Abstract
Purpose
The purpose of this study was to evaluate the prognostic effect of patient compliance with supportive periodontal treatment (PC-SPT). Chronic periodontitis patients were classified based on their compliance level, and factors affecting PC-SPT and the prognosis of PC-SPT were investigated.
Methods
This study selected 206 patients who started SPT after receiving periodontal treatment between 2010 and 2012. Patients who continued SPT through February 2016 were included. The patients were classified according to whether they exhibited complete compliance (100% of visits), excellent compliance (≥70% of visits), incomplete compliance (<70% of visits), or non-compliance (only 2 visits). Patient characteristics that could affect PC-SPT, such as age, sex, distance of the clinic from their residence, implantation, and periodontal treatment, were investigated. The number of newly decayed and extracted teeth, alveolar bone level changes around the teeth and implants, and implant removal were examined to evaluate the prognosis of PC-SPT.
Results
Sex and the presence of an implant significantly affected PC-SPT. Additionally, the number of newly decayed and extracted teeth and changes in alveolar bone levels around the teeth and implants were significant prognostic factors related to PC-SPT.
Conclusions
PC-SPT in chronic periodontitis patients will help maintain periodontal health and prevent further periodontal disease.
Keywords: Chronic periodontitis, Patient compliance, Periodontal treatment, Prognosis
Graphical Abstract
INTRODUCTION
Chronic periodontitis is a disease of the oral cavity characterized by inflammation that spreads from the gingiva into the periodontal tissue, resulting in periodontal pocket formation, destruction and absorption of alveolar bone, loss of the attached gingiva, gingival recession, and increased tooth mobility [1]. It is easily neglected in the gingivitis stage or during early periodontitis because very few subjective symptoms are present. Thus, treatment usually begins after progression to a later stage, which is more difficult to cure due to the development of alveolar bone destruction [2]. As with most chronic diseases, such as diabetes and hypertension, constant maintenance and management are required.
Once periodontal treatment is completed, supportive periodontal treatment (SPT) should be continued to maintain the outcomes of treatment and to progressively assess the patient's prognosis. The American Academy of Periodontology has emphasized the importance of SPT, defining it as treatment to prevent or minimize the recurrence and progression of periodontal disease in patients with gingivitis, periodontitis, and peri-implantitis. Furthermore, SPT helps to reduce tooth loss through periodic examinations of natural teeth and periodontal tissues, which help to identify other oral diseases or conditions that may require immediate treatment [3,4].
In a long-term study on SPT, Lang et al. [5] reported that in patients with incipient and moderate periodontitis, 4 years of periodic SPT with regular visits resulted in a well-maintained initial treatment without any further deepening of the periodontal pocket. In addition, in non-smokers, 5 years of SPT after periodontal surgery led to a decrease in the depth of the periodontal pocket and a significant increase in alveolar bone height [6]. Furthermore, only 4% of 572 patients with moderate periodontitis experienced tooth removal during a 4-year SPT period, with an annual mean alveolar bone height increase of 0.02 mm [7]. Therefore, SPT plays a critical role in preventing the development and deterioration of disease, and in maintaining healthy periodontal tissue, regardless of the severity of periodontitis or the applied treatment methods [8].
Patient compliance (PC) is an important factor for SPT to achieve its full effect. In a previous study investigating PC with SPT (PC-SPT) [9], 521 patients were monitored for 14 years. That study showed that PC-SPT was higher in females than in males. In the final year of the study period, only 27.4% of the patients were fully compliant. In addition, significantly higher PC-SPT was observed after non-surgical treatment than after surgical treatment. PC decreased from 13.9% to 9% in the first 6 years of SPT. However, as dentists continued to inform patients of the importance of SPT and the patients continued to attend follow-up appointments, PC-SPT increased to 48.4% over the next 5 years. During the last 5 years of SPT, the average PC-SPT stabilized at 43.2%. This finding indicates that sustained improvements in PC-SPT are attainable in patients as long as its importance is regularly emphasized.
Consistent with these observations, Demirel et al. [10] investigated 462 patients and reported that PC-SPT in female patients was higher than in male patients, and that patients who completely complied with SPT experienced less tooth loss during SPT than non-compliant patients. Novaes et al. [11] also reported that 46% of the 874 patients studied were completely compliant and that the number of non-compliant patients was higher in the age group of 40 years or less.
Based on the various studies mentioned above, it can be concluded that PC-SPT is higher in females aged over 40 years, and that the effects of periodontal treatment could be stably maintained if PC-SPT is increased to near 100%.
A 7-year follow-up study investigating the factors affecting PC-SPT reported that only 42% of patients were completely compliant [12]. However, expansion of dental insurance for surgical and active dental treatment contributed to improvements in PC. Therefore, if the factors affecting PC-SPT can be identified during SPT in patients with chronic periodontitis and the effects of PC-SPT on the overall prognosis of periodontal treatment are analyzed, PC-SPT can be predicted and improved. Doing so would also help to establish a future follow-up plan that can improve the treatment prognosis.
However, studies of PC-SPT in Korean patients are rare. In addition, the majority of studies mainly focused on classifying patients based on previous dental treatments and on conducting comparisons based on clinical indices in periodontal tissues without considering the SPT period [13,14,15]. Additionally, it is important to retrospectively and comprehensively evaluate the effects of patient characteristics on PC-SPT and the treatment prognosis associated with PC-SPT.
Therefore, the purpose of this study was to analyze the effects of PC-SPT in Korean patients. To do so, this study classified patients based on the extent of their compliance with follow-up appointments during the SPT period after chronic periodontitis treatment. Additionally, patient-related factors affecting PC-SPT and the effect of PC-SPT on the prognosis of periodontal treatment were investigated and evaluated. Predicting the patient-related factors with the most significant impact on the prognosis of periodontal treatment will help to promote the successful maintenance of periodontal health.
