Key Points
Question
Is developmentally adapted cognitive processing therapy more effective than a wait-list condition with treatment advice in adolescents and young adults with posttraumatic stress disorder related to childhood sexual and/or physical abuse?
Findings
In a multicenter, randomized clinical trial of 88 participants (aged 14-21 years), developmentally adapted cognitive processing therapy resulted in greater improvement in blinded, rater-assessed posttraumatic stress disorder severity and in self-reported secondary outcomes than a wait-list condition with treatment advice. Treatment success was greatest during the trauma-focused core phase and remained stable to the 3-month follow-up.
Meaning
Developmentally adapted cognitive processing therapy is more effective than a wait-list condition with treatment advice and well tolerated in adolescents and young adults with abuse-related posttraumatic stress disorder.
This multicenter randomized clinical trial examines whether developmentally adapted cognitive processing therapy is more effective than a wait-list condition with treatment advice among adolescents with symptoms of posttraumatic stress disorder related to childhood sexual and/or physical abuse.
Abstract
Importance
Despite the high prevalence, evidence-based treatments for abuse-related posttraumatic stress disorder (PTSD) in adolescents have rarely been studied.
Objective
To examine whether developmentally adapted cognitive processing therapy (D-CPT) is more effective than a wait-list condition with treatment advice (WL/TA) among adolescents with PTSD related to childhood abuse.
Design, Setting, and Participants
This rater-blinded, multicenter, randomized clinical trial (stratified by center) enrolled treatment-seeking adolescents and young adults (aged 14-21 years) with childhood abuse–related PTSD at 3 university outpatient clinics in Germany from July 2013 to June 2015, with the last follow-up interview conducted by May 2016. Of 194 patients, 88 were eligible for randomization.
Interventions
Participants received D-CPT or WL/TA. Cognitive processing therapy was enhanced by a motivational and alliance-building phase, by including emotion regulation and consideration of typical developmental tasks, and by higher session frequency in the trauma-focused core CPT phase. In WL/TA, participants received treatment advice with respective recommendations of clinicians and were offered D-CPT after 7 months.
Main Outcomes and Measures
All outcomes were assessed before treatment (baseline), approximately 8 weeks after the start of treatment, after the end of treatment (posttreatment), and at the 3-month follow-up. The primary outcome, PTSD symptom severity, was assessed in clinical interview (Clinician-Administered PTSD Scale for Children and Adolescents for DSM-IV [CAPS-CA]). Secondary outcomes were self-reported PTSD severity, depression, borderline symptoms, behavior problems, and dissociation.
Results
The 88 participants (75 [85%] female) had a mean age of 18.1 years (95% CI, 17.6-18.6 years). In the intention-to-treat analysis, the 44 participants receiving D-CPT (39 [89%] female) demonstrated greater improvement than the 44 WL/TA participants (36 [82%] female) in terms of PTSD severity (mean CAPS-CA scores, 24.7 [95% CI, 16.6-32.7] vs 47.5 [95% CI, 37.9-57.1]; Hedges g = 0.90). This difference was maintained through the follow-up (mean CAPS-CA scores, 25.9 [95% CI, 16.2-35.6] vs 47.3 [95% CI, 37.8-56.8]; Hedges g = 0.80). Treatment success was greatest during the trauma-focused core phase. The D-CPT participants also showed greater and stable improvement in all secondary outcomes, with between-groups effect sizes ranging from 0.65 to 1.08 at the posttreatment assessment (eg, for borderline symptoms, 14.1 [95% CI, 8.0-20.2] vs 32.0 [95% CI, 23.8-40.2]; Hedges g = 0.91).
Conclusions and Relevance
Adolescents and young adults with abuse-related PTSD benefited more from D-CPT than from WL/TA. Treatment success was stable at the follow-up and generalized to borderline symptoms and other comorbidities.
Trial Registration
German Clinical Trials Register identifier: DRKS00004787
Introduction
Numerous studies document the high prevalence of child sexual and/or physical abuse and its detrimental consequences for mental health.1,2 In particular, child sexual abuse is not only related to posttraumatic stress disorder (PTSD) but to depression, anxiety, suicide attempts, substance use, sexual risk-taking, health problems, and welfare dependence in adulthood.3,4 The probability of PTSD is especially high, with prevalence rates in adolescents ranging from 31% for physical abuse to 41% for rape.5
Cognitive processing therapy (CPT)6,7 is one of the most extensively studied treatments for adult PTSD. Meta-analyses8,9 indicate that cognitive interventions yield large effect sizes. Until the present, CPT has rarely been tested in traumatized youth and has not been adapted to the specific needs of young people with a history of abuse.
Recent meta-analyses of PTSD treatment in youth10,11,12 reported large overall effect sizes when compared with a wait-list condition or no treatment (eg, Hedges g = 0.89) and moderate effect sizes when compared with treatment as usual or active control conditions (Hedges g = 0.45).11 Results for controlled outcomes focusing exclusively on child sexual and/or physical abuse–related symptoms in adolescents are still scarce. To our knowledge, only 1 randomized clinical trial (RCT) specifically targeted adolescents with PTSD after child sexual abuse; Foa and colleagues13 found greater improvement in PTSD symptom severity and several secondary outcomes when comparing prolonged exposure with supportive counseling in 61 adolescent girls.
In a previous uncontrolled pilot study, Matulis et al14 adapted CPT to adolescents with child sexual and/or physical abuse–related PTSD (developmentally adapted CPT [D-CPT]) and successfully evaluated its effects. We therefore hypothesized that D-CPT would be superior to a wait-list condition with treatment advice (WL/TA) at posttreatment and 3-month follow-up assessments in reducing interviewer-assessed PTSD severity, self-reported PTSD severity, depression, dissociative experiences, borderline symptoms, and behavior problems.
