Abstract
Objective
To understand how real-time opioid prescribing cognitions by emergency medicine (EM) providers are influenced by review of the state prescription drug monitoring program (PDMP).
Methods
We collected prospective data from a convenience sample of 103 patient encounters for pain from 23 unique EM providers. After seeing the patient, before and immediately after reviewing the PDMP, EM providers answered how much they thought “the patient need[ed] an opioid to help manage their pain?”, how concerned they were “about drug abuse and/or diversion?”, and whether they planned to prescribe an opioid (yes/no). If they changed their decision to prescribe after querying the PDMP, they were asked to provide comments. We categorized encounters by opioid prescribing plan before/after PDMP review (e.g., O+/O− means plan changed from “yes” to “no”) and examined changes in cognitions across categories.
Results
Ninety-two of 103 (89.3%) encounters resulted in no change in opioid prescribing plan (61/92 [66.3%] O+/O+; 31/92 [33.7%] O−/O−). For the four O+/O− encounters, perceived patient opioid need decreased 75% of the time and concern for opioid abuse and/or diversion increased 75% of time. For the seven O−/O+ encounters, providers reported increased perceived patient opioid need 28.6% of the time and decreased concern for opioid abuse and/or diversion 14.3% of time.
Conclusions
PDMP data rarely alter plans to prescribe an opioid among emergency providers. When changes in opioid prescribing plan were made, this was reflected by changes in cognitions. Findings support the need for a properly powered study to identify how specific PDMP findings alter prescribing cognitions.
Keywords: Opioids, PDMP, Prescriptions, Substance Abuse
Prescription drug monitoring programs (PDMPs) are electronic databases maintained by individual states that can be accessed by care providers so that they can review a patient’s prior use of prescribed controlled substances. The anticipated effect was that providers would identify individuals with PDMP records of either frequent or undisclosed prescriptions, and thus decrease further opioid prescribing [1]. Despite this intent, studies to date have shown mixed effects of the PDMP on opioid prescribing by care providers [2]. Given these findings and the potential for unanticipated consequences of PDMP implementation on physician practice [3], it is important to clarify mechanisms by which the PDMP influences opioid prescribing [4].
In this study, we aim to understand how review of PDMP data influences real-time provider cognitions about perceived need for an opioid and concern for abuse and/or diversion as they relate to opioid prescribing plans. We focus on emergency medicine (EM) providers given that they frequently prescribe opioids to treat pain, often with very little historical data to inform assessment of patient risk for drug abuse and/or diversion [5]. We replicate and expand upon prior research showing that PDMP review by EM providers may result in either no changes [6] or higher rates of opioid prescribing [7] by examining the mechanisms through which cognitions are related to prescribing decisions. We hypothesized that among the encounters where the plan to prescribe an opioid changed, there would be concurrent changes in cognitions related to perceived need and concern for opioid abuse and/or diversion. Our preliminary findings could help inform why others have not found a definitive effect of the PDMP on opioid prescribing and could help design future interventions to aid providers in making safe opioid prescribing decisions.
Methods
Setting
The study was conducted at UPMC Mercy Hospital, a level I trauma and academic medical center in Pittsburgh, Pennsylvania. This ED had 62,222 visits for the year to date, ending on the final day of recruitment. During the period of recruitment, ED patients were 51.7% female, mean age was 44.5 years, 59% were white, 36% were black, and 5% reported other race. Insurance status included 31% medical assistance, 22% Medicare, 38% commercial insurance, and 9% self-pay. The most common chief complaints were abdominal pain, chest pain, and back pain. Also, during the period of recruitment, the percentage of patients with pain being prescribed an opioid at discharge from this ED was around 12% [8]. The study was approved by the Institutional Review Board at the University of Pittsburgh.
