Abstract
OBJECTIVE
To evaluate whether quadrivalent human papillomavirus vaccine (4vHPV) administered during the periconceptional period or during pregnancy was associated with increased risks for adverse obstetric events, adverse birth outcomes, or selected major structural birth defects.
METHODS
We conducted a retrospective, observational cohort study using administrative and health care data from the Vaccine Safety Datalink. Insured women 13–27 years old with singleton pregnancies and a live birth from January 1, 2007, through September 1, 2013, who received 4vHPV during the periconceptional period (2 weeks before to 2 weeks after their last menstrual period), during pregnancy, or during both periods combined were compared with women who had a live birth during the same time period and received 4vHPV 4–18 months before their last menstrual period. We examined risks of gestational diabetes, hypertensive disorders of pregnancy, chorioamnionitis, preterm birth, small-for-gestational-age birth, and selected major structural birth defects in offspring. We estimated relative risks associated with receipt of 4vHPV during the periconceptional period, during pregnancy, and both exposure periods combined using a generalized linear model with Poisson distribution including a propensity score that included relevant maternal demographic and pregnancy characteristics.
RESULTS
Of 92,579 potentially eligible pregnant women, 720 received 4vHPV during the periconceptional period, 638 received 4vHPV during pregnancy, and 8,196 received 4vHPV during the comparison period. Administration of 4vHPV during pregnancy was not associated with increased risk of adverse obstetric events, birth outcomes. Preterm birth occurred in 7.9% of pregnancies with vaccine exposures during pregnancy compared with 7.6% of pregnancies with vaccination in the comparison period (adjusted relative risk 0.97, 95% CI 0.72–1.3). Major structural birth defects were diagnosed in 2.0% of pregnancies with vaccine exposure during pregnancy compared with 1.8% of pregnancies with vaccine exposure during the comparison period (adjusted prevalence ratio 1.0, 95% CI 0.52–1.9). Results were similar for 4vHPV exposure during the periconceptional period.
CONCLUSION
Quadrivalent HPV vaccine inadvertently administered in pregnancy or during the periconceptional period was not associated with adverse pregnancy or birth outcomes.
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States.1 Although most infections are asymptomatic and resolve spontaneously,2 persistent infections with high-risk HPV genotypes can cause cervical, anogenital, and oropharyngeal cancers. The quadrivalent HPV vaccine (4vHPV) has been shown effective in preventing precancerous cervical disease.3
Since 2006, the Advisory Committee on Immunization Practices has recommended routine HPV vaccination for girls 11–12 years of age.4,5 Human papillomavirus vaccines are also recommended for females aged 13–26 years, if not previously vaccinated, opening a window for vaccine exposures during childbearing years.5 In 2014, the U.S. birth rate for teenagers 15–19 years of age was 24.5 per 1,000 and the mean maternal age at first birth was 26.3 years.6 The available HPV vaccines are inactivated; even so, they are not intended for administration during pregnancy. Nevertheless, pregnancy testing before vaccination is not recommended.4,7
Studies on vaccination with 4vHPV and risks of adverse maternal or infant outcomes after inadvertent 4vHPV exposures in pregnancy have primarily been through passive surveillance or post hoc evaluations of pregnancies occurring among clinical trial participants and have not shown an increased risk.8,9 Observational studies have been few and limited by size and design with the exception of a recent study from the Netherlands.10,11 The guidelines on pregnancy and HPV vaccine are therefore based on limited data regarding inadvertent vaccination during pregnancy or during the periconceptional period.
The goals of our study were to evaluate whether inadvertent 4vHPV exposures in the periconceptional period, or during pregnancy, were associated with increased risks for adverse maternal or infant outcomes.
MATERIALS AND METHODS
This retrospective, observational cohort study was conducted within the Vaccine Safety Datalink. The Vaccine Safety Datalink is a collaborative effort between the Centers for Disease Control and Prevention’s Immunization Safety Office and several large health systems to monitor the safety of vaccines and conduct studies about rare and serious adverse events after immunizations administered within the United States.12
In this study we used standardized data from seven Vaccine Safety Datalink sites (Kaiser Permanente Northern California, Kaiser Permanente Southern California, Kaiser Permanente Northwest, Group Health Cooperative, Kaiser Permanente Colorado, Marshfield Clinic, and HealthPartners) located in six states. We identified maternal–infant pairs who met the following criteria: singleton pregnancy resulting in a live birth between January 1, 2007, and September 1, 2013; and a mother between the ages of 13 and 27 years at the end of pregnancy, with continuous insurance coverage from 6 months before her last menstrual period through 6 weeks postpartum and with at least one outpatient visit at an affiliated site during the study period. For one site, data on 4vHPV exposures during January 1, 2008, through March 20, 2008, were not available. Pregnancies were identified using a validated algorithm based on administrative, electronic health records and claims data13 utilized in recent studies of both vaccine safety14–16 and vaccine coverage during pregnancy.17,18
To better control for confounders, we also limited our sample to live births with birth weight and gestational age in our automated Vaccine Safety Datalink files. Gestational age at delivery was based on clinician assessment. We excluded women who 1) received one or more live virus vaccines during pregnancy or 4vHPV in the third trimester (greater than 28 weeks of gestation); 2) had a multiple gestation; or 3) who never received 4vHPV. We also excluded live births with an implausible gestational age (less than 20 and greater than 43 weeks of gestation) or birth weight (less than 350 g) (Fig. 1). During the study period, 4vHPV was the only HPV vaccine administered at the participating sites.