Methods
More details on this open rater-blinded, multicenter, 2-armed RCT with 4 major assessment points (for D-CPT, at baseline, after emotion regulation, posttreatment, and 3 months after the end of treatment; for WL/TA, at baseline and 2, 4, and 7 months after baseline) can be found in the study protocol in Supplement 1.15 The study was approved by the institutional review boards of Catholic University Eichstätt-Ingolstadt, Eichstätt, Germany; the Freie Universitaet of Berlin, Berlin, Germany; and the Goethe University Frankfurt, Frankfurt am Main, Germany. Written informed consent was obtained from all participants and from parents or guardians of minors.
Participants
Participants were adolescents and young adults (aged 14-21 years) seeking treatment at 3 university outpatient clinics in Germany and enrolled from July 23, 2013, through June 17, 2015. A primary diagnosis of child sexual and/or physical abuse–related PTSD was required for inclusion. In light of the ongoing discussion on diagnostic criteria for PTSD in children and adolescents,16 the diagnostic threshold for PTSD diagnosis was lowered; participants had to present a minimum of 2 avoidance symptoms in the clinical interview instead of the 3 defined in the DSM-IV-TR.17 Moreover, to be included, participants had to have sufficient German language skills, had to be receiving no or stable psychopharmacological medication (for ≥3 weeks), and had to have stable living conditions (ie, no ongoing abuse and not homeless). Exclusion criteria were current severe suicidality or severe and life-threatening suicidality or self-harming behavior within the last 6 months, an IQ of 75 or less, and/or any documented pervasive developmental disorder, concurrent psychotherapy, and the following diagnoses according to DSM-IV-TR: lifetime psychotic or bipolar disorder (unclear cases were included), current substance dependence (abstinence <6 months), or a substance-induced disorder.
Procedure
Sample size estimations controlled for type I error to 5% with statistical power of 0.8. For WL/TA, we estimated baseline to posttreatment effect sizes of Cohen d = 0.3 based on the effect sizes available then for supportive interventions.18 A baseline to posttreatment Cohen d effect size of 0.9 was assumed for D-CPT.19 Not accounting for attrition, 2 groups of 45 participants were required for the trial.
Participants were recruited through referrals from therapists, psychiatric clinics, or youth welfare institutions as well as flyers and press releases. Potential participants underwent screening using a self-report measure of PTSD. Adolescents who met immediately checkable inclusion criteria were invited for further baseline assessment. At this point, informed consent was obtained from them and—in the case of minors—from their parents or legal guardians. For randomization, study coordinators received individual allocations per automated email to ensure allocation concealment (the randomization list was generated independently with SAS/STAT software [version 9.3; SAS Institute Inc] following a simple random design, stratified by study center).
Assessment
Interviewers blinded to treatment condition administered all measures at separate appointments, including a checklist concerning serious adverse events. To improve reliability, interviewer training included the rating of training videos presenting criterion B of the Clinician-Administered PTSD Scale for Children and Adolescents for DSM-IV (CAPS-CA), which interviewers found the most difficult, and 2 frequently occurring diagnoses from the Structured Clinical Interview for DSM-IV (SCID), sections A and F (major depressive episode and social phobia). Participants each received €20 (US $23) for attending the midtreatment and posttreatment assessments and €30 (US $35) for attending the follow-up assessment.
Primary Outcome
Severity of PTSD was measured at each assessment point using the CAPS-CA.20,21 This structured clinical interview rates frequency and intensity of PTSD symptoms on a scale ranging from 0 (never/no problem) to 4 (most of the time/extreme), with a total score ranging from 0 to 136.
Secondary Outcomes
A self-rating of PTSD symptoms was obtained weekly during D-CPT and at every assessment point using the University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index (UCLA-PTSD-RI22,23; range, 0-68, with higher scores indicating greater severity of symptoms). At the pretreatment and posttreatment assessments and at follow-up, comorbidity was assessed using the SCID-I24 and SCID-II,25,26 borderline personality disorder only,26 complemented by parts of the Diagnostic Interview for Mental Disorders in Childhood and Adolescence27 and the nicotine section of the Expert System for Diagnosing Mental Disorders.28 Further secondary outcomes that were assessed were the following:
Beck Depression Inventory29,30 (range, 0-63, with higher scores indicating greater severity of symptoms)
Borderline Symptom List 2331 (range, 0-92, with higher scores indicating greater severity of symptoms)
Youth Self-report32,33 (range, 0-202, with higher scores indicating greater severity of symptoms)
Adolescent Dissociative Experiences Scale34,35 (range, 0-300, with higher scores indicating greater severity of symptoms)
Additional exploratory variables not presented herein are given in the study protocol in Supplement 1.15
Treatments
Treatment was delivered by 14 master-level or postdoctoral therapists (including J.G.; 10 female), with 10 licensed psychotherapists and 4 in training. Therapists had a mean (SD) of 46.1 (19.3) months of clinical experience, with 3.3 (5.6) cases of PTSD. All therapists treated 1 training case to familiarize themselves with D-CPT before entering the trial.
Therapists attended a 3-day workshop in D-CPT and a later refresher workshop. Treatment sessions were videotaped. Therapeutic adherence was ensured by weekly local supervisions administered by 3 of us (R.R., B.R., and R.S.). In addition, therapists were invited to a joint biweekly telephone case consultation. Therapeutic adherence and therapeutic competence in D-CPT were assessed by 2 trained raters (J.G. and F.S.). Results reflected good therapeutic adherence and competence (based on 2 sessions per case) (eMethods in Supplement 2).
We adapted CPT to the needs of adolescents and young adults after sexual and/or physical abuse by (1) beginning with a commitment phase to enhance treatment motivation and therapeutic alliance and to establish the formal framework for administering therapy; (2) integrating emotion management techniques36,37 early in D-CPT; (3) increasing treatment intensity by administering the middle part of the therapeutic protocol (ie, actual CPT) at a high frequency (approximately 15 sessions in 4 weeks) to address the fluctuating motivation in adolescents38; and (4) giving special consideration to developmental tasks, such as career choice and romantic relationships, because adolescent patients are at risk of dropping out of school, starting relationships with abusive partners, or being abused again. Altogether, D-CPT was to be completed in thirty 50-minute sessions (with 6 optional sessions, eg, with a caregiver or for crisis intervention) in 16 to 20 weeks (eTable 1 in Supplement 2). More on the rationale for adapting CPT can be found in Matulis et al.14
Participants in WL/TA were advised to seek treatment outside the trial. In line with suggestions of the institutional review boards, D-CPT was offered to these participants after the 3-month follow-up. For standardization, we developed a protocol for how study coordinators should instruct participants to find a psychotherapist. Because treatment costs in Germany are covered by health insurance, psychotherapy was accessible to each participant. Interventions in the WL/TA group were recorded in detail.