MATERIALS AND METHODS
Study population
A total of 206 patients from the Department of Periodontology who were treated for chronic periodontitis and started SPT between January 2010 and December 2012 were included in this study. The study period lasted until February 29, 2016, and the following patients were excluded from the study: 1) patients who stopped SPT and restarted periodontal treatment, 2) patients whose clinical and radiographic data were not sufficient, 3) patients who became pregnant, 4) patients with uncontrolled systemic diseases, 5) patients who died or moved to other areas or overseas, 6) patients who were unable to move independently, 7) patients over 80 years old, and 8) patients judged inappropriate for inclusion in the study based on the author's discretion.
In order to objectively standardize the definition of chronic periodontitis, the diagnosis was made by a periodontal specialist with extensive clinical experience. Chronic periodontitis was also diagnosed in patients who had significant bone loss in the interdental space and the tooth root furcation on panoramic radiographs, which were routinely taken in the Department of Periodontology.
The periodontists who performed the previous periodontal treatment and SPT included both professors and residents. Two investigators jointly reviewed patients' clinical and radiographic records. In addition, radiographic measurements were performed using the scale tool of the picture archiving and communication system (GE Healthcare, Seongnam, Korea) and the mean value obtained by 2 investigators was used.
Ethical approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of the School of Medicine, Ewha Womans University (approval No. EUMC 16-04-042). In this retrospective study, consent from the patients was not necessary because no personal information that could identify the patients was used. The Institutional Review Board of the School of Medicine, Ewha Womans University also did not require the submission of patient consent forms. This study only dealt with patients' clinical and radiographic records, which were not considered to contain any sensitive personal information. Therefore, this study complied with the necessary ethical regulations for preparing an article, as confirmed by the ethical review process.
Classification of patients
The clinical and radiographic records of all patients during the study period were examined at least 3 times by the 2 investigators. The visit rate of patients who visited every 3–6 months was converted to a percentage on a 1 year basis, which was used to classify them according to PC-SPT [16]; for instance, the PC-SPT would be 75% for a patient undergoing SPT every 3 months who visited 3 times a year. The duration of SPT in this study varied from 3 to 5 years, so PC-SPT calculations were based on the SPT period for each patient. If a patient changed or canceled the follow-up appointment, the investigators identified the corresponding visit and obtained the relevant data from the patient's clinical records. To confirm changes in the patient's prognosis, patients who visited at least 2 times during the SPT period were evaluated. Patients were classified according to compliance as follows:
• Complete compliance group (CCG): 100% of visits
• Excellent compliance group (ECG): 70%–100% of visits
• Incomplete compliance group (ICG): <70% of visits, but with at least 3 visits during the SPT period
• Non-compliance group (NCG): only 2 visits during the SPT period
Patient characteristics
This study investigated patient characteristics such as age, sex, distance of the clinic from their residence, implantation, and periodontal treatment using patients' clinical and radiographic records. In addition, this study examined how these patient characteristics affected PC-SPT.
Based on the addresses listed in patients' clinical records, areas within 10 km from Ewha Womans University Medical Center (EUMC) were considered short-distance and areas over 10 km from EUMC were considered long-distance [17].
Before SPT was started, patients were grouped on the basis of the periodontal treatments performed. Scaling and root planing (SRP) and flap operation (FO) were defined as periodontitis treatments. Implantation (including bone graft) and mucogingival surgery (e.g., keratinized gingiva widening, root coverage, gingivectomy, and gingivoplasty) were defined as other treatments.
Patients who only received scaling with a healthy periodontal state or mild gingivitis underwent scaling regularly over the course of a year. They were classified separately from the patients who received SRP of periodontitis treatment procedure because their treatment was less intense.
Evaluation of treatment prognosis
Using patients' clinical and radiographic records, the number of newly decayed teeth, alveolar bone level changes around the teeth and implants, the number of newly extracted teeth, and implant removal during SPT were examined. Subsequently, the effect of PC-SPT on the prognosis of periodontal treatment was evaluated.
The changes in alveolar bone levels around all remaining teeth were measured using X-ray views. The lowest margin of restorations or the cementoenamel junction of natural teeth was set as the reference point. The distance from the reference point to the alveolar bone crest was measured on the mesial and distal sides of the tooth, and the mean distance value was used as the change in alveolar bone level for each tooth [6,18]. The measurements before and after SPT were compared and classified as having exhibited a decrease (−), maintenance (0), or an increase (+).
The changes in alveolar bone levels around all remaining implants were also measured using X-ray views. The distance from the top point of the fixture to the alveolar bone crest was measured on the mesial and distal sides of the implant, respectively. The mean value of the distance was used as the change in alveolar bone level for each implant [19,20]. Subsequently, the same classification of groups was used as for the teeth.
Statistical analysis
Statistical analysis was performed using SPSS software (version 20.0, IBM Corp., Armonk, NY, USA). Frequency analysis was used to assess the distribution of the data. The χ2 test was applied to non-continuous variables to compare patient characteristics and to evaluate the treatment prognosis among the patient groups. The cutoff for statistical significance was set at P<0.05.
RESULTS
Analysis of patient characteristics
The study included a total of 206 patients.
The majority of patients (n=162, 78.6%) were in their 30s, 40s, and 50s. When patients in their 40s were used as a fixed basis for comparison, the ratio of younger and older patients was relatively uniform. Males constituted 49.0% and females constituted 51.0% of the study population, while the proportion of patients who lived within 10 km from the hospital was 75.2%. Patients who had implants before SPT initiation accounted for 32.5% of the study population.
Before SPT began, 75.7% of the patients had treatment for periodontitis alone, 14.6% of the patients had regular scaling, 6.3% of the patients had treatment for periodontitis along with treatment for other issues, and 3.4% of the patients had only other treatments. Among the patients who received periodontitis treatment, 50.0% had SRP. Patients who were diagnosed with moderate or advanced periodontitis and underwent FO on 1–2 or more than 3 sextants accounted for 20.4% and 5.3% of the study population, respectively. Other treatments were divided into implantation and mucogingival surgery, and in total, 9.7% of patients received other treatments, including both those who did and did not receive periodontitis treatment (Table 1).
