Abstract
Background
Neonates being nonverbal are unable to express their pain leading to underestimation of their pain and hence insufficient pain relief. Neonatal pain is assessed by pain scales based on the behavioural and physiological changes that occur in response to painful stimuli. This cross sectional study was conducted at a tertiary care centre using Premature Infant Pain Profile (PIPP) score with 4% lidocaine as local anaesthetic agent to produce surface anaesthesia of skin prior to intravenous cannulation.
Methods
Sample size was collected by simple randomisation method. Our study groups included 50 term and 50 preterm neonates with POG of 28–40 weeks requiring IV cannulation. Heart rate (HR), SpO2, facial expressions and behavioural state were noted before venipuncture and after venipuncture using PIPP scale. Same cohort of patients was assessed for pain response after applying 4% lidocaine cream during future venipuncture with help of PIPP score.
Results
The PIPP score in preterm group before and after anesthesia was 11.28 ± 3.72 and 9.58 ± 3.39. PIPP score in term group before and after anesthesia was 11.54 ± 2.84 and 9.04 ± 2.97. There was reduction in mean PIPP score after using topical anesthetic agent in both study groups and the results were statistically significant.
Conclusion
This study found that topical anesthetic agents were effective in reducing pain during venipuncture. Based on the facts of the study, it is recommended that pain scoring should be a part of routine monitoring in neonatal intensive care units and appropriate measures should be used to reduce pain.
Keywords: New Ballard Score, Premature Infant Pain Profile, Period of gestation, Low birth weight, Topical anaesthesia
Introduction
Neonates being nonverbal are unable to express their pain leading to underestimation of their pain and hence insufficient pain relief.1 Pain may adversely affect neurodevelopment and cause permanent injuries to the growing brain.2, 3 Various pain scales have been developed to measure neonatal pain objectively. These scales are based on changes in physiological responses and certain behavioural cues the infant displays on exposure to pain.4, 5
The commonly used pain measuring scales are: Premature Infant Pain Profile (PIPP), Neonatal Facial Coding System (NFCS) and Neonatal Infant Pain Scale (NIPS).4, 5, 6 PIPP is a validated pain scale for both term and preterm babies and is based on behavioural and physiological changes they display in response to a painful stimulus. Pain relief measures are commonly used for neonates during and after a major surgical procedure,7 but pain-reducing therapies are often underused for the numerous minor procedures.8, 9 In the past, non pharmacological measures like music therapy, singing and cuddling the neonates, etc. were tried to reduce neonatal pain. However, many studies have found that various topical anaesthetic agents can also be tried to reduce pain from minor procedures such as venipuncture and lumbar puncture.10, 11, 12 4% lidocaine chemically is 2-diethylaminoaceto-2,6-xylidide. It acts by blocking nerve impulse conduction by interfering with voltage dependent sodium channels, hence preventing initiation and transmission of nerve impulses. Being a topical drug, its safety level is very high. 4% lidocaine cream has several advantages including faster onset of action and no risk of methemoglobinemia in preterm infants.
Each neonatal unit should have more humane approach towards neonatal pain and hence develop strategies to provide effective pain relief for all procedures.10, 13, 14 The purpose of this study was to focus on measuring pain responsiveness using PIPP score and evaluating the analgesic effects of topical anaesthetic agent (4% lidocaine cream) with a view to provide adequate pain management during period of NICU stay.
Material and methods
This study was conducted as a cross sectional study in the Department of Pediatrics and Neonatology at a tertiary care centre. The sample size was collected by simple random sampling. The study comprised of 100 neonates (50 preterm and 50 term) admitted in NICU during two calendar years. Consent of parents was sought before inclusion in this study. This study had the approval of hospital ethical committee.
Inclusion criteria:
-
1.
Birth at 28–40 weeks of gestation.
-
2.
Neonates requiring IV cannulation.
Exclusion criteria:
-
1.
Neonates on mechanical ventilation.
-
2.
Neonates with multiple congenital anomalies.
-
3.
Neonates with neurological disorder.
-
4.
Neonates born with birth trauma.
