Abstract
Trigeminal neuralgia is caused by compression of trigeminal nerve root and it leads to demyelination gradually. It was almost idiopathic and occurred unexpected. The upper cervical spinal cord contains the spinal trigeminal tract and nucleus. Fibers with cell bodies in the trigeminal ganglion enter in the upper pons and descend caudally to C2 level. We experienced a rare patient with facial pain, which was paroxysmal attack with severe pain after a clear event, cervical spinal injury (C2). So, this case reminds us of a possible cause of trigeminal neuralgia after a trauma of the head and neck.
Keywords: Trigeminal neuralgia, Spinal injury, Spinal cord
INTRODUCTION
The most common type of facial and pharyngeal pain is trigeminal neuralgia. Trigeminal neuralgia also called tic douloureux or the suicide disease, is a long-lasting and important condition affecting the fifth cranial nerve, one of the largest nerves in the head.5) And it can develop after cervical instability on the C2 level. This case describes a patient with trigeminal symptom due to atlantoaxial instability after C2 spinal fracture.
CASE REPORT
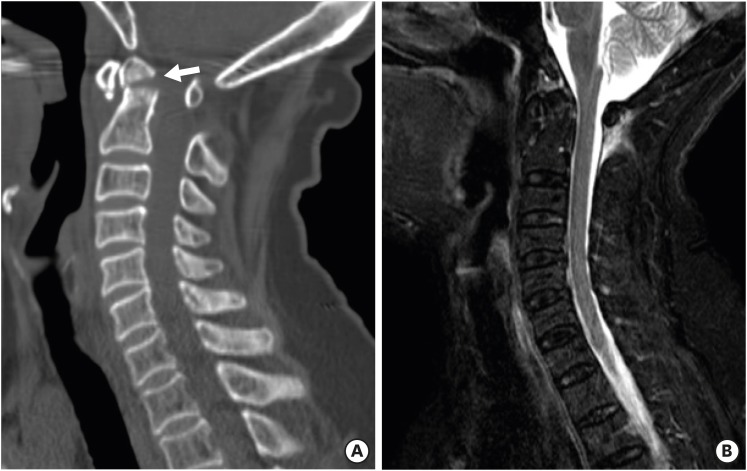
A 70-year-old male with no significant previous medical history was admitted to the emergency department with posterior midline neck pain following a motor vehicle collision. Initially, he had hypesthesia on the neck and left shoulder. Initial cervical spine radiography revealed cervical odontoid process fracture. The computerized tomography showed odontoid process fracture type II and T2 sagittal magnetic resonance imaging (MRI) showed acute traumatic lesion in C2 complex areas. (FIGURE 1). After 4 months, he complained of severe left facial pain according to the left maxillary division of trigeminal nerve. The pain was sharp, paroxysmal and worsed. Neurological examination revealed a decrease of superficial sensation accompanied by pain and dysesthesia in the areas innervated by the left maxillary division of trigeminal nerve, a pain scale of face was 10. MRI showed evidence of cord injury (high signal of cord) and significant spinal cord compression at the atlantoaxial level with C1/2 instability in flexion and extension cervical spine X-ray (FIGURE 2). We explained to the patient that the surgery was needed. But, he did not want the surgery. He took a medicine for treatment the trigeminal neuralgia, oral administration of carbamazepine could achieve partial remission in early stages. The facial pain was decreased below 50%. More and more, the pain of patient was well improved (pain scale of face 3, when discharged from the hospital).
FIGURE 1. The computed tomography (A) reveals odontoid process fracture, type II (white arrow), T2-weighted fat suppression magnetic resonance imaging (B) shows high signal change in C2 posterior complex areas.
FIGURE 2. Sagittal (A) and axial (B) T2 weighted magnetic resonance imaging shows increased atlantoaxial interval with decreased anteroposterior diameter of bony central canal, causing compressive myelopathy of C1/2 (white arrow). The computed tomography (C) shows narrow spinal canal due to C1/2 instability. The lateral radiography on flexion (D) and extension (E) shows C1/2 instability.