Statistical Analysis
Follow-up was completed by May 31, 2016, and data were analyzed according to the intention-to-treat approach. Before unblinding, the original analysis plan was adapted to more sophisticated missing value treatment (eMethods in Supplement 2). Statistical analysis was performed in the following 3 steps. First, potential sampling bias due to dropout was scrutinized by pattern mixture models classifying participants according to their pattern of missing values for the 4 major assessment points (baseline, midtreatment, posttreatment, and follow-up). No hint of selection bias was found. Second, the main study hypothesis was evaluated using a random-coefficient model, with time as piecewise level 1 regressor variables within participants (level 2), to allow for nonlinear shapes of therapeutic progress (see also Foa and colleagues13 for this approach). Each participant contributed 4 or fewer records to the data set. Calculations for pattern mixture models were achieved by SAS Proc Mixed (version 9.3; SAS Institute Inc). Piecewise hierarchical modeling was performed using HLM software (version 7.03; Scientific Software International, Inc) growth curve modeling. Third, we calculated effect sizes for differences between WL/TA and D-CPT groups by performing the respective contrast 2-tailed, unpaired t tests between groups (at midtreatment, posttreatment, and follow-up assessments using Hedges g) or separately for both groups (baseline vs later measurements using Cohen d).
Results
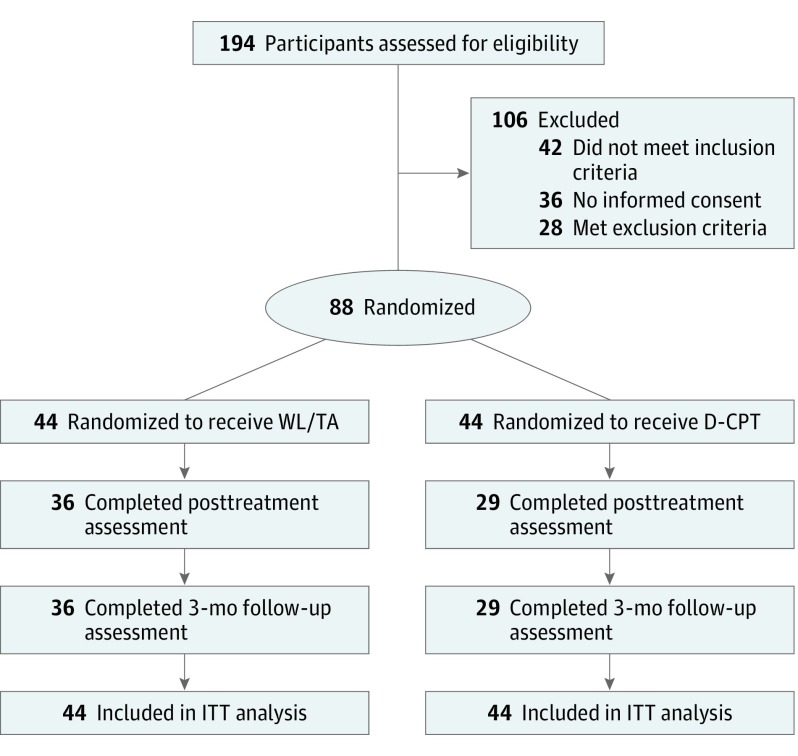
A total of 88 participants (75 female [85%] and 13 male [15%]; mean age, 18.1 years [95% CI, 17.6-18.6 years]) were enrolled from July 23, 2013, through June 17, 2015 (Figure 1). Participants in the D-CPT group attended a mean (SD) of 25.4 (11.6) sessions (range, 0-36); completers attended a mean (SD) of 31.6 (3.3) sessions (range, 19-36). Early completion of D-CPT required the therapist and patient to agree that treatment aims had been reached. Two D-CPT participants dropped out before the first therapy session, 2 during the commitment phase, 5 during emotion regulation phase, and 3 during the core CPT phase. Of the 12 D-CPT dropouts (27%), 5 had been erroneously randomized (eg, having substance dependence revealed later or having invented the trauma) and were offered alternative treatment or referral. In terms of primary outcome, 8 D-CPT participants missed the midtreatment assessment and 15 missed the posttreatment and follow-up assessments. In the WL/TA group, 24 participants received no further treatment (55%; some of them waiting to be admitted to D-CPT), and 12 received some kind of psychosocial support and/or psychological or psychiatric treatment (27%), with 8 participants reporting that the trauma was addressed. In terms of primary outcome, 8 WL/TA participants (18%) did not complete the posttreatment and/or follow-up assessment. The last follow-up interview was conducted by May 31, 2016.
Figure 1. CONSORT Diagram of Participant Flow.
D-CPT indicates developmentally adapted cognitive processing therapy; ITT, intention-to-treat; and WL/TA, wait-list/treatment advice.
Table 1 contains demographic data, and Table 2 gives symptom scores. No significant differences between the D-CPT and WL/TA groups at baseline (no adjustment for type I error risk inflation), except for higher WL/TA scores for dissociation (mean Adolescent Dissociative Experiences Scale scores, 99.3 [95% CI, 82.1-116.4] vs 75.4 [95% CI, 59.1-91.7]) and prevalence of nicotine dependence (22 [50%] vs 11 [25%]), occurred.