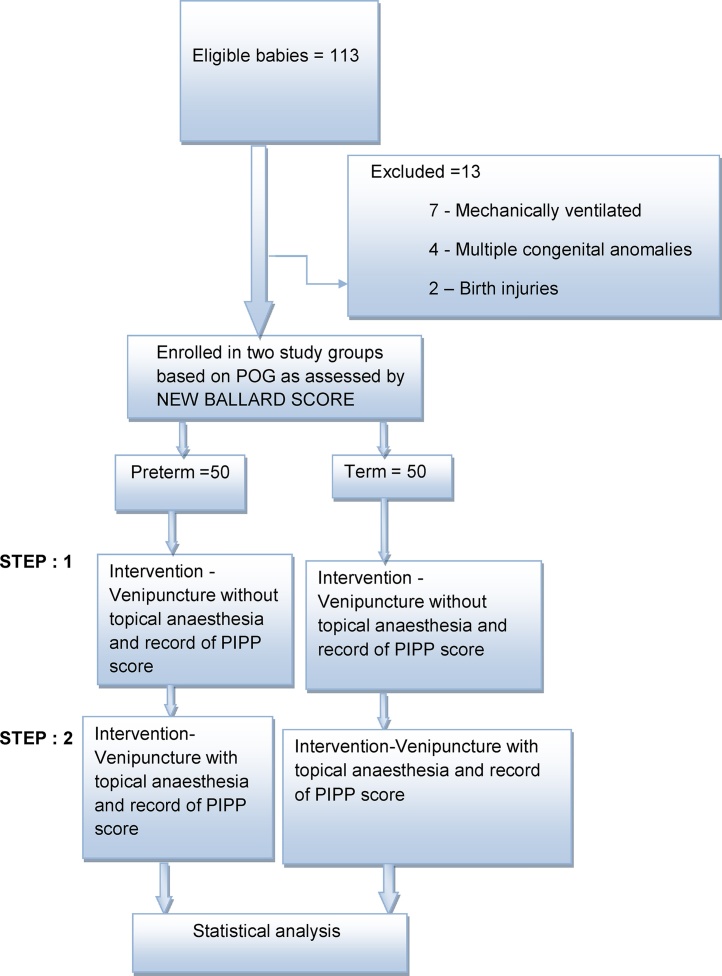
Once the candidacy for the study was established, the study population was grouped into two sets: preterm and term group after assessing gestational age as per New Ballard Score (Fig. 1).
Fig. 1.
Study outline.
The steps followed were as under:
-
1.
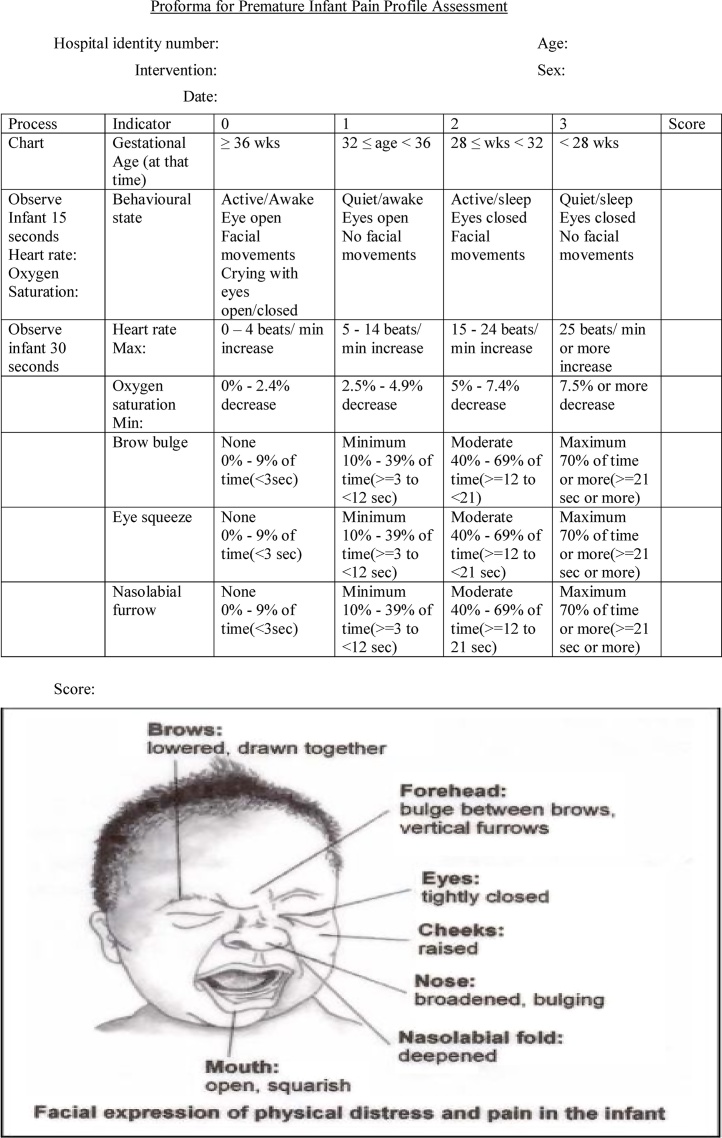
Scoring the behavioural state and facial expression as per PIPP guidelines (as shown in Fig. 2) before venipuncture by observing the infant for 30 s.
