Summary
Background
Evidence suggests that black, Asian and minority ethnic (BAME) groups have an increased risk of involuntary psychiatric care. However, to our knowledge, there is no published meta-analysis that brings together both international and UK literature and allows for comparison of the two. This study examined compulsory detention in BAME and migrant groups in the UK and internationally, and aimed to expand upon existing systematic reviews and meta-analyses of the rates of detention for BAME populations.
Methods
For this systematic review and meta-analysis, we searched five databases (PsychINFO, MEDLINE, Cochrane Controlled Register of Trials, Embase, and CINAHL) for quantitative studies comparing involuntary admission, readmission, and inpatient bed days between BAME or migrant groups and majority or native groups, published between inception and Dec 3, 2018. We extracted data on study characteristics, patient-level data on diagnosis, age, sex, ethnicity, marital status, and occupational status, and our outcomes of interest (involuntary admission to hospital, readmission to hospital, and inpatient bed days) for meta-analysis. We used a random-effects model to compare disparate outcome measures. We assessed explanations offered for the differences between minority and majority groups for the strength of the evidence supporting them. This study is prospectively registered with PROSPERO, number CRD42017078137.
Findings
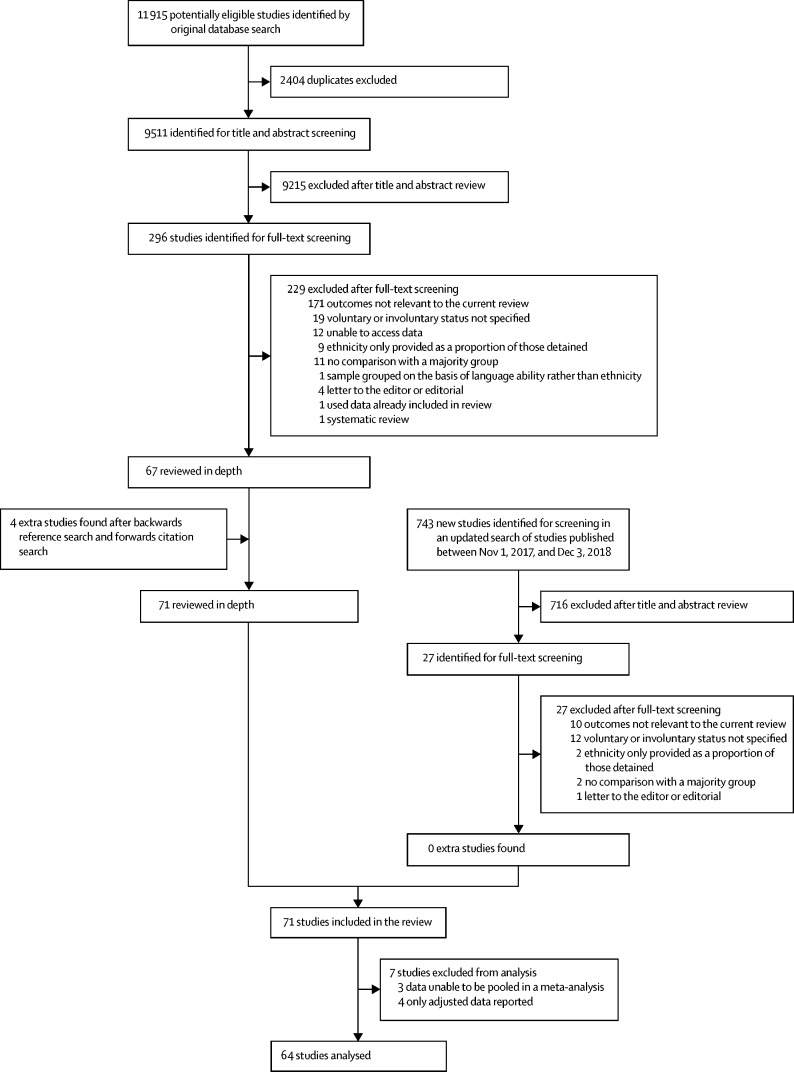
Our search identified 9511 studies for title and abstract screening, from which we identified 296 potentially relevant full-text articles. Of these, 67 met the inclusion criteria and were reviewed in depth. We added four studies after reference and citation searches, meaning 71 studies in total were included. 1 953 135 participants were included in the studies. Black Caribbean patients were significantly more likely to be compulsorily admitted to hospital compared with those in white ethnic groups (odds ratio 2·53, 95% CI 2·03–3·16, p<0·0001). Black African patients also had significantly increased odds of being compulsorily admitted to hospital compared with white ethnic groups (2·27, 1·62–3·19, p<0·0001), as did, to a lesser extent, south Asian patients (1·33, 1·07–1·65, p=0·0091). Black Caribbean patients were also significantly more likely to be readmitted to hospital compared with white ethnic groups (2·30, 1·22–4·34, p=0·0102). Migrant groups were significantly more likely to be compulsorily admitted to hospital compared with native groups (1·50, 1·21–1·87, p=0·0003). The most common explanations for the increased risk of detainment in BAME populations included increased prevalence of psychosis, increased perceived risk of violence, increased police contact, absence of or mistrust of general practitioners, and ethnic disadvantages.
Interpretation
BAME and migrant groups are at a greater risk of psychiatric detention than are majority groups, although there is variation across ethnic groups. Attempts to explain increased detention in ethnic groups should avoid amalgamation and instead carry out culturally-specific, hypothesis-driven studies to examine the numerous contributors to varying rates of detention.
Funding
University College London Hospitals National Institute for Health Research (NIHR) Biomedical Research Centre, NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust, King's College London, and NIHR Collaboration for Leadership in Applied Health Research and Care North Thames at Bart's Health NHS Trust.
Introduction
Ethnic minorities are subject to a disproportionate risk of involuntary psychiatric detention.1, 2, 3 Research has suggested that patients from black, Asian and minority ethnic (BAME) groups have more compulsory admissions to hospital,4, 5 longer inpatient stays,6 and more readmissions.7 However, other studies have reported no or weak associations between BAME populations and increased detention.8, 9 Furthermore, the risk of involuntary psychiatric detention is not consistently higher in all or specific ethnic groups,8, 9, 10 potentially undermining actions to reduce inequalities and inform policy. Although evidence from the UK suggests increased detention under the Mental Health Act (MHA) for black populations,11, 12 less is known about south Asian (including Bangladeshi, Indian, Pakistani, Sri Lankan, and Nepali people)9, 10, 13, 14 and migrant populations.15 Several explanations have been suggested for the observed disparities between minority and majority ethnic groups, such as increased prevalence of schizophrenia in some minority ethnic4, 11 and migrant16, 17 populations, insufficient patient awareness of mental health issues,10, 18 more frequent adverse experiences with mental health services,19 experience of racism or health-care provider discrimination,20, 21 and differing use of psychiatric services.22, 23 However, few of these explanations provide adequate supporting evidence.10 A meta-analysis3 highlighted the importance of ethnic specificity in study design, considering black Caribbean patients separately and in addition to black patients more generally. However, there has otherwise been little evidence to systematically update and pool knowledge of the over-representation of BAME populations in those detained under the MHA in England since its revision and, to our knowledge, no systematic review or meta-analysis has been done from an international perspective. This study aims to expand upon existing systematic reviews and meta-analyses1, 3, 10 on the rates of detention for specific BAME populations from an international perspective, and outline explanations for any disparities between populations. Novel considerations of migrant populations are also reported.
Research in context.
Evidence before this study
A large body of evidence suggests that black, Asian, and minority ethnic (BAME) groups are at an increased risk of compulsory detention under the Mental Health Act in England and Wales. However, there is marked variation in the composition of ethnic groups, definitions of ethnic groups, sample sizes, and reported magnitude of the effect sizes. The literature has typically focused on a small number of countries (primarily the UK) and has often neglected migrant populations. We searched MEDLINE (between Jan 1, 1946, and Nov 27, 2017), and PsycINFO (between Jan 1, 1806, and Nov 13, 2017), for systematic reviews and meta-analyses published in English with the search terms “minority groups” or “ethnic groups” or “BME” or “BAME” or “immigrants” or “refugees” and “Mental Health Act” or “commitment” or “admission” and “psychosis” or “schizophrenia” or “psychotic disorders”. We found no meta-analyses covering both the international and UK literature.
Added value of this study
To our knowledge, this is the first systematic review and meta-analysis to review both international and UK-based studies of compulsory detention, and the first to consider compulsory detention in migrant populations. This systematic review benefits from separate consideration of different ethnic groups where possible, avoiding grouping of culturally diverse populations. UK-based and international research showed significantly increased compulsory detention in several different ethnic minority and migrant populations, although UK research showed a more pronounced result.
Implications of all the available evidence
Our findings support that compulsory detention and readmission in all BAME populations is significantly increased compared with majority groups, as is that of migrant populations compared with host nation populations. Detention rates vary across different BAME groups, with the highest rate seen in black Caribbean populations, and less marked, but still significantly increased rates in south Asian populations. Future research should aim to establish the causes of ethnic disparities in involuntary care and should avoid cultural stereotypes and assumptions. Amalgamation of ethnic groups should be discouraged to better inform policy and practice.
