Abstract
Background
Rhinoplasty has a tremendous psychosocial impact. A good surgical correction may not guarantee an expected response from the patient. This is due to the fact that there may be associated psychological distress, the assessment of which may have to be incorporated while evaluating the surgical result. We aimed to identify if the questionnaire may help in identifying patients who might be less satisfied psychologically to the surgical result. This aspect of psychological assessment is not standardized, although it is reported in Western literature and recently in Asian Koreans. Similar studies in an Indian scenario merit deliberation.
Methods
Fifty-one patients who underwent cosmetic rhinoplasty from August 2011 to July 2013 were administered the Derriford Questionnaire preoperatively and postoperatively at 3 months at a mid-zonal hospital. The responses were scored on a five-point Likert scale and analyzed.
Results
The overall postoperative score improved from 1.32 ± 0.24 to 1.27 ± 0.24. There was statistically significant improvement in subscales of general, sociosexual, and bodily self-consciousness of appearance. However, the improvement in facial self-consciousness of appearance and negative self-concept was not statistically significant.
Conclusion
We recommend the use of the Derriford Assessment Scale (DAS) for objective assessment of psychological distress associated with living with a problem of appearance, in addition to assessment of anatomical deformity in patients undergoing cosmetic rhinoplasty. Better preoperative counseling may benefit those with a high score for negative self-concept and facial self-consciousness of appearance.
Keywords: Cosmetic surgery, Rhinoplasty, Outcome assessment, Patient
Introduction
Cosmetic problems can have a remarkable effect on a person's emotional state. There has always been an onus on the cosmetic surgeon to preoperatively counsel the patient about a realistic expectation from the results of surgery. The surgeon may offer the best possible clinical result; however, this may not corroborate with what the patient perceives, as there may be a psychological aspect, which varies from patient to patient. This may affect the patient's perception of what the surgeon feels to be a good surgical result. Therefore, psychological improvement after surgery is very important from a patient's perspective. Hence, the surgeon would be benefitted from identification of certain aspects of the patient's personality, which might influence the patient's response to a good clinical outcome, which may not seem realistic, from a surgical viewpoint.
Most surgeons use preoperative and postoperative photographs in various views to analyze the results of surgery. But these alone do not enable a comprehensive preoperative assessment of these patients. Surgeons have felt the need to do a psychological assessment of cosmetic rhinoplasty using questionnaires; however, there is no standardization of any psychological assessment tool for cosmetic rhinoplasty.1 In this study, we administered the Derriford Appearance Scale 59 (DAS 59) Questionnaire to patients undergoing cosmetic rhinoplasty before and after surgery. This questionnaire, which is validated in literature, assesses various aspects of the patient's psychology.2, 3 Based on the responses, we aimed to identify if the questionnaire may help in identifying patients who might be less satisfied psychologically to the surgical result. The DAS 59 has been used in assessing septorhinoplasty results in Korean patients.4 An extensive search of peer-reviewed, English language literature revealed this to be the first such study to perform a psychological assessment in cosmetic rhinoplasty in an Indian setting.
Materials and methods
Study setting and participants
A prospective study was performed on 51 patients who had attended the ENT clinic for cosmetic rhinoplasty from September 2011 to August 2013 at a mid-zonal hospital. The study was conducted after obtaining informed consent from all patients before enlisting their participation in the study.
Inclusion criteria
All patients who underwent cosmetic rhinoplasty with a minimum follow-up of 3 months were included in the study.
Exclusion criteria
Two patients with chronic sinusitis, one patient with allergic rhinitis, and two patients who underwent revision surgery were excluded.
Psychological scale
All patients were administered the DAS 59, which is a validated tool for cosmetic and reconstructive surgery patients.2 The questionnaire was filled preoperatively and at 3 months postoperatively.
The factorial scores were calculated for the following:
-
a)
General self-consciousness of appearance (GSC)
-
b)
Social self-consciousness of appearance (SSC)
-
c)
Sexual and bodily consciousness of appearance (SBSC)
-
d)
Negative self-concept (NSC)
-
e)
Facial self-consciousness of appearance (FSC)
-
f)
Physical distress and dysfunction (PDD)
Two questions were not specific and do not load on any particular factor.