-
2.
Recording the baseline heart rate and oxygen saturation before the venipuncture.
-
3.
Observing the infant for 30 s immediately following venipuncture and scoring facial and physiological changes (HR and SpO2) seen during this time and recording immediately.
-
4.
Infant's behavioural responses to pain was recorded using a video camera (model: DSCH-20, Sony).
-
5.
The video recordings and monitor records of the infants in both groups were analysed to generate data as per proforma for the study (Fig. 2).
-
6.
Pain response was assessed without local anaesthesia using PIPP score at the first venipuncture done after admission in neonatal intensive care unit.
-
7.
Since admitted neonates often required multiple venipunctures during the period of NICU stay, same cohort of patients was assessed for pain response using topical anaesthetic agent used in this study, i.e. 4% lidocaine cream during next venipuncture with help of PIPP score.
-
8.
After examining the infant, suitable site for the procedure was selected ensuring the intactness of skin. Lidocaine cream was applied to the selected site in single layer to cover an area of 2.5 cm × 2.5 cm and left in situ for 30 min. Lidocaine application was left undisturbed using occlusive dressing (Tegaderm) to prevent disturbance/interference by the patient or external factors. Since anaesthesia is usually obtained within 30 min of application, the cream was removed from the site using clean gauze swab. Venipuncture was done within 5 min after removing the cream and response to pain studied using PIPP scores in neonate.
-
9.
Interpretation of PIPP score was as under:
Minimum score was zero and maximum score was 21. The higher the score the greater the response to pain.
-
10.
The results of the study were statistically analysed in detail by using Student's-t test (paired) and Chi-square test. The results of the study were considered statistically significant if p value was less than 0.05, highly significant if less than 0.01, and very highly significant if less than 0.001.
Fig. 2.
PIPP scale components.
Results
Average period of gestation (mean ± 2SD) in preterm group was 33.08 ± 2.41 weeks and term group was 37.52 ± 0.73 weeks. Average age in hours at the time of first venipuncture in preterm group was 0.60 ± 0.75 h and that in term group was 0.54 ± 0.90 h. There were a total of 26 male babies and 24 female babies in preterm group vis-a-vis 22 male babies and 28 female babies in term group. The various causes of NICU admission were prematurity, respiratory distress syndrome, low birth weight, feed intolerance and transient tachypnea of newborn. Average duration of NICU stay was 7 days for preterm and 4 days for term baby. Average frequency of venipuncture during this period was once in 2 days for preterm and once in 3 days for term group. Common indications of venipuncture were cannulation for medication, blood sampling, Intravenous fluid and antibiotic administration. Various components of PIPP score are depicted in Table 1, Table 2, Table 3, Table 4, Table 5, Table 6. Total PIPP score of preterm and term study groups was 11.28 ± 3.72 and 11.54 ± 2.84 respectively. There was statistically significant reduction in total PIPP score in both preterm and term study group using 4% lidocaine cream (p value <0.01).
Table 1.