Methods
Search strategy and selection criteria
For this systematic review and meta-analysis, we included studies of samples in which two or more ethnic groups of any age were compared, and that compared the risk of compulsory inpatient psychiatric care in minority and majority ethnic groups. Included study outcomes were compulsory inpatient admission to hospital, compulsory inpatient readmission to hospital, and inpatient length of stay, and we considered only quantitative data.
We developed our search strategy in consultation with an information scientist with experience in mental health, with a combination of keyword and subject heading searches. We searched MEDLINE (between Jan 1, 1946, and Nov 27, 2017), PsycINFO (between Jan 1, 1806, and Nov 13, 2017), Embase (between Jan 1, 1974, and Nov 20, 2017), Cochrane Controlled Register of Trials (between inception and Nov 27, 2017), and CINAHL (between Jan 1, 1981, and Nov 30, 2017).
Although our search was not confined to countries in which black and other non-white ethnicities are minorities, all papers meeting inclusion criteria used either white or the dominant national group as their comparison group. Full search strategies are available in the appendix (pp 1–20).
We contacted study authors; however, none contacted replied. We did not assess grey literature sources. Articles were translated to English, but none of the translated articles ended up being included. We sought summary estimate data rather than individual patient-level data.
Two reviewers (EM and KA) independently screened all titles and abstracts identified and excluded studies that did not meet the inclusion criteria. Full articles were subsequently reviewed in duplicate and in cases of disagreement, consensus was achieved through the referral of a third senior reviewer (HM). An update search was done on Dec 4, 2018, to identify any additional papers published between Nov 1, 2017, and Dec 3, 2018. We supplemented the search strategy with a backward reference search of included studies and a forward citation search using Scopus. References for all included studies are available in the appendix (pp 44–46).
The main change to our methods following protocol registration was that we expanded our inclusion criteria to encompass international literature in addition to literature from England and Wales. This change was made to provide an international context for our study, to further our understanding, and to include migrant populations, who are focused on more frequently in the international literature. Additionally, we did post-hoc meta-regression analyses to explore potential associations between predictor variables and ethnicity and to account for heterogeneity.
Data analysis
Four independent reviewers (PB, EM, HG, and KA) extracted the data and all extraction was reviewed for accuracy. An electronic Microsoft Excel-based form was used to record data extraction. We planned to exclude studies which reported data already included in our dataset, but we did not find any duplicates.
We calculated overall summary estimates (odds ratios [ORs]) and 95% CIs with a random-effects model using the R package metafor version 2.0.24 P<0·05 was considered to indicate a significant difference. We used ORs because most papers identified in our search either provided the number of events and sample sizes to calculate ORs, or gave statistics in the format of ORs when raw data were not provided.
Studies varied in their specificity of classification of ethnic groups. Unlike previous studies, we attempted to avoid aggregate comparisons. Where possible, we organised studies into the subgroups black Caribbean, black African, south Asian, and east Asian. We classified studies solely reporting data for black or black, other groups as black, unspecified. We constructed a further non-specific classification of BAME, unspecified to contain studies reporting a mixture of minority ethnicities, for example, non-white British. We also did an analysis of studies comparing migrant groups (those born outside the host country) with host populations. We included only unadjusted data in the main analysis.
We did four post-hoc meta-regressions with Comprehensive Meta-Analysis software (version 3) to explore possible causes of heterogeneity and to investigate differences between UK and international literature. With these meta-regressions, we examined possible predictors of the effect of ethnicity on compulsory admission and included mean age, proportion of women, publication year, and national context (England and Wales or internationally). We also did sensitivity analyses, including only studies rated as high quality or higher ethnic specificity for the primary outcome of compulsory admission.
Four reviewers (PB, EM, HG, and KA) quality assessed the included studies. First, we applied the 14-item quality assessment checklist devised by Kmet and colleagues25 to each study. Each study was assessed against the 14 items using a 3-point scale with a score of 2 representing fully met, 1 representing partially met, and 0 meaning a study did not meet the criterion. A total score was calculated by adding up the scores achieved for each item. If a criterion was not applicable, it was excluded from the score calculation, and therefore from the maximum total score that could be achieved. A summary score (total sum divided by the total possible sum) was then calculated, representing the methodological quality of each study. These scores were calculated as a linear score from 0 to 100 and divided into three categories: low (≤49), moderate (50–74), or high (≥75) quality studies. Second, we assessed the quality of each study in terms of ethnic specificity with an adapted version of Raine's26 review of gender differences within health care, which was developed by Bhui and colleagues1 and has been used in previous similar reviews.10 Quality rating scores were between 0 and 14 and were categorised as follows: 0–3 (low), 4–7 (medium), and 8–14 (high). For both scales, quality assessment was discussed until a consensus was obtained and disagreements were resolved through consultation with two senior reviewers (SP and HM).
We extracted data on study design, sample size, population type, country, diagnosis, age, sex, ethnicity, marital status, living status (living alone, with family, or with a significant other), education, occupation, the legal system or act (eg, whether it was the Mental Health Act, and if yes which version, or if a different country, which legal ruling the person was detained under, although this was rarely reported), and the previously mentioned study outcomes of interest (ie, involuntary admission to hospital, readmission to hospital, and inpatient bed days) and their associated statistical data. As in the study by Singh and colleagues,10 we extracted explanations for differences in psychiatric detention of BAME groups from included studies. We summarised these explanations and recorded any support from primary evidence (data from the paper itself). Unsupported explanations were those that were untested by the design of the study. We classified explanations into five domains adapted from Singh and colleagues:10 patient-related, illness-related, service-related, culture-related, and service-patient interface. If studies were previously summarised by Singh and colleagues,10 those explanations were retained. We reported explanations only when primary evidence for an association was identified.
We assessed the degree of publication bias by visual examination of funnel plots.27
We calculated heterogeneity between studies with the I2 statistic. A value of 0% indicated no observed heterogeneity and 25%, 50%, or 75% tentatively signified low, moderate, or high heterogeneity between studies, respectively.28
This study follows the PRISMA guidelines29 and is prospectively registered with PROSPERO, number CRD42017078137.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Our search identified 9511 studies for title and abstract screening, from which 296 potentially relevant full-text articles were identified (figure). Of these, 67 studies met inclusion criteria and were reviewed in depth. We also included an additional four studies after reference and citation searches. An updated search done on Dec 4, 2018, for studies published between Nov 1, 2017, and Dec 3, 2018, found no additional studies that met inclusion criteria. 1 953 135 participants were included in the studies we reviewed.
Figure.
Study selection
Study characteristics are summarised in table 1. The 71 studies included in our review reported compulsory admission (63 studies), compulsory readmission (11 studies), and inpatient bed days (two studies). Two studies reported rate ratios7, 47 and one reported a risk ratio,46 which could not be pooled and included in our meta-analysis. Four studies reported adjusted data only so were also excluded from our main analysis.22, 35, 82, 90 Most studies reported routine data from specific hospitals or districts, although some compared population rates of admission. Studies were from high-income countries, and predominantly the UK (49 studies). Other countries represented were Canada (two studies), Italy (three studies), Ireland (two studies), the Netherlands (four studies), USA (five studies), Norway (one study), Switzerland (two studies), Denmark (one study), Spain (one study), and New Zealand (one study). We found high variability in study quality and scores awarded on the ethnicity checklist,11, 26 with scores ranging from 2 to 12. The main areas of bias centred on insufficient consideration of confounding variables. We examined funnel plots to investigate publication bias and found that studies were evenly distributed around the SE (appendix), suggesting that publication bias did not significantly affect our results. However, we observed high heterogeneity for all outcomes (table 2).
Table 1.
