Abstract
Background
Gastro laryngeal tube (GLT) is a newly introduced device. It is an advanced purpose specific design (essentially a modified laryngeal tube) which especially provides a separate wide channel specifically designed for the introduction of a gastroscope for endoscopic retrograde cholangio-pancreatography (ERCP), simultaneously functioning as a supra-glottic airway device for ventilation.
Methods
In a randomized controlled trial on 100 patients undergoing ERCP under GA, GLT was compared with endotracheal tube as an alternative airway device. Device insertion conditions, oxygenation and ventilation parameters were recorded.
Results
GLT was found to be comparable with ETT. Success rate of insertion of GLT was high (92%) and the insertion time of GLT was significantly shorter 42 (20–210) s vs. 206 (176–320) s – median (range). Both the devices were equally effective in normal oxygenation and ventilation. The recovery time was significantly shorter and postoperative complications such as hoarseness and dysphonia were less common in GLT group. Inserting conditions for the duodenoscope were better in GLT group.
Conclusion
In this study, likely to be first of its kind, it is concluded that the GLT is a suitable and better alternative to ETT as it allows adequate ventilation and is associated with faster recovery times and minimal extubation-related complications while enhancing operative conditions for gastroenterologists. Its regular use in patients undergoing ERCP is strongly recommended.
Keywords: Endoscopic retrograde cholangio-pancreatography, Gastro-laryngeal tube, Endotracheal intubation
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) in recent times is fast emerging as a therapeutic procedure rather than a diagnostic one, requiring anaesthetic support for successful completion of the procedure.1 The procedure can be uncomfortable especially due to prone positioning, multiple passages of endoscope, air insufflations, dilatation of ductal structures and prolonged duration which requires high degree of cooperation from patients. A large number of patients need to be given general anaesthesia (GA), in order to minimize incidence of adverse respiratory and haemodynamic events in the peri-procedure period. The advantage GA with endotracheal intubation (ETT) or supraglottic devices offers is the protection of the airway, reduced ERCP failure and complication rates.2, 3 However, ETT involves rigid laryngoscopy with consequent undesirable haemodynamic responses4 and use of neuromuscular blocking drugs. It also has the disadvantage of a longer recovery time5 and possibility of injury to the oro-pharynx at insertion.
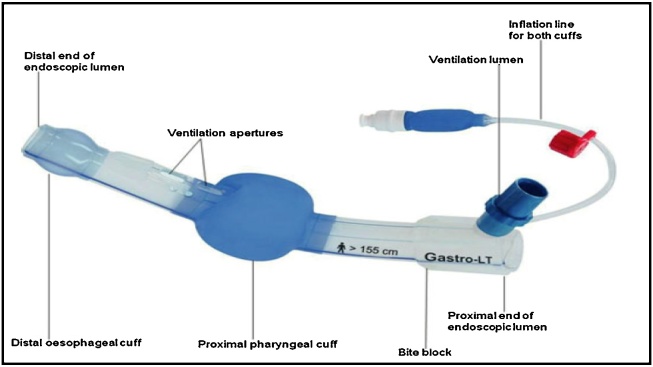
Gastro-laryngeal tube (GLT) is a supraglottic device specifically designed for ERCP and has been recently introduced in the clinical practice (Fig. 1). The GLT (VBM Medizintechnik GmbH, Sulz, Germany) is an advanced purpose specific design (essentially a modified laryngeal tube) which especially provides a separate wide channel for the introduction of a gastroscope, at the same instance acts as a supraglottic airway device for ventilation. Like the laryngeal tube design it incorporates two cuffs which are interconnected, high-volume, low-pressure, inflatable by a single channel. The proximal pharyngeal cuff acts as an oro-nasopharyngeal seal, which also serves to stabilize the tube; while the distal oesophageal cuff behaves like an oesophageal obturator, reducing the risk of pulmonary aspiration.6 The gastro laryngeal tube is available in only one size suitable for patients above 155 cm only and the 16 mm channel has an integrated bite block to protect the gastroscope.
Fig. 1.
Gastro laryngeal tube.
The use of GLT in ERCP was described recently in small groups of patients with encouraging results with many advantages.7, 8 Use of a supraglottic airway device not only maintains a patent airway, it has the undeniable benefit of airway protection during ERCP, at the same time avoiding disadvantages associated with tracheal intubation. With the hypothesis that use of GLT will improve conditions for the procedure and patient and reduce complications, this study was designed as a randomized controlled trial to compare GLT as an alternative airway device vs. the gold standard - ETT for airway management, in patients undergoing ERCP under GA.