Statistical analysis
The DAS 59 questionnaire was administered on 51 patients who reported for cosmetic rhinoplasty, and the responses were scored on a Likert scale. Internal consistency of subscales was assessed using Cronbach alpha values. The normality of data was checked using Kolmogorov–Smirnov test and Shapiro–Wilk test with Q–Q plot. Mean and standard deviation were calculated for each subdomain (GSC, SSC, SBSC, NSC, FSC, and PDD) in preoperative and postoperative status and compared using paired t test. Ninety-five percent error charts for mean and box plot were made to see the changes in responses graphically. Data were entered and coded in MS Excel and analyzed using IBM SPSS (version 21.0; Illinois, Chicago). A p value of less than 0.05 was considered to be statistically significant.
Results
A total of 51 patients were administered the DAS before surgery, and they again filled the same questionnaire at 3 months after surgery.
Demographic data
The study population comprised 44 males and 7 females. The age ranged from 11 to 45 years. The mean age for the entire study group was 22.94 ± 6.18 years with a mean of 23.45 ± 5.93 years for males and a mean of 19.71 ± 7.20 years for females. There were 15 married and 36 unmarried patients. Of the married patients, 2 had an income of >Rs 50,000 per month and 13 had an income of Rs 15,000–50,000 per month. Of the 36 who were unmarried, 11 were students, of which, 3 were earning a stipend of <15,000 per month and the rest were not drawing any income. Of the remaining 25, 5 had an income of >Rs 50,000 per month and 20 had an income of Rs 15,000–50,000 per month.
Scale validation
The Cronbach alpha values of total responses on the DAS 59 were 0.89. The combined values for GSC, SSC, SBSC, NSC, FSC, NS, and PDD were 0.89, 0.89, 0.76, 0.78, 0.77, 0.70, and 0.32, respectively. The preoperative and postoperative alpha values for the total response and subscales are shown in Table 1. The Cronbach alpha values for preoperative and postoperative responses show good internal consistency.
Table 1.
Comparisons of preoperative and postoperative scores of subscales of the DAS 59 (Derriford Appearance Scale).
| Domain name | Preoperative (mean ± SD) | Postoperative (mean ± SD) | Percentage change | t value | p value |
|---|---|---|---|---|---|
| GSC | 2.16 ± 0.49 | 1.53 ± 0.30 | (+) 29.17 | 15.70 | 0.000 |
| SSC | 1.43 ± 0.41 | 1.12 ± 0.19 | (+) 21.68 | 6.77 | 0.000 |
| SBSC | 1.04 ± 0.33 | 0.92 ± 0.35 | (+) 11.54 | 6.93 | 0.000 |
| NSC | 1.76 ± 0.55 | 1.67 ± 0.51 | (+) 5.11 | 1.94 | 0.057 |
| FSC | 1.29 ± 0.42 | 1.25 ± 0.31 | (+) 3.10 | 1.12 | 0.266 |
| PDD | 1.10 ± 0.24 | 1.03 ± 0.15 | (+) 6.36 | 1.63 | 0.109 |
| Total | 1.32 ± 0.24 | 1.27 ± 0.24 | (+) 3.79 | 10.71 | 0.000 |
The bold values show statistical significant p value (p < 0.05).
FSC, facial self-consciousness of appearance; GSC, general self-consciousness of appearance; NSC, negative self-concept; PDD, physical distress and dysfunction; SBSC, sexual and bodily consciousness of appearance; SD, standard deviation; SSC, social self-consciousness of appearance.
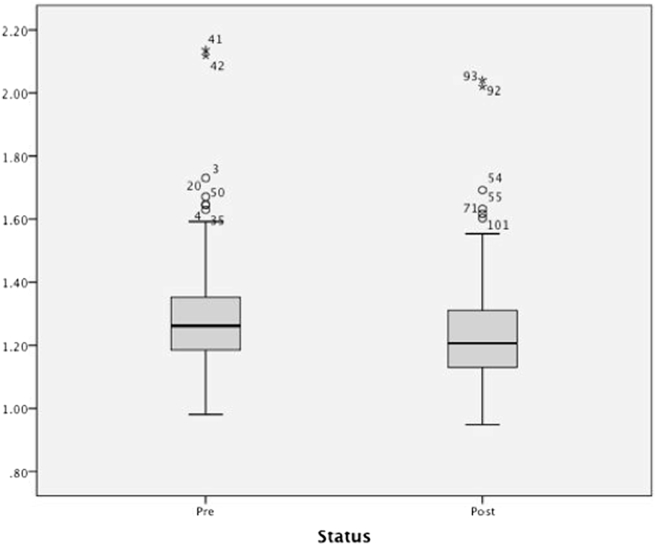
DAS 59 scores
The total mean preoperative score showed a decline from 1.32 ± 0.24 to 1.27 ± 0.24 in the postoperative score. This overall reduction in the mean postoperative score was statistically significant (p value for paired t test = 0.000). We observed that a mean difference beyond 7% showed that the patient was psychologically satisfied. The results are shown in Table 1. Fig. 1, Fig. 2 show the box plot and error bar showing the overall change in preoperative and postoperative scores on the DAS, respectively.