DISCUSSION
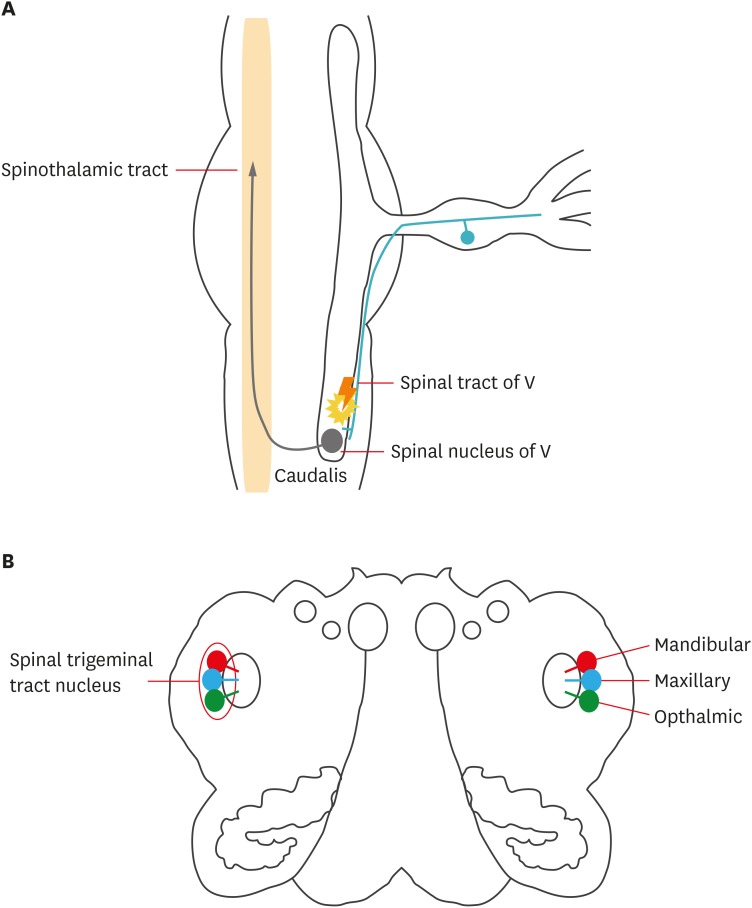
Referred pain frequently arises in the orofacial lesion when headache arises and it can be originated from cervical lesion. Explanations of the pathogenesis are based on evidence from animal studies that found the trigeminal nerve to converge between the cervical spinal nerves at the dorsal horn in the caudal part of the medulla and in the upper level of the cervical spine.9) Afferent trigeminal root fibers, which enter at upper pons descend in the dorsolateral part of the brain stem and project as far as the C2 spinal level and it constitute the spinal trigeminal tract. (FIGURE 3A) Even if the longitudinal aspect of this nucleus is not uniform, it must be pointed out that the 3 branches of the trigeminal nerve are represented along this course through the spinal trigeminal tract (FIGURE 3B). Fibers in the spinal trigeminal tract convey impulses concerned with thermal, tactile sense, and pain from the face, forehead, and mucous membranes of the nose and mouth. Trigeminal neuralgia is a chronic severe pain that affects the trigeminal nerve from face to brain. And even mild stimulation of face may trigger an excruciating pain.2) Trigeminal neuralgia can occur as a result of aging, swollen blood vessel, tumors with nerve compression, multiple sclerosis, or a other disorders that damages the myelin sheath. Trigeminal neuralgia pain originates also from damage to the central trigeminal system in the upper spinal cord and the ponto-medullary levels in the brainstem.4) Therefore, concussive trauma to the head and neck or upper back that cause injury to nerve pathways in the spinal cord and brain stem and it can be cause of trigeminal neuralgia.6) After cervical trauma, facial pain can be triggered immediately or can occur months or years later. Our case suggests that trigeminal neuralgia results from spinal injury due to atlantoaxial instability after C2 odontoid process fracture. It is meaningful that the injury of upper cervical cord affects on trigeminal tract, nucleus. Surgical decompression was needed to our patient, but he refused the surgery, so he was treated with medications for symptoms control. Generally, trigeminal neuralgia can be treated with medications to relieve symptoms, the usual therapy is with an anticonvulsant such as carbamazepine or gabapentin.3) Occasionally, sodium valproate and tricyclic antidepressant can be used, while others have reported cases cured by carbamazepine treatment alone.1) For patients with side effects to oral administration of carbamazepine, surgical intervention such as microvascular decompression(in brain lesion), balloon compression, rhizolysis or rhizotomies and radio-frequency thermo-coagulation, regional nerve blockage also be utilized to achieve therapeutic effects.8) Although it is a dangerous procedure, upper cervical chiropractic care is done to reverse the trauma-induced upper neck injury, thereby reducing irritation to the nerves in the brain stem and spinal cord that can trigger trigeminal neuralgia.7) However, in case of using this method, specialized, skillful, and safe skills are needed.
