Abstract
Background:
Delirium in intensive care units (ICUs) is associated with long ICU stay, long hospital stay and increased costs of treatment. Unfortunately, delirium in ICU is significantly underestimated and overlooked by healthcare providers.
Aims:
The aim of this tudy is to determine the incidence and associated risk factors of delirium among critically ill patients in Saudi Arabia.
Methods:
This is a prospective study. Patients were assessed for delirium using the confusion assessment method for the ICU. Delirium was the independent variable in this study.
Results:
Fifty-nine patients (17.3%) showed positive delirium at least once compared to 283 patients (82.7%) who did not show positive delirium. Certain factors for delirium found to be significantly correlated with delirium (P < 0.005); including receiving sedation, mode of sedation, receiving mechanical ventilation, resistance to mechanical ventilator, and baseline Glasgow Coma Scale.
Conclusion:
Delirium occurred in >17% of our ICU patients. More efforts should be directed to consider ICU delirium and to minimize its triggering factors.
Keywords: Delirium, incidence, intensive care unit, risk factors
INTRODUCTION
The American Psychiatric Association's Diagnostic and Statistical Manual, 5th edition (DSM-5) defines delirium as a disturbance of consciousness characterized by acute onset and fluctuating course of inattention accompanied by either a change in cognition or a perceptual disturbance, so that a patient's ability to receive, process, store, and recall information is impaired.[1] A lot of intensive care unit (ICU) patients (30%–80%) are showing delirium at some point during their stay in ICU.[2,3,4,5,6,7] Delirium in ICU was found to be associated with longer ICU stay, longer hospital stay, and increased costs of treatment.[7,8,9,10] Unfortunately, delirium is significantly underestimated and overlooked by healthcare providers.[2,4,11] There are many validated tools that have been used to assess delirium in ICU. One of the most common recommend tools is the confusion assessment method for the ICU (CAM-ICU).[1,12,13,14] This tool can help healthcare providers to better estimate and diagnose delirium and recommended to be included in the routine daily assessment of ICU patient.[2,15] Several factors have been proven to be associated with the risk of delirium. Use of sedation and analgesics is linked to increased delirium.[10,16,17] After searching several research databases and to the best of our knowledge, there are only little data regarding delirium among critically ill patients in ICUs of Saudi Arabia and the middle east countries.
Aim of the study
The aim of this study is to determine the incidence and associated risk factors of delirium among critically ill patients in Saudi Arabia.
METHODS
This prospective study was carried out between March 2017 and March 2018. A total number of 494 ICU patients who had met the inclusive criteria were assessed independently for delirium by well-trained bedside nurses using valid delirium tool; the CAM-ICU is used as a validated screening tool for delirium.[1,13,14,15]
Inclusion criteria
All ICU patients after 24 h of admission to ICU, older than 14 years old were assessed for delirium using CAM-ICU tool. Exclusion criteria are patients with structural or metabolic neurological deficit (as identified by admission medical diagnosis), patients with unknown baseline mental status and patients who were found to be “Unable to Assess (UTA)” as defined by CAM-ICU, patients who had been readmitted to the ICU after participating in the trial were also excluded after readmission. Informed consent had been obtained from each patient guardian/relative. Study participants were observed for any incidence of delirium over 24 h on a daily basis for 1 week, any single observed delirium incidence was counted as positive delirium. Any repeated delirium incidence for the same patient during the same admission stay was not counted in study incidence.
For all study participants, delirium was the independent variable in this study; positive delirium or negative delirium as evidenced by CAM ICU tool, other factors included in data collection and considered as dependent variables included: patients demographics and variables (i.e., age, gender, admission diagnosis, any sedatives, sedation mode, sedation vacation opportunity, any assisted mechanical ventilation, resistance (asynchrony) to assisted mechanical ventilator, and discharge outcome. This is observational study, so no treatment or specific therapy was given to any patients who were found to have positive delirium. The decision to start any treatment was left for treating physician/s.