Fig. 1.
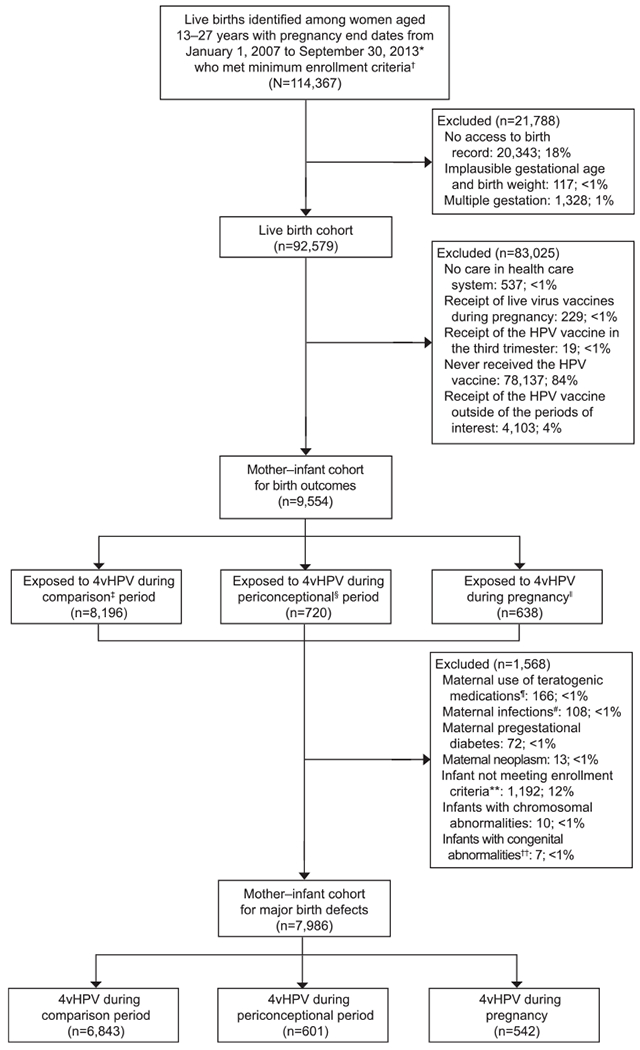
Flowchart. 4vHPV, quadrivalent human papillomavirus (HPV) vaccine. *Except for one site, January 20, 2009–September 30, 2013. †Continuous insurance enrollment from 6 months before their last menstrual period through 6 weeks postpartum. ‡Eighteen to 4 months before pregnancy. §Two weeks before to 2 weeks after last menstrual period. ‖Two to 28 weeks of gestation. ¶Isotretinoin, bexarotene, acitretin, misoprostol, methotrexate, mycophenolate mofetil, azathioprine, thalidomide, warfarin, lithium, amiodarone, dronedarone, carbamazepine, fosphenytoin, phenytoin, mephobarbital, phenobarbital, primidone, topiramate, valproate, leflunamide. #Toxoplasmosis, syphilis, varicella, rubella, and cytomegalovirus in mother’s chart. **Infants surviving to age 1 year; enrollment consists of 4 non-consecutive months during the first year of life, at least 1 month of insurance in the first 3 months of life, and at least one care encounter. Infants who died during the first year of life and those hospitalized for more than 30 days after birth were not required to meet criteria. Twelve percent of infants did not meet enrollment criteria: 10.7% of during-pregnancy exposures, 12.1% of exposures during the periconceptional period, and 12.9% of the comparison group for these birth defect analyses. ††Toxoplasmosis, syphilis, varicella, rubella, and cytomegalovirus in infant chart.
To evaluate the risk of major structural birth defects after inadvertent 4vHPV exposure, we performed separate analyses with a subset of the full cohort (Fig. 1). For these analyses, we examined maternal–infant pairs with at least 4 months of infant insurance enrollment and one or more infant outpatient visits at the relevant Vaccine Safety Datalink site. In the case of infant mortality or for infants hospitalized for more than 30 days, these inclusion criteria were not applied and these infants were included in the cohort. Additional exclusions for this subset were maternal use of teratogenic medication during pregnancy or within 6 months of their last menstrual period, congenital infections (toxoplasmosis, syphilis, varicella, rubella, and cytomegalovirus based on maternal or infant diagnoses), maternal neoplasm, maternal pregestational diabetes, and infant chromosomal abnormalities (Fig. 1).
Receipt of 4vHPV was identified from the standardized Vaccine Safety Datalink vaccine files. We then classified vaccination for exposed women as occurring during the periconceptional period (defined as the period from 2 weeks before 2 weeks after their last menstrual period) or during pregnancy (defined as the period from 2 weeks of gestation through 28 weeks of gestation) (Fig. 2). Our comparison group consisted of pregnant women who received one or more doses of 4vHPV between 4 and 18 months before their last menstrual period with no 4vHPV exposures during the periconceptional period or during pregnancy.