Table 1. Patient characteristics.
| Variable | No. (%) | ||
|---|---|---|---|
| Age (yr) | |||
| <30 | 24 (11.7) | ||
| 30–39 | 47 (22.8) | ||
| 40–49 | 61 (29.6) | ||
| 50–59 | 54 (26.2) | ||
| ≥60 | 20 (9.7) | ||
| Sex | |||
| Male | 101 (49.0) | ||
| Female | 105 (51.0) | ||
| Distance between hospital and residence | |||
| Short (within 10 km) | 155 (75.2) | ||
| Long (more than 10 km) | 51 (24.8) | ||
| Implantation | |||
| Yes | 67 (32.5) | ||
| No | 139 (67.5) | ||
| Periodontal treatment | |||
| Periodontitis treatment | 156 (75.7) | ||
| SRP | 103 (50.0) | ||
| SRP+FO 1–2 | 42 (20.4) | ||
| SRP+FO 3– | 11 (5.3) | ||
| Periodontitis treatment+other treatment | 13 (6.3) | ||
| Periodontitis treatment+implantation | 3 (1.5) | ||
| Periodontitis treatment+MGS | 10 (4.8) | ||
| Other treatment | 7 (3.4) | ||
| Implantation | 5 (2.4) | ||
| MGS | 2 (1.0) | ||
| Scaling only | 30 (14.6) | ||
SRP: scaling and root planning, FO 1–2: flap operation on 1–2 sextants, FO 3–: flap operation on 3 or more sextants, MGS: mucogingival surgery.
Patient groups classified by compliance
When patients were classified based on their compliance with SPT, the ECG was the largest group (36.4%), followed by the ICG (33.0%), the NCG (16.5%), and the CCG (14.1%). That is, the proportions of high PC-SPT (CCG and ECG) and low PC-SPT (ICG and NCG) groups were almost even at 50.5% and 49.5%, respectively (Table 2).
Table 2. Classification of patient groups according to PC-SPT.
| Compliance group | No. (%) |
|---|---|
| CCG | 29 (14.1) |
| ECG | 75 (36.4) |
| ICG | 68 (33.0) |
| NCG | 34 (16.5) |
| Total | 206 (100) |
PC-SPT: patient compliance with supportive periodontal treatment, CCG: complete compliance group, ECG: excellent compliance group, ICG: incomplete compliance group, NCG: non-compliance group.
Treatment prognosis during SPT
The treatment prognosis was evaluated by regular clinical and radiographic examinations during SPT. Overall, 67.5% of the patients showed no newly decayed teeth, but at least 1 decayed tooth was found in 32.5% of the patients. The alveolar bone levels around the teeth were maintained in the majority of patients (55.8%), and decreased in 26.7%. The alveolar bone levels around implants were maintained in 81.1% of patients and decreased in 18.9%, suggesting that the implants were maintained better than teeth. However, no increase in alveolar bone levels around implants was found, unlike in teeth (17.5%). New extraction of teeth and implant removal took place in 23.8% and 3% of patients, respectively. Therefore, the maintenance rate of implants was higher than that of teeth, similar to the changes in alveolar bone levels (Table 3).
Table 3. Treatment prognosis during SPT.
| Variable | No. (%) | |
|---|---|---|
| No. of newly decayed teeth | ||
| 0 | 139 (67.5) | |
| 1 | 32 (15.5) | |
| 2–3 | 24 (11.7) | |
| ≥4 | 11 (5.3) | |
| Alveolar bone level changes around teeth | ||
| Decreased | 55 (26.7) | |
| Maintained | 115 (55.8) | |
| Increased | 36 (17.5) | |
| Alveolar bone level changes around implants | ||
| Decreased | 39 (18.9) | |
| Maintained | 167 (81.1) | |
| Increased | 0 (0.0) | |
| No. of newly extracted teeth | ||
| 0 | 157 (76.2) | |
| 1 | 27 (13.1) | |
| ≥2 | 22 (10.7) | |
| Implant removal | ||
| No | 65 (97.0) | |
| Yes | 2 (3.0) | |
SPT: supportive periodontal treatment.
Analysis of patient characteristics related to patient groups
Next, we examined how patient characteristics affected PC-SPT.
Of patients in their 40s and under, 79.3% were in the CCG. In the other groups, patients in their 30s, 40s, and 50s accounted for the majority (ECG, 80.0%; ICG, 83.8%; and NCG, 76.4%). There was a tendency for age to increase moving from the CCG to the low PC-SPT groups, but no statistically significant difference was found (P=0.100).
In terms of distance of the clinic from patients' residence, in all groups, it was most common for patients to live at a short distance from the clinic (CCG, 79.3%; ECG 72.0%; ICG, 75.0%; and NCG, 79.4%), confirming the hypothesis that patients visit clinics near their residences. The effect on PC-SPT was not statistically significant (P=0.801).
Patients who received treatment for periodontitis alone accounted for more than 70% of all groups (CCG, 79.3%; ECG, 72.0%; ICG, 79.4%; and NCG, 73.5%). Those who underwent SRP only accounted for approximately 50% of all groups (CCG, 51.7%; ECG, 49.3%; ICG, 51.5%; and NCG, 47.1%). Those who only received scaling treatment accounted for more than 10% of all groups (CCG, 13.8%; ECG, 14.7%; ICG, 14.7%; and NCG, 14.7%); in other words, most of the patients received basic periodontal treatment. The periodontal treatment method before SPT had no significant effect on PC-SPT (P=0.883).
Male patients accounted for 62.1% and 57.3% of the CCG and ECG, respectively, and female patients comprised 58.8% and 64.7% of the ICG and NCG, respectively. That is, female sex was associated with lower PC-SPT, and this effect was significant (P=0.040).
In the NCG, 82.4% of patients had no implants, which was the highest proportion of no implantation across all groups. In the ECG, the rate of patients with implants was 48.0%, which was higher than the other PC-SPT groups. High PC-SPT was significantly associated with the presence of an implant (P=0.003) (Table 4).
