Abstract
Background
Anorexia nervosa (AN) is characterised by a failure to maintain a normal body weight due to a paucity of nutrition, an intense fear of gaining weight or behaviour that prevents the individual from gaining weight, or both. The long‐term prognosis is often poor, with severe developmental, medical and psychosocial complications, high rates of relapse and mortality. 'Family therapy approaches' indicate a range of approaches, derived from different theories, that involve the family in treatment. We have included therapies developed on the basis of dominant family systems theories, approaches that are based on or broadly similar to the family‐based therapy derived from the Maudsley model, approaches that incorporate a focus on cognitive restructuring, as well as approaches that involve the family without articulation of a theoretical approach.This is an update of a Cochrane Review first published in 2010.
Objectives
To evaluate the efficacy of family therapy approaches compared with standard treatment and other treatments for AN.
Search methods
We searched the Cochrane Common Mental Disorders Controlled Trials Register (CCMDCTR) and PsycINFO (OVID) (all years to April 2016). We ran additional searches directly on Cochrane Central Register for Controlled Trials (CENTRAL), MEDLINE, Ovid Embase, and PsycINFO (to 2008 and 2016 to 2018). We searched the World Health Organization (WHO) trials portal (ICTRP) and ClinicalTrials.gov, together with four theses databases (all years to 2018). We checked the reference lists of all included studies and relevant systematic reviews. We have included in the analyses only studies from searches conducted to April 2016.
Selection criteria
Randomised controlled trials (RCTs) of family therapy approaches compared to any other intervention or other types of family therapy approaches were eligible for inclusion.
We included participants of any age or gender with a primary clinical diagnosis of anorexia nervosa.
Data collection and analysis
Four review authors selected the studies, assessed quality and extracted data. We used a random‐effects meta‐analysis. We used the risk ratio (with a 95% confidence interval) to summarise dichotomous outcomes and both the standardised mean difference and the mean difference to summarise continuous measures.
Main results
We included 25 trials in this version of the review (13 from the original 2010 review and 12 newly‐included studies). Sixteen trials were of adolescents, eight trials of adults (seven of these in young adults aged up to 26 years) and one trial included three age groups: one adolescent, one young adult and one adult. Most investigated family‐based therapy or variants. Reporting of trial conduct was generally inadequate, so that in a large number of studies we rated the risk of bias as unclear for many of the domains. Selective reporting bias was particularly problematic, with 68% of studies rated at high risk of bias in this area, followed by incomplete outcome data, with 44% of studies rated at high risk of bias in this area. For the main outcome measure of remission there was some low‐quality evidence (from only two studies, 81 participants) suggesting that family therapy approaches might offer some advantage over treatment as usual on rates of remission, post intervention (risk ratio (RR) 3.50, 95% confidence interval (CI) 1.49 to 8.23; I2 = 0%). However, at follow‐up, low‐quality evidence from only one study suggested this effect was not maintained. There was very low‐quality evidence from only one trial, which means it is difficult to determine whether family therapy approaches offer any advantage over educational interventions for remission (RR 9.00, 95% CI 0.53 to 153.79; 1 study, N = 30). Similarly, there was very low‐quality evidence from only five trials for remission post‐intervention, again meaning that it is difficult to determine whether there is any advantage of family therapy approaches over psychological interventions (RR 1.22, 95% CI 0.89 to 1.67; participants = 252; studies = 5; I2 = 37%) and at long‐term follow‐up (RR 1.08, 95% CI 0.91 to 1.28; participants = 200; studies = 4 with 1 of these contributing 3 pairwise comparisons for different age groups; I2 = 0%). There was no indication that the age group had any impact on the overall treatment effect; however, it should be noted that there were very few trials undertaken in adults, with the age range of adult studies included in this analysis from 20 to 27. There was some evidence of a small effect favouring family based therapy compared with other psychological interventions in terms of weight gain post‐intervention (standardised mean difference (SMD) 0.32, 95% CI 0.01 to 0.63; participants = 210; studies = 4 with 1 of these contributing 3 pairwise comparisons for different age groups; I2 = 11%) . Overall, there was insufficient evidence to determine whether there were any differences between groups across all comparisons for most of the secondary outcomes (weight, eating disorder psychopathology, dropouts, relapse, or family functioning measures), either at post‐intervention or at follow‐up.
Authors' conclusions
There is a limited amount of low‐quality evidence to suggest that family therapy approaches may be effective compared to treatment as usual in the short term. This finding is based on two trials that included only a small number of participants, and both had issues about potential bias. There is insufficient evidence to determine whether there is an advantage of family therapy approaches in people of any age compared to educational interventions (one study, very low quality) or other psychological therapies (five studies, very low quality). Most studies contributing to this finding were undertaken in adolescents and youth. There are clear potential impacts on how family therapy approaches might be delivered to different age groups and further work is required to understand what the resulting effects on treatment efficacy might be. There is insufficient evidence to determine whether one type of family therapy approach is more effective than another. The field would benefit from further large, well‐conducted trials.
Plain language summary
Family therapy for those diagnosed with anorexia nervosa
Review Question
This review investigated whether family therapy approaches reduce rates of anorexia nervosa (AN), or associated symptoms, compared to other treatments.
Background
People with AN have a deliberately maintained low body weight and distorted body image. They also experience related medical and psychological problems, and the risk of dying from the disease (mortality) is relatively high. Family therapy approaches are one form of treatment used in AN.
Search date
The evidence is current up to 8 April 2016.
Study characteristics
We included 25 trials in the review. Fourteen trials used family‐based therapy, one used systems family therapy, one used structural family therapy and seven studies used therapy with family involvement but did not provide specific details about the theory behind the therapy or its procedures, termed other family therapy. Two studies included two family therapy arms each: one included family‐based therapy and systems family therapy arms, and one included systems family therapy and other family therapy arms. Four studies compared family therapy approaches to treatment as usual, six compared family therapy approaches to other psychological interventions and two compared family therapy to educational interventions. Twelve studies compared various forms of family therapy approaches to each other. Two studies included both a treatment as usual as well as other psychological intervention arms.
Key results
Overall there was some low‐quality evidence from only two trials to suggest that family therapy approaches may be better than treatment as usual in the short term. The size and very low quality of the evidence base and the consistency of the trial outcomes are insufficient at this time to draw conclusions about whether family therapy approaches offer any clear advantage over educational or psychological interventions. We found very few differences between treatment groups on measures of weight, eating disorder symptoms and family functioning, and these differences were generally not maintained at follow‐up. The reporting of death rates was not clear enough to assess whether death is reduced for those treated with family therapy approaches compared to other interventions. There was very little information about the effects of the interventions on general or family functioning.
Quality of the evidence
The way the trials were run was not adequately described in many studies and we found potential risks of bias in most of the studies. This limited the meaningful conclusions that we could draw from the studies.
Authors' conclusions
Overall, there is a very limited evidence base in this field. There is some low‐quality evidence to suggest that family therapy approaches may be effective compared to treatment as usual in the short term. There is insufficient evidence to be able to determine whether family therapy approaches offer any advantage over educational interventions, other types of psychological therapy, or whether one type of family therapy approach is more effective than another. Most of the studies contributing to the findings were undertaken in adolescents and young adults. There are clear implications about how family therapy approaches might be delivered to different age groups, and we need further research to understand what the resulting effects on treatment might be.
Summary of findings
Background
Description of the condition
The standard diagnostic criteria for anorexia nervosa (AN) are based on ICD (WHO 1992) and DSM (APA 2013) diagnostic systems. The criteria include a failure to maintain a normal body weight due to a paucity of nutrition, an intense fear of gaining weight or compulsive behaviour (e.g. excessive exercise) that prevents the individual from gaining weight, or both. A distorted body image or distorted perception of dangerously low body weight is also present, as well as a link between self‐evaluation and body shape and weight. Individuals with AN will typically use any or all of three strategies for losing weight or reducing the possibility for weight gain, or both. These strategies are 1) food restriction, 2) purging food (e.g. vomiting, use of laxatives), and 3) excessive exercise. High rates of severe medical, developmental and psychosocial complications, including the loss of menses in females, is also common (Katzman 2005; Zipfel 2003). AN is associated with high morbidity and mortality rates compared to other psychiatric disorders (Harris 1998). In longitudinal follow‐up studies of chronically ill adults with AN, mortality rates of between 9% and 20% have been observed over 12‐ to 20‐year follow‐up periods (Fichter 2006; Sullivan 1995). The long‐term prognosis for the illness is often poor and high rates of relapse have been reported (Berkman 2007). Many patients never receive treatment, and there are high rates of treatment refusal, treatment avoidance and treatment dropout (Pingani 2012; Tolkien II Team 2006).
Lifetime prevalence for AN according to DSM‐IV criteria (APA 1994) was previously reported as 0.9% for females and 0.3% for males (Hudson 2007). However, in recent years the DSM criteria for AN have been revised in the DSM‐5 (APA 2013), with the previous criteria of weight loss, fear of weight gain and amenorrhoea removed. The changes have reportedly led to a considerable increase of between 50% to 60% in female lifetime prevalence rates in those who met DSM‐5 criteria compared to those assessed with DSM‐IV criteria (Mustelin 2016; Smink 2014).
There is acknowledgement of the complex aetiology of eating disorders with the interaction of psychological and environmental factors with genetic factors at play (Culbert 2015). Genetic factors have been implicated in the development of AN, with studies reporting high heritability estimates ranging from 58% to 90% (Kaye 2000; Wade 2000). Early models of family therapy were based on explanatory models that assumed that there were specific family processes that interacted with a vulnerability in the child to give rise to an eating disorder (e.g. the Psychosomatic Family Model of Minuchin 1975) but the empirical evidence supporting such models is unconvincing. Moreover, it is important to point out that while a number of studies have found some association between eating disorders and aspects of family environment and family functioning e.g. attachment, parenting style, communication, conflict (Cerniglia 2017; Jewell 2016; Miller‐Day 2006; Soenens 2008), this does not imply these cause AN. Indeed the research is often reliant on retrospective recall in cross‐sectional studies, does not take into account potential confounding such as the co‐existence of other psychosocial disorders, and does not consider the possibility that what is being observed is an outcome of having someone in the family with an eating disorder which impacts the whole family (Whitney 2005). Those with eating disorders exist in a variety of family contexts and focusing on the experience of those families has been proposed as more beneficial in terms of understanding how to support families in the treatment of someone with an eating disorder (Eisler 2005). Position papers from within the field have stressed the importance of the avoidance of the placement of blame on families of sufferers of eating disorders, and emphasised the utility of including families in the treatment process for many sufferers (Le Grange 2010). Current models of family therapy for eating disorders emphasize that families are primarily a resource rather than a target of treatment i.e. a treatment with the family rather than of the family (Simic 2018).
Description of the intervention
One common goal of treatment for AN is weight restoration, with treatment typically beginning with nutritional rehabilitation (Fairburn 2003). In addition, a range of psychological and pharmacological therapies have been used to augment or follow weight restoration. There is a lack of evidence to support the use of antidepressants (Claudino 2006) or antipsychotic medication (Court 2008) in AN treatment. No specific psychological intervention is considered more efficacious for treating AN, including cognitive behavioural therapy (CBT) ‐ enhanced, interpersonal therapy, cognitive analytic therapy, behavioural therapy, psychodynamic therapy, or specialist supportive clinical management (Bulik 2007; Carter 2011; Hay 2015; Le Grange 1992). Nevertheless, specific types of psychological interventions may be effective for specific populations. For example, CBT for reducing relapse rates in adults who have already achieved restoration of a normal body weight (Bulik 2007), CBT‐AN for severe and enduring AN with a focus on improving the quality of life rather than weight restoration (Touyz 2013; Touyz 2015), and family therapy for children and young people with AN (Bulik 2007; Le Grange 2005b; NICE 2017).
How the intervention might work
A range of different family therapies have been considered in this review and each has a different approach. Earlier approaches were based on a model of change derived from an explanatory model of family functioning. However, as described above, current models emphasise the utility of engaging families as a resource. The models of change that inform these current approaches are still evolving.
(Note: the following includes descriptive labels to group together broadly similar approaches based on the description of the therapies provided in the trials. Full descriptions of therapy used, including how the trial authors named the therapy, are provided in Characteristics of included studies).
Family systems theory describes how family dynamics/processes can contribute to the development or maintenance or both of problems within the family system. Two dominant approaches to applying family systems theory are Structural Family Therapy and Strategic Family Therapy.
Minuchin's 1974 Structural Family Therapy examines and challenges dysfunctional family dynamics (Minuchin 1974). Within this theory, AN is viewed as a consequence of an over‐involved, conflict‐avoidant and rigid family structure (Minuchin 1978). These family factors are thought to combine with some type of physiological predisposition to developing AN. The aim of Structural Family Therapy is to alter the family's processes that contribute to the problem and therefore treat the AN. Family processes are evaluated during the therapy session and subsystems within the entire family examined. This approach was the first to emphasise the importance of including the family in treatment and addressing some of the problematic patterns that were present.
A follow‐on approach, Strategic Family Therapy, moves away from hypothesising about the onset of AN and instead focuses on inducing change in AN symptoms and acknowledging the effect of the illness on all family members. Dysfunctional family processes are discussed and a focus on communicating and problem‐solving is maintained by methods such as reframing and paradoxical intervention (Madanes 1981). Strategic interventions may still be used in other forms of individual or family therapy in order to address family difficulties.
Current models, which in this review are grouped in a category called family based therapy (FBT) disregard the notion that the family dynamic is a direct causative agent in the pathogenesis of the disorder (Lock 2005; Le Grange 1999). Instead, FBT has a behavioural and educative focus. FBT aims to assist families in managing the eating behaviours of the family member with AN by providing education about AN, encouraging parents/caregivers to generate strategies for increasing food intake and limiting physical activity. There are three principal phases to the treatment process that are described in early and more recent investigations into the efficacy of FBT (e.g. Dare 1990; Le Grange 2012). In the first phase, the principal focus is on refeeding (ensuring adequate caloric and nutritional intake) and weight restoration. This is achieved by placing responsibility for the family member's eating patterns in the hands of the parents/caregivers and emphasising the individual's inability to control eating patterns due to the effects of starvation. Parents/caregivers are given the responsibility to refeed and the therapist provides ongoing support and encouragement. However, when implemented with adult patients, parents/caregivers are not encouraged to take control of the family member's eating behaviour in the same way as when working with younger people (e.g. Dare 2001). In the second phase of FBT, the individual with AN develops their independence with eating and parents/caregivers take the focus off food. There may also be some assistance with problem‐solving about family and psychological issues that interfere with refeeding and weight restoration. The third phase addresses any concerns that are not directly related to AN. These concerns may be related to normal adolescent development, including the (re‐)establishment of healthy family boundaries. There are two subtypes of FBT. Conjoint family therapy (Eisler 2000; Le Grange 1992; Le Grange 2016) occurs when the phases described above are implemented in joint therapy sessions involving both the person with AN and their family. Implementing this framework with the family and individual in the session together allows the therapist to directly observe and interact with family dynamics. Contrastingly, separated family therapy (Eisler 2000) or family counselling (Le Grange 1992) occurs when the FBT framework is implemented through therapy sessions where the individual with AN is seen separately from their parents/caregivers.
A further therapy described in the literature that we have grouped in the category of FBT, behavioural family systems therapy (BFST), also has three stages to treatment, that are very similar in nature to those used in FBT (Ball 2004; Le Grange 2017; Robin 1994; Robin 1995). The main difference is the focus on cognitive restructuring that is used in order to reduce problematic cognitions about food and weight. In addition to this, the BFST therapist also assists families in reducing problematic dynamics and processes such as enmeshment, triangulation, and coalitions by addressing eating disorder psychopathology, behavioural patterns and problems with the family structure (Robin 1994; Robin 1995).
In addition to these formally described family therapy interventions, families are involved in other ways of supporting recovery from AN. This involvement may take various forms, and while they may not necessarily have such a well‐described theoretical underpinning, may also have an important influence on recovery. Hence, we describe family therapy approaches as a way to include these as well as more formally described family therapy interventions.
Why it is important to do this review
Our original Cochrane Review investigating family therapy in AN was published in 2010 (Fisher 2010), from a literature search that was conducted on 1 August 2008. The aim of this review was to determine whether family involvement in therapy, of any description, is beneficial to those with AN and what effect this involvement might have. The overall conclusion from the original review was that there was some evidence to suggest that family therapy may be effective compared to treatment as usual in the short term. However, this was based on few trials that included only a small number of participants, all of which had issues about potential bias. There was insufficient evidence to be able to determine whether family therapy offers any advantage over other types of psychological interventions, or whether one type of family therapy is more effective than another. It was suggested that the field would benefit from a large, well‐conducted trial.
The purpose of this updated review is to provide a systematic review of the current literature into the efficacy of family therapy approaches for AN. The results of this review will be useful for treatment institutions interested in implementing evidence‐based models of care for individuals with AN.
Objectives
To evaluate the efficacy of family therapy approaches compared with standard treatment and other treatments in AN.
Methods
Criteria for considering studies for this review
Types of studies
We include all published or unpublished randomised controlled trials (RCTs). We would also have included cluster‐randomised controlled trials and cross‐over trials, but we found none.
There were no language restrictions, nor did we exclude studies on the basis of the date of publication.
Types of participants
We included people of any age or gender with a primary clinical diagnosis of anorexia nervosa (AN), either or both purging or restricting subtypes, based on DSM (APA 2013) or ICD criteria (WHO 1992) or clinicians' judgement, and of any severity. We included those with chronic AN. We included those with psychiatric comorbidity, with the details of comorbidity documented.
Participants may have received the intervention in any setting (including in‐, day‐ or outpatient) and may have started in the trial at the beginning of treatment or part‐way through (e.g. after discharge from hospital or some other indication/definition of stabilisation).
We included those living in a family unit (of any nature, as described/defined by study authors), and those living outside of a family unit.
Types of interventions
Interventions Trials where the intervention describes inclusion of the family in some way and is labelled 'family therapy'. These interventions may have been delivered as a monotherapy or in conjunction with other interventions (including standard care, which may or may not be in the context of an inpatient admission).
The main categories of family therapy approaches considered were:
Structural family therapy
Systems (systemic) family therapy
Strategic family therapy
Family‐based therapy and its variants (including short‐term, long‐term, and separated) and behavioural family systems therapy (these two therapies were grouped together, given the similarity of approach)
Other (including other approaches that use family involvement in therapy but are less specific about the theoretical underpinning of the therapy and its procedures).
Control Conditions
Family therapy approaches were compared with:
Standard care or treatment as usual
Biological interventions (for example, antidepressants, antipsychotics, mood stabilisers, anxiolytics, neutraceuticals, and other agents such as anti‐glucocorticoids)
Educational interventions (for example, nutritional interventions and dietetics)
Psychological interventions (for example, cognitive behavioural therapy (CBT) and its derivatives, cognitive analytical therapy, interpersonal therapy, supportive therapy, psychodynamic therapy, play therapy, other)
Alternative or complementary interventions (for example, massage, exercise, light therapies).
Additionally, different types of family therapy approaches were compared to each other. The addition of a family therapy approach to other interventions (including standard care) was also compared to other interventions alone.
Main comparisons
The main comparisons made included:
Family therapy approaches versus standard care/treatment as usual
Family therapy approaches versus psychological interventions
Family therapy approaches versus educational interventions
Family therapy approach versus other type of family therapy approach.
We would also have included the following comparisons: Family therapy approaches versus biological interventions; and Family therapy approaches versus alternative/complementary interventions; however, we had neither the relevant trials nor useable data from these.
Types of outcome measures
Primary outcomes
Remission (by DSM or ICD or trialist‐defined cut‐off on standardised scale measure for remission versus no remission)
All‐cause mortality
Secondary outcomes
Family functioning as measured on standardised, validated and reliable measures, e.g. Family Environment Scale (Moos 1994), Expressed Emotions (Vaughn 1976), FACES III (Olson 1985)
General functioning, measured by return to school or work, or by general mental health functioning measures, e.g. Global Assessment of Functioning (GAF) (APA 1994)
Dropout (by rates per group during treatment)
Eating disorder psychopathology (evidence of ongoing preoccupation with weight/shape/food/eating by eating‐disorder symptom measures using any recognised validated eating disorders questionnaire or interview schedule, e.g. the Morgan‐Russell Assessment Schedule (Morgan 1988), Eating Attitudes Test (EAT, Garner 1979), Eating Disorders Inventory (Garner 1983; Garner 1991).
Weight, including all representations of this measure such as kilograms, body mass index (BMI, kg/m2) and average body weight (ABW) calculations. We included this measure after the finalisation of our protocol, due to the lack of universal reporting on remission, and the differing definitions used for remission
Relapse (by DSM or ICD or trialist‐defined criteria for relapse or hospitalisation)
We had planned to provide a description of any adverse outcomes from each trial, but adverse outcomes other than mortality were not generally reported in the trials.
The primary outcomes were reported first, followed by the secondary outcomes, in the order outlined above.
We classified outcomes as: 1) immediate post‐intervention; 2) short‐term (< 12 months) follow‐up, and; 3) long‐term (> 12 months) follow‐up.