Fig. 2.
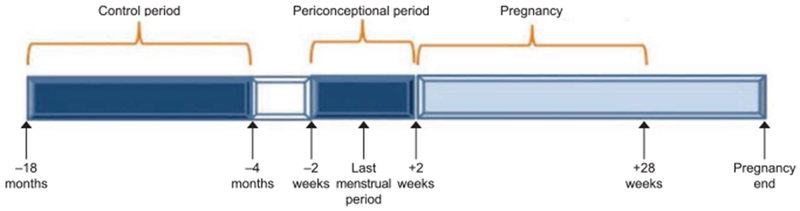
Exposure periods of interest for quadrivalent human papillomavirus vaccination: control period*, periconceptional period†, and during pregnancy‡. *Eighteen months to 4 months before last menstrual period. †Two weeks before to 2 weeks after last menstrual period. ‡Two weeks to 28 weeks of gestation.
The adverse birth outcomes examined were small for gestational age (SGA) and preterm birth. Preterm birth was defined as delivery before 37 weeks of gestation and was based on a clinician’s estimate recorded in the electronic health record or state birth records. Birth weights also came from the electronic health record or state birth records. Weight for gestational age percentiles was assigned based on reference values derived by Oken et al19 with a cutoff of less than the 10th percentile used to classify a birth as SGA.
Adverse obstetric outcomes examined were chorioamnionitis, hypertensive disorders of pregnancy, and gestational diabetes. These obstetric outcomes were chosen because they are both common and important markers of maternal health and also represent maternal risks for preterm birth. All potential adverse obstetric events were identified from International Classification of Diseases, 9th Revision (ICD-9) codes recorded in maternal electronic health records. Specific definitions have been used in our prior maternal vaccine safety assessments.16 Chorioamnionitis (ICD-9 658.4) was limited to inpatient diagnoses occurring at the time of birth. Hypertensive disorders, specifically gestational hypertension, and preeclampsia or eclampsia (ICD-9 642.3–642.7, 642.9) were required to have onset at 20 weeks of gestation or later and after the 4vHPV receipt date. Gestational hypertension and preeclampsia without severe features were required to have at least two outpatient diagnoses or one inpatient diagnosis. Severe preeclampsia or eclampsia was only included if diagnosed at an inpatient or emergency department visit. Gestational diabetes (ICD-9 648.8) was included if diagnosed after 20 weeks of gestation and after the vaccine was given.
We also examined risk for selected major structural birth defects diagnosed up to 12 months of life, which would be expected to affect infant health, survival, or long-term function. This list includes more than 50 birth defects included in the National Birth Defects Prevention Study and the European Surveillance of Congenital Anomalies20,21 and was adapted based on expert consensus and validity of their ICD-9 codes. As previously described, to increase specificity for identifying birth defects, using an iterative process, outcome-specific algorithms were developed.22 These birth defect outcomes have been applied in prior maternal vaccine safety evaluation from our group.23 Maternal demographic and pregnancy characteristics were examined as potential confounders (Table 1). We examined for socioeconomic status using proxies at the census tract level for each woman, defined as the percent of families within their census tract with income below 150% of the federal poverty level. Missing census data were imputed using the expectation maximization algorithm.24
Table 1.
Baseline Demographics and Clinical Data for Pregnant Women With Live Births, Vaccine Safety Datalink, 2007–2013, Who Received Quadrivalent Human Papillomavirus Vaccine During Pregnancy, the Periconceptional Period, or the Comparison Period
| Quadrivalent HPV Vaccine |
|||
|---|---|---|---|
| Maternal or Pregnancy Characteristics | During the Periconceptional Period (n=720) | During Pregnancy (n = 638) | During the Comparison Period (n=8,196) |
| Age at delivery* (y) | |||
| 13–14 | 3 (0.4) | 5 (0.8) | 20 (0.2) |
| 15–19 | 231 (32.1) | 256 (40.1) | 2,719 (33.2) |
| 20–24 | 261 (36.3) | 224 (35.1) | 2,900 (35.4) |
| 25–27 | 225 (31.3) | 153 (24.0) | 2,557 (31.2) |
| Race–ethnicity | |||
| Asian, non-Hispanic | 36 (5.0) | 23 (3.6) | 413 (5.0) |
| Black, non-Hispanic | 92 (12.8) | 99 (15.5) | 990 (12.1) |
| Hispanic | 323 (44.9) | 290 (45.5) | 3,650 (44.5) |
| Other | 67 (9.3) | 62 (9.7) | 743 (9.1) |
| White, non-Hispanic | 202 (28.1) | 164 (25.7) | 2,400 (29.3) |
| Year of delivery* | |||
| 2007 | 24 (3.3) | 29 (4.5) | 6 (0.1) |
| 2008 | 68 (9.4) | 83 (13.0) | 459 (5.6) |
| 2009 | 202 (28.1) | 176 (27.6) | 1,520 (18.5) |
| 2010 | 150 (20.8) | 101 (15.8) | 2,254 (27.5) |
| 2011 | 65 (9.0) | 70 (11.0) | 1,678 (20.5) |
| 2012 | 116 (16.1) | 101 (15.8) | 1,325 (16.2) |
| 2013 | 95 (13.2) | 78 (12.2) | 954 (11.6) |
| Medical care in 1st trimester | 662 (91.9) | 591 (92.6) | 7,460 (91.0) |
| Prenatal care index | |||
| Adequate or plus | 570 (79.2) | 478 (74.9) | 6,299 (76.9) |
| Intermediate | 110 (15.3) | 120 (18.8) | 1,378 (16.8) |
| Inadequate | 40 (5.6) | 40 (6.3) | 519 (6.3) |
| Hospitalizations before 20 wk of gestation | 99 (13.8) | 94 (14.7) | 1,172 (14.3) |
| No. of HPV doses including current* | |||
| 1 | 314 (43.6) | 273 (42.8) | 3,051 (37.2) |
| 2 | 231 (32.1) | 191 (29.9) | 2,412 (29.4) |
| 3 or more | 175 (24.3) | 174 (27.3) | 2,733 (33.3) |
| Received another vaccine during pregnancy*† | 522 (72.5) | 452 (70.8) | 5,476 (66.8) |
| Pre-existing comorbidities‡ | 154 (21.4) | 138 (21.6) | 1,642 (20.0) |
| Poverty§ | 21.9 (3.6) | 21.1 (3.8) | 21.9 (3.6) |
HPV, human papillomavirus.
