Abstract
Background and Purpose
We aimed to elucidate independent predictors of adverse outcomes in caregivers of patients with dementia using readily available clinical and demographic data of patients with dementia and their caregivers.
Methods
We reviewed patient-caregiver data from the Clinical Research Center for Dementia of South Korea and Caregivers of Alzheimer Disease Research study. The clinical factors of the patients and the demographics of both patients and caregivers were used to predict adverse outcomes for caregivers. Correlation and linear regression analyses were performed.
Results
We enrolled 454 patients and their caregivers for the present study. The general burden for the caregiver was higher amongst female caregivers, patients with further decreased the level of activities of daily living (ADL), patients with more abnormal behavior, or younger patients. The time spent by the caregivers was more in cases of patients with higher Caregiver Administered Neuropsychiatric Inventory scores, younger patients and for patients with decreased level of ADL. Depression amongst caregivers was more prominent in patients with higher Clinical Dementia Rating Sum of Boxes scores. Physical health-related quality of life (HRQoL) was lower in female caregivers, more physically affected patients, and older caregivers. Lastly, mental HRQoL was lower in younger, more physically affected, and in patients with abnormal behaviors.
Conclusions
Clinical and demographic characteristics of patients and caregivers predict adverse outcomes for caregivers. Therefore, these factors should be considered to provide support to both patients and their caregivers.
Keywords: Dementia, Caregivers, Burden
INTRODUCTION
Patients with dementia experience a gradual and progressive cognitive, functional, and behavioral decline, which may lead to a significant need for support from family caregivers. In our aging society, there is an increasing prevalence of dementia and a corresponding increase in the number of caregivers and social burden of caring. Although sometimes rewarding, caring for patients with dementia is usually very stressful, and caregivers experience high levels of physical and psychological morbidity.1,2,3 As the disease progresses, caregivers often have to manage the increasing complexity of multiple care challenges, which can affect their own well-being.4 Therefore, it is necessary to consider problems experienced by the caregivers who act as primary carers for patients with dementia.
Numerous studies have focused on adverse outcomes and their predictors in caregivers for patients with dementia. One of the most studied adverse outcomes is the caregiver burden, which is usually evaluated with structured questionnaires such as the Zarit Burden Interview (ZBI).1 Other adverse outcomes, such as decreased mental and physical health-related quality of life (HRQoL), increased time spent in caring, and depressive mood may also result from caregiving.5,6,7 Regarding the predictors of adverse outcomes, factors associated with patients and their caregivers should be considered comprehensively. Specific symptoms of dementia have been frequently highlighted as causes of adverse outcomes of caregiving, including severity of cognitive dysfunction, neuropsychiatric presentation, and decreased ability to perform daily activities.6,8,9,10 Furthermore, factors associated with caregivers including age, sex, personality, religiosity, depression, and physical conditions may also play a role in causing adverse outcomes of caregiving.11,12,13 However, in clinical settings, it is difficult to consider the caregiver's characteristics except for basic demographics such as age and sex. Therefore, for physicians, it seems to be useful to develop simplified models to predict various adverse outcomes of caregiving using readily available data such as the patient's clinical characteristics, and caregiver's age and sex.
In the present study, we investigated the patient's and caregiver's factors associated with adverse outcomes in caregivers of patients with dementia. The outcomes considered included the burden on caregiver, mental and physical quality of life, time spent in caring, and depression. We aimed to elucidate independent predictors for each adverse outcome.
METHODS
Participants
We reviewed data from the Caregivers of Alzheimer Disease Research (CARE) study. The CARE study was a sub-study of the Clinical Research Center for Dementia of South Korea study, a nationwide multicenter cohort study conducted at university-affiliated hospitals.13,14 The CARE survey was conducted in 2012 during visits to caregivers of patients from 12 participating centers in South Korea. Participants were 476 primary caregivers of patients living at home who had been diagnosed with Alzheimer's disease or subcortical vascular dementia. We excluded patients who had been inpatients or who lived in a residential care home.
