Abstract
HIV-positive women who engage in postpartum unsafe sex are at risk for STI acquisition, unintended pregnancy, and secondary transmission of HIV to uninfected partners. One factor that may increase risk for postpartum unsafe sex among HIV-positive women is IPV victimization, however, few studies have examined this association. To this end, the current longitudinal study examined whether patterns of psychological, physical, and sexual IPV, assessed during pregnancy, predicted unsafe sex at 14 weeks postpartum among South African women diagnosed as HIV-positive during pregnancy (n=561). In a three-step latent class analysis IPV class membership predicted postpartum unsafe sex; compared to non-victims, victims of multiform severe controlling IPV were significantly more likely to engage in postpartum unsafe sex (p=.01), even after adjusting for key confounders. Moderate IPV was not associated with postpartum unsafe sex. Findings support the need for targeted sexual risk reduction interventions for HIV-positive pregnant women who have experienced severe patterns of IPV.
Keywords: intimate partner violence, unsafe sex, HIV-positive women, postpartum period, latent class analysis
Introduction
Programs that effectively prevent unsafe sex among those who are newly diagnosed with HIV are key to reducing risk of secondary transmission [1–3], particularly in regions such as sub-Saharan Africa where HIV is highly prevalent and a large proportion of couples are discordant [4,5]. Such programs may be of particular importance for postpartum HIV-positive women in sub-Saharan Africa; research suggests that, despite repeated contact with health services, and thus opportunity for safe sex counseling, between 30 and 60% of sexually active HIV positive women report engaging in unprotected sex during the postpartum period [6–8].
One important factor that may attenuate the effects of safe sex counseling for HIV-positive women during pregnancy and contribute to sustained risk for unsafe sex during the postpartum period is intimate partner violence (IPV). Theoretical models suggest that IPV victimization may contribute to traumatic stress and harmful relationship power dynamics that limit women’s ability to negotiate and engage in safe sex [9–12]. Consistent with this notion, empirical research, including research in sub-Saharan Africa, has generally found a positive association between IPV victimization and sexual risk behaviors and outcomes among women [9,13–16]. However, a number of key methodological limitations of extant research constrain generalizability and interpretation of these findings. In particular, most research examining the link between IPV and sexual risk outcomes and behaviors has been cross-sectional, precluding the ability to establish temporality, and/or has failed to control for important third variables, including number of sexual partners and early childhood experiences (child maltreatment, age at first sex), that have been associated with IPV and sexual risk and thus may produce spurious associations[12,14,16].
In addition to these design flaws, measurement problems plague extant research. For example, most studies examining the link between IPV and sexual risk have using crude binary measures of only one type of IPV (e.g., physical abuse) or composite measures of abuse [12,15]. The few studies that have assessed multiple abuse types have generally focused on identifying the unique effect of each abuse type, controlling for the others, and with the assumption that this contribution applies across all people. Yet, theory and emerging research suggests that this approach may fail to capture the key configurations of IPV experiences that jointly predict sexual risk. For example, typological theoretical perspectives suggest there may be a subgroup of women who experience coercive controlling violence, a pattern of IPV characterized by severe chronic multiform IPV in conjunction with male partner controlling behavior [17]. Women who experience this pattern of IPV may be at greater risk for engaging in unprotected sex than women who experience situational couple violence that results from conflict that occasionally escalates into IPV and is not rooted in a dynamic of power and control [17].
Finally, very little research has examined whether and how IPV is related to unsafe sex among women who are aware they are HIV-infected and only one previous study, to our knowledge, has examined whether IPV is associated with sexual risk among HIV-infected women during the postpartum period [8]. That study, which was conducted with a sample of 480 sexually-active HIV-positive South African women recruited between 3–12 months post-delivery, found a positive association between any physical IPV victimization in the past six months and unsafe sex, defined as having had unprotected sex in the past three months with an HIV-uninfected or unknown-status partner. However, reflecting the weaknesses described above for the broader literature, the study was limited in that it was cross-sectional, did not adjust for childhood risk factors that may confound relationships, and used a crude binary measure of only one type of IPV (physical abuse).