Table 1. Demographic Variablesa.
| Characteristic | Study Population | P Value | ||
|---|---|---|---|---|
| All (N = 88) | D-CPT Group (n = 44) | WL/TA Group (n = 44) | ||
| Age, mean (95% CI), y | 18.1 (17.6-18.6) | 18.2 (17.5-18.8) | 18.1 (17.4-18.7) | .82b |
| Female, No. (%) | 75 (85) | 39 (89) | 36 (82) | .37c |
| Immigration background, No. (%) | 23 (26) | 13 (30) | 10 (23) | .47c |
| Subthreshold PTSD, No. (%)d | 11 (12) | 5 (11) | 6 (14) | .75c |
| Comorbid DSM-IV disorders, No. (%)e | ||||
| 0 | 18 (20) | 10 (23) | 8 (18) | .60c |
| 1 or 2 | 41 (47) | 23 (52) | 18 (41) | .28c |
| ≥3 | 29 (33) | 11 (25) | 18 (41) | .11c |
| Most frequent DSM-IV disorders, No. (%) | ||||
| Mood disorders | 44 (50) | 21 (48) | 23 (52) | .67c |
| Anxiety disorders | 35 (40) | 14 (32) | 21 (48) | .13c |
| Nicotine dependence | 33 (38) | 11 (25) | 22 (50) | .02c |
| Borderline personality disorder | 14 (16) | 5 (11) | 9 (20) | .24c |
| No. of suicide attempts before treatment, mean (95% CI) | 1.0 (0.4-1.6) | 0.7 (0.3-1.5) | 1.3 (0.5-2.4) | .35b |
| Out-of-home placement or institutional care, No. (%) | 25 (28) | 11 (25) | 14 (32) | .44c |
Abbreviations: D-CPT, developmentally adapted cognitive processing therapy; PTSD, posttraumatic stress disorder; WL/TA, wait-list/treatment advice.
Intention-to-treat sample.
Calculated from independent, 2-sided unpaired t test.
Calculated from Pearson χ2 test.
Subthreshold PTSD was defined as having 2 avoidance symptoms (all else according to DSM-IV-TR).
Includes nicotine dependence and borderline personality disorder.
Table 2. Primary and Secondary Outcomes at All Assessment Points.
| Assessment Point | All (N = 88) | D-CPT Group (n = 44) | WL/TA Group (n = 44) | Effect Size, Hedges g | |||
|---|---|---|---|---|---|---|---|
| No. of Participants | Assessment Data, Mean Score (95% CI) |
No. of Participants | Assessment Data, Mean Score (95% CI) |
No. of Participants | Assessment Data, Mean Score (95% CI) |
||
| Primary Outcome | |||||||
| Interviewer-rated PTSD, CAPS-CAa | |||||||
| Baseline | 88 | 65.6 (60.9-70.3) | 44 | 65.6 (58.5-72.8) | 44 | 65.5 (59.2-71.9) | 0.00 |
| Midtreatment | 77 | 57.0 (51.2-62.8) | 36 | 56.9 (48.8-65.0) | 41 | 57.2 (48.6-65.8) | 0.01 |
| Posttreatment | 65 | 37.3 (30.4-44.2) | 29 | 24.7 (16.6-32.7) | 36 | 47.5 (37.9-57.1) | 0.90 |
| 3-mo Follow-up | 65 | 37.8 (30.6-44.9) | 29 | 25.9 (16.2-35.6) | 36 | 47.3 (37.8-56.8) | 0.80 |
| Clinically relevant response, No. (%) | |||||||
| Posttreatment | 65 | 14 (22) | 29 | 11 (38) | 36 | 3 (8) | NA |
| 3-mo Follow-up | 65 | 14 (22) | 29 | 11 (38) | 36 | 3 (8) | NA |
| Secondary Outcomes | |||||||
| Self-reported PTSD, UCLA-PTSD-RIb | |||||||
| Baseline | 88 | 42.2 (39.6-44.8) | 44 | 41.2 (37.8-44.6) | 44 | 43.2 (39.2-47.2) | 0.17 |
| Posttreatment | 59 | 27.3 (22.7-32.0) | 27 | 18.1 (12.4-23.8) | 32 | 35.1 (29.0-41.2) | 1.08 |
| 3-mo Follow-up | 60 | 27.8 (23.2-32.4) | 25 | 16.1 (9.8-22.4) | 35 | 36.1 (31.1-41.1) | 1.35 |
| Depression, BDI-IIc | |||||||
| Baseline | 86 | 28.8 (25.9-31.6) | 44 | 27.5 (23.7-31.2) | 42 | 30.1 (25.6-34.6) | 0.20 |
| Posttreatment | 60 | 19.7 (15.9-23.5) | 28 | 12.8 (8.0-17.6) | 32 | 25.8 (20.7-30.9) | 0.98 |
| 3-mo Follow-up | 59 | 18.8 (14.5-23.1) | 25 | 11.6 (5.6-17.6) | 34 | 24.1 (18.5-29.6) | 0.81 |
| Borderline symptom severity, BSL-23d | |||||||
| Baseline | 87 | 38.0 (33.3-42.8) | 44 | 35.8 (29.4-42.2) | 43 | 40.3 (33.1-47.5) | 0.20 |
| Posttreatment | 59 | 23.8 (18.2-29.4) | 27 | 14.1 (8.0-20.2) | 32 | 32.0 (23.8-40.2) | 0.91 |
| 3-mo Follow-up | 60 | 23.3 (17.6-29.0) | 25 | 14.4 (5.6-23.1) | 35 | 29.7 (22.7-36.8) | 0.74 |
| Behavior problems, YSRe | |||||||
| Baseline | 86 | 69.7 (64.8-74.5) | 44 | 66.7 (61.0-72.4) | 42 | 72.8 (64.8-80.8) | 0.27 |
| Posttreatment | 60 | 53.2 (46.0-60.4) | 28 | 40.1 (30.2-50.1) | 32 | 64.6 (55.7-73.6) | 0.97 |
| 3-mo Follow-up | 60 | 48.7 (41.7-55.7) | 25 | 34.7 (24.4-44.9) | 35 | 58.7 (50.4-67.1) | 1.00 |
| Dissociation, A-DESf | |||||||
| Baseline | 87 | 87.2 (75.3-99.1) | 44 | 75.4 (59.1-91.7) | 43 | 99.3 (82.1-116.4) | 0.44 |
| Posttreatment | 60 | 60.4 (47.1-73.6) | 28 | 43.4 (25.6-61.1) | 32 | 75.2 (56.6-93.8) | 0.65 |
| 3-mo Follow-up | 60 | 53.2 (39.7-66.7) | 25 | 27.5 (13.1-42.0) | 35 | 71.6 (52.6-90.6) | 0.92 |
Abbreviations: A-DES, Adolescent Dissociative Experiences Scale; BDI-II, Beck Depression Inventory–II; BSL-23, Borderline Symptom List 23; CAPS-CA, Clinician-Administered PTSD Scale for Children and Adolescents for DSM-IV; D-CPT, developmentally adapted cognitive processing therapy; NA, not applicable; PTSD, posttraumatic stress disorder; UCLA-PTSD-RI, University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index; WL/TA, wait-list/treatment advice; YSR, Youth Self-report.