The study has been approved by the Institutional Review Board (IRB) (Reference number: H1R1-20-Apr17-01, IRB registration Number with KACST, KSA: H-01-R-053) and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All authors declare that there is no conflict of interest regarding the publication of this article.
Setting
The research was conducted in the ICU of King Saud Medical City which has 120-bed capacity and provides care for different categories of critically ill patients who need comprehensive stabilization. Averagely, 196 patients are admitted every month. Around 100 patients are receiving care in ICU every day, 50–60 patients on an average are connected to assisted mechanical ventilation (MV) and needs some amount of sedation based on the clinical decision.
Sampling technique
Cohort sampling technique was used for selecting the patients for the study. All newly admitted patients who had been admitted from the 1st day of the month (May–September 2018) and had met the inclusive criteria were recruited for the study.
Statistical analysis
The data were analyzed using SPSS version 22 (IBM Corp., Armonk, NY, USA), and the results are presented as descriptive statistics– frequency, percent, age, mean, standard deviation, and inferential statistics– Chi-square test, risk ratio (RR) with 95% confidence interval (CI), Student's– t-test for independent samples for α = 0.05 and 5% level of significance.
RESULTS AND DISCUSSION
We had observed 494 patients for this study and 342 patients (69.23%) were qualified for delirium assessment and found to have positive or negative delirium, compared to 152 patients (30.76%) who were not qualified (labeled as “UTA”) for delirium assessment as they had been deeply sedated, discharged, or died before completion of assessment. Figure 1 presents the Flow Chart of the study.
Figure 1.
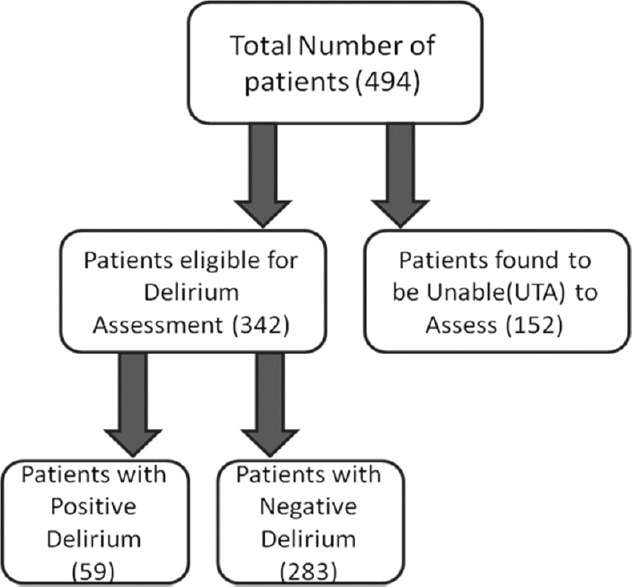
Flow chart for study subjects recruitment
The incidence of delirium in ICU was 17.3%. Of 342 patients who had been qualified for delirium assessment, 59 patients (17.3%) showed positive delirium at least once compared to 283 patients (82.7%) who did not show any single delirium incidence during the study period. Table 1 presents the association between observed delirium and other associated factors and Table 2 presents associated factors RRs.
Table 1.