The Current Study
A better understanding of whether and how IPV is related to sexual risk during the postpartum period among HIV-positive women has the potential to inform interventions to promote sexual health and prevent secondary HIV transmission in this high-risk population. To this end, the current study examining the longitudinal association between patterns of IPV, reported during pregnancy and assessed using latent class analysis, and postpartum unsafe sex (unprotected sex with a partner who is HIV-negative or of unknown status) in a sample of South African women who were newly diagnosed with HIV during pregnancy. We hypothesized that HIV-positive women who reported having experienced coercive controlling IPV victimization in their current relationship would be more likely to report postpartum unsafe sex than women experiencing other patterns. Further, we hypothesized that these relationships would be attenuated but remain statistically significant when controlling for potential confounder variables including: age at first sex, lifetime number of sexual partners, and child abuse.
Methods
Parent study design and procedure
Analyses for this study used baseline and follow-up data from a randomized controlled trial that aimed to examine the efficacy of enhanced HIV counseling for risk reduction during the perinatal period. Participants were pregnant women seeking antenatal care from a primary health care clinic in Umlazi township in the province of Kwazulu Natal (KZN). Eligible women were greater than 18 years old, had been with their intimate partner for at least six months, and were unaware of their HIV status (never tested for HIV or tested negative at least 3 months prior to enrollment). At baseline (first antenatal visit), 1480 eligible women who consented to participate completed a Computer-Assistant Personal Interview (CAPI) in English or Zulu, were randomized to receive either enhanced counseling or standard of care counseling and were tested for HIV using a point-of-care HIV test (Determine: Abbott Laboratories, Abbott Park, IL). If a reactive result was obtained with the Determine rapid HIV test, the participant’s HIV status was confirmed with a second test (Smart Check: World Diagnostic Inc, Miami Lakes, FL). Follow-up interviews and HIV testing were conducted at 14 weeks postpartum with 80% (n=1183) of baseline study participants. Women were reimbursed 70 South African Rand, equivalent to $8 USD at each assessment visit. Informed consent was obtained from all individual participants in the current study and all procedures were approved by the institutional review board at the University of North Carolina Chapel Hill and the University of KwaZulu-Natal. Additional details on recruitment, randomization, intervention, data collection, and retention strategy are included in the study protocol and supporting CONSORT checklist [18].
Analytic Sample
For the current study, we restricted the sample to those participants who were diagnosed as HIV-positive at baseline (n=571; 39% of the total sample). Ten participants (<2%) were missing data on study covariates (demographic or confounder variables) and were dropped from the sample yielding a final analytic sample of 561 HIV-positive women. The average age of participants in the sample was 26.4 years (SD = 5.12); average gestational age at baseline was 24.6 weeks (SD=6.31) and 29% reported having had no previous pregnancies; 29% of women reported living with their current partner and the average relationship length was 3.88 years (SD=3.55). Over half of the sample (58%) reported their highest level of education as high-school or less; 52% reported having no indoor toilet facility; and 11% reported having no electricity in their household. Approximately 75% of the baseline analytic sample (n=421) were retained in the study at 14 weeks postpartum.
Measures
Measures are based on participant self-report. Descriptive statistics for the indicators used to define the latent IPV classes, putative confounder variables, and postpartum unsafe sex are presented in Table 1.
Table 1.