Table 4. Relationship between patient characteristics and patient groups.
| Variable | CCG (n=29) | ECG (n=75) | ICG (n=68) | NCG (n=34) | P | ||
|---|---|---|---|---|---|---|---|
| Age (yr) | 0.100 | ||||||
| <30 | 8 (27.6) | 6 (8.0) | 6 (8.8) | 4 (11.8) | |||
| 30–39 | 6 (20.7) | 12 (16.0) | 23 (33.8) | 6 (17.6) | |||
| 40–49 | 9 (31.0) | 24 (32.0) | 16 (23.5) | 12 (35.3) | |||
| 50–59 | 4 (13.8) | 24 (32.0) | 18 (26.5) | 8 (23.5) | |||
| ≥60 | 2 (6.9) | 9 (12.0) | 5 (7.4) | 4 (11.8) | |||
| Sex | 0.040a) | ||||||
| Male | 18 (62.1) | 43 (57.3) | 28 (41.2) | 12 (35.3) | |||
| Female | 11 (37.9) | 32 (42.7) | 40 (58.8) | 22 (64.7) | |||
| Distance between hospital and residence | 0.801 | ||||||
| Short (within 10 km) | 23 (79.3) | 54 (72.0) | 51 (75.0) | 27 (79.4) | |||
| Long (more than 10 km) | 6 (20.7) | 21 (28.0) | 17 (25.0) | 7 (20.6) | |||
| Implantation | 0.003a) | ||||||
| No | 23 (79.3) | 39 (52.0) | 49 (72.1) | 28 (82.4) | |||
| Yes | 6 (20.7) | 36 (48.0) | 19 (27.9) | 6 (17.6) | |||
| Periodontal treatment | 0.883 | ||||||
| Periodontitis treatment | 23 (79.3) | 54 (72.0) | 54 (79.4) | 25 (73.5) | |||
| SRP | 15 (51.7) | 37 (49.3) | 35 (51.5) | 16 (47.1) | |||
| SRP+FO 1–2 | 8 (27.6) | 13 (17.3) | 17 (25.0) | 4 (11.8) | |||
| SRP+FO 3– | 0 (0.0) | 4 (5.3) | 2 (2.9) | 5 (14.7) | |||
| Periodontitis treatment+other treatment | 2 (6.9) | 7 (9.3) | 2 (2.9) | 2 (5.9) | |||
| Periodontitis treatment+implantation | 0 (0.0) | 3 (4.0) | 0 (0.0) | 0 (0.0) | |||
| Periodontitis treatment+MGS | 2 (6.9) | 4 (5.3) | 2 (2.9) | 2 (5.9) | |||
| Other treatment | 0 (0.0) | 3 (4.0) | 2 (2.9) | 2 (5.9) | |||
| Implantation | 0 (0.0) | 3 (4.0) | 1 (1.5) | 1 (2.9) | |||
| MGS | 0 (0.0) | 0 (0.0) | 1 (1.5) | 1 (2.9) | |||
| Scaling only | 4 (13.8) | 11 (14.7) | 10 (14.7) | 5 (14.7) | |||
Data are number (%) values except where indicated otherwise.
CCG: complete compliance group, ECG: excellent compliance group, ICG: incomplete compliance group, NCG: non-compliance group, SRP: scaling and root planning, FO 1–2: flap operation on 1–2 sextants; FO 3–: flap operation on 3 or more sextants, MGS: mucogingival surgery.
a)Statistically significant difference (P<0.05).
Evaluation of treatment prognosis according to patient group
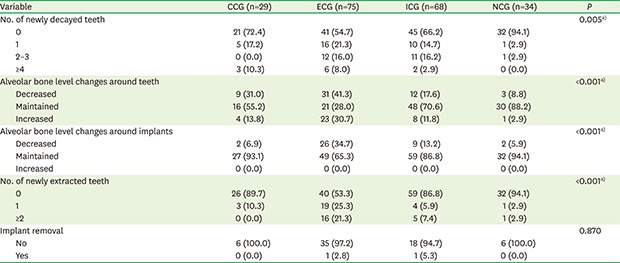
During the SPT period, the treatment prognosis was examined in each PC-SPT group.
In the NCG, 94.1% of patients had 0 newly decayed teeth, which was the highest proportion in any of the groups, and no patients had 4 or more newly decayed teeth. The CCG showed the highest proportion (10.3%) of patients with 4 and more newly decayed teeth, and the total proportion of newly decayed teeth was highest in the ECG (45.3%) (P=0.005).
Changes in alveolar bone levels around teeth were compared across the PC-SPT groups. Maintenance was less common in the high PC-SPT groups (CCG [55.2%] and ECG [28.0%]) than in the low PC-SPT groups (ICG [70.6%] and NCG [88.2%]). Decreased alveolar bone levels were more common in the high PC-SPT groups (CCG [31.0%] and ECG [41.3%]) than in the low PC-SPT groups (ICG [17.6%] and NCG [8.8%]). Increased alveolar bone levels were also more common in the high PC-SPT groups (CCG [13.8%] and ECG [30.7%]) than in the low PC-SPT groups (ICG [11.8%] and NCG [2.9%]). Unstable outcomes (i.e., either a decrease or increase) were more common in the high PC-SPT groups, and the highest proportions of both decreased and increased alveolar bone levels were found in the ECG (P=0.000).
In terms of changes in alveolar bone levels around implants, maintenance was most common in the NCG and CCG (94.1% and 93.1%, respectively). In addition, as with changes in alveolar bone levels around teeth, decreased alveolar bone levels were most common in the ECG (34.7%). However, unlike around teeth, in no cases did the alveolar bone level around the implants increase (P=0.000).
The NCG group had the highest proportion of patients with 0 newly extracted teeth (94.1%). The proportions of newly extracted teeth and 2 or more newly extracted teeth were highest in the ECG (46.6% and 21.3%, respectively). In the CCG, 89.7% of patients had 0 newly extracted teeth, which was a lower proportion than that observed in the NCG, but no patients in the CCG had 2 or more newly extracted teeth (P=0.000).
Implants were maintained in over 90% of patients in all groups, although 1 implant was removed in the ECG (2.8%) and in the ICG (5.3%) (P=0.870).
