The indications for reverse shoulder arthroplasty have expanded over the last decade and with more numbers now being performed, the number of patients with complications is increasing. Reverse shoulder arthroplasty requires adequate re-tensioning of the deltoid to achieve elevation and implant stability. Instability remains a feared complication, and it is well known that most cases of early instability are attributable to inadequate tissue tension from inaccurate component size or component malposition. Along with adequate deltoid tension, restoring the glenoid offset in reverse shoulder arthroplasty is crucial, albeit an often under-recognised step in achieving a stable construct.
Reverse shoulder arthroplasty (RSA) was originally designed to treat pseudoparalysis with cuff tear arthropathy.1,2 Owing to its success, the indications for RSA have expanded to also include massive rotator cuff tears, acute trauma, trauma sequelae, failed arthroplasty and tumours.3, 4, 5, 6, 7, 8 The UK National Joint Registry (NJR) shows a year-on-year increase in the number of primary RSAs performed with 806 in 2012–3015 in 2016, representing 50.7% of all primary shoulder arthroplasties performed in that year.9 There are currently only four years of outcome data demonstrating a cumulative percentage probability of revision of 3.4%. Elsewhere, the New Zealand Arthroplasty Registry shows a 93% RSA survivorship at 13 years.10
Despite the success of RSA in improving pain and function, complication rates remain high with instability reported to be the commonest complication.6,9,11, 12, 13 In RSA, the tensioned deltoid compensates for a deficient rotator cuff and provides the stable fulcrum for active elevation and prosthetic stability. Failure to adequately tension the deltoid contributes to prosthetic instability.14 In order to achieve the correct deltoid tension both the humeral length and offset should be restored and we present our algorithm for the treatment of prosthetic instability.
Surgery is performed under a general anaesthetic with an interscalene block. The patient is positioned in the beach chair position, prepped and draped, leaving the shoulder exposed. A deltopectoral approach is used and following a subscapularis tenotomy the joint is dislocated to expose the humerus. The humerus is prepared in a standard fashion in line with the operative technique for that implant. The glenoid is then exposed and prepared followed by implantation of definitive components in neutral to restore the joint line, which is aided by a preoperative computer tomography (CT) scan. Attention is then turned to the humerus and a trial reduction performed, as outlined below, before implantation of definitive components in 20° of retroversion. Rehabilitation is supervised by a physiotherapist within a comfortable safe zone, as defined at surgery.
We perform a standardised routine when testing for implant stability. No single test is perfectly accurate and by combining tests even subtle instability can be recognised more readily. Prior to performing these tests we either remove or relax any self retainers, which may introduce a false-negative and instead use a hand-held retractor to visualise the joint. We start by assessing the range of motion and in particular looking for hinged opening of the joint during external rotation. Stability is also tested with the arm in a position of extreme external rotation and abduction, followed by testing in extreme internal rotation and flexion. Further testing includes the ‘shuck test’ involving traction along the longitudinal axis of the humerus to assess for pistoning and checking the resting tension within the conjoint tendon.