Correlation matrix and descriptive statistics for measures of intimate partner violence, covariates, and postpartum unprotected sex (n=561).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|
| Moderate psychological IPV | Severe psychological IPV | Moderate physical IPV | Severe physical IPV | Sexual IPV | Partner controlling behavior | Childhood abuse | Age at first sex (years) | Lifetime no. of sexual partners | Postpartum unsafe sex | |
| 1 | -- | |||||||||
| 2 | 0.33 | -- | ||||||||
| 3 | 0.44 | 0.40 | -- | |||||||
| 4 | 0.36 | 0.36 | 0.41 | -- | ||||||
| 5 | 0.23 | 0.27 | 0.21 | 0.31 | -- | |||||
| 6 | 0.19 | 0.25 | 0.16 | 0.18 | 0.18 | -- | ||||
| 7 | 0.06 | 0.1 | 0.03 | 0.03 | 0.08 | 0.10 | -- | |||
| 8 | 0.12 | 0.14 | 0.11 | 0.09 | 0.08 | 0.16 | 0.03 | -- | ||
| 9 | 0.07 | 0.05 | 0.09 | 0.06 | 0.02 | −0.06 | −0.01 | 0.08 | -- | |
| 10 | 0.07 | 0.02 | 0.07 | 0.12 | 0.09 | 0.06 | −0.01 | 0.03 | 0.09 | -- |
| % or mean (SD) | 33 | 10 | 27 | 15 | 8 | 20 | 6 | 16.3 (2.3) | 2.83 (1.87) | 6 |
Note. Bolded correlation coefficients are significant at p<.05. Italicized correlations are significant at p<.10.
Latent class (IPV) indicators.
A modified version of the World Health Organization Violence Against Women instrument was used to measure psychological (moderate and severe), physical (moderate and severe) and sexual IPV [19]. The instrument was modified so that participants were asked to report acts that had been perpetrated against them during or prior to pregnancy by their current partner. Two items assessed moderate psychological violence (insulted you or made you feel bad about yourself; belittled or humiliated you in front of others) and two items assessed severe psychological violence (did things to scare or intimidate you on purpose; threatened to hurt you or someone you cared about). Two items assessed moderate physical IPV (slapped or thrown something at you that could hurt you; pushed or shoved you) and four items assessed severe physical IPV (hit you with his fist or something else that could hurt you; kicked you, dragged you, or beat you up; choked or burnt you on purpose; threatened to use or actually used a gun, knife or other weapon that could hurt you). Three items assessed sexual IPV (physically forced you to have sex when you did not want to; used threats to make you have sex; forced you to do something sexual you found degrading or humiliating). Response options for each item ranged from “never” to “ten or more times.” Scores on items assessing each type of abuse were summed and dichotomized to create five binary indicators that denoted the presence or absence of each type of abuse in the woman’s current relationship. For example, severe physical abuse was coded as “1” if the woman had experienced at least one act of severe physical abuse by current partner before or during pregnancy and as “0” if the women reported their current partner had never perpetrated an act of severe physical abuse against them.
Male controlling behavior was assessed using 14 items from the relationship control subscale of the Sexual Relationship Power Scale (SRPS; α=.82) [20]. Women were asked to report the extent to which they agreed or disagreed that their partner engaged in different controlling behaviors towards them (e.g., controlling who she could spend time with). Items assessing each controlling behavior were dichotomously coded as “1” if the respondent strongly agreed that their partner engaged in the behavior and “0” otherwise. Scores across items were then summed and dichotomized so that those whose scores fell into the upper quartile (>4) were coded as “1” to denote high male controlling behavior and “0” otherwise.
Past 30-day unsafe sex
At baseline (during pregnancy) and follow-up (14 weeks postpartum) participants were asked about sexual activity with their last five sexual partners starting with their current or most recent partner. Sex was described to participants as encompassing both vaginal and anal sex with explicit definitions provided for both. Unsafe sex was coded as 1 if the participant reported having had sex without using a condom with a sexual partner who was HIV-negative or of unknown status in the past 30 days and 0 otherwise.
Childhood risk covariates
Experience of childhood abuse was measured by two items assessing whether the participant had undergone any “unwanted sexual experiences” (defined as inappropriate touching or unwanted sexual intercourse) or experienced “serious physical violence” (defined as being hit, punched, kicked, or beaten up in a way that resulted in serious harm) prior to age 12. Earlier age at first sex was determined by asking participants, “how old were you when you had sex for the first time.” Based on the skewed distribution of responses, this variable was categorized as follows: ≤ 14 years (5), 15 years (4), 16 years (3), 17 years (2), or 18 (1), or 19 or older (0).