Chi-square test of association for the factors and observation of delirium
| Characteristics | n (%) | Delirium observed n | Delirium not observed n | χ2, (P) |
|---|---|---|---|---|
| Gender | ||||
| Male | 264 (77.2) | 46 | 218 | 0.024 |
| Female | 78 (22.8) | 13 | 65 | (P=0.876) |
| Sedation | ||||
| Receiving Sedation | 75 (21.9) | 25 | 50 | 17.40 |
| Not Receiving Sedation | 267 (78.1) | 34 | 233 | (P˂0.001) |
| Mode of Sedation Administration (only for sedated patients) | ||||
| Infusion | 60 (80.0) | 19 | 41 | 20.09 |
| Intermittent | 5 (6.67) | 3 | 2 | (P˂0.001) |
| Mixed | 10 (13.33) | 3 | 7 | |
| Ventilated | ||||
| Yes | 119 (34.8) | 33 | 86 | 14.04 |
| No | 223 (65.2) | 26 | 197 | (P˂0.001) |
| Mechanical Ventilator (MV) Resistance | ||||
| Yes | 11 (3.2) | 6 | 5 | 20.14 |
| No | 108 (31.6) | 27 | 81 | (P˂0.001) |
| Not connected to MV | 223 (65.2) | 26 | 197 | |
| Discharge Outcome | ||||
| Alive | 317 (92.7) | 52 | 265 | 2.18 |
| Dead | 25 (7.3) | 7 | 28 | (P=0.140) |
*Statistically significant at 5% level
Table 2.
Risk Ratio of Significant associated factors with delirium observation
| Parameter | Number of patients | Risk ratio | 95%CI |
|---|---|---|---|
| Sedation - Received | 75 | 2.618* | 1.67-4.09 |
| Did not receive | 267 | 1 | --- |
| Mode of sedation - Infusion | 60 | 0.53 | 0.23-1.18 |
| Intermittent | 5 | 1 | --- |
| Patient on - Sedation Vacation | 43 | 2.10* | 1.17-3.79 |
| NOT on Sedation Vacation | 80 | 1 | --- |
| Patient - received assisted MV | 119 | 2.37* | 1.49-3.78 |
| Did not receive assisted MV | 223 | 1 | --- |
| Patient on assisted MV | |||
| Showed resistance to MVDid NOT show resistance to MV | 11 | 2.18* | 1.16-4.10 |
| Did NOT show resistance to MV | 108 | 1 | --- |
*Statistically significant
Sedation and delirium
Data analysis has shown a strong statistically significant association between delirium and sedation; the patient has sedation started in ICU during the study period or not, Chi-square = 17.405 (P = <0.001). RR analysis has shown that patients who received sedation (n = 75, 21.9%) had 2.61 times the risk of developing delirium compared to patients who did not receive any sedation during stay in ICU (n = 267, 78.1%). RR 2.618; 95% CI 1.67–4.09, P = <0.001). This result is consistent with other studies findings in the reviewed literature. Ouimet et al. observed that the use of sedation was significantly associated with delirium; (odds ratio [OR] = 3.2, 95% CI = 1.5–6.8).[10] Pandharipande et al. had defined that midazolam (OR 2.75, CI 1.43–5.26, P = 0.002) exposure as the strongest independent risk factor for transitioning to delirium among surgical ICU (SICU) and trauma ICU (TICU) patients.[16] Another study conducted by Pandharipande et al. concluded that patients treated with lorazepam on a given ICU day are more likely to be delirious on the following day than if lorazepam were not administered; (OR = 1.2, 95% CI = 1.2–1.4).[18] Pisani et al. concluded that receipt of a benzodiazepine or opioid (RR = 1.64, 95% CI = 1.27–2.10) was associated with increased delirium duration in medical intensive care.[17] Vasilevskis et al. had concluded in their study, that among a large number of risk factors discovered, administration of potent sedative medications, most notably benzodiazepines, is most consistently and strongly associated with an increased burden of delirium.[19]
Mode of sedation and delirium
Sedation can be started as a continuous infusion or as intermittent dosages. Schulingkamp et al. had found no difference in the incidence of delirium between patients who received sedation as continuous or as intermittent.[20] Junior and Park had investigated the association of sedation mode (continuous or intermittent) with delirium and found no differences between both groups (P = 0.472).[21] In our study for patients who received sedation, there was a strong statistically significant association between delirium incidence and mode of sedation (intermittent versus continuous) Chi-square = 20.090 (P = <0.001).