The primary caregiver was defined as the patient's family member who spent most of the time in taking care of the patient. These caregivers were interviewed by trained nurses or surveyors and completed self-report questionnaires in the outpatient clinic or their caregiver's home. Twenty-two cases were excluded due to incomplete data. Apparently, data from 454 patients and their primary caregivers were included in the statistical analyses. Written informed consent was obtained from all the participants, and ethical approval was obtained from the Institutional Review Boards at each participating hospital (AJIRB-MED-SUR-12-046).
Assessments of patients with dementia
Patient factors associated with adverse outcomes for caregivers included cognitive function, the severity of dementia, daily living performance, and neuropsychiatric symptoms. Cognitive dysfunction was evaluated with the Korean version of the Mini-Mental State Examination (K-MMSE),15 while the severity of dementia was evaluated with the Clinical Dementia Rating Sum of Boxes (CDR-SB).16 The patient's ability to perform daily activities was evaluated with the Seoul Instrumental Activities of Daily Living (S-IADL) and Barthel Activity of Daily Living (BADL) scales.17 S-IADL can determine the performance of instrumental daily activities, which refers to daily activities necessary to maintain a social life. It is evaluated by interviewing a caregiver about the patient's condition during the past month. BADL is an indicator of basic daily activities and shows the level of ability to perform physical self-management activities needed to care for and maintain the body, such as eating meals, walking, bathing, and using the toilet. Neuropsychiatric features of patients were evaluated with the Caregiver Administered Neuropsychiatric Inventory (CGA-NPI).18 The CGA-NPI is based on the following 12 abnormal behavioral symptoms commonly observed in patients with dementia: delusions, hallucinations, agitation, aggression, depression, discouragement, anxiety, indifference, disinhibition, abnormal movement, sleep, nighttime behavior, and changes in appetite or eating habits.
Assessments of caregivers
Adverse outcomes for caregivers were assessed with the ZBI, Korean version of the Caregiver Activity Survey (CAS-K), Beck Depression Inventory (BDI), and Korean version of the Short Form Health Survey (SF-36) for both physical and mental HRQoL. The ZBI was designed to assess caregivers' psychological health, finances, emotional wellbeing, social and family life, and degree of control over their life. It consists of 22 items, each scored from 0 to 4, with a total score ranging from 0 to 88.19 The CAS-K examines the time spent by the caregivers in supporting the patient during the previous 24 hours from the time of the test.20 As much as possible, information was collected on weekdays, and the time spent on each item was recorded in hours and minutes for 6 items related to daily life support and behavior management of patients with dementia. The 6 items were: communicating with the person, using transportation, dressing, eating, looking after one's appearance, and supervising the person. The BDI is a reliable, accurate, and easy-to-use depression screening tool that can diagnose latent depression at an earlier stage.21 In the SF-36, the Physical Component Summary (PCS) and Mental Component Summary (MCS) are related to the caregiver's HRQoL and are the summarized indicators of physical and mental factors, which are calculated using the SF-36 health survey measuring HRQoL with a questionnaire consisting of 36 items.22
Statistical analysis
Demographics and general characteristics of caregivers and patients were analyzed with descriptive statistics. Pearson's correlation analysis was performed to examine relationships between the characteristics of the patient and caregiver. Multivariate linear regression analyses were performed to identify independent predictors associated with adverse outcomes for caregivers using stepwise backward variable selection. The age and sex of the patients and caregivers, and patient factors (K-MMSE, CDR-SB, S-IADL, BADL, and CGA-NPI) were included as predictors and caregiver factors (ZBI, CAS-K, BDI, and physical and mental HRQoL) were included as dependent variables. Statistical significance was inferred at p<0.05. All statistical analyses were performed using commercial software (SPSS 18.0; SPSS Inc., Chicago, IL, USA).
RESULTS
Characteristics of the patients and caregivers
Table 1 shows the characteristics of the patients and their caregivers enrolled in the present study. The mean age of the patients and their caregivers was 75.8 years and 57.1 years, respectively. Approximately 67.8% of patients and 72.9% of caregivers were female. The mean years of education in patients and caregivers were 6.8 years and 12.5 years, respectively.