Fig. 1.
Graph (boxplot and error bar) showing overall change in the preoperative and postoperative scores on the DAS 59. DAS, Derriford Appearance Scale.
Fig. 2.
Error bar showing overall change in the preoperative and postoperative scores on the DAS 59. CI, confidence interval; DAS, Derriford Appearance Scale.
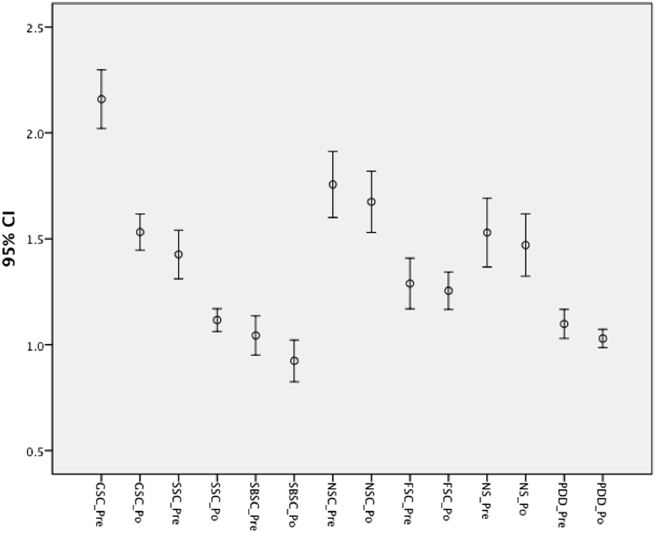
Factorial scores
There was a reduction in the mean scores for all the subscales postoperatively. The mean preoperative score showed a decline from 2.16 ± 0.49 to 1.53 ± 0.30 for GSC, from 1.43 ± 0.41 to 1.12 ± 0.19 at postoperative evaluation for SSC, and from 1.04 ± 0.33 to 0.92 ± 0.35 for SBSC. This difference for GSC, SSC, and SBSC was statistically significant (p = 0.000) using the paired t test. Although NSC, FSC, and PDD also showed a decline from 1.76 ± 0.55 to 1.67 ± 0.51, 1.29 ± 0.42 to 1.25 ± 0.31, and 1.10 ± 0.24 to 1.03 ± 0.15, respectively, the postoperative change for NSC, FSC, and PDD was not statistically significant (p > 0.05). For NSC, the p value was 0.057, almost reaching statistical significance. Fig. 3 depicts the error bar showing the preoperative and postoperative scores of the GSC, SSC, SBSC, NSC, FSC, and PDD.
Fig. 3.
Error bar showing preoperative and postoperative change for GSC, SSC, SBSC, NSC, FSC, and PDD. CI, confidence interval; GSC_Pre, general self-consciousness of appearance preoperative; GSC_Po, general self-consciousness of appearance postoperative; SSC_Pre, social self-consciousness of appearance preoperative; SSC_Po, social self-consciousness of appearance postoperative; SBSC_Pre, sexual and bodily self-consciousness of appearance preoperative; SBSC_Po, sexual and bodily self-consciousness of appearance postoperative; NSC_Pre, negative self-concept preoperative; NSC_Po, negative self-concept postoperative, FSC_Pre, facial self-consciousness of appearance preoperative; FSC_Po, facial self-consciousness of appearance postoperative; PDD_Pre, physical distress and dysfunction preoperative; PDD_Po, physical distress and dysfunction postoperative.