In the evaluation of treatment prognosis according to the PC-SPT groups, all categories except for the removal of implants showed statistically significant differences (Table 5).
Table 5. Relationships between patient group and treatment prognosis.
| Variable | CCG (n=29) | ECG (n=75) | ICG (n=68) | NCG (n=34) | P | |
|---|---|---|---|---|---|---|
| No. of newly decayed teeth | 0.005a) | |||||
| 0 | 21 (72.4) | 41 (54.7) | 45 (66.2) | 32 (94.1) | ||
| 1 | 5 (17.2) | 16 (21.3) | 10 (14.7) | 1 (2.9) | ||
| 2–3 | 0 (0.0) | 12 (16.0) | 11 (16.2) | 1 (2.9) | ||
| ≥4 | 3 (10.3) | 6 (8.0) | 2 (2.9) | 0 (0.0) | ||
| Alveolar bone level changes around teeth | <0.001a) | |||||
| Decreased | 9 (31.0) | 31 (41.3) | 12 (17.6) | 3 (8.8) | ||
| Maintained | 16 (55.2) | 21 (28.0) | 48 (70.6) | 30 (88.2) | ||
| Increased | 4 (13.8) | 23 (30.7) | 8 (11.8) | 1 (2.9) | ||
| Alveolar bone level changes around implants | <0.001a) | |||||
| Decreased | 2 (6.9) | 26 (34.7) | 9 (13.2) | 2 (5.9) | ||
| Maintained | 27 (93.1) | 49 (65.3) | 59 (86.8) | 32 (94.1) | ||
| Increased | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| No. of newly extracted teeth | <0.001a) | |||||
| 0 | 26 (89.7) | 40 (53.3) | 59 (86.8) | 32 (94.1) | ||
| 1 | 3 (10.3) | 19 (25.3) | 4 (5.9) | 1 (2.9) | ||
| ≥2 | 0 (0.0) | 16 (21.3) | 5 (7.4) | 1 (2.9) | ||
| Implant removal | 0.870 | |||||
| No | 6 (100.0) | 35 (97.2) | 18 (94.7) | 6 (100.0) | ||
| Yes | 0 (0.0) | 1 (2.8) | 1 (5.3) | 0 (0.0) | ||
Data are number (%) values except where indicated otherwise.
CCG: complete compliance group, ECG: excellent compliance group, ICG: incomplete compliance group, NCG: non-compliance group.
a)Statistically significant difference (P<0.05).
DISCUSSION
Chronic periodontitis is a slowly progressing disease that is affected by a patient's lifestyle, systemic condition, and external environmental factors [21,22]. This disease usually becomes evident in adults in their 30s or later due to its slow progressive nature, but it may also develop in adolescents with chronic dental plaque and calculus depositions due to lack of capability or awareness of the need for oral hygiene management [1]. SPT, which is performed after completion of periodontal treatment with the diagnosis of chronic periodontitis, has been reported to be an essential process for maintaining the outcome of periodontal treatment and ensuring the stability of treatment outcomes through additional evaluations [23,24]. In other words, regular long-term visits and check-ups, with continuous education and guidance from dentists, are the most effective strategy for preventing the recurrence of chronic periodontitis and minimizing the loss of teeth and periodontal tissues [23,24]. Therefore, for SPT to be effective, patients need to recognize the importance of maintaining periodontal health through continuous and regular visits to the dental clinic [25].
Therefore, PC-SPT, as investigated in this study, is a clinically effective index for determining the prognosis of periodontal treatment.
The patient education and guidance regarding SPT in this study can be assumed to have been thorough, as confirmed by clinical records. The CCG, which comprised patients with a 100% visit rate, was the smallest (n=29, 14.1%) of all the PC-SPT groups. However, in the study population, 65.5% of the patients were in their 40s or older, 90.3% received treatment for periodontitis and scaling only, and 67.5% did not have any expensive treatments such as implants. In addition, the large-scale outbreak of Middle East respiratory syndrome in 2015 in Korea dramatically reduced the frequency with which patients made medical visits. Thus, a visit rate of 100% was difficult to achieve, and the selection of this study population was appropriate because it reflected actual clinical circumstances [9].
The results of this study suggest that sex and the presence of an implant significantly affected PC-SPT.
Mendoza et al. [12] and Novaes et al. [26] reported that sex did not affect PC with follow-up appointments, but Demirel et al. [10] reported that female patients had a higher compliance rate and a higher tendency to re-visit. One reason for this could be that fewer women than men are active in the workforce, and women are therefore likely to have more spare time. In this study, the ratio of male and female patients was evenly distributed (49.0% and 51.0%, respectively), and men accounted for 62.1% and 57.3% of the CCG and the ECG, respectively. Combined, male patients constituted 60.4% of the high PC-SPT groups (the CCG and ECG), whereas female patients accounted for 58.8% and 64.7% of the ICG and the NCG, respectively, and 59.0% of both low PC-SPT groups (ICG and NCG). This finding is not in accordance with the results of previous studies, and this discrepancy may be because males engage in more social activities and interpersonal relationships than females, and are therefore more cognizant of the importance and necessity of dental treatment [27,28]. In addition, in the 2007 study of Heft et al. [29], women experienced more fear and pain associated with dental treatments than men. Greater fear may also be cause lower PC-SPT.
Cardaropoli et al. [30] reported that patients with at least 1 implant showed higher compliance than those without implants. This may be due to the pain of tooth loss, the time required for dental treatment, and the financial burden involved. These patients therefore realize the importance of regular dental examinations, leading to a higher compliance rate. In this study, 32.5% of the patients had at least 1 implant, and 62.7% of the patients who had an implant were in the high PC-SPT groups. These results are also validated by previous studies [16,31,32]. In addition, 55.4% of patients without any implants were in the ICG and the NCG. The observation that 82.4% of the patients in the NCG had no implants suggests a significant relationship between the presence of an implant and PC-SPT. Patients with implants usually undergo periodontal surgery and prosthodontics, and thus have more opportunities to visit different dental departments. This is related to higher PC-SPT.