Data are n (%).
P<.001.
Other vaccines administered during pregnancy included: inactivated influenza vaccines (69.8%);tetanus, diphtheria, pertussis (29.7%); other (1.5%).
Diagnoses at inpatient, outpatient or emergency department visits, from 6 months before pregnancy start up through the end of the pregnancy for hypertension, pulmonary, pregestational diabetes, heart disease, and renal complications.
Percentage of families in census tract whose income is below 150% of the federal poverty level.
Descriptive statistics were used to compare baseline demographic variables, comorbidities, and health care utilization variables among the three cohort groups. We performed three propensity score analyses using logistic regression to estimate the odds of receiving 4vHPV during the exposure periods of interest compared with receipt of 4vHPV before these exposure periods: 1) the periconceptional period compared with the comparison period, 2) during pregnancy compared with the comparison period, and 3) the periconceptional period or during pregnancy compared with the comparison period. The propensity scores included the following variables: maternal age at delivery, year of delivery, Kotelchuck Adequacy of prenatal care utilization index, preexisting comorbidities, mean census tract poverty level, and Vaccine Safety Datalink site.
A generalized linear model with Poisson distribution with robust variance and log link was used to obtain adjusted risk ratios and adjusted prevalence ratios with 95% CIs. Similarly, a generalized linear model with Poisson distribution with identity link was used to obtain adjusted risk differences and adjusted prevalence differences. The propensity score was added in the models parameterized as quintiles. Given the available sample of women who received 4vHPV during the periconceptional period or during pregnancy, with α=0.05 and using a two-sided test, the study was powered a priori to detect a risk ratio of 1.7 (1.9 rate difference) for outcomes with a background rate of 2 per 100. All analyses were conducted using SAS 9.4. This study was approved by the institutional review boards at all participating Vaccine Safety Datalink sites and the Centers for Disease Control and Prevention.
RESULTS
From January 1, 2007, through September 1, 2013, in the seven Vaccine Safety Datalink sites, there were 114,367 pregnancies ending in a live birth among women age 13–27 years with continuous insurance enrollment (Fig. 1). Among eligible pregnancies, 720 (0.8%) received 4vHPV during the periconceptional period, 638 (0.7%) received 4vHPV during pregnancy (2–28 weeks after their last menstrual period), and 8,196 received one or more doses of 4vHPV between 4 and 18 months before their last menstrual period and had no further doses during the periconceptional period or during pregnancy (comparison group) (Fig. 1).
Forty percent of those who received 4vHPV during pregnancy were 20 years old or younger compared with 32% who received 4vHPV during the periconceptional period and 33% of those vaccinated in the comparison period (P<.001; Table 1). The remaining baseline characteristics, including maternal race–ethnicity, poverty, prenatal care in the first trimester, hospitalization before 28 weeks of gestation, and maternal comorbidities, did not differ significantly between groups.
The total number of 4vHPV doses received differed between the exposed and comparison groups (P<.01). Vaccination in the comparison period was more likely to be the third recorded 4vHPV dose. Sixty-six percent of the comparison group received other vaccines at the same time as 4vHPV compared with 70.8% of women who received 4vHPV during the periconceptional period and 72.5% who received 4vHPV during pregnancy. Most women received only a single 4vHPV dose during pregnancy. However, 20 women received two doses and one received three 4vHPV doses during pregnancy.
Among women who received 4vHPV in one or both exposure time periods compared with those who received 4vHPV in the comparison period, 4–18 months before their last menstrual period, there was no increased risk of chorioamnionitis, hypertension of pregnancy, or gestational diabetes (Tables 2–4). Receipt of 4vHPV in one or both exposure periods was also not associated with increased risk for preterm or SGA births. Specifically, the occurrence of preterm birth was 7.4% among women receiving 4vHPV during the periconceptional period, 7.9% among those receiving the vaccine during pregnancy, compared with 7.6% among women receiving the vaccine 4–18 months before their last menstrual period. Among women receiving 4vHPV during the periconceptional period or during pregnancy or during either exposure period, rates for SGA were 11.8%, 11.7%, and 11.6%, respectively, as compared with 11.1% among women receiving 4vHPV in the comparison period (Tables 2–4).