Demographic covariates
Baseline age was coded by subtracting the participant’s birthdate from the baseline interview date and was coded as number of years. Education was coded as “0” for those who reported that the highest standard passed was 5 or less (grade 7 or lower); those who reported reaching standards 6–9 (grades 8–11) were coded as “1”; and those who reported matriculation from high school or higher were coded as “2.” Relationship length was assessed by asking participants “how long have you been in your current relationship” and was coded as number of months. Lives with current partner was coded as “1” for those who reported currently living with their partner (regardless of marital status) and as “0” otherwise.
Analytic Strategy
The current study builds from previous research in which we conducted a series of latent class analysis to identify respondents with similar patterns of responses on the six IPV indicators using the full sample of HIV-positive and HIV-negative participants in the parent study and found that a three-class model provided the best fit to the data [21]. In the current study, which included only those who tested positive for HIV at baseline, we used the same approach, in which we estimated and compared models with increasing numbers of classes based on different model fit indices using Mplus 7.4[22], to identify the best fitting model. Statistical fit indices included the: the Akaike information criterion (AIC), the sample size adjusted Bayesian Information Criterion (ssBIC), and the Lo-Mendel-Rubin Likelihood Ratio Test (LMR-LRT). The best-fitting most parsimonious models are those that minimize the AIC and ssBIC and for which adding an additional class results in a significant decrease in model fit as indicated by a p-value of less than .05 for the LMR-LRT.
Consistent with our previous research, a three-class model provided the best fit to the current study sample. The AIC and ssBIC were lowest for the three-class model and the LMR-LRT was statistically significant for the three-class (p=.002), but not the four-class (p=.41) model (fit indices are available from the author upon request). The entropy value for the three-class model was .77 and average posterior probabilities for each class were all greater than point .80, indicating good correspondence of the three-class model to the data. Parameter estimates for the three-class model, including item response probabilities and prevalence estimates, are provided in Table 2 and were nearly identical to those found using the full sample. The first class was labeled non-victims (prevalence=74%) because members had low probabilities of endorsing any of the IPV indicators. The second class was labeled moderate IPV (prevalence=20%) because members had high probabilities (>.50) of endorsing moderate psychological and physical violence and low probabilities of endorsing any other IPV indicator. The third class was labeled multiform severe controlling IPV (prevalence=5%), based on high probabilities of endorsing all of the IPV indicators, including severe psychological and physical victimization and male controlling behavior.
Table 2.
Class prevalences and item-response probabilities (probability of reporting each type of intimate partner violence given latent class) for the three-class model
| Class 1 | Class 2 | Class 3 | |
|---|---|---|---|
| Non-victims (74%, n=417) | Moderate IPV (20%, n=115) | Multiform Severe Controlling IPV (5%, n=29) | |
| Victimization Type | |||
| Psychological | |||
| Moderate | 0.14 | 0.70 | 1.00 |
| Severe | 0.003 | 0.27 | 0.69 |
| Psychological | |||
| Moderate | 0.07 | 0.70 | 0.93 |
| Severe | 0.03 | 0.33 | 1.00 |
| Sexual | 0.03 | 0.09 | 0.69 |
| Controlling behavior | 0.13 | 0.30 | 0.60 |
Note: IPV=Intimate partner violence. Item response probabilities greater than .50 are bolded to facilitate interpretation of class differences.