Table 1. Characteristics of patients and caregivers.
| Subjects | Values | |
|---|---|---|
| Patients (n=454) | ||
| Age (yr) | 75.8±8.4 | |
| Sex (female) | 308 (67.8) | |
| Education (yr) | 6.8±5.3 | |
| K-MMSE | 16.1±5.7 | |
| CDR-SB | 7.1±4.4 | |
| S-IADL | 22.0±12.5 | |
| BADL | 17.3±4.6 | |
| CGA-NPI | 15.9±9.8 | |
| Caregivers (n=454) | ||
| Age (yr) | 57.1±12.9 | |
| Sex (female) | 331 (72.9) | |
| Education (yr) | 12.5±3.9 | |
| Duration of care (yr) | 4.1±4.4 | |
| ZBI | 40.7±20.3 | |
| CAS-K (hr) | 11.9±6.6 | |
| BDI | 14.1±9.9 | |
| Physical HRQoL | 46.6±10.4 | |
| Mental HRQoL | 38.0±15.0 | |
Data are shown as mean±standard deviation or number (%).
K-MMSE: Korean version of the Mini-Mental State Examination, CDR-SB: Clinical Dementia Rating Sum of Boxes, BADL: Barthel Activity of Daily Living, S-IADL: Seoul Instrumental Activities of Daily Living, CGA-NPI: Caregiver Administered Neuropsychiatric Inventory, ZBI: Zarit Burden Interview, CAS-K: Korean version of the Caregiver Activity Survey, BDI: Beck Depression Inventory, HRQoL: health-related quality of life.
Regarding clinical features, the mean K-MMSE score was 16.1±5.7 and mean CDR-SB score was 7.1±4.4. Basic Activities of Daily Living (ADL) were measured with the BADL, with a mean score of 17.3±4.6, while instrumental ADL were measured with the S-IADL, with a mean score of 22.0±12.5. Neuropsychiatric features of patients were measured with the CGA-NPI, with a mean score of 15.9±9.8.
The mean score for caregiver burden, measured with the ZBI, was 40.7±20.3, and the total time spent supporting the patients in the preceding 24 hours was 11.9±6.6 hours. Depression in the caregiver was measured with the BDI, with a mean score of 14.1±9.9. In the SF36, the mean score for the PCS and the MCS was 46.6±10.4 and 38.0±15.0, respectively.
Correlation and linear regression analyses
Results from the Pearson's correlation analyses are summarized in Table 2. There were various correlations among factors, including age and sex of patients and caregivers, as well as other patient and caregiver characteristics. Assuming that the correlations between patient and caregiver factors could be reciprocal, we simplified the correlations to identify independent predictors for adverse outcomes in caregivers and subsequently performed linear regression analyses.
Table 2. Correlation matrix of patient and caregiver variables.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Patient age | 1 | |||||||||||||
| 2. Patient sex | 0.045 | 1 | ||||||||||||
| 3. K-MMSE | −0.058 | −0.099 | 1 | |||||||||||
| 4. CDR-SB | 0.047 | −0.036 | −0.707 | 1 | ||||||||||
| 5. BADL | −0.135 | −0.025 | 0.548 | −0.674 | 1 | |||||||||
| 6. S-IADL | 0.063 | −0.021 | −0.559 | 0.800 | −0.633 | 1 | ||||||||
| 7. CGA-NPI | −0.035 | 0.000 | −0.305 | 0.481 | −0.377 | 0.478 | 1 | |||||||
| 8. Caregiver age | 0.053 | −0.113 | 0.015 | 0.115 | −0.135 | 0.162 | 0.079 | 1 | ||||||
| 9. Caregiver sex | 0.083 | −0.085 | 0.016 | 0.027 | −0.015 | −0.029 | 0.075 | −0.184 | 1 | |||||
| 10. ZBI | −0.123 | −0.071 | −0.258 | 0.407 | −0.371 | 0.389 | 0.432 | 0.133 | 0.115 | 1 | ||||
| 11. CAS-K | −0.208 | −0.075 | −0.176 | 0.204 | −0.127 | 0.251 | 0.235 | 0.053 | 0.030 | 0.338 | 1 | |||
| 12. BDI | −0.113 | −0.092 | −0.171 | 0.221 | −0.331 | 0.242 | 0.352 | 0.077 | 0.131 | 0.553 | 0.252 | 1 | ||
| 13. Physical HRQoL | −0.038 | 0.081 | 0.039 | −0.159 | 0.268 | −0.220 | −0.171 | −0.360 | −0.103 | −0.357 | −0.163 | −0.435 | 1 | |
| 14. Mental HRQoL | 0.153 | 0.096 | 0.175 | −0.211 | 0.287 | −0.213 | −0.280 | −0.009 | −0.150 | −0.643 | −0.343 | −0.695 | 0.361 | 1 |
K-MMSE: Korean version of the Mini-Mental State Examination, CDR-SB: Clinical Dementia Rating Sum of Boxes, BADL: Barthel Activity of Daily Living, S-IADL: Seoul Instrumental Activities of Daily Living, CGA-NPI: Caregiver Administered Neuropsychiatric Inventory, ZBI: Zarit Burden Interview, CAS-K: Korean version of the Caregiver Activity Survey, BDI: Beck Depression Inventory, HRQoL: health-related quality of life.
