The in vitro activity of omadacycline, a new tetracycline derivative, was evaluated against isolates of Mycobacterium abscessus, Mycobacterium chelonae, and Mycobacterium fortuitum using a broth microtiter dilution assay. Omadacycline had MIC90 values of 2 μg/ml, 0.25 μg/ml, and 0.5 μg/ml, respectively.
KEYWORDS: nontuberculous mycobacteria, antimicrobials, in vitro
ABSTRACT
The in vitro activity of omadacycline, a new tetracycline derivative, was evaluated against isolates of Mycobacterium abscessus, Mycobacterium chelonae, and Mycobacterium fortuitum using a broth microtiter dilution assay. Omadacycline had MIC90 values of 2 μg/ml, 0.25 μg/ml, and 0.5 μg/ml, respectively. The in vitro activity of omadacycline against rapidly growing mycobacteria indicates that it may have the potential to improve therapy for infections caused by these organisms.
INTRODUCTION
Infections caused by Mycobacterium abscessus, Mycobacterium chelonae, and Mycobacterium fortuitum occur more frequently in immunocompromised individuals than in healthy humans. When they do occur, they are difficult to treat and do not respond well to antimicrobials used for other mycobacterial infections (1).
M. abscessus is the third most common nontuberculous mycobacterial (NTM) respiratory pathogen recovered from lungs in the United States (1). Clinical infections can range from asymptomatic to severe bronchiectasis and/or cavitary lung disease. M. abscessus is inherently multidrug resistant. Drug regimens are selected on the basis of results from in vitro susceptibility studies. The optimal therapeutic regimen and treatment duration are not well established. M. chelonae causes a range of diseases, including cellulitis and eye infections. M. chelonae is often found in water heaters, pedicure beds, and tattoo parlors (2). It is often treated with azithromycin or clarithromycin. M. fortuitum is usually associated with soft tissue infections and hospital-acquired postoperative infections in immunocompromised hosts.
Omadacycline (OMC) is a new intravenous and oral tetracycline derivative with potent in vitro and in vivo activities against many drug-resistant pathogens, including common Gram-positive aerobes, many Gram-negative aerobes, anaerobes, and atypical bacterial pathogens (3, 4). The activity of OMC in the presence of tetracycline-specific efflux pumps and ribosomal protection is conferred by substitutions at C-7 and C-9, respectively (Fig. 1).
FIG 1.
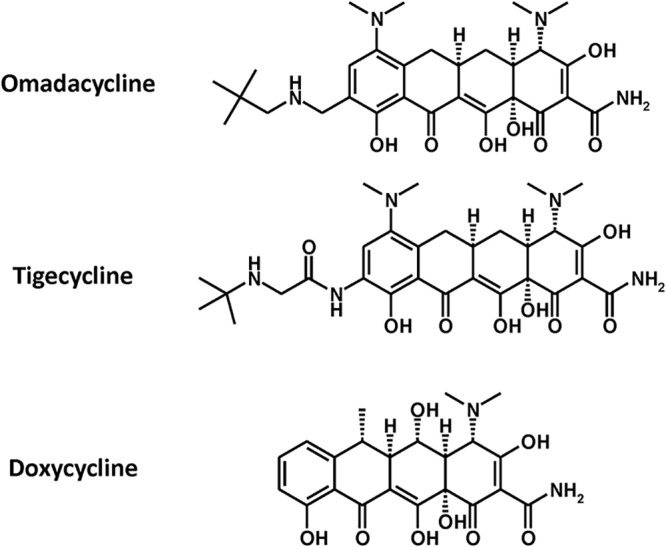
Chemical structures of omadacycline, tigecycline, and doxycycline.
The purpose of the present study was to evaluate the in vitro activities of OMC, doxycycline (DOX), and tigecycline (TGC) against clinical isolates of M. abscessus complex, M. chelonae, and M. fortuitum. Amikacin (AMK) served as a control drug.
OMC, TGC, DOX, and AMK were obtained from Paratek Pharmaceuticals (Boston, MA), Carbosynth (San Diego, CA), Sigma Chemical Co. (St. Louis, MO), and Bristol Meyers Squibb (Princeton, NJ), respectively. OMC, TGC, and DOX were dissolved in double-distilled water at a final concentration of 2 mg/ml and sterile filtered through a 0.22-μm filter (Corning, Inc., Corning, NY). AMK was dissolved in dimethyl sufoxide at a final concentration of 5 mg/ml. The drugs were frozen at −20°C until used.
M. abscessus complex and M. fortuitum isolates were kindly provided by Barbara Body (LabCorp, Burlington, NC) and Barbara Brown-Elliot (University of Texas Health Science Center, Tyler, TX). The isolates were grown in cation-adjusted Mueller-Hinton broth (CAMHB; Becton-Dickinson, Sparks, MD) on a rotary shaker at 37°C for 2 or 5 days, respectively. The cultures were diltuted to 10 Klett units (equivalent to 5 × 107 CFU/ml) (photoelectric colorimeter; Manostat Corp., New York, NY) and frozen at −70°C until used. M. chelonae isolates were provided by Barbara Brown-Elliot. The isolates were grown on cation-adjusted Mueller-Hinton agar at 32°C for 3 to 5 days prior to testing.