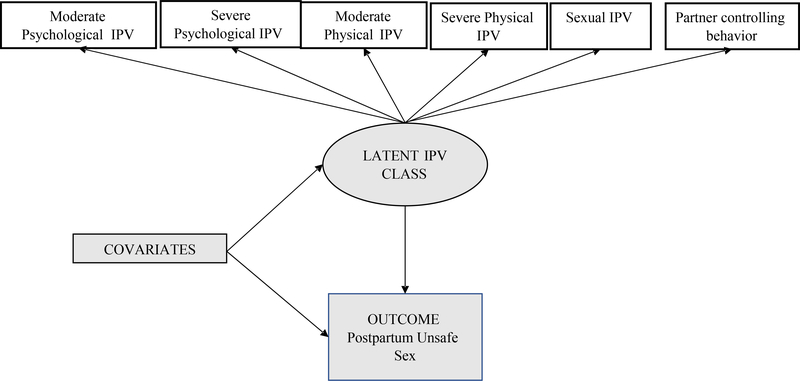
To examine study hypotheses, we used the approach developed in Vermunt (2010) to examine associations between latent class membership and postpartum unsafe sex while adjusting for covariate effects on class membership and the outcome variables and accounting for measurement error due to uncertainty of class classification (for more details see, Vermunt 2010, and Asporouhov and Muthén 2014) [23,24]. To examine the influence of covariates that were conceptualized as potential confounders (childhood abuse, age at first sex, lifetime # of sexual partners), we used a two-stage modeling process that enabled us to examine attenuation of the association between IPV latent class and the unsafe sex attributable to the putative confounder variables. Model 1 included only demographic variables, as well as baseline unsafe sex and treatment group status, as covariates. Model 2 built on Model 1 to add the putative confounders. Figure 1 provides a conceptual model depicting the model pathways that were estimated.
Figure 1.
Conceptual model of hypothesized relationships among study variables. Covariates included baseline unsafe sex, treatment group status, age, education, relationship length, cohabitation status, childhood abuse, age at first sex, and lifetime number of sexual partners.
Treatment group status was included as a covariate in all models because participants were part of a randomized control trial, however treatment group status was not associated with either IPV or postpartum unsafe sex and sensitivity analysis suggest that findings did not differ when it was excluded. Missing data on the LCA indicators and outcome variable was accounted for using full information maximum likelihood, which provides unbiased parameter estimates under the assumption that data are missing at random [25].
Results
Unsafe sex, defined in this study as having had unprotected in the past 30 days with an HIV-uninfected or unknown status partner, was reported by 6% of study participants assessed at 14 weeks postpartum (26/421). When including only those who reported having had sex in the past 30 days in the denominator (n=163; 39%), this proportion increased to approximately 16%.
Table 3 presents parameter estimates from the two models examining the longitudinal effects of latent IPV class membership on postpartum unsafe sex. As hypothesized, membership in the multiform severe controlling IPV class was associated with significantly increased odds of unsafe sex compared to membership in the non-victim class in both Model 1 (demographics only; OR= 7.19, 95% CI=1.60, 32.33) and Model 2 (all covariates; OR=7.74, 95% CI=1.59, 37.71). Membership in the moderate IPV class vs. the non-victim class was not associated with postpartum unsafe sex in either model 1 or model 2. Based on model 2, the adjusted predicted probability of postpartum unsafe sex for HIV-infected women in the multiform severe IPV class was 8% compared to 2% for the moderate IPV class and 1% for the non-victim class.
Table 3.
Effects of IPV class membership on postpartum unsafe sex adjusting for demographic and childhood risk covariates.
| Postpartum Unsafe Sex | ||
|---|---|---|
| Predictors | Model 1 | Model 2 |
| OR (95% CI) | OR (95% CI) | |
| Latent IPV Class (ref=non-victims class) | ||
| Multiform severe controlling | 7.19 (1.60, 32.33)* | 7.74 (1.59, 37.71)* |
| Moderate | 2.10 (0.64, 6.88) | 2.12 (0.67, 6.69) |
| Demographic covariates | ||
| Age | 0.96 (0.88, 1.04) | 0.91 (0.83, 0.999)* |
| Education | 0.71 (0.35, 1.42) | 0.62 (0.30, 1.30) |
| Relationship length | 0.95 (0.83, 1.10) | 0.99 (0.86, 1.15) |
| Lives with current partner | 2.15 (0.86, 5.40) | 2.67 (1.06, 6.75)* |
| Controls | ||
| Child abuse | -- | 0.49 (0.04, 5.62) |
| Age at first sex | -- | 0.92 (0.77, 1.09) |
| Lifetime # of sexual partners | -- | 1.55 (1.18, 2.04)** |
p<.05
p<.01.
