. Violence among individuals in substance abuse treatment: The role of alcohol and cocaine consumption. Drug and alcohol dependence. 2002;66:29–37. doi: 10.1016/s0376-8716(01)00180-6. [DOI] [PubMed] [Google Scholar]
- 33.Chermack ST, Wryobeck JM, Walton MA, Blow FC. Distal and proximal factors related to aggression severity among patients in substance abuse treatment: family history, alcohol use and expectancies. Addictive behaviors. 2006;31:845–58. doi: 10.1016/j.addbeh.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 34.Beer A, Faulkner D. Housing transitions through the life course: aspirations, needs and policy. Policy Press; 2011. [Google Scholar]
- 35.Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. Journal of family practice. 2000;49:147. [PubMed] [Google Scholar]
- 36.Goldstick JE, Bohnert KM, Davis AK, et al. Dual trajectories of depression/anxiety symptoms and alcohol use, and their implications for violence outcomes among drug-using urban youth. Alcohol and Alcoholism. 2018 doi: 10.1093/alcalc/agy036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goldstick JE, Carter PM, Walton MA, et al. Development of the SaFETy score: a clinical screening tool for predicting future firearm violence risk. Annals of internal medicine. 2017;166:707–14. doi: 10.7326/M16-1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walton MA, Epstein-Ngo Q, Carter PM, et al. Marijuana use trajectories among drug-using youth presenting to an urban emergency department: Violence and social influences. Drug & Alcohol Dependence. 2017;173:117–25. doi: 10.1016/j.drugalcdep.2016.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]