Behaviour state score of preterm and term groups.
| Behaviour state score (mean ± 2SD) | Preterm mean ± 2SD |
Term mean ± 2SD |
Total (n = 100) |
p value |
|
|---|---|---|---|---|---|
| Preterm | Term | ||||
| Before anaesthesia | 1.86 ± 0.98 | 2.16 ± 1.07 | 50 | 0.15 | 0.15 |
| After anaesthesia | 1.82 ± 1.17 | 1.82 ± 1.17 | 50 | 0.80 | 0.80 |
Table 2.
Heart rate score in preterm and term groups.
| Increase in HR score (beats/min) | Preterm mean ± 2SD |
Term mean ± 2SD |
Total (n = 100) |
p value |
|
|---|---|---|---|---|---|
| Preterm | Term | ||||
| Before anaesthesia | 16.02 ± 9.21 | 16.60 ± 8.70 | 50 | 0.72 | 0.01 |
| After anaesthesia | 15.36 ± 8.99 | 11.84 ± 7.82 | 50 | 0.72 | 0.01 |
Table 3.
O2 saturation score of preterm and term groups.
| Decrease in O2 saturation (%) | Preterm mean ± 2SD |
Term mean ± 2SD |
TOTAL (n = 100) |
p value |
|
|---|---|---|---|---|---|
| Preterm | Term | ||||
| Before anaesthesia | 2.90 ± 1.61 | 2.52 ± 1.13 | 50 | .001 | 0.23 |
| After anaesthesia | 1.78 ± 2.35 | 2.30 ± 0.97 | 50 | .001 | 0.30 |
Table 4.
Brow bulge and eye squeeze score of preterm and term group.
| Preterm mean ± 2SD |
Term mean ± 2SD |
Total (n = 100) |
p value |
||
|---|---|---|---|---|---|
| Preterm | Term | ||||
| Brow bulge score (s) | |||||
| Before anaesthesia | 15.70 ± 8.64 | 19.22 ± 7.49 | 50 | 0.23 | 0.006 |
| After anaesthesia | 13.60 ± 8.93 | 14.54 ± 8.98 | 50 | 0.23 | 0.006 |
| Eye squeeze score (s) | |||||
| Before anaesthesia | 16.64 ± 9.09 | 18.58 ± 7.69 | 50 | 0.17 | 0.05 |
| After anaesthesia | 14.14 ± 9.29 | 15.42 ± 8.48 | 50 | 0.17 | 0.05 |
Table 5.
Nasolabial furrow score of preterm and term group.
| Nasolabial furrow squeeze (s) | Preterm mean ± 2SD |
Term mean ± 2SD |
Total (n = 100) |
p value |
|
|---|---|---|---|---|---|
| Preterm | Term | ||||
| Before anaesthesia | 16.52 ± 9.46 | 18.56 ± 8.63 | 50 | 0.22 | 0.01 |
| After anaesthesia | 14.28 ± 8.82 | 14.14 ± 8.34 | 50 | 0.22 | 0.01 |
Table 6.
Total PIPP score of preterm and term group.
| Total score | Preterm mean ± 2SD |
Term mean ± 2SD |
Total (n = 100) |
p value |
|
|---|---|---|---|---|---|
| Preterm | Term | ||||
| Before anaesthesia | 11.28 ± 3.72 | 11.54 ± 2.84 | 50 | 0.01 | 0.001 |
| After anaesthesia | 9.58 ± 3.39 | 9.04 ± 2.97 | 50 | 0.01 | 0.001 |
Discussion
Lack of verbal communication, limited behavioural expression, non-specific physiological responses and inability of the care providers to assess the neonatal pain properly, puts them at risk of frequent painful experiences during NICU admission. Unless measured properly, adequate pain relief policies cannot be formulated. In this study, we have tried to measure the neonatal pain objectively using a validated pain scale, i.e. PIPP. This scale was chosen since it is the only tool that is applicable to measure both preterm and term neonatal pain.15 Venipuncture is one of the most common minor procedures done in NICU and hence was chosen to study the effect of 4% lidocaine, a relatively new drug to relieve minor procedural pain. The authors did an extensive literature search and found that this is the first study involving use of topical 4% lidocaine for assessing pain response in neonates during venipuncture. Most of the other studies done to assess pain response in neonates during venipuncture or other procedures like administering IM injections, lumbar puncture or heel lancing have used either amethocaine or eutectic mixture of local anaesthetics (EMLA) as the topical anaesthetic of choice for assessing pain response.