Participants and Procedures
Prior to study onset, verbal informed consent was obtained from EM attending physicians and midlevel providers (nurse practitioners and physician assistants) to study their cognitions and opioid prescribing plans. After consent was obtained, but prior to any patient encounters, EM providers filled out a baseline survey collecting measures of attitudes toward and comfort with communicating about opioids with patients. Between June 5 and August 11, 2017, on randomly selected days between 10 am to 10 pm, an investigator stationed in the Emergency Department identified patients with pain-related complaints seen by participating EM providers. If the EM provider indicated that the patient was in acute pain—they had reviewed the electronic medical record and seen the patient and decided that they were likely to be discharged to home—the provider was asked to answer four questions (pre-PDMP survey). Although we did not systematically record the number of times a provider refused to complete the survey, it is estimated that this occurred less than 10 times over the entire period of recruitment. We did not select specific subgroups of patients with pain-related complaints (e.g., back pain). The investigator then waited until the EM provider accessed and inspected the PDMP. Current state law requires all prescribing providers to query the PDMP and to document their query “each time a patient is prescribed an opioid drug product or benzodiazepine.” When indicated, providers opened a Web browser, navigated to the state PDMP website (https://pennsylvania.pmpaware.net/login), logged in with their credentials, and entered the patient name and birth date into the search fields. The website would then list all prescriptions for controlled substances filled at a pharmacy in Pennsylvania in the past 12 months. Immediately following review of the PDMP, to isolate the effect from other care-related data, the investigator again provided the post-PDMP survey, which contained identical questions to the pre-PDMP survey.
Measures
To understand enrolled EM provider attitudes and comfort when treating patients who have pain but who have a concerning history for opioid abuse and/or diversion, we collected baseline measures taken from Donovan et al. [8]. To understand how perceptions of opioid need, concern for drug abuse and/or diversion, and plan to prescribe opioids for a given patient encounter varied from before to after review of PDMP data, we created a brief questionnaire. We searched the literature for validated items to measure perceived patient need for pain medication and/or concern for abuse, but could not find any that were relevant. We therefore developed our own single items to capture each key content area to minimize interruption of care and optimize real-time data collection. We specifically chose to use a Likert scale for ratings of perceived patient need for opioids and concern for abuse and/or diversion because in piloting the questions we found that there was heterogeneity if we chose a “forced” yes/no response. Items included: 1) On a scale from 0 (not at all) to 10 (completely), how much do you think this patient needs an opioid to help manage their pain? 2) On a scale from 0 (not at all) to 10 (completely), how concerned are you about drug abuse and/or diversion? 3) If you had to decide right now whether or not to prescribe an opioid, would you prescribe one? (coded as no/yes). Item 4 was an open-ended space entitled “explanation.” For this space, providers were asked to provide insight into their decision-making at that time point.
Analyses
We excluded cases (N = 2) where the post-PDMP surveys were not completed. Given the distribution of responses to ordinal rated questions from pre- and post-PDMP surveys, we calculated the median and interquartile range (IQR) for perceived patient opioid need and concern for drug abuse and/or diversion ratings. We categorized encounters by opioid prescribing plan from before/after PDMP review as follows: plan to prescribe an opioid both before and after PDMP review (O+/O+); plan to prescribe opioid changes from “yes” to “no” (O+/O−); no plan to prescribe an opioid both before and after PDMP review (O−/O−); plan to prescribe opioid changes from “no” to “yes” (O−/O+). We examined changes in cognitions across categories using Wilcoxon rank sum tests, and we visually displayed distributions of ratings in boxplots. We summarized qualitative explanations from EM providers when opioid prescribing plans changed from the pre- to post-PDMP period.
Results
EM Provider Characteristics
We consented 18 MDs and five midlevel providers to participate, all of whom provided at least one patient encounter to the data set. At baseline, 70% of enrolled EM providers reported feeling comfortable managing patients with a suspicion for opioid abuse and/or diversion, 64% felt uncomfortable prescribing them opioids, and 48% felt comfortable discussing changes in treatment plans (including nonopioid analgesics) (Table 1). Among the 103 paired questionnaires included in the final analysis, 65 (63.1%) were completed by MDs and 38 (36.9%) were reported by midlevel providers.
Table 1.