RR analysis has shown that patients who received sedation as “infusion mode”(n = 60, 80%) had a 47% reduction in risk of developing delirium compared to patients who received sedation as “intermittent mode” (n = 5, 6.7%) dosages during length of stay in ICU; RR = 0.53,95% CI 10.23–1.18, P = <0.001). Svenningsen et al. had investigated the impact of fluctuating sedation levels on the incidence of delirium in ICU and found that continuous infusion of sedatives (midazolam) was associated with a decrease in delirium incidence (OR: 0.38; P = 0.002).[22]
Daily sedation interruption and delirium
Holding sedation on a daily basis to assess neurological status (daily sedation interruption [DSI]) is a common practice for sedated patients that can reduce sedation.[23,24,25] Our data analysis showed no statistically significant association between delirium and DSI (P = 0.412). Many other studies had shown similar finding; no significant association between DSI and delirium.[26,27,28]
Assisted mechanical ventilation and delirium
Out of the 342 qualified patients for delirium assessment, 119 patients (34.80%) received assisted MV during the study period compared to 223 (65.20%) patients who did not receive any assisted MV during the study period. Many studies had found a strong association between the incidence of delirium and ventilation time.[29,30] Studies had shown that the prevalence of delirium is reaching 80% among ventilated patients in medical, surgical, and TICUs.[31] Data analysis in this study showed a strong statistically significant association between delirium and assisted MV (i.e., the patient received assisted MV during the study period); Chi-square = 14.04 (P = <0.001). RR analysis has shown that patients who received assisted MV (n = 119, 34.8%) had 2.37 times the risk of developing delirium compared to patients who did not receive assisted MV (n = 223, 65.2%) during stay in ICU. RR = 2.37, 95% CI 1.49–3.78, P = <0.001).
Patients who are MV may experience unpleasant effects as a result of asynchrony in breathing, some ventilator settings, distress from ventilator devices and tubes, difficult communication with others while ventilated.[32,33] Patient-ventilator dyssynchrony (PVD) is defined as ineffective patient triggering, double-triggering, short-cycle breaths, and long-cycle breaths.[34] It suggests a faulty interaction between the patient and ventilator that is commonly managed by sedation and advanced ventilator modes and adjustments.[35] PVD can be identified by direct observation of “patient fight with ventilator” as described by nurses or by detecting changes in the pressure/flow waveform as described by respiratory therapists.[35] In this study, we had found that of 119 patients connected to ventilator, only 11 patients (9.24%) had shown resistance (asynchrony) to MV. Analysis has shown a strong statistically significant association and resistance to MV; Chi-square = 20.14 (P = <0.001). RR analysis has shown that patients who showed resistance/asynchrony to MV (n = 11, 3.2%) had 2.18 times the risk of developing delirium compared to patients who did not show any resistance/asynchrony to MV (n = 108, 31.6%) during stay in ICU. RR = 2.18, 95% CI = 1.16–4.10, P = <0.001).
Baseline level of consciousness and delirium
Glasgow Coma Scale (GCS) has been used to measure the level of consciousness for patients, especially those with brain injury.[36,37] Data analysis has shown a strong statistically significant association between delirium incidence and baseline GCS. Chi-square = 72.69 (P = <0.001). Figure 2 presents the frequency distribution of patients eligible for delirium assessment (n = 342) and their baseline GCS score. In one study investigated delirium among 115 trauma patients admitted to the SICU, GCS Score <15 on admission was found to be one of the positive predictors of delirium.[38] Another study investigated traumatic brain injury patients in the neurosurgical ward, concluded that those with low GCS score on admission in the emergency department were more likely to have delirium in the first 4 days after admission.[39]
Figure 2.