As with the comparisons, we anticipate that in future updates we will reduce the number of outcomes in order to reduce the likelihood of multiple analyses generating spurious results. We will limit outcomes to:
Remission
Mortality
Family functioning
Eating disorder psychopathology
Weight
Search methods for identification of studies
Cochrane Common Mental Disorders Controlled Trials Register (CCMD‐CTR) The Cochrane Common Mental Disorders Group maintains a specialised register of randomised controlled trials, the CCMD‐CTR. This register contains over 40,000 reference records (reports of RCTs) for anxiety disorders, depression, bipolar disorder, eating disorders, self‐harm and other mental disorders within the scope of this Group. The CCMD‐CTR is a partially studies‐based register with more than 50% of reference records tagged to around 12,500 individually PICO‐coded study records. Reports of trials for inclusion in the register are collated from (weekly) generic searches of MEDLINE (1950 onwards), Embase (1974 onwards) and PsycINFO (1967 onwards), quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review‐specific searches of additional databases. Reports of trials are also sourced from international trial registries, drug companies, the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. Details of CCMD's core search strategies (used to identify RCTs) can be found on the Group's website, with an example of the core MEDLINE search displayed in Appendix 1.
In 2016 the Group’s Specialised Register (CCMD‐CTR) became out of date with the Editorial Group’s move from Bristol to York.
Electronic searches
1. Cochrane Specialised Register (CCMD‐CTR) (to April 2016)
The Information Specialist with the Cochrane Common Mental Disorders Group (CCMD) searched their group's specialised register (CCMD‐CTR‐Studies and CCMD‐CTR‐References) (1 August 2008 to 8 April 2016), using the following terms:
((*family or families) and (anorexi* or "eating disorder*" or EDNOS)) [All Fields]
An earlier search of the CCMD‐CTR (all years to 2008) is displayed in Appendix 2.
2. Additional bibliographic database searches
The Information Specialist performed an additional search of PsycINFO (2008 to 21 April 2016) and PubMed (current year) to help ensure that we had missed no studies from the Group's specialised register (Appendix 3).
In May 2018, the Information Specialist ran an update search on the following databases (as the CCMD‐CTR had become out of date at the time) (Appendix 4). We had also searched these databases in 2008 for the first version of the review, but as all studies were accounted for by the CCMD‐CTR we did not repeat this exercise, whilst the specialised register was in date:
Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 5 of 12, May 2018);
Ovid Embase (2016 to 31 May 2018);
Ovid MEDLINE (2016 to 31 May 2018);
Ovid PsycINFO (2016 to May Week 4 2018).
3. International Trials Registers
Relevant trial protocols from the WHO's trials portal (ICTRP) and ClinicalTrials.gov had already been incorporated into the CCMD group's specialised register (to April 2016) and we performed a separate update search on 4 June 2018.
We applied no restriction by date, language or publication status to the searches. We have included only studies from searches conducted to 2016 in the analysis.
Searching other resources
1. Theses
We searched the following databases to identify relevant PhD theses (to 4 June 2018):
DART‐Europe E‐theses Portal (www.dart‐europe.eu/);
EThOS ‐ the British Libraries e‐theses online service (ethos.bl.uk/);
Open Acces Theses and Dissertations (oatd.org);
ProQuest Dissertations and theses database (c/o dissexpress.umi.com/).
2. Reference lists
We checked the reference lists of all included studies and relevant systematic reviews to identify additional studies missed from the original electronic searches (for example, unpublished or in‐press citations).
3. Personal communication
We contacted the first author of included trials contained in the original 2010 review. We attempted contact with one study author of the new trials included in this updated review.
Data collection and analysis
Selection of studies
Three review authors (CF, SS and SH) independently selected studies for possible inclusion in the review. First, we independently reviewed the titles and abstracts of trials identified from the search. Secondly, two out of the four review authors independently examined the full text of all studies that they considered to be of possible relevance. Each review author compiled a list of studies that they believed met the inclusion criteria. We compared the contents of each review author's list, and discussed any discrepancies. We resolved any disagreement by discussion and consensus between all of the review authors.
Data extraction and management
Three review authors (CF, SS and KR) independently extracted the data using specially developed data extraction forms. Each included study underwent data extraction by two review authors. We collected information provided about the descriptors that may have an impact on the treatment effect as listed below.
In order to understand the context to which the trial results are relevant, and to inform generalisability, we documented the following descriptors: age, gender, how the diagnosis was made, setting of care, the subtype of AN, length of treated and untreated illness, age at onset, previous treatment, baseline weight and BMI, baseline eating disorder scale measure as a measure of severity, comorbidity, living arrangements, family educational and occupational details. We also documented the recruitment strategies, the exclusion criteria and the country in which the trial was undertaken.
We recorded the type of family therapy approach, including the name and the major specific interventions. This allowed for discussion of how different types of family therapy approaches may impact on the outcome, as well as grouping of the different types of family therapy approaches in the analysis.
We also documented the intended and delivered 'dosage' including number of sessions, length of sessions, total length of the treatment intervention, who delivered the treatment, whether the treatment was manualised, the training and qualifications of the care deliverers, whether treatment was supervised and whether adherence to the treatment approach was measured.
We independently extracted the point estimates and measures of variability as well as relevant frequency counts for dichotomous variables (CF, SS and KR).
One review author (CF) compiled all comparisons and entered the outcome data into Review Manager 5 (RevMan) for meta‐analysis. A second review author (SH) performed double‐data entry to ensure accuracy of results.
Assessment of risk of bias in included studies
Two of four review authors independently assessed the risks of bias of each of the included trials using a descriptive approach as described by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For the following items we noted a description of the methods and described them in a 'Risk of bias' table, and made our judgements about the resulting risks of bias:
Was the allocation sequence adequately generated?
Was the allocation adequately concealed?
Was knowledge of the allocated interventions adequately prevented during the trial (outcome assessors)? (Blinding of participants and therapists not possible).
Were incomplete outcome data adequately addressed (numbers and reasons for dropout by group and an intention‐to‐treat analysis)?
Are reports of the trial free of the suggestion of selective outcome reporting? If the protocol was available, then we compared outcomes in the protocol and the published report. If not, then we compared outcomes listed in the Methods section of the article with those for which results were reported. We noted whether non‐significant results were mentioned but not reported adequately, as well as noting which of the review outcomes were only reported in terms of significant differences between groups. We also noted the other outcomes (not collected for the review) reported by the trialists in the paper publication(s).
Was the trial apparently free of other problems that could put it at a high risk of bias?
We graded each criterion as low risk of bias, high risk of bias or unclear risk of bias, according to the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When we scored criteria as unclear, one review author attempted to obtain further information from the authors of the trial. The review authors discussed any disagreement in the assessment of risks of bias to reach a consensus.
Measures of treatment effect
For dichotomous outcomes such as 'remission', we expressed the results from each trial as a risk ratio (RR) with a 95% confidence interval (CI), and combined them in meta‐analysis.
We present continuous outcomes, such as symptom measures, in several ways. When absolute values of post‐treatment means and standard deviations (SDs) were given, using the same rating scale across trials, we used them to calculate the mean difference (MD) and 95% confidence interval. If different scales were used to measure the same outcomes, we calculated the standardised mean difference (SMD) with a 95% confidence interval and then combined them for meta‐analysis. Results from linear regression models were not commonly reported and therefore were not extracted or pooled using inverse variance meta‐analysis.
Unit of analysis issues
Where a trial had more than one active treatment arm, we extracted the appropriate arms for each of our main comparisons. If more than one comparison was relevant, we included both in their designated sections (e.g. if a study compared family therapy approaches to both standard care/treatment as usual and another type of psychological therapy, then we included the comparison to standard care/treatment as usual in Comparision 1, while the comparison to psychology therapy appeared in Comparision 2). If a study contained more than one comparison group that could be used for a particular analysis, we chose one comparison group, and included this group in the relevant analysis. Where this occurred (e.g. Dare 2001), we stated it clearly in the Results section.
Dealing with missing data
We imputed missing data where necessary (e.g. calculating SDs from standard errors and P values), and this is clearly documented in the review. We used intention‐to‐treat data where available, with a note of the methods used (such as last observation carried forward or other types of modelling) for imputing missing data. However, we acknowledge that this was often unclear or not available, and in that case we used what was available, which was often the observed case number of participants. In no case were we able to use both last observation carried forward and observed case data to check results for robustness.
Assessment of heterogeneity
Clinical homogeneity was satisfied when we considered participants, interventions and outcome measures to be similar. For trials that were clinically heterogeneous or presented insufficient information for pooling, we provide a descriptive analysis. We assessed statistical homogeneity on the basis of the Cochrane Handbook's recommendations (I2 values of 0% to 40%: might not be important; 30% to 60%: may represent moderate heterogeneity; 50% to 90%: may represent substantial heterogeneity; 75% to 100%: considerable heterogeneity).
We also considered the Chi2 and its P value and the direction and magnitude of the treatment effects, because the importance of the observed I2 depends on (i) magnitude and direction of effects and (ii) strength of evidence for heterogeneity, in addition to the I2 value (Higgins 2003). Because the Chi2 test is underpowered to detect heterogeneity in meta‐analysis that includes only a few studies, we used a P value of 0.10 as a threshold of statistical significance.
When statistical heterogeneity was evident, the aim was to examine it using specified subgroup and sensitivity analyses; however, this was often not possible due to the paucity of trials.
Assessment of reporting biases
We had planned to investigate the potential for publication bias using a funnel plot for the primary outcomes relating to AN remission or symptoms or both. Publication bias has long been associated with funnel plot asymmetry; however, asymmetry may be due to reasons other than publication bias and is difficult to assess in the case of a small number of trials, as in this review. We have therefore not included a funnel plot for publication bias. For this reason, we also include an assessment of the risk of selective outcome reporting bias, as stated above.
Data synthesis
When appropriate, we performed meta‐analysis and obtained pooled effect estimates, using the Review Manager 5 statistical software programme. Meta‐analytic methods used are presented below. For all meta‐analyses, we used a random‐effects model (DerSimonian 1986).
Subgroup analysis and investigation of heterogeneity
We undertook subgroup analysis for the two main comparisons (Family therapy approaches versus standard care/treatment as usual; and Family therapy approaches versus psychological interventions) to investigate the impact of age on the magnitude of the treatment effect. We define adolescents as those aged 12.0 to 18.9 years, and adults as 19 years and older. We used a total mean age for the entire trial, where this was reported. Where mean age was reported by group, we used the average of the mean ages by group to classify trials into the adolescent or adult subgroups.
Given the paucity of trials, subgroup analysis on chronicity was not possible.
we conducted subgroup analysis by the type of family therapy approaches; however, in most comparisons there were only trials using one type of family therapy.
Sensitivity analysis
We planned sensitivity analyses to assess the effect of risk of bias, based on the following groups:
Allocation concealment is rated as inadequate, not used or unclear (and attempts to clarify with authors fail) (A)
Blinding of outcome assessment is not done or unclear (and attempts to clarify with authors fail) (B)
Incomplete outcome data were assessed as high or unclear risk of bias (and attempts to clarify with authors fail) (C).
These criteria for assessing the risks of bias have been shown to influence estimates of treatment effect (Juni 2001). We planned sensitivity analyses for trials excluding those categorised as A, B or C. However, there were too few trials to undertake a meaningful sensitivity analysis on this basis.
Timeline
The review will be updated according to the latest version of the Cochrane Handbook (Higgins 2011).
GRADE and 'Summary of findings' tables
We constructed 'Summary of findings' tables (Higgins 2016), for the following comparisons:
Family therapy approaches versus standard care/treatment as usual;
Family therapy approaches versus psychological interventions; and
Family therapy approaches versus educational interventions
We used the following outcomes:
Remission at short‐term follow‐up;
Remission at long‐term follow‐up; and
Follow‐up mortality.
In the 'Summary of findings' tables we have used the principles of the GRADE approach (Guyatt 1998) to assess the extent to which there can be confidence that the obtained effect estimate reflects the true underlying effect. We judged the quality of the body of evidence on the basis of the included studies’ risks of bias, the directness of the evidence, unexplained heterogeneity, imprecision, and the risk of publication bias. We used the average rate in all the arms of included trials as the 'Assumed risk' for each outcome. As we were not aiming to target any particularly high‐ or low‐risk populations, all the tables were for medium‐risk populations.
Results
Description of studies
Results of the search
The update search for this review (to April 2016) yielded 220 records from the CCMD‐CTR (including 36 trial registry records), 103 from PsycINFO, 179 from PubMed and a further three papers from reference list and theses database searches, resulting in a total of 505 references, leaving 230 papers after duplicates were removed. We selected 91 papers from title and abstract screening for full‐text review. Of these, we excluded 27 papers. We retained a total of 25 studies for inclusion, for which there are multiple companion papers. One of these studies reported data separately for three different age groups and is included in the review as three studies (Russell 1987a; Russell 1987b; Russell 1987c). We describe the characteristics of the included studies below (see Characteristics of included studies). The included studies comprise the 13 studies included in the original 2010 review (Ball 2004; Crisp 1991; Dare 2001; Eisler 2000; Espina 2000; Geist 2000; Hall 1987; Le Grange 1992; Lock 2005; Rausch Herscovici 2006 (previously labelled as Rausch 2006); Robin 1999; Russell 1987; Whitney 2012 (previously labelled as Whitney unpublished)), as well as 12 additional studies (Agras 2014; Besharat 2001; Godart 2012; Herpertz‐Dahlmann 2014; Herscovici 2017; Le Grange 2016; Li 2006; Lock 2010; Lock 2015; Madden 2015; Onnis 2012; Rhodes 2008). Twenty‐one of the included studies had useable data, with four studies (Besharat 2001; Geist 2000; Li 2006; Onnis 2012) not providing any data that could be used for analysis.
See Figure 1 for a summary of the flow of study inclusion.
1.
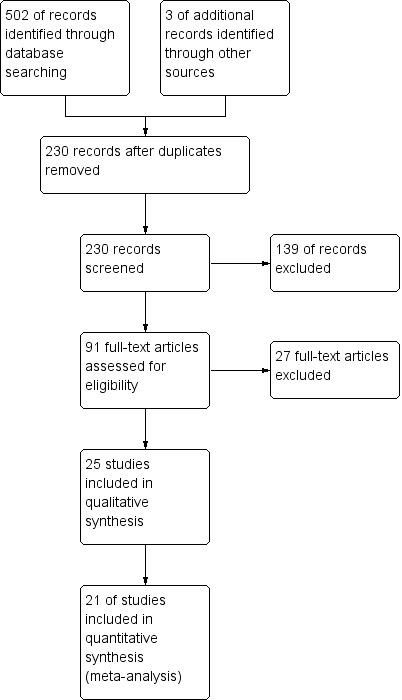
Study flow diagram (from searches conducted to April 2016).
In May 2018 a further update search identified 105 references. We de‐duplicated and dual‐screened these for eligibility. We found three published trial reports for studies previously listed as ongoing (Dimitropoulos 2014; Eisler 2006; Lock 2014), four new ongoing study protocols (Bilyk 2017; Carrot 2017; Hildebrandt 2016; Lock 2017) and 10 additional, companion papers matching the following included studies: Agras 2014; Herscovici 2017; Le Grange 2016; Madden 2015; Lock 2010.
A study protocol, previously listed as ongoing (NCT01579682) was confirmed by the trialist to match the included study Lock 2015.
We have incorporated only those studies identified from the April 2016 search into the current analyses. The three newly‐reported studies (Dimitropoulos 2014; Eisler 2006; Lock 2014) identified in 2018 have been added to those studies already awaiting classification, and will be incorporated at a later date, as appropriate. The results to Dimitropolous 2014 were published on ClinicalTrials.gov in July 2016 (NCT02106728).
Included studies
Participants
Please see Characteristics of included studies table for specific details of each included study. The UK was the location of eight of the trials, while four were conducted in the USA, three in Australia , and one in Canada. Seven trials were conducted in non‐English‐speaking countries including three trials in the Spanish‐speaking countries of Spain and Argentina, one in France, one in Italy, one in Germany and one in China. While not described in the trial report, personal correspondence revealed the trial by Besharat 2001 was located in the UK. In a further trial the location of the study was not explicitly stated, although author affiliation for this remaining study was listed as the USA (Lock 2015).
Most of the trials (16/25) reported using referrals to specialist eating disorder treatment units for recruitment. One trial recruited participants who had been admitted to the casualty ward of a hospital for malnutrition and medical compromise (Rhodes 2008). Three trials sought potential participants by sending letters to community care providers and schools, and publicised the trial using presentations and announcements (Herscovici 2017; Lock 2010; Robin 1999). Five trials provided no details about their recruitment strategy (Besharat 2001; Espina 2000; Li 2006; Lock 2015; Russell 1987).
Most trials were conducted on an outpatient basis. Twelve trials reported solely outpatient treatment, three reported that the selection of participants occurred whilst participants were receiving inpatient treatment, but that therapy began after discharge, two further trials involved the provision of outpatient therapy but investigators noted that some participants required hospitalisation during the trial. Five trials used both inpatient and outpatient treatment, and only one trial reported the provision of solely inpatient treatment (Whitney 2012). In two trials the treatment setting was not specified (Besharat 2001; Espina 2000).
Generally, most trials used some form of the DSM diagnostic criteria for the selection of participants with AN. Ten trials used the relevant DSM criteria of the era, e.g. DSM‐III, DSM‐IIIR or DSM‐IV, without variation, while a further three used these criteria, but removed the amenorrhoea requirement. Four trials used DSM criteria but included participants whose current body weight exceeded the diagnostic weight criterion of being less than 85% of their expected body weight. Thus, these trials may represent samples of people with a lower level of severity. One trial employed DSM diagnostic criteria, but excluded participants with a history of AN for more than 10 years, possibly representing a less chronic sample of participants. Two trials used both DSM‐IV and ICD 10 criteria, two trials used the diagnostic criteria of “Great Ormond Street”, while one used the Chinese Classification of Mental Disorders (CCMD‐3) criteria for anorexia. In two trials the method used to diagnose was not specified (Espina 2000; Hall 1987). In six trials, information about purging or restricting behaviour/subtype was reported.
Both the reporting of exclusion criteria and the types of exclusion criteria used were mixed. Nine trials provided no details about whether exclusion criteria were applied. Of the trials that provided details, five trials excluded participants on the basis of suicidal ideation/high suicide risk. Eleven excluded participants due to serious comorbid medical or psychiatric/psychological conditions. Three excluded participants who were currently receiving psychological therapy. Six trials also used upper or lower age limits or both for participants. As stated above, some reported exclusion criteria based on the chronicity of participants' AN while others excluded participants due to very low baseline body mass index (BMI)/average body weight (ABW) scores. One trial excluded male participants (Geist 2000).
There was some variation in the average ages and age ranges of trial participants. Sixteen trials included adolescent participants. Four trials included those between the ages of 18 and 23. One trial separated the treatment groups by age, with those 18 years and younger in two groups and those 19 years and over in another. Four trials comprised adult participants, with only one of these reporting an average age over 30 (Li 2006).
All but one study (Besharat 2001) provided information about gender. Most participants across these trials were female. Twelve trials included male participants. In all but one of these studies males did not exceed 12% of the total participants. In the remaining study (Li 2006) males comprised 43% of the sample.
The provision of details about the severity of participants' AN at baseline was mixed. Eight trials provided information about the age of onset of participants’ AN, while all but three provided information about the duration of the participants’ AN. Two trials reported no information about participants’ baseline weight. The remaining trials reported on weight in kilograms, in BMI, in ABW, in expected body weight (EBW), in ideal body weight (IBW) or percentile/percentage scores of these measures. Fourteen studies provided baseline BMI data. The average BMIs ranged between 14.9 and 17.3 across most trials, with the exception of Onnis 2012 (BMI averages of 14.5 and 14.2 across treatment groups) and Whitney 2012 (average baseline BMI of 13.3), with the Whitney study in particular potentially representing a more severe participant sample. Most studies (20) used an established eating disorder psychopathology scale (e.g. Morgan‐Russell Scales, Eating Attitudes Test) to indicate the severity of participants’ core eating disorder psychopathology at baseline. Twelve trials provided information about participants’ comorbid psychiatric diagnoses. Six trials had specified that co‐existing psychiatric conditions were part of their exclusion criteria. Eleven trials provided information about the living arrangements of the participants, such as whether they lived with their primary family unit, alone, with partners or in shared accommodation. Nine trials provided information about the educational/occupational background or social class of the participants or their families.
Interventions and comparisons
Four trials (Espina 2000; Godart 2012; Onnis 2012) compared family therapy approaches with standard care or treatment as usual. Six trials compared family therapy approaches with other psychological interventions, (cognitive behavioural therapy (CBT): Ball 2004; cognitive analytic therapy: Besharat 2001; psychotherapy: Besharat 2001; : individual supportive therapy/counselling: Besharat 2001; Russell 1987; and ego‐oriented individual therapy/adolescent‐focused therapy: Lock 2010; Robin 1999). Two trials compared family therapy approaches with educational interventions (Geist 2000 with family psychoeducation and Hall 1987 with psychoeducation). Twelve trials compared various family therapy approaches with each other (Agras 2014; Eisler 2000; Herpertz‐Dahlmann 2014; Herscovici 2017; Le Grange 1992; Le Grange 2016; Lock 2005; Lock 2015; Madden 2015; Rausch Herscovici 2006; Rhodes 2008; Whitney 2012). Two trials (Crisp 1991; Dare 2001) included multiple comparison arms, each a standard care or treatment as usual, and a psychological intervention (cognitive analytic therapy Dare 2001; psychotherapy Crisp 1991) were included in two separate comparisons, due to the use of multiple treatment conditions in each trial. Although Besharat 2001 had three comparative treatment arms in addition to a family therapy approach, the data were not provided in a format that was useable for analysis.
