Staphylococcal enterotoxin B (SEB) is a protein exotoxin found on the cell surface of Staphylococcus aureus that is the source for multiple pathologies in humans. When purified and concentrated in aerosol form, SEB can cause an acute and often fatal intoxication and thus is considered a biological threat agent.
KEYWORDS: Macaca mulatta, aerosol, antibody therapy, staphylococcal enterotoxin
ABSTRACT
Staphylococcal enterotoxin B (SEB) is a protein exotoxin found on the cell surface of Staphylococcus aureus that is the source for multiple pathologies in humans. When purified and concentrated in aerosol form, SEB can cause an acute and often fatal intoxication and thus is considered a biological threat agent. There are currently no vaccines or treatments approved for human use. Studies with rodent models of SEB intoxication show that antibody therapy may be a promising treatment strategy; however, many have used antibodies only prophylactically or well before any clinical signs of intoxication are apparent. We assessed and compared the protective efficacies of two monoclonal antibodies, Ig121 and c19F1, when administered after aerosol exposure in a uniformly lethal nonhuman primate model of SEB intoxication. Rhesus macaques were challenged using small-particle aerosols of SEB and then were infused intravenously with a single dose of either Ig121 or c19F1 (10 mg/kg of body weight) at either 0.5, 2, or 4 h postexposure. Onset of clinical signs and hematological and cytokine response in untreated controls confirmed the acute onset and potency of the toxin used in the challenge. All animals administered either Ig121 or c19F1 survived SEB challenge, whereas the untreated controls succumbed to SEB intoxication 30 to 48 h postexposure. These results represent the successful therapeutic in vivo protection by two investigational drugs against SEB in a severe nonhuman primate disease model and punctuate the therapeutic value of monoclonal antibodies when faced with treatment options for SEB-induced toxicity in a postexposure setting.
INTRODUCTION
The staphylococcal enterotoxins (SEs) are a well-characterized family of proteins secreted by Staphylococcus aureus that known to be toxic at very low concentrations (1). Staphylococcal enterotoxin B (SEB) is a member of the family of superantigens (SAgs), which are microbial proteins that induce polyclonal T-cell activation, in contrast to conventional antigens that undergo proteolytic processing by antigen-presenting cells (APCs) and are presented as a major histocompatibility complex (MHC)/peptide complex (2–4). SAgs bypass these specific mechanisms of antigen presentation by binding outside the peptide binding groove of MHC class II (MHC-II) on APCs and the variable region of T-cell receptor (TCR) β chain on T cells (5–7). Cross-linking of MHC-II and TCR by SAgs activates both APCs and T cells. SAg binding activates 5 to 20% of circulating T cells bearing specific V beta regions, leading to massive release of proinflammatory cytokines, activation of cell adhesion molecules, increased T-cell proliferation, and eventual T-cell apoptosis/anergy (8). This sequence of events can culminate in a life-threatening condition clinically referred to as toxic shock syndrome (TSS), marked by cytokine storm, rash, hypotension, fever, multisystem dysfunction, and death (9).
SEB is a prototype SAg with a potential to be used as an airborne, foodborne, or waterborne toxic agent and therefore classified by the CDC as a select agent and by the U.S. National Institutes of Health as a category B priority pathogen. It was developed as a bioweapon in the 20th century due to its incapacitating or lethal nature at much a lower dose than required by many chemical agents. SEB has been considered a high-risk toxin because of its relative ease of production, temperature-independent stability, and exquisite toxicity by the inhalation route. Inhalation of SEB aerosols far exceeds other modalities of exposure in terms of potency and deleterious effects, all initiating at a remarkably low (inhaled) dose. When inhaled, nanogram levels of SEB are incapacitating in humans (half-maximal effective dose [ED50] = 0.0004 μg/kg of body weight), while microgram doses of SEB can be lethal (half-maximal lethal dose [LD50] = 0.02 μg/kg) (1). Inhaled SEB initiates a nearly instantaneous response in the lungs after inhalation, marked by neutrophilic influx, massive cytokine release, and marked pathological changes (10–14). Major osmotic shifts in the lung tissue from SEB inhalation result in a primarily localized inflammatory response which leads to progressive vascular leak, microcapillary hemorrhage, and alveolar flooding (10, 15, 16). The use of animal models of SEB intoxication to evaluate potential treatments is complicated by decreasing sensitivity based upon phylogenetic evolution; murine species are generally unresponsive to SEB unless genetically manipulated (17) or the reaction is potentiated by coadministration of an agent such as lipopolysaccharide (LPS) (15, 18). Nonhuman primate species have been shown to be the closest disease model to study pathophysiology of SEB-induced toxicity or in the testing of promising therapies and vaccine products (11, 19–22).
There are currently no vaccines or therapies approved by the U.S. Food and Drug Administration for either preventing or treating SEB intoxication by any modality of exposure. To date the development of a vaccine has been decidedly slow (23), although research has progressed on the development of STEBVax (24). Research and development on possible therapeutic agents have been even less successful. Known anti-inflammatories, such as dexamethasone, have been used with some success when administered prophylactically (25). Experimental treatments such as CD44 ligand, MyD88 mimetic, and interleukin 1 (IL-1) binding products have also shown promise (26–29) as treatment for SEB-induced shock and acute lung injury. Currently, the most promising postexposure treatment for SEB intoxication appears to be from experimental monoclonal antibodies (MAbs) engineered to target binding and effectively neutralizing any further processing of the molecule by host systems (30–33). The monoclonal antibody Ig121 was shown to protect against systemic exposure in a murine potentiation challenge model (34), although this particular effort did not include small-particle aerosol exposure as a modality of challenge. The c19F1 MAb product has shown to be protective in follow-up murine SEB challenge studies in our laboratories, although the product was one of three MAbs administered as a combination product (35).
In this study, we tested two monoclonal antibodies (IgG121 and c19F1) in a severe model of aerosol SEB intoxication in the nonhuman primate. Each MAb targets different areas of the SEB molecule: Ig121 targets the T-cell receptor, whereas c19F1 binds to the variable β binding region of SEB (34). Binding differences between products are demonstrated in vitro using either SEB or the STEBVax vaccine product in preliminary experiments. In the animal experiments, we exposed naive rhesus macaques to a lethal dose of aerosolized SEB and treated them via intravenous (i.v.) infusion at prescribed times after exposure (either 0.5, 2, or 4 h) to test the ability of each MAb product to ameliorate and/or prevent the effects of intoxication.
RESULTS
Binding ELISA.