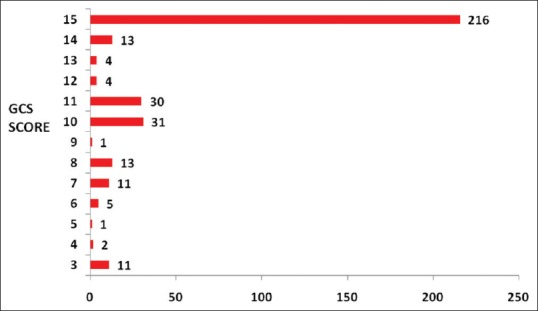
The baseline Glasgow Coma Scale of eligible patients (n = 342)
Other factors and delirium
Data analysis showed no statistically significant association between delirium incidence and ICU admitting diagnosis, age, gender, and discharge outcome; (P = 0.95, 0.58, 0.88, and 0.14, respectively). Chi-square = 2.183 (P = 0.140). Ely et al. had investigated 275 MV patients and found similar findings; no significant difference in age and admission diagnosis between group of patients with delirium and group of patients without delirium.[6] Aldemir et al. had investigated the predisposing factors for delirium for 818 patients in a SICU; in their findings, there was no significant correlation between delirium and age, gender, and admission diagnosis.[40] On the other hand, Zaal et al. had included 33 studies in their systematic review of risk factors for delirium in the ICU. Among findings, age and admission diagnosis/status were strong risk factors for delirium in >70% of studies included but not gender.[41] Mattar et al. had reviewed 22 published articles about delirium predisposing factors in ICUs (medical, surgical, or cardiac) from 1990 to 2012; they concluded that old age is a common risk factor for delirium in critically ill adult patients.[42]
CONCLUSION
Despite methodological limitations, delirium occurred in >17% of our ICU patients populations. Certain factors for delirium have been found to be significantly correlated with delirium (P < 0.005). These factors include receiving sedation, mode of sedation, receiving MV, resistance to MV, and baseline GCS score. Other factors found to be not significantly contributed to developing of delirium among studied populations, including age, gender, admission diagnosis, and discharge outcome. Given the fact that delirium is extremely overlooked syndrome in ICUs of the Middle East and Saudi Arabia; additional studies are necessary to investigate delirium and its associated factors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Diagnostic And Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Spronk PE, Riekerk B, Hofhuis J, Rommes JH. Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med. 2009;35:1276–80. doi: 10.1007/s00134-009-1466-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dubois MJ, Bergeron N, Dumont M, Dial S, Skrobik Y. Delirium in an intensive care unit: A study of risk factors. Intensive Care Med. 2001;27:1297–304. doi: 10.1007/s001340101017. [DOI] [PubMed] [Google Scholar]
- 4.Roberts B, Rickard CM, Rajbhandari D, Turner G, Clarke J, Hill D, et al. Multicentre study of delirium in ICU patients using a simple screening tool. Aust Crit Care. 2005;18:6, 8. doi: 10.1016/s1036-7314(05)80019-0. [DOI] [PubMed] [Google Scholar]
- 5.Roberts B. Screening for delirium in an adult intensive care unit. Intensive Crit Care Nurs. 2004;20:206–13. doi: 10.1016/j.iccn.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–62. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 7.Thomason JW, Shintani A, Peterson JF, Pun BT, Jackson JC, Ely EW, et al. intensive care unit delirium is an independent predictor of longer hospital stay: A prospective analysis of 261 non-ventilated patients. Crit Care. 2005;9:R375–81. doi: 10.1186/cc3729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Milbrandt EB, Deppen S, Harrison PL, Shintani AK, Speroff T, Stiles RA, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. 2004;32:955–62. doi: 10.1097/01.ccm.0000119429.16055.92. [DOI] [PubMed] [Google Scholar]
- 9.Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27:1892–900. doi: 10.1007/s00134-001-1132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007;33:66–73. doi: 10.1007/s00134-006-0399-8. [DOI] [PubMed] [Google Scholar]