Most trials used family‐based treatment (and its variants, including short‐term, long‐term and separated) (Agras 2014; Ball 2004; Dare 2001; Eisler 2000; Herscovici 2017; Le Grange 1992; Le Grange 2016; Lock 2005; Lock 2010; Lock 2015; Madden 2015; Rausch Herscovici 2006; Rhodes 2008; Robin 1999; Russell 1987).Espina 2000 and Whitney 2012 used systems family therapy, while Onnis 2012 used structural family therapy. Seven trials deployed family therapy approaches that used family involvement, but did not provide specific details about the theoretical underpinning of the therapy and its procedures (Besharat 2001; Crisp 1991; Geist 2000; Godart 2012; Hall 1987; Herpertz‐Dahlmann 2014; Li 2006; Whitney 2012). We therefore categorised these approaches as Other family therapy approaches. Agras 2014 compared family‐based treatment with systems family therapy and Whitney 2012 compared systems family therapy with an approach classed as other.
Outcomes
We extracted the data we believed equivalent to remission, or similar to it, across the trials wherever possible. Several trials used close to equivalent definitions of 'good' and 'intermediate' response or outcome (Ball 2004; Eisler 2000; Godart 2012; Le Grange 1992; Russell 1987). Dare 2001 and Crisp 1991 used similar definitions but labelled these as 'recovered', 'significantly improved', 'well' and ‘nearly well'. For all these trials the best level of outcome included restoration of weight to within 85% of an average body weight, restoration of regular menstruation and absence of bulimic symptoms; the definition of the next level of outcome was restoration of weight to within 85% of an average body weight, menstruation may not have returned and/or occasional bulimic symptoms. Ball 2004 added an additional criterion, where participants had to have gained at least four kilograms. We combined the numbers of participants who met all of these levels (good, intermediate, recovered, significantly improved, well and nearly well) of outcome in each trial for the outcome 'remission’, based on Dare 2001, who stated that participants in all of these categories no longer met DSM‐IV criteria for AN. Other trials used remission criteria that were primarily based on weight‐derived outcomes (Agras 2014 95%+ IBW; Herpertz‐Dahlmann 2014 BMI; Lock 2005, 90%+ IBW; Lock 2015 and Herscovici 2017 95%+ EBW) or a combination of multiple outcome results (Le Grange 2016 95% mBMI + eating disorder examination (EDE) Global score < 1.59; Lock 2010 95% IBW + EDE score within 1 SD of global mean published norms; Madden 2015, > 95% EBW and a global EDE within 1 SD of published norms). Robin 1999 provided data for the remission outcome, the definition of which was the target weight set by the clinician. Hall 1987 and Besharat 2001 provided no definitions for their remission/recovered outcomes. Most of the trials that reported on the remission outcome therefore used different definitions of remission. In seven trials there were no data provided on remission, and no definition given for what this might equate to (Espina 2000; Geist 2000; Li 2006; Onnis 2012; Rausch Herscovici 2006; Rhodes 2008; Whitney 2012). Relapse was defined as the number of participants who had achieved remission (as defined above) during the trial, but were at a later point found no longer to meet the criteria for remission.
Of the trials that provided useable data from eating disorder psychopathology scale measures, the measures used were varied. Eight trials (Crisp 1991; Ball 2004; Dare 2001; Eisler 2000; Herscovici 2017; Le Grange 1992; Rausch Herscovici 2006; Russell 1987) used the Morgan‐Russell Assessment Schedule (Morgan 1988). Three trials (Eisler 2000; Le Grange 1992; Robin 1999) used the eating attitudes test (EAT; Garner 1979; Garner 1983). Six trials (Agras 2014; Le Grange 2016; Lock 2010; Lock 2015; Lock 2005; Madden 2015) used a version of the EDE (Cooper 1987b). However, as Lock 2005 only provided global EDE scores for follow‐up (not post‐intervention results) we used the other measure in this trial, the Yale‐Brown‐Cornell Eating Disorders Scale (Sunday 1995) total score, for the post‐intervention outcome in our analysis. Three trials used the eating disorders inventory (EDI) or EDI‐2 (Godart 2012; Herpertz‐Dahlmann 2014; Herscovici 2017). One trial (Whitney 2012) used the short evaluation of eating disorders (SEED) (Kordy 2005).
Nine trials measured family functioning. Of those that did, Le Grange 1992 and Eisler 2000 used the standardised clinical family interview (SCFI) (Kinston 1984), Expressed Emotions measure (Vaughn 1976), and FACES III (Olson 1979; Olson 1985), while Besharat 2001 used the SCFI alone. Robin 1999 used a scale called the general and eating‐related conflict scale (Robin 1990), and observed family conflict during interactions using a behaviour code for videotaped interactions. Geist 2000 used a general family functioning measure (Skinner 1991). Rausch Herscovici 2006 used the family health scale. Lock 2010 used the McMaster family assessment device (FAD). Whitney 2012 used several scales, of which the data are extracted from the level of expressed emotion scale (LEE) (Cole 1988). Onnis 2012 the Wiltwyck family task test. Of these, only Rausch Herscovici 2006 and Whitney 2012 provided outcome data in a useable format.
General functioning was rarely reported on. Only Godart 2012 reported useable general functioning outcome data with the global outcome assessment scale (GOAS: Morgan 1988; Jeammet 1991).
For evaluating weight outcomes, we used standard BMI scores whenever possible (Ball 2004; Godart 2012; Lock 2005; Lock 2015; Rausch Herscovici 2006; Robin 1999, Whitney 2012). Other measures that were used for analysis included BMI percentile (Lock 2010), percentage median BMI (Le Grange 2016), percentage ABW (Eisler 2000; Le Grange 1992; Russell 1987), percentage EBW (Herpertz‐Dahlmann 2014; Herscovici 2017) and percentage EBW change (Madden 2015). We have specified the measure used for weight for each analysis.
Excluded studies
See Characteristics of excluded studies table for reasons for excluding 27 trials.
Studies awaiting classification
See Characteristics of studies awaiting classification table for details on 10 studies awaiting classification.
Ongoing studies
See Characteristics of ongoing studies table for details of six ongoing trials.
New studies included in this update (to 8 April 2016)
New included studies found for this update were: Agras 2014; Besharat 2001; Godart 2012; Herpertz‐Dahlmann 2014; Herscovici 2017; Le Grange 2016; Li 2006; Lock 2010; Lock 2015; Madden 2015; Onnis 2012; Rhodes 2008; Whitney 2012, with details provided in the Characteristics of included studies table.
Risk of bias in included studies
For a summary of the risks of bias across the studies see Figure 2; and Figure 3. See the Study tables for full details.
2.
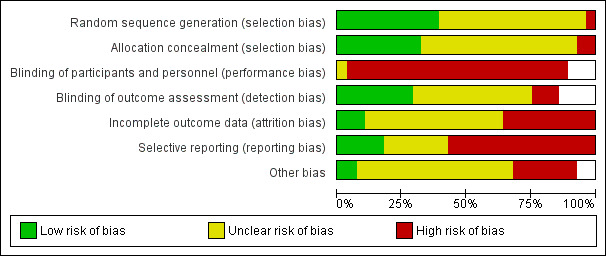
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
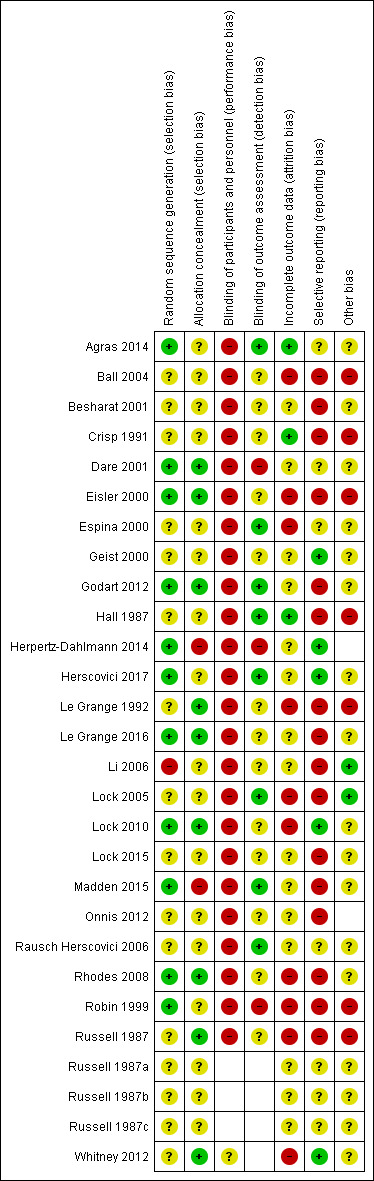
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
For most trials (13/25), no or unclear information was provided about whether a random sequence was generated for allocation or how this was generated, or both (Ball 2004; Besharat 2001; Crisp 1991; Espina 2000; Geist 2000; Hall 1987; Le Grange 1992; Lock 2005; Lock 2015; Onnis 2012; Rausch Herscovici 2006; Russell 1987; Whitney 2012). In 11 trials we considered the randomisation sequence to be adequately generated (Agras 2014; Dare 2001; Eisler 2000; Godart 2012; Herpertz‐Dahlmann 2014; Herscovici 2017; Le Grange 2016; Lock 2010; Madden 2015; Rhodes 2008; Robin 1999), while in one trial the generation of the randomisation sequence was inadequate (Li 2006). In two trials allocation was not adequately concealed (Herpertz‐Dahlmann 2014; Madden 2015), in nine trials we judged that allocation was adequately concealed (Dare 2001, Eisler 2000, Godart 2012, Le Grange 1992; Le Grange 2016, Lock 2010, Rhodes 2008, Russell 1987, Whitney 2012). In the remainder (14 trials) no or unclear information about concealment was provided.
Blinding
The blinding of participants and personnel to treatment is not possible for family therapy approaches. Blinding of outcome assessors is not possible for self‐reported outcomes, only for clinician‐rated outcomes. For clinician‐rated outcomes blinding was not carried out, or was unmasked, in three trials (Dare 2001; Herpertz‐Dahlmann 2014; Robin 1999), was carried out and maintained in six (Agras 2014; Espina 2000; Godart 2012; Herscovici 2017; Lock 2005; Madden 2015) and was unclear in the remaining 16 trials (Ball 2004; Besharat 2001; Crisp 1991; Eisler 2000; Geist 2000; Hall 1987; Le Grange 1992; Le Grange 2016; Li 2006; Lock 2010; Lock 2015; Onnis 2012; Rausch Herscovici 2006; Rhodes 2008; Russell 1987; Whitney 2012).
Incomplete outcome data
We considered a trial to have adequately addressed incomplete data (i.e. low risk of bias) if both the amount of missing data was clearly reported, and an intention‐to‐treat analysis was undertaken. This was the case in three trials (Agras 2014; Crisp 1991; Hall 1987). We considered the method in which incomplete outcome data were addressed to be unclear if there were inconsistencies in the numbers of dropouts or treatment group numbers throughout the paper, if the details reported about the dropouts was unclear (e.g. which treatment group they were in), if the method of analysis (e.g. intention‐to‐treat, last observation carried forward, observed case) was unclear, and if there were more than 15% missing data for any outcome measures (Besharat 2001; Dare 2001; Geist 2000; Godart 2012; Herpertz‐Dahlmann 2014; Herscovici 2017; Le Grange 2016; Li 2006; Lock 2015; Madden 2015; Onnis 2012; Whitney 2012). We rated trials at high risk of attrition bias if they did not report any details on dropouts, or if dropouts occurred and intention‐to‐treat analysis did not appear to have been undertaken on at least one or more outcome measure (Ball 2004; Eisler 2000; Espina 2000; Le Grange 1992; Lock 2005; Lock 2010; Rausch Herscovici 2006; Rhodes 2008; Robin 1999; Russell 1987).
Selective reporting
Selective reporting bias includes the lack of reporting of the data from an outcome measure that was stated to have been collected, and follow‐up data reported to have been collected but not reported. We judged 16 studies to have some form of reporting bias (Ball 2004; Besharat 2001; Crisp 1991; Dare 2001; Eisler 2000; Godart 2012; Le Grange 1992; Le Grange 2016; Li 2006; Lock 2005; Lock 2015; Madden 2015; Onnis 2012; Rhodes 2008; Robin 1999; Russell 1987), while in five the level of selective reporting bias was unclear (Agras 2014; Espina 2000; Hall 1987; Rausch Herscovici 2006), and the risk of bias was low in five studies.
Other potential sources of bias
We found other potential sources of bias. These included baseline group imbalances for particular core characteristics (Agras 2014; Ball 2004; Crisp 1991; Dare 2001; Hall 1987; Herpertz‐Dahlmann 2014; Herscovici 2017; Le Grange 1992; Robin 1999; Russell 1987), inconsistencies between the description of the results in the text, and the actual outcome data given in tables (Ball 2004; Crisp 1991; Dare 2001), and inconsistencies in the participant numbers reported for various outcome measures throughout trials (Besharat 2001; Dare 2001; Robin 1999; Russell 1987). Other problems included small sample sizes with a number of studies containing fewer than 30 participants (Ball 2004; Geist 2000; Herscovici 2017; Le Grange 1992; Onnis 2012; Rausch Herscovici 2006; Rhodes 2008); uneven or unspecified treatment dosages/durations (Besharat 2001; Crisp 1991; Dare 2001; Godart 2012; Herpertz‐Dahlmann 2014; Herscovici 2017; Robin 1999; Russell 1987), the use of within‐group analysis (Hall 1987; Robin 1999); no or very little between‐group analysis reported (Besharat 2001; Robin 1999; Russell 1987), and potential contamination from the same therapist(s) conducting both types of therapy (Dare 2001; Eisler 2000; Russell 1987).
Overall, there appeared to be considerable risks of bias in the included studies.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings for the main comparison. Family therapy compared to standard care/treatment as usual for anorexia nervosa.
| Family therapy compared to standard care/treatment as usual for anorexia nervosa | |||||
|
Participants: People of any age or gender with a primary clinical diagnosis of anorexia nervosa (AN) Intervention: Family therapy Comparator: Standard care/treatment as usual | |||||
| Outcomes | № of participants (studies) Follow up | Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | |
| Risk with standard care/treatment as usual | Risk difference with family therapy | ||||
| Remission post‐intervention | 81 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b | RR 3.83 (1.60 to 9.13) | Study population | |
| 128 per 1000 | 363 more per 1000 (77 more to 1042 more) | ||||
| Remission at long‐term follow‐up | 41 (1 RCT) | ⊕⊕⊝⊝ LOWc,d | RR 6.09 (0.33 to 110.84) | Study population | |
| 0 per 1000 | 0 fewer per 1000 (0 fewer to 0 fewer) | ||||
| Mortality at long‐term follow‐up | 0 (0 studies) | ‐ | not pooled | Study population | |
| not pooled | not pooled | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
aEvidence downgraded by one level for unclear risk of selection bias due to inadequate reporting of random sequence generation and allocation concealment in one study. Evidence also downgraded for high or unclear risk of performance and detection bias across studies. Evidence also downgraded for high risk of reporting bias due to selective reporting across both studies (some data not reported), including uneven treatment doses, participants crossing over groups and reporting anomalies. bEvidence downgraded by one level for imprecision, as there are only two trials with a total of 81 participants and wide confidence intervals. cEvidence downgraded by one level for high risk of performance bias and detection bias. Some discrepancy in numbers reported in dropouts. dEvidence downgraded by one level for imprecision as there was only one trial with 41 participants.
Summary of findings 2. Family therapy compared to psychological interventions for anorexia nervosa.
| Family therapy compared to psychological interventions for anorexia nervosa | |||||
|
Participants: People of any age or gender with a primary clinical diagnosis of anorexia nervosa (AN) Intervention: Family therapy Comparator: Psychological interventions | |||||
| Outcomes | № of participants (studies) Follow up | Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | |
| Risk with psychological interventions | Risk difference with Family therapy | ||||
| Remission post‐intervention | 252 (5 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b,c | RR 1.22 (0.89 to 1.67) | Study population | |
| 488 per 1000 | 107 more per 1000 (54 fewer to 327 more) | ||||
| Remission at long‐term follow‐up | 200 (4 RCTs) | ⊕⊝⊝⊝ VERY LOWa,d,e | RR 1.08 (0.91 to 1.28) | Study population | |
| 703 per 1000 | 56 more per 1000 (63 fewer to 197 more) | ||||
| All‐cause mortality ‐ long‐term outcome | 0 ( studies) | ‐ | not pooled | Study population | |
| not pooled | not pooled | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
aEvidence downgraded by one level due to high risk of selection bias in studies, arising from inadequate reporting of random sequence generation or allocation concealment. Evidence was also downgraded due to high risk of performance bias across all trials and often high risk of detection bias; there were several instances of reporting anomalies, some instances of missing data (at times high: up to 29.5% in one trial) not being adequately dealt with; and difficulties with outcomes being reported by subgroup or by total (in contrast to what was described in methods), or data from outcome measures not being reported at all. bEvidence downgraded by one level for inconsistency, as although heterogeneity was 37% and potentially not considered serious, the direction of effects variously favoured family therapy and psychological therapy. cEvidence downgraded by one level for imprecision, as the small effect observed was based on only five trials with 252 participants with wide confidence intervals that cross the line of no effect. dEvidence downgraded by one level for inconsistency, as although heterogeneity was 0%, the direction of effects variously favoured family therapy and psychological therapy. eEvidence downgraded by one level for imprecision, as the small effect observed was based on only four trials with 200 participants with wide confidence intervals that cross the line of no effect.
Summary of findings 3. Family therapy compared to educational interventions for anorexia nervosa.
| Family therapy compared to educational interventions for anorexia nervosa | |||||
|
Participants: People of any age or gender with a primary clinical diagnosis of anorexia nervosa (AN) Intervention: Family therapy Comparator: Educational interventions | |||||
| Outcomes | № of participants (studies) Follow up | Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | |
| Risk with educational interventions | Risk difference with Family therapy | ||||
| Remission at long‐term follow‐up ‐ other | 30 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b,c | RR 9.00 (0.53 to 153.79) | Study population | |
| 0 per 1000 | 0 fewer per 1000 (0 fewer to 0 fewer) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
aEvidence downgraded by one level for unclear risk of selection bias, due to inadequate reporting of random sequence generation and allocation concealment and also downgraded due to high risk of performance bias. bEvidence downgraded by one level for imprecision, as there was only one trial. cEvidence downgraded by one level for inconsistency, due to wide confidence intervals.
Comparison 1: Family therapy approaches versus standard care/treatment as usual
Four trials (286 participants) compared family therapy approaches with treatment as usual. Dare 2001 used family‐based therapy, Espina 2000 used a systems approach, and Crisp 1991 and Godart 2012 used more general forms of family therapy, which we classified under the Other family therapy approaches category. We classed three of the trials as being in adult populations (Crisp 1991; Dare 2001; Espina 2000) and one as a trial in an adolescent population (Godart 2012).
Primary outcomes
Remission
Two trials reported on remission post‐intervention (Crisp 1991; Dare 2001). There was some evidence that family therapy approaches may improve the rates of remission post‐intervention compared to standard care/treatment as usual groups (risk ratio (RR) 3.50, 95% confidence interval (CI) 1.49 to 8.23 (RR 3.50, 95% CI 1.49 to 8.23; participants = 81; I2 = 0%)) Analysis 1.1). Only one of these trials (Dare 2001) collected data on remission at long‐term follow‐up (12 months +), with no differences between groups in rates of remission and very wide confidence intervals (RR 6.09, 95% CI 0.33 to 110.84, 41 participants; Analysis 1.2).
1.1. Analysis.
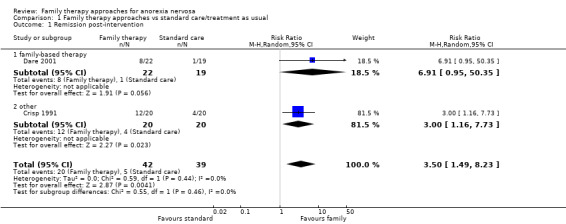
Comparison 1 Family therapy approaches vs standard care/treatment as usual, Outcome 1 Remission post‐intervention.
1.2. Analysis.
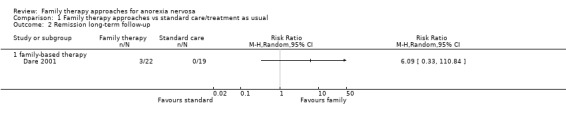
Comparison 1 Family therapy approaches vs standard care/treatment as usual, Outcome 2 Remission long‐term follow‐up.
Both of these trials were undertaken in adults so we are unclear about the impact on adolescents.
All‐cause mortality
Dare 2001 reported on mortality, stating that there was one participant from the standard care/treatment as usual group who died during the treatment phase. One death was reported following randomisation, but prior to the start of treatment in Crisp 1991, in the outpatient group therapy condition (this arm of the trial was not used in the review).
Secondary outcomes
Functioning
No trials reported on family functioning. However, Godart 2012 reported on general functioning, with little evidence that family therapy approaches improved family functioning compared with standard care/treatment as usual (mean difference (MD) 0.50, 95% CI −0.62 to 1.62, 59 participants; Analysis 1.3). Given only one trial of adolescents reporting on this outcome, we were unable to conduct subgroup analysis based on age.
1.3. Analysis.
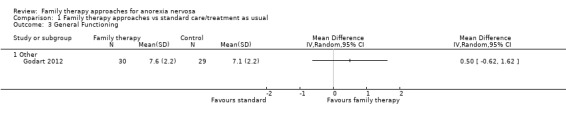
Comparison 1 Family therapy approaches vs standard care/treatment as usual, Outcome 3 General Functioning.
Dropouts
Three trials reported on dropouts during therapy (Dare 2001; Espina 2000; Godart 2012), with no evidence of a difference between family therapy approaches and standard care/treatment as usual (RR 1.01, 95% CI 0.44 to 2.34; participants = 137); Analysis 1.4).