Table 2.
Frequency of Selected Adverse Maternal and Infant Outcomes and Adjusted Relative Risks for Receipt of Quadrivalent Human Papillomavirus Vaccine During the Periconceptional and Comparison Periods, Vaccine Safety Datalink, 2007–2013
| Quadrivalent HPV Vaccine |
||||
|---|---|---|---|---|
| Outcome | During the Periconceptional Period (n=720) | During the Comparison Period (n=8,196) | Adjusted RR* (95% CI) | Adjusted Risk Difference/100 Live Births (95% CI) |
| Chorioamnionitis | 54 (7.5) | 595 (7.3) | 1.06 (0.80–1.4) | 0.3 (−1.7 to 2.4) |
| Hypertensive disorders | 51 (7.1) | 671 (8.2) | 0.86 (0.65–1.15) | −1.2 (−3.2 to 0.8) |
| Gestational diabetes | 37 (5.2) | 396 (4.9) | 1.02 (0.73–1.4) | 0.1 (−1.6 to 1.8) |
| Preterm delivery (less than 37 wk of gestation) | 53 (7.4) | 616 (7.6) | 0.92 (0.69–1.22) | −0.6 (−2.6 to 1.4) |
| SGA, less than the 10th percentile | 84 (11.8) | 902 (11.1) | 1.05 (0.84–1.3) | 0.7 (−1.8 to 0.3) |
HPV, human papillomavirus; RR, relative risk; SGA, small for gestational age.
Data are n (%) unless otherwise specified.
Propensity-adjusted, quintiles of propensity score included in the model parameterized as a five-category variable. Variables included in the model were site, maternal age, year of delivery, prenatal care index, poverty, pre-existing maternal conditions.
Table 4.
Frequency of Selected Adverse Maternal and Infant Outcomes and Adjusted Relative Risks for Receipt of Quadrivalent Human Papillomavirus Vaccine During the Periconceptional Period or Pregnancy and the Comparison Period, Vaccine Safety Datalink, 2007–2013
| Quadrivalent HPV Vaccine |
||||
|---|---|---|---|---|
| Outcome | Periconceptional Period or During Pregnancy (n=1,358) | During Comparison Period (n=8,196) | Adjusted RR* (95% CI) | Adjusted Risk Difference/100 Live Births (95% CI) |
| Chorioamnionitis | 100 (7.3) | 595 (7.3) | 1.05 (0.85–1.3) | 0.3 (−1.3 to 1.8) |
| Hypertensive disorders | 106 (7.8) | 671 (8.2) | 0.95 (0.77–1.2) | −0.4 (−2.0 to 1.2) |
| Gestational diabetes | 67 (4.9) | 396 (4.9) | 1.0 (0.77–1.3) | 0.2 (−1.1 to 1.5) |
| Preterm delivery (less than 37 wk of gestation) | 103 (7.6) | 616 (7.6) | 0.97 (0.79–1.2) | −0.3 (−1.8 to 1.3) |
| SGA, less than the 10th percentile | 158 (11.6) | 902 (11.1) | 1.04 (0.88–1.3) | 0.6 (−1.3 to 2.5) |
HPV, human papillomavirus; RR, relative risk; SGA, small for gestational age.
Data are n (%) unless otherwise specified.
Propensity-adjusted, quintiles of propensity score included in the model parameterized as a five-category variable. Variables included in the model were site, maternal age, year of delivery, prenatal care index, poverty, pre-existing maternal conditions.
When examining risks for major structural birth defects, 1,192 (12%) of the infants in the full study cohort did not meet the minimum enrollment criteria, 166 (less than 1%) were excluded for maternal use of teratogenic medications in pregnancy, 108 (less than 1%) were identified as potentially exposed to maternal congenital infections during pregnancy, and 10 (less than 1%) had chromosomal abnormalities. The analyses of major structural birth defects included 601 infants whose mothers received 4vHPV during the periconceptional period, 542 whose mothers received 4vHPV during pregnancy, and 6,483 whose mothers received one or more doses of 4vHPV in the comparison period (Table 5).
Table 5.
Frequency of Major Birth Defects and Adjusted Relative Risks for Receipt of Quadrivalent Human Papillomavirus Vaccine During the Periconceptional Period, During Pregnancy, or Both Exposure Periods Compared With Receipt of the Quadrivalent Human Papillomavirus Vaccine During the Comparison Period, Vaccine Safety Datalink, 2007–2013
| Quadrivalent HPV Vaccine | No. of Live Births | Major Birth Defects | Adjusted Prevalence Ratio* (95% CI) | Adjusted Prevalence Difference/10,000 Live Births (95% CI) |
|---|---|---|---|---|
| During periconceptional period | 601† | 11 (1.8) | 1.04 (0.75–1.5) | 0.3 (−1.7 to 2.4) |
| During pregnancy | 542 | 11 (2.0) | 1.0 (0.52–1.9) | 0.1 (−1.2 to 1.4) |
| During periconceptional period or during pregnancy | 1,143 | 22 (1.9) | 1.04 (0.66–1.7) | 0.2 (−0.7 to 1.1) |
| During comparison period | 6,843† | 120 (1.8) | Referent | Referent |
HPV, human papillomavirus.