Materials and methods
The study was designed as a prospective randomized controlled pilot study from Jan 2013 till Feb 2015. It was a single blind study, where the patients were blinded to the device which was used during their procedure. The sample size was chosen on the basis of the average annual work load of ERCP in the centre since a review of literature did not reveal any study comparing the two techniques. Patients in ASA physical status grade I and II of either sex with Mallampati classification I or II, aged 18–75 years and a height more than 155 cm were included in the study. Patients with anticipated difficult airway, restricted head and neck mobility, gross morphological abnormalities of head and neck, pulmonary disease (Respiratory tract disease or Restrictive lung disease), increased risk of aspiration (hiatus hernia, gastro-oesophageal reflux disease, as well as pregnant patients) were excluded from the study.
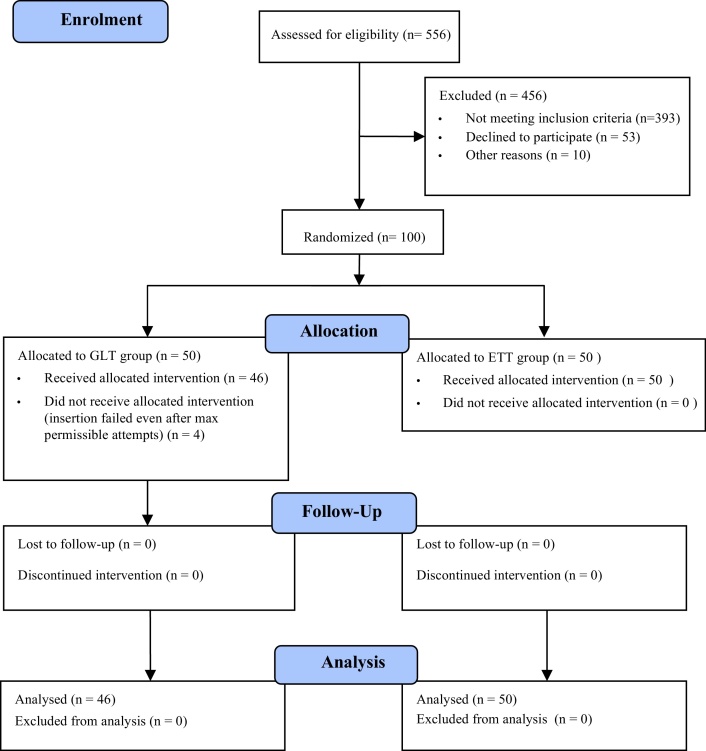
Ethics committee clearance was obtained and 556 patients were prospectively enrolled for the study. 393 patients who did not meet the inclusion criteria were excluded. A further 53 patients who declined to participate in the study and 10 who had uncertain procedure duration or gave history of adverse events such as haemodynamic instability or severe nausea and vomiting during previous GA were also excluded. Written informed consent was taken from the patients after counselling and the study was carried out on the remaining 100 patients scheduled for ERCP under GA (Fig. 2).
Fig. 2.
CONSORT flow diagram of the study.
Random allocation of the patients to the groups GLT or ETT each having 50 patients, was done by simple randomization. Patients were asked to randomly pick up sealed opaque envelopes which had generated numbers either 1 or 2, which assigned them to either of the two groups. The Group GLT had patients who had gastro-laryngeal tube inserted while in the second group named as Group ETT, patients were intubated with endotracheal tube of appropriate size. All the patients received premedication with Glycopyrrolate 0.2 mg and Ondansetron 4 mg intravenously (IV) 30 min prior to procedure. Patients were pre-oxygenated for 3–4 min before induction of GA with Fentanyl (up to 2 μg/kg) and Propofol (2–3 mg/kg) till loss of eye lash reflex. ETT was inserted 60–90 s after administration of 2 mg/kg of Inj. Suxamethonium, while no muscle relaxants were used for GLT insertion. After securing the airway device, patients in GLT group were allowed to breathe spontaneously a mixture of oxygen and air, and only where necessary assisted manual ventilation was provided. While in ETT group patients were paralyzed subsequently with Atracurium (0.5–0.6 mg/kg) intermittently and kept on controlled ventilation. A continuous infusion of Propofol at 100–150 μg/kg/min was used to maintain the depth of anaesthesia.