Polystyrene 96-well round-bottom microtiter plates (Corning, Inc., Corning, NY) were prepared by adding 50 μl of CAMHB to each well. The antimicrobial compounds were thawed and diluted in CAMHB. Fifty microliters of each solution was added to the first well and serially diluted, leaving the last well with broth only (positive-control well). M. abscessus and M. fortuitum isolates were thawed and diluted in CAMHB to a final concentration of approximately 1 × 105 CFU/ml (inoculum range for M. abscessus, 1.2 × 104 to 2.6 × 105 CFU/ml, and for M. fortuitum, 1.3 × 104 to 2.4 × 106 CFU/ml). M. chelonae was prepared by placing several colonies of each isolate in CAMHB, sonicating for 5 to 10 min, and diluting to approximately 1 × 105 CFU/ml (inoculum range, 2.6 × 104 to 3.2 × 106 CFU/ml). To each well, 50 μl of the appropriate mycobacterial cell suspension was added. Plates were sealed and incubated at 37°C in ambient air for 2 days (M. fortuitum) or 5 days (M. abscessus) or incubated at 32°C for 4 days (M. chelonae) prior to reading. Each isolate was tested in duplicate, with one isolate of each species serving as a control strain. The MIC was defined as the lowest concentration of antimicrobial agent yielding no visible turbidity. The MIC50 and MIC90 values are defined as the concentrations at which 50% and 90% of the isolates were inhibited, respectively.
The MICs of OMC, TGC, DOX, and AMK against 24 isolates of the M. abscessus complex are presented in Table 1. The MIC50 and MIC90 of OMC, DOX, and AMK against M. abscessus were 1 μg/ml and 2 μg/ml, >64 μg/ml and >64 μg/ml, and 2 μg/ml and 8 μg/ml, respectively. TGC was tested against a subset of these organisms (n = 14) and was found to have activity similar to that of OMC.
TABLE 1.
MICs of omadacycline, doxycycline, and tigecycline against 24 isolates of the Mycobacterium abscessus complex
| Isolate | MIC (μg/ml) for: |
|||
|---|---|---|---|---|
| Amikacin | Doxycycline | Omadacycline | Tigecycline | |
| BB2 | 8 | >64 | 1 | 2 |
| BB4 | 8 | 2 | 4 | 2 |
| 5922a | 2 | 16 | 0.125 | 0.25 |
| BB3 | 2 | 4 | 0.06 | 0.06 |
| BB6 | 4 | 16 | 0.06 | 0.125 |
| 5908a | 2 | >64 | 1 | 2 |
| BB7 | 0.5 | 0.25 | 2 | 2 |
| 6031a | 0.5 | 2 | 0.25 | 1 |
| 5785a | 1 | 2 | 0.25 | 0.5 |
| BB8 | 2 | >64 | 1 | |
| 6111a | 2 | >64 | 1 | 0.5 |
| 6005a | 4 | >64 | 1 | 0.5 |
| 5605a | 2 | >64 | 1 | |
| 5931a | 0.5 | 16 | 1 | |
| BB1 | 2 | >64 | 2 | |
| BB5 | 8 | >64 | 2 | 1 |
| 5812a | 4 | >64 | 2 | |
| 5901a | 2 | >64 | 1 | |
| 5960a | 1 | 8 | 8 | 8 |
| 6142a | 4 | >64 | 1 | |
| 5922a | 2 | 32 | 0.5 | |
| LT949 | 8 | >64 | 1 | |
| 6025a | 8 | >64 | 1 | 1 |
| 6153a | 8 | >64 | 2 | |
M. abscessus complex isolates were determined further to the species level using rpoB and erm gene sequences.
The MICs of OMC, TGC, DOX, and AMK against 22 isolates of M. chelonae are presented in Table 2. The MIC50 and MIC90 of OMC, TGC, DOX, and AMK against M. chelonae were 0.125 μg/ml and 0.25 μg/ml, 0.06 μg/ml and 0.25 μg/ml, 32 μg/ml and 64 μg/ml, and 4 μg/ml and 8 μg/ml, respectively.
TABLE 2.