Baseline EM provider cognitions
| Thoughts About Patients who Present with Pain who Have a Concerning History of Opioid Abuse and/or Diversion | Strongly Agree, No. (%) | Agree, No. (%) | Neither Agree nor Disagree, No. (%) | Disagree, No. (%) | Strongly Disagree, No. (%) |
|---|---|---|---|---|---|
| A key responsibility of emergency providers is effective communication with these patients | 15 (65) | 5 (22) | 0 | 0 | 3 (13) |
| I dread having to treat them | 2 (9) | 5 (22) | 10 (43) | 5 (22) | 1 (4) |
| I will be able to help them improve their lives | 2 (9) | 0 | 11 (48) | 9 (39) | 1 (4) |
| They are abusing the health care system | 1 (4) | 7 (31) | 9 (39) | 5 (22) | 1 (4) |
| I feel bad that they are suffering | 4 (17) | 15 (65) | 3 (13) | 1 (4) | 0 |
|
| |||||
| Comfort with Patients who Present with Pain who Have a Concerning History of Opioid Abuse and/or Diversion | Totally Comfortable | Somewhat Comfortable | Neither Comfortable nor Uncomfortable | Somewhat Uncomfortable | Totally Uncomfortable |
|
| |||||
| Managing these patients | 8 (35) | 8 (35) | 2 (9) | 4 (17) | 1 (4) |
| Prescribing opioids to them | 1 (4) | 5 (22) | 0 | 13 (57) | 4 (17) |
| Discussing changes in pain management with them | 3 (13) | 8 (35) | 3 (13) | 9 (39) | 0 |
| Referring them to substance use treatment | 9 (39) | 6 (26) | 4 (17) | 3 (13) | 1 (4) |
EM = emergency medicine.
Pre-PDMP Opioid Prescribing Plan and Cognitions
Prior to viewing the PDMP, EM providers indicated that they planned on prescribing an opioid analgesic in 65/103 (63.1%) encounters. The median (IQR) rating of perceived patient need for opioid was 6 (3–8), with 0 reported 9/103 times (8.7%). The median (IQR) rating for concern for drug abuse and/or diversion was 4 (1–6), with 0 reported 17/103 times (16.5%) Ratings of perceived patient need for opioid analgesics were higher when an opioid was planned to be prescribed vs not prescribed (median [IQR] = 7 [6–8] vs 3 [1–5]; P < 0.0001). Ratings of concern for opioid abuse and/or diversion were lower when an opioid was planned to be prescribed vs not prescribed (median [IQR] = 3 [1–5] vs 6 [4–8]; P < 0.0001). Pre-PDMP qualitative comments supporting not prescribing an opioid included low pain suspicion, prior ED visits, and patient-stated allergies to non-narcotics. All qualitative comments can be seen in the Supplementary Data.
Change in Opioid Prescribing Plan
Immediately after viewing the PDMP, EM providers indicated that they planned on prescribing an opioid analgesic in 68/103 (66.0%) encounters. The median (IQR) rating of perceived patient need for opioid was 6 (3–8), with 0 reported 11/103 times (10.7%). The median (IQR) rating for concern for drug abuse and/or diversion was 2 (0–6), with 0 reported 26/103 times (25.2%). Boxplots demonstrating changes from before to after PDMP review in cognitions are shown in Figures 1 and 2.
Figure 1.
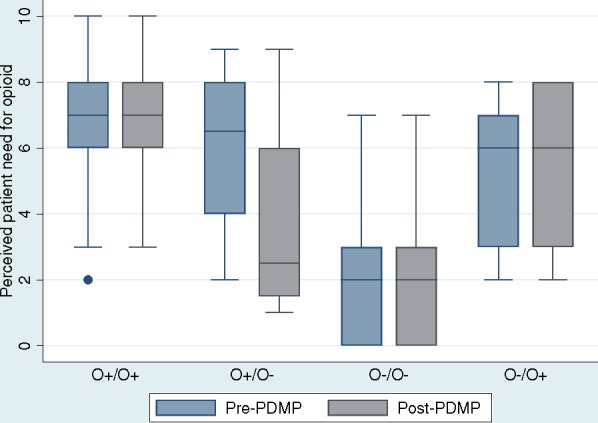
Perceived need for opioid before and after prescription drug monitoring program (PDMP) review by prescribing plan. Boxplots show median (line), interquartile range (box), and outliers (dots). O+/O+ = plan to prescribe an opioid both before and after PDMP review; O+/O− = plan to prescribe opioid changes from “yes” to “no”; O−/O− = no plan to prescribe an opioid both before and after PDMP review; O−/O+ = plan to prescribe opioid changes from “no” to “yes.”
Figure 2.