Discussion
Rhinoplasty has historically been a very popular cosmetic procedure. The nose has always been given a lot of importance aesthetically and psychologically from a structure signifying beauty to pride. Not only manufacturers of clothing and cosmetic products but also otolaryngologists and plastic surgeons have a stake in facial appearance. Cosmetic surgeons are very vulnerable to criticism because the results of plastic surgery are visible to all.4 However, there is also the aspect of vulnerability to the patients underlying emotional state. The psychological aspect of cosmetic rhinoplasty has long been recognized. Satisfaction from surgery may be affected by patient expectations, which may differ in individuals. In fact, few patients might adjust to a less than good functional correction if esthetic result satisfied them.5 Therefore, the improvement in psychosocial distress after cosmetic surgery such as rhinoplasty is very important from the patient's point of view. Various questionnaires have been used for preoperative and postoperative assessment of patient psychology in cosmetic surgeries.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 Harris et al2 developed the DAS 59 to objectively measure psychological distress experienced by patients with problems of appearance, as plastic surgeons felt that psychosocial distress experienced by patients who undergo cosmetic surgery as measured on the DAS 59 would be more relevant than the scales of mental health questionnaires used by psychiatrists. Also, they felt that patients who undergo cosmetic surgery did not exhibit specific personality types as measured by mental health questionnaires. Hence, other scales of body image lacked sensitivity to the nature of the dysfunction. We have carried out a study on 51 patients who underwent rhinoplasty by administering the DAS 59, which is a validated tool for assessing patients who undergo facial cosmetic surgery and reconstructive surgery as reported by Harris et al.2 We found it easy to administer and score.
Patients who undergo cosmetic rhinoplasty would have a different psychological perspective as compared with other patients who undergo plastic or reconstructive surgery, as the nose is given a significant esthetic importance, traditionally. An objective psychological assessment is very important for the surgeon to give him an idea about the psychological profile of the patient. This aspect needs to be incorporated while assessing the clinical result. Quality of life measures are very important for the patient, as more and more patients seek surgery not only as a measure to save life and limb, but also, to improve physical appearance. Hence, psychological improvement is important along with surgical improvement. This emphasizes the need to assess exact patient expectations from the intervention. Cosmetic surgery has a psychological impact, which would vary from person to person and also from place to place. The DAS 59 has been used for assessing septorhinoplasty results in Korean patients.4 An extensive search of peer-reviewed, English language literature revealed this to be the first such study, in an Asian Indian setting, to perform a psychological assessment using the DAS 59 in cosmetic rhinoplasty.
Patient satisfaction is very pertinent in determining success of surgery, but measurement of this especially in relation to psychological satisfaction after rhinoplasty objectively is difficult to standardize. Studies have tried to assess various tools in measuring this.1, 20 These have been used to evaluate self-esteem, general psychological well-being assessment, and personality disorders. However, we feel that patients who undergo cosmetic rhinoplasty may have certain subtle aspects in their personality regarding self-consciousness of appearance, which is identified using the DAS 59.
With a mean NSC score of 1.76 ± 0.55 and FSC score of 1.29 ± 0.42, preoperatively, a mean difference of 5.11 and 3.10 was achieved postoperatively. This is not significant for FSC and just reaches 0.05 (i.e, statistical significance) for NSC. This possibly means that at least a mean preoperative score of 1.76 ± 0.55 for NSC and lower than 1.29 ± 0.42 for FSC would be required preoperatively to show significant improvement, as these show only marginal improvement, postoperatively, implying that this is the subset of patients who require better preoperative psychological counseling to achieve desired benefit even after a good surgical correction.
Comparison with other studies
Studies mention overall psychological improvement in patients after cosmetic nasal surgery.20 We found an overall reduction in psychosocial distress after surgery which was statistically significant.
Harris et al2 have reported significant reduction in SBSC scores for treatment of bodily features and significant reduction in FSC scores for patients treated for facial features.
However, in our patients, NSC, FSC, and PDD did not show a statistically significant improvement. This may be due to the fact that Harris et al studied all patients who underwent plastic surgery, and our rhinoplasty subset may have a different profile. FSC might be more important in cosmetic surgery of face such as aging face. The factor of NSC has shown a better improvement than FSC or PDD. The difference may also be due to the fact that as psychosocial aspects may vary from place to place, the psychological profile of patients might also vary. Litner et al21 have used the DAS in a cohort, which includes rhinoplasty and facial cosmetic surgery, of 93 patients, who might have different psychological profiles. Overall improvement is similar to our study; however, male patients showed improvement only in factor GSC in their study, which is different from ours. This again emphasizes that psychosocial factors concerning appearance vary in societies. The mean preoperative score and the alpha value for PDD were found to be low compared with other subscales, in our study. Hence, we feel that PDD measure may be more relevant in reconstructive surgery such as mammoplasty or after cancer surgery, and hence, there is no significant change in our class of patients. This factor may not be required to be incorporated in evaluating rhinoplasty; however, larger patient numbers may be required to assess this further.