In GLT group, the GLT was introduced while the patient was in supine position and it was fixed in the midline. Both balloons of the GLT were inflated through the single inflation channel using air till the intra-balloon pressure reached 80 cmH2O as measured by a cuff pressure manometer. The Inflate/deflate valve was then opened to release the pressure gradually till 60 cmH2O. In ETT group, an appropriate size (7.5–8.5 mm) ETT was placed after laryngoscopy. Observation of bilaterally equal chest movement, auscultation of breath sounds, negative gastric insufflation and the appearance of a satisfactory capnogram waveform confirmed the proper placement of the airway devices. An expired tidal volume of at least 7–8 ml/kg during gentle manual ventilation was the benchmark selected for confirming effective and adequate airway. A maximum of three attempts at insertion were permitted and the number attempts of insertion were recorded. The insertion time – defined as time interval between Propofol administration and obtaining a satisfactory capnograph was also recorded.
Successful insertion of GLT/ETT was confirmed after which the patients were placed in prone position with the head rotated to the right lateral position and again the GLT/ETT was re-assessed for any dislodgement during the manoeuvre.
The outcome parameters assessed were:
- Primary outcome: patient parameters
-
•During the procedure (5 min intervals)
-
-Peak airway pressure (PAP)
-
-Exhaled tidal volume (ETV)
-
-End tidal CO2
-
-
-
•After termination of procedure. Patients in both groups were interviewed in the post-anaesthesia care unit for:
-
-Sore throat,
-
-Dysphonia,
-
-Trauma to the airway (assessed by presence of blood staining on GLT/ETT)
-
-
- Secondary outcome: procedure parameters
-
•Ease of insertion
-
•Number of insertion attempts for GLT
-
•Oro-pharyngeal leak pressure (in GLT group only)
-
•Recovery time
-
•
In addition, in GLT group oropharyngeal leak pressure (OLP) was ascertained by completely closing the expiratory valve of the circle system with a fixed gas flow of 3 l/min and noting the airway pressure at which the pressure in the circuit stabilized. ERCP was carried out with a 13.8-mm duodenoscope (Fig. 3). During and after termination of the procedure, response of the gastroenterologists was taken regarding inserting conditions for the Gastroenterologist, scope manoeuvrability and any other relevant observations made by them. These were graded according to the criteria as in Table 1.
Fig. 3.
Patient in prone position with GLT in situ and gastroduodenoscopein the channel.
Table 1.
Grades of difficulty.
| Description of insertion | Scope inserting conditions |
|---|---|
| Duodenoscope – easily inserted without any resistance. Scope manoeuvrability – good without any resistance. |
Excellent |
| Duodenoscope – inserted with slight resistance. Scope manoeuvrability – restricted but possible. |
Good |
| Duodenoscope – requires forceful insertion. Scope manoeuvrability – restricted requires adjustments. |
Poor |
| Duodenoscope – could not be inserted at all forcing change of airway device. | Impossible |
Statistical analysis
Statistical analysis was done using SPSS (Statistical Package for Social Sciences) Version 22.0 statistical Analysis Software. Continuous data between study groups was compared using Mann Whitney U test since the distribution of the data was not normal. Results are expressed as the medians and range, or numbers and percentages using unpaired t tests, whereas categorical data was compared using the chi-squared test or Fisher's exact test as appropriate. p value < 0.05 was considered to be significant.
Results
There was no significant difference between the groups with respect to age and sex (p-value > 0.05) while there was a significant difference in height between the groups (p-value < 0.05), however height as a variable is unlikely to affect the outcomes of the study. Various study parameters have been depicted in Table 2, Table 3. All the patients in ETT group could be successfully intubated. However, in GLT group, successful insertion was possible in 46 (92%) cases while in remaining 4 (8%) patients, it was not possible to insert the device satisfactorily despite maximum number of attempts allowed. Hence, these were excluded from further data analysis. ETT was successfully inserted in first attempt in 46 (92%) patients while GLT was successfully inserted in first attempt in 39 (84.78%) patients. 3 (6%) and 7 (15.22%) patients required more than one insertion attempt in ETT and GLT respectively, however this difference was not significant between the study groups (p-value > 0.05).
Table 2.