In this study, approximately 80% of the patients in the CCG were under 50 years of age, implying that younger patients perceived SPT as more important. Regardless of PC-SPT, patients tend to prefer hospitals close to their homes. However, patient characteristics such as age and distance of the clinic from their residence showed tendencies that were not statistically significant. Many previous studies have reported conflicting results regarding the effect of age on PC [9,11,17,33]. Since most of the patients received only basic periodontitis treatment, it was not possible to conduct a meaningful analysis of PC-SPT according to the periodontal treatment method. Matthews et al. [34] reported that patients who underwent surgical periodontitis treatment had a higher rate of re-visits. However, in this study, nonsurgical periodontitis treatment accounted for more than 50% of the patients, and no statistical significance was found.
The effect of PC-SPT on treatment prognosis was evaluated by studying its relationship with the number of newly decayed and extracted teeth and the direction of alveolar bone change around teeth and implants.
The number of newly decayed teeth does not have a direct relationship to the periodontal treatment received prior to SPT. However, it was included in this study in order to confirm the effect of SPT as a method intended to prevent tooth caries through regular check-ups. In the NCG, 94.1% of the patients did not have newly decayed teeth. This result can be interpreted as indicating that these patients did not visit regularly during SPT, and thus newly decayed teeth were not found at all. This prediction can be made on the basis of the finding that newly decayed teeth were found at the highest rate (45.3%) in the ECG, which contained patients with a visit rate of more than 70% during SPT.
Maintenance of the alveolar bone level around teeth was higher in the low PC-SPT groups (ICG [70.6%] and NCG [88.2%]) than in the high PC-SPT groups (CCG [55.2%] and ECG [28.0%]). This is an unexpected result. However, based on the finding that 75.0% of the patients in whom the alveolar bone level increased were in the high PC-SPT groups, it can be inferred that continuous and regular SPT after periodontal treatment improves patients' ability to manage their oral hygiene, leading to regeneration of periodontal tissue. Kocher et al. [7] also reported that the mean alveolar bone height increased by 0.02 mm annually after SPT. The periodontists who treated patients in the high PC-SPT groups who experienced decreased alveolar bone levels included relatively less skilled residents; thus, it can be assumed that an iatrogenic decrease in the clinical attachment level might occur during the course of periodontal treatment. Regarding the relatively low frequency of decreased alveolar bone levels in the low PC-SPT groups, the low compliance of these groups may be relevant; as such, re-evaluation at recall check-ups is essential.
Increased alveolar bone levels around implants were not found in any of the PC-SPT groups, in contrast to the changes around teeth; this discrepancy most likely occurred because implants do not have the periodontal ligament, which plays an important role in the regeneration of periodontal tissue [35]. Relatively few of the patients who experienced maintenance of alveolar bone levels around implants were in the high PC-SPT groups (45.5%), whereas relatively many of those who experienced decreased alveolar bone levels were in those groups (71.8%). This means that the skills and experience of the periodontist should be confirmed in the high PC-SPT groups. Moreover, at the beginning of SPT, it is necessary to evaluate the overall condition of periodontal tissue, as well as the patient's oral hygiene management in daily life, dietary factors, smoking, and systemic disease [31]. Decreased alveolar bone levels around teeth and implants were most common in the ECG, which had a PC-SPT of over 70%; therefore, it is necessary to further investigate the abovementioned patient factors.
In a previous study of tooth loss during SPT, it was reported that patients with lower compliance had 5.6 times more tooth loss than those with higher PC-SPT [36], and a significantly lower rate of tooth loss occurred in patients with higher compliance [37,38]. In contrast, in this study, the NCG group had the greatest proportion of patients with 0 newly extracted teeth (94.1%), and the highest percentage of patients with newly extracted teeth was found in the ECG (46.6%). This can be interpreted in the same way as the number of newly decayed teeth. Patients in the NCG made very few visits, so it can be considered that teeth requiring extraction were not identified or treated. In addition, Tonetti et al. [39] and Cattabriga et al. [40] reported that tooth loss could occur due to other oral problems even if PC-SPT is excellent. This limitation highlights the fact that the cause of tooth loss cannot be deduced by simply evaluating PC. In fact, a patient who belonged to the ECG in this study underwent tooth extraction due to a tooth fracture, which bore no relationship to periodontitis.
Implant removal can occur due to mechanical complications (e.g., implant component fracture), which is not related to PC-SPT at all. This result was not statistically significant in this study, and a limitation of this study is that it did not investigate such problems.
In conclusion, PC-SPT is evaluated based on PC with planned re-visit appointments; as such, it is affected by many variables, and has been evaluated differently in different studies [16]. In this retrospective study, sex and the presence of an implant had a significant effect on PC-SPT. In addition, the number of newly decayed and extracted teeth and alveolar bone level changes around teeth and implants were found to be important factors in determining how PC-SPT affected the treatment prognosis.
Regarding the impact of periodontal treatment on the prognosis associated with PC-SPT, more significant results would have been obtained if more patients who underwent surgical periodontal treatment had been included.
This study had a relatively short follow-up period of 3–5 years, and its limitations include the need for a more extensive and detailed analysis of patient factors such as smoking, alcohol consumption, malocclusion, bite force, and economic status. Therefore, further research will require a longer-term analysis of PC-SPT. However, this study is clinically relevant as there is a lack of data from follow-up studies regarding PC-SPT in patients with chronic periodontitis in the Korean population. A future study with sufficient collection of data on patient characteristics affecting PC-SPT and a long-term evaluation of the treatment prognosis should be conducted to establish a foundation that can be used in periodontal treatment planning.
ACKNOWLEDGEMENTS
We certify that this study was an academic study conducted in our department and that all information in this study has been fully acknowledged.
Footnotes
Funding: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant No. 2018R1D1A1B07041400) and Research Activation Project for the Interdisciplinary Creative Topic funded by the Ewha Womans University (Grant No. 1-2018-000-001-1).
- Conceptualization: Eun-Kyoung Pang.