Synopsis of findings and recommendations
Although most patients show overall reduction in psychosocial distress after cosmetic rhinoplasty, patients with a high score of NSC, FSC, and PDD may not show significant improvement. We found the DAS 59 easy to administer and score. There was an overall improvement in the mean postoperative score. For feature-specific subscores, there was an improvement in all subscales. The improvement in GSC, SSC, and SBSC was statistically significant. However, for NSC, FSC, and PDD, the improvement was not statistically significant. Hence, we recommend that patients with high NSC and FSC scores on preoperative evaluation may be sent for psychological counseling. PDD may be more appropriate in a patient who undergoes reconstructive surgery, for example, after cancer surgery where there is an element of physical pain and discomfort. We feel that this factor may not be important for a patient who undergoes cosmetic rhinoplasty; however, it may need larger data to validate it further.
Strengths and limitations of the study
Our study has evaluated the clinical applicability of using the DAS 59 in 51 patients who underwent cosmetic rhinoplasty. An extensive search of peer-reviewed, English language literature revealed this to be the first such study in an Asian Indian setting. This objective measure may be relevant in cosmetic rhinoplasty to better counsel the subset of patients who might be expected to show a poorer psychological satisfaction to a good surgical result. The severity of the deformity and the surgeon's assessment of the outcome may need to be incorporated for a more comprehensive evaluation for a larger number of patients using the DAS 59. A long-term evaluation at 1 year may bring out further suggestions.
The subset of patients who have associated septal deviation may have a different response compared with rhinoplasty alone, and this may be assessed and compared separately in a larger sample. As cases with rhinosinusitis and who underwent revision surgeries were excluded, the bias resulting from the same cannot be ascertained.
Clinical applicability
An objective assessment of change in psychological distress after surgery can be carried out using the DAS 59. It is easy to administer and score. We recommend the use of an objective tool such as the DAS 59 for performing psychological assessment of all patients being planned for cosmetic rhinoplasty.
Conclusion
Patients who undergo rhinoplasty require objective assessment for psychological distress associated with living with a problem of appearance, in addition to assessment of anatomical deformity. We recommend that the use of a questionnaire such as the DAS 59 may help in identifying patients with a high score for NSC and FSC, who may be benefitted by better preoperative counseling, in addition to surgical correction alone. Further research can incorporate factors such as preoperative assessment of deformity and the surgeon's assessment of the outcome in a larger number of patients. These measures incorporated along with an objective questionnaire such as the DAS 59 may help in better patient assessment and preoperative patient counseling so that the patients feel more satisfied with the clinical result. This would prove beneficial to both the patient and the doctor.
Conflict of interest
The authors have none to declare.
References
- 1.Ching S., Thoma A., McCabe R.E., Antony M.M. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111:469–480. doi: 10.1097/01.PRS.0000036041.67101.48. [DOI] [PubMed] [Google Scholar]
- 2.Harris D.L., Carr A.T. Derriford Appearance Scale (DAS59): a new psychometric scale for the evaluation of patients with disfigurements and aesthetic problems of appearance. Br J Plast Surg. 2001;54:216–222. doi: 10.1054/bjps.2001.3559. [DOI] [PubMed] [Google Scholar]
- 3.Carr T., Harris D., James C. The Derriford Appearance Scale (DAS-59): a new scale to measure individual responses to living with problems of appearance. Br J Health Psychol. 2000;5:201–215. doi: 10.1348/135910705X27613. [DOI] [PubMed] [Google Scholar]