Data are n (%) unless otherwise specified.
Propensity-adjusted, quintiles of propensity score included in the model parameterized as a five-category variable. Variables included in the model were site, year of delivery, maternal age, prenatal care index, poverty, pre-existing maternal conditions.
For major birth defects analyses, we excluded infants with less than 4 months’ insurance enrollment, no outpatient visits at a Vaccine Safety Datalink site, maternal use of teratogenic medication during pregnancy or within 6 months of last menstrual period, maternal congenital infections (toxoplasmosis, syphilis, varicella, rubella, and cytomegalovirus), pre-existing maternal diabetes.
There was no difference in the occurrence of selected major structural birth defects between the 4vHPV exposure groups (Table 5). The occurrence of these defects is also similar to their expected background rate in our Vaccine Safety Datalink population (Table 6).22 Of note, only one infant in our study was diagnosed with two birth defects among women who received 4vHPV during the periconceptional period or pregnancy (microcephalus and hypospadias). By comparison, 12 infants were identified with a diagnosis of two or more birth defects among mothers in the comparison group (data not shown).
Table 6.
List of Major Birth Defects Among Women Receiving Quadrivalent Human Papillomavirus Vaccination During Pregnancy, the Periconceptional Period, and the Comparison Period, Vaccine Safety Datalink, 2007–2013
| Quadrivalent HPV Vaccine |
|||
|---|---|---|---|
| Major Birth Defect | Periconceptional Period (n=601) | Pregnancy (n=542) | Comparison Period (n=6,943) |
| Gastroschisis or omphalocele | 1 | 1 | 11 |
| Diaphragmatic hernia | 1 | 0 | 1 |
| Cleft lip or cleft palate | 1 | 2 | 9 |
| Spina bifida | 1 | 0 | 1 |
| Holoprosencephaly | 1 | 0 | 3 |
| Esophageal atresia±tracheoesophageal fistula | 1 | 0 | 2 |
| Congenital hydronephrosis | 1 | 3 | 26 |
| Ear defect | 0 | 1 | 3 |
| Microcephalus | 0 | 1 | 5 |
| Limb deficiency | 0 | 0 | 1 |
| Sacral agenesis | 0 | 0 | 1 |
| Encephalocele, cranial meningocele, encephalomyelocele | 0 | 0 | 2 |
| Intestinal atresia or stenosis | 0 | 0 | 6 |
| Pyloric stenosis | 0 | 0 | 9 |
| Hypospadias—second- or third-degree | 0 | 1 | 2 |
| Renal agenesis or hypoplasia | 0 | 0 | 1 |
| Severe cardiac defects | 1 | 0 | 10 |
| Other cardiac defects | 3 | 2 | 39 |
HPV, human papillomavirus.
DISCUSSION
In this large, multisite observational cohort, inadvertent administration of 4vHPV during the periconceptional period or during pregnancy was not associated with increased risks of choriamnionitis, preterm birth, SGA birth, or selected major structural birth defects. Administration of 4vHPV during the periconceptional period or before 20 weeks of gestation was also not associated with hypertensive disorders of pregnancy or gestational diabetes.
Prior data on 4vHPV during pregnancy have been reassuring but limited. One large observational study using the Denmark Medical Birth Register evaluated exposures to 4vHPV and major birth defects, spontaneous abortion, preterm birth, and SGA and found no association.10 Our exposure windows for vaccination differed from the Danish cohort. In addition, we evaluated outcomes not included in the Danish study such as gestational diabetes, chorioamnionitis, and gestational hypertension. In the 4vHPV clinical trials, participants had pregnancy testing immediately before vaccination, and women were not vaccinated if positive.9 Information on adverse pregnancy outcomes for exposed trial participants was limited.8 Documentation on timing of vaccine exposure was unclear, and no adjustment was made for factors that may influence adverse pregnancy outcomes.8
A review of 147 nonmanufacturer reports to the Vaccine Adverse Event Reporting System of pregnant women who received 4vHPV during June 2006 through December 2013 found no unexpected patterns in maternal or fetal outcomes. The most frequent adverse events reported were spontaneous abortion, elective termination of pregnancy, and maternal fever. There were two reports of major birth defects, one lower limb defect and one cardiac defect.25
Across all phase III trials, there were 70 identified infants or fetuses with one or more major birth defects (40 among vaccinated women and 30 in the placebo groups). The types of defects observed were diverse and consistent with those generally observed in a population of young pregnant women. We also observed major structural birth defects to occur among women exposed to 4vHPV during pregnancy at rates consistent with background rates in our Vaccine Safety Datalink population,22 although we had limited power to evaluate specific birth defects.8,26
Although pregnancy tests were not routinely performed before 4vHPV administration, among 92,579 women with eligible live births during our study period, few received the vaccine during the periconceptional period or during pregnancy, 720 (0.8%) and 638 (0.7%), respectively. In addition, few pregnancies occurred in adolescents younger than 15 years (less than 0.05%). Given the increasing efforts to target vaccination at the recommended ages of 11–12 years and with the transition to a two-dose schedule, concerns regarding inadvertent HPV vaccination during pregnancy may be further reduced.27
Our study was limited to continuously insured women with live births; results may differ in a population at higher risk for adverse pregnancy or birth outcomes. We were unable to assess the risks for spontaneous abortion or stillbirth after 4vHPV exposures in this study. We were also not able to evaluate those who may have terminated a pregnancy. Spontaneous abortion and stillbirths are the focus of an ongoing study by our group, as part of the Vaccine Safety Datalink, with individual adjudication of cases after chart review. We were also limited by incomplete capture of prior vaccinations. Vaccines administered before the period of required continuous enrollment, more than 6 months before their last menstrual period, may have been missed. Finally, although our point estimates are all close to 1.0, given our sample size, we cannot rule out small increases in risks for rare outcomes after inadvertent 4vHPV exposures.