Characteristics of included studies
| Study type | Sample size, n | Outcomes | Population | Country | Mean age (range), years | Sex, % female | Ethnicity | Study quality | Ethnicity checklist | |
|---|---|---|---|---|---|---|---|---|---|---|
| Afuwape et al30 (2006) | Cohort | 213 | Compulsory admission | Community | England | 37·5 (NR) | 16·4 | White: 55%; black Caribbean: 8%; black African: 10%; black British: 26% | High | Medium |
| Agius et al31 (2008) | Cohort | 61 | Compulsory admission | Community | England | NR | 24·2 | Caucasian: 43%; African Caribbean: 16%; south Asian: 41% | Low | Low |
| Ajnakina et al32 (2017) | Cohort | 245 | Compulsory admission | Clinic | England | NR (18–65) | 44·0 | White British: 38%; black African: 34·7%; black Caribbean: 27·3% | High | Medium |
| Ali et al13 (2007) | Cohort | 294 387 | Compulsory admission | Clinic | England | NR (18–65) | NR | Caucasian: 81% (of those detained); Asian: 19% (of those detained) | Moderate | Medium |
| Archie et al33 (2010) | Cross-sectional | 200 | Compulsory admission | Clinic | Canada | NR (16–50) | 22·0 | White: 60·2%; black: 15·4%; Asian: 12·5% | High | Medium |
| Balducci et al34 (2017) | Case-control | 848 | Compulsory admission | Hospital | Italy | 41·6 (NR) | NR | Foreign nationality: 15·6%; native: 84·4% | Moderate | Medium |
| Bansal et al35 (2014) | Cohort | NR | Compulsory admission | Clinic and community | Scotland | 46·3 (NR) | NR | NR | High | Medium |
| Bebbington et al4 (1994) | Cross-sectional | 376 | Compulsory admission | Hospital | England | NR | 52·9 | White: 79·5%; black Caribbean: 20·5% (of those compulsorily detained) | Moderate | Medium |
| Bhui et al11 (1998) | Cross-sectional | 277 | Compulsory admission | Prison | England | NR | 0 | White: 70%; black Caribbean:11%; black African: 6%; black British: 5%; Asian or other: 7% | High | High |
| Borschmann et al36 (2010) | Case-control | 887 | Compulsory admission | Community | England | 37·1 (NR) | NR | White: 71·6%; black: 17·2%; Asian: 6·7%; mixed: 1·8%; Chinese: 1·7% | Low | Medium |
| Bowers et al37 (2009) | Cross-sectional | NR | Compulsory admission | Hospital | England | NR | 50·9 | White: 73·13%; Irish: 2·3%; Caribbean: 6·5%; African: 5·3%; south Asian: 6·4%; other: 6·4% | Moderate | High |
| Burnett et al38 (1999) | Cohort | 909 | Compulsory admission, readmission | Hospital and community | England | NR (17–62) | 35·0 | White: 38%; African Caribbean: 38%; Asian: 24% | Moderate | Medium |
| Callan39 (1996) | Cohort | 144 | Compulsory admission | Hospital | England | NR | 39·5 | White British: 51%; African Caribbean: 52% | Moderate | Medium |
| Coid et al40 (2000) | Case-control | 3155 | Compulsory admission | Hospital | England and Wales | 31·4 (NR) | 13·7 | White: 74%; black: 21%; Asian: 3%; other: 2% | High | Medium |
| Cole et al41 (1995) | Case-control | 93 | Compulsory admission | Hospital | England | 29·0 (17–53) | 46·2 | White: 42%; black Caribbean: 20%; black African: 15%; black other: 5%; Indian: 5%; Pakistani: 3%; other Asian: 3% | Moderate | Medium |
| Commander et al42 (1999) | Cohort | 240 | Compulsory admission | Hospital | England | NR (16–60) | 50·4 | White: 33%; black: 33%; Asian: 33% | Moderate | Medium |
| Cope and Ndegwa43 (1990) | Case-control | 115 | Compulsory admission, readmission | Hospital | England | 32·0 (18–70) | 10·4 | White: 56·5%; African Caribbean: 38·3%; Asian: 5·2% (excluded) | Moderate | Medium |
| Corrigal and Bhugra12 (2013) | Case note review | 435 | Compulsory admission | Hospital | England | 16·3 (12–17) | 53·0 | White: 32%; black: 49%; Asian: 3%; other: 16% | High | Medium |
| Crowley and Simmons44 (1992) | Case note review | 152 | Compulsory admission | Community and hospital | England | NR | 46·7 | White: 49·3%; African Caribbean: 50·7% | Moderate | Medium |
| Curley et al45 (2016) | Case-control | 1099 | Compulsory admission | Hospital | Ireland | 40·2 (16·4–81·9) | 52·9 | Irish: 86·2%; other European: 6·82%; Asian: 1·36%; African: 4·73%; American: 0·09% | Moderate | Low |
| Davies et al46 (1996) | Cohort | 439 | Compulsory admission | Community and hospital | England | 42·7 (NR) | 52·6 | White: 61·5%; Caribbean: 27·8%; black African: 7·0%; other: 3·6% | Moderate | Medium |
| de Wit et al47 (2012) | Case-control | 2646 | Compulsory admission | Hospital | Netherlands | NR | 40·9 | Dutch: 1289; Surinamese: 404; Antillean: 74; Moroccan: 169; Turkish: 96; other western: 384; other non-western: 230 | Moderate | High |
| Dunn and Fahy48 (1990) | Case note review | 268 | Readmission | Hospital | England | 33·2 (18–85) | 37·9 | White: 61%; black: 33%; Asian: 3% (excluded) | Low | Low |
| Fassaert et al49 (2016) | Case-control | 30 655 | Compulsory admission | Clinic | Netherlands | 36·5 (NR) | 38·1 | Dutch natives: 58·8%; Antillean: 1·4%; Surinamese: 4·3%; Moroccan: 4%; Turkish: 2·3%; other non-western: 6·5%; other western: 6%; ethnicity unknown: 17·7% | High | High |
| Gajwani et al5 (2016) | Cohort | 863 | Compulsory admission | Community and hospital | England | NR | NR | White: 51·1%; Asian Pakistani: 14·9%; African Caribbean: 14%; black African: 7% | Moderate | Medium |
| Goater et al50 (1999) | Cohort | 93 | Compulsory admission | Community and hospital | England | NR | NR | White: 41·9%; black: 40·9%; Asian: 11·8%; other: 5·4% | Moderate | Medium |
| Gray Houston et al51 (2001) | Cohort | 487 | Compulsory admission | Hospital | USA | 35·8 (18–65) | 52·0 | Euro-American: 53%; African-American: 34%; Hispanic American: 13% | Low | Low |
| Hamilton et al52 (2015) | Cohort | 5183 | Compulsory admission | Hospital | USA | 35·7 (NR) | 38·1 | African American: 51·6%; non-Hispanic white: 48·4% | Moderate | Medium |
| Harrison et al53 (1984) | Case note review | 203 | Readmission | Hospital | England | NR | NR | White: 86·7%; West Indian: 13·3% | Low | Low |
| Ineichen et al54 (1984) | Cohort | 264 | Compulsory admission | Hospital | England | NR | 60·3 | NR | Low | Medium |
| Iverson and Morgan55 (2003) | Case-control | 3053 | Compulsory admission | Hospital | Norway | 41·1 (NR) | 48·7 | Immigrants: 35·3%; asylum seekers: 14·7%; Norwegian: 50% | Moderate | Medium |
| Dannerbeck Janku and Yan8 (2009) | Case-control | 379 | Compulsory admission | Prison | USA | NR | NR | Caucasian: 48%; African American: 52% | Moderate | Medium |
| Johnson et al56 (1998) | Cohort | 286 | Compulsory admission | Community | England | 42·1 (NR) | 52·0 | White: 63%; black Caribbean: 26%; black African: 6%; other: 5% | Moderate | High |
| Kelly et al57 (2015) | Cohort | 518 | Compulsory admission | Hospital | Ireland | 40·1 (16–80) | 49·6 | Irish: 84%; other European: 6·6%; Asian: 2·3%; African: 5·6%; American: 0·8%; Australian: 0·8% | Low | Low |
| Kilbourne et al58 (2005) | Cross-sectional | 330 | Compulsory admission | Hospital | USA | 46·6 (NR) | 10·0 | White: 76%; American Indian or Alaska native: 4%; Asian or Pacific islander: 5%; black: 14%; Hispanic: 5%; other: 5% | Moderate | Medium |
| Koffman et al59 (1997) | Cross-sectional | 3978 | Compulsory admission | Hospital | England | NR | NR | White: 75%; black:16%; Asian: 4% | Moderate | Medium |
| Lawlor et al60 (2012) | Case-control | 287 | Compulsory admission | Hospital | England | 40·1 (18–69) | 100 | White British: 50·9%; white other: 15·7%; black Caribbean: 9·1%; black African: 14·3%; black other: 10·1% | High | High |
| Law-Min et al61 (2003) | Case-control | 189 | Compulsory admission, readmission | Hospital | England | 40·0 (NR) | 40·0 | White: 66%; African Caribbean: 16%; Asian: 15%; other: 3% | Low | Low |
| Lay et al22 (2005) | Case-control | 23 377 | Compulsory admission | Hospital | Switzerland | 37·3 (18–65) | 47·0 | Switzerland: 80·6%; southern Europe: 5·3%; west or northern Europe: 3%; former Yugoslavia: 4·3%; Turkey: 1·9%; eastern Europe: 0·8%; other: 4·2% | High | Medium |
| Lay et al62 (2011) | Cross-sectional | 9698 | Compulsory admission | Hospital | Switzerland | 40·4 (18–70) | 51·0 | Switzerland: 78·3%; foreign national: 21·7% | High | High |
| Lindsey et al63 (1989) | Cross-sectional | 227 | Inpatient bed days, readmission | Hospital | USA | 35·3 (18–65) | 45·8 | White: 50·7%; black: 49·3% | Moderate | Medium |
| Lloyd and Moodley64 (1992) | Cross-sectional | 138 | Compulsory admission | Hospital | England | NR | NR | White: 73·2%; black: 26·8% | Moderate | Medium |
| Mann et al65 (2014) | Cohort | 674 | Compulsory admission | Hospital | England | 24·0 (18–35) | 35·0 | White British: 23·4%; white other: 13·8%; mixed: 5·3%; south Asian: 5·5%; other Asian: 4·3%; black British: 8·2%; black Caribbean: 11·6%; black African: 27·9% | High | Medium |