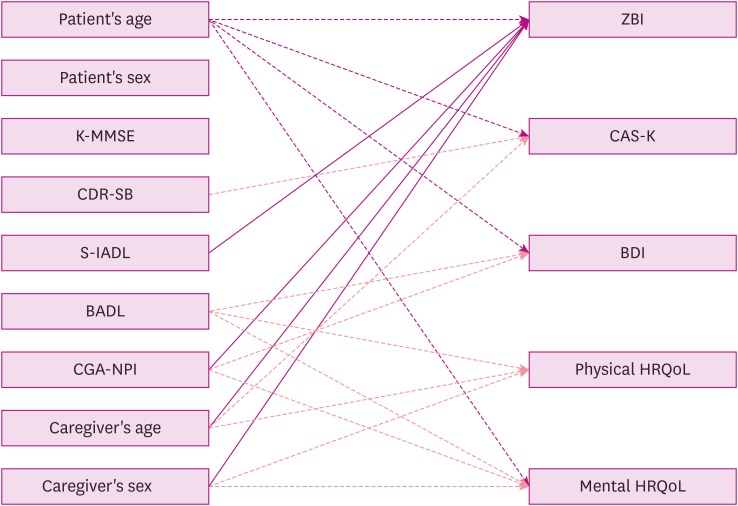
Results from the linear regression analyses are shown in Table 3 and Fig. 1. First, ZBI scores were higher in female caregivers (0.160, p<0.005) and positively correlated with patients' S-IADL (0.258, p<0.001) and CGA-NPI scores (0.278, p<0.001). On the contrary, patients' age was negatively correlated with ZBI scores (−0.221, p<0.001). There was also a positive correlation between time spent caring with patients' and CGA-NPI scores (0.272, p<0.001) while time spent caring with patients was negatively correlated with patients' age (−0.230, p<0.001) and BADL (−0.229, p<0.001).
Table 3. Results of multivariate linear regression analyses.
| Variables | Adjusted R2 | Patient age | Patient sex | K-MMSE | CDR-SB | BADL | S-IADL | CGA-NPI | Caregiver age | Caregiver sex | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coeff | p-value | Coeff | p-value | Coeff | p-value | Coeff | p-value | Coeff | p-value | Coeff | p-value | Coeff | p-value | Coeff | p-value | Coeff | p-value | ||
| ZBI | 0.299 | −0.221 | <0.001 | 0.258 | <0.001 | 0.278 | <0.001 | 0.142 | 0.013 | 0.160 | 0.005 | ||||||||
| CAS-K | 0.155 | −0.230 | <0.001 | −0.229 | <0.001 | 0.272 | <0.001 | ||||||||||||
| BDI | 0.189 | −0.132 | 0.022 | 0.269 | <0.001 | 0.141 | 0.017 | ||||||||||||
| Physical HRQoL | 0.214 | 0.195 | 0.001 | −0.395 | <0.001 | −0.196 | 0.001 | ||||||||||||
| Mental HRQoL | 0.146 | 0.198 | 0.001 | 0.165 | 0.010 | −0.208 | 0.001 | −0.124 | 0.038 | ||||||||||
K-MMSE: Korean version of the Mini-Mental State Examination, CDR-SB: Clinical Dementia Rating Sum of Boxes, BADL: Barthel Activity of Daily Living, S-IADL: Seoul Instrumental Activities of Daily Living, CGA-NPI: Caregiver Administered Neuropsychiatric Inventory, ZBI: Zarit Burden Interview, CAS-K: Korean version of the Caregiver Activity Survey, BDI: Beck Depression Inventory, HRQoL: health-related quality of life, Coeff: coefficient.