1.4. Analysis.
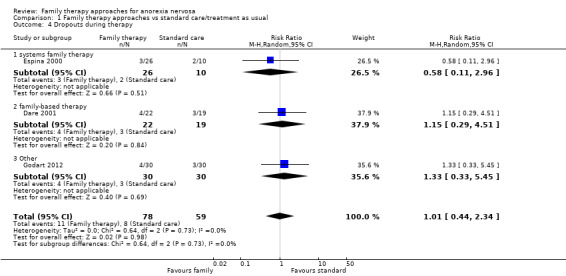
Comparison 1 Family therapy approaches vs standard care/treatment as usual, Outcome 4 Dropouts during therapy.
There was no evidence that age group modified the effect of family therapy approaches, compared with standard therapy post‐intervention for dropouts (Chi2 = .06; df = 1; P = 0.81; Analysis 13.4).
13.4. Analysis.
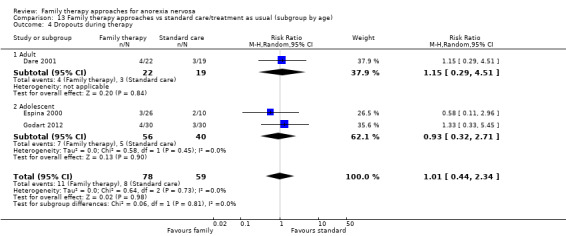
Comparison 13 Family therapy approaches vs standard care/treatment as usual (subgroup by age), Outcome 4 Dropouts during therapy.
Eating disorder psychopathology
Two trials (Crisp 1991; Godart 2012) reported scores with little evidence for an effect of family therapy approaches on eating disorder psychopathology outcomes (standardised mean difference (SMD) −0.11, 95% CI −0.49 to 0.27, I2 = 0%, 109 participants; Analysis 1.5) compared with standard care/treatment as usual, post‐intervention.
1.5. Analysis.
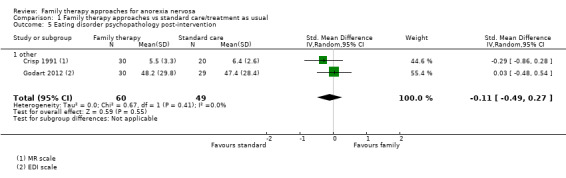
Comparison 1 Family therapy approaches vs standard care/treatment as usual, Outcome 5 Eating disorder psychopathology post‐intervention.
There was no evidence that age group modified the effect of family therapy approaches, compared with standard therapy post‐intervention (Chi2 = .67; df = 1; P = 0.41; Analysis 13.5).
13.5. Analysis.
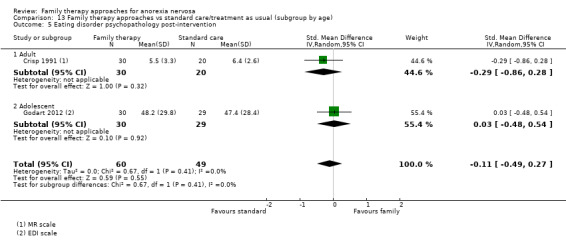
Comparison 13 Family therapy approaches vs standard care/treatment as usual (subgroup by age), Outcome 5 Eating disorder psychopathology post‐intervention.
Weight
One trial (Godart 2012) reported on BMI weight outcomes, with little evidence for an effect of family therapy approaches compared with standard care/treatment as usual (MD 0.40, 95% CI 0.−75 to 1.55, 59 participants; Analysis 1.6).
1.6. Analysis.
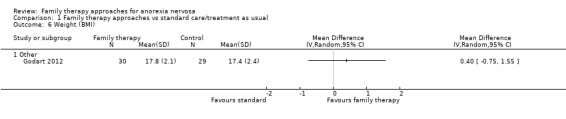
Comparison 1 Family therapy approaches vs standard care/treatment as usual, Outcome 6 Weight (BMI).
Given only one trial of adolescents reporting on this outcome, we were unable to conduct subgroup analysis based on age.
Relapse
Two trials (Dare 2001; Godart 2012) reported on relapse, and while the effect favoured family therapy approaches compared with standard care/treatment as usual, this did not reach statistical significance (RR 0.65, 95% CI 0.37 to 1.15; participants = 100); Analysis 1.7).
1.7. Analysis.
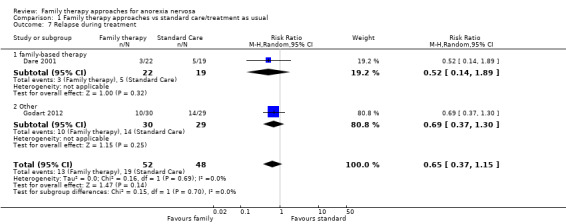
Comparison 1 Family therapy approaches vs standard care/treatment as usual, Outcome 7 Relapse during treatment.
There was no evidence that age group modified the effect of family therapy approaches, compared with standard therapy post‐intervention (Chi2 = .15; df = 1; P = 0.70; Analysis 13.7).
13.7. Analysis.
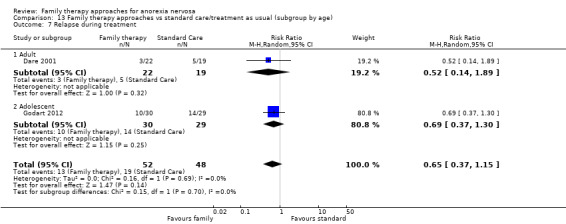
Comparison 13 Family therapy approaches vs standard care/treatment as usual (subgroup by age), Outcome 7 Relapse during treatment.
Comparison 2: Family therapy approaches versus psychological interventions
Six trials (414 participants) compared family therapy approaches with psychological interventions. Five trials used family‐based therapy (Ball 2004; Dare 2001; Lock 2010; Robin 1999; Russell 1987). One trial (Crisp 1991) described more general family therapy embedded into individual outpatient work, categorised as Other family therapy. The participants in the Russell 1987 trial were grouped by age of onset and duration of illness. The comparison group in Russell 1987 was individual supportive therapy, in Robin 1999 and Lock 2010 ego‐oriented individual therapy/adolescent‐focused therapy, in Crisp 1991 group sessions of more general psychotherapy, in Ball 2004 CBT, and in Dare 2001 cognitive analytical group was used as a comparator (rather than the psychoanalytic psychotherapy arm).
Primary outcomes
Remission
Five trials reported on remission post‐intervention (all but Crisp 1991), with Russell 1987 reporting results for their three subgroups separately. While the effect favoured family therapy approaches compared with other psychological therapies, this did not reach statistical significance (RR 1.22, 95% CI 0.89 to 1.67; I2 = 37%, 252 participants; Analysis 2.1). Only one study (Lock 2010) reported follow‐up rates for remission at short‐term follow‐up (less than 12 months), favouring family therapy approaches but showing no statistically significant difference between groups (RR 1.16, 95% CI 0.94 to 1.44, 89 participants; Analysis 2.2). Similarly, the results for remission from four studies at long‐term follow‐up showed the same pattern (Ball 2004; Lock 2010; Robin 1999; Russell 1987) (RR 1.08, 95% CI 0.91 to 1.28; I2 = 0%, 200 participants; Analysis 2.3).
2.1. Analysis.
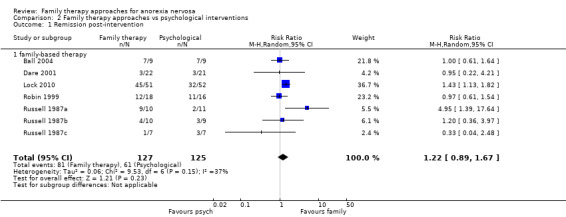
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 1 Remission post‐intervention.
2.2. Analysis.
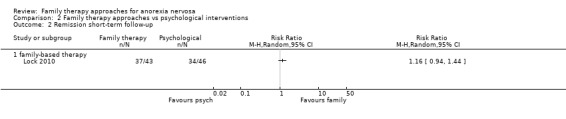
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 2 Remission short‐term follow‐up.
2.3. Analysis.
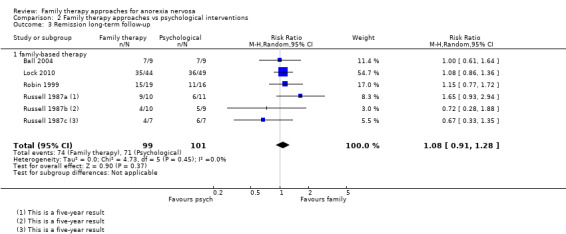
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 3 Remission long‐term follow‐up.
There was little evidence that age group modified the effect of family therapy approaches, compared with psychological therapies post‐intervention (Chi2 = .62; df = 1; P = 0.43; Analysis 14.1). At short‐term follow‐up there was only one trial in an adolescent population. At long‐term follow‐up, while effect sizes favoured psychological therapies for adults, and family therapy approaches for adolescents, there was no evidence that age group modified the effect (Chi2 = 2.67; df = 1; P = 0.10; Analysis 14.3).
14.1. Analysis.
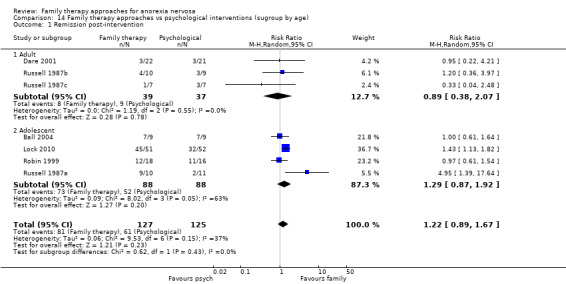
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 1 Remission post‐intervention.
14.3. Analysis.
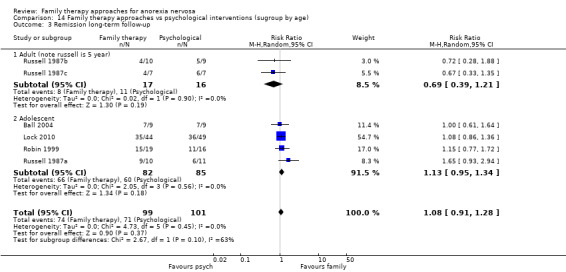
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 3 Remission long‐term follow‐up.
All‐cause mortality
Three trials (Crisp 1991; Dare 2001; Russell 1987) reported on mortality. Russell 1987 stated that there were no deaths at the post‐intervention assessment. The paper reporting follow‐up (Eisler 1997) stated that by five‐year follow‐up three participants had died, but does not state to which treatment group they belonged. No participants in the family therapy approaches or individual psychological treatment group had died in Dare 2001. As above, one death was reported following randomisation but prior to treatment in Crisp 1991, in the outpatient group therapy condition.
Secondary outcomes
Functioning
None of the six trials reported useable data on family or general functioning.
Dropouts
Four trials reported on dropouts during therapy (Ball 2004; Dare 2001; Lock 2010; Russell 1987), with little evidence of a difference in the number of dropouts between those receiving family therapy approaches and those receiving psychological interventions (RR 1.13, 95% CI 0.46 to 2.78; I2 = 46%, 229 participants; Analysis 2.4).
2.4. Analysis.
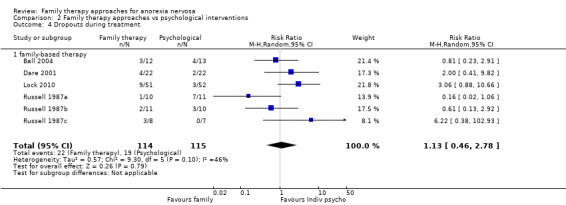
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 4 Dropouts during treatment.
There was little evidence that age group modified the effect of family therapy approaches, compared with psychological therapies post‐intervention (Chi2 = .30; df = 1; P = 0.58; Analysis 14.4).
14.4. Analysis.
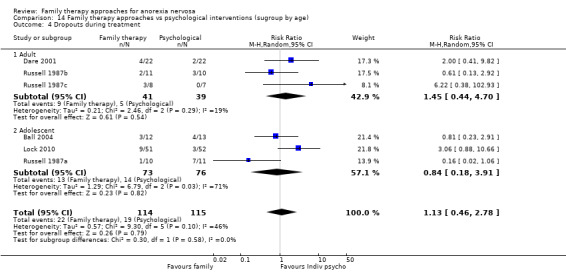
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 4 Dropouts during treatment.
Eating disorder psychopathology
We combined the Morgan‐Russell data from Ball 2004, Crisp 1991 and Russell 1987 (reported separately in three subgroups; these data are reported in Eisler 2008) with the EAT data from Robin 1999, and the EDE data from Lock 2010. There was little evidence of an effect of family therapy approaches compared with psychological interventions on these measures (SMD 0.17, 95% CI −0.32 to 0.66, 262 participants; Analysis 2.5).
2.5. Analysis.
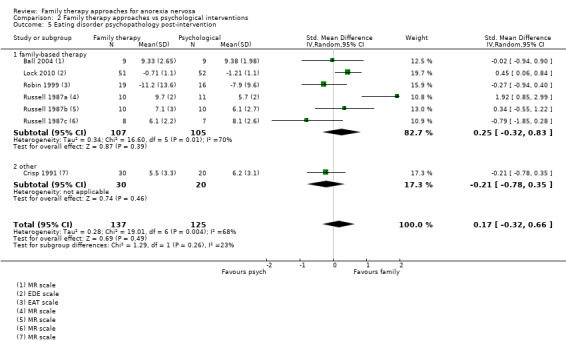
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 5 Eating disorder psychopathology post‐intervention.
One trial (Lock 2010) reported on eating disorder psychopathology at less than 12 months follow‐up, with little evidence of a difference between family‐based therapy versus the psychological intervention (ego‐oriented individual therapy/adolescent‐focused therapy) (MD −0.23, 95% CI −0.69 to 0.23, 89 participants; Analysis 2.6). Four trials (Ball 2004; Lock 2010; Robin 1999; Russell 1987 (reported separately in three subgroups; these data are reported in Eisler 1997)) measured eating disorder psychopathology at long‐term follow‐up (more than 12 months), with the longest follow‐up time point taken for each trial. Again, there was little evidence of a difference, with effect sizes in various directions and moderate heterogeneity between those who received family therapy approaches and those who received other psychological interventions (SMD −0.01, 95% CI −0.50 to 0.47; I2 = 57%, 197 participants; Analysis 2.7).
2.6. Analysis.
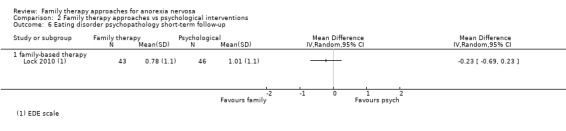
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 6 Eating disorder psychopathology short‐term follow‐up.
2.7. Analysis.
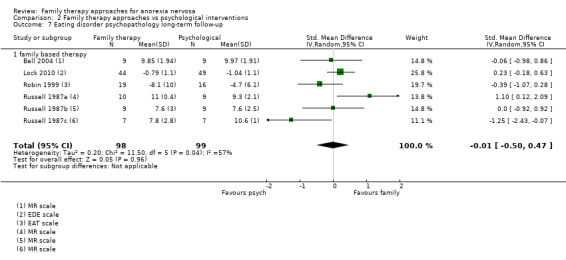
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 7 Eating disorder psychopathology long‐term follow‐up.
Post‐intervention, while effect sizes favoured psychological therapies for adults and family therapy approaches for adolescents, there was little evidence that age group modified the effect (Chi2 = 1.87; df = 1; P = 0.17; Analysis 14.5). At short‐term follow‐up there was only one trial in an adolescent population. At long‐term follow‐up, again while effect sizes favoured psychological therapies for adults and family therapy approaches for adolescents, there was little evidence that age group modified the effect post‐intervention (Chi2 = 1.17; df = 1; P = 0.28; Analysis 14.7).
14.5. Analysis.

Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 5 Eating disorder psychopathology post‐intervention.
14.7. Analysis.
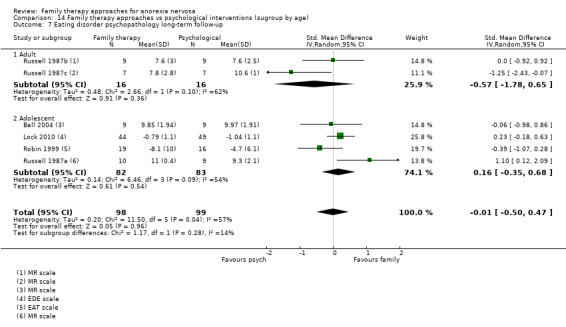
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 7 Eating disorder psychopathology long‐term follow‐up.
Weight
Four trials (Ball 2004; Lock 2010; Robin 1999; Russell 1987) reported on weight at the end of intervention (BMI, BMI percentile, ABW percentage), with some evidence that family therapy approaches resulted in greater improvements in weight than psychological therapy (SMD 0.32, 95% CI 0.01 to 0.63; participants = 210); Analysis 2.8). The one trial reporting on this (Lock 2010) found no difference in weight (BMI percentile) at short‐term follow‐up (MD 2.30, 95% CI ‐7.28 to 11.88); Analysis 2.9). Four trials (Ball 2004; Lock 2010; Robin 1999; Russell 1987) reported on weight at long‐term follow‐up (BMI, BMI percentile, ABW percentage), and while the effects were in the same direction as at the end of intervention, the effect was no longer statistically significant (SMD 0.14, 95% CI −0.16 to 0.45; I2 = 7%, 198 participants; Analysis 2.10).
2.8. Analysis.
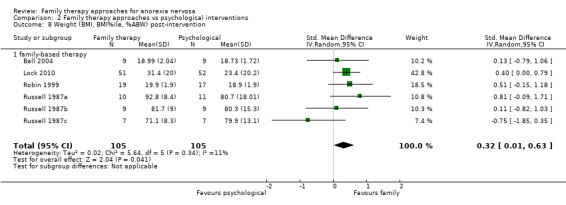
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 8 Weight (BMI, BMI%ile, %ABW) post‐intervention.
2.9. Analysis.
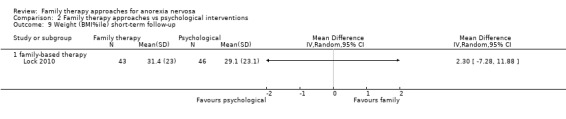
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 9 Weight (BMI%ile) short‐term follow‐up.
2.10. Analysis.
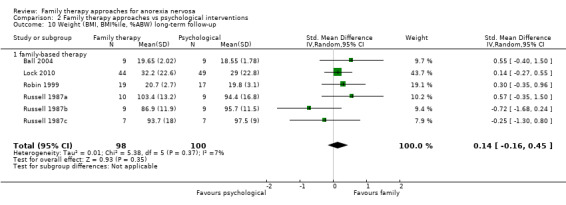
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 10 Weight (BMI, BMI%ile, %ABW) long‐term follow‐up.
Post‐intervention, while effect sizes favoured psychological therapies for adults and family therapy approaches for adolescents, there was not enough evidence to demonstrate that age group modified the effect (Chi2 = 2.45; df = 1; P = 0.12; Analysis 14.8). At short‐term follow‐up there was only one trial of an adolescent population. At long‐term follow‐up, there were statistically non‐significant results favouring psychological therapy for adults in the two trial arms in Russell 1987 (SMD −0.50, 95% CI −1.21 to 0.21; I2 = 0%) and favouring family therapy approaches for adolescents in four trials (SMD 0.27, 95% CI −0.04 to 0.57; I2 = 0%), with evidence that age group modified the treatment effect (Chi2 = 3.82; df = 1; P = 0.05; Analysis 14.10).
14.8. Analysis.
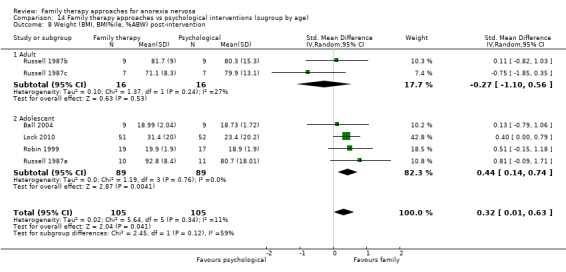
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 8 Weight (BMI, BMI%ile, %ABW) post‐intervention.
14.10. Analysis.
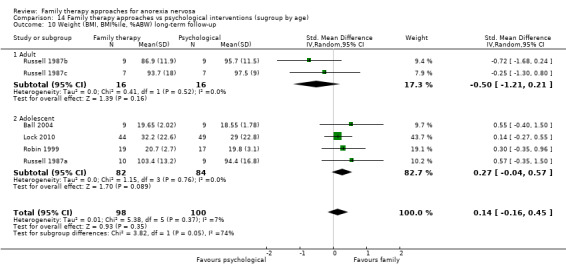
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 10 Weight (BMI, BMI%ile, %ABW) long‐term follow‐up.
Relapse
Two trials (Dare 2001; Russell 1987; reported separately in three subgroups) reported on relapse at end of treatment, with little evidence of a difference between family therapy approaches and psychological interventions (RR 1.06, 95% CI 0.54 to 2.08, I2 = 0%, 101 participants Analysis 2.11).
2.11. Analysis.
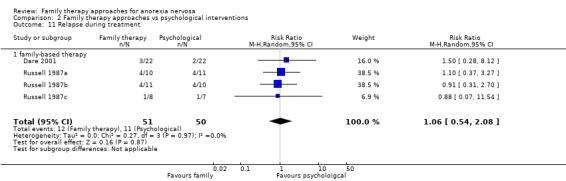
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 11 Relapse during treatment.