In a recent Cochrane review, eight RCTs regarding assessing pain response in neonates were studied and they compared either EMLA and placebo or amethocaine and placebo. Both EMLA and amethicone were found useful to relieve minor procedural pain like venipuncture or heel lancing.16 However, EMLA carried the risk of methemoglobinemia for preterm neonates. Local swelling, redness or blanching was higher with use of EMLA.16 In our study, we did not encounter any such local skin reaction to 4% lidocaine cream. Detailed analysis of the results of our study showed that most of the babies under study were found in stage two or stage one behaviour state. Mean score in preterm group before and after anaesthesia was 1.86 ± 0.98 and 1.82 ± 1.17 respectively and in term group was 2.16 ± 1.07 and 1.82 ± 1.17 respectively. There was no significant change in behaviour state in both study groups and the results were not statistically significant with topical anaesthetic agent. Mean HR score in preterm group before and after applying topical anaesthetic agent was 16.02 ± 9.21 and 15.36 ± 8.99 beats/min respectively and in term group was 16.60 ± 8.70 and 11.84 ± 7.82 beats/min respectively. Topical anaesthetic agent was effective in reducing mean HR score in term group and results were highly significant statistically.
There was statistically highly significant effect on fall in oxygen saturation score in preterm group with score of 2.90 ± 1.61 before topical anaesthesia and 1.78 ± 2.35 after application of topical anaesthetic agent. However the results were not significant in term group with mean score of 2.52 ± 1.13 before topical anaesthesia and 2.30 ± 0.97 after topical anaesthesia. There was statistically highly significant reduction in brow bulge score of term group after topical anaesthesia with mean score of 19.22 ± 7.49 before and 14.54 ± 8.98 after anaesthesia. However the results were not significant in preterm group with mean score of 15.70 ± 8.64 before and 13.60 ± 8.93 after topical anaesthesia.
There was statistically significant reduction in eye squeeze score in term study group with topical anaesthetic agent. Mean score was 18.58 ± 7.69 before and 15.42 ± 8.48 after topical anaesthesia in term group. However the results were not statistically significant in preterm group with mean score of 16.64 ± 9.09 before and 14.14 ± 9.29 after topical anaesthesia. There was no statistically significant reduction in nasolabial furrow score in preterm group with score of 16.52 ± 9.46 before and 14.28 ± 8.82 after topical anaesthetic agents. However the results were statistically highly significant in term group with mean score of 18.56 ± 8.63 before and 14.14 ± 8.34 after topical anaesthesia.
Total PIPP score in preterm and term study groups before and after topical anaesthetic agent was 11.28 ± 3.72, 9.58 ± 3.39 and 11.54 ± 2.84, 9.04 ± 2.97 respectively. PIPP score was higher in term study group as compared to preterm group before applying topical anaesthetic agent. This may be attributable to more mature brain resulting in better perception of pain by the term neonate. Moreover, facial expression of term neonates are better perceived compared to preterm neonates. This is in line with the findings of our study. Preterm neonates exhibited much of their pain by more changes in physiological responses as compared to behavioural cues. There was reduction in mean PIPP score after using topical anaesthetic agent in both study groups and the results were significant statistically in preterm group and term group.
Though objective assessment of pain of neonates is difficult, still the issue is garnering more attention in recent times due to possible adverse sequelae. Our study results have shown that neonates undergo significant amount of pain during venipuncture and topical anaesthetic agent 4% lignocaine can help reduce such pain.
Conclusion and recommendation
-
1.
This study concludes that neonates undergo significant amount of pain during venipuncture during their NICU stay and use of topical 4% lignocaine reduces the pain of venipuncture in both preterm and term neonates.
-
2.
The study recommends that pain scoring should be a part of routine monitoring in neonatal intensive care units and hence adequate training should be provided to healthcare providers to assess pain in neonates. Each neonatal intensive care unit should formulate a policy to provide adequate pain relief. This should include minimizing the number of painful exposures as much as possible and use of measures like 4% lidocaine to relieve minor procedural pain.