Demographic & study parameters.
| Groups | ETT Median (range) |
GLT Median (range) |
p-Value |
|---|---|---|---|
| Parameters | |||
| Age (yrs) | 51.5 (19–84) | 54 (21–75) | 0.3987 |
| Height (cm) | 161.5 (150–182) | 168.50 (152–182) | 0.0363 |
| Weight (kg) | 57.00 (35–80) | 60.00 (44–75) | 0.1091 |
| Insertion time (s) | 206 (176–320) | 42 (20–210) | <0.0001 |
| Procedure time (min) | 47 (22–77) | 50.5 (22–82) | 0.2079 |
| Recovery time (s) | 443 (180–930) | 51 (10–192) | <0.0001 |
| Peak airway pressure (cm of H2O) | 24 (18–37) | 3 (2–7) | <0.0001 |
| Exhaled tidal volume (ml) | 520 (320–680) | 335 (220–540) | <0.0001 |
| End tidal CO2 (mm Hg) | 38 (33–48) | 41.5 (34–46) | 0.0103 |
Table 3.
Insertion attempts.
| Parameters | GLT no. (%)a | ETT no. (%) | p-Value |
|---|---|---|---|
| Insertion attempt 1 | 39 (84.78) | 47 (94) | 0.19b |
| Insertion attempt more than 1 | 7 (15.21) | 3 (6) |
4 cases excluded from the analysis in the GLT group.
Fisher Exact two tailed p-value.
The median insertion time (range) were noted as 206 (176–320) s and 42 (20–210) s in ETT and GLT groups respectively, there was a highly significant difference in mean insertion time between the study groups (p-value < 0.0001).
The median peak airway pressure (range) were noted as 24 (18–37) and 3 (2–7) cm of H2O in ETT and GLT groups respectively, there was a highly significant difference in mean peak airway pressure between the study groups (p-value < 0.0001).
The median exhaled tidal volume (range) were noted as 520 (320–680) and 335 (220–540) ml in ETT and GLT groups respectively, there was a highly significant difference in mean exhaled tidal volume between the study groups (p-value < 0.0001).
The median End tidal CO2 (range) were noted as 38 (33–48) and 41.5 (34–46) mm Hg in ETT and GLT groups respectively, there was a significant difference in mean End tidal CO2 between the study groups (p-value < 0.05), median End tidal CO2 was lower in ETT group however it was within normal range in both the groups.
The median recovery time (range) were noted as 443 (180–930) s and 51 (10–192) s in ETT and GLT groups respectively, there was a highly significant difference in mean recovery time between the study groups (p-value < 0.0001), the median recovery time was lower in GLT as compared to ETT group.
The median procedure time (range) were noted as 47 (22–77) and 50.5 (22–82) min in ETT and GLT groups respectively, there was no significant difference in mean procedure time between the study groups (p-value > 0.05).
The mean (SD) oro-pharyngeal leak pressure (which is a parameter relevant to supraglottic devices) of GLT was 32.7 (1.8) cm H2O, whereas the same was not recorded in the ETT group.
In the post anaesthesia care unit (PACU), patients were asked about various events 30 min after cessation of procedure (Table 4), there was no significant difference between the study groups with respect to occurrence of events like sore throat, dysphonia and blood in oral cavity (p-value > 0.05) whereas there was a significant difference between the study groups for occurrence of hoarseness (p-value < 0.05).
Table 4.
Post procedure complications.
| Groups parameters | GLT (n = 46) No. (%) |
ETT (n = 50) No. (%) |
p-Value |
|---|---|---|---|
| Sore throat | 18 (39.10) | 18 (36) | 0.92a |
| Hoarseness | 1 (2.20) | 12 (24) | 0.0047a |
| Dysphonia | 1 (2.20) | 4 (8) | 0.36b |
| Blood in oral cavity | 12 (26.10) | 6 (12) | 0.13a |
Yates corrected p-value.
Fisher Exact two tailed p-value.
The inserting conditions were found to be excellent in 84% and 97.82% patients in ETT and GLT study groups respectively and there was a significant difference between the study groups (p-value < 0.05). In both the groups however, the inserting conditions of the duodenoscope were never recorded to be poor or impossible (Table 5).
Table 5.
Inserting conditions for the gastroenterologist.
| Group Difficulty level |
GLT No. (%) |
ETT No. (%) |
p-Value |
|---|---|---|---|
| Excellent | 45 (97.82%) | 42 (84%) | 0.032a |
| Good | 1 (2.18%) | 8 (16%) |
Fisher Exact two tailed p-value.