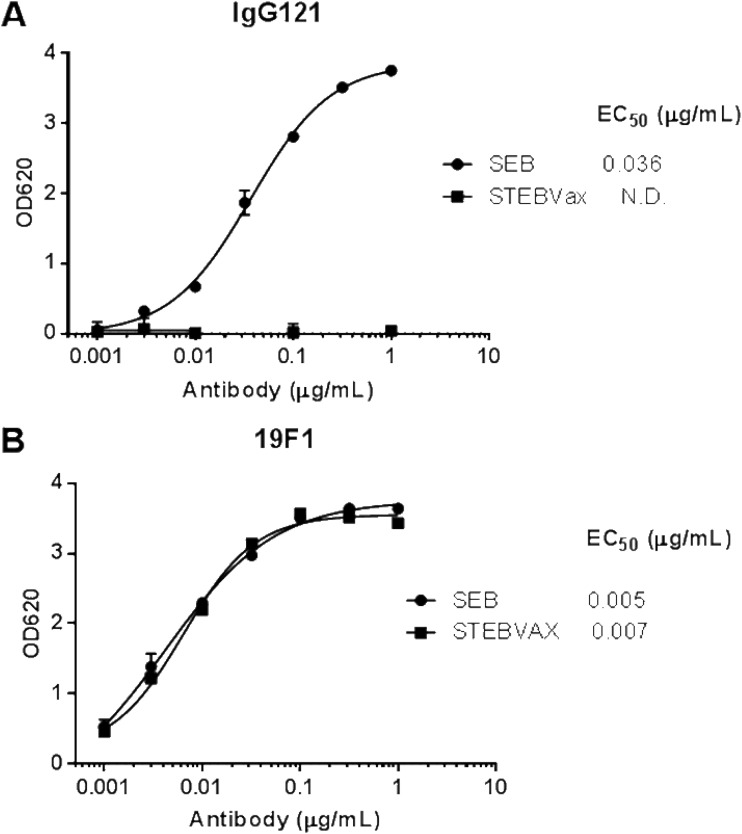
In order to evaluate the differences in potential binding regions between c19F1 and IgG121, enzyme-linked immunosorbent assays (ELISAs) were developed that use SEB or an attenuated form of SEB (STEBVax) as a coating antigen. STEBVax is a recombinant mutated form of SEB containing three point mutations (L45R, Y89A, and Y94A) that disrupt the interaction of the toxin with human MHC class II receptors and render the protein nontoxic while retaining the immunogenicity (36). When these antibodies were tested in the two ELISAs, c19F1 was able to bind to SEB and STEBVax with similar half-maximal effective concentrations (EC50). In contrast, IgG121 was able to bind to SEB but failed to bind to STEBVax at antibody concentrations as high as 1 μg/ml (Fig. 1). These data suggest that IgG121 binds to the MHC binding surface of SEB while c19F1 binds to a distinct neutralizing site.
FIG 1.
Binding of 121 and 19F1 to SEB or STEBVax. (A) Binding of 121 to SEB and STEBVax. (B) Binding of 19F1 to SEB and STEBVax. N.D., not determined.
MAbs IgG121 and c19F1 protection of rhesus macaques after SEB challenge.
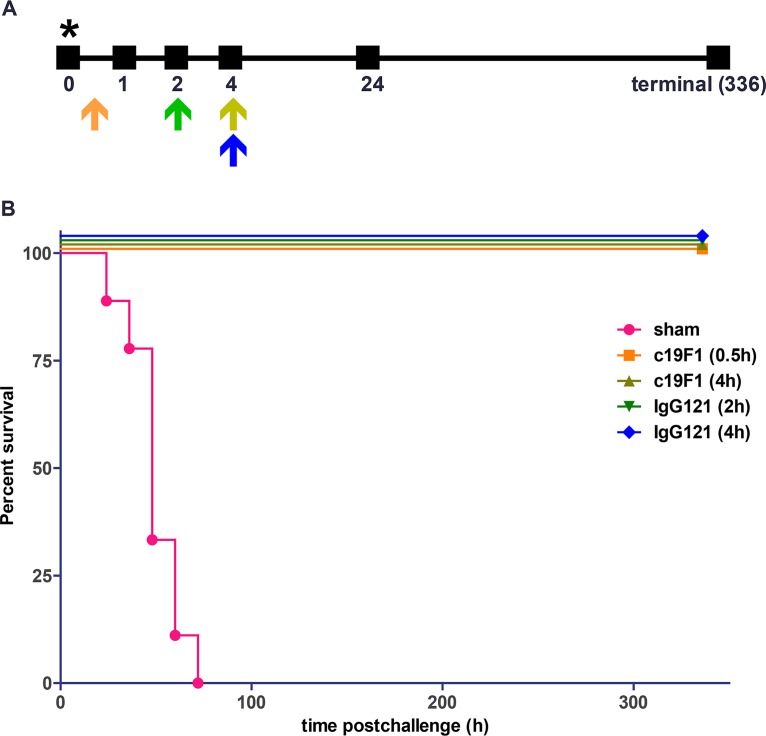
Rhesus macaques were challenged via the aerosol route with SEB toxin, and the challenge was measured as consistent between sham- and antibody-treated groups (Fig. 2). The candidate MAbs were i.v. administered at a dose of 10 mg/kg at 0.5 h or 4 h (c19F1) or 2 h or 4 h (Ig121) and yielded complete survival, in comtrast to zero survival in sham-treated control groups (Fig. 3).
FIG 2.
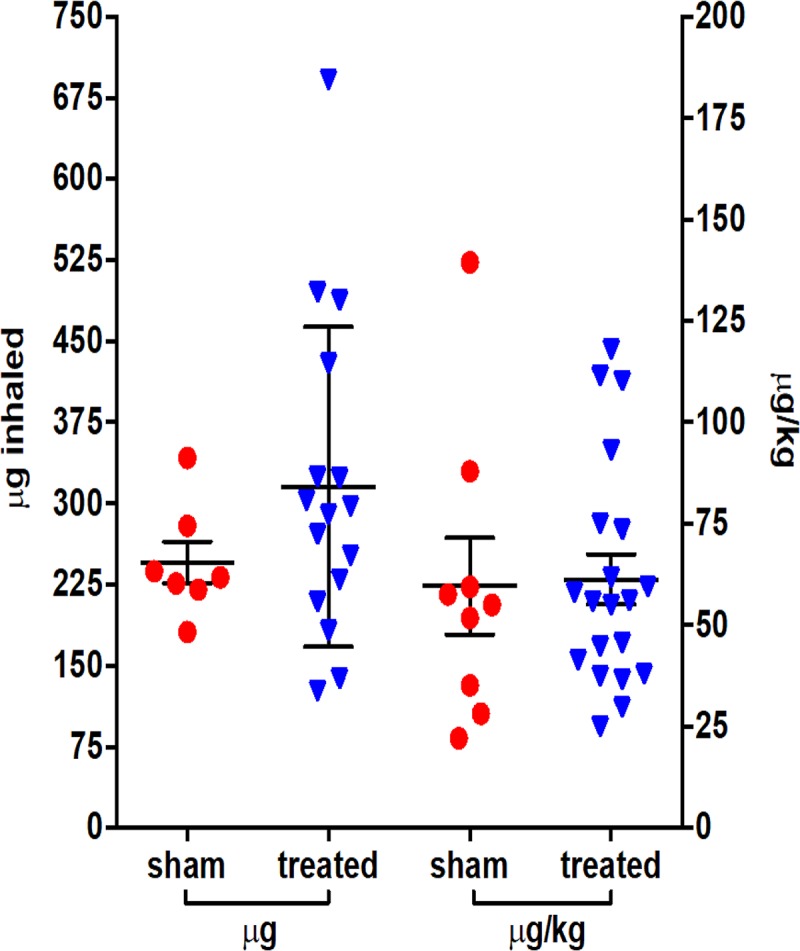
Individual inhaled challenge doses of rhesus macaques with aerosolized SEB toxin expressed as total micrograms inhaled and by a per-weight basis. The line and error bars represent the means and SDs for either antibody-treated or sham groups across all experiments for both measures (n = 23). There was no statistically significant difference between challenge doses in group comparison of total micrograms (P = 0.2392) or microgram-per-kilogram values (P = 0.8942).