MICs of OMC, DOX, and TGC against 22 isolates of Mycobacterium chelonae
| Isolate | MIC (μg/ml) for: |
|||
|---|---|---|---|---|
| Amikacin | Doxycycline | Omadacycline | Tigecycline | |
| 7323 | 4 | 64 | 0.125 | 0.125 |
| 7534 | 8 | 32 | 0.03 | 0.03 |
| 7368 | 16 | 64 | 0.03 | 0.03 |
| 7514 | 8 | 32 | 0.06 | 0.06 |
| 7584 | 4 | 64 | 0.06 | 0.06 |
| 7192 | 4 | 16 | 0.015 | 0.03 |
| 7466 | 2 | 32 | 0.03 | 0.03 |
| 7533 | 4 | 64 | 0.25 | 0.125 |
| 7579 | 4 | 16 | 0.125 | 0.03 |
| 7614 | 8 | 64 | 0.125 | 0.125 |
| 7414 | 4 | 32 | 0.125 | 0.06 |
| 7313 | 2 | 32 | 0.125 | 0.25 |
| 7281 | 8 | 64 | 0.25 | 0.5 |
| 7328 | 8 | 16 | 0.015 | 0.015 |
| 7294 | 8 | 32 | 0.25 | 0.125 |
| 14-S-03 | 4 | 64 | 0.06 | 0.5 |
| 14-S-04 | 4 | 32 | 0.06 | 0.06 |
| 14-S-05 | 8 | 32 | 0.125 | 0.125 |
| 14-S-06 | 8 | 64 | 0.03 | 0.03 |
| 14-S-07 | 4 | 32 | 0.06 | 0.06 |
| 35757 | 2 | 32 | 0.125 | 0.125 |
| 7302 | 4 | 64 | 0.25 | 0.25 |
The MICs of OMC, TGC, DOX, and AMK against 20 isolates of M. fortuitum are presented in Table 3. The MIC50 and MIC90 of OMC, TGC, DOX, and AMK against M. fortuitum were 0.125 μg/ml and 0.5 μg/ml, 0.25 μg/ml and 0.5 μg/ml, 8 μg/ml and 64 μg/ml, and 0.5 μg/ml and 4 μg/ml, respectively.
TABLE 3.
MICs of OMC, DOX, and TGC against 20 isolates of Mycobacterium fortuitum
| Isolate | MIC (μg/ml) for: |
|||
|---|---|---|---|---|
| Amikacin | Doxycycline | Omadacycline | Tigecycline | |
| 3349 | 8 | 16 | 0.25 | 0.25 |
| 3499 | 0.25 | 0.06 | 0.03 | 0.015 |
| 2797 | 2 | >64 | 0.125 | 0.06 |
| 32 | 1 | 0.125 | 0.25 | 0.25 |
| 33 | 2 | 0.125 | 0.125 | 0.125 |
| 3489 | 1 | 8 | 0.125 | 0.015 |
| 3491 | 1 | <0.06 | 0.125 | 0.015 |
| 54 | 0.5 | <0.06 | 0.06 | 0.03 |
| 38 | 0.5 | 0.5 | 0.125 | 0.06 |
| 36 | 1 | 0.125 | 0.125 | 0.03 |
| 3480 | 0.5 | 16 | 0.25 | 0.25 |
| 3126 | 0.5 | 16 | 0.125 | 0.25 |
| 3579 | 1 | 16 | 0.25 | 0.25 |
| 7484 | 16 | 64 | 0.5 | 0.5 |
| 3488 | 0.5 | 32 | 0.5 | 0.25 |
| 3276 | 0.5 | 0.25 | 0.25 | 0.25 |
| 3442 | 0.5 | 0.25 | 1 | 1 |
| 3316 | 0.125 | 32 | 0.125 | 0.25 |
| 3490 | 0.5 | 16 | 0.25 | 0.25 |
| 2491 | 4 | >64 | 1 | 0.5 |
OMC and TGC had similar in vitro activities against M. abscessus, M. chelonae, and M. fortuitum. The MICs of OMC were lower than those of DOX and were less than or equal to those of AMK for all isolates tested. In vitro evaluation of OMC against a larger group of isolates would be useful, as would in vivo studies in a murine test system. The in vitro activity of OMC suggests that further development as a potential therapy for infections caused by rapidly growing mycobacteria is warranted.
ACKNOWLEDGMENT
This work was supported in part by Paratek Pharmaceuticals, Inc.
REFERENCES
- 1.Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K. 2007. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 175:367–416. doi: 10.1164/rccm.200604-571ST. [DOI] [PubMed] [Google Scholar]
- 2.Falkinham J. 2011. Nontuberculous mycobacteria from household plumbing of patients with nontuberculous mycobacteria disease. Emerg Infect Dis 17:419–424. doi: 10.3201/eid1703.101510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macone AB, Caruso BK, Leahy Rg, Donatelli J, Weir S, Draper MP, Tanaka SK, Levy SB. 2014. In vitro and in vivo antibacterial activities of omadacycline, a novel aminomethylcycline. Antimicrob Agents Chemother 58:1127–1135. doi: 10.1128/AAC.01242-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka SK, Steenbergen J, Villano S. 2016. Discovery, pharmacology, and clinical profile of omadacycline, a novel aminomethylcycline antibiotic. Bioorg Med Chem 24:6409–6419. doi: 10.1016/j.bmc.2016.07.029. [DOI] [PubMed] [Google Scholar]