In this cohort of insured adolescents and young adults, inadvertent vaccination with 4vHPV during the periconceptional period or during pregnancy was not associated with selected adverse maternal or infant outcomes compared with vaccination 4–18 months before pregnancy. This study provides needed data for clinicians and expectant mothers on the relative safety of 4vHPV when inadvertently administered in pregnancy.
Table 3.
Frequency of Selected Adverse Maternal and Infant Outcomes and Adjusted Relative Risks for Receipt of Quadrivalent Human Papillomavirus Vaccine During Pregnancy and the Comparison Period, Vaccine Safety Datalink, 2007–2013
| Quadrivalent HPV Vaccine |
||||
|---|---|---|---|---|
| Outcome | During Pregnancy (n=638) | During Comparison Period (n=8,196) | Adjusted RR* (95% CI) | Adjusted Risk Difference/100 Live Births (95% CI) |
| Chorioamnionitis | 46 (7.2) | 595 (7.3) | 0.95 (0.70–1.3) | −0.3 (−2.4 to 1.8) |
| Hypertensive disorders | 55 (8.7) | 671 (8.2) | 1.04 (0.79–1.4) | 0.4 (−1.9 to 2.7) |
| Gestational diabetes | 30 (4.7) | 396 (4.9) | 0.98 (0.67–1.4) | 0.2 (−1.7 to 2.1) |
| Preterm delivery (less than 37 wk of gestation) | 50 (7.9) | 616 (7.6) | 0.97 (0.72–1.3) | −0.3 (−2.5 to 1.9) |
| SGA, less than the 10th percentile | 74 (11.7) | 902 (11.1) | 1.04 (0.82–1.3) | 0.4 (−2.3 to 3.0) |
HPV, human papillomavirus; RR, relative risk; SGA, small for gestational age.
Data are n (%) unless otherwise specified.
Propensity-adjusted, quintiles of propensity score included in the model parameterized as a five-category variable. Variables included in the model were site, maternal age, year of delivery, prenatal care index, poverty, pre-existing maternal conditions.
Acknowledgments
Supported by the Centers for Disease Control and Prevention, Contract 200-2012-53526. Findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors thank Beth Molitor, MBA, Leslie Kuckler, MPH, and James Donahue DVM, PhD, MPH, for their assistance with data collection and interpretation of data.
Each author has indicated that he or she has met the journal’s requirements for authorship.
Financial Disclosure
Dr. Naleway has received research support from Merck, Medimmune, and Pfizer. Dr. Klein has received research support from GlaxoSmithKline, Sanofi Pasteur, Merck & CO, Pfizer, Medimmune, Novartis (now GlaxoSmithKline), and Protein Science. Dr. Hechter has received research support from GlaxoSmithKline. Dr. Jackson has received research support from Sanofi Pasteur. The other authors did not report any potential conflicts of interest.
Footnotes
Presented at the 37th Annual Society for Maternal-Fetal Medicine Pregnancy Meeting, January 26–28, 2017, Las Vegas, Nevada.