Discussion
Among all endoscopic procedures, ERCP has the maximum rate of complications and adverse events the highest of which are respiratory (depression/obstruction) associated with sedation-related morbidity and mortality. In a survey involving 16,855 patients, an ERCP-attributable complication rate of 6.85% with an incidence of 0.33% mortality was recorded.8 Minimal sedation with topical anaesthesia allows the procedure to be done as a day case but is associated with adverse effects like aspiration.9 Successful completion of the ERCP may require more than conscious or deep sedation. ERCP failure rates were observed to have doubled when performed under conscious sedation as compared to GA.2 Endoscopies performed under sedation have reported a high incidence of hypoxaemia.10, 11 Reshef et al. noted that risks related to prevalence of hypoxaemia in endoscopic procedures are as high as 28–50%.11 Besides prolonging the procedure time, an increased risk of post-ERCP pancreatitis has been observed in patients with desaturation of arterial oxygen less than 90%.12 ERCP with anaesthesiologist-administered sedation was studied in 528 patients and found to have an increased rate of respiratory and cardiac events associated with higher ASA class and BMI.13
While administering GA, endotracheal intubation provides the safest airway. However, as described earlier, airway control with endotracheal intubation has several downsides such as laryngoscopic stress response, use of muscle relaxants and prolonged procedure time. Hence there is a need of a better alternative to tracheal intubation. Use of a supraglottic airway device to secure the airway during ERCP has the advantage of protection and maintenance of a patent airway, at the same instance avoiding the disadvantages associated with laryngoscopy and tracheal intubation.4 Amongst supraglottic devices, ERCP with laryngeal mask airway (LMA) has been successfully used and was found to have shorter recovery times compared to the tracheal tube.14
This study (likely to be first of its kind) compared the safety and effectiveness of GLT, a new supraglottic device, with ETT as airway device for patients undergoing ERCP. An extensive search of the literature yielded only two studies evaluating GLT in ERCP.5, 7 In our study, GLT was noted to be associated with several advantages and it was found to be comparable with ETT on several fronts. The insertion time of endotracheal tube was significantly longer since the GLT was placed soon after administration of Propofol. However, it must be mentioned here that the mean insertion time of GLT was 50.5 s which was much higher than that reported by Gaitini et al. who achieved a mean insertion time of 26 s only.5 This variance can be explained by the difference in definition of insertion time which was taken as time interval between Propofol given and capnograph obtained in our study.
Success rate of insertion was lower, though not significant, in the GLT group than in ETT group (92% vs. 100%). Gaitini et al. were able to place GLT successfully in all patients with 90% at first attempt. In this study, we were able to place GLT successfully in 78% of cases in first attempt. As mentioned before, our success rates improved substantially in later part of the study.
Both the devices were equally effective in achieving normal oxygenation and ventilation during all procedures in all patients. There were no incidences of hypoxaemia or desaturation. Even though peak airway pressures and tidal volumes obtained were higher in the ETT group on account of mechanical ventilation, end-tidal CO2 values were numerically comparable. The difference in EtCO2 was not clinically significant. Thus, it was evident that GLT offered an acceptable level of ventilatory efficacy when compared with ETT. It is also pertinent to note that the oropharyngeal leak pressure (OLP) of GLT was 32.7 (1.8) cm H2O. This allowed adequate manual delivery of required tidal volume whenever it was felt necessary clinically. This indicates that GLT, like several other supraglottic devices such as Proseal LMA and i-gel, does establish a good oropharyngeal seal allowing satisfactory ventilation. Gaitini et al. recorded a mean seal pressure of 33.7 cm H2O which is comparable to our study.5
Even more interestingly and perhaps understandably, the recovery time was significantly shorter in GLT group as compared with ETT group (49.5 vs. 461.8 s). This can be attributed to avoidance of long acting muscle relaxants in GLT group. This has important implications for practitioners since it implies faster turnover time and enhanced efficiency. Even though we used Inj. Suxamethonium for insertion of ETT as well as GLT for the sake of maintaining uniformity in the study design, our subsequent experience with the GLT device indicated that it is indeed possible to place GLT without relaxants in spontaneously breathing patients after administering an adequate dose of Propofol. GLT also scored over ETT in terms of complications such as hoarseness and dysphonia. However, all the complications were transient and resolved within 24 h without any residual effect and thus were of no significant consequence.