Scores range from 0 to 136, with higher scores indicating greater severity of symptoms.
Scores range from 0 to 68, with higher scores indicating greater severity of symptoms.
Scores range from 0 to 63, with higher scores indicating greater severity of symptoms.
Scores range from 0 to 92, with higher scores indicating greater severity of symptoms.
Scores range from 0 to 202, with higher scores indicating greater severity of symptoms.
Scores range from 0 to 300, with higher scores indicating greater severity of symptoms.
Primary Outcome
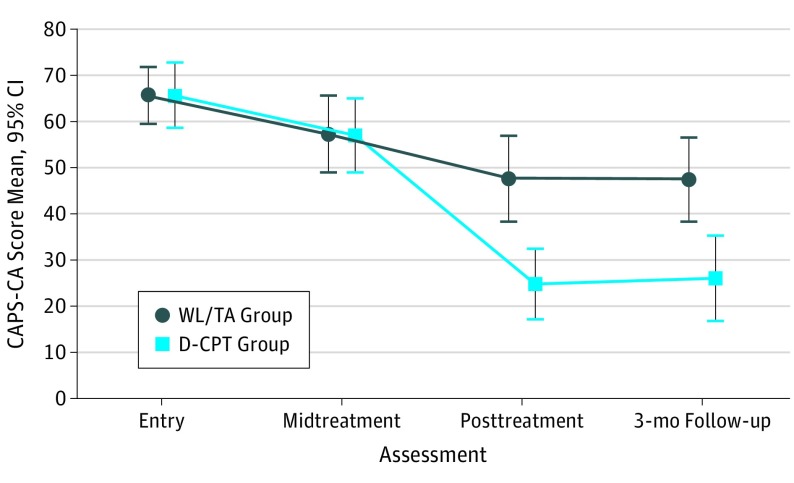
Including all participants undergoing measurement at the respective time point yielded the mean CAPS-CA scores indicated in Table 2 (see also Figure 2). The midtreatment assessment was reached after a mean (SD) of 83 (27) days from study entry; posttreatment assessment, 173 (42) days; and follow-up assessment, 261 (49) days. We found no significant differences between conditions.
Figure 2. Clinician-Administered Posttraumatic Stress Disorder Scale for Children and Adolescents for DSM-IV (CAPS-CA) by Assessment Point.
Scores for the CAPS-CA range from 0 to 136, with higher scores indicating greater severity of PTSD. D-CPT indicates developmentally adapted cognitive processing therapy; WL/TA, wait-list/treatment advice.
Both groups showed a significant reduction in PTSD symptom severity (CAPS-CA) between study entry and the posttreatment assessment (D-CPT: t28 = 9.87 [P < .001; Cohen d = 1.83]; WL/TA: t35 = 6.10 [P < .001; Cohen d = 1.02]). However, D-CPT resulted in a considerably better outcome in comparison with WL/TA (mean CAPS-CA score at posttreatment assessment, 24.7 [95% CI, 16.6-32.7] vs 47.5 [95% CI, 37.9-57.1]; between-groups Hedges g = 0.90) (Table 2). Between the posttreatment and follow-up assessments, treatment gains were stable, with the advantage for D-CPT maintained (mean CAPS-CA scores at 3-month follow-up, 25.9 [95% CI, 16.2-35.6] vs 47.3 [95% CI, 37.8-56.8]; Hedges g = 0.80).
Piecewise regression analysis permits a more fine-grained inspection (Table 3). Starting from individual initial levels of symptom load (β00), a slight uniform reduction of symptom load of 0.07 points per day (β10) occurred to the midtreatment assessment. After the midtreatment assessment, which marks the beginning of the CPT phase in the D-CPT condition, both groups showed larger reductions (β20) in individual shapes, but in D-CPT this general effect was nearly doubled (β21). Between the posttreatment and follow-up assessments, a further individually varying improvement was observed among both groups (β30), but again with clear superiority of D-CPT (β31). The final regression model was not improved by adjusting for potentially confounding effects (treatment center, age, sex, and pattern of missing values).
Table 3. Final Piecewise Linear Random Coefficient Regression Model on PTSD Severity Scorea.
| Effect | Coefficient | Estimate (SE) | Wald Test (df) | P Value |
|---|---|---|---|---|
| Global intercept | Random β00 | 63.1253 (2.4297) | 25.638 (87) | <.001 |
| Slope from entry to midtreatment assessment | Fixed β10 | −0.0685 (0.0218) | −3.146 (30) | .005 |
| Slope from midtreatment to posttreatment assessments | Random β20 | −0.1877 (0.0318) | −5.907 (86) | <.001 |
| Influence of D-CPT on slope from midtreatment to posttreatment assessments | Random β21 | −0.1638 (0.0434) | −3.773 (86) | <.001 |
| Slope from posttreatment to 3-mo follow-up assessments | Random β30 | −0.2211 (0.0358) | −6.171 (86) | <.001 |
| Influence of D-CPT on slope from posttreatment to 3-mo follow-up assessments | Random β31 | −0.1912 (0.0636) | −3.004 (86) | .003 |
Abbreviations: D-CPT, developmentally adapted cognitive processing therapy; PTSD, posttraumatic stress disorder.