Conflicts of interest
The authors have none to declare.
References
- 1.McGrath P.J., Finley G.A. Attitudes and beliefs about medication and pain management in children. J Palliat Care. 1996;12:46–50. [PubMed] [Google Scholar]
- 2.Stevens B.J., Franck L. Special needs of preterm infants in the management of pain and discomfort. J Obstet Gynecol Neonatal Nurs. 1995;24:856–862. doi: 10.1111/j.1552-6909.1995.tb02571.x. [DOI] [PubMed] [Google Scholar]
- 3.Anand K.J. Pain, plasticity, and premature birth: a prescription for permanent suffering? Nat Med. 2000;6(9):971–973. doi: 10.1038/79658. [DOI] [PubMed] [Google Scholar]
- 4.Craig K.D., Whitfield M.F., Grunau R.V., Linton J., Hadjistavropoulos H.D. Pain in the preterm neonate: behavioural and physiological indices. Pain. 1993;52(3):287–299. doi: 10.1016/0304-3959(93)90162-I. [DOI] [PubMed] [Google Scholar]
- 5.Grunau R., Craig K. Pain expression in neonates: facial action and cry. Pain. 1987;28:395–410. doi: 10.1016/0304-3959(87)90073-X. [DOI] [PubMed] [Google Scholar]
- 6.Lawrence J., Alcock D., McGrath P., Kay J., MacMurray B., Dulberg C. The development of a tool to assess neonatal pain. Neonatal Netw. 1993;12:59–66. [PubMed] [Google Scholar]
- 7.Anand K.J. Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med. 2001;155:173–180. doi: 10.1001/archpedi.155.2.173. [DOI] [PubMed] [Google Scholar]
- 8.Simons S.H., van Dijk M., Anand K.S., Roofthooft D., van Lingen R.A., Tibboel D. Do we still hurt newborn babies? A prospective study of procedural pain and analgesia in neonates. Arch Pediatr Adolesc Med. 2003;157:1058–1064. doi: 10.1001/archpedi.157.11.1058. [DOI] [PubMed] [Google Scholar]
- 9.Porter F.L., Wolf C., Gold J., Lotsoff D., Miller J.P. Pain and pain management in newborn infants: a survey of physicians and nurses. Pediatrics. 1997;100:626–632. doi: 10.1542/peds.100.4.626. [DOI] [PubMed] [Google Scholar]
- 10.Gibbins S., Stevens B., Asztalos E. Assessment and management of acute pain in high-risk neonates. Expert Opin Pharmacother. 2003;4:475–483. doi: 10.1517/14656566.4.4.475. [DOI] [PubMed] [Google Scholar]
- 11.Long C.P., McCafferty D.F., Sittlington N.M., Halliday H.L., Woolfson A.D., Jones D.S. Randomized trial of novel tetracaine patch to provide local anaesthesia in neonates undergoing venepuncture. Br J Anaesth. 2003;91:514–518. doi: 10.1093/bja/aeg216. [DOI] [PubMed] [Google Scholar]
- 12.Kaur G., Gupta P., Kumar A. A randomized trial of eutectic mixture of local anesthetics during lumbar puncture in newborns. Arch Pediatr Adolesc Med. 2003;157:1065–107020. doi: 10.1001/archpedi.157.11.1065. [DOI] [PubMed] [Google Scholar]
- 13.International Association for the Study of Pain Subcommittee on Taxonomy Pain terms: a list with definitions and notes on usage. Pain. 1979;6:249–252. [PubMed] [Google Scholar]
- 14.Halimaa S.L. Pain management in nursing procedures on premature babies. J Adv Nurs. 2003;42:587–597. doi: 10.1046/j.1365-2648.2003.02662.x. [DOI] [PubMed] [Google Scholar]
- 15.Stevens B., Jhonston C., Petryshen P., Taddio A. Premature infant pain profile: development & initial validation. Clin J Pediatr. 1996;12(1):13–22. doi: 10.1097/00002508-199603000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Foster J.P., Taylor C., Spence K. Topical anaesthesia for needle-related pain in newborn infants. Cochrane Database Syst Rev. 2017;2:CD010331. doi: 10.1002/14651858.CD010331.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]