The response of the Gastroenterologists and acceptability of the device to them was also studied. It was clear that the device was well accepted by them. This aspect of GLT has not been studied earlier. The scope insertion conditions were noted to be excellent in case of GLT. The gastroenterologists were also of the opinion that rotational manoeuvres of the duodenoscope were much better when scope was inserted through the GLT. Despite the availability of the GLT in a single size in this study it has shown to be a better alternative to the ETT. In the future once different sizes of GLT become available it is hoped that use of GLT will prove a safer and superior alternative to ETT.
Conclusion
In conclusion, GLT is suitable alternative to ETT in cases requiring GA for ERCP. The GLT is easy to insert and allows adequate ventilation. Adequate control over the airway minimizes the instances of desaturation and interruptions in the procedure. This is also associated with faster recovery times and minimal extubation-related complications. All this collectively translates into faster turnover and improvement in safety profile of the anaesthesia as well as the procedure. The device also enhances operative conditions for the Gastroenterologists. It can be safely concluded that GLT is an appropriately suited device for ERCP. This study was limited by a small sample size, however a larger multicentric study is likely to improve the power of the study as well as show significant differences in the parameters of interest.
Conflicts of interest
The authors have none to declare.
References
- 1.Goulson D.T., Fragneto R.Y. Anesthesia for gastrointestinal endoscopic procedures. Anesthesiol Clin. 2009;27:71–85. doi: 10.1016/j.anclin.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Raymondos K., Panning B., Bachem I., Manns M.P., Piepenbrock S., Meier P.N. Evaluation of endoscopic retrograde cholangiopancreatography under conscious sedation and general anesthesia. Endoscopy. 2002;34:721–726. doi: 10.1055/s-2002-33567. [DOI] [PubMed] [Google Scholar]
- 3.Etzorn K.P., Diab F., Brown R. Endoscopic retrograde cholangiopancreatography under general anesthesia: indications and results. Gastrointest Endosc. 1998;47:363–367. doi: 10.1016/s0016-5107(98)70219-6. [DOI] [PubMed] [Google Scholar]
- 4.Shribman A.J., Smith G., Achola K.J. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–299. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 5.Gaitini L.A., Lavi A., Stermer E., Charco Mora P., Pott L.M., Vaida S.J. Gastro-Laryngeal Tube for endoscopic retrograde cholangiopancreatography: a preliminary report. Anaesthesia. 2010;65:1114–1118. doi: 10.1111/j.1365-2044.2010.06510.x. [DOI] [PubMed] [Google Scholar]
- 6.2012. VBM Medizintechik GbmH.http://www.vbm-medical.com/ Accessed 08.08.12. [Google Scholar]
- 7.Fabbri C., Luigiano C., Cennamo V. The Gastro-Laryngeal Tube for interventional endoscopic biliopancreatic procedures in anesthetized patients. Endoscopy. 2012;44(11):1051–1054. doi: 10.1055/s-0032-1310159. [DOI] [PubMed] [Google Scholar]
- 8.Andruilli A., Loperfido S., Napolitano G. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781–1790. doi: 10.1111/j.1572-0241.2007.01279.x. [DOI] [PubMed] [Google Scholar]
- 9.Evans L.T., Saberi S., Kim H.M. Pharyngeal anesthesia during sedated EGDs: is “the spray” beneficial? A meta-analysis and systematic review. Gastrointest Endosc. 2006;63:761–766. doi: 10.1016/j.gie.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 10.Coté G.A., Hovis R.M., Ansstas M.A. Incidence and sedation-related complication with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010;8:103–104. doi: 10.1016/j.cgh.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Reshef R., Shiller M., Kinberg R. A prospective study evaluating the usefulness of continuous supplemental oxygen in various endoscopic procedures. Isr J Med Sci. 1996;32:736–740. [PubMed] [Google Scholar]
- 12.Freeman M. Sedation and monitoring for gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 1994;4:475–499. [PubMed] [Google Scholar]
- 13.Berzin T.M., Sanaka S., Barnett S.R. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73(4):710–717. doi: 10.1016/j.gie.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Osborn I.P., Cohen J., Soper R.J., Roth L.A. Laryngeal mask airway—a novel method of airway protection during ERCP: comparison with endotracheal intubation. Gastrointest Endosc. 2002;56:122–128. doi: 10.1067/mge.2002.125546. [DOI] [PubMed] [Google Scholar]