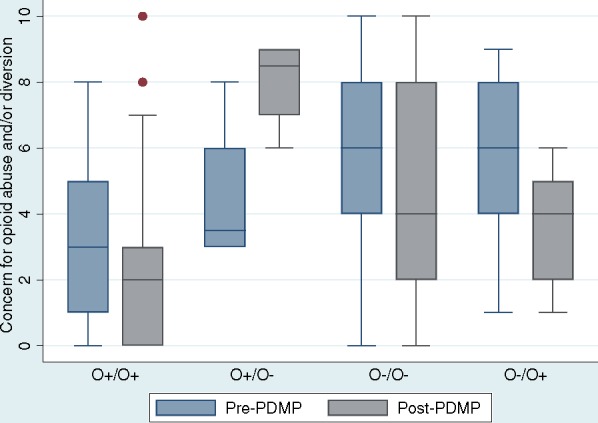
Perceived opioid abuse and/or diversion before and after prescription drug monitoring program (PDMP) review by opioid prescribing plan. Boxplots show median (line), interquartile range (box), and outliers (dots). O+/O+ = plan to prescribe an opioid both before and after PDMP review; O+/O− = plan to prescribe opioid changes from “yes” to “no”; O−/O− = no plan to prescribe an opioid both before and after PDMP review; O−/O+ = plan to prescribe opioid changes from “no” to “yes.”
Ninety-two of 103 (89.3%) encounters resulted in no change in opioid prescribing plan: Opioids were planned on being prescribed both before and after PDMP review (O+/O+) in 61/92 encounters (66.3%). Opioids were not planned on being prescribed both before and after PDMP review (O−/O−) in 31/92 encounters (33.7%). For the four encounters when the plan changed from “yes” to “no” (O+/O−), providers reported decreased perceived patient opioid need 75% of time and increased concern for opioid abuse and/or diversion 75% of time. In these encounters, providers cited suspicious PDMP data, including multiple prior opioid prescriptions or undisclosed ongoing opioid use.
For the seven encounters when the plan changed from “no” to “yes” (O−/O+), providers reported increased perceived patient opioid need 28.6% of the time and decreased concern for opioid abuse and/or diversion 14.3% of time. Providers who changed their plan from “no” to “yes” (O−/O+) cited the absence of a risky PDMP history in justification of the change.
Discussion
Consistent with prior studies [7], we found that review of PDMP data rarely alters plans to prescribe an opioid among emergency providers. We also found that when changes in opioid prescribing plan were made, this was reflected by changes in cognitions both related to perceived patient need for opioids and concern for drug abuse and/or diversion. Among the four times that a provider altered their opioid prescribing plan from “yes” to “no,” there were concurrent reductions in the perceived patient need for opioids as well as increases in concern for opioid abuse and/or diversion. The qualitative findings indicated that EM providers either found evidence of prior opioid prescriptions or controlled substance use that was not disclosed in-person.
Among the seven times that a provider altered their opioid prescribing plan from “no” to “yes,” there were predominantly only decreases in concern for opioid abuse and/or diversion. In these cases, qualitative findings suggest that EM providers were reassured when the PDMP either did not have any record of prior opioid use or when it reinforced the veracity of a patient’s history.
While opioid prescribing in our EDs has declined over time and since review of PDMPs has become mandatory [8], it is unclear whether these changes are generically related to altered societal norms or whether review of PDMP data actually alters prescribing-related cognitions. Our study may help shed some light on this knowledge gap. It appears that the PDMP more often makes EM providers, who may have higher baseline concern for opioid abuse and/or diversion than other providers who have greater knowledge of patients’ histories, more comfortable prescribing opioids to patients. Although this could be perceived as a positive outcome of PDMP use in that it increases trust between providers and patients, it could also be viewed as potentially problematic by providing a false sense of comfort with opioid prescribing. This is somewhat concerning in that the PDMP is limited in its ability to gauge opioid abuse risk and that the majority of nonmedical users get their meds from friends/family, so they wouldn’t even show up in the PDMP.
There are several strengths to this study. Prior studies have been largely limited to retrospective or summary surveys of provider feelings about the PDMP [9] or retrospective database studies examining the temporal relationship of instituting the PDMP with prescribing habits [10]. In this study, we capture aspects of individual cognitions and prescribing decisions as they are made, thus ensuring that effects are isolated to the PDMP. Relatedly, we were present during the procedures to ensure temporality to survey completion and minimize possible effects from other (non-PDMP) data elements. We sampled prescribing data from a variety of providers, including both physician and midlevel providers, with varying levels of experience, baseline beliefs, and comfort with caring for patients in pain with a history of drug abuse and/or diversion. Finally, we complement quantitative findings with qualitative comments from EM providers, further supporting our interpretations of quantitative findings.