Fig. 1. Summary diagram of the results of linear regression analysis.
K-MMSE: Korean version of the Mini-Mental State Examination, CDR-SB: Clinical Dementia Rating Sum of Boxes, S-IADL: Seoul Instrumental Activities of Daily Living, BADL: Barthel Activity of Daily Living, CGA-NPI: Caregiver Administered Neuropsychiatric Inventory, ZBI: Zarit Burden Interview, CAS-K: Korean version of the Caregiver Activity Survey, BDI: Beck Depression Inventory, HRQoL: health-related quality of life.
Depression amongst caregivers measured with the BDI was positively correlated with patients' CDR-SB scores (0.269, p<0.001). Physical HRQoL indicated by PCS scores was lower in female caregivers (−0.196, p<0.01) and exhibited positive correlation with BADL scores (0.195, p<0.001) but negative correlation with caregivers' age (−0.395, p<0.001). Lastly, mental HRQoL indicated by MCS scores was higher in patients with a more increased level of ADL (0.165, p<0.01) and older patients (0.198, p<0.001), but lower in patients with more abnormal behaviors (−0.208, p<0.001).
DISCUSSION
We investigated independent predictors of adverse outcomes in caregivers, including caregiver burden, depression, increased time spent caring, and poor physical and mental quality of life in a well-defined patient-caregiver cohort. We developed simplified prediction models using limited information that could be acquired easily in the physician's office. In addition to subjective adverse outcomes measured with the ZBI, we added an objective measure of time spent caring and tried to find meaningful diverse relationships.
Of all the adverse outcome measures, ZBI scores showed relationships with the largest number of patient and caregiver factors. As already mentioned in the introduction, ZBI is one of the most widely used measures of caregiver burden and is considered as an integrated score to measure subjective care burden. The ZBI results showed that female caregivers experienced a significantly higher care burden and this relationship with caregiver characteristics is consistent with previous studies.23,24,25,26 Regarding patient factors, increased S-IADL impairment and CGA-NPI scores were associated with an increased care burden, while BADL and K-MMSE scores were not observed as independent predictors of care burden. Our finding that S-IADL impairment was more strongly associated with caregiver burden than BADL was in agreement with some previous studies,9,27 but contrary to other studies.23,28 This may be due to the fact that patients who had been inpatients or who had lived in a residential care home were excluded and the participants' BADL were relatively preserved in the present study. There remains some controversy regarding the complicated associations of care burden measured with the ZBI with cognitive decline, functional decline, and behavioral symptoms.2,9,10,27
CAS-K scores were influenced by patients' CGA-NPI scores, age, and BADL. These findings are different from the results of previous studies, which showed that time spent caring was significantly correlated with only cognition and ADL.5,29 However, previous studies did not include the severity of dementia as an independent factor. In the present study, CDR-SB, which reflects the severity of dementia, was not correlated with any subjective measures of adverse outcome except for BDI, which is a measure of caregiver depression.
We observed that both physical and mental HRQoL were lower with worse patient BADL scores and in female caregivers. Physical HRQoL also decreased as caregivers became older and mental HRQoL decreased as patient's CGA-NPI scores increased. Regarding the relationship between functional and psychological impairment and caregivers' HRQoL, several previous studies have shown consistent results with the present study.6,30,31 However, there is controversy regarding the relationship between caregivers' HRQoL and demographic factors such as caregivers' age and sex.6 A recent meta-analysis indicated that caregivers' age and sex were not associated with caregivers' HRQoL.6 However, in some studies, a female caregiver's HRQoL was more negatively affected compared to that of male caregivers.30,32 Another study also reported an association between caregivers' age and HRQoL, which suggested that HRQoL decreased as caregivers became older.32 It could be presumed that older age influences the individual's ability and fatigability following physical activity, which would be linked directly with physical HRQoL.