- 4.Won T.B., Park K.T., Moon S.J. The effect of septorhinoplasty on quality of life and nasal function in Asians. Ann Plast Surg. 2013;71:40–44. doi: 10.1097/SAP.0b013e3182414641. [DOI] [PubMed] [Google Scholar]
- 5.Bradbury E. Meeting the psychological needs of patients with facial disfigurement. Br J Oral Maxillofac Surg. 2012;50:193–196. doi: 10.1016/j.bjoms.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Dinis P.B., Dinis M., Gomes A. Psychosocial consequences of nasal aesthetic and functional surgery; a controlled prospective study in an ENT setting. Rhinology. 1998;36:32–36. [PubMed] [Google Scholar]
- 7.Mohamed W.S., El Shazly M.M., El- Sonbaty M.A., Eloteify M.M. Objective versus subjective assessment for rhinoplasty. Egypt J Plast Reconstr Surg. 2013;37:73–79. [Google Scholar]
- 8.Cemal C., Murat S., Cengiz B. Outcomes research in rhinoplasty: body image and quality of life. Am J Rhinol Allergy. 2011;25:263–267. doi: 10.2500/ajra.2011.25.3649. [DOI] [PubMed] [Google Scholar]
- 9.Pecorari G., Gramaglia C., Garzaro M. Self-esteem and personality in subjects with and without body dysmorphic disorder traits undergoing cosmetic rhinoplasty: preliminary data. J Plast Reconstr Aesthet Surg. 2010;63:493–498. doi: 10.1016/j.bjps.2008.11.070. [DOI] [PubMed] [Google Scholar]
- 10.Tasman A.J. The psychological aspects of rhinoplasty. Curr Opin Otalaryngol Head Neck Surg. 2010;18:290–294. doi: 10.1097/MOO.0b013e32833b51e6. [DOI] [PubMed] [Google Scholar]
- 11.Slupchynskyj O., Gieniusz M. Rhinoplasty for African American patients: a retrospective review of 75 cases. Arch Facial Plast Surg. 2008;10:232–236. doi: 10.1001/archfaci.10.4.232. [DOI] [PubMed] [Google Scholar]
- 12.Hellings P.W., Trenité G.J.N. Long-term patient satisfaction after revision rhinoplasty. Laryngoscope. 2007;117:985–989. doi: 10.1097/MLG.0b013e31804f8152. [DOI] [PubMed] [Google Scholar]
- 13.Zojaji R., Javanbakht M., Ghanadan A., Hosien H., Sadeghi H. High prevalence of personality abnormalities in patients seeking rhinoplasty. Otolaryngol Head Neck Surg. 2007;137:83–87. doi: 10.1016/j.otohns.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 14.Veale D., Haro L.D., Lambrou C. Cosmetic rhinoplasty in body dysmorphic disorder. Br J Plast Surg. 2003;56:546–551. doi: 10.1016/s0007-1226(03)00209-1. [DOI] [PubMed] [Google Scholar]
- 15.Hern J., Hamann J., Tostevin P., Rowe-Jones J., Hinton A. Assessing psychological morbidity in patients with nasal deformity using the CORE® questionnaire. Clin Otolaryngol Allied Sci. 2002;27:359–364. doi: 10.1046/j.1365-2273.2002.00595.x. [DOI] [PubMed] [Google Scholar]
- 16.Kosowski T.R., McCarthy C., Reavey P.L. A systematic review of patient-reported outcome measures after facial cosmetic surgery and/or nonsurgical facial rejuvenation. Plast Reconstr Surg. 2009;123:1819–1827. doi: 10.1097/PRS.0b013e3181a3f361. [DOI] [PubMed] [Google Scholar]
- 17.Lohuis P.J.F.M., Hakim S., Duivesteijn W., Knobbe A., Tasman A.J. Benefits of a short, practical questionnaire to measure subjective perception of nasal appearance after aesthetic rhinoplasty. Plast Reconstr Surg. 2013;132:913–923. doi: 10.1097/01.prs.0000434403.83692.95. [DOI] [PubMed] [Google Scholar]
- 18.Izu S.C., Kosugi E.M., Lopes A.S. Validation of the rhinoplasty outcomes evaluation (ROE) questionnaire adapted to Brazilian Portuguese. Qual Life Res. 2014;23:953–958. doi: 10.1007/s11136-013-0539-x. [DOI] [PubMed] [Google Scholar]
- 19.Cingi C., Toros S.Z., Cakli H., Gürbüz M.K. Patient-reported outcomes after endonasal rhinoplasty for the long nose. J Craniofac Surg. 2013;24:1002–1006. doi: 10.1097/SCS.0b013e31829024db. [DOI] [PubMed] [Google Scholar]
- 20.Rhee J.S. Measuring outcomes in nasal surgery: realities and possibilities. Arch Facial Plast Surg. 2009;11:416–419. doi: 10.1001/archfacial.2009.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Litner J.A., Rotenberg B.W., Dennis M., Adamson P.A. Impact of cosmetic facial surgery on satisfaction with appearance and quality of life. Arch Facial Plast Surg. 2008;10:79–83. doi: 10.1001/archfaci.10.2.79. [DOI] [PubMed] [Google Scholar]