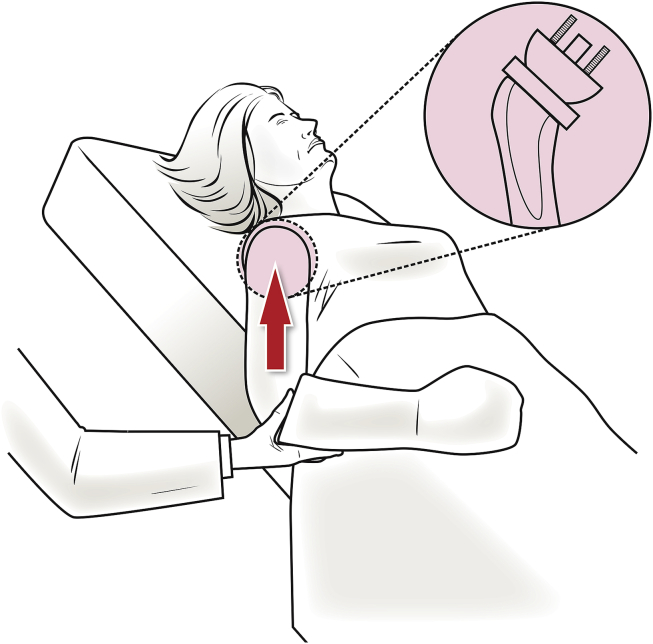
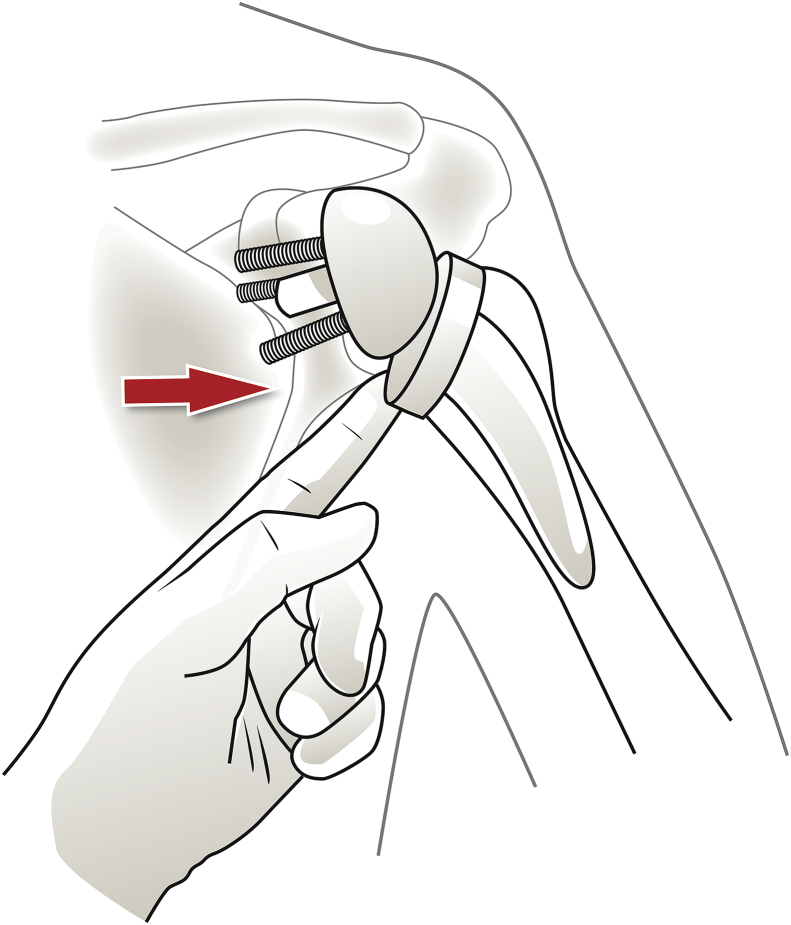
We then proceed to the “Bed Shuffle Test” bringing the shoulder into adduction and extension with the application of a proximally directed force along the humeral shaft to try and dislocate the prosthesis antero-superiorly (Fig. 1). This is an effort to recreate the action when the patient is shuffling themselves up the bed whilst weight bearing via the elbow. We then perform the Lateral Thrust Test with the arm in line with the torso and the shoulder in neutral rotation. The index finger is placed on the medial aspect of the proximal humerus and a force applied laterally to displace the proximal humerus off the glenosphere (Fig. 2). The ability to dislocate the reverse prosthesis using a laterally directed force indicates inadequate mediolateral offset. If any alterations are made to the construct, we simply repeat the full gamut of tests until optimal stability is achieved. This test may alternatively be performed using a Hohmann retractor instead of the surgeon's finger. The aforementioned tests are summarised and demonstrated in Table 1 and Video 1.
Fig. 1.