One trial (Lock 2010) reported on relapse at long‐term follow‐up, with evidence of a difference between groups (RR 2.49, 95% CI 0.55 to 11.21, 77 participants; Analysis 2.12).
2.12. Analysis.
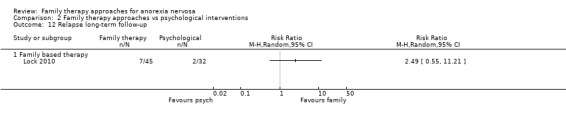
Comparison 2 Family therapy approaches vs psychological interventions, Outcome 12 Relapse long‐term follow‐up.
Post‐intervention, there was little evidence that age group modified the effect (Chi2 = .01; df = 1; P = 0.93; Analysis 14.11), and there was only one trial reported in an adolescent population at long‐term follow‐up.
14.11. Analysis.
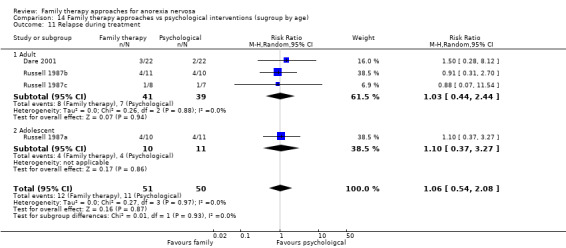
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 11 Relapse during treatment.
Comparison 3: Family therapy approaches vs educational interventions
There was one trial (Hall 1987; 30 participants) comparing family therapy approaches with an educational intervention. The trial compared a combination of individual and family work (categorised as Other family therapy) to dietary advice.
Primary outcomes
Remission
There were no data on remission post‐intervention. At short‐term follow‐up (9 months) there was little evidence, with very wide confidence intervals, that there was a difference between a family therapy approach and those receiving dietary advice in the percentage of participants who recovered (RR 9.00, 95% CI 0.53 to 153.79; participants = 30), Analysis 3.1).
3.1. Analysis.
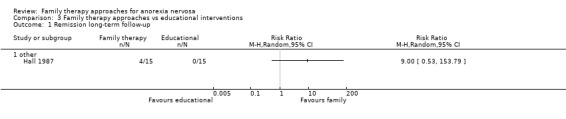
Comparison 3 Family therapy approaches vs educational interventions, Outcome 1 Remission long‐term follow‐up.
All‐cause mortality
Mortality was not reported.
Secondary outcomes
Functioning
There were no useable data reported on family or general functioning.
Dropouts
There were no dropouts reported in either intervention group.
Eating disorder psychopathology
There were no useable data reported on eating disorder psychopathology outcomes.
Weight
Weight was not reported as an outcome.
Relapse
There were no data on relapse reported.
Comparison 4: Short‐term versus long‐term family therapy approaches
Efficacy outcomes
One trial (Lock 2005; 86 participants) examined the effectiveness of six‐month (short‐term) compared with 12‐month (long‐term) family‐based therapy.
Primary outcomes
Remission
The data on remission post‐intervention were not reported. At follow‐up (mean 3.96 years) there was little evidence of any difference in the percentage of participants who recovered between those who received short‐term and those who received long‐term family‐based therapy (RR 0.95, 95% CI 0.80 to 1.12, 71 participants; Analysis 4.1) .
4.1. Analysis.
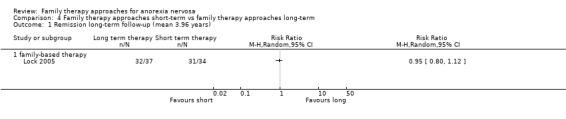
Comparison 4 Family therapy approaches short‐term vs family therapy approaches long‐term, Outcome 1 Remission long‐term follow‐up (mean 3.96 years).
All‐cause mortality
Mortality was not reported.
Secondary outcomes
Functioning
Lock 2005 examined attending school or work as a way of estimating general functioning; there was little evidence of any difference in functioning at follow‐up between those receiving short‐term and those receiving long‐term family‐based therapy (RR 1.03, 95% CI 0.95 to 1.12, 71 participants; Analysis 4.2).
4.2. Analysis.
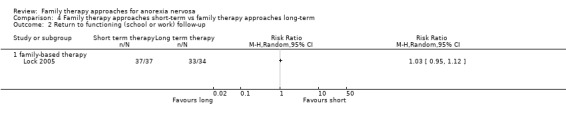
Comparison 4 Family therapy approaches short‐term vs family therapy approaches long‐term, Outcome 2 Return to functioning (school or work) follow‐up.
Dropouts
There was little evidence of any difference in the rate of dropouts during therapy between the group receiving short‐term and long‐term family‐based therapy (RR 3.67, 95% CI 0.81 to 16.66, 86 participants; Analysis 4.3).
4.3. Analysis.
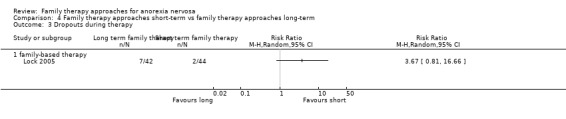
Comparison 4 Family therapy approaches short‐term vs family therapy approaches long‐term, Outcome 3 Dropouts during therapy.
Eating disorder psychopathology
At follow‐up, the EDE scale scores were provided and there was little evidence of any difference between the short‐term and long‐term family‐based therapy groups (MD −0.43, 95% CI −1.23 to 0.37, 35 participants; Analysis 4.4).
4.4. Analysis.
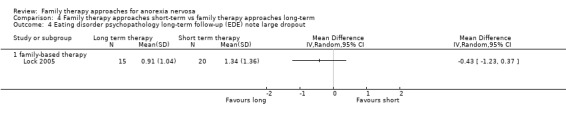
Comparison 4 Family therapy approaches short‐term vs family therapy approaches long‐term, Outcome 4 Eating disorder psychopathology long‐term follow‐up (EDE) note large dropout.
Weight
There was little evidence of differences in BMI between the groups receiving short‐term and long‐term family‐based therapy at the end of treatment (MD 0.50, 95% CI −0.43 to 1.43, 86 participants; Analysis 4.5) or at follow‐up (MD 0.17, 95% CI −0.83 to 1.17, 71 participants; Analysis 4.6).
4.5. Analysis.
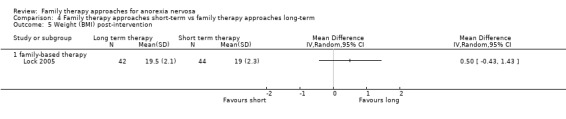
Comparison 4 Family therapy approaches short‐term vs family therapy approaches long‐term, Outcome 5 Weight (BMI) post‐intervention.
4.6. Analysis.
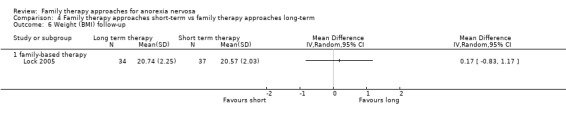
Comparison 4 Family therapy approaches short‐term vs family therapy approaches long‐term, Outcome 6 Weight (BMI) follow‐up.
Relapse
There was little evidence of differences in relapse during therapy between the groups receiving short‐term and long‐term family‐based therapy (RR 0.94, 95% CI 0.43 to 2.09, 86 participants; Analysis 4.7).
4.7. Analysis.
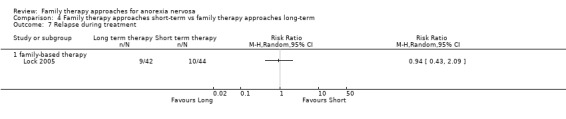
Comparison 4 Family therapy approaches short‐term vs family therapy approaches long‐term, Outcome 7 Relapse during treatment.
Comparison 5: Conjoint family therapy approaches versus separated family therapy approaches
Three trials (Eisler 2000; Le Grange 1992; Le Grange 2016) compared conjoint family‐based therapy, where the family and the participant were seen together, with separated family‐based therapy, where the family and participant were seen separately, with a total of 165 participants. In all cases family‐based therapy was the approach used.
Primary outcomes
Remission
Two studies reported on remission post‐intervention (Eisler 2000; Le Grange 2016), with some evidence to show rates might be higher for those in the separated family‐based therapy condition (RR 0.56, 95% CI 0.38 to 0.83; participants = 134; I2 = 0%); Analysis 5.1). The direction of effect was consistent across short‐term (only one study; Le Grange 2016) (RR 0.48, 95% CI 0.28 to 0.84;, 74 participants; Analysis 5.2) and long‐term follow‐up, but by long‐term follow‐up the effect was no longer statistically significant (RR 0.86, 95% CI 0.67 to 1.09; participants = 100; I2 = 0%); Analysis 5.3) (Eisler 2000; Le Grange 2016).
5.1. Analysis.
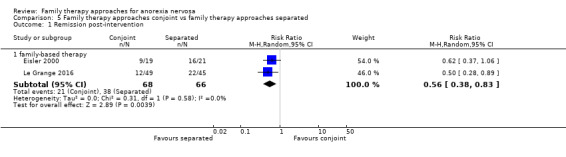
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 1 Remission post‐intervention.
5.2. Analysis.
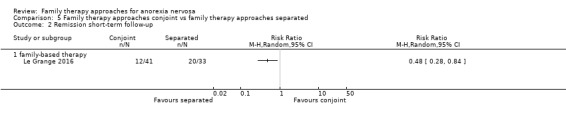
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 2 Remission short‐term follow‐up.
5.3. Analysis.
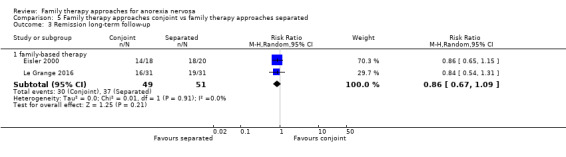
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 3 Remission long‐term follow‐up.
All‐cause mortality
Only Eisler 2000 reported on mortality, stating that there were no deaths in either of their treatment groups during treatment or over the five years of follow‐up.
Secondary outcomes
Functioning
Neither trial reported useable data on family or general functioning.
Dropouts
Eisler 2000 and Le Grange 2016 reported on dropout numbers at the end of treatment, with little evidence that there was any difference in the number of dropouts between those receiving conjoint family‐based therapy and those receiving separately‐based family therapy (RR 1.26, 95% CI 0.60 to 2.68; participants = 134; I2 = 0%); Analysis 5.4). Eisler 2000 reported long‐term (five‐year) follow‐up dropouts and found no difference between the groups, but with very large confidence intervals suggesting that the effect size could not be reliably established (RR 1.11, 95% CI 0.07 to 16.49, 38 participants; Analysis 5.5).
5.4. Analysis.
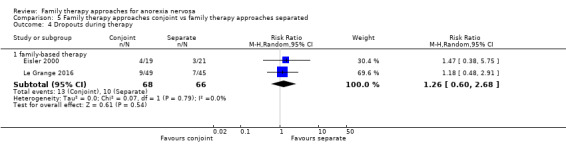
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 4 Dropouts during therapy.
5.5. Analysis.
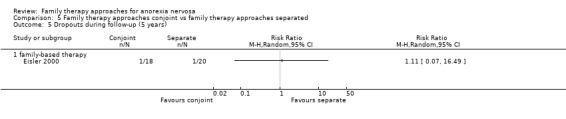
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 5 Dropouts during follow‐up (5 years).
Eating disorder psychopathology
A large range of eating disorder scale measures were used to assess eating disorder psychopathology, including the EAT, Morgan‐Russell Scales, EDI and EDE, across the three studies. There was little evidence of difference in outcomes between conjoint and separated family‐based therapy across any of these measures, and notable that the confidence intervals are often very wide, suggesting that the effect size can not be reliably estimated. This included Eisler 2000 and Le Grange 1992 EAT scores at the end of treatment (MD −1.85, 95% CI −10.01 to 6.31, 58 participants; Analysis 5.6), Eisler 2000 EAT long‐term follow‐up (five years) data (MD 4.40, 95% CI −25.72 to 34.52, 14 participants; Analysis 5.7), Eisler 2000 and Le Grange 1992 post‐intervention Morgan‐Russell scales scores (MD −0.96, 95% CI −1.95 to 0.03, 58 participants; Analysis 5.8), Eisler 2000 post‐intervention EDI scores (MD −10.50, 95% CI −26.96 to 5.96, 40 participants; Analysis 5.9) and long‐term follow‐up EDI scores (MD −7.90, 95% CI −37.73 to 21.93, 20 participants; Analysis 5.10), as well as Le Grange 2016 EDE scores at post‐intervention (MD 0.29, 95% CI −0.22 to 0.80, 94 participants; Analysis 5.11), short‐term (MD 0.24, 95% CI −0.28 to 0.76, 74 participants; Analysis 5.12) and long‐term follow‐up (MD 0.23, 95% CI −0.36 to 0.82, 62 participants; Analysis 5.13). As no one scale was used consistently across the studies, and change scores (rather than exact scale scores) were reported for some of the data, it was not possible to combine the scale results into a single meta‐analysis.
5.6. Analysis.
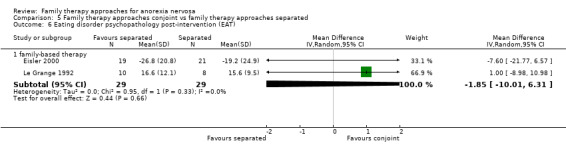
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 6 Eating disorder psychopathology post‐intervention (EAT).
5.7. Analysis.
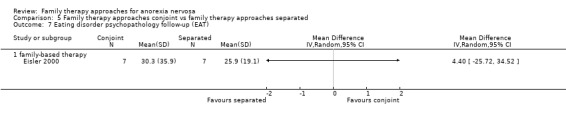
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 7 Eating disorder psychopathology follow‐up (EAT).
5.8. Analysis.
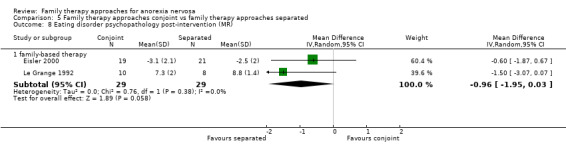
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 8 Eating disorder psychopathology post‐intervention (MR).
5.9. Analysis.
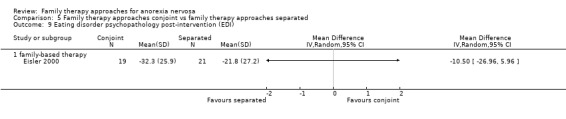
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 9 Eating disorder psychopathology post‐intervention (EDI).
5.10. Analysis.
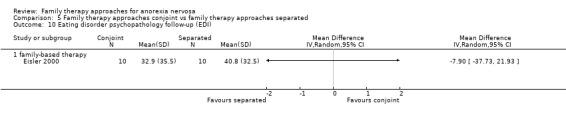
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 10 Eating disorder psychopathology follow‐up (EDI).
5.11. Analysis.
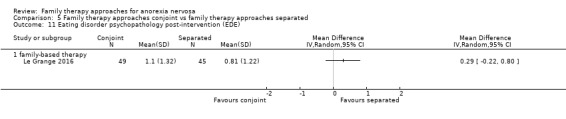
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 11 Eating disorder psychopathology post‐intervention (EDE).
5.12. Analysis.
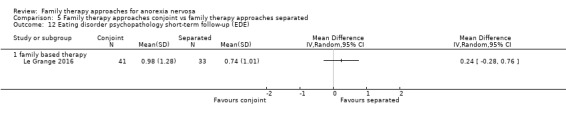
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 12 Eating disorder psychopathology short‐term follow‐up (EDE).
5.13. Analysis.
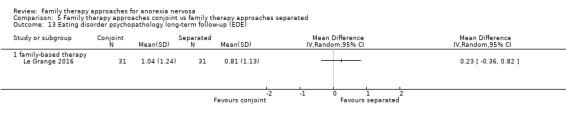
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 13 Eating disorder psychopathology long‐term follow‐up (EDE).
Weight
Similarly, the reporting of change scores in one study also prevented pooling of weight data across percentage ABW and percentage median BMI scores. Eisler 2000 and Le Grange 1992 both reported percentage ABW at post‐intervention. When these results are combined there is little evidence to support any difference between the conjoint and separated family‐based therapy groups (MD ‐2.75, 95% CI ‐18.50 to 13.00; participants = 58; I2 = 84%); Analysis 5.17), nor at five‐year follow‐up (one trial only; Eisler 2000) (MD −6.70, 95% CI −14.14 to 0.74, 33 participants; Analysis 5.18). Le Grange 2016 reported percentage median BMI scores with little evidence of a difference between groups post‐intervention (MD −3.20, 95% CI −7.09 to 0.69, 94 participants; Analysis 5.14), short‐term (MD −2.20, 95% CI −7.13 to 2.73, 74 participants; Analysis 5.15) or long‐term (MD −2.30, 95% CI −7.20 to 2.60, 62 participants; Analysis 5.16) .
5.17. Analysis.
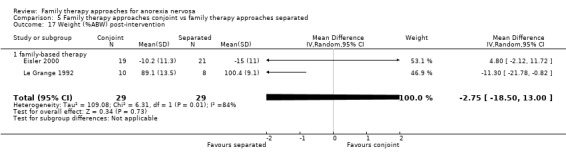
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 17 Weight (%ABW) post‐intervention.
5.18. Analysis.
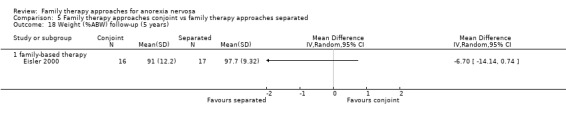
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 18 Weight (%ABW) follow‐up (5 years).
5.14. Analysis.
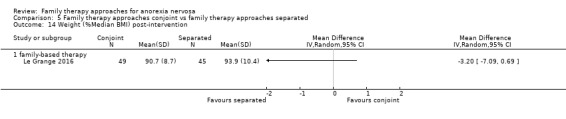
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 14 Weight (%Median BMI) post‐intervention.
5.15. Analysis.
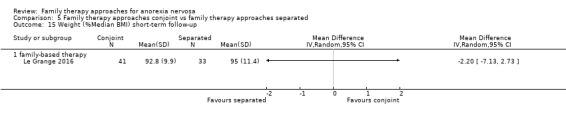
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 15 Weight (%Median BMI) short‐term follow‐up.
5.16. Analysis.
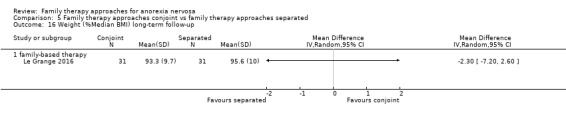
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 16 Weight (%Median BMI) long‐term follow‐up.
Relapse
Only one trial (Eisler 2000) reported on relapse and found little evidence of a treatment effect post‐intervention (RR 3.32, 95% CI 0.38 to 29.23, 40 participants; Analysis 5.19) or after five‐year follow‐up (RR 0.56, 95% CI 0.12 to 2.68, 38 participants; Analysis 5.20).
5.19. Analysis.
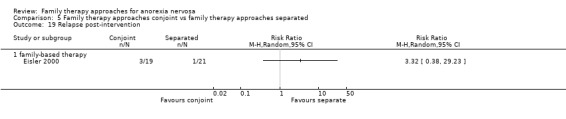
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 19 Relapse post‐intervention.
5.20. Analysis.
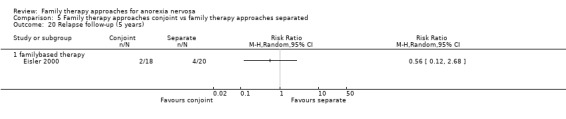
Comparison 5 Family therapy approaches conjoint vs family therapy approaches separated, Outcome 20 Relapse follow‐up (5 years).
Comparison 6: Family therapy approaches versus family therapy approaches plus meal
Two trials examined the efficacy of family‐based therapy compared with family‐based therapy that included a family meal as an intervention, with a combined total of 35 participants (Herscovici 2017; Rausch Herscovici 2006).
Primary outcomes
Remission
At the end of treatment there was little evidence of a difference in the numbers of remitted participants between family‐based therapy plus meal and family‐based therapy alone, with very high heterogeneity (RR 0.70, 95% CI 0.23 to 2.10; participants = 35; I2 = 88%); Analysis 6.1). There was little evidence of any difference in levels of remission at short‐term follow‐up in Herscovici 2017 (RR 0.69, 95% CI 0.35 to 1.35, 23 participants; Analysis 6.2), or at long‐term follow‐up in Rausch Herscovici 2006 (RR 1.00, 95% CI 0.75 to 1.34, 12 participants; Analysis 6.3).
6.1. Analysis.
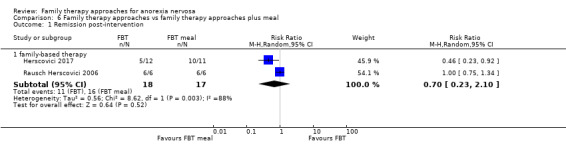
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 1 Remission post‐intervention.
6.2. Analysis.
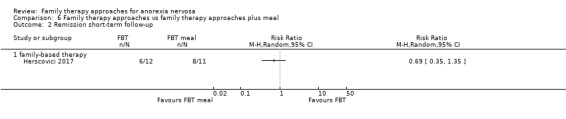
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 2 Remission short‐term follow‐up.
6.3. Analysis.
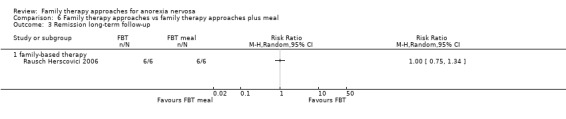
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 3 Remission long‐term follow‐up.
All‐cause mortality
Mortality was not reported.