IPV=Intimate partner violence.
Age, partner cohabitation status, and number of lifetime sexual partners also predicted postpartum unsafe sex. In particular, results from model 2 suggest that older HIV-positive women were less likely to report postpartum unsafe sex (OR=0.91, 95% CI=0.83, 1.00, p=.048); in contrast, women who reported living together with a current partner (OR=2.67, 95% CI=1.06, 6.75, p=.038) and a greater number of lifetime sexual partners (OR=1.55, 95% CI=1.18, 2.04, p=.001), were more likely to report postpartum unsafe sex.
Although not directly related to study hypotheses, we also note that age, education cohabitation status, age at first sex, and experience of childhood abuse were each associated with latent IPV class membership in model 2. In particular, older women were less likely to belong to the multiform severe controlling IPV class as compared to the non-victim group (OR=0.87, 95% CI=0.79, 0.97, p=.01). In contrast, cohabitation with current partner (OR=4.60, 95% CI=1.54, 13.78, p=.01), earlier age at first sex (marginal association, OR=1.23, 95% CI=0.97, 1.57, p=.09), and experience of childhood abuse (OR=5.55, 95% CI=1.40, 21.91, p=.02) were each associated with increased odds of membership in the multiform severe controlling IPV class as compared to the non-victim group. Only age and education distinguished the moderate IPV class from the non-victim group; in particular, both age (OR=0.94, 95% CI=0.88, 1.00, p=.04) and education (OR=0.57, 95% CI=0.36, 0.91) were negatively associated with (i.e., protected against) membership in the moderate IPV class as compared to the non-victim class.
Discussion
This study aimed to examine the longitudinal association between IPV victimization and postpartum unsafe sex among HIV-infected women in South Africa. As expected, IPV victimization prospectively predicted postpartum sexual risk; however, associations differed for subgroups of women with distinct patterns of IPV victimization. In particular, HIV-positive women who reported during pregnancy that they had experienced multiple forms (physical, psychological, sexual) of severe controlling IPV in their current relationship were at increased risk for postpartum unsafe sex compared to non-victims. HIV-positive women who reported that they had experienced only moderate physical and psychological IPV, however, were not at increased risk for postpartum unsafe sex compared to non-victims.
The finding that multiform severe controlling IPV victimization was uniquely predictive of postpartum unsafe sex is consistent with theory and empirical research that suggests that different patterns of partner violence, abuse, and control may have different consequences for victims [26–28]. Compared to non-victims and those who have only experienced moderate forms of IPV, HIV-positive women who are victims of more severe controlling patterns of IPV, a type of IPV that has been referred to as “intimate terrorism” [17], may be more likely to fear negative repercussions if they try to abstain from sex or negotiate condom use. Further, victims of this type of abuse may be more likely to experience negative psychosocial outcomes, such as post-traumatic stress symptomology and substance use that in turn increase risk for unsafe sex.
In terms of prevention implications, findings suggest that programs that prevent or reduce multiform severe controlling IPV victimization among pregnant HIV-positive women may reduce risk of postpartum unsafe sex and, in turn, reduce risk for negative health outcomes including: STI acquisition, unplanned pregnancy, and secondary HIV transmission. Further, findings suggest that safe-sex programs that target HIV-infected pregnant women with a history of IPV should identify women with distinct IPV profiles and ensure that program content addresses the particular psychosocial processes that put women who have experienced multidomain severe controlling IPV at risk for unsafe sex and its negative health consequences.