Bed Shuffle Test (arrow indicates direction of applied force).
Fig. 2.
Lateral Thrust Test (arrow indicates direction of applied force).
Table 1.
Intraoperative stability assessment of Reverse Shoulder Arthroplasty.
| Test | Abnormal finding | Management options |
|---|---|---|
| External Rotation in neutral | Hinged opening | Check posterior bony impingement acting as a hinge |
| Larger glenosphere | ||
| Abduction/External Rotation | Anterior dislocation | Build humeral height |
| Check posterior bony impingement acting as a hinge | ||
| Larger glenosphere | ||
| Adduction/Internal Rotation | Posterior dislocation | Build humeral height |
| Check anterior bony impingement acting as a hinge | ||
| Larger glenosphere | ||
| Conjoint tendon tension | Excessive tension | Reduce humeral height |
| “Shuck test” | Excessive pistoning | Build humeral height |
| Eccentric glenosphere | ||
| “Bed shuffle Test” | Anterosuperior translation | Build glenoid offset |
| Larger glenosphere with or without lateralisation | ||
| Lateralised humeral liner | ||
| “Lateral Thrust Test” | Lateral dislocation | Build glenoid offset |
| Larger glenosphere with or without lateralisation | ||
| Lateralised humeral liner |
Supplementary video related to this article can be found at https://doi.org/10.1016/j.jcot.2018.11.006.
The following is the supplementary data related to this article:
Intraoperative stability assessment of reverse shoulder arthroplasty.
Modern RSA designs and improvements in surgical technique have reduced the rate of complications reported in earlier designs.6,8 Prosthetic instability remains the most common clinically significant complication of RSA and is usually diagnosed within the first postoperative year.8,12,14,15 Ekelund in his series of 1255 primary RSAs reported a dislocation rate of 1.4% with Trappey et al. reporting a rate of 5% in his series of 212 patients.13,16 Furthermore, the incidence of instability is significantly higher at 9.4% in those patients receiving a RSA for a failed primary arthroplasty. Insufficient soft tissue tensioning accounts for most cases of instability with other causes being medialisation of the glenoid component leading to a poor deltoid wrapping angle, poor implant position, impingement and infection.14,16
In order to achieve the correct deltoid tension both the humeral length and offset should be restored.4 For a primary RSA the native joint line should be re-established as guided by a preoperative CT scan, as medialisation can lead to an inadequate deltoid wrap predisposing to lateral instability.17,18 In our experience the lateral thrust test provides feedback for adequate soft tissue tension in the mediolateral plane.
Management of prosthetic instability depends on the causative mechanism which in most cases is inadequate soft tissue tensioning.12,13,17 Closed reduction may be considered during the initial postoperative weeks and there is some evidence supporting the use of an abduction wedge, which promotes deltoid shortening and enhances the implant's coaptation force.12,17,19 Failed closed reduction or chronic cases require revision surgery and a preoperative CT scan is helpful for planning. Boileau et al. found humeral shortening of more than 15mm and humeral axis medialisation of more than 15mm to be significant risk factors for instability and routinely use full-length scaled radiographs of both humeri to plan surgery.12,17 Due to the lack of standardisation we prefer a preoperative CT scan and intraoperative assessment to guide treatment of the unstable RSA.
Insufficient deltoid tension in the vertical plane (humeral shortening) is usually treated with a thicker liner. Rarely, more significant humeral shortening may require the insertion of a larger stem proximally. Insufficient deltoid tension in the horizontal plane due to medialisation of the glenoid is most efficiently treated with a larger glenosphere. Furthermore, such inadequate mediolateral offset may be addressed using the humeral lateralised liner, which is available on most modern modular systems. Building up the glenoid offset using the BIO -RSA technique (Bone Increased Offset) or using metallic augments has the added advantage of reducing the risk of glenoid notching and increased range of movement along with restoring the mediolateral offset. This is indeed the most desirable way of restoring adequate offset when performed pre-emptively, however in a revision situation exchanging the baseplate adds morbidity and time to the surgery.