Secondary outcomes
Functioning
Family functioning was measured on the Family Health Scale by Rausch Herscovici 2006, with some limited evidence of an improvement for those receiving the family‐based therapy plus meal compared to those receiving family‐based therapy alone after intervention (MD −0.62, 95% CI −1.16 to −0.08; 12 participants; Analysis 6.4). There were no useable data on family functioning at follow‐up.
6.4. Analysis.
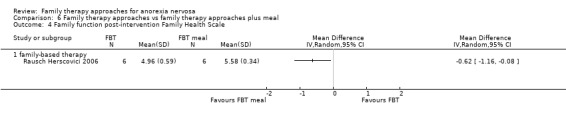
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 4 Family function post‐intervention Family Health Scale.
There were no useable data on general functioning.
Dropouts
Both studies (Herscovici 2017; Rausch Herscovici 2006) reported on dropouts, with some limited evidence that there were no differences in the rate of dropouts during therapy between the groups (RR 0.33, 95% CI 0.02 to 6.86; participants = 35; I2 = 0%); Analysis 6.5).
6.5. Analysis.
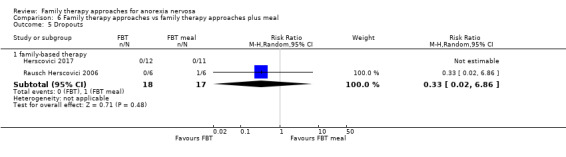
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 5 Dropouts.
Eating disorder psychopathology
Both studies (Herscovici 2017; Rausch Herscovici 2006) used the Morgan‐Russell scales. Combined data showed some limited evidence that there may be little difference between the groups on eating disorder psychopathology at the end of intervention (MD 0.54, 95% CI ‐0.78 to 1.85; participants = 35; I2 = 0%); Analysis 6.6), at short‐term follow‐up in Herscovici 2017 (MD −0.10, 95% CI −1.78 to 1.58, 23 participants; Analysis 6.7) or at long‐term follow‐up in Rausch Herscovici 2006 (MD 0.33, 95% CI −1.85 to 2.51, 12 participants; Analysis 6.8).
6.6. Analysis.
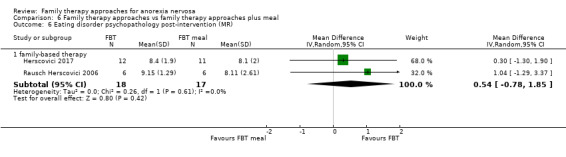
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 6 Eating disorder psychopathology post‐intervention (MR).
6.7. Analysis.
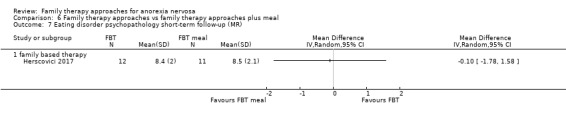
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 7 Eating disorder psychopathology short‐term follow‐up (MR).
6.8. Analysis.
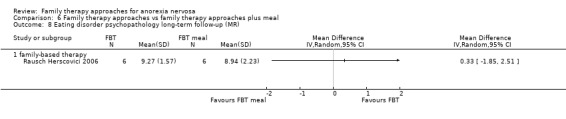
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 8 Eating disorder psychopathology long‐term follow‐up (MR).
Weight
There was little evidence of differences in weight (BMI and EBW percentage) between the groups receiving family‐based therapy and the groups receiving family‐based therapy plus meal at the end of treatment or at long‐term follow‐up (SMD ‐0.19, 95% CI ‐0.85 to 0.48; participants = 35; I2 = 0%); Analysis 6.9), with both study results combined. There was little evidence of difference in EBW percentages at short‐term follow‐up in Herscovici 2017 (MD −5.30, 95% CI −15.05 to 4.45, 23 participants; Analysis 6.10), or in BMI scores in Rausch Herscovici 2006 (MD 0.60, 95% CI −2.10 to 3.30, Analysis 6.11).
6.9. Analysis.
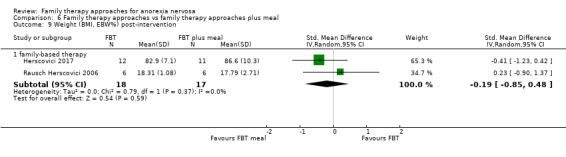
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 9 Weight (BMI, EBW%) post‐intervention.
6.10. Analysis.
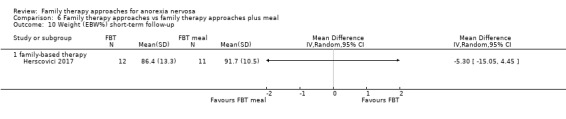
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 10 Weight (EBW%) short‐term follow‐up.
6.11. Analysis.
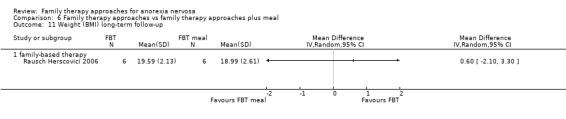
Comparison 6 Family therapy approaches vs family therapy approaches plus meal, Outcome 11 Weight (BMI) long‐term follow‐up.
Relapse
There were no useable data reported on relapse.
Comparison 7: Individual family therapy approaches versus group family therapy approaches
There was one trial in this condition (Whitney 2012). In this trial a ‘specific family therapy’ approach was applied to individual families in one condition (categorised as Other family therapy), while systems family therapy was used to treat families in a group setting in the other, with a total of 48 participants.
Primary outcomes
Remission
There were no useable data on remission.
All cause mortality
No data about mortality were reported.
Secondary outcomes
Functioning
Family functioning was measured using the carers' level of expressed emotion (LEE) scale (Cole 1988). There was little evidence of any differences between the groups on family functioning at the end of treatment (MD 1.10, 95% CI −2.93 to 5.13, 66 participants; Analysis 7.1) or at follow‐up (MD −0.90, 95% CI −5.23 to 3.43, 58 participants; Analysis 7.2).
7.1. Analysis.
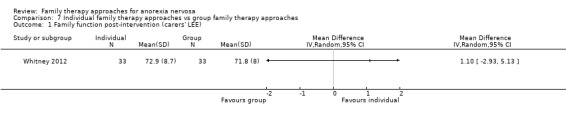
Comparison 7 Individual family therapy approaches vs group family therapy approaches, Outcome 1 Family function post‐intervention (carers' LEE).
7.2. Analysis.
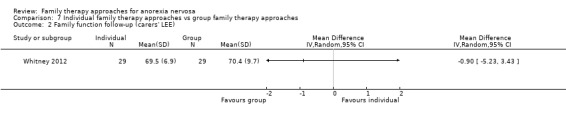
Comparison 7 Individual family therapy approaches vs group family therapy approaches, Outcome 2 Family function follow‐up (carers' LEE).
There were no data on general functioning.
Dropouts
There was little evidence of any differences in the rate of dropouts between groups (RR 1.09, 95% CI 0.24 to 4.86, 48 participants; Analysis 7.3).
7.3. Analysis.
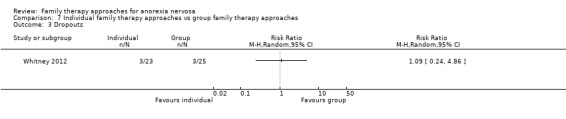
Comparison 7 Individual family therapy approaches vs group family therapy approaches, Outcome 3 Dropouts.
Eating disorder psychopathology
Whitney 2012 measured eating disorder psychopathology using the short evaluation of eating disorders‐anorexia nervosa (SEED‐AN); there was little evidence on this measure of a difference between the groups post‐intervention (MD 0.20, 95% CI −0.62 to 1.02, 25 participants; Analysis 7.4) or at follow‐up (MD −0.20, 95% CI −0.79 to 0.39, 29 participants; Analysis 7.5).
7.4. Analysis.
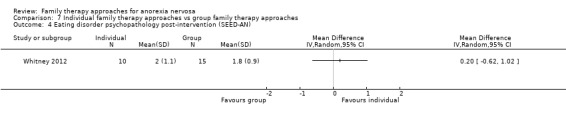
Comparison 7 Individual family therapy approaches vs group family therapy approaches, Outcome 4 Eating disorder psychopathology post‐intervention (SEED‐AN).
7.5. Analysis.
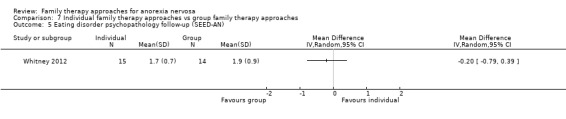
Comparison 7 Individual family therapy approaches vs group family therapy approaches, Outcome 5 Eating disorder psychopathology follow‐up (SEED‐AN).
Weight
There was little evidence of a difference between the groups in BMI at the end of treatment (MD −0.80, 95% CI −1.86 to 0.26, 47 participants; Analysis 7.6) or at follow‐up (MD 1.00, 95% CI −0.42 to 2.42, 44 participants; Analysis 7.7).
7.6. Analysis.
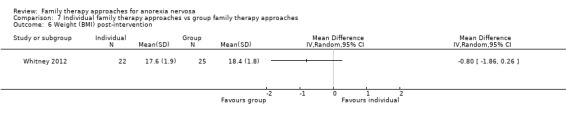
Comparison 7 Individual family therapy approaches vs group family therapy approaches, Outcome 6 Weight (BMI) post‐intervention.
7.7. Analysis.
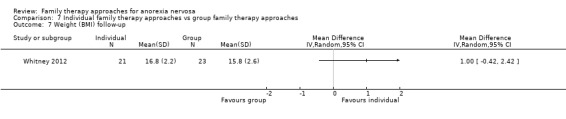
Comparison 7 Individual family therapy approaches vs group family therapy approaches, Outcome 7 Weight (BMI) follow‐up.
Mortality
No data about mortality were reported.
Relapse
No useable data on relapse were provided.
Comparison 8: Family‐based therapy versus systemic family therapy
There was one trial (Agras 2014; 158 participants) for this comparison of family‐based therapy to systemic family therapy.
Primary outcomes
Remission
There was little evidence of any difference in remission rates between family‐based therapy and systemic family therapy post‐intervention (RR 1.33, 95% CI 0.81 to 2.18, 158 participants; Analysis 8.1), or at short‐term follow‐up (RR 1.06, 95% CI 0.72 to 1.55, 158 participants; Analysis 8.2).
8.1. Analysis.
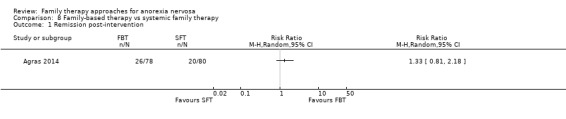
Comparison 8 Family‐based therapy vs systemic family therapy, Outcome 1 Remission post‐intervention.
8.2. Analysis.
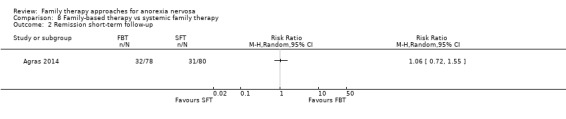
Comparison 8 Family‐based therapy vs systemic family therapy, Outcome 2 Remission short‐term follow‐up.
All‐cause mortality
The study reported that there were no deaths of participants in either intervention at the end of treatment or at short‐term follow‐up (less than 12 months).
Secondary outcomes
Functioning
There were no useable data reported on family functioning or general functioning.
Dropouts
There was little evidence of any difference in dropout rates between family‐based therapy and systemic family therapy during the intervention.(RR 1.03, 95% CI 0.60 to 1.75, 158 participants; Analysis 8.3).
8.3. Analysis.
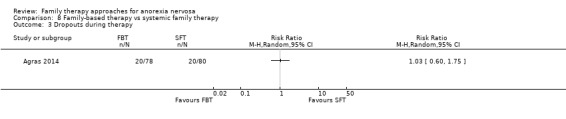
Comparison 8 Family‐based therapy vs systemic family therapy, Outcome 3 Dropouts during therapy.
Eating disorder psychopathology
There were no useable data reported on eating disorder psychopathology.
Weight
There were no usable data reported on weight.
Mortality
No data about mortality were reported.
Relapse
No useable data were provided about relapse.
Comparison 9: Inpatient family therapy versus day‐patient family therapy
There was one trial (Herpertz‐Dahlmann 2014; 161 participants) for this comparison of inpatient family therapy to day‐patient family therapy. We categorised both interventions as Other family therapy and incorporated family therapy along with other therapeutic approaches.
Primary outcomes
Remission
There was little evidence of any difference in remission rates between an inpatient family therapy approach and a day‐patient family therapy approach at short‐term follow‐up (less than 12 months) (RR 1.15, 95% CI 0.79 to 1.66, 161 participants; Analysis 9.1).
9.1. Analysis.
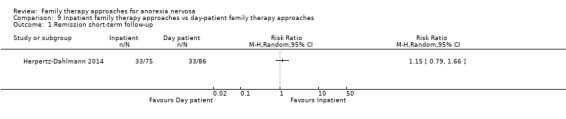
Comparison 9 Inpatient family therapy approaches vs day‐patient family therapy approaches, Outcome 1 Remission short‐term follow‐up.
All‐cause mortality
The study reported that there were no deaths of participants in either intervention at the end of treatment or at short‐term follow‐up (less than 12 months).
Secondary outcomes
Functioning
No useable data were provided about family functioning or general functioning.
Dropouts
There was little evidence of any difference in dropout rates between an inpatient family therapy approach and a day‐patient family therapy approach during the intervention (RR 0.60, 95% CI 0.30 to 1.22, 161 participants; Analysis 9.2).
9.2. Analysis.
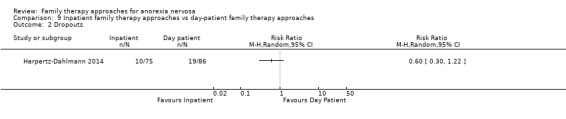
Comparison 9 Inpatient family therapy approaches vs day‐patient family therapy approaches, Outcome 2 Dropouts.
Eating disorder psychopathology
The EDI was used to assess eating disorder psychopathology. There was little evidence of any difference between an inpatient family therapy approach and a day‐patient family therapy approach at short‐term follow‐up (MD 8.00, 95% CI −15.22 to 31.22, 161 participants; Analysis 9.3).
9.3. Analysis.
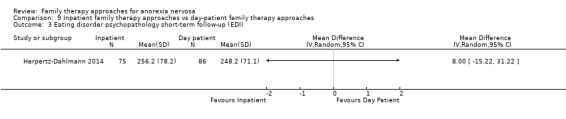
Comparison 9 Inpatient family therapy approaches vs day‐patient family therapy approaches, Outcome 3 Eating disorder psychopathology short‐term follow‐up (EDI).
Weight
Weight was assessed by percentile EBW. There was little evidence of any difference between an inpatient family therapy approach and a day‐patient family therapy approach at short‐term follow‐up (MD −1.20, 95% CI −3.92 to 1.52, 161 participants; Analysis 9.4).
9.4. Analysis.
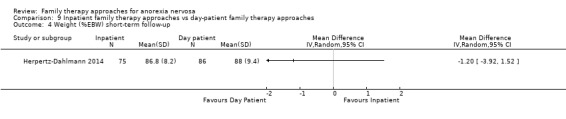
Comparison 9 Inpatient family therapy approaches vs day‐patient family therapy approaches, Outcome 4 Weight (%EBW) short‐term follow‐up.
Mortality
The study reported that there were no deaths of participants in either intervention at the end of treatment or at short‐term follow‐up (less than 12 months).
Relapse
There was little evidence of any difference in rates of relapse between an inpatient family therapy approach and a day‐patient family therapy approach at short‐term follow‐up (RR 1.68, 95% CI 0.89 to 3.16, 161 participants; Analysis 9.5).
9.5. Analysis.
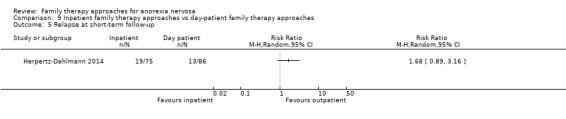
Comparison 9 Inpatient family therapy approaches vs day‐patient family therapy approaches, Outcome 5 Relapse at short‐term follow‐up.
Comparison 10: Family‐based therapy versus family‐based therapy plus parent coaching
There was one trial (Lock 2015; 45 participants) comparing family‐based therapy to family‐based therapy plus parent coaching for those with poor early weight restoration.
Primary outcomes
Remission
There was little evidence of any difference in remission rates between family‐based therapy and family‐based therapy plus parent coaching post‐intervention (RR 1.03, 95% CI 0.51 to 2.09, 45 participants; Analysis 10.1).
10.1. Analysis.
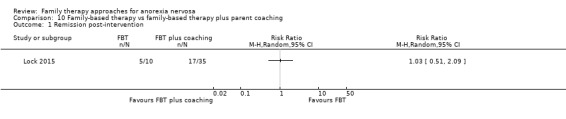
Comparison 10 Family‐based therapy vs family‐based therapy plus parent coaching, Outcome 1 Remission post‐intervention.
All‐cause mortality
No useable data were provided about mortality.
Secondary outcomes
Functioning
No useable data were provided about family functioning or general functioning.
Dropouts
There was little evidence of any difference in dropout rates between family‐based therapy and family‐based therapy plus parent coaching post‐intervention (RR 1.00, 95% CI 0.25 to 4.08, 45 participants; Analysis 10.2).
10.2. Analysis.
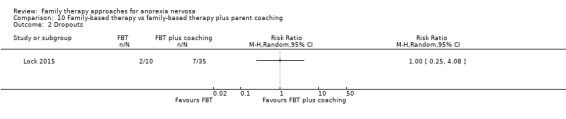
Comparison 10 Family‐based therapy vs family‐based therapy plus parent coaching, Outcome 2 Dropouts.
Eating disorder psychopathology
The EDE scale was used to assess eating disorder psychopathology at post‐intervention. There was some limited evidence of a difference in EDE results, favouring family‐based therapy over family‐based therapy plus parent coaching (MD −0.80, 95% CI −1.39 to −0.21, 36 participants; Analysis 10.3).
10.3. Analysis.

Comparison 10 Family‐based therapy vs family‐based therapy plus parent coaching, Outcome 3 Eating disorder psychopathology post‐intervention (EDE).
Weight
There was little evidence of any difference in weight measured using BMI between family‐based therapy and family‐based therapy plus parent coaching (MD −0.10, 95% CI −1.08 to 0.88, 36 participants; Analysis 10.4).
10.4. Analysis.
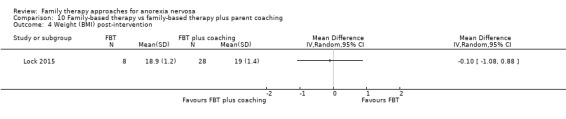
Comparison 10 Family‐based therapy vs family‐based therapy plus parent coaching, Outcome 4 Weight (BMI) post‐intervention.
Relapse
No useable data were provided about relapse.
Comparison 11: Family therapy approach plus medical stabilisation versus family therapy approach plus weight restoration
There was one trial (Madden 2015; 82 participants) for this comparison. We categorised both of these interventions as family‐based therapy.
Primary outcomes
Remission
There was little evidence of any difference in rates of remission between family‐based therapy plus medical stability compared with family‐based therapy plus weight restoration at post‐intervention (RR 1.13, 95% CI 0.78 to 1.64, 78 participants; Analysis 11.1), at short‐term follow‐up (RR 0.78, 95% CI 0.56 to 1.08, 78 participants; Analysis 11.2) or at long‐term follow‐up (RR 0.86, 95% CI 0.69 to 1.07, 78 participants; Analysis 11.3).
11.1. Analysis.
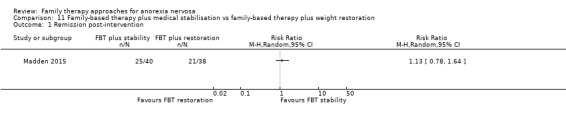
Comparison 11 Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration, Outcome 1 Remission post‐intervention.
11.2. Analysis.
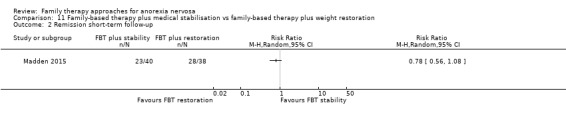
Comparison 11 Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration, Outcome 2 Remission short‐term follow‐up.
11.3. Analysis.
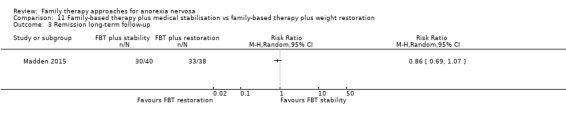
Comparison 11 Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration, Outcome 3 Remission long‐term follow‐up.
All‐cause mortality
No useable data were provided about mortality.
Secondary outcomes
Functioning
No useable data were provided about family functioning or general functioning.
Dropouts
There was little evidence of any difference in dropout rates between family therapy plus medical stability compared with family therapy plus weight restoration (RR 0.33, 95% CI 0.04 to 3.07, 82 participants; Analysis 11.4).
11.4. Analysis.
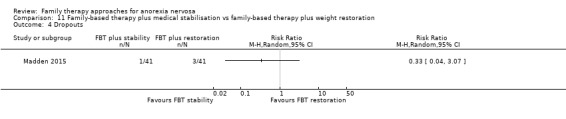
Comparison 11 Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration, Outcome 4 Dropouts.
Eating disorder psychopathology
There was little evidence of any difference in eating disorder psychopathology on the EDE at long‐term follow‐up between family‐based therapy plus medical stability compared with family‐based therapy plus weight restoration (MD −0.18, 95% CI ‐0.90 to 0.54, 69 participants; Analysis 11.5).