Among the predictors, patients' age exhibited a major relationship with various adverse outcomes. Younger patients had increased ZBI scores, caregivers' BDI scores, and CAS-K scores, while they had lower mental HRQoL. These findings were in accordance with previous studies showing a greater care burden in caregivers of younger patients with dementia than in caregivers of older patients with dementia.7,33,34,35,36 However, the reasons for an increased care burden with younger patients is yet to be determined. The increase in subjective care burden indicated by BDI scores and mental HRQoL could be explained based on the presence of an association between psychological stress and the need for caregivers to accept the diagnosis of dementia at a younger age.7 The increase in objective caring time could be due to difficulties in controlling young patients with dementia who remain physically able and stronger compared to older patients. Interestingly, K-MMSE scores did not independently predict any adverse outcomes for caregivers. These results are in accordance with findings from previous studies suggesting that caregiver burden was not associated with the patient's cognitive status, but exhibited association with ADL impairment.31,37,38 These results emphasize the importance of functional evaluation of a patient's ability to care for themselves, rather than just cognition.
Although the present study provides several meaningful insights, some limitations should be borne in mind when considering our results. First, we developed simplified models for the analysis and did not include other characteristics of the caregiver such as the caregiver's relationship with the patient, spirituality, religion, personality, and social institutional arrangements. As already mentioned, we attempted to predict various adverse outcomes with data that can be easily obtained in the physician's office. Second, some studies have investigated reciprocal and multidimensional relationships between patient and caregiver factors, and even within caregiver factors; whereas we did not measure such a relationship. In the present study, we did not consider these relationships. Further investigation is needed to develop a comprehensive model for precise prediction of adverse outcomes.
Footnotes
Funding: This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant No. HI18C0479).
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Lee SM, Lee Y, Choi SH, Lim TS, Moon SY.
- Data curation: Moon SY.
- Investigation: Lee SM, Moon SY.
- Methodology: Lee SM, Lee Y, Choi SH, Lim TS.
- Writing - original draft: Lee SM.
- Writing - review & editing: Lee SM, Choi SH, Lim TS.
References
- 1.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 2.Etters L, Goodall D, Harrison BE. Caregiver burden among dementia patient caregivers: a review of the literature. J Am Acad Nurse Pract. 2008;20:423–428. doi: 10.1111/j.1745-7599.2008.00342.x. [DOI] [PubMed] [Google Scholar]
- 3.Brodaty H, Hadzi-Pavlovic D. Psychosocial effects on carers of living with persons with dementia. Aust N Z J Psychiatry. 1990;24:351–361. doi: 10.3109/00048679009077702. [DOI] [PubMed] [Google Scholar]
- 4.Hazzan AA, Shannon H, Ploeg J, Raina P, Gitlin LN, Oremus M. The association between caregiver well-being and care provided to persons with Alzheimer's disease and related disorders. BMC Res Notes. 2016;9:344. doi: 10.1186/s13104-016-2150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis KL, Marin DB, Kane R, Patrick D, Peskind ER, Raskind MA, et al. The Caregiver Activity Survey (CAS): development and validation of a new measure for caregivers of persons with Alzheimer's disease. Int J Geriatr Psychiatry. 1997;12:978–988. doi: 10.1002/(sici)1099-1166(199710)12:10<978::aid-gps659>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 6.Farina N, Page TE, Daley S, Brown A, Bowling A, Basset T, et al. Factors associated with the quality of life of family carers of people with dementia: a systematic review. Alzheimers Dement. 