FIG 3.
(A) Diagram of antibody treatment schedule, representing single dosage time point/group, and sampling time after SEB challenge in macaques. Orange arrow, c19F1 0.5-h treatment; olive arrow, c19F1 4-h treatment; green arrow, IgG121 2-h treatment; blue arrow, IgG121 4-h treatment. The asterisk represents the hour of SEB challenge. (B) Kaplan-Meier survival curve for the sham group (n = 9) and groups treated with c19F1 at 0.5 h (n = 8), c19F1 at 4 h (n = 4), IgG121 at 2 h (n = 4), and IgG121 at 4 h (n = 4).
Hematology.
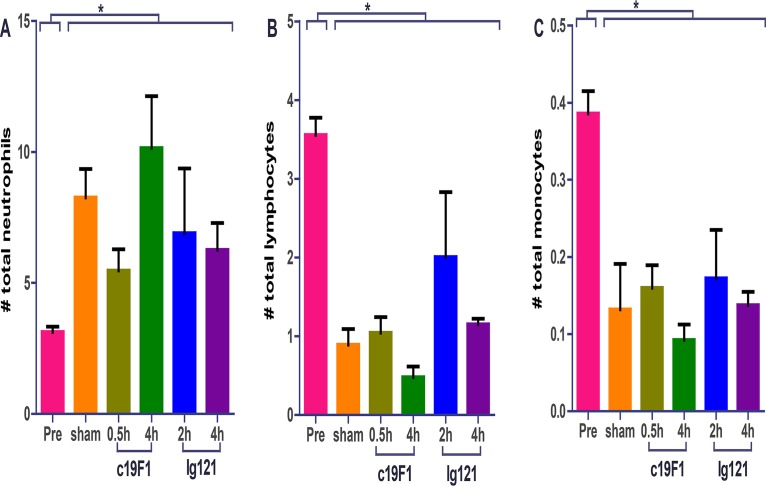
Hematological differences between control and treatment groups were minimal. MAb-treated and sham-treated groups showed a dramatic increase of neutrophils postexposure compared to preexposure values (Fig. 4). Neutrophil percentages of values of the survivors in the treatment group were similar to those in the control group animals. Similarly, lymphocyte changes in both groups were similar in profile; change in preexposure values significantly decreased postexposure. Decreases were also observed in monocyte percentages.
FIG 4.
Cellularity from peripheral blood from all animals (n = 23) prior to SEB challenge (Pre) and 24 h postchallenge and/or treatment with either antibody. Each graph represents neutrophil (A), lymphocyte (B), or monocyte (C) count. All postchallenge values for either sham- or antibody-treated animals were significantly different (*, P < 0.05) from preexposure values. There was no statistical difference between sham control and treatment animals postexposure for any of the values presented.
Clinical chemistries.
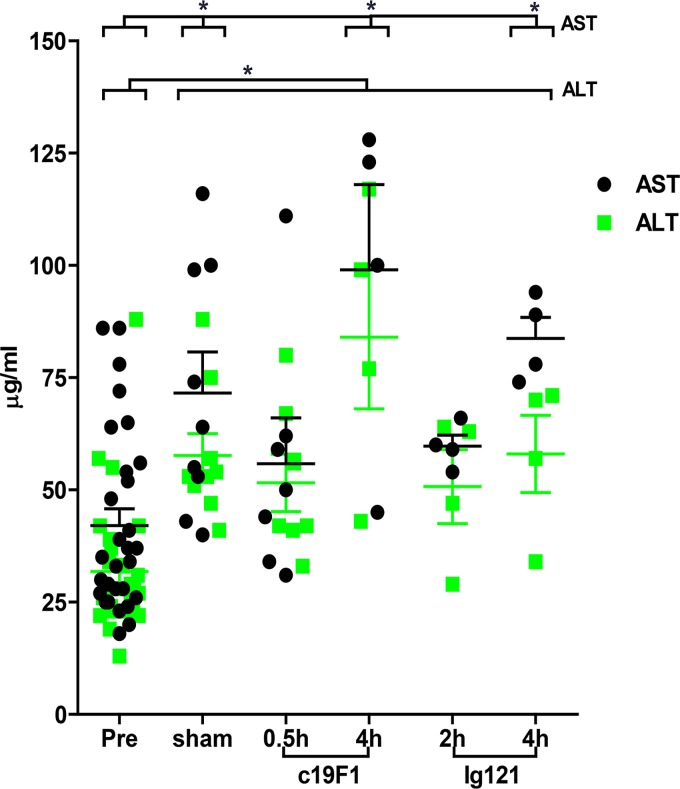
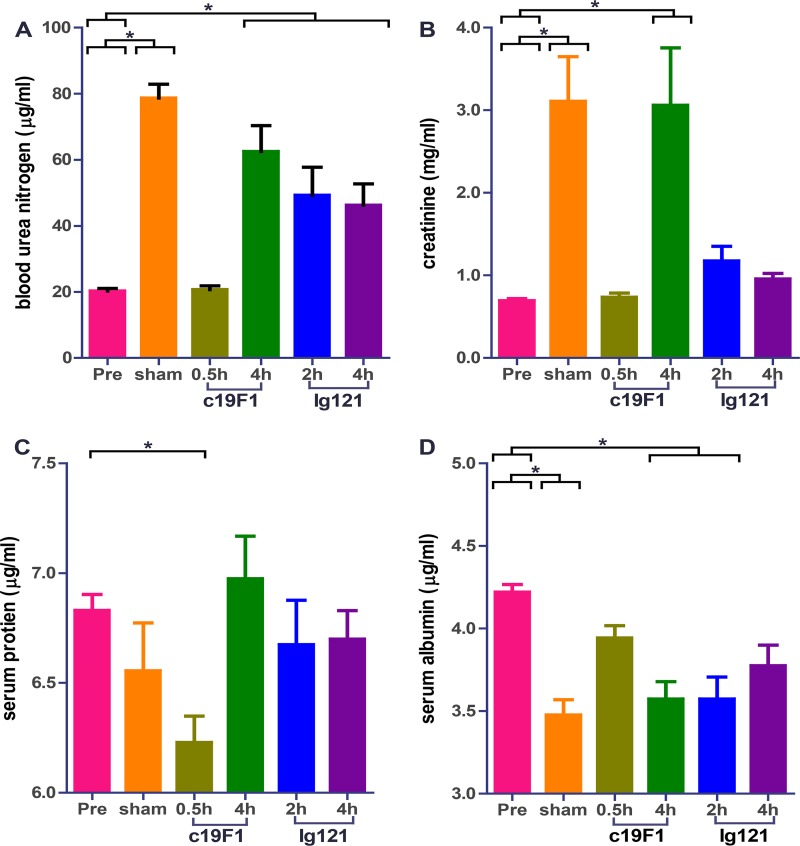
There were blood chemistry differences between the control group and treatment group. The average aspartate aminotransferase (AST) was observed to increase in sham-treated control animals compared to prechallenge levels (Fig. 5), and the early time point MAb interventions for both c19F1 (0.5 h) and IgG121 (2 h) showed no change compared to prechallenge control. The AST levels increased to levels comparable with those of sham-treated controls in the 4-h MAb-treated groups for both c19F1 and IgG121. A notable increase in alanine aminotransferase (ALT) was present in the sham-treated control animals and the MAb-treated animals. Other parameters of note included blood urea nitrogen (BUN) and creatinine increases in all controls and all but the 0.5-h c19F1 (BUN) and 0.5-h c19F1 and 4 h IgG121 (creatinine) groups (Fig. 6). Other notable changes were a significant decrease in serum protein in the 0.5-h c19F1 treatment group and a reduction in serum albumin in sham control and 4-h c19F1 and 2-h IgG121 treatment groups.