| McGovern et al66 (1994) | Cohort | 75 | Readmission | Hospital | England | 22·2 (16–29) | 30·6 | White: 44%; black: 66% | Moderate | Medium |
| McKenzie et al67 (1995) | Cohort | 113 | Readmission | Hospital | England | NR (16–60) | 30·9 | White: 53·1%; African Caribbean: 46·9% | Moderate | High |
| Mohan at el6 (2006) | Cohort | 140 | Compulsory admission, inpatient bed days | Community | England | 41·8 (NR) | 43·8 | White: 65·7%; African Caribbean: 34·3% | Moderate | Medium |
| Moodley and Perkins68 (1991) | Cross-sectional | 52 | Compulsory admission | Hospital | England | 39·0 (18–64) | 63·5 | White: 48%; African Caribbean: 42% | Low | Medium |
| Morgan et al69 (2005) | Cohort | 462 | Compulsory admission | Hospital | England | NR (16–65) | 42·2 | White British: 51·3%; African Caribbean: 27·7%; black African: 13·9%; other white: 7·1% | Moderate | Medium |
| Mulder et al23 (2006) | Cohort | 720 | Compulsory admission | Community | Netherlands | 37·0 (NR) | 45·4 | Dutch natives: 67%; immigrants: 33% | Moderate | Medium |
| Norredam et al70 (2010) | Cohort | 312 300 | Compulsory admission | Hospital | Denmark | 30·0 (NR) | 54·80 | Refugees: 9·3%; immigrants: 10·7%; Danish born: 80% | Moderate | Medium |
| Oluwatayo and Gaterl71 (2004) | Case note review | 200 | Readmission | Hospital | England | 33·0 (16–65) | 41·0 | White British: 50%; African Caribbean: 50% | Moderate | Medium |
| Owens et al72 (1991) | Case-control | 275 | Compulsory admission | Hospital | England | NR | 49·8 | White: 56·4%; African Caribbean: 43·6% | Moderate | Low |
| Parkman et al73 (1997) | Case note review | 202 | Compulsory admission | Community and hospital | England | 43·2 (NR) | 46·9 | White: 73%; black Caribbean: 27% | Moderate | High |
| Perez-Rodriguez et al74 (2006) | Cohort | 1015 | Compulsory admission | Hospital | Spain | NR | NR | NR | Moderate | Medium |
| Priebe et al7 (2009) | Case-control | 778 | Readmission | Hospital | England | 37·1 (18–65) | 38·0 | White: 73%; black: 18%; Asian: 6%; other: 3% | High | Medium |
| Reeves et al75 (2002) | Cohort | 44 | Compulsory admission | Hospital | England | NR | 75·9 | British born: 50%; Caribbean born: 50% | Moderate | Medium |
| Rotenberg et al76 (2017) | Cohort | 765 | Compulsory admission | Hospital | Canada | 38·0 (NR) | 36·7 | East Asian: 17·9%; south Asian: 11·9%; black African: 12·9%; black Caribbean: 18·4%; white North American: 19·6%; white European: 19·2% | High | High |
| Selten and Sijben77 (1994) | Cohort | 813 | Compulsory admission | Hospital | Netherlands | NR (15–34) | 0 | Native Dutch: 83·4%; Surinamese: 2·6%; Antillean: 1·0%; Turkish: 0·5%; Moroccan: 1·7% | Low | Low |
| Singh et al78 (1998) | Cross-sectional | 417 | Compulsory admission | Hospital | England | NR (16–NR) | 49·2 | White European: 81·5%; black Caribbean: 7·3%; black African: 0·4%; Pakistani: 1·7%; Indian: 2·5%; Bangladeshi: 0·2%; Chinese: 0·2%; mixed ethnic origin: 2·8% | High | Medium |
| Singh et al2 (2014) | Cohort | 4275 | Compulsory admission | Hospital | England | NR | 43·5 | White: 61·6%; black: 19·3%; Asian: 10·4%; other: 8·6% | High | Medium |
| Singh et al79 (2015) | Cohort | 123 | Compulsory admission | Hospital | England | 23·2 (14–37) | 26·0 | White: 36·6%; black: 28·4%; Asian: 35% | High | High |
| Sohler et al80 (2004) | Case-control | 501 | Compulsory admission | Hospital | England | NR | 42·80 | Black: 16·2%; white: 83·8% | Moderate | High |
| Spinogatti et al81 (2015) | Case-control | NR | Compulsory admission | NR | Italy | NR (17–NR) | NR | NR | Low | Medium |
| Takei et al82 (1998) | Cohort | 88 | Compulsory admission | Hospital | England | 22·9 (18–44) | 37·1 | White: 60·5%; African Caribbean: 39·5% | Moderate | Medium |
| Tarsitani et al83 (2013) | Case-control | 200 | Compulsory admission | Hospital | Italy | 35·9 (NR) | 58·0 | Natives: 50%; immigrants: 50% | Moderate | Medium |
| Thomas et al84 (1993) | Case-control | 1534 | Compulsory admission; readmission | NR | England | 36·6 (16–NR) | 47·9 | UK: 82·5%; Asian: 4·9%; African Caribbean: 12·6% | Moderate | Medium |
| Thornicroft et al85 (1999) | Case note review | 439 | Compulsory admission | Hospital | England | 42·7 (NR) | 52·6 | White: 57·9%; black Caribbean: 26·2%; black African: 6·6%; other: 3·4% | High | Medium |
| Tolmac and Hodes86 (2004) | Cross-sectional | 113 | Compulsory admission | Hospital | England | NR (13–17) | 53·0 | White: 60%; black: 19%; Asian: 10%; other: 11% | Moderate | Medium |
| Webber and Huxley87 (2004) | Case note review | 300 | Compulsory admission | Hospital | England | 39·5 (NR) | 48·6 | White British: 62%; non-white British: 38% | Moderate | Medium |
| Weich et al88 (2017) | Cross-sectional | 1 238 188 | Compulsory admission | Hospital | England | NR | 55·3 | White: 80·2%; black: 3·4%; Asian: 4%; mixed: 1%; other: 2% | High | High |
| Wheeler et al89 (2005) | Case note review | 932 | Compulsory admission | Hospital | New Zealand | NR (16–68) | 44 | European: 60·3%; New Zealand Maori: 23·4%; Pacific nations: 10·7%; Asian: 4·3%; other 1·3% | Moderate | Medium |
NR=not reported.
Table 2.
Association of involuntary psychiatric care with ethnicity
| Number of studies | Odds ratio (95% CI) | p value | I2 | |
|---|---|---|---|---|
| Compulsory inpatient admission | ||||
| Black African | 10 | 2·27 (1·62–3·19) | <0·0001 | 71·11% |
| Black Caribbean | 25 | 2·53 (2·03–3·16) | <0·0001 | 70·69% |
| Black, unspecified | 20 | 2·00 (1·28–3·11) | 0·0022 | 98·08% |
| South Asian | 20 | 1·33 (1·07–1·65) | 0·0091 | 83·38% |
| East Asian | 3 | 2·17 (1·47–3·22) | 0·0001 | 8·88% |
| Other minority ethnicities | 13 | 1·66 (1·29–2·14) | <0·0001 | 81·14% |
| Migrants | 12 | 1·50 (1·21–1·87) | 0·0003 | 87·15% |
| Compulsory inpatient readmission | ||||
| Black Caribbean | 7 | 2·30 (1·22–4·34) | 0·0102 | 81·95% |
| Black, unspecified | 4 | 1·30 (0·69–2·44) | 0·4118 | 66·87% |
| South Asian | 2 | 2·34 (0·61–8·99) | 0·2161 | 89·57% |
| Compulsory inpatient bed days | ||||
| Black, combined* | 2 | 0·88 (0·18–4·19) | 0·8687 | 83·61% |
All groups were compared with white populations except migrants, who were compared with host nation populations.
For inpatient bed days, black, combined comprises black and African Caribbean patients.
Black ethnic groups were significantly more likely to be compulsorily admitted to hospital compared with white ethnic groups (black, unspecified OR 2·00, 95% CI 1·28–3·11, p=0·0022; black Caribbean 2·53, 2·03–3·16, p<0·0001; black African 2·27, 1·62–3·19, p<0·0001; table 2). Black Caribbean patients were also significantly more likely to be readmitted to hospital compared with white ethnic groups (2·30, 1·22–4·34, p=0·0102). We found no significant association between ethnicity and inpatient bed days (0·88, 0·18–4·19, p=0·8687), although this comparison included only two studies (table 2). People from Asian ethnic groups were significantly more likely to be compulsorily admitted to hospital compared with people from white ethnic groups (south Asian 1·33, 1·07–1·65, p=0·0091; east Asian 2·17, 1·47–3·22, p=0·0001). Only two studies reported compulsory inpatient readmission in south Asian patients and the results of these were not significant. Other minority ethnicities were significantly more likely to be compulsorily admitted to hospital compared with majority groups (1·66, 1·29–2·14, p<0·0001), as were migrant populations compared with host nation populations (1·50, 1·21–1·87, p=0·0003). Forest plots for our analyses are provided in the appendix (pp 25–30).
Study location was a significant predictor of compulsory admission in black, unspecified groups, such that UK-based studies reported significantly increased odds of compulsory admission in black ethnic groups compared with international studies (table 3). The proportion of women in the sample was also a significant predictor of compulsory admission to hospital in black, unspecified, black Caribbean, and south Asian groups. This association remained significant when adjusted for age in black, unspecified and black Caribbean groups, but was no longer significant in south Asian groups. Publication date was a significant predictor of compulsory admission to hospital only in black Caribbean groups, and mean age was not a significant predictor of compulsory admission (table 3). Scatter plots of these data are provided in the appendix (p 31–35).
Table 3.