Calculated using the Clinician-Administered PTSD Scale for Children and Adolescents for DSM-IV and expressed as significant variance components for global intercept, slope from midtreatment to posttreatment assessment, and slope from posttreatment to 3-month follow-up assessment (all P < .03).
To permit comparison with published studies on adolescents, additional analyses were performed by age, splitting the sample into the following 2 groups: younger than 18 years (n = 40) and 18 years or older (n = 48). The results were similar, although younger participants seemed to profit more from D-CPT (eTable 2 in Supplement 2).
Secondary Outcomes
Self-reported PTSD symptom severity (UCLA-PTSD-RI score) corresponded with the results from blinded, interview-rated PTSD assessment, displaying the same pattern of improvement but with somewhat larger between-groups effect sizes at the posttreatment (mean scores, 18.1 [95% CI, 12.4-23.8] vs 35.1 [95% CI, 29.0-41.2]; Hedges g = 1.08) and follow-up (mean scores, 16.1 [95% CI, 9.8-22.4] vs 36.1 [95% CI, 31.1-41.1]; Hedges g = 1.35) assessments. Also, participants in both groups improved significantly from pretreatment to posttreatment assessments in all other secondary outcomes, but again D-CPT resulted in more and stable treatment gains, with between-groups effect sizes ranging from 0.65 for Adolescent Dissociative Experiences Scale (mean scores, 43.4 [95% CI, 25.6-61.1] vs 75.2 [95% CI, 56.6-93.8]) to 0.98 for Beck Depression Inventory–II (mean scores, 12.8 [95% CI, 8.0-17.6] vs 25.8 [95% CI, 20.7-30.9]) at the posttreatment assessment and 0.74 for the Borderline Symptom List 23 (mean scores, 14.4 [95% CI, 5.6-23.1] vs 29.7 [95% CI, 22.7-36.8]) to 1.00 for Youth Self-report (mean scores, 34.7 [95% CI, 24.4-44.9] vs 58.7 [95% CI, 50.4-67.1]) at the follow-up assessment (Table 2).
Clinically Relevant Response
A clinically relevant or good response was defined as an improvement of at least 2 SD39 below baseline in interview-rated PTSD scores (CAPS-CA) at the posttreatment and/or follow-up assessments. Altogether, 15 participants in the D-CPT group (34% of the intention-to-treat subsample) showed a good response as opposed to 4 in WL/TA (9%) (χ2 = 12.26; P < .001 [n = 69]) (for details, see Table 2). Twenty participants could not improve this much per definition because they started treatment with scores below the cutoff of 2 SD. No clinically relevant worsening of symptoms was observed.
In terms of rater-based serious adverse event assessment according to the International Council for Harmonization Guideline for Good Clinical Practice,40 1 D-CPT participant was admitted to the hospital (for a somatic reason unrelated to the study) vs 6 WL/TA participants. Another D-CPT participant was admitted to inpatient psychiatric treatment vs 6 WL/TA participants. One WL/TA participant attempted suicide. In 11 cases, data were missing at the midtreatment assessment and in 23 cases at the posttreatment assessment.
Discussion
In this multicenter RCT with 88 adolescents and young adults, participants in D-CPT reported more improvement in PTSD symptoms assessed in clinical interviews and in self-report than those receiving WL/TA, with a higher rate of clinically relevant responses. Effect sizes for differences between the 2 interventions were large, with Hedges g values of 0.90 at the posttreatment and 0.80 at the follow-up assessments. Moreover, participants in D-CPT demonstrated greater improvements in all secondary outcomes (depression, borderline symptom severity, behavior problems, and dissociation). These results are comparable to effect sizes reported for CPT in adults8 and to overall effect sizes reported in meta-analyses on PTSD treatment for children and adolescents.11,12 For depression, effect sizes of 0.37 (compared with active controls) and 0.60 (compared with a wait-list condition) were reported,11 whereas we found a large effect size of 0.98 for reduction of depressive symptoms. We also found a substantial effect size for borderline symptoms (0.91), whereas a recent meta-analysis with adult samples reported an effect size of 0.35.41 Early PTSD treatment might help to prevent borderline symptoms from becoming chronic.
From the piecewise regression, it became evident that the most effective part of D-CPT is the high-intensity CPT phase starting at the midtreatment assessment. Improvements during the first 2 phases of treatment (commitment and emotion regulation) did not differ from those during WL/TA. This finding further challenges the need for a stabilization phase or emotion regulation training before trauma-focused treatment, at least in adolescents with abuse-related PTSD (De Jongh and colleagues42 discuss current recommendations for complex PTSD in adults).
The only other study we found on treating abuse-related PTSD in young people did not include an emotion regulation phase.13 However, in this trial by Foa and colleagues,13 preparatory sessions to address case management issues preceded randomization, which led to the exclusion of 29 eligible girls. We decided to randomize all eligible participants for the purpose of generalizability instead. Therefore, when interpreting D-CPT’s dropout rate of 27% (n = 12), one should take into account that 5 participants were erroneously enrolled; they had to be referred elsewhere or dropped out when therapeutic focus needed to change. Our results are not directly comparable to those of the study by Foa et al13 for several other reasons. Foa et al13 only included girls who had experienced sexual abuse, used a different set of outcome measures, evaluated another trauma-focused treatment (prolonged exposure), and used a different control condition (supportive counseling). However, both interventions showed large between-groups effect sizes for their primary outcomes. In both studies, pretreatment to posttreatement differences in controls were substantial too. This finding might be especially surprising in our study, where most WL/TA participants did not receive any treatment. These findings are in line with the results of 2 other published European multicenter trials43,44 that applied similar methods (eg, CAPS-CA as primary outcome) but targeted PTSD after miscellaneous trauma in children and adolescents. Effect sizes in control groups were also large (0.88 for treatment as usual44; 0.88 for waitlist43). Some methodologic issues in these studies (ie, the prospect of receiving treatment after the waiting period, but also extensive preassessment) might encourage more constructive symptom management. Moreover, in our study, one-third of WL/TA participants received some kind of professional support, with 8 reporting that the trauma was addressed.