This study has several limitations. We were not powered to show differences between prescribing cognition ratings due to resource limitations, and therefore our findings should be viewed as preliminary. The patient encounters studied were a convenience sample and do not represent our general pool of ED patients who present with pain. For instance, EM providers in this study planned on prescribing an opioid more than 60% of the time, which is much higher than our baseline rate of 12% at this site [8]. This suggests that EM providers referred patients to the study who had a much higher probability of receiving an opioid, which most likely biased findings related to perceived need, as it would have appeared higher than it actually is.
Despite these limitations, we believe that our findings can begin to inform interventions to help aid providers in making safer prescribing decisions. For example, providers should be educated that the PDMP is only one way to help identify patients at risk for opioid misuse, and that individuals with no prior opioid use can develop opioid misuse from initial short-term prescriptions [11,12]. Screening for traits such as impulsivity or psychiatric disorders that are known to be associated with substance abuse [13] could be incorporated into existing health screens for patients for whom an opioid analgesic is being considered in addition to PDMP reviews. Also, there may be many individuals who have heretofore not used prescription opioids yet have had past illicit opioid or other drug abuse. In these cases, urine drug screens could be added to procedures for targeted patients to identify other drugs of abuse.
Supplementary Data
Supplementary data are available at Pain Medicine online.
Supplementary Material
Acknowledgments
Funding sources: Research funding was provided by an internal grant from the Department of Emergency Medicine at the University of Pittsburgh. B. Suffoletto is supported by a K23 from the National Institute on Alcohol Abuse and Alcoholism (AA023284).
Conflicts of interest: Authors have no conflicts of interest related to this study.
References
- 1. Rutkow L, Smith KC, Lai AY, et al. Prescription drug monitoring program design and function: A qualitative analysis. Drug Alcohol Depend 2017;180:395–400. [DOI] [PubMed] [Google Scholar]
- 2. Weiner SG, Griggs CA, Mitchell PM, et al. Clinician impression versus prescription drug monitoring program criteria in the assessment of drug-seeking behavior in the emergency department. Ann Emerg Med 2013;624:281–9. [DOI] [PubMed] [Google Scholar]
- 3. Finley EP, Garcia A, Rosen K, et al. Evaluating the impact of prescription drug monitoring program implementation: A scoping review. BMC Health Serv Res 2017;171:420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leichtling GJ, Irvine JM, Hildebran C, et al. Clinicians’ use of prescription drug monitoring programs in clinical practice and decision-making. Pain Med 2017;186:1063–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Doyle S, Leichtling G, Hildebran C, Reilly C.. Research to support optimization of prescription drug monitoring programs. Pharmacoepidemiol Drug Saf 2017;2611:1425–7. [DOI] [PubMed] [Google Scholar]
- 6. Barnett ML, Olenksi AR, Jena AB.. Opioid prescribing by emergency physicians and risk of long-term use. N Engl J Med 2017;37619:1895. [DOI] [PubMed] [Google Scholar]
- 7. Weiner SG, Baker O, Poon SJ, et al. The effect of opioid prescribing guidelines on prescriptions by emergency physicians in Ohio. Ann Emerg Med 2017;706:799–808.e1 [DOI] [PubMed] [Google Scholar]
- 8. Donovan AK, Wood GJ, Rubio DM, Day HD, Spagnoletti CL.. Faculty communication knowledge, attitudes, and skills around chronic non-malignant pain improve with online training. Pain Med 2016;1711:1985–92. [DOI] [PubMed] [Google Scholar]
- 9. Hildebran C, Cohen DJ, Irvine JM, et al. How clinicians use prescription drug monitoring programs: A qualitative inquiry. Pain Med 2014;157:1179–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Paulozzi LJ, Kilbourne EM, Desai HA.. Prescription drug monitoring programs and death rates from drug overdose. Pain Med 2011;125:747–54. [DOI] [PubMed] [Google Scholar]
- 11. Hoppe JA, Kim H, Heard K.. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med 2015;655:493–9.e4. [DOI] [PubMed] [Google Scholar]
- 12. Shah A, Hayes CJ, Martin BC.. Factors influencing long-term opioid use among opioid naive patients: An examination of initial prescription characteristics and pain etiologies. J Pain 2017;1811:1374–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Webster LR. Risk factors for opioid-use disorder and overdose. Anesth Analg 2017;1255:1741–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