FIG 5.
Aspartate aminotransferase (AST) and alanine transaminase (ALT) measured from peripheral blood from all animals (n = 23) prior to SEB challenge and 24 h postchallenge and/or treatment with either antibody. Significant differences (P < 0.05) for either sham control or treated animals compared to preexposure values are indicated with an asterisk.
FIG 6.
Relevant clinical chemistries derived from peripheral blood from all animals (n = 23) prior to SEB challenge and 24 h postchallenge and/or treatment with either antibody. Each graph shows blood urea nitrogen (A), creatinine (B), serum protein (C), or serum albumin (D). Significant differences (P < 0.05) for either sham control or treated animals from preexposure values is indicated with an asterisk.
Cytokines.
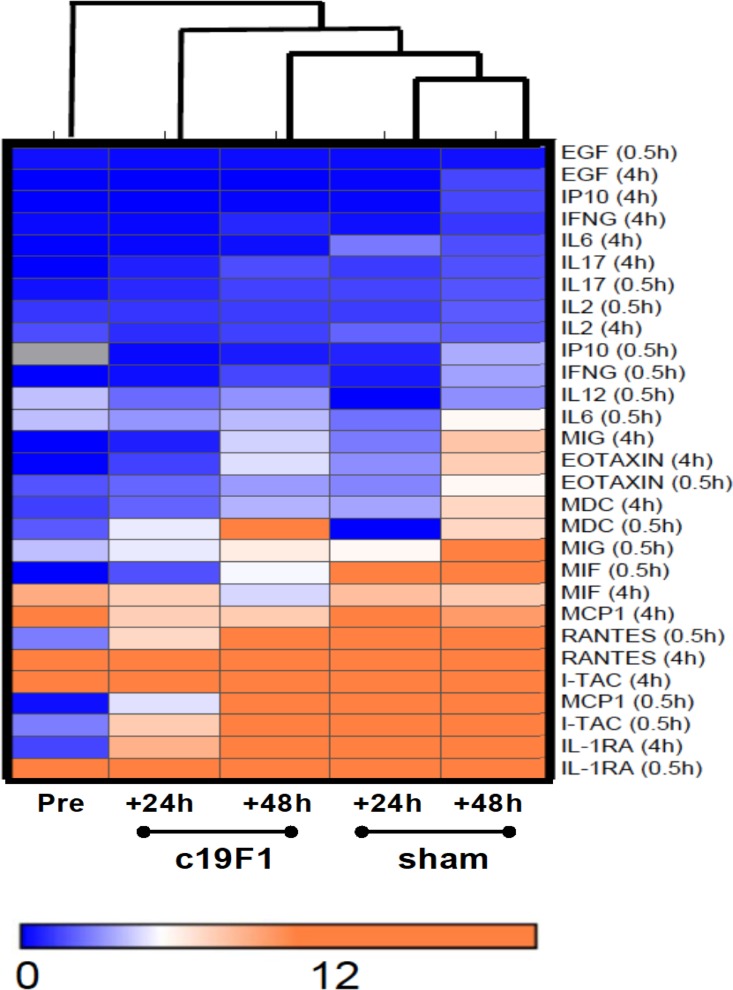
Cytokine and chemokines were measured in replicate serum samples in all animals prior to and 24 h and 48 h after intoxication SEB challenge. Analysis was performed using a Bio-Plex 200 suspension array system, allowing analysis for 28 analytes in a single serum sample. Results of this analysis indicated a strong inflammatory systemic response as a consequence of SEB challenge, with discretion of cytokine response between treated and control animals (Fig. 7). Notably lower concentrations were mainly early-phase proinflammatory cytokines and chemokines, including interleukin 1 receptor antagonist (IL-1RA), macrophage migration inhibitory factor (MIF), monokine-induced gamma (MIG), monocyte attractant protein 1 (MCP1), eotaxin (eosinophilic chemoattractant), and interleukin 6 (IL-6) at the early (0.5-h) c19F1 treatment intervention at 24 h postinfection (p.i.) compared to preexposure levels. There was a noticeable distinction between the gradient of concentrations of cytokines and chemokines between time points in the course of response (24 h versus 48 h) in both the treated and control animals.
FIG 7.
Hierarchical cluster analysis of cytokine data between c19F1-treated animals and controls. Each column represents blood collection time point prior to SEB exposure or postexposure (either 24 or 48 h) for c19F1 or sham-treated animal groups. Each horizontal category refers to time of treatment (either 0.5 or 4 h p.i.) and corresponding timed sham treatments. Orange indicates cytokines with a greater concentration relative to the geometrical mean of the naive values, and blue indicates cytokines with a concentration lower than the naive geometrical mean.
Lung pathology.
Lung damage due to SEB aerosol exposure was measured through wet lung weight in all sham and MAb treatment groups. In all cases treatment with either c19F1 or IgG121 resulted in a significant reduction in wet lung weight, with no difference distinguishable among the treatment groups (Fig. 8).