Strengths and Limitations
This RCT has several strengths. It followed a rigorous design, with the primary outcome assessed in clinical interviews by blinded raters, and was performed in a naturalistic setting with 14 therapists providing treatment. Unlike most studies in the field, we extended the participants’ age range to 21 years in accordance with German health care, where youth as old as 21 years may be treated by child therapists. To permit comparisons with other studies, we provide results for both age groups, adolescents vs young adults. Limitations of the trial are the still rather small and predominantly female (85%) sample. Excluding participants with recent severe, life-threatening behaviors and participants with substance dependence with less than 6 months of abstinence might further limit overall generalizability. Regarding treatment fidelity ratings, allegiance bias might be considered. In addition, a 3-month follow-up does not provide information on long-term effects. Finally, when interpreting the between-groups effect sizes, the heterogeneous nature of our control group, which did not control for treatment dosage, should be kept in mind. However, recent RCTs reported similar effect sizes for wait-list and treatment as usual.43,44
Conclusions
Young people with abuse-related PTSD experienced greater benefit from D-CPT than from WL/TA. This advantage was stable to the 3-month follow-up. In future studies, dismantling designs should be used to further address the question as to whether emotion regulation training should precede trauma-focused interventions in this age group.
Trial Protocol
eMethods. Statistical Analysis and Treatment Integrity
eTable 1. Overview of D-CPT
eTable 2. Primary and Secondary Outcomes at All Assessment Points for Younger (<18 Years [n = 40]) and Older (18-21 Years [n = 48]) Age Groups
eReferences.
Data Sharing Statement
References
- 1.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68-81. doi: 10.1016/S0140-6736(08)61706-7 [DOI] [PubMed] [Google Scholar]
- 2.Sethi D, Bellis M, Hughes K, Gilbert R, Mitis F, Galea G. European Report on Preventing Child Maltreatment. Copenhagen, Denmark: World Health Organization, Regional Office for Europe; 2013. [Google Scholar]
- 3.Cutajar MC, Mullen PE, Ogloff JRP, Thomas SD, Wells DL, Spataro J. Psychopathology in a large cohort of sexually abused children followed up to 43 years. Child Abuse Negl. 2010;34(11):813-822. doi: 10.1016/j.chiabu.2010.04.004 [DOI] [PubMed] [Google Scholar]
- 4.Fergusson DM, McLeod GFH, Horwood LJ. Childhood sexual abuse and adult developmental outcomes: findings from a 30-year longitudinal study in New Zealand. Child Abuse Negl. 2013;37(9):664-674. doi: 10.1016/j.chiabu.2013.03.013 [DOI] [PubMed] [Google Scholar]
- 5.McLaughlin KA, Koenen KC, Hill ED, et al. . Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2013;52(8):815-830.e14. doi: 10.1016/j.jaac.2013.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resick PA, Nishith P, Griffin MG. How well does cognitive-behavioral therapy treat symptoms of complex PTSD? an examination of child sexual abuse survivors within a clinical trial. CNS Spectr. 2003;8(5):340-355. doi: 10.1017/S1092852900018605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Resick PA, Schnicke MK. Cognitive Processing Therapy for Rape Victims: A Treatment Manual. Newsbury Park, CA: Sage; 1993. [Google Scholar]
- 8.Lenz AS, Haktanir A, Callender K. Meta-analysis of trauma-focused therapies for treating the symptoms of posttraumatic stress disorder. J Couns Dev. 2017;95(3):339-353. doi: 10.1002/jcad.12148 [DOI] [Google Scholar]
- 9.Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J Clin Psychiatry. 2013;74(6):e541-e550. doi: 10.4088/JCP.12r08225 [DOI] [PubMed] [Google Scholar]
- 10.Gillies D, Maiocchi L, Bhandari AP, Taylor F, Gray C, O’Brien L. Psychological therapies for children and adolescents exposed to trauma. Cochrane Database Syst Rev. 2016;10:CD012371. doi: 10.1002/14651858.CD012371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gutermann J, Schreiber F, Matulis S, Schwartzkopff L, Deppe J, Steil R. Psychological treatments for symptoms of posttraumatic stress disorder in children, adolescents, and young adults: a meta-analysis. Clin Child Fam Psychol Rev. 2016;19(2):77-93. doi: 10.1007/s10567-016-0202-5 [DOI] [PubMed] [Google Scholar]
- 12.Morina N, Koerssen R, Pollet TV. Interventions for children and adolescents with posttraumatic stress disorder: a meta-analysis of comparative outcome studies. Clin Psychol Rev. 2016;47:41-54. doi: 10.1016/j.cpr.2016.05.006 [DOI] [PubMed] [Google Scholar]
- 13.Foa EB, McLean CP, Capaldi S, Rosenfield D. Prolonged exposure vs supportive counseling for sexual abuse-related PTSD in adolescent girls: a randomized clinical trial. JAMA. 2013;310(24):2650-2657. doi: 10.1001/jama.2013.282829 [DOI] [PubMed] [Google Scholar]
- 14.Matulis S, Resick PA, Rosner R, Steil R. Developmentally adapted cognitive processing therapy for adolescents suffering from posttraumatic stress disorder after childhood sexual or physical abuse: a pilot study. Clin Child Fam Psychol Rev. 2014;17(2):173-190. doi: 10.1007/s10567-013-0156-9 [DOI] [PubMed] [Google Scholar]
- 15.Rosner R, König H-H, Neuner F, Schmidt U, Steil R. Developmentally adapted cognitive processing therapy for adolescents and young adults with PTSD symptoms after physical and sexual abuse: study protocol for a randomized controlled trial. Trials. 2014;15:195. doi: 10.1186/1745-6215-15-195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen JA, Bukstein O, Walter H, et al. ; AACAP Work Group on Quality Issues . Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2010;49(4):414-430. [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 18.Deblinger E, Stauffer LB, Steer RA. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreat. 2001;6(4):332-343. doi: 10.1177/1077559501006004006 [DOI] [PubMed] [Google Scholar]