Notably, more research is needed to inform the development of tailored IPV and sexual risk reduction approaches that differentiate among different patterns or forms of IPV victimization and perpetration. For example, future research should aim to identify the unique etiological pathways that increase risk for multiform severe controlling IPV and determine whether extant programs designed to reduce risk for IPV victimization among HIV-positive pregnant women and/or reduce risk of IPV perpetration by male partners are effective in preventing this type of IPV. Further, studies are needed to identify the mechanisms that explain why HIV-positive pregnant women who have experienced multiform severe controlling IPV are at risk for unsafe sex and determine whether the protective effects of extant sexual risk reduction counseling and other programs for HIV-positive women with a history of IPV differ depending on participants’ baseline victimization patterns. While more research is needed to replicate findings, the current study also suggests the need to develop more nuanced antenatal IPV screening protocols that enable providers to identify women experiencing different patterns of IPV and provide them with tailored support and integrated services sensitive to their relationship context and experiences.
The current study has several limitations including a small sample size, reliance on self-report, and a short follow-up. Although we measured several forms of IPV victimization we only assessed IPV that had occurred in the current relationship and did not assess IPV perpetration; a more comprehensive assessment of participants’ involvement in violence across the life-course may have further distinguished violence profiles. The use of a convenience sample of adult women (≥ 18 years old) recruited from one antenatal clinic limits the generalizability of findings to other populations (e.g., adolescent populations, women from rural areas). We note that the prevalence of postpartum unsafe sex among HIV-positive women in the current study (6% overall; 14% among those sexually active) was lower than that reported in other studies in sub-Saharan Africa [6–8]. However, this different in prevalence rates may have been due to the fact that all women in the current study were newly diagnosed with HIV at baseline and thus all had recently received sexual risk reduction counseling in conjunction with their HIV testing.
Notwithstanding the aforementioned limitations the current study had several strengths. The study was the first to examine the association between IPV and postpartum unsafe sex using a longitudinal design that enabled temporality to be established between exposure and outcome. Use of a person-centered approach, latent class analysis, allowed for the differentiation of distinct patterns of IPV victimization experiences, enabling a more nuanced assessment of IPV and its consequences. Finally, the use of a three-step analytic approach allowed us to adjust for key confounders as well as classification bias in the assessment of IPV patterns.
Conclusion
The present study is the first to examine the prospective relationship between patterns of IPV victimization, assessed during pregnancy, and postpartum unsafe sex among HIV positive women in South Africa. The IPV patterns identified are consistent with previous research and theory, providing more evidence of two distinct subgroups of IPV victims: a larger group characterized by experiencing only moderate forms of IPV victimization and a smaller group characterized by experiencing severe forms of IPV in conjunction with male partner controlling behavior. HIV-positive women who reported that they had experienced multiform severe controlling IPV in their current relationship were at increased risk for postpartum unsafe sex, suggesting that this form of IPV should be targeted by sexual risk reduction programs for this population. Findings suggest the need to differentiate distinct patterns of IPV when examining the consequences of victimization. Future research should build on the current study to examine the mechanisms explaining the link between IPV patterns and postpartum unsafe sex as well as other sexual risk behaviors and determine whether and how associations generalize across different populations.
Acknowledgements
This research was supported by a grant from the National Institute of Child Health and Development (Grant # 1-R03-HD089140-01) to the corresponding author.