11.5. Analysis.
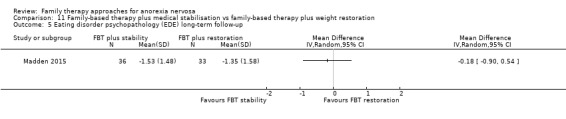
Comparison 11 Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration, Outcome 5 Eating disorder psychopathology (EDE) long‐term follow‐up.
Weight
There was little evidence of any difference in percentage EBW change at long‐term follow‐up between family‐based therapy plus medical stability compared with family‐based therapy plus weight restoration (MD 2.02, 95% CI −2.57 to 6.61, 78 participants; Analysis 11.6).
11.6. Analysis.
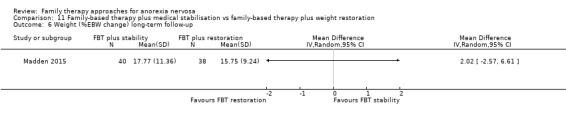
Comparison 11 Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration, Outcome 6 Weight (%EBW change) long‐term follow‐up.
Relapse
Relapse was defined as requiring readmission to hospital in the 12‐month follow‐up period. There was little evidence of any difference between the family‐based therapy plus medical stability compared with family‐based therapy plus weight restoration (RR 0.95, 95% CI 0.53 to 1.72, 78 participants; Analysis 11.7).
11.7. Analysis.
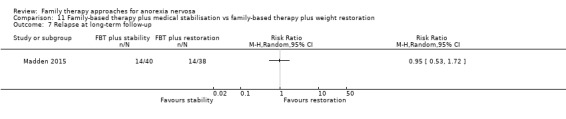
Comparison 11 Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration, Outcome 7 Relapse at long‐term follow‐up.
Comparison 12: Family‐based therapy versus family‐based therapy plus consultation
One trial (Rhodes 2008; 20 participants) compared family‐based therapies, with and without parent‐to‐parent consultation.
Primary outcomes
Remission
There was little evidence of any difference in rates of remission between family‐based therapy compared with family‐based therapy plus consultation at post‐intervention (RR 1.14, 95% CI 0.69 to 1.90, 20 participants; Analysis 12.1).
12.1. Analysis.
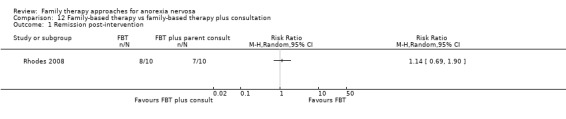
Comparison 12 Family‐based therapy vs family‐based therapy plus consultation, Outcome 1 Remission post‐intervention.
All‐cause mortality
No useable data were provided about mortality.
Secondary outcomes
Functioning
No useable data were provided about family functioning or general functioning.
Dropouts
No useable data were provided about dropouts.
Eating disorder psychopathology
No useable data were provided about eating disorder psychopathology.
Weight
No useable data were provided about weight, as percentage IBW results were missing standard deviations and were reported by outcome categories and not by treatment group totals.
Relapse
No useable data were provided about relapse.
Discussion
Summary of main results
The first primary outcome measure in this review was remission. The definition of remission varied widely across studies, with this heterogeneity affecting the comparability of the results. Of the 12 comparisons conducted, useable data for remission were available for at least one time point (post‐intervention, short‐term less than 12‐month follow‐up or long‐term 12‐month and longer follow‐up) in 11 analyses. Based on these results there is a very small evidence base (two trials) of low‐quality evidence that suggests that family therapy approaches may be more effective than treatment as usual post‐intervention, but this difference does not appear to be maintained at long‐term follow‐up, based on one trial. There was insufficient and low‐quality evidence (five trials post intervention and four trials at long term follow‐up; one of these trials presented three pair‐wise comparisons for different age groups) contributing to a comparison of family therapy approaches and psychological interventions, meaning it is difficult to conclude whether there are advantages of one approach over the other. The same was true for family therapy approaches and educational interventions (one trial). Given this lack of evidence for a clear advantage of family therapy, the choice of treatment for those with AN may include individual psychological therapy or educational interventions, which can be less costly and more accessible than family therapy.
When we compared different types of family therapy approaches head‐to‐head, we found few differences in rates of remission between treatments, and those that we found were no longer evident at long‐term follow‐up, although frequently such findings were based on very few trials and wide confidence intervals. There was some evidence, based on two trials, that remission rates might be higher for separated compared to conjoint family‐based therapy at post‐intervention, and at short‐term follow‐up based on one trial; however, there was not strong evidence of a difference between separated and conjoint family‐based therapy remission rates at long‐term follow‐up, based on two trials. Given that the current evidence does not allow us to determine whether there is any advantage of family therapy approaches compared with psychological interventions, the utility of focusing on comparisons between different types of family therapy approaches could also be questionable.
The second primary outcome measure was mortality. Information about mortality was not reported for seven of the 12 comparisons. In those where mortality data were available, it was often not provided for all trials, or was provided in an incomplete or unclear manner. One death was reported following randomisation but prior to treatment in Crisp 1991. Across all studies, four deaths were reported either at post‐intervention or at follow‐up. One death was reported in one study (occurring in the treatment‐as‐usual condition; Dare 2001). There were also three deaths at five‐year follow‐up in Russell 1987, but it was unclear in which treatment groups these deaths occurred. As a large number of the remaining trials had incomplete analysis of participants at follow‐up, or anomalies in the reported follow‐up data, it was not possible to determine whether these were in fact the only deaths across all trial participants. Consequently, it is difficult to make an overall comment on any potential harms resulting from the interventions under evaluation. However, based on the available evidence, the mortality rates in the included trials appear to be lower for all types of interventions compared to the rates of mortality reported in individuals with AN in the general literature (Fichter 2006; Harris 1998; Sullivan 1995). This may reflect the fact that the most severely unwell people may not have been included in the trials, or it may reflect an improvement in care.
For the secondary outcomes, almost all the remaining comparisons for the outcome measures of eating disorder psychopathology, family or general functioning, relapse, weight measures and dropouts from treatment, there was insufficient evidence to determine whether there were differences between treatment conditions. There was a limited amount of evidence, based on four trials, to suggest that there may be greater gains in weight for those receiving family therapy approaches compared with other psychological therapies, but this effect was less clear at long‐term follow‐up. There was also some limited evidence of a difference in eating disorder psychopathology, favouring family‐based therapy over family‐based therapy plus parent coaching at post‐intervention, with no follow‐up data reported (Lock 2015). There was some limited evidence of an improvement in family functioning on the Family Health Scale in the family‐based therapy plus meal group compared to the family‐based therapy alone group after intervention, in one trial (Rausch Herscovici 2006). Useable follow‐up data on family functioning were not reported. Overall, across all of the trials comparing one type of family therapy to another, there was insufficient evidence to determine if there is a significant advantage of any particular type of family therapy over another.
Very few trials provided useable data on the key measures of general functioning (2/25) and family functioning (2/25). While remission rates are very important to assess, general functioning (i.e. participation in major life activities such as school, work, socialisation, etc.) is also extremely important and it would be beneficial to the research field if more information were available about general functioning post‐AN treatment and recovery. As all trials used some form of family therapy approach, it is to be expected that the trialists would be interested in assessing the impact of the interventions on functioning within the family structure. The low rates of assessment of family functioning were therefore disappointing. It would have been valuable for family functioning factors to have been explored more commonly as an outcome measure, and to have been reported in more detail.
Useable data about relapse rates for participants were reported in some form for six of the 12 comparisons. There was not enough evidence to determine if there are meaningful differences in relapse rates across any of the comparisons of family therapy versus non‐family therapy interventions, or between different forms of family therapy when compared head‐to‐head.
This review is a major update of the original version (Fisher 2010). It incorporates a further 12 studies, bringing the total number of included studies up to 25. The number of comparison analyses has also doubled, from six to 12. As a result, there is a large spread of analyses, with many of the new trials contributing to analyses investigating small variations within the same family therapy approach (e.g. family‐based therapy with family meal versus no meal; family‐based therapy with parental coaching to early poor weight restorers versus no parental coaching), rather than strengthening the evidence in the major comparisons of interest. The overall results from the primary outcome measure (remission) are similar to the original version of the review, with both versions presenting low‐quality evidence to suggest that family therapy may be more effective than treatment as usual on rates of remission in the short term, but insufficient evidence to determine if there is a significant advantage of family therapy compared with educational interventions or other psychological interventions. In this update we implemented subgroup analysis to investigate the impact of age group on treatment effects; however, overall there was insufficient evidence to draw robust conclusions. There are few adult trials and most of these include participants who might be classed as youth (United Nations class youth as 15 to 24 years), with studies postulating that this group are not necessarily dissimilar from adolescents (Sawyer 2018). Very few studies have been undertaken in adults over the age of 30, although we note that there are some additional trials listed in Characteristics of studies awaiting classification that include adults. It is inevitable that the application of family therapy approaches will be different in adolescents, youth and adults, and that the impact of age on treatment effect requires further investigation. Indeed, it would make sense for this review to be split so that the efficacy of family therapy approaches in adults can be examined separately.
We also anticipated that in updates of this review it might be possible to investigate whether there were any differences in treatment effectiveness based on how long an individual met criteria for AN. However, due to the trial designs and the nature in which the data were reported (i.e. few studies that stratified the results according to chronicity) it was not possible to conduct analyses to investigate the impact of chronicity on treatment effectiveness.
Overall completeness and applicability of evidence
The available trials allowed for the comparison of family therapy approaches to standard treatment, and to other treatments, meeting the first major objective of the review. However, in many of the comparison analyses there were few trials with small numbers of participants. The comparison that included the greatest number of trials was family therapy approaches versus other psychological interventions, which comprised six trials (only 5 contributing to the primary outcome remission) with a total of 414 AN patients. This was followed by family therapy approaches versus standard care/treatment as usual, which comprised four trials with 286 participants.
The second major objective of the review was to compare the efficacy of different forms of family therapy approaches. Nine analyses were possible that directly compared different forms of family therapy approaches. However, it is important to note that most of these involved the use of two family interventions that were theoretically very similar (or identical), but with a single point of difference or a modification between the two interventions, i.e. short‐term versus long‐term, conjoint versus separated, family meal versus no meal, inpatient versus outpatient, parent coaching versus no parent coaching, pre‐therapy medical stability versus weight restoration. The two exceptions to this were family‐based therapy versus systems family therapy (one trial), and specific individual family therapy (other) versus systems group family therapy (one trial). The comparison with the highest number of participants was conjoint versus separated family‐based therapy (three trials, 165 participants). This was followed by inpatient family therapy approaches versus day‐patient family therapy approaches (one trial, 161 participants) and family‐based therapy versus systemic family therapy (one trial, 158 participants).
There were a limited number of trials and useable data, and a lack of specificity about the theoretical underpinning of the family therapy approach used in a number of trials. It was therefore not possible to compare trials with different theoretical approaches in the family therapy approaches versus other therapy analyses (i.e. treatment as usual, psychological interventions and educational interventions). We therefore conclude that there is insufficient evidence to be able to determine whether or not there are differences between different types of family therapy.
The primary outcome of the review was remission; however, this was variously defined across trials and only reported in 15 of the 25 trials at end of treatment and in 14 at follow‐up. While improvements in eating disorder psychopathology and weight are important to patients, returning to normal functioning is likely to be a more important outcome measure. Unfortunately, only two trials reported useable data for a measure of general functioning. This lack of consistency in the reporting of key outcome measures, and a lack of more generalised assessments of functioning, has compromised the capacity of our review to investigate clear outcome results from the trials. Many trials also failed to report on between‐group differences (e.g. Hall 1987; Russell 1987; Robin 1999).
Eighteen trials reported at least some information on the rate of dropouts prior to the post‐intervention assessment. A further nine trials reported on the rate of dropouts at follow‐up. However, due to the nature of the reporting of this information it was at times unclear to which treatment arms the dropouts belonged. It was also often unclear how dropouts had been managed during the analysis of the outcome data. Given the nature of the disorder, it is possible that a proportion of participants who dropped out of the intervention fared poorly, in terms of clinical outcomes. The numbers of dropouts in the reviewed trials may therefore have the effect of artificially inflating the effectiveness of the interventions.
A wide variety of weight measures were used across the trials (BMI, kilograms, IBW percentage, ABW, EBW percentage), making it difficult to determine if participants included in these trials were similar to those seen in clinical practice. Of the 13 trials that reported mean BMI scores at baseline, most fell between 14.9 and 17.5, with just two trials reporting BMI means below 14.9. Three of the trials that reported their exclusion criteria excluded participants with very low weight: Agras 2014 excluded those less than 75% of IBW; Ball 2004 those with a BMI below 13.5; Dare 2001 those with "extremely low body weight". Three trials excluded people with longer durations of AN: Crisp 1991 excluding clients with more than 10 years of illness; Godart 2012 and Madden 2015 excluding people with more than three years of illness, while Le Grange 1992 excluded those with less than three years of illness. Participants with comorbidities, including suicidal risk and other psychiatric disorders, were often excluded. Participants were included both from inpatient and from outpatient settings. However, most were outpatients and consequently were more likely to be stabilised. It is important to note that men and boys were either excluded or represented a small proportion of the samples, so it may be that the results are not generalisable to male patients with AN. Furthermore, as noted, most of the studies included participants either exclusively or predominantly from an adolescent age range. The findings may therefore not be generalisable to older people with AN.
We have not examined treatment cost effectiveness in the review, but is an important factor when considering the overall applicability of a treatment to a particular cohort and setting. Treatments that are more therapist time‐intensive, and those in which participants received or required inpatient admissions throughout the therapy are likely to have been more costly than less intensive outpatient therapies. Evaluating treatment cost effectiveness would be a useful addition to any future update of this review.
Quality of the evidence
The reporting of aspects of risks of bias across the trials was generally inadequate. It is therefore difficult to estimate what the effect of bias on the treatment might be. This was particularly evident for concealment of allocation, as inadequate concealment is known to have a large effect on treatment estimates (Juni 2001). The blinding of care providers and participants is not possible in trials of therapy. Similarly, blinding of self‐reported outcome measures is also not possible. However, in this review clinician‐assessed outcomes were common, and little detail was provided about the blinding of these outcome assessors, with just five trials reporting the blinding of outcome assessors. In the remaining 20 trials this was either not conducted or was not reported or unclear. The risks of bias in the reporting of trial results were also high, with just 12% rated at low risk of attrition bias, 16% at low risk of reporting bias and just 4% at low risk of other potential sources of bias.
A number of trials suffered from other problems relating to the eccentricities of trials conducted in this field. For example, several appeared to have baseline imbalances (e.g. Crisp 1991; Eisler 2000; Hall 1987; Le Grange 1992; Robin 1999; Whitney 2012). In some cases the same therapist conducted the therapy in both family therapy and comparison treatment groups (e.g. Agras 2014; Eisler 2000; Russell 1987). There were often issues with the delivery of treatment or with treatment integrity, e.g. in Crisp 1991 participants were allowed to change treatment conditions; there was little consistency in treatment dosage in Dare 2001; Crisp 1991; Russell 1987; in one trial participants also received individual psychodynamic therapy, but there was no psychodynamic therapy‐alone comparison group (Hall 1987).
Risk of bias is one domain of the GRADE rating system of quality that we therefore consistently downgraded. We also downgraded for inconsistency, where in some cases the direction of effect varied (investigated in subgroup analyses by age group, but with too little data available for adults this was underpowered), and for imprecision, with few trials and with wide confidence intervals attributable to few participants.
Potential biases in the review process
Three of the trials included in the review were not published in English. Two of these trials were reported in Spanish and thus the data for two trials were extracted by a Spanish‐speaking colleague. One trial was published in Chinese and the data were extracted by a Chinese‐speaking colleague. We made every effort to ensure the accuracy and consistency of these extractions. However, the fact that the data were extracted by another individual, not as well‐practised in extraction for this particular review, may have affected the quality of the information obtained from these papers.
In most cases we used end‐point data in the review, rather than change scores, as these were not generally available. End‐point data are more sensitive to baseline imbalances in the data, and thus may have affected the accuracy of the results.
Most of the data were obtained through published trial reports. However, some of the data were obtained through personal correspondence after we contacted all lead trial authors. As not all authors responded to our requests for missing data, or provided clarifications of data anomalies, it is possible that there remains a proportion of the existing data that we were not able to include in this review. Also, as we acquired extra data from a number of the responding authors through personal communication, the current review may under‐represent the extent of the level of reporting bias in the published papers, as originally published.
Agreements and disagreements with other studies or reviews
Based on the data available in this update, there is insufficient evidence to be able to determine the relative efficacy of family therapy approaches over other interventions, other than treatment as usual. There is insufficent evidence to be able to determine the relative efficacy of family therapy approaches over educational or other psychological interventions, and little clear evidence to indicate that family therapy approaches are more effective for adolescents compared to older persons (19 years +) with AN. This contrasts with recommendations in some recent guidelines (NICE 2017).
Several reviews of the efficacy of family therapy approaches have previously been published. Typically, these have based their conclusions on narrative summaries of individual trial results, not meta‐analyses. Of these, a review of intervention studies for the treatment of AN in adolescents (Keel 2008) highlighted the paucity of studies for this population. They concluded that the Maudsley model of family therapy (family‐based therapy) is the only intervention that has been tested and that based on two small studies (Russell 1987; Robin 1999) family‐based therapy is superior to the other psychological interventions investigated in these trials. In a systematic review of intervention studies for the treatment of AN in all age groups (Berkman 2006), the Agency for Healthcare Research and Quality states that the efficacy of family therapy approaches in treating adults with AN has not yet been completely addressed and that various forms of family therapy are efficacious in treating adolescents. The report highlights the fact that the statement about the efficacy of family therapy for adolescents with AN is based on the results of Robin 1999 and on the results of the subgroup of younger participants with shorter duration of illness in the Russell 1987 trial. This review contextualises these findings in terms of the quality of the conduct of the trials, and highlights the small sample sizes and lack of statistical power to detect differences across treatment groups in the included trials. In a systematic review of the evidence for psychological treatments in eating disorders (Hay 2013), the authors state that in adolescents with AN there has been progress in the evidence for the use of family‐based treatment and cognitive behaviour therapy.
One recent systematic review (Couturier 2013) did undertake a meta‐analysis and examined the efficacy of family‐based treatment for adolescents with eating disorders. Due to the selection criteria, only three trials were included, only one of which included participants with AN, and two others with bulimia nervosa (BN) and eating disorders not otherwise specified (EDNOS). The authors concluded that family‐based treatment does not appear to be superior to individual treatment at end of treatment, but at follow‐up appears to show significant benefits for adolescents with eating disorders. Given the inclusion of trials with eating disorders other than AN, it is difficult to make any clear comparisons with our review.
Authors' conclusions
Implications for practice.
The research literature into family therapy approaches for the treatment of AN is growing, with the available studies meeting criteria for this review almost doubling over the eight‐year period between the first and second versions (2008 to 2016). However, it is important to note that the evidence base still remains relatively small. Several recent moderate‐sized trials have been conducted, but many still involve small sample sizes, and all have potentially significant risks of bias, with many details about the conduct of the trials not reported. What evidence there is generally of low quality, and while it suggests that family therapy may be effective compared to standard or routine treatment (predominantly outpatient management with individual consultations with general practitioner/family doctor, psychiatrist or other health professionals that may be group‐based) in the short term, there is insufficient evidence to be able to determine the relative efficacy of family therapy, and educational and other psychological interventions. The main type of family therapy investigated remains family‐based therapy and its variants. There is insufficient evidence to be able to determine whether there are any significant differences in effectiveness between different family therapy approaches. Nor is there sufficient evidence to determine the impact of age on treatment efficacy, with most trials undertaken in adolescents and youth. We did not address treatment cost effectiveness as part of this review.
Implications for research.
The effectiveness of different family therapy approaches has not been well studied, with some major classes of family therapy intervention not investigated in trials to date. Further research into the efficacy of other psychological interventions versus family therapy is warranted, as are trials comparing different schools of family therapy. Such trials should include the following factors:
Given the lack of reporting about the conduct of trials and the potential impact of bias on these trials, there is a need for large, well‐conducted trials that include all elements designed to reduce the risk of bias;
This would include using standard clinically meaningful outcomes for participants;
Of particular interest would be trials that carefully investigated the impact of family therapy on family functioning, and in turn on clinical outcomes;
Within such trials, the impact of chronicity should be carefully investigated and distinguished from age.
It is clear that the impact of age requires further significant examination and this should be done in a review that separates out adult studies.
Feedback
Recommendations for revisions to the 'Family therapy for anorexia nervosa' review, 11 May 2010
Summary
First, I would like Cochrane to consider revising the 'Main Results', 'Authors' Conclusions', and 'Plain Language Summary' sections, which currently say that family based therapy has "no significant advantage," and "little advantage," compared to other interventions.
Those statements are inconsistent with the main body of the paper, including page 14, where it is acknowledged that for anorexia nervosa patients with an age of onset of less than 18, who have been ill less than three years, the "Maudsley" model of family based therapy has a "statistically significant" advantage over other forms of therapy. Consequently, it is inconsistent and misleading to say in the 'Main Results', 'Authors' Conclusions' and 'Plain Language Summary' that all forms of family therapy have "no significant advantage" or "little advantage" over other interventions. A "statistically significant" advantage is not the same as "no significant" or "little" advantage. In this respect, please note two other reviews that have been published on the subject of treatments for anorexia nervosa. One, Berkman, et al. 2006 (under contract with the U.S. Agency for Healthcare Research and Quality (http://www.ahrq.gov/downloads/pub/evidence/pdf/eatingdisorders/eatdis.pdf)) concludes that the "Maudsley model is 'efficacious in treating adolescents' and leads to 'clinically meaningful weight gain and psychological change'." A second, Keel, et al (http://www.ncbi.nlm.nih.gov/pubmed/18444053) judges that the evidence base is "strongest" for the Maudsley model of family therapy. I ask, therefore, that the Cochrane review restate its main result, conclusions, and summary so that they are consistent with its own findings and with the conclusions of other published reviews, including Berkman and Keel.