REFERENCES
- 1.Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis 2013;40:187–93. [DOI] [PubMed] [Google Scholar]
- 2.Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998;338:423–8. [DOI] [PubMed] [Google Scholar]
- 3.Smith LM, Strumpf EC, Kaufman JS, Lofters A, Schwandt M, Levesque LE. The early benefits of human papillomavirus vaccination on cervical dysplasia and anogenital warts. Pediatrics 2015;135:e1131–40. [DOI] [PubMed] [Google Scholar]
- 4.Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER, et al. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2007;56:1–24. [PubMed] [Google Scholar]
- 5.Petrosky E, Bocchini JA Jr, Hariri S, Chesson H, Curtis CR, Saraiya M, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep 2015;64:300–4. [PMC free article] [PubMed] [Google Scholar]
- 6.Hamilton BE, Martin JA, Osterman MJ, Curtin SC, Mathews TJ. Births: final data for 2014. Natl Vital Stat Rep 2015;64: 1–64. [PubMed] [Google Scholar]
- 7.Human papillomavirus vaccination. Committee Opinion No. 704. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;129:e173–8.28346275 [Google Scholar]
- 8.Goss MA, Lievano F, Buchanan KM, Seminack MM, Cunningham ML, Dana A. Final report on exposure during pregnancy from a pregnancy registry for quadrivalent human papillomavirus vaccine. Vaccine 2015;33:3422–8. [DOI] [PubMed] [Google Scholar]
- 9.Garland SM, Ault KA, Gall SA, Paavonen J, Sings HL, Ciprero KL, et al. Pregnancy and infant outcomes in the clinical trials of a human papillomavirus type 6/11/16/18 vaccine: a combined analysis of five randomized controlled trials. Obstet Gynecol 2009;114:1179–88. [DOI] [PubMed] [Google Scholar]
- 10.Scheller NM, Pasternak B, Molgaard-Nielsen D, Svanström H, Hviid A. Quadrivalent HPV vaccination and the risk of adverse pregnancy outcomes. N Engl J Med 2017;376:1223–1233. [DOI] [PubMed] [Google Scholar]
- 11.Baril L, Rosillon D, Willame C, Angelo MG, Zima J, van den Bosch JH, et al. Risk of spontaneous abortion and other pregnancy outcomes in 15-25 year old women exposed to human papillomavirus-16/18 AS04-adjuvanted vaccine in the United Kingdom. Vaccine 2015;33:6884–91. [DOI] [PubMed] [Google Scholar]
- 12.Baggs J, Gee J, Lewis E, Fowler G, Benson P, Lieu T, et al. The Vaccine Safety Datalink: a model for monitoring immunization safety. Pediatrics 2011;127(suppl 1):S45–53. [DOI] [PubMed] [Google Scholar]
- 13.Naleway AL, Gold R, Kurosky S, Riedlinger K, Henninger ML, Nordin JD, et al. Identifying pregnancy episodes, outcomes, and mother-infant pairs in the Vaccine Safety Datalink. Vaccine 2013;31:2898–903. [DOI] [PubMed] [Google Scholar]
- 14.Nordin JD, Kharbanda EO, Vazquez-Benitez G, Lipkind H, Lee GM, Naleway AL. Monovalent H1N1 influenza vaccine safety in pregnant women, risks for acute adverse events. Vaccine 2014;32:4985–92. [DOI] [PubMed] [Google Scholar]
- 15.Kharbanda EO, Vazquez-Benitez G, Lipkind HS, Klein NP, Cheetham TC, Naleway AL, et al. Maternal Tdap vaccination: coverage and acute safety outcomes in the vaccine safety datalink, 2007–2013. Vaccine 2016;34:968–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kharbanda EO, Vazquez-Benitez G, Lipkind HS, Klein NP, Cheetham TC, Naleway A, et al. Evaluation of the association of maternal pertussis vaccination with obstetric events and birth outcomes. JAMA 2014;312:1897–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kharbanda EO, Vazquez-Benitez G, Lipkind H, Naleway AL, Klein NP, Cheetham TC, et al. Receipt of pertussis vaccine during pregnancy across 7 Vaccine Safety Datalink sites. Prev Med 2014;67:316–9. [DOI] [PubMed] [Google Scholar]
- 18.Groom HC, Henninger ML, Smith N, Koppolu P, Cheetham TC, Glanz JM, et al. Influenza vaccination during pregnancy: influenza seasons 2002–2012, Vaccine Safety Datalink. Am J Prev Med 2016;50:480–8. [DOI] [PubMed] [Google Scholar]
- 19.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr 2003;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dolk H EUROCAT: 25 years of European surveillance of congenital anomalies. Arch Dis Child Fetal Neonatal Ed 2005;90:F355–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoon PW, Rasmussen SA, Lynberg MC, Moore CA, Anderka M, Carmichael SL, et al. The National Birth Defects Prevention Study. Public Health Rep 2001;116(suppl 1):32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kharbanda EO, Vazquez-Benitez G, Romitti PA, Naleway AL, Cheetham TC, Lipkind HS, et al. Identifying birth defects in automated data sources in the Vaccine Safety Datalink. Pharmacoepidemiol Drug Saf 2017;26:412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeSilva M, Vazquez-Benitez G, Nordin JD, Lipkind HS, Romitti PA, DeStefano F, et al. Tdap vaccination during pregnancy and microcephaly and other structural birth defects in offspring. JAMA 2016;316:1823–1825. [DOI] [PubMed] [Google Scholar]
- 24.Little R, Rubin DB. Statistical analysis with missing data. 2nd ed New York (NY): John Wiley; 2002. [Google Scholar]
- 25.Moro PL, Zheteyeva Y, Lewis P, Shi J, Yue X, Museru OI, et al. Safety of quadrivalent human papillomavirus vaccine (Gardasil) in pregnancy: adverse events among non-manufacturer reports in the Vaccine Adverse Event Reporting System, 2006–2013. Vaccine 2015;33:519–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Angelo MG, Zima J, Tavares Da Silva F, Baril L, Arellano F. Post-licensure safety surveillance for human papillomavirus-16/18-AS04-adjuvanted vaccine: more than 4 years of experience. Pharmacoepidemiol Drug Saf 2014;23:456–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cullen KA, Stokley S, Markowitz LE. Uptake of human papillomavirus vaccine among adolescent males and females: Immunization Information System sentinel sites, 2009–2012. Acad Pediatr 2014;14:497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]