Footnotes
Compliance with Ethical Standards
The authors report no conflict of interest. Informed consent was obtained from all individual participants in the current study and all procedures performed in the study that involved human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Cohen MS, Shaw GM, McMichael AJ, Haynes BF. Acute HIV-1 infection. N. Engl. J. Med 2011; 364:1943–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pettifor A, MacPhail C, Corneli A, et al. Continued high risk sexual behavior following diagnosis with acute HIV infection in South Africa and Malawi: implications for prevention. AIDS Behav. 2011; 15:1243–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. JAIDS J. Acquir. Immune Defic. Syndr 2005; 39:446–53. [DOI] [PubMed] [Google Scholar]
- 4.Rosenberg NE, Pettifor AE, Bruyn GDE, et al. HIV testing and counseling leads to immediate consistent condom use among South African stable HIV-discordant couples. J. Acquir. Immune Defic. Syndr 2013; 62:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. UNAIDS: Global Report: UNAIDS report on the global AIDS epidemic. Geneva: World Health Organization, 2010. [Google Scholar]
- 6.Bii SC, Otieno-Nyunya B, Siika A, Rotich JK. Infant feeding practices among HIV infected women receiving prevention of mother-to-child transmission services at Kitale District Hospital, Kenya. East Afr. Med. J 2008; 85:156–61. [DOI] [PubMed] [Google Scholar]
- 7.Irungu E, Chersich MF, Sanon C, et al. Changes in sexual behaviour among HIV-infected women in west and east Africa in the first 24 months after delivery. Aids. 2012; 26:997–1007. [DOI] [PubMed] [Google Scholar]
- 8.Peltzer K Sexual behaviour among HIV-infected new mothers in South Africa 3–12 months after delivery. AIDS Care. 2014; 26:186–90. [DOI] [PubMed] [Google Scholar]
- 9.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010; 376:41–8. [DOI] [PubMed] [Google Scholar]
- 10.Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc. Sci. Med 2000; 50:459–78. [DOI] [PubMed] [Google Scholar]
- 11.Pettifor AE, Measham DM, Rees H V, Padian NS. Sexual power and HIV risk, South Africa. Emerg. Infect. Dis 2004; 10:1996–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stockman JK, Lucea MB, Campbell JC. Forced sexual initiation, sexual intimate partner violence and HIV risk in women: a global review of the literature. AIDS Behav. 2013; 17:832–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunkle KL, Jewkes RK, Brown HC, et al. Prevalence and patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, South Africa. Am. J. Epidemiol 2004; 160:230–239. [DOI] [PubMed] [Google Scholar]
- 14.Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J. Int. AIDS Soc 2014;17: 18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maxwell L, Devries K, Zionts D, Alhusen JL, Campbell J. Estimating the effect of intimate partner violence on women’s use of contraception: a systematic review and meta-analysis. PLoS One. 2015; 10:e0118234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kouyoumdjian FG, Findlay N, Schwandt M, Calzavara LM. A systematic review of the relationships between intimate partner violence and HIV/AIDS. PLoS One. 2013;8:e81044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson MP. Patriarchal terrorism and common couple violence: Two forms of violence against women. J. Marriage Fam 1995;283–94. [Google Scholar]
- 18.Maman S, Moodley D, McNaughton-Reyes HL, Groves AK, Kagee A, Moodley P. Efficacy of enhanced HIV counseling for risk reduction during pregnancy and in the postpartum period: a randomized controlled trial. PLoS One. 2014; 9:e97092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. Multi-country study on women’s health and domestic violence: core questionnaire and WHO instrument. Version 9. Geneva: World Health Organization, 2000. [Google Scholar]
- 20.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000; 42:637–60. [Google Scholar]
- 21.Reyes HLM, Maman S, Chen MS, Groves AK, & Moodley D (2017) Patterns of intimate partner violence victimization among South African women and their relation to emotional distress during pregnancy and postpartum. [DOI] [PMC free article] [PubMed]
- 22.Muthén LK, & Muthén BO. Mplus User’s Guide (Version 7). Los Angeles, CA: Muthén & Muthén; 2015. [Google Scholar]
- 23.Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Polit. Anal 2010; 18:450–69. [Google Scholar]
- 24.Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Struct. Equ. Model. A Multidiscip. J 2014; 21:329–41. [Google Scholar]
- 25.Allison PD. Missing Data. Thousand Oaks, CA: Sage Publications, Inc.; 2001. [Google Scholar]
- 26.Johnson MP, Leone JM. The differential effects of patriarchal terrorism and common couple violence: Findings from the National Violence Against Women survey. J Fam Issues. 2005; 26: 322–49. [Google Scholar]
- 27.Cavanaugh CE, Messing JT, Petras H, et al. Patterns of Violence Against Women: A Latent Class Analysis. Psychol. Trauma 2012; 4:169–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ansara DL, Hindin MJ. Exploring gender differences in the patterns of intimate partner violence in Canada: a latent class approach. J. Epidemiol. Community Heal 2010; 64:849–54. [DOI] [PubMed] [Google Scholar]