Predictors of involuntary psychiatric admission by ethnicity
| Number of studies | R2 | p value | Coefficient (95% CI) | |
|---|---|---|---|---|
| Publication date | ||||
| Black African | 10 | 0% | 0·6157 | −0·0126 (−0·0620 to 0·0367) |
| Black Caribbean | 25 | 42% | 0·0006 | −0·0361 (−0·0567 to −0·0156) |
| Black, unspecified | 20 | 7% | 0·9626 | 0·0013 (−0·0543 to 0·0570) |
| South Asian | 19 | 0% | 0·6401 | −0·0098 (−0·0403 to 0·0206) |
| Migrants | 12 | 0% | 0·4400 | 0·0146 (−0·0225 to 0·0517) |
| Proportion of women | ||||
| Black Caribbean | 24 | 59% | <0·0001 | 0·0247 (0·0135 to 0·0359) |
| Black, unspecified | 15 | 64% | 0·0344 | 0·0191 (0·0014 to 0·0367) |
| South Asian | 15 | 30% | 0·0345 | 0·0178 (0·0003 to 0·0354) |
| Mean age | ||||
| Black Caribbean | 12 | 25% | 0·0646 | 0·0452 (−0·0019 to 0·0924) |
| International study location | ||||
| Black, unspecified | 20 | 31% | 0·0434 | −0·8976 (−1·7685 to −0·0267) |
All groups were compared with white populations except migrants, who were compared with host nation populations.
We did secondary analyses on compulsory admission data to examine the effect of study quality on results (table 4). When including only studies scoring highly on the ethnicity checklist, results remained significant. When including only studies rated highly with the Kmet quality assessment scale, results remained significant in all black ethnic groups, but became non-significant in south Asian groups. Only six studies scored highly on both quality assessment scales, making these analyses difficult to draw conclusions from.
Table 4.
Association of involuntary inpatient admission and ethnicity, restricted to high-quality studies
| Number of studies | Odds ratio (95% CI) | p value | I2 | |
|---|---|---|---|---|
| Black African | ||||
| All studies | 10 | 2·27 (1·62–3·19) | <0·0001 | 71·11% |
| Kmet study quality | 6 | 2·63 (1·80–3·83) | <0·0001 | 44·85% |
| Ethnicity checklist | 5 | 2·49 (1·62–3·82) | <0·0001 | 56·89% |
| Both | 3 | 2·40 (0·84–6·89) | 0·1038 | 77·39% |
| Black Caribbean | ||||
| All studies | 25 | 2·53 (2·03–3·16) | <0·0001 | 70·69% |
| Kmet study quality | 7 | 2·15 (1·48–3·13) | 0·0001 | 56·53% |
| Ethnicity checklist | 6 | 2·45 (1·81–3·32) | <0·0001 | 32·86% |
| Both | 3 | 2·03 (0·86–4·77) | 0·1045 | 65·92% |
| Black, unspecified | ||||
| All studies | 20 | 2·00 (1·28–3·11) | 0·0022 | 98·08% |
| Kmet study quality | 9 | 2·25 (1·15–4·37) | 0·0172 | 98·01% |
| Ethnicity checklist | 5 | 3·31 (1·72–6·38) | 0·0003 | 84·41% |
| Both | 4 | 4·35 (4·22–4·49) | <0·0001 | 0 |
| South Asian | ||||
| All studies | 20 | 1·33 (1·07–1·65) | 0·0091 | 83·38% |
| Kmet study quality | 8 | 1·07 (0·71–1·61) | 0·7543 | 89·89% |
| Ethnicity checklist | 4 | 1·89 (1·82–1·97) | <0·0001 | 0 |
| Both | 3 | 1·90 (1·83–1·98) | <0·0001 | 0 |
Other groups had insufficient numbers of high quality or high ethnicity checklist scoring studies for analysis.
We did a sensitivity analysis to investigate if studies excluded for reporting only adjusted data22, 35, 82, 90 could have significantly affected results (appendix p 36). We included three studies in the sensitivity analysis because they adjusted for demographic variables (age and sex) only.22, 82, 90 We observed only marginal differences, with no consequent difference in interpretation. One study35 adjusted for additional variables (car ownership and housing tenure) in addition to age and sex and reported only risk ratios; we excluded this study from the sensitivity analysis.
We extracted explanations for disparities in psychiatric detentions from all papers included in the review (appendix pp 37–43). Of the 71 studies, 12 offered no explanation for differences in psychiatric detention of BAME groups, 21 solely offered explanations unsupported by primary evidence, and 38 offered at least one explanation supported by primary evidence (appendix pp 37–43). 24 classifications of explanations emerged over five domains (appendix p 37), of which ten were unsupported by any of the included literature, seven had a mix of supporting and contradictory primary evidence, and seven were supported by primary evidence. The most common explanations with supporting evidence included increased prevalence of psychosis, increased perceived risk of violence, increased police contact, absence of or mistrust of general practitioners, and ethnic disadvantages. By contrast, frequently mentioned unsupported explanations for disparities in detention included higher comorbid drug use in BAME groups, language barriers, poorer detection of mental illness, and greater stigma than in majority groups.
Discussion
This review expands on previous research on the use of involuntary psychiatric detention in ethnic minority communities, through examination of both UK and international data. Black ethnic groups (black Caribbean, black African, and black, unspecified) were more likely to be involuntarily admitted to hospital compared with those of white ethnicity. Black Caribbean individuals also had an increased risk of readmission to hospital. South Asian groups had a significantly increased risk of involuntary admission, as did east Asian patients, although interpretation was restricted by small study numbers. Our observed associations between compulsory admission to hospital and ethnicity remained significant when restricted to studies we assessed as being of high ethnic specificity. Following restriction of analysis to studies with a high methodological quality rating, only the south Asian association became non-significant. This result could suggest that less methodologically sound studies drove the reported higher risk for detention in south Asian populations. By contrast, continued significance when examining only studies with high ethnic specificity (regardless of other methodological aspects) contradicts this result. We could draw the most confidence from studies of both high methodological quality and clarity and consistency of ethnic classification, but only seven studies met these criteria.
Both ethnically and culturally heterogeneous BAME, unspecified and migrant groups also had an increased risk of involuntary admission to hospital, which suggests that, although effect estimates were lower than some previous literature,1, 10 all minority populations in the countries studied, including migrants, are subject to increased risks of detention.
Publication date predicted an association between black Caribbean ethnicity and involuntary care, with more recent studies reporting lower effect estimates. This result might reflect more rigorous study designs in recent literature. UK-based studies also showed a higher risk of compulsory admission to hospital for black, unspecified groups compared with international literature. Despite our attempts to provide specific ethnic classifications, the high heterogeneity for all groups could also reflect this variation in the UK and internationally. However, this effect is difficult to disentangle because the international studies were few and typically lacked the specificity of ethnic classification more common to British studies, preventing further post-hoc examination across all groups. The proportion of women in the sample strengthened associations in black Caribbean, black, unspecified, and south Asian groups. However, whole sample proportions cannot adequately describe intersectional experiences of race and sex91 and future robust investigation is required. Data on readmission to hospital and length of stay were scarce, and socioeconomic and clinical moderators by ethnic group and involuntary status were infrequently reported, preventing meaningful investigation.
Of the 71 papers included in our systematic review, 34 (48%) offered no explanation for the variation in risk of detention among minority groups, or solely offered explanations without support from primary evidence. Untested explanations perpetuated in the literature largely dealt with lifestyle, cultural health beliefs, clinical characteristics, and demographic-bound assumptions of minority ethnic groups (eg, more drug use and greater community stigma of mental illness). Such untested hypotheses are of little use and are problematic when applied to aggregated and non-specific ethnic groupings, which often contain populations with varying lifestyles, health beliefs, culture, religion, and other demographic variables. Application of assumptions to combined groups, which fail to consider intersectionality in the perpetuation of risk,92, 93 precludes further inquiry into the range of risks to which these groups are subject. Likewise, explanations with supporting evidence, such as increased rates of psychoses in minority groups, require close examination. Psychosis alone is not a criterion for detention under the MHA, therefore the prevalence of psychoses in BAME communities is insufficient to explain ethnic inequalities in detention. The excess of detentions in BAME groups also applies to readmissions and not just those presenting with a first episode, so might be a function of the care experienced by those with established psychoses. Differences leading to mental illness trajectories that result in detention, such as perceived risk of violence, also warrant further investigation.23, 64
This study has several limitations. First, included studies examined psychiatric hospitalisation only. This investigation provides a good basis for examining inequalities in psychiatric care, but ethnic differences in other psychiatric contexts should also be examined through robust research. Additionally, the insufficient data on other aspects of care provided in most studies and the pooling of data in a meta-analysis cannot provide the necessary detail on the nature of differences in admissions, both for compulsory detention and treatment where the patient agrees to care. Coercive non-formal admissions can also happen, and perceived coercion can substantially affect a patient's experience of care.94 Furthermore, both civil and forensic commitment were combined in the analysis. This strategy allowed a broader inclusion of literature, but important differences between the two forms of compulsory hospital admission could have been missed. Similarly, important differences in legal systems in the different countries included in this systematic review should not be ignored. However, we believe that providing international data on ethnic disparity gives a clearer picture of the shortcomings of present research in tackling a global problem.