- 19.Harvey ST, Taylor JE. A meta-analysis of the effects of psychotherapy with sexually abused children and adolescents. Clin Psychol Rev. 2010;30(5):517-535. doi: 10.1016/j.cpr.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 20.Nader K, Kriegler JA, Blake DD. The Clinician-Administered PTSD Scale for Children and Adolescents for DSM-IV (CAPS-CA). White River Junction, VT: National Centre for PTSD; 2002. [Google Scholar]
- 21.Steil R, Füchsel G. Interviews zu Belastungsstörungen bei Kindern und Jugendlichen (IBS-KJ): Diagnostik der Akuten und der Posttraumatischen Belastungsstörung. Göttingen, Germany: Hogrefe; 2006. [Google Scholar]
- 22.Ruf M, Schauer M, Elbert T. UPID-UCLA PTSD index for DSM IV In: Barkmann C, Schulte Markwort M, Brähler E, eds. Fragebögen zur Diagnostik psychischer Störungen des Kindes- und Jugendalters. Göttingen, Germany: Hogrefe; 2010. [Google Scholar]
- 23.Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Curr Psychiatry Rep. 2004;6(2):96-100. doi: 10.1007/s11920-004-0048-2 [DOI] [PubMed] [Google Scholar]
- 24.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). New York, NY: Biometric Research Department; 1997. [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). New York, NY: Biometric Research Department; 1994. [Google Scholar]
- 26.Wittchen H-U, Zaudig M, Fydrich T. SKID: Strukturiertes klinisches Interview für DSM-IV: Achse I und II. Göttingen, Germany: Hogrefe; 1997. [Google Scholar]
- 27.Schneider S, Unnewehr S, Margraf J. Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter (Kinder-DIPS). 2nd ed Berlin, Germany: Springer; 2009. [Google Scholar]
- 28.Wittchen H-U, Pfister H. DIA-X-Interviews: Manual für Screening-Verfahren und Interview; Interviewheft. Frankfurt, Germany: Swets & Zeitlinger; 1997. [Google Scholar]
- 29.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 30.Hautzinger M, Keller F, Kühner C. Beck Depressions-Inventar (BDI-II) Revision. Frankfurt, Germany: Harcourt Test Services; 2006. [Google Scholar]
- 31.Bohus M, Kleindienst N, Limberger MF, et al. . The short version of the Borderline Symptom List (BSL-23): development and initial data on psychometric properties. Psychopathology. 2009;42(1):32-39. doi: 10.1159/000173701 [DOI] [PubMed] [Google Scholar]
- 32.Achenbach TM. Manual for the Youth Self-report and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 33.Döpfner M. Fragebogen für Jugendliche; deutsche Bearbeitung der Youth Self Report Form der Child Behavior Checklist (YSR). Köln, Germany: Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik; 1998. [Google Scholar]
- 34.Armstrong JG, Putnam FW, Carlson EB, Libero DZ, Smith SR. Development and validation of a measure of adolescent dissociation: the Adolescent Dissociative Experiences Scale. J Nerv Ment Dis. 1997;185(8):491-497. doi: 10.1097/00005053-199708000-00003 [DOI] [PubMed] [Google Scholar]
- 35.Brunner R, Resch F, Parzer P, Koch E. Heidelberger Dissoziations-Inventar (HDI): Manual. Frankfurt, Germany: Pearson; 2008. [Google Scholar]
- 36.Steil R, Dyer A, Priebe K, Kleindienst N, Bohus M. Dialectical behavior therapy for posttraumatic stress disorder related to childhood sexual abuse: a pilot study of an intensive residential treatment program. J Trauma Stress. 2011;24(1):102-106. doi: 10.1002/jts.20617 [DOI] [PubMed] [Google Scholar]
- 37.Bohus M, Dyer AS, Priebe K, et al. . Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: a randomised controlled trial. Psychother Psychosom. 2013;82(4):221-233. doi: 10.1159/000348451 [DOI] [PubMed] [Google Scholar]
- 38.Ehlers A, Clark DM, Hackmann A, et al. . Intensive cognitive therapy for PTSD: a feasibility study. Behav Cogn Psychother. 2010;38(4):383-398. doi: 10.1017/S1352465810000214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59(1):12-19. doi: 10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- 40.International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). Integrated addendum to ICH E6(R1): Guideline for Good Clinical Practice E6(R2). http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R2__Step_4_2016_1109.pdf. Published November 9, 2016. Accessed July 11, 2018.
- 41.Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74(4):319-328. doi: 10.1001/jamapsychiatry.2016.4287 [DOI] [PubMed] [Google Scholar]
- 42.De Jongh A, Resick PA, Zoellner LA, et al. . Critical analysis of the current treatment guidelines for complex PTSD in adults. Depress Anxiety. 2016;33(5):359-369. doi: 10.1002/da.22469 [DOI] [PubMed] [Google Scholar]
- 43.Goldbeck L, Muche R, Sachser C, Tutus D, Rosner R. Effectiveness of trauma-focused cognitive behavioral therapy for children and adolescents: a randomized controlled trial in eight German mental health clinics. Psychother Psychosom. 2016;85(3):159-170. doi: 10.1159/000442824 [DOI] [PubMed] [Google Scholar]
- 44.Jensen TK, Holt T, Ormhaug SM, et al. . A randomized effectiveness study comparing trauma-focused cognitive behavioral therapy with therapy as usual for youth. J Clin Child Adolesc Psychol. 2014;43(3):356-369. doi: 10.1080/15374416.2013.822307 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eMethods. Statistical Analysis and Treatment Integrity
eTable 1. Overview of D-CPT
eTable 2. Primary and Secondary Outcomes at All Assessment Points for Younger (<18 Years [n = 40]) and Older (18-21 Years [n = 48]) Age Groups
eReferences.
Data Sharing Statement