FIGURE 3. Spinal trigeminal tract descending as far as Caudal medulla and ascending through spinothalamic tract (A, sagittal view) Three branch of central trigeminal bundle connecting with trigeminal nucleus in pons (B, axial view).
CONCLUSION
This case demonstrates an etiology of trigeminal neuralgia from upper cervical cord injury due to atlantoaxial instability after upper cervical trauma. However, more clinical study in the area of trigeminal neuralgia and cervical spine lesion and dysfunction should be conducted to elucidate the correlation between them.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Brownstone PK, Ballenger JJ, Vick NA. Bilateral superior laryngeal neuralgia: its successful treatment with carbamazepine. Arch Neurol. 1980;37:525. doi: 10.1001/archneur.1980.00500570073014. [DOI] [PubMed] [Google Scholar]
- 2.FitzGerld MJT, Folan J. Clinical neuroanatomy and related neuroscience. ed 4. Philadelphia, PA: WB Saunders Company; 2002. [Google Scholar]
- 3.Jorns TP, Zakrzewska JM. Evidence-based approach to the medical management of trigeminal neuralgia. Br J Neurosurg. 2007;21:253–261. doi: 10.1080/02688690701219175. [DOI] [PubMed] [Google Scholar]
- 4.Knibestöl M, Hildingsson C, Toolanen G. Trigeminal sensory impairment after soft-tissue injury of the cervical spine. A quantitative evaluation of cutaneous thresholds for vibration and temperature. Acta Neurol Scand. 1990;82:271–276. doi: 10.1111/j.1600-0404.1990.tb01618.x. [DOI] [PubMed] [Google Scholar]
- 5.Manzoni GC, Torelli P. Epidemiology of typical and atypical craniofacial neuralgias. Neurol Sci. 2005;26(Suppl 2):s65–s67. doi: 10.1007/s10072-005-0410-0. [DOI] [PubMed] [Google Scholar]
- 6.McGlone R, Morton RJ, Sloan JP. Trigeminal pain due to whiplash injury. Injury. 1988;19:366. doi: 10.1016/0020-1383(88)90118-0. [DOI] [PubMed] [Google Scholar]
- 7.Rodine RJ, Aker P. Trigeminal neuralgia and chiropractic care: a case report. J Can Chiropr Assoc. 2010;54:177–186. [PMC free article] [PubMed] [Google Scholar]
- 8.Spatz AL, Zakrzewska JM, Kay EJ. Decision analysis of medical and surgical treatments for trigeminal neuralgia: how patient evaluations of benefits and risks affect the utility of treatment decisions. Pain. 2007;131:302–310. doi: 10.1016/j.pain.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 9.Shinozaki T, Sakamoto E, Shiiba S, Ichikawa F, Arakawa Y, Makihara Y, et al. Cervical plexus block helps in diagnosis of orofacial pain originating from cervical structures. Tohoku J Exp Med. 2006;210:41–47. doi: 10.1620/tjem.210.41. [DOI] [PubMed] [Google Scholar]