To our knowledge, this systematic review and meta-analysis is the most comprehensive to date on ethnicity and involuntary psychiatric hospitalisation, integrating international comparisons and psychiatric detention of migrants. However, a substantial portion of the literature presented lacked the methodological quality to allow us to draw mechanistic or causal inferences from it. The included studies provide restricted information on socioeconomic, cultural, and structural determinants of detention, and integration of data on detention with such factors is an important area for further research. Retention of untested explanations in the studies covered by this systematic review might serve to entrench narratives of racial determinism and contribute little to a fuller understanding of the range of inequalities faced by minority ethnic groups who come into contact with psychiatric services. Research should prioritise longitudinal study designs that can investigate clinical, socioeconomic, and demographic contributions, and avoid simple techniques to analyse complicated problems95—ethnicity is a complex construct that comprises multiple interacting variables. Research should also integrate qualitative assessment of service provider biases, group level stigma, or patient mistrust of health-care services to gain a thorough understanding of individual patient experience. Decision-making processes in psychiatric detention, which exclude patient and family input to risk management,96 should also be examined because their interaction with situational factors, such as available alternative treatment and under-resourced services,97 might reflect area deprivation experienced by BAME communities.
Panel. Lived experience commentary.
Steve Gilbert: “Reading the research presented in this systematic review makes it clear that although research has been done with the best of intentions and hopes for change, it has not been adequately rooted in the people it is trying to help. Attempts to highlight injustices have backfired and given ammunition to those people who are not willing to stop and think—we have left our research too open to interpretation. We need to be asking different questions when considering study design—that is, we should seek not just to say what the state of play is, but also why the state of play is how it is. Another key question is, who is doing the research? Research can and should be done by a range of people who have followed different trajectories. Relevant to ethnicity and compulsory detention, experience of the criminal justice system, ethnic discrimination, or low-income households will positively contribute to the conclusions drawn. Furthermore, the methodology of research to date has felt distant—it does not reflect real experience. Data are good and useful to contribute to a fuller understanding, but have we become entrenched in the data? It is wrong to assume that if data say something is true then it must be true?”
This meta-analysis showed that all minority populations studied were subject to an increased risk of involuntary psychiatric detention. We are no closer to understanding or effectively addressing these ethnic inequalities in psychiatric care. Only research committed to well-designed longitudinal studies and multisectoral, intersectional approaches will be able to untangle the causes of this health-care inequality.
Acknowledgments
Acknowledgments
This paper is based on independent research and was written in collaboration with the National Institute for Health Research Mental Health Policy Research Unit. Steve Gilbert is a member of the Mental Health Act review working group, and provided a statement to acompany this study. SS is a committee member for the Independent Mental Health Act Review, chaired by Professor Sir Simon Wessely, and was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. PB attests that all listed authors meet authorship criteria and no others meeting authorship criteria have been omitted. SP was supported by funding from the University College London Hospitals NIHR Biomedical Research Centre. KB is supported by the NIHR Collaboration for Leadership in Applied Health Research and Care North Thames at Bart's Health NHS Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or its arm's length bodies, and other Government Departments.
Contributors
SS was responsible for the original study proposal. SS, RG, and HM drafted the original protocol. SP, HM, and PB revised the proposal. PB, HG, KA, and EM independently screened papers and extracted data. HM acted as a senior reviewer in case of disagreement. HM and PB wrote the statistical analysis plan and did the statistical analysis. PB wrote the initial draft of the manuscript. SP, SS, KB, and KH provided content expertise, methodological guidance, and interpreted the findings in the context of the wider literature. All authors contributed to consecutive drafts and approved the final manuscript.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Bhui K, Stansfeld S, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and use of specialist mental health services in the UK: systematic review. Br J Psychiatry. 2003;182:105–116. doi: 10.1192/bjp.182.2.105. [DOI] [PubMed] [Google Scholar]
- 2.Singh S, Burns T, Tyrer P, Islam Z, Parsons H, Crawford M. Ethnicity as a predictor of detention under the Mental Health Act. Psychol Med. 2014;44:997–1004. doi: 10.1017/S003329171300086X. [DOI] [PubMed] [Google Scholar]
- 3.Singh S, Islam Z, Brown L, Gajwani R, Rubina J, Rabiee F. Ethnicity, detention and early intervention: reducing inequalities and improving outcomes for black and minority ethnic patients: the ENRICH programme, a mixed-methods study. In: Programme Grants for Applied Research. NIHR Journals Library; Southampton: 2013. [PubMed] [Google Scholar]
- 4.Bebbington P, Feeney S, Flannigan C, Glover GR, Lewis S, Wing J. Inner London collaborative audit of admissions in two health districts: II: Ethnicity and the use of the Mental Health Act. Br J Psychiatry. 1994;165:743–749. doi: 10.1192/bjp.165.6.743. [DOI] [PubMed] [Google Scholar]
- 5.Gajwani R, Parsons H, Birchwood M, Singh SP. Ethnicity and detention: are black and minority ethnic (BME) groups disproportionately detained under the Mental Health Act 2007? Soc Psychiatry Psychiatr Epidemiol. 2016;51:703–711. doi: 10.1007/s00127-016-1181-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohan R, McCrone P, Szmukler G, Micali N, Afuwape S, Thornicroft G. Ethnic differences in mental health service use among patients with psychotic disorders. Soc Psychiatry Psychiatr Epidemiol. 2006;41:771–776. doi: 10.1007/s00127-006-0094-7. [DOI] [PubMed] [Google Scholar]
- 7.Priebe S, Katsakou C, Amos T. Patients' views and readmissions 1 year after involuntary hospitalisation. Br J Psychiatry. 2009;194:49–54. doi: 10.1192/bjp.bp.108.052266. [DOI] [PubMed] [Google Scholar]
- 8.Dannerbeck Janku A, Yan J. Exploring patterns of court-ordered mental health services for juvenile offenders: is there evidence of systemic bias? Crim Justice Behav. 2009;36:402–419. [Google Scholar]
- 9.Gupta S. Psychosis in migrants from the Indian subcontinent and English-born controls: a preliminary study on the use of psychiatric services. Br J Psychiatry. 1991;159:222–225. doi: 10.1192/bjp.159.2.222. [DOI] [PubMed] [Google Scholar]
- 10.Singh SP, Greenwood N, White S, Churchill R. Ethnicity and the mental health act 1983. Br J Psychiatry. 2007;191:99–105. doi: 10.1192/bjp.bp.106.030346. [DOI] [PubMed] [Google Scholar]
- 11.Bhui K, Brown P, Hardie T, Watson JP, Parrott J. African-Caribbean men remanded to Brixton Prison. Psychiatric and forensic characteristics and outcome of final court appearance. Br J Psychiatry. 1998;172:337–344. doi: 10.1192/bjp.172.4.337. [DOI] [PubMed] [Google Scholar]
- 12.Corrigall R, Bhugra D. The role of ethnicity and diagnosis in rates of adolescent psychiatric admission and compulsory detention: a longitudinal case-note study. J R Soc Med. 2013;106:190–195. doi: 10.1177/0141076813480995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali S, Dearman S, McWilliam C. Are Asians at greater risk of compulsory psychiatric admission than Caucasians in the acute general adult setting? Med Sci Law. 2007;47:311–314. doi: 10.1258/rsmmsl.47.4.311. [DOI] [PubMed] [Google Scholar]
- 14.Audini B, Lelliott P. Age, gender and ethnicity of those detained under Part II of the Mental Health Act 1983. Br J Psychiatry. 2002;180:222–226. doi: 10.1192/bjp.180.3.222. [DOI] [PubMed] [Google Scholar]
- 15.Alegría M, Canino G, Ríos R. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatr Serv. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- 16.Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med. 2011;41:897–910. doi: 10.1017/S0033291710001406. [DOI] [PubMed] [Google Scholar]
- 17.Missinne S, Bracke P. Depressive symptoms among immigrants and ethnic minorities: a population based study in 23 European countries. Soc Psychiatry Psychiatr Epidemiol. 2012;47:97–109. doi: 10.1007/s00127-010-0321-0. [DOI] [PubMed] [Google Scholar]