- 11.van Eijk MM, van Marum RJ, Klijn IA, de Wit N, Kesecioglu J, Slooter AJ. Comparison of delirium assessment tools in a mixed intensive care unit. Crit Care Med. 2009;37:1881–5. doi: 10.1097/CCM.0b013e3181a00118. [DOI] [PubMed] [Google Scholar]
- 12.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: Validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–10. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 13.Devlin JW, Fong JJ, Schumaker G, O'Connor H, Ruthazer R, Garpestad E. Use of a validated delirium assessment tool improves the ability of physicians to identify delirium in medical intensive care unit patients. Crit Care Med. 2007;35:2721–4. doi: 10.1097/01.ccm.0000292011.93074.82. [DOI] [PubMed] [Google Scholar]
- 14.Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 15.Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest. 2007;132:624–36. doi: 10.1378/chest.06-1795. [DOI] [PubMed] [Google Scholar]
- 16.Pandharipande P, Cotton BA, Shintani A, Thompson J, Pun BT, Morris JA, Jr, et al. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008;65:34–41. doi: 10.1097/TA.0b013e31814b2c4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pisani MA, Murphy TE, Araujo KL, Slattum P, Van Ness PH, Inouye SK, et al. Benzodiazepine and opioid use and the duration of intensive care unit delirium in an older population. Crit Care Med. 2009;37:177–83. doi: 10.1097/CCM.0b013e318192fcf9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pandharipande P, Shintani A, Peterson J, Pun BT, Wilkinson GR, Dittus RS, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21–6. doi: 10.1097/00000542-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Vasilevskis EE, Han JH, Hughes CG, Ely EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012;26:277–87. doi: 10.1016/j.bpa.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schulingkamp D, Woo S, Nguyen A, Sich N, Shadis R. Assessment of continuous sedation versus intermittent sedation in mechanically ventilated patients. Crit Care Med. 2016;44:292. [Google Scholar]
- 21.Nassar Junior AP, Park M. Daily sedative interruption versus intermittent sedation in mechanically ventilated critically ill patients: A randomized trial. Ann Intensive Care. 2014;4:14. doi: 10.1186/2110-5820-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Svenningsen H, Egerod I, Videbech P, Christensen D, Frydenberg M, Tønnesen EK, et al. Fluctuations in sedation levels may contribute to delirium in ICU patients. Acta Anaesthesiol Scand. 2013;57:288–93. doi: 10.1111/aas.12048. [DOI] [PubMed] [Google Scholar]
- 23.Schweickert WD, Gehlbach BK, Pohlman AS, Hall JB, Kress JP. Daily interruption of sedative infusions and complications of critical illness in mechanically ventilated patients. Crit Care Med. 2004;32:1272–6. doi: 10.1097/01.ccm.0000127263.54807.79. [DOI] [PubMed] [Google Scholar]
- 24.O'Connor M, Bucknall T, Manias E. A critical review of daily sedation interruption in the intensive care unit. J Clin Nurs. 2009;18:1239–49. doi: 10.1111/j.1365-2702.2008.02513.x. [DOI] [PubMed] [Google Scholar]
- 25.Kress JP, Pohlman AS, O'Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000;342:1471–7. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- 26.Mehta S, Burry L, Cook D, Fergusson D, Steinberg M, Granton J, et al. Daily sedation interruption in mechanically ventilated critically ill patients cared for with a sedation protocol: A randomized controlled trial. JAMA. 2012;308:1985–92. doi: 10.1001/jama.2012.13872. [DOI] [PubMed] [Google Scholar]