FIG 8.
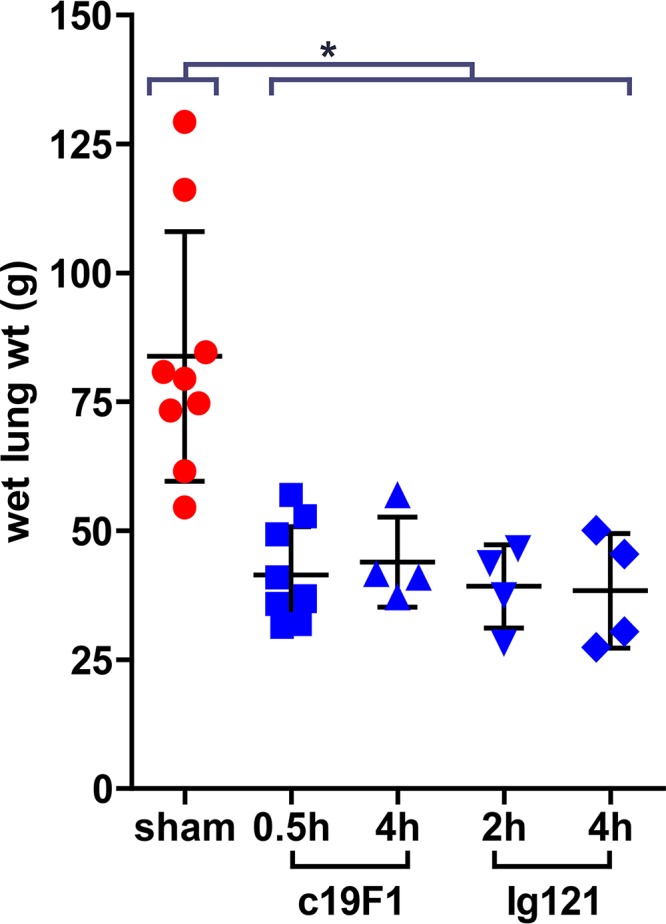
Wet lung weights of animals at necropsy. Lines and error bars represent means and SDs of each group. Weights of sham-treated animals were significantly different than all treated groups. *, significance at a P value of <0.05. There was no significant difference in lung weight between treatment groups.
Histopathology.
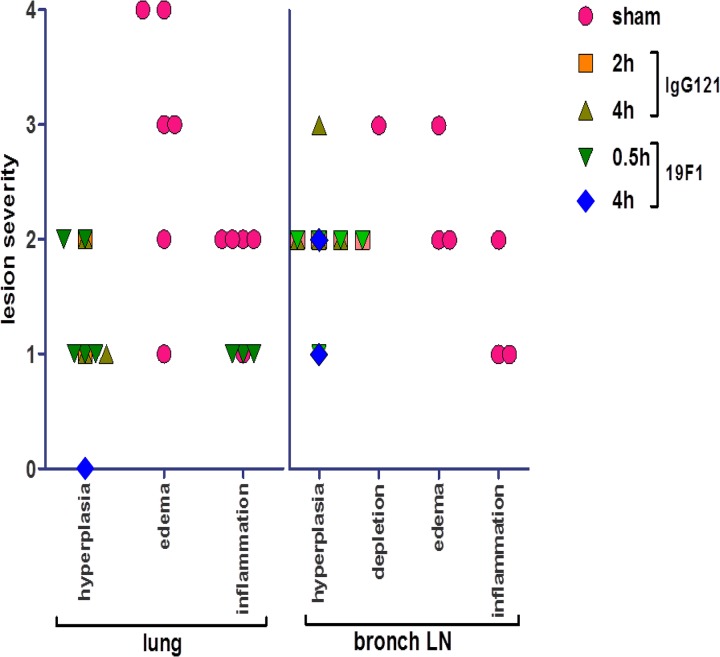
Five of six SEB-exposed sham treatment group animals developed severe pulmonary edema and mild intra-alveolar inflammation dominated by neutrophils, with most demonstrating edema and acute mild inflammation in the bronchial node (Fig. 9). One animal had minimal pulmonary edema without inflammation but acute randomly distributed necrotizing hepatitis and a small abscess in the mesenteric node consistent with bacterial infection. Mild chronic colitis was detected in four of six animals.
FIG 9.
Representative tissues from MAb-treated (IgG121 and 19F1 at 10 mg/kg each) and sham controls. Lungs from treated animals showed minimal inflammation; bronchial lymph nodes of treated animals showed mild lymphoid, diffuse hyperplasia. Lungs from sham-treated animals showed severe inflammation and acute fibrinous accumulation; bronchial lymph nodes showed inflammation and edema. The bar represents 100 μm.
SEB-exposed animals treated with IgG121 or c19F1 were nearly indistinguishable, as evidenced by similar categorical lesion scores of lung tissue from both treatment groups in contrast to the sham-treated animals (Fig. 10). Most had minimal to mild lymphoid hyperplasia in the lung and mild to moderate lymphoid hyperplasia of the bronchial node and spleen, and only three in the c19F1 group presented with minimal widely scattered foci of chronic inflammation in the lungs. Edema was not present in lung or bronchial nodes, and only one animal in the c19F1 group had a minimal degree of colitis.
FIG 10.
Categorical scoring of lesion severity in lungs and bronchial lymph nodes for major representative histological changes in each tissue type examined. Categories are represented as follows: 0, normal; 1, minimal; 2, mild; 3, moderate; and 4, severe.
DISCUSSION
The misuse of biological toxins such as SEB remains a threat to both the military and civilian populations. Recent attempts of poisonings through various mechanisms, including the U.S. postal service (37), are demonstrative of the ever-present threat and corresponding medical need for rapid-acting countermeasures. In this study, we have addressed the possibility of providing efficacious postexposure therapies to prevent the effects associated with SEB intoxication that would be suitable for use in humans after an accidental or intentional misuse exposure to SEB. The results reported are an important demonstration of a protective outcome in a nonhuman primate model of SEB intoxication and pathogenesis using one of two monoclonal antibodies. c19F1 and Ig121 are the only drug candidates demonstrated to be effective postexposure against aerosolized SEB in the rhesus macaque model, which is uniformly lethal given the appropriate dose and modality of exposure (aerosol).
The animals that survived exposure through the therapeutic administration of either of the MAbs showed a different profile in clinical response than the untreated controls. Hematological and blood chemistry changes showed minimal differences when group responses were compared. Pathological outcomes show clear differences in damage in the control animals that died from exposure compared to treated survivors, which showed minimal changes in the lung as a result of aerosol exposure. Together, the data derived from the efficacy experiments to date indicate that the anti-SEB MAbs c19F1 and IgG121 are the only effective antitoxin therapies that have been identified that could potentially be used to treat intoxication in humans. In order to develop these MAbs as treatments for SEB intoxication, however, further work is needed. Elucidation of the mechanism of action, binding sites, and toxicological studies is needed to ensure that there are no safety concerns. In addition, the prospect of humanizing c19F1 in order to increase protection while reducing unwanted human immunogenicity may be warranted and may further improve the acceptability of this combination treatment as an emergency clinical product.