In our experience the introduction of the lateral thrust and bed shuffle tests have dramatically reduced the incidence of instability of RSA in our practice. They have also been invaluable in the management of revising an unstable RSA. They provide a simple and practical technique for checking whether the cause for prosthetic instability is inadequate longitudinal deltoid tension or inadequate offset.
Declaration of conflicting interest and funding
There is no conflicting interest or external source of funding in preparation of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2018.11.006.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Boileau P., Watkinson D., Hatzidakis A.M., Hovorka I. Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–540. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Grammont P.M., Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 3.Affonso J., Nicholson G.P., Frankle M.A. Complications of the reverse prosthesis: prevention and treatment. Instr Course Lect. 2012;61:157–168. [PubMed] [Google Scholar]
- 4.Boileau P., Watkinson D.J., Hatzidakis A.M., Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14 doi: 10.1016/j.jse.2004.10.006. 147S-61S. [DOI] [PubMed] [Google Scholar]
- 5.Cuff D., Pupello D., Virani N., Levy J., Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am. 2008;90:1244–1251. doi: 10.2106/JBJS.G.00775. [DOI] [PubMed] [Google Scholar]
- 6.Ladermann A., Williams M.D., Melis B., Hoffmeyer P., Walch G. Objective evaluation of lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:588–595. doi: 10.1016/j.jse.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Middernacht B., De Wilde L., Mole D., Favard L., Debeer P. Glenosphere disengagement: a potentially serious default in reverse shoulder surgery. Clin Orthop Relat Res. 2008;466:892–898. doi: 10.1007/s11999-007-0090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wall B., Nove-Josserand L., O'Connor D.P., Edwards T.B., Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 9.2017. National Joint Registry of England, Wales, Northern Ireland and the Isle of Man.http://www.njrreports.org.uk/Portals/0/PDFdownloads/NJR%2014th%20Annual%20Report%202017.pdf 14th Annual Report. (date last accessed 30/12/2017) [Google Scholar]
- 10.2016. The New Zealand Joint Registry.http://nzoa.org.nz/system/files/NZJR%2017%20year%20Report.pdf Seventeen Year Report, January 1999 to December 2015. (date last accessed 30/12/2017) [Google Scholar]
- 11.Bohsali K.I., Bois A.J., Wirth M.A. Complications of shoulder arthroplasty. J Bone Joint Surg [Am] 2017;99(3):256–269. doi: 10.2106/JBJS.16.00935. [DOI] [PubMed] [Google Scholar]
- 12.Boileau P., Melis B., Duperron D., Moineau G., Rumian A.P., Han Y. Revision surgery of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1359–1370. doi: 10.1016/j.jse.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Ekelund A.L. Management of painful reverse shoulder arthroplasty. Shoulder Elbow. 2017;9(3):212–222. doi: 10.1177/1758573217702333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farshad M., Gerber C. Reverse total shoulder arthroplasty from the most to the least common complication. Int Orthop. 2010;34:1075–1082. doi: 10.1007/s00264-010-1125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zumstein M.A., Pinedo M., Old J., Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Trappey G.J., O'Connor D.P., Edwards T.B. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011;469(9):2505–2511. doi: 10.1007/s11999-010-1686-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res. 2016;102(1 Suppl):S33–S43. doi: 10.1016/j.otsr.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 18.Lädermann A., Denard P.J., Boileau P. Effect of humeral stem design on humeral position and range of motion in reverse shoulder arthroplasty. Int Orthop. 2015;39(11):2205–2213. doi: 10.1007/s00264-015-2984-3. [DOI] [PubMed] [Google Scholar]
- 19.Chalmers P.N., Rahman Z., Romeo A.A., Nicholson G.P. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(5):737–744. doi: 10.1016/j.jse.2013.08.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative stability assessment of reverse shoulder arthroplasty.