2017;13:572–581. doi: 10.1016/j.jalz.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Covinsky KE, Newcomer R, Fox P, Wood J, Sands L, Dane K, et al. Patient and caregiver characteristics associated with depression in caregivers of patients with dementia. J Gen Intern Med. 2003;18:1006–1014. doi: 10.1111/j.1525-1497.2003.30103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Springate BA, Tremont G. Dimensions of caregiver burden in dementia: impact of demographic, mood, and care recipient variables. Am J Geriatr Psychiatry. 2014;22:294–300. doi: 10.1016/j.jagp.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim H, Chang M, Rose K, Kim S. Predictors of caregiver burden in caregivers of individuals with dementia. J Adv Nurs. 2012;68:846–855. doi: 10.1111/j.1365-2648.2011.05787.x. [DOI] [PubMed] [Google Scholar]
- 10.Torrisi M, De Cola MC, Marra A, De Luca R, Bramanti P, Calabrò RS. Neuropsychiatric symptoms in dementia may predict caregiver burden: a Sicilian exploratory study. Psychogeriatrics. 2017;17:103–107. doi: 10.1111/psyg.12197. [DOI] [PubMed] [Google Scholar]
- 11.Beerens HC, Zwakhalen SM, Verbeek H, Ruwaard D, Hamers JP. Factors associated with quality of life of people with dementia in long-term care facilities: a systematic review. Int J Nurs Stud. 2013;50:1259–1270. doi: 10.1016/j.ijnurstu.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Kim SK, Park M, Lee Y, Choi SH, Moon SY, Seo SW, et al. Influence of personality on depression, burden, and health-related quality of life in family caregivers of persons with dementia. Int Psychogeriatr. 2017;29:227–237. doi: 10.1017/S1041610216001770. [DOI] [PubMed] [Google Scholar]
- 13.Yoon KH, Moon YS, Lee Y, Choi SH, Moon SY, Seo SW, et al. The moderating effect of religiosity on caregiving burden and depressive symptoms in caregivers of patients with dementia. Aging Ment Health. 2018;22:141–147. doi: 10.1080/13607863.2016.1232366. [DOI] [PubMed] [Google Scholar]
- 14.Park HK, Na DL, Han SH, Kim JY, Cheong HK, Kim SY, et al. Clinical characteristics of a nationwide hospital-based registry of mild-to-moderate Alzheimer's disease patients in Korea: a CREDOS (Clinical Research Center for Dementia of South Korea) study. J Korean Med Sci. 2011;26:1219–1226. doi: 10.3346/jkms.2011.26.9.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang Y, Na DL, Hahn S. A validity study on the Korean mini-mental state examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997;15:300–308. [Google Scholar]
- 16.Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 17.Ku HM, Kim JH, Kwon EJ, Kim SH, Lee HS, Ko HJ, et al. A study on the reliability and validity of Seoul-Instrumental Activities of Daily Living (S-IADL) J Korean Neuropsychiatr Assoc. 2004;43:189–199. [Google Scholar]
- 18.Choi SH, Na DL, Kwon HM, Yoon SJ, Jeong JH, Ha CK. The Korean version of the neuropsychiatric inventory: a scoring tool for neuropsychiatric disturbance in dementia patients. J Korean Med Sci. 2000;15:609–615. doi: 10.3346/jkms.2000.15.6.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee HS, Kim DK, Ko HJ, Ku HM, Kwon EJ, Kim JH. Measurement of stress in the caregivers of dementia patients: reliability and validity of the revised-memory and behavior problem checklist and the burden interview. Korean J Clin Psychol. 2004;23:1029–1050. [Google Scholar]
- 20.Kim JM, Shin IS, Kim SW, Yang SJ, Jeong SK, Yoon JS. Development of ‘Korean version of Caregiver Activity Survey (CAS-K)’ in caregivers of community dwelling elderly with dementia. J Korean Neurol Assoc. 2004;22:322–327. [Google Scholar]
- 21.Hahn HM, Yum TH, Shin YW, Kim KH, Yoon DJ, Chung KJ. A standardization study of Beck Depression Inventory in Korea. J Korean Neuropsychiatr Assoc. 1986;25:487–500. [Google Scholar]
- 22.Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M. Development of the Korean version of short-form 36-item health survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med. 2004;203:189–194. doi: 10.1620/tjem.203.189. [DOI] [PubMed] [Google Scholar]