- 18.Bhugra D, Corridan B, Rudge S, Leff J, Mallett R. Early manifestations, personality traits and pathways into care for Asian and white first-onset cases of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 1999;34:595–599. doi: 10.1007/s001270050180. [DOI] [PubMed] [Google Scholar]
- 19.Cochrane R, Sashidharan SP. Mental health and ethnic minorities: a review of the literature and implications for services. February, 1995. http://www.brown.uk.com/brownlibrary/ETHMENT.htm
- 20.McKenzie K, Bhui K. Institutional racism in mental health care. BMJ. 2007;334:649. doi: 10.1136/bmj.39163.395972.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paradies Y, Truong M, Priest N. A systematic review of the extent and measurement of healthcare provider racism. J Gen Intern Med. 2014;29:364–387. doi: 10.1007/s11606-013-2583-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lay B, Lauber C, Rössler W. Are immigrants at a disadvantage in psychiatric in-patient care? Acta Psychiatr Scand. 2005;111:358–366. doi: 10.1111/j.1600-0447.2004.00509.x. [DOI] [PubMed] [Google Scholar]
- 23.Mulder CL, Koopmans GT, Selten JP. Emergency psychiatry, compulsory admissions and clinical presentation among immigrants to the Netherlands. Br J Psychiatry. 2006;188:386–391. doi: 10.1192/bjp.188.4.386. [DOI] [PubMed] [Google Scholar]
- 24.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48. [Google Scholar]
- 25.Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Heritage Foundation for Medical Research; Edmonton: 2004. [Google Scholar]
- 26.Raine R. Does gender bias exist in the use of specialist health care? J Health Serv Res Policy. 2000;5:237–249. doi: 10.1177/135581960000500409. [DOI] [PubMed] [Google Scholar]
- 27.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Afuwape SA, Johnson S, Craig TJK. Ethnic differences among a community cohort of individuals with dual diagnosis in South London. J Ment Health. 2006;15:551–567. [Google Scholar]
- 31.Agius M, Shah S, Ramkisson R, Persaud A, Murphy S, Zaman R. Three year outcomes in an early intervention service for psychosis in a multicultural and multiethnic population. Psychiatr Danub. 2008;20:494–499. [PubMed] [Google Scholar]
- 32.Ajnakina O, Lally J, Di Forti M. Patterns of illness and care over the 5 years following onset of psychosis in different ethnic groups; the GAP-5 study. Soc Psychiatry Psychiatr Epidemiol. 2017;52:1101–1111. doi: 10.1007/s00127-017-1417-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Archie S, Akhtar-Danesh N, Norman R, Malla A, Roy P, Zipursky RB. Ethnic diversity and pathways to care for a first episode of psychosis in Ontario. Schizophr Bull. 2010;36:688–701. doi: 10.1093/schbul/sbn137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Balducci PM, Bernardini F, Pauselli L, Tortorella A, Compton MT. Correlates of involuntary admission: findings from an Italian inpatient psychiatric unit. Psychiatr Danub. 2017;29:490–496. doi: 10.24869/psyd.2017.490. [DOI] [PubMed] [Google Scholar]
- 35.Bansal N, Bhopal R, Netto G, Lyons D, Steiner MF, Sashidharan SP. Disparate patterns of hospitalisation reflect unmet needs and persistent ethnic inequalities in mental health care: the Scottish health and ethnicity linkage study. Ethn Health. 2014;19:217–239. doi: 10.1080/13557858.2013.814764. [DOI] [PubMed] [Google Scholar]
- 36.Borschmann RD, Gillard S, Turner K, Lovell K, Goodrich-Purnell N, Chambers M. Demographic and referral patterns of people detained under Section 136 of the Mental Health Act (1983) in a south London Mental Health Trust from 2005 to 2008. Med Sci Law. 2010;50:15–18. doi: 10.1258/msl.2009.009003. [DOI] [PubMed] [Google Scholar]
- 37.Bowers L, Jones J, Simpson A. The demography of nurses and patients on acute psychiatric wards in England. J Clin Nurs. 2009;18:884–892. doi: 10.1111/j.1365-2702.2008.02362.x. [DOI] [PubMed] [Google Scholar]
- 38.Burnett R, Mallett R, Bhugra D, Hutchinson G, Der G, Leff J. The first contact of patients with schizophrenia with psychiatric services: social factors and pathways to care in a multi-ethnic population. Psychol Med. 1999;29:475–483. doi: 10.1017/s0033291798008125. [DOI] [PubMed] [Google Scholar]
- 39.Callan AF. Schizophrenia in Afro-Caribbean immigrants. J R Soc Med. 1996;89:253–256. doi: 10.1177/014107689608900505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coid J, Kahtan N, Gault S, Jarman B. Ethnic differences in admissions to secure forensic psychiatry services. Br J Psychiatry. 2000;177:241–247. doi: 10.1192/bjp.177.3.241. [DOI] [PubMed] [Google Scholar]
- 41.Cole E, Leavey G, King M, Johnson-Sabine E, Hoar A. Pathways to care for patients with a first episode of psychosis: A comparison of ethnic groups. Br J Psychiatry. 1995;167:770–776. doi: 10.1192/bjp.167.6.770. [DOI] [PubMed] [Google Scholar]
- 42.Commander MJ, Cochrane R, Sashidharan SP, Akilu F, Wildsmith E. Mental health care for Asian, black and white patients with non-affective psychoses: pathways to the psychiatric hospital, in-patient and after-care. Soc Psychiatry Psychiatr Epidemiol. 1999;34:484–491. doi: 10.1007/s001270050224. [DOI] [PubMed] [Google Scholar]
- 43.Cope R, Ndegwa D. Ethnic differences in admission to a regional secure unit. J Forens Psychiatry Psychol. 1990;1:365–378. [Google Scholar]
- 44.Crowley JJ, Simmons S. Mental health, race and ethnicity: a retrospective study of the care of ethnic minorities and whites in a psychiatric unit. J Adv Nurs. 1992;17:1078–1087. doi: 10.1111/j.1365-2648.1992.tb02042.x. [DOI] [PubMed] [Google Scholar]
- 45.Curley A, Agada E, Emechebe A. Exploring and explaining involuntary care: the relationship between psychiatric admission status, gender and other demographic and clinical variables. Int J Law Psychiatry. 2016;47:53–59. doi: 10.1016/j.ijlp.2016.02.034. [DOI] [PubMed] [Google Scholar]
- 46.Davies S, Thornicroft G, Leese M, Higgingbotham A, Phelan M. Ethnic differences in risk of compulsory psychiatric admission among representative cases of psychosis in London. BMJ. 1996;312:533–537. doi: 10.1136/bmj.312.7030.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.de Wit MA, Tuinebreijer WC, van Brussel GH, Selten JP. Ethnic differences in risk of acute compulsory admission in Amsterdam, 1996–2005. Soc Psychiatry Psychiatr Epidemiol. 2012;47:111–118. doi: 10.1007/s00127-010-0312-1. [DOI] [PubMed] [Google Scholar]
- 48.Dunn J, Fahy TA. Police admissions to a psychiatric hospital. Demographic and clinical differences between ethnic groups. Br J Psychiatry. 1990;156:373–378. doi: 10.1192/bjp.156.3.373. [DOI] [PubMed] [Google Scholar]
- 49.Fassaert T, Heijnen H, de Wit MA, Peen J, Beekman AT, Dekker J. The association between ethnic background and characteristics of first mental health treatment for psychotic disorders in the Netherlands between 2001 and 2005. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1591–1601. doi: 10.1007/s00127-016-1248-x. [DOI] [PubMed] [Google Scholar]
- 50.Goater N, King M, Cole E. Ethnicity and outcome of psychosis. Br J Psychiatry. 1999;175:34–42. doi: 10.1192/bjp.175.1.34. [DOI] [PubMed] [Google Scholar]
- 51.Gray Houston K, Mariotto M, Hays JR. Outcomes for psychiatric patients following first admission: relationships with voluntary and involuntary treatment and ethnicity. Psychol Rep. 2001;88:1012–1014. doi: 10.2466/pr0.2001.88.3c.1012. [DOI] [PubMed] [Google Scholar]
- 52.Hamilton JE, Heads AM, Cho RY, Lane SD, Soares JC. Racial disparities during admission to an academic psychiatric hospital in a large urban area. Compr Psychiatry. 2015;63:113–122. doi: 10.1016/j.comppsych.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 53.Harrison G, Ineichen B, Smith J, Morgan HG. Psychiatric hospital admissions in Bristol: II. Social and clinical aspects of compulsory admission. Br J Psychiatry. 1984;145:605–611. doi: 10.1192/bjp.145.6.605. [DOI] [PubMed] [Google Scholar]
- 54.Ineichen B, Harrison G, Morgan HG. Psychiatric hospital admissions in Bristol: I. Geographical and ethnic factors. Br J Psychiatry. 1984;145:600–604. doi: 10.1192/bjp.145.6.600. [DOI] [PubMed] [Google Scholar]
- 55.Iversen VC, Morken G. Acute admissions among immigrants and asylum seekers to a psychiatric hospital in Norway. Soc Psychiatry Psychiatr Epidemiol. 2003;38:515–519. doi: 10.1007/s00127-003-0664-x. [DOI] [PubMed] [Google Scholar]
- 56.Johnson S, Leese M, Brooks L. Frequency and predictors of adverse events. PRiSM psychosis study 3. Br J Psychiatry. 1998;173:376–384. doi: 10.1192/bjp.173.5.376. [DOI] [PubMed] [Google Scholar]
- 57.Kelly BD, Emechebe A, Anamdi C, Duffy R, Murphy N, Rock C. Custody, care and country of origin: demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatry. 2015;38:1–7. doi: 10.1016/j.ijlp.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 58.Kilbourne AM, Bauer MS, Pincus H. Clinical, psychosocial, and treatment differences in minority patients with bipolar disorder. Bipolar Disord. 2005;7:89–97. doi: 10.1111/j.1399-5618.2004.00161.x. [DOI] [PubMed] [Google Scholar]