MATERIALS AND METHODS
Study design.
An initial pharmacokinetics study was performed at the Tulane National Primate Research Center (TNPRC) to determine the optimal route of administration for each of the antibodies (data not shown); animals were administered either antibody either intramuscularly (i.m.) or i.v. and bled according to a predetermined schedule. Serum was analyzed via Biacore (L. Zeitlin) for determination of concentration of the antibody. Intravenous infusion was determined to be the optimal route of administration based upon the rapidity (<30 min) which the antibodies reached serum levels consistent with protection. In the therapeutic studies, all animals were first exposed to SEB aerosols at a target dose consistent with lethality. Thereafter, groups were administered either c19F1 or IgG1 via i.v. infusion at equivalent doses (10 mg/kg) at prescribed times (0.5, 2, or 4 h) postexposure. Sham-treated animals were administered sterile water for injection by that same route.
Animals.
Age- and sex-matched rhesus macaques (Macaca mulatta) weighing between 4 and 8 kg, free of simian immunodeficiency virus (SIV), simian type D retrovirus, and simian T-lymphotropic virus, were used. All experiments using macaques were approved by the Tulane Institutional Animal Care and Use Committee. The Tulane National Primate Research Center (TNPRC) is an Association for Assessment and Accreditation of Laboratory Animal Care International (AAALAC)-accredited facility (AAALAC no. 000594). The U.S. National Institutes of Health (NIH) Office of Laboratory Animal Welfare assurance number for the TNPRC is A3071-01. Nonhuman primate housing consisted of individual open metal caging units that allowed visual recognition and protected contact with other study animals in the room. Animals were maintained on standard primate chow supplemented daily with fresh fruits and vegetables. Animals were provided standard environmental enrichment during this study, which included manipulable items in cages, perches, foraging/task-oriented feeding methods, and human interactions with caretakers and research staff. All clinical procedures, including administration of anesthesia and analgesics, were carried out under the direction of a laboratory animal veterinarian. Animals were anesthetized with ketamine hydrochloride for blood collection procedures. All possible measures are taken to minimize discomfort of all the animals used in this study. Animals were closely monitored daily following surgery for any signs of illness such as anorexia, lethargy, diarrhea, vomiting, and dehydration. Appropriate medical care was implemented if any of these signs of illness were noted. If euthanasia was required in the judgment of the TNPRC veterinary staff, animals were euthanized in accordance with the recommendations of the panel on Euthanasia of the American Veterinary Medical Association. The standard method of euthanasia for nonhuman primates at the TNPRC is anesthesia with ketamine hydrochloride (10 mg/kg) followed by an overdose of sodium pentobarbital. Tulane University complies with NIH policy on animal welfare, the Animal Welfare Act, and all other applicable federal, state, and local laws.
SEB binding ELISA.
Purified SEB or attenuated SEB (STEBVax) was immobilized at 200 ng/well on 96-well Nunc MaxiSorp plates (Thermo Fisher Scientific) and incubated with serial dilutions of purified antibodies. Bound antibodies were detected using a horseradish peroxidase (HRP)-conjugated anti-human secondary antibody (KPL) and tetramethylbenzidene (TMB) substrate (Life Technologies). Absorbance values determined at 620 nm were transformed using Softmax 4 parameter curve-fit (Molecular Devices). The half-maximal effective concentration (EC50) at the inflection point of the curve was determined.
Animal challenge and therapy.
SEB toxin was obtained from BEI Resources (Manassas, VA) and was accompanied by results of purity testing shown by electrophoresis. The toxin was reconstituted in phosphate-buffered saline immediately before being placed into the aerosol-generating nebulizer. Animals were exposed to the toxin using a dynamic head-only inhalation exposure apparatus controlled by an electronic flow process platform (Biaera Technologies, Hagerstown, MD) and which has been described previously (38, 39). Briefly, anesthetized animals are transported into a class III biological safety cabinet outfitted with the head-only inhalation configuration. The aerosol concentration and the estimated inhaled dose were calculated as described previously (40) using the minute volume measured during plethsymography and the SEB concentration in the aerosol as determined by protein assays of the all-glass impinger samples.
Antibodies.
The antibodies were provided by IBT (IgG121) and Mapp (c19F1) as a liquid product in a sealed glass vacuum vial. The doses for the evaluation were derived from the starting concentration and administration of the antibody was based upon prevailing body weights of the animals enrolled in the study. During the time between the extraction and use of the antibody, the sterile syringes were stored at 4°C (in the dark) until administration. Care was taken to ensure that the antibody remained in solution prior to administration.
Hematology, serum biochemistry, and blood coagulation.
Hematologic analysis was performed with blood samples collected in EDTA anticoagulant using a Sysmex XT-2000i analyzer, and analysis of serum from clotted samples of blood was done on an Olympus AU400 chemistry analyzer, with results automatically downloaded to the Animal Record System.
Cytokine analysis.
Cytokine levels in serum were assayed using the Milliplex MAP primate/rhesus cytokine/chemokine polystyrene bead panel (PRCYTOMAG-40K; Millipore Corp. [Billerica, MA]). This assay provides analysis for selected cytokines and chemokines within a single sample, which are granulocyte colony-stimulating factor (G-CSF), vascular endothelial growth factor (VEGF), tumor necrosis factor alpha (TNF-α), transforming growth factor α (TGF-α), sCD40L, MIP-1β, MIP-1α, MCP-1, IL-18, IL-17, IL-15, IL-13, IL-12/23 (p40), IL-10, IL-8, IL-6, IL-5, IL-4, IL-2, IL-1β, IL-1RA, gamma interferon (IFN-γ), and granulocyte-macrophage colony-stimulating factor (GM-CSF). Briefly, collected blood serum samples from the primates are disturbed by vortex and then individually clarified through filter spin columns (catalog no. UFC30DV00; Millipore Corp.) by spinning at 12,000 × g for 4 min at room temperature. Each standard, control, or undiluted sample, in 25 μl, is added in duplicate to antibody-conjugated beads and incubated in a 96-well filter plate overnight at 2 to 8°C with shaking at 650 rpm. After 16 to 18 h, wells are washed, and 25 μl of detection antibody is added to each well. After 1 h of incubation at room temperature with shaking, 25 μl of streptavidin-phycoerythrin is added to each well and incubated for 30 min with shaking. After final washes are completed, 150 μl of sheath fluid is added to each well. The plate is analyzed using a Bio-Plex 200 suspension array system (Bio-Rad). The instrument settings are as follows: 50 events/bead, 100-μl sample size, and gate settings at 8,000 to 15,000. The software used to perform the assay and analyze data is Bio-Plex Manager version 6.0, which calculates concentrations in picograms per milliliter based on the respective standard curve for each cytokine.