- Data curation: Jong-Bin Lee, Hye-Jung Shin, Dae-Yeob Kim, Eun-Kyoung Pang.
- Formal analysis: Jong-Bin Lee, Hye-Jung Shin, Dae-Yeob Kim, Eun-Kyoung Pang.
- Funding acquisition: Jong-Bin Lee.
- Investigation: Jong-Bin Lee, Hye-Jung Shin, Dae-Yeob Kim, Eun-Kyoung Pang.
- Methodology: Jong-Bin Lee, Hye-Jung Shin, Dae-Yeob Kim, Eun-Kyoung Pang.
- Project administration: Eun-Kyoung Pang.
- Resources: Hye-Jung Shin, Dae-Yeob Kim.
- Software: Hye-Jung Shin, Dae-Yeob Kim.
- Supervision: Jong-Bin Lee, Eun-Kyoung Pang.
- Validation: Jong-Bin Lee, Eun-Kyoung Pang.
- Visualization: Jong-Bin Lee, Eun-Kyoung Pang.
- Writing - original draft: Jong-Bin Lee, Hye-Jung Shin, Dae-Yeob Kim.
- Writing - review & editing: Jong-Bin Lee, Eun-Kyoung Pang.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza's clinical periodontology. 11th ed. St. Louis (MO): Elsevier/Saunders; 2012. [Google Scholar]
- 2.Gaurilcikaite E, Renton T, Grant AD. The paradox of painless periodontal disease. Oral Dis. 2017;23:451–463. doi: 10.1111/odi.12537. [DOI] [PubMed] [Google Scholar]
- 3.Renvert S, Persson GR. Supportive periodontal therapy. Periodontol 2000. 2004;36:179–195. doi: 10.1111/j.1600-0757.2004.03680.x. [DOI] [PubMed] [Google Scholar]
- 4.Agrawal N, Jain R, Jain M, Agarwal K, Dubey A. Compliance with supportive periodontal therapy among patients with aggressive and chronic periodontitis. J Oral Sci. 2015;57:249–254. doi: 10.2334/josnusd.57.249. [DOI] [PubMed] [Google Scholar]
- 5.Lang NP, Tonetti MS, Suter J, Sorrell J, Duff GW, Kornman KS. Effect of interleukin-1 gene polymorphisms on gingival inflammation assessed by bleeding on probing in a periodontal maintenance population. J Periodontal Res. 2000;35:102–107. doi: 10.1034/j.1600-0765.2000.035002102.x. [DOI] [PubMed] [Google Scholar]
- 6.Boström L, Linder LE, Bergström J. Influence of smoking on the outcome of periodontal surgery. A 5-year follow-up. J Clin Periodontol. 1998;25:194–201. doi: 10.1111/j.1600-051x.1998.tb02428.x. [DOI] [PubMed] [Google Scholar]
- 7.Kocher T, König J, Dzierzon U, Sawaf H, Plagmann HC. Disease progression in periodontally treated and untreated patients--a retrospective study. J Clin Periodontol. 2000;27:866–872. doi: 10.1034/j.1600-051x.2000.027011866.x. [DOI] [PubMed] [Google Scholar]
- 8.Lee HW, Park JW, Suh JY, Lee JM. Patient compliance with supportive periodontal therapy. J Korean Acad Periodontol. 2009;39:193–198. [Google Scholar]
- 9.Demetriou N, Tsami-Pandi A, Parashis A. Compliance with supportive periodontal treatment in private periodontal practice. A 14-year retrospective study. J Periodontol. 1995;66:145–149. doi: 10.1902/jop.1995.66.2.145. [DOI] [PubMed] [Google Scholar]
- 10.Demirel K, Efeodlu A. Retrospective evaluation of patient compliance with supportive periodontal treatment. J Nihon Univ Sch Dent. 1995;37:131–137. doi: 10.2334/josnusd1959.37.131. [DOI] [PubMed] [Google Scholar]
- 11.Novaes AB, Jr, Novaes AB. Compliance with supportive periodontal therapy. Part 1. Risk of non-compliance in the first 5-year period. J Periodontol. 1999;70:679–682. doi: 10.1902/jop.1999.70.6.679. [DOI] [PubMed] [Google Scholar]
- 12.Mendoza AR, Newcomb GM, Nixon KC. Compliance with supportive periodontal therapy. J Periodontol. 1991;62:731–736. doi: 10.1902/jop.1991.62.12.731. [DOI] [PubMed] [Google Scholar]
- 13.Kim YI, Heo HY. A analysis on the patient's awareness of periodontal diseases. J Korean Acad Dent Hyg Educ. 2008;8:107–114. [Google Scholar]
- 14.Lee YS, Yun CY, Kim SM, Kim BO, Han KY. Investigation of age and treatment modalities in the periodontally treated(1981–1995) patients. J Korean Acad Periodontol. 2001;31:225–231. [Google Scholar]
- 15.Kim JH, Chung HJ. The comparison of c linical changes during maintenance phase after non-surgical or surgical therapy of chronic periodontitis. J Korean Acad Periodontol. 2006;36:69–84. [Google Scholar]
- 16.Park WK, Lee JK, Chang BS, Um HS. A retrospective study on patients' compliance with supportive periodontal therapy. J Korean Acad Periodontol. 2009;39:59–70. [Google Scholar]
- 17.Ojima M, Hanioka T, Shizukuishi S. Survival analysis for degree of compliance with supportive periodontal therapy. J Clin Periodontol. 2001;28:1091–1095. doi: 10.1034/j.1600-051x.2001.281202.x. [DOI] [PubMed] [Google Scholar]
- 18.Hausmann E, Allen K, Carpio L, Christersson LA, Clerehugh V. Computerized methodology for detection of alveolar crestal bone loss from serial intraoral radiographs. J Periodontol. 1992;63:657–662. doi: 10.1902/jop.1992.63.8.657. [DOI] [PubMed] [Google Scholar]
- 19.Serino G, Turri A. Outcome of surgical treatment of peri-implantitis: results from a 2-year prospective clinical study in humans. Clin Oral Implants Res. 2011;22:1214–1220. doi: 10.1111/j.1600-0501.2010.02098.x. [DOI] [PubMed] [Google Scholar]