Second, I request that the Cochrane review delete all existing references to risk factors or etiology, including but not limited to the statement on page 3 that "family conflict" is a risk factor for anorexia nervosa. None of the six studies cited on page 3 provide evidence to support that assertion, and as noted by the American Psychiatric Association, no evidence exists to prove that families cause eating disorders. The APA further cautions that clinicians should avoid articulating theories that imply blame or permit family members to blame one another or themselves, and warns that doing so is harmful to both families and to patients (http://www.psychiatryonline.com/pracGuide/pracGuideTopic_12.aspx)
The subject of risk factors and etiology with respect to anorexia nervosa should not be addressed in a review focused on treatment of anorexia nervosa. The topics of risk factors and etiology are simply too complex, and not enough is known about them at this time, to be able to reach conclusions that meet Cochrane's standard of "conclusive evidence." To the extent that Cochrane wishes to publish a review of available evidence of risk factors and etiology, I suggest that it do so in a separate paper where full attention can be given to the subject.
Chris Berka Chairman of the Board F.E.A.S.T. (Families Empowered and Supporting Treatment of Eating Disorders) www.FEAST‐ED.org
Reply
We would like to thank Mr Berka for his extremely helpful and detailed feedback on our recently published Cochrane review, Family Therapy for Anorexia Nervosa. Our goal was to make this review helpful to patients, their families and the healthcare professionals who support them and commentaries like this one provide invaluable on‐going peer‐review post‐ publication. We are most grateful to Mr Berka for taking the time to provide these comments and for querying some of the methodology and the information presented. We are pleased to have the opportunity to respond to these points and hope that our replies and any associated changes will increase the value of the review to organisations like F.E.A.S.T.
In response, firstly, we thank Mr Berka for sending details of some significant reviews of family therapy (FT) for anorexia nervosa (AN). We have included a discussion of their findings in relation to our review in the final section of the 'Discussion'. We are in agreement with these reviews about the paucity of studies in this area. This is why we have, based on the careful consideration of the results of our systematic review and meta‐analysis, concluded that more research is required before definitive conclusions can be drawn about the effectiveness of family therapy compared with other psychological interventions or of one type of family therapy compared to others. We have indicated that there is evidence from a subgroup of 22 participants in the study by Russell and his colleagues that family therapy is beneficial, as have the reviews Mr Berka pointed out. However, we believe that this does not constitute a sufficiently large enough evidence base on which to draw conclusions about efficacy. We have highlighted that this is a promising finding that should be followed up with more research.
Where possible throughout the review, we have now clarified that this means there is insufficient evidence to be able to conclude that there are differences between FT and other psychological interventions or between different types of FT, as opposed to no evidence that one form of therapy is more effective than another. We think this conclusion is consistent with the approach of F.E.A.S.T who have recommended the Maudsley/Family Based Treatment in the absence of evidence for other treatments.
Secondly, we were very concerned to see that the 'Background' section on risk factors might be interpreted to suggest that parents are in some way responsible for or contribute to the development of anorexia in their children. The potential risk factors listed are simply the social, cultural, demographic and personality factors that appear to place an individual at an increased level of risk of having a particular disorder. While a number of risk factors are listed we did not intend to imply that these risk factors are causally associated with the development of an eating disorder.
We would like to clarify that it is not our opinion, nor do we think the literature indicates that the family or family structure is causal in the aetiology of eating disorders. We hoped this was clear from the information in the section summarising how the intervention might work: “Whether or not the family dynamic acts as a major contributing factor to the development of an eating disorder is still being debated”. However, to ensure that it is clear, we have altered the wording and removed reference to family factors in the Background and hope that this makes clear that family factors are in no way regarded as being causative of eating disorders.
Mr Berka kindly identified the statement by the American Psychiatric Association that highlights the point that there is no evidence that families cause eating disorders. We agree that the Background section would benefit from updating and we are grateful for Mr Berka’s contribution to this aspect of our review. We have not included reference to this statement from the APA, however; as we thought it preferable to remove any reference to the family when we discussed risk. We think that the Background now presents a broader discussion of risk factors and we will continue to take account of future publications each time the review is updated.
Caroline Fisher and Sarah Hetrick
Contributors
This feedback was prepared by Rachel Churchill and Jane Dennis, Coordinating Editor and Managing Editor for CCDAN, in consultation with the submitter and the authors of the review.
Feedback received by email, 19 December 2018
Summary
The authors of this review and Cochrane Common Mental Disorders received feedback via email about the review from an anonymous contributor. Concern was expressed that information presented in the background section of the review might be misleading, specifically with regard to the aetiology of eating disorders and the family environment.
Reply
The authors and Cochrane Common Mental Disorders are grateful for the helpful feedback provided. It was not the intention of the authors to be misleading. The author team has worked with Cochrane Common Mental Disorders and an external expert to amend the Description of the condition and How the intervention might work sections of the background to improve the text and avoid any possible misrepresentation of the literature. Correspondence also revealed that Besharat 2001 was undertaken in the UK, the review has also been updated to include this information. The authors would like to acknowledge the very helpful advisory input of Professor Ivan Eisler, Maudsley Centre for Child Adolescent Eating Disorders, London.
Contributors
This feedback was prepared by Peter Coventry and Jessica Hendon, Feedback Editor and Managing Editor for Cochrane Common Mental Disorders, in consultation with the contributor and the authors of the review.
What's new
| Date | Event | Description |
|---|---|---|
| 15 April 2019 | New citation required but conclusions have not changed | The background has been substantively updated and new references added following feedback on the review |
| 15 April 2019 | Feedback has been incorporated | Feedback was received and the authors have responded |
| 15 April 2019 | Amended | A section in the background of the review has been amended to improve the text and avoid any possible misrepresentation of the literature |
History
Protocol first published: Issue 2, 2004 Review first published: Issue 4, 2010
| Date | Event | Description |
|---|---|---|
| 12 October 2018 | New search has been performed | The review has been updated. |
| 12 October 2018 | New citation required but conclusions have not changed | The title of the review has been changed. Conclusions not changed. This update includes 12 new studies not included in the original 2010 review. |
| 12 May 2010 | Feedback has been incorporated | In response to comments from a reader (reproduced in the 'Feedback' section of this review), we have made changes to the review in the 'Background', 'Discussion', the 'Conclusions', 'Abstract' and 'Plain Language Summary'. |
| 14 April 2010 | Amended | Data on some ongoing studies has been added |
| 14 July 2008 | Amended | Converted to new review format. |
| 14 March 2008 | Amended | New author team produced revised and updated protocol |
Notes
The current review is an update of the original review, published by the research team in 2010 (Fisher 2010).
Acknowledgements
Thanks to the Cochrane Common Mental Disorders Group's editorial team for ongoing support and advice.
Thanks to Mario Álvarez‐Jiménez for his translation of and assistance with two Spanish language articles.
Thanks to Vincent Cheng for his screening and data extraction of one Chinese language article.
Orygen, The National Centre of Excellence in Youth Mental Health is thankful for the support of the Colonial Foundation and Federal Government funding.
Thanks to authors who sent us data, including trial authors Eisler (provided data for Russell 1987, Dare 2001, Eisler 2000, Le Grange 1992), Herscovici, Robin, and Whitney.
Appendices
Appendix 1. Specialised Register: CCMD's core Medline search strategy
The search strategy listed below is the weekly OVID Medline search used to inform the Group’s specialised register. It is based on a list of terms for all conditions within the scope of the Cochrane Common Mental Disorders Group plus a sensitive RCT filter. 1. [MeSH Headings]: eating disorders/ or anorexia nervosa/ or binge‐eating disorder/ or bulimia nervosa/ or female athlete triad syndrome/ or pica/ or hyperphagia/ or bulimia/ or self‐injurious behavior/ or self mutilation/ or suicide/ or suicidal ideation/ or suicide, attempted/ or mood disorders/ or affective disorders, psychotic/ or bipolar disorder/ or cyclothymic disorder/ or depressive disorder/ or depression, postpartum/ or depressive disorder, major/ or depressive disorder, treatment‐resistant/ or dysthymic disorder/ or seasonal affective disorder/ or neurotic disorders/ or depression/ or adjustment disorders/ or exp antidepressive agents/ or anxiety disorders/ or agoraphobia/ or neurocirculatory asthenia/ or obsessive‐compulsive disorder/ or obsessive hoarding/ or panic disorder/ or phobic disorders/ or stress disorders, traumatic/ or combat disorders/ or stress disorders, post‐traumatic/ or stress disorders, traumatic, acute/ or anxiety/ or anxiety, castration/ or koro/ or anxiety, separation/ or panic/ or exp anti‐anxiety agents/ or somatoform disorders/ or body dysmorphic disorders/ or conversion disorder/ or hypochondriasis/ or neurasthenia/ or hysteria/ or munchausen syndrome by proxy/ or munchausen syndrome/ or fatigue syndrome, chronic/ or obsessive behavior/ or compulsive behavior/ or behavior, addictive/ or impulse control disorders/ or firesetting behavior/ or gambling/ or trichotillomania/ or stress, psychological/ or burnout, professional/ or sexual dysfunctions, psychological/ or vaginismus/ or Anhedonia/ or Affective Symptoms/ or *Mental Disorders/
2. [Title/ Author Keywords]: (eating disorder* or anorexia nervosa or bulimi* or binge eat* or (self adj (injur* or mutilat*)) or suicide* or suicidal or parasuicid* or mood disorder* or affective disorder* or bipolar i or bipolar ii or (bipolar and (affective or disorder*)) or mania or manic or cyclothymic* or depression or depressive or dysthymi* or neurotic or neurosis or adjustment disorder* or antidepress* or anxiety disorder* or agoraphobia or obsess* or compulsi* or panic or phobi* or ptsd or posttrauma* or post trauma* or combat or somatoform or somati#ation or medical* unexplained or body dysmorphi* or conversion disorder or hypochondria* or neurastheni* or hysteria or munchausen or chronic fatigue* or gambling or trichotillomania or vaginismus or anhedoni* or affective symptoms or mental disorder* or mental health).ti,kf.
3. [RCT filter]: (controlled clinical trial.pt. or randomised controlled trial.pt. or (randomi#ed or randomi#ation).ab,ti. or randomly.ab. or (random* adj3 (administ* or allocat* or assign* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)).ab. or placebo*.ab,ti. or drug therapy.fs. or trial.ab,ti. or groups.ab. or (control* adj3 (trial* or study or studies)).ab,ti. or ((singl* or doubl* or tripl* or trebl*) adj3 (blind* or mask* or dummy*)).mp. or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or randomised controlled trial/ or pragmatic clinical trial/ or (quasi adj (experimental or random*)).ti,ab. or ((waitlist* or wait* list* or treatment as usual or TAU) adj3 (control or group)).ab.)
4. (1 and 2 and 3)
Records are screened for reports of RCTs within the scope of the Cochrane Common Mental Disorders Group. Secondary reports of RCTs are tagged to the appropriate study record.
Appendix 2. Database searches (2008)
The Cochrane Collaboration Depression, Anxiety and Neuroses Controlled Trials Register (CCDANCTR) was searched in August 2008 using the following terms:
CCDANCTR‐Studies Diagnosis = Anorexia or "Eating Disorders" and Intervention = "Family Therapy"
CCDANCTR‐References Keyword = Anorexia or "Eating Disorders" and Title ="Family Therapy" or "Family Intervention" or "Family Treatment" or "Family‐Based" or "Family Based" or Abstract = "Family Therapy" or "Family Intervention" or "Family Treatment" or "Family‐Based" or "Family Based" or Keyword = "Family Therapy" or "Family Intervention" or "Family Treatment" or "Family Based" or "Family‐Based"
A search of the following electronic databases was undertaken by the review authors:
MEDLINE (1950‐Week 2 January 2008)
PSYCINFO (1950‐Week 2 January 2008)
EMBASE (1950‐Week 2 January 2008)
The search string used to search each of these databases is listed below:
| Medline | PsycInfo | Embase |
| 1. exp Eating Disorders/ 2. Anorexia/ or Anorexia Nervosa/ 3. 1 or 2 4. Family Therapy/ 5. family therap$.tw. 6. family based therap$.tw. 7. family‐based therap$.tw. 8. systems therap$.tw. 9. family system$ therap$.tw. 10. family treatment$.tw. 11. family intervention$.tw. 12. or/4‐11 13. 3 and 12 14. clinical trial.pt. 15. clinical trial$.mp. 16. random$.mp. 17. placebo.ti,ab. 18. groups.ti,ab. 19. or/14‐18 20. 13 and 19 |
1. exp Eating Disorders/ 2. Anorexia Nervosa/ 3. 1 or 2 4. Family Therapy/ 5. Family Intervention/ 6. Conjoint Therapy/ 7. family therap$.tw. 8. family based therap$.tw. 9. family‐based therap$.tw. 10. systems therap$.tw. 11. family system$ therap$.tw. 12. family treatment$.tw. 13. family intervention$.tw. 14. conjoint therap$.tw. 15. or/4‐14 16. 3 and 15 17. Clinical Trials/ 18. controlled trial$.tw. 19. (controlled studies or controlled study).tw. 20. random$.tw. 21. Random Sampling/ 22. ((singl$ or doubl$ or trebl$ or tripl$) adj5 (blind$ or dummy or mask$)).tw. 23. placebo$.mp. 24. or/17‐23 25. 16 and 24 |
1. exp Eating Disorders/ 2. Anorexia Nervosa/ 3. 1 or 2 4. Family Therapy/ 5. Family Intervention/ 6. family therap$.tw. 7. family based therap$.tw. 8. family‐based therap$.tw. 9. systems therap$.tw. 10. family system$ therap$.tw. 11. family treatment$.tw. 12. family intervention$.tw. 13. conjoint therap$.tw. 14. or/4‐13 15. exp controlled study/ 16. (controlled trial$ or controlled study or controlled studies).tw. 17. exp clinical trial/ 18. (clinical trial$ or clinical study or clinical studies).tw. 19. random$.tw. 20. single blind procedure/ 21. double blind procedure/ 22. ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$ or dummy)).tw. 23. placebo$.mp. 24. or/15‐23 25. 3 and 4 and 24 |
Additionally, ClinicalTrials.gov and the ANZAED Conference abstract book (to 2007) were also searched at this time.
Appendix 3. Database searches (2016)
OVID PsycINFO (21‐Apr‐2016) [RCT filter] 1. treatment effectiveness evaluation.sh. 2. clinical trials.sh. 3. mental health program evaluation.sh. 4. placebo.sh. 5. placebo$.ti,ab. 6. randomly.ab. 7. randomi#ed.ti,ab. 8. trial$.ti,ab. 9. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 10. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 11. "2000".md. 12. factorial$.ti,ab. 13. allocat$.ti,ab. 14. assign$.ti,ab. 15. volunteer$.ti,ab. 16. (crossover$ or cross over$).ti,ab. 17. (quasi adj (experimental or random$)).mp. 18. ((waitlist* or wait* list* or treatment as usual or TAU) adj3 (control or group)).ab. 19. (random* adj3 (administ* or class* or control* or determine* or divide* or distribut* or expose* or fashion or number* or place* or recruit* or subsitut* or treat*)).ab. 20. or/1‐19 [Condition] 21. exp Anorexia Nervosa/ 22. anorexi*.ti,ab,id. 23. or/21‐22 [Intervention] 24. exp FAMILY THERAPY/ 25. FAMILY INTERVENTION/ 26. "3313".cc. 27. family based.ti,ab,id. 28. (family adj2 (therap* or psychotherap* or intervention* or treatment*)).ti,ab,id. 29. FBT.ab. 30. or/24‐29 31. (20 and 23 and 30) 32. (2008* or 2009* or 2010* or 2011* or 2012* or 2013* or 2014* or 2015* or 2016*).yr,an,up. 33. (31 and 32)
PubMed (all years to 21‐Apr‐2016) #15 (#6 AND #9 AND #14) #14 (#10 OR #11 OR #12 OR #13)) #13 "eating disorder" OR "eating disorders" #12 "Feeding and Eating Disorders"[Majr] #11 anorexi*[Title/Abstract] #10 "Anorexia Nervosa"[Mesh] #9 (#7 OR #8) #8 (family[Title/Abstract] OR multifamily[Title/Abstract] OR families[Title/Abstract]) #7 "Family Therapy"[Mesh] #6 (#1 OR #2 OR #3 OR #4 OR #5) #5 (randomised OR randomised OR RCT) #4 (random* AND (allocat* OR assign* OR divid*)) #3 randomly[Title/Abstract] #2 (treatment as usual[Title/Abstract]) OR TAU[Title/Abstract] #1 (((waitlist OR (wait* AND list*)) AND (control OR group)))
Appendix 4. Database searches (2018)
CENTRAL 31
MEDLINE 10
Embase 30
PsycINFO 24
Total=95 Duplicates=38 To screen, n=57
World Health Organisations' trials portal (ICTRP), n=8
ClinicalTrials.gov, n=14
DART‐Europe E‐theses Portal, n= 3
EThOS ‐ the British Libraries e‐theses online service, n= 2
Open Access Theses and Dissertations, n=18
ProQuest Dissertations and theses database, n=3
Search Strategies
1. Bibliographic Databases
Cochrane Central Register of Controlled Trials : Issue 5 of 12, May 2018 Date Run:01/06/18 10:50:40.895 #1 MeSH descriptor: [Feeding and Eating Disorders] 1 tree(s) exploded 1400 #2 (eat* near/3 disorder*) 2628 #3 MeSH descriptor: [Anorexia] this term only 327 #4 MeSH descriptor: [Anorexia Nervosa] this term only 483 #5 anorexi* 4852 #6 #1 or #2 or #3 or #4 or #5 6972 #7 MeSH descriptor: [Family Therapy] this term only 942 #8 (famil* near/3 therap*) 3415 #9 family based 11793 #10 fbt 117 #11 (famil* near/2 (therap* or psychotherap* or intervention* or treatment*)) 4809 #12 (#7 or #8 or #9 or #10 or #11) 14938 #13 (#6 and #12) 515 [170, became 31 when pre 2016 results were removed]
Ovid MEDLINE(R) ALL 1946 to May 31, 2018 1 exp Eating Disorders/ 27799 2 (eat$ adj3 disorder$).ti,ab,kw,ot. 18202 3 Anorexia/ 4699 4 Anorexia Nervosa/ 12187 5 anorexi*.ti,ab,kw,ot. 30509 6 (1 or 2 or 3 or 4 or 5) 53264 7 Family Therapy/ 8478 8 (famil$ adj3 therap$).ti,ab,kw,ot. 6096 9 family based.ti,ab,kw,ot. 6515 10 fbt.ti,ab,kw,ot. 334 11 (famil$ adj2 (therap* or psychotherap* or intervention* or treatment*)).ti,ab,kw,ot. 14676 12 (7 or 8 or 9 or 10 or 11) 26208 13 (6 and 12) 825 14 randomized controlled trial.pt.462930 15 controlled clinical trial.pt.92455 16 (randomized or randomised).ab.495272 17 placebo.ab.189699 18 clinical trials as topic.sh.183920 19 randomly.ab.291800 20 trial.ti.183563 21 (13 and 20) 30 22 (2016* or 2017* or 2018*).yr,dt,ed,ep.3784603 23 (21 and 22) 10
Ovid Embase 1974 to 2018 May 31 Search Strategy 1 exp eating disorder/46316 2 (eat$ adj3 disorder$).ti,ab,kw,ot.25280 3 anorexia/54644 4 anorexi*.ti,ab,kw,ot.42798 5 Family Therapy/12941 6 (famil$ adj3 therap$).ti,ab,kw,ot.9601 7 family based.ti,ab,kw,ot.7846 8 fbt.ti,ab,kw,ot.453 9 (famil$ adj2 (therap* or psychotherap* or intervention* or treatment*)).ti,ab,kw,ot.16805 10 or/1‐4113157 11 or/5‐931751 12 (10 and 11) 1323 13 random$.ti,ab,kw,ot.1311508 14 (12 and 13) 163 15 (2016* or 2017* or 2018*).yr,dc.4325141 16 (14 and 15) 30
Ovid PsycINFO 1987 to May Week 4 2018 1 exp eating disorders/26155 2 (eat$ adj3 disorder$).ti,ab.23032 3 anorexi$.ti,ab.13073 4 (1 or 2 or 3) 33827 5 exp family therapy/16661 6 exp Family Intervention/2748 7 (famil$ adj3 therap$).ti,ab.16649 8 family based.ti,ab.3663 9 fbt.ti,ab.234 10 (famil$ adj2 (therap* or psychotherap* or intervention* or treatment*)).ti,ab.22732 11 (5 or 6 or 7 or 8 or 9 or 10) 32113 12 (4 and 11) 1233 13 random$.ti,ab.160444 14 (12 and 13) 139 15 (2016* or 2017* or 2018*).yr,an,up. 502889 16 (14 and 15) 24
2. Theses Databases
DART‐Europe E‐theses Portal Searched via: http://www.dart‐europe.eu/ Searched on: Monday June 4th 2018 ((anorexia) and (family)) EThOS ‐ the British Libraries e