- 59.Koffman J, Fulop NJ, Pashley D, Coleman K. Ethnicity and use of acute psychiatric beds: one-day survey in North and South Thames regions. Br J Psychiatry. 1997;171:238–241. doi: 10.1192/bjp.171.3.238. [DOI] [PubMed] [Google Scholar]
- 60.Lawlor C, Johnson S, Cole L, Howard LM. Ethnic variations in pathways to acute care and compulsory detention for women experiencing a mental health crisis. Int J Soc Psychiatry. 2012;58:3–15. doi: 10.1177/0020764010382369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Law-Min R, Oyebode F, Haque MS. First compulsory admissions under part II of the Mental Health Act 1983: a retrospective five-year study. Med Sci Law. 2003;43:248–254. doi: 10.1258/rsmmsl.43.3.248. [DOI] [PubMed] [Google Scholar]
- 62.Lay B, Nordt C, Rössler W. Variation in use of coercive measures in psychiatric hospitals. Eur Psychiatry. 2011;26:244–251. doi: 10.1016/j.eurpsy.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 63.Lindsey KP, Paul GL, Mariotto MJ. Urban psychiatric commitments: disability and dangerous behavior of black and white recent admissions. Hosp Community Psychiatry. 1989;40:286–294. doi: 10.1176/ps.40.3.286. [DOI] [PubMed] [Google Scholar]
- 64.Lloyd K, Moodley P. Psychotropic medication and ethnicity: an inpatient survey. Soc Psychiatry Psychiatr Epidemiol. 1992;27:95–101. doi: 10.1007/BF00788512. [DOI] [PubMed] [Google Scholar]
- 65.Mann F, Fisher HL, Major B. Ethnic variations in compulsory detention and hospital admission for psychosis across four UK Early Intervention Services. BMC Psychiatry. 2014;14:256. doi: 10.1186/s12888-014-0256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McGovern D, Hemmings P, Cope R, Lowerson A. Long-term follow-up of young Afro-Caribbean Britons and white Britons with a first admission diagnosis of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 1994;29:8–19. doi: 10.1007/BF00796443. [DOI] [PubMed] [Google Scholar]
- 67.McKenzie K, van Os J, Fahy T. Psychosis with good prognosis in Afro-Caribbean people now living in the United Kingdom. BMJ. 1995;311:1325–1328. doi: 10.1136/bmj.311.7016.1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Moodley P, Perkins RE. Routes to psychiatric inpatient care in an Inner London Borough. Soc Psychiatry Psychiatr Epidemiol. 1991;26:47–51. doi: 10.1007/BF00783581. [DOI] [PubMed] [Google Scholar]
- 69.Morgan C, Mallett R, Hutchinson G. Pathways to care and ethnicity. 1: sample characteristics and compulsory admission. Report from the AESOP study. Br J Psychiatry. 2005;186:281–289. doi: 10.1192/bjp.186.4.281. [DOI] [PubMed] [Google Scholar]
- 70.Norredam M, Garcia-Lopez A, Keiding N, Krasnik A. Excess use of coercive measures in psychiatry among migrants compared with native Danes. Acta Psychiatr Scand. 2010;121:143–151. doi: 10.1111/j.1600-0447.2009.01418.x. [DOI] [PubMed] [Google Scholar]
- 71.Oluwatayo O, Gater R. The role of engagement with services in compulsory admission of African/Caribbean patients. Soc Psychiatry Psychiatr Epidemiol. 2004;39:739–743. doi: 10.1007/s00127-004-0794-9. [DOI] [PubMed] [Google Scholar]
- 72.Owens D, Harrison G, Boot D. Ethnic factors in voluntary and compulsory admissions. Psychol Med. 1991;21:185–196. doi: 10.1017/s003329170001477x. [DOI] [PubMed] [Google Scholar]
- 73.Parkman S, Davies S, Leese M, Phelan M, Thornicroft G. Ethnic differences in satisfaction with mental health services among representative people with psychosis in South London: PRiSM study 4. Br J Psychiatry. 1997;171:260–264. doi: 10.1192/bjp.171.3.260. [DOI] [PubMed] [Google Scholar]
- 74.Perez-Rodriguez MM, Baca-Garcia E, Quintero-Gutierrez FJ. Demand for psychiatric emergency services and immigration. Findings in a Spanish hospital during the year 2003. Eur J Public Health. 2006;16:383–387. doi: 10.1093/eurpub/ckl021. [DOI] [PubMed] [Google Scholar]
- 75.Reeves S, Stewart R, Howard R. Service contact and psychopathy in very-late-onset schizophrenia-like psychosis: the effects of gender and ethnicity. Int J Geriatr Psychiatry. 2002;17:473–479. doi: 10.1002/gps.614. [DOI] [PubMed] [Google Scholar]
- 76.Rotenberg M, Tuck A, Ptashny R, McKenzie K. The role of ethnicity in pathways to emergency psychiatric services for clients with psychosis. BMC Psychiatry. 2017;17:137. doi: 10.1186/s12888-017-1285-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Selten JP, Sijben N. First admission rates for schizophrenia in immigrants to the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 1994;29:71–77. doi: 10.1007/BF00805625. [DOI] [PubMed] [Google Scholar]
- 78.Singh SP, Croudace T, Beck A, Harrison G. Perceived ethnicity and the risk of compulsory admission. Soc Psychiatry Psychiatr Epidemiol. 1998;33:39–44. doi: 10.1007/s001270050020. [DOI] [PubMed] [Google Scholar]
- 79.Singh SP, Brown L, Winsper C. Ethnicity and pathways to care during first episode psychosis: the role of cultural illness attributions. BMC Psychiatry. 2015;15:287. doi: 10.1186/s12888-015-0665-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sohler NL, Bromet EJ, Lavelle J, Craig TJ, Mojtabai R. Are there racial differences in the way patients with psychotic disorders are treated at their first hospitalization? Psychol Med. 2004;34:705–718. doi: 10.1017/S0033291703001363. [DOI] [PubMed] [Google Scholar]
- 81.Spinogatti F, Civenti G, Conti V, Lora A. Ethnic differences in the utilization of mental health services in Lombardy (Italy): an epidemiological analysis. Soc Psychiatry Psychiatr Epidemiol. 2015;50:59–65. doi: 10.1007/s00127-014-0922-0. [DOI] [PubMed] [Google Scholar]
- 82.Takei N, Persaud R, Woodruff P, Brockington I, Murray RM. First episodes of psychosis in Afro-Caribbean and white people. An 18-year follow-up population-based study. Br J Psychiatry. 1998;172:147–153. doi: 10.1192/bjp.172.2.147. [DOI] [PubMed] [Google Scholar]
- 83.Tarsitani L, Pasquini M, Maraone A. Acute psychiatric treatment and the use of physical restraint in first-generation immigrants in Italy: a prospective concurrent study. Int J Soc Psychiatry. 2013;59:613–618. doi: 10.1177/0020764012450985. [DOI] [PubMed] [Google Scholar]
- 84.Thomas CS, Stone K, Osborn M, Thomas PF, Fisher M. Psychiatric morbidity and compulsory admission among UK-born Europeans, Afro-Caribbeans and Asians in Central Manchester. Br J Psychiatry. 1993;163:91–99. doi: 10.1192/bjp.163.1.91. [DOI] [PubMed] [Google Scholar]
- 85.Thornicroft G, Davies S, Leese M. Health service research and forensic psychiatry: a black and white case. Int Rev Psychiatry. 1999;11:250–257. [Google Scholar]
- 86.Tolmac J, Hodes M. Ethnic variation among adolescent psychiatric in-patients with psychotic disorders. Br J Psychiatry. 2004;184:428–431. doi: 10.1192/bjp.184.5.428. [DOI] [PubMed] [Google Scholar]
- 87.Webber M, Huxley P. Social exclusion and risk of emergency compulsory admission. A case-control study. Soc Psychiatry Psychiatr Epidemiol. 2004;39:1000–1009. doi: 10.1007/s00127-004-0836-3. [DOI] [PubMed] [Google Scholar]
- 88.Weich S, McBride O, Twigg L. Variation in compulsory psychiatric inpatient admission in England: a cross-classified, multilevel analysis. Lancet Psychiatry. 2017;4:619–626. doi: 10.1016/S2215-0366(17)30207-9. [DOI] [PubMed] [Google Scholar]
- 89.Wheeler A, Robinson E, Robinson G. Admissions to acute psychiatric inpatient services in Auckland, New Zealand: a demographic and diagnostic review. N Z Med J. 2005;118:U1752. [PubMed] [Google Scholar]
- 90.Johnson S, Craig TJK, Miles H, Leese M, Mohan R, Thornicroft G. Ethnic differences among a community cohort of individuals with dual diagnosis in South London. J Ment Health. 2006;15:551–567. [Google Scholar]
- 91.Crenshaw K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum. 1989;1989:139–167. [Google Scholar]
- 92.Hankivsky O, Cormier R, De Merich D. Intersectionality: moving women's health research and policy forward. Women's Health Research Network; Vancouver: 2009. [Google Scholar]
- 93.Livingston JD. Experiences of stigma and compulsory treatment in the forensic and civil mental health systems of British Columbia. 2010. summit.sfu.ca/system/files/iritems1/11443/etd6262_JLivingston.pdf
- 94.Poythress NG, Petrila J, McGaha A, Boothroyd R. Perceived coercion and procedural justice in the Broward mental health court. Int J Law Psychiatry. 2002;25:517–533. doi: 10.1016/s0160-2527(01)00110-8. [DOI] [PubMed] [Google Scholar]
- 95.Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 96.Coffey M, Cohen R, Faulkner A, Hannigan B, Simpson A, Barlow S. Ordinary risks and accepted fictions: how contrasting and competing priorities work in risk assessment and mental health care planning. Health Expect. 2017;20:471–483. doi: 10.1111/hex.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Quirk A, Lelliott P, Audini B, Buston K. Non-clinical and extra-legal influences on decisions about compulsory admission to psychiatric hospital. J Ment Health. 2003;12:119–130. doi: 10.1080/0963823031000103434. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.