- 20.Heitz-Mayfield LJ, Salvi GE, Mombelli A, Loup PJ, Heitz F, Kruger E, et al. Supportive peri-implant therapy following anti-infective surgical peri-implantitis treatment: 5-year survival and success. Clin Oral Implants Res. 2018;29:1–6. doi: 10.1111/clr.12910. [DOI] [PubMed] [Google Scholar]
- 21.Page RC, Schroeder HE. Pathogenesis of inflammatory periodontal disease. A summary of current work. Lab Invest. 1976;34:235–249. [PubMed] [Google Scholar]
- 22.Page RC, Kornman KS. The pathogenesis of human periodontitis: an introduction. Periodontol 2000. 1997;14:9–11. doi: 10.1111/j.1600-0757.1997.tb00189.x. [DOI] [PubMed] [Google Scholar]
- 23.Ramfjord SP, Morrison EC, Burgett FG, Nissle RR, Shick RA, Zann GJ, et al. Oral hygiene and maintenance of periodontal support. J Periodontol. 1982;53:26–30. doi: 10.1902/jop.1982.53.1.26. [DOI] [PubMed] [Google Scholar]
- 24.Knowles JW. Oral hygiene related to long-term effects of periodontal therapy. J Mich Dent Assoc. 1973;55:147–150. [PubMed] [Google Scholar]
- 25.Lindhe J, Lang NP, Berglundh T, Giannobile WV, Sanz M. Clinical periodontology and implant dentistry. 6th ed. Chichester: John Wiley and Sons, Inc.; 2015. [Google Scholar]
- 26.Novaes AB, Jr, de Lima FR, Novaes AB. Compliance with supportive periodontal therapy and its relation to the bleeding index. J Periodontol. 1996;67:976–980. doi: 10.1902/jop.1996.67.10.976. [DOI] [PubMed] [Google Scholar]
- 27.Kang H, Yoon Y, Park J, Sung M, Bae G, Kim J. Awareness of patients with periodontal disease under treatments at initial and maintenance phase. J Korean Acad Oral Health. 2005;29:271–280. [Google Scholar]
- 28.Perrell-Jones C, Ireland RS. What factors influence patient compliance with supportive periodontal therapy in a general practice setting? Br Dent J. 2016;221:701–704. doi: 10.1038/sj.bdj.2016.904. [DOI] [PubMed] [Google Scholar]
- 29.Heft MW, Meng X, Bradley MM, Lang PJ. Gender differences in reported dental fear and fear of dental pain. Community Dent Oral Epidemiol. 2007;35:421–428. doi: 10.1111/j.1600-0528.2006.00344.x. [DOI] [PubMed] [Google Scholar]
- 30.Cardaropoli D, Gaveglio L. Supportive periodontal therapy and dental implants: an analysis of patients' compliance. Clin Oral Implants Res. 2012;23:1385–1388. doi: 10.1111/j.1600-0501.2011.02316.x. [DOI] [PubMed] [Google Scholar]
- 31.Wilson TG, Jr, Glover ME, Schoen J, Baus C, Jacobs T. Compliance with maintenance therapy in a private periodontal practice. J Periodontol. 1984;55:468–473. doi: 10.1902/jop.1984.55.8.468. [DOI] [PubMed] [Google Scholar]
- 32.Frisch E, Ziebolz D, Vach K, Ratka-Krüger P. Supportive post-implant therapy: patient compliance rates and impacting factors: 3-year follow-up. J Clin Periodontol. 2014;41:1007–1014. doi: 10.1111/jcpe.12298. [DOI] [PubMed] [Google Scholar]
- 33.Novaes AB, Novaes AB, Jr, Moraes N, Campos GM, Grisi MF. Compliance with supportive periodontal therapy. J Periodontol. 1996;67:213–216. doi: 10.1902/jop.1996.67.3.213. [DOI] [PubMed] [Google Scholar]
- 34.Matthews DC, Smith CG, Hanscom SL. Tooth loss in periodontal patients. J Can Dent Assoc. 2001;67:207–210. [PubMed] [Google Scholar]
- 35.Sbordone L, Bortolaia C. Oral microbial biofilms and plaque-related diseases: microbial communities and their role in the shift from oral health to disease. Clin Oral Investig. 2003;7:181–188. doi: 10.1007/s00784-003-0236-1. [DOI] [PubMed] [Google Scholar]
- 36.Checchi L, Montevecchi M, Gatto MR, Trombelli L. Retrospective study of tooth loss in 92 treated periodontal patients. J Clin Periodontol. 2002;29:651–656. doi: 10.1034/j.1600-051x.2002.290710.x. [DOI] [PubMed] [Google Scholar]
- 37.Kim SY, Lee JK, Chang BS, Um HS. Effect of supportive periodontal therapy on the prevention of tooth loss in Korean adults. J Periodontal Implant Sci. 2014;44:65–70. doi: 10.5051/jpis.2014.44.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee CT, Huang HY, Sun TC, Karimbux N. Impact of patient compliance on tooth loss during supportive periodontal therapy: a systematic review and meta-analysis. J Dent Res. 2015;94:777–786. doi: 10.1177/0022034515578910. [DOI] [PubMed] [Google Scholar]
- 39.Tonetti MS, Steffen P, Muller-Campanile V, Suvan J, Lang NP. Initial extractions and tooth loss during supportive care in a periodontal population seeking comprehensive care. J Clin Periodontol. 2000;27:824–831. doi: 10.1034/j.1600-051x.2000.027011824.x. [DOI] [PubMed] [Google Scholar]
- 40.Cattabriga M, Rotundo R, Muzzi L, Nieri M, Verrocchi G, Cairo F, et al. Retrospective evaluation of the influence of the interleukin-1 genotype on radiographic bone levels in treated periodontal patients over 10 years. J Periodontol. 2001;72:767–773. doi: 10.1902/jop.2001.72.6.767. [DOI] [PubMed] [Google Scholar]