Histopathology.
Tissue samples were fixed for 48 h in zinc-modified formalin (Z-Fix; Anatech, Ltd., Battle Creek, MI), dehydrated in a series of alcohols, embedded in paraffin, and sectioned at a thickness of 5 μm before deparaffinized sections were stained with hematoxylin and eosin. Sections were examined by light microscopy on a Leica DMLB microscope equipped with a Leica EC3 camera.
Statistical analysis.
Data were analyzed using Prism software (GraphPad Software, Inc.). In vivo survival curves were analyzed using the log rank (Mantel Cox) test.
REFERENCES
- 1.Ulrich RG. 2007. Staphylococcal enterotoxin B and related toxins. Borden Insitute, Washington, DC. [Google Scholar]
- 2.Stiles BG, Bavari S, Krakauer T, Ulrich RG. 1993. Toxicity of staphylococcal enterotoxins potentiated by lipopolysaccharide: major histocompatibility complex class II molecule dependency and cytokine release. Infect Immun 61:5333–5338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koning F, Rust C. 1992. Staphylococcal enterotoxin-mediated human T-T cell interactions. J Immunol 149:317–322. [PubMed] [Google Scholar]
- 4.Drake CG, Kotzin BL. 1992. Superantigens: biology, immunology, and potential role in disease. J Clin Immunol 12:149–162. doi: 10.1007/BF00918083. [DOI] [PubMed] [Google Scholar]
- 5.Tiedemann RE, Fraser JD. 1996. Cross-linking of MHC class II molecules by staphylococcal enterotoxin A is essential for antigen-presenting cell and T cell activation. J Immunol 157:3958–3966. [PubMed] [Google Scholar]
- 6.Buxser ES, Bonventre PF, Archer DL. 1983. Staphylococcal enterotoxin induced mitogenesis: toxin binding and cell-cell interactions. Microbiologica 6:181–190. [PubMed] [Google Scholar]
- 7.Williams O, Aroeira LS, Mengel J. 1995. T cell-dependent antibody response to staphylococcal enterotoxin B. Scand J Immunol 42:305–310. doi: 10.1111/j.1365-3083.1995.tb03660.x. [DOI] [PubMed] [Google Scholar]
- 8.Bell SJ, Vroegop SM, Buxser SE. 1994. Early activation and cell trafficking induced by staphylococcal enterotoxin B: effects of high- versus low-dose challenge on induction of anergy. Cell Immunol 154:440–452. doi: 10.1006/cimm.1994.1090. [DOI] [PubMed] [Google Scholar]
- 9.Kotzin BL. 1994. Superantigens and their role in disease. Hosp Pract (Off Ed) 29:59–63, 68–70. doi: 10.1080/21548331.1994.11443108. [DOI] [PubMed] [Google Scholar]
- 10.Saeed AI, Rieder SA, Price RL, Barker J, Nagarkatti P, Nagarkatti M. 2012. Acute lung injury induced by staphylococcal enterotoxin B: disruption of terminal vessels as a mechanism of induction of vascular leak. Microsc Microanal 18:445–452. doi: 10.1017/S1431927612000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattix ME, Hunt RE, Wilhelmsen CL, Johnson AJ, Baze WB. 1995. Aerosolized staphylococcal enterotoxin B-induced pulmonary lesions in rhesus monkeys (Macaca mulatta). Toxicol Pathol 23:262–268. doi: 10.1177/019262339502300304. [DOI] [PubMed] [Google Scholar]
- 12.Peterson BT, Miller EJ, Morris D. 1999. Neutrophil influx and migration in rabbit airways in response to staphylococcal enterotoxin-A. Exp Lung Res 25:41–54. doi: 10.1080/019021499270411. [DOI] [PubMed] [Google Scholar]
- 13.Komisar JL, Weng CF, Oyejide A, Hunt RE, Briscoe C, Tseng J. 2001. Cellular and cytokine responses in the circulation and tissue reactions in the lung of rhesus monkeys (Macaca mulatta) pretreated with cyclosporin A and challenged with staphylococcal enterotoxin B. Toxicol Pathol 29:369–378. doi: 10.1080/019262301316905336. [DOI] [PubMed] [Google Scholar]
- 14.Neumann B, Engelhardt B, Wagner H, Holzmann B. 1997. Induction of acute inflammatory lung injury by staphylococcal enterotoxin B. J Immunol 158:1862–1871. [PubMed] [Google Scholar]
- 15.Roy CJ, Warfield KL, Welcher BC, Gonzales RF, Larsen T, Hanson J, David CS, Krakauer T, Bavari S. 2005. Human leukocyte antigen-DQ8 transgenic mice: a model to examine the toxicity of aerosolized staphylococcal enterotoxin B. Infect Immun 73:2452–2460. doi: 10.1128/IAI.73.4.2452-2460.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savransky V, Rostapshov V, Pinelis D, Polotsky Y, Korolev S, Komisar J, Fegeding K. 2003. Murine lethal toxic shock caused by intranasal administration of staphylococcal enterotoxin B. Toxicol Pathol 31:373–378. doi: 10.1080/01926230390201093. [DOI] [PubMed] [Google Scholar]
- 17.DaSilva L, Welcher BC, Ulrich RG, Aman MJ, David CS, Bavari S. 2002. Humanlike immune response of human leukocyte antigen-DR3 transgenic mice to staphylococcal enterotoxins: a novel model for superantigen vaccines. J Infect Dis 185:1754–1760. doi: 10.1086/340828. [DOI] [PubMed] [Google Scholar]
- 18.LeClaire RD, Hunt RE, Bavari S, Estep JE, Nelson GO, Wilhelmsen CL. 1996. Potentiation of inhaled staphylococcal enterotoxin B-induced toxicity by lipopolysaccharide in mice. Toxicol Pathol 24:619–626. doi: 10.1177/019262339602400513. [DOI] [PubMed] [Google Scholar]
- 19.Bavari S, Hunt RE, Ulrich RG. 1995. Divergence of human and nonhuman primate lymphocyte responses to bacterial superantigens. Clin Immunol Immunopathol 76:248–254. doi: 10.1006/clin.1995.1123. [DOI] [PubMed] [Google Scholar]
- 20.Lowell GH, Colleton C, Frost D, Kaminski RW, Hughes M, Hatch J, Hooper C, Estep J, Pitt L, Topper M, Hunt RE, Baker W, Baze WB. 1996. Immunogenicity and efficacy against lethal aerosol staphylococcal enterotoxin B challenge in monkeys by intramuscular and respiratory delivery of proteosome-toxoid vaccines. Infect Immun 64:4686–4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krakauer T, Pitt L, Hunt RE. 1997. Detection of interleukin-6 and interleukin-2 in serum of rhesus monkeys exposed to a nonlethal dose of staphylococcal enterotoxin B. Mil Med 162:612–615. doi: 10.1093/milmed/162.9.612. [DOI] [PubMed] [Google Scholar]