- 27.Khan BA, Fadel WF, Tricker JL, Carlos WG, Farber MO, Hui SL, et al. Effectiveness of implementing a wake up and breathe program on sedation and delirium in the ICU. Crit Care Med. 2014;42:e791–5. doi: 10.1097/CCM.0000000000000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mehta S, Cook D, Devlin JW, Skrobik Y, Meade M, Fergusson D, et al. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults. Crit Care Med. 2015;43:557–66. doi: 10.1097/CCM.0000000000000727. [DOI] [PubMed] [Google Scholar]
- 29.Shehabi Y, Riker RR, Bokesch PM, Wisemandle W, Shintani A, Ely EW, et al. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Crit Care Med. 2010;38:2311–8. doi: 10.1097/CCM.0b013e3181f85759. [DOI] [PubMed] [Google Scholar]
- 30.Lat I, McMillian W, Taylor S, Janzen JM, Papadopoulos S, Korth L, et al. The impact of delirium on clinical outcomes in mechanically ventilated surgical and trauma patients. Crit Care Med. 2009;37:1898–905. doi: 10.1097/CCM.0b013e31819ffe38. [DOI] [PubMed] [Google Scholar]
- 31.Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, et al. Dexmedetomidine vs. midazolam for sedation of critically ill patients: A randomized trial. JAMA. 2009;301:489–99. doi: 10.1001/jama.2009.56. [DOI] [PubMed] [Google Scholar]
- 32.Weinhouse GL, Schwab RJ. Sleep in the critically ill patient. Sleep. 2006;29:707–16. doi: 10.1093/sleep/29.5.707. [DOI] [PubMed] [Google Scholar]
- 33.Bosma K, Ferreyra G, Ambrogio C, Pasero D, Mirabella L, Braghiroli A, et al. Patient-ventilator interaction and sleep in mechanically ventilated patients: Pressure support versus proportional assist ventilation. Crit Care Med. 2007;35:1048–54. doi: 10.1097/01.CCM.0000260055.64235.7C. [DOI] [PubMed] [Google Scholar]
- 34.Robinson BR, Blakeman TC, Toth P, Hanseman DJ, Mueller E, Branson RD, et al. Patient-ventilator asynchrony in a traumatically injured population. Respir Care. 2013;58:1847–55. doi: 10.4187/respcare.02237. [DOI] [PubMed] [Google Scholar]
- 35.Mellott KG, Grap MJ, Munro CL, Sessler CN, Wetzel PA. Patient-ventilator dyssynchrony: Clinical significance and implications for practice. Crit Care Nurse. 2009;29:41–55. doi: 10.4037/ccn2009612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jennett B, Teasdale G. Aspects of coma after severe head injury. Lancet. 1977;1:878–81. doi: 10.1016/s0140-6736(77)91201-6. [DOI] [PubMed] [Google Scholar]
- 37.Zuercher M, Ummenhofer W, Baltussen A, Walder B. The use of Glasgow coma scale in injury assessment: A critical review. Brain Inj. 2009;23:371–84. doi: 10.1080/02699050902926267. [DOI] [PubMed] [Google Scholar]
- 38.Bryczkowski SB, Lopreiato MC, Yonclas PP, Sacca JJ, Mosenthal AC. Risk factors for delirium in older trauma patients admitted to the surgical intensive care unit. J Trauma Acute Care Surg. 2014;77:944–51. doi: 10.1097/TA.0000000000000427. [DOI] [PubMed] [Google Scholar]
- 39.Maneewong J, Maneeton B, Maneeton N, Vaniyapong T, Traisathit P, Sricharoen N, et al. Delirium after a traumatic brain injury: Predictors and symptom patterns. Neuropsychiatr Dis Treat. 2017;13:459–65. doi: 10.2147/NDT.S128138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aldemir M, Ozen S, Kara IH, Sir A, Baç B. Predisposing factors for delirium in the surgical intensive care unit. Crit Care. 2001;5:265–70. doi: 10.1186/cc1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zaal IJ, Devlin JW, Peelen LM, Slooter AJ. A systematic review of risk factors for delirium in the ICU. Crit Care Med. 2015;43:40–7. doi: 10.1097/CCM.0000000000000625. [DOI] [PubMed] [Google Scholar]
- 42.Mattar I, Chan MF, Childs C. Risk factors for acute delirium in critically ill adult patients: A systematic review. ISRN Crit Care. 2013:1–10. doi: 10.11124/jbisrir-2012-3. [DOI] [PubMed] [Google Scholar]