- 23.Rinaldi P, Spazzafumo L, Mastriforti R, Mattioli P, Marvardi M, Polidori MC, et al. Predictors of high level of burden and distress in caregivers of demented patients: results of an Italian multicenter study. Int J Geriatr Psychiatry. 2005;20:168–174. doi: 10.1002/gps.1267. [DOI] [PubMed] [Google Scholar]
- 24.Serrano-Aguilar PG, Lopez-Bastida J, Yanes-Lopez V. Impact on health-related quality of life and perceived burden of informal caregivers of individuals with Alzheimer's disease. Neuroepidemiology. 2006;27:136–142. doi: 10.1159/000095760. [DOI] [PubMed] [Google Scholar]
- 25.Akpınar B, Küçükgüçlü O, Yener G. Effects of gender on burden among caregivers of Alzheimer's patients. J Nurs Scholarsh. 2011;43:248–254. doi: 10.1111/j.1547-5069.2011.01402.x. [DOI] [PubMed] [Google Scholar]
- 26.Kim MD, Hong SC, Lee CI, Kim SY, Kang IO, Lee SY. Caregiver burden among caregivers of Koreans with dementia. Gerontology. 2009;55:106–113. doi: 10.1159/000176300. [DOI] [PubMed] [Google Scholar]
- 27.Park M, Sung M, Kim SK, Kim S, Lee DY. Multidimensional determinants of family caregiver burden in Alzheimer's disease. Int Psychogeriatr. 2015;27:1355–1364. doi: 10.1017/S1041610215000460. [DOI] [PubMed] [Google Scholar]
- 28.Sussman T, Regehr C. The influence of community-based services on the burden of spouses caring for their partners with dementia. Health Soc Work. 2009;34:29–39. doi: 10.1093/hsw/34.1.29. [DOI] [PubMed] [Google Scholar]
- 29.Marin DB, Dugue M, Schmeidler J, Santoro J, Neugroschl J, Zaklad G, et al. The Caregiver Activity Survey (CAS): longitudinal validation of an instrument that measures time spent caregiving for individuals with Alzheimer's disease. Int J Geriatr Psychiatry. 2000;15:680–686. doi: 10.1002/1099-1166(200008)15:8<680::aid-gps180>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 30.Andreakou MI, Papadopoulos AA, Panagiotakos DB, Niakas D. Assessment of health-related quality of life for caregivers of Alzheimer's disease patients. Int J Alzheimers Dis. 2016;2016:9213968. doi: 10.1155/2016/9213968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruvik FK, Ulstein ID, Ranhoff AH, Engedal K. The quality of life of people with dementia and their family carers. Dement Geriatr Cogn Disord. 2012;34:7–14. doi: 10.1159/000341584. [DOI] [PubMed] [Google Scholar]
- 32.Markowitz JS, Gutterman EM, Sadik K, Papadopoulos G. Health-related quality of life for caregivers of patients with Alzheimer disease. Alzheimer Dis Assoc Disord. 2003;17:209–214. doi: 10.1097/00002093-200310000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Freyne A, Kidd N, Coen R, Lawlor BA. Burden in carers of dementia patients: higher levels in carers of younger sufferers. Int J Geriatr Psychiatry. 1999;14:784–788. [PubMed] [Google Scholar]
- 34.Jones C, Edwards RT, Hounsome B. Health economics research into supporting carers of people with dementia: a systematic review of outcome measures. Health Qual Life Outcomes. 2012;10:142. doi: 10.1186/1477-7525-10-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaiser S, Panegyres PK. The psychosocial impact of young onset dementia on spouses. Am J Alzheimers Dis Other Demen. 2006;21:398–402. doi: 10.1177/1533317506293259. [DOI] [PubMed] [Google Scholar]
- 36.van Vliet D, de Vugt ME, Bakker C, Koopmans RT, Verhey FR. Impact of early onset dementia on caregivers: a review. Int J Geriatr Psychiatry. 2010;25:1091–1100. doi: 10.1002/gps.2439. [DOI] [PubMed] [Google Scholar]
- 37.Ankri J, Andrieu S, Beaufils B, Grand A, Henrard JC. Beyond the global score of the Zarit Burden Interview: useful dimensions for clinicians. Int J Geriatr Psychiatry. 2005;20:254–260. doi: 10.1002/gps.1275. [DOI] [PubMed] [Google Scholar]
- 38.Bergvall N, Brinck P, Eek D, Gustavsson A, Wimo A, Winblad B, et al. Relative importance of patient disease indicators on informal care and caregiver burden in Alzheimer's disease. Int Psychogeriatr. 2011;23:73–85. doi: 10.1017/S1041610210000785. [DOI] [PubMed] [Google Scholar]