- 22.Boles JW, Pitt ML, LeClaire RD, Gibbs PH, Torres E, Dyas B, Ulrich RG, Bavari S. 2003. Generation of protective immunity by inactivated recombinant staphylococcal enterotoxin B vaccine in nonhuman primates and identification of correlates of immunity. Clin Immunol 108:51–59. doi: 10.1016/S1521-6616(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 23.Coffman JD, Zhu J, Roach JM, Bavari S, Ulrich RG, Giardina SL. 2002. Production and purification of a recombinant staphylococcal enterotoxin B vaccine candidate expressed in Escherichia coli. Protein Expr Purif 24:302–312. doi: 10.1006/prep.2001.1556. [DOI] [PubMed] [Google Scholar]
- 24.Proctor RA. 2012. Is there a future for a Staphylococcus aureus vaccine? Vaccine 30:2921–2927. doi: 10.1016/j.vaccine.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 25.Krakauer T. 1995. Differential inhibitory effects of interleukin-10, interleukin-4, and dexamethasone on staphylococcal enterotoxin-induced cytokine production and T cell activation. J Leukoc Biol 57:450–454. doi: 10.1002/jlb.57.3.450. [DOI] [PubMed] [Google Scholar]
- 26.Krakauer T. 1994. Cell adhesion molecules are co-receptors for staphylococcal enterotoxin B-induced T-cell activation and cytokine production. Immunol Lett 39:121–125. doi: 10.1016/0165-2478(94)90096-5. [DOI] [PubMed] [Google Scholar]
- 27.McKallip RJ, Fisher M, Gunthert U, Szakal AK, Nagarkatti PS, Nagarkatti M. 2005. Role of CD44 and its v7 isoform in staphylococcal enterotoxin B-induced toxic shock: CD44 deficiency on hepatic mononuclear cells leads to reduced activation-induced apoptosis that results in increased liver damage. Infect Immun 73:50–61. doi: 10.1128/IAI.73.1.50-61.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun J, Law GP, Bridges CC, McKallip RJ. 2012. CD44 as a novel target for treatment of staphylococcal enterotoxin B-induced acute inflammatory lung injury. Clin Immunol 144:41–52. doi: 10.1016/j.clim.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Kissner TL, Ruthel G, Alam S, Mann E, Ajami D, Rebek M, Larkin E, Fernandez S, Ulrich RG, Ping S, Waugh DS, Rebek J Jr, Saikh KU. 2012. Therapeutic inhibition of pro-inflammatory signaling and toxicity to staphylococcal enterotoxin B by a synthetic dimeric BB-loop mimetic of MyD88. PLoS One 7:e40773. doi: 10.1371/journal.pone.0040773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Varshney AK, Wang X, MacIntyre J, Zollner RS, Kelleher K, Kovalenko OV, Pechuan X, Byrne FR, Fries BC. 2014. Humanized staphylococcal enterotoxin B (SEB)-specific monoclonal antibodies protect from SEB intoxication and Staphylococcus aureus infections alone or as adjunctive therapy with vancomycin. J Infect Dis 210:973–981. doi: 10.1093/infdis/jiu198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.MacIntyre JL, Varshney AK, Wang X, Gatto S, Friedman C, Liu Y, Kerns K, Kovalenko O, Adkins K, Zollner R, Fries BC, Byrne FR. 2015. Optimization of experimental conditions for functional in vitro characterization of humanized antibodies specific for staphylococcal enterotoxin B. Int Immunopharmacol 28:354–358. doi: 10.1016/j.intimp.2015.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Drozdowski B, Zhou Y, Kline B, Spidel J, Chan YY, Albone E, Turchin H, Chao Q, Henry M, Balogach J, Routhier E, Bavari S, Nicolaides NC, Sass PM, Grasso L. 2010. Generation and characterization of high affinity human monoclonal antibodies that neutralize staphylococcal enterotoxin B. J Immune Based Ther Vaccines 8:9. doi: 10.1186/1476-8518-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Larkin EA, Stiles BG, Ulrich RG. 2010. Inhibition of toxic shock by human monoclonal antibodies against staphylococcal enterotoxin B. PLoS One 5:e13253. doi: 10.1371/journal.pone.0013253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karauzum H, Chen G, Abaandou L, Mahmoudieh M, Boroun AR, Shulenin S, Devi VS, Stavale E, Warfield KL, Zeitlin L, Roy CJ, Sidhu SS, Aman MJ. 2012. Synthetic human monoclonal antibodies toward staphylococcal enterotoxin B (SEB) protective against toxic shock syndrome. J Biol Chem 287:25203–25215. doi: 10.1074/jbc.M112.364075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sully EK, Whaley K, Bohorova N, Bohorov O, Goodman C, Kim D, Pauly M, Velasco J, Holtsberg FW, Stavale E, Aman MJ, Tangudu C, Uzal FA, Mantis NJ, Zeitlin L. 2014. A tripartite cocktail of chimeric monoclonal antibodies passively protects mice against ricin, staphylococcal enterotoxin B and Clostridium perfringens epsilon toxin. Toxicon 92:36–41. doi: 10.1016/j.toxicon.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bavari S, Dyas B, Ulrich RG. 1996. Superantigen vaccines: a comparative study of genetically attenuated receptor-binding mutants of staphylococcal enterotoxin A. J Infect Dis 174:338–345. doi: 10.1093/infdis/174.2.338. [DOI] [PubMed] [Google Scholar]
- 37.Audi J, Belson M, Patel M, Schier J, Osterloh J. 2005. Ricin poisoning: a comprehensive review. JAMA 294:2342–2351. doi: 10.1001/jama.294.18.2342. [DOI] [PubMed] [Google Scholar]
- 38.Roy CJ, Adams AP, Wang E, Leal G, Seymour RL, Sivasubramani SK, Mega W, Frolov I, Didier PJ, Weaver SC. 2013. A chimeric Sindbis-based vaccine protects cynomolgus macaques against a lethal aerosol challenge of eastern equine encephalitis virus. Vaccine 31:1464–1470. doi: 10.1016/j.vaccine.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pincus SH, Bhaskaran M, Brey RN III, Didier PJ, Doyle-Meyers LA, Roy CJ. 2015. Clinical and pathological findings associated with aerosol exposure of macaques to ricin toxin. Toxins (Basel) 7:2121–2133. doi: 10.3390/toxins7062121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roy CJ, Pitt L. 2005. Infectious disease aerobiology: aerosol challenge methods, p 61–76. In Swearengen JR. (ed), Biodefense: research methodology and animal models. CRC Press Taylor & Francis Group, Boca Raton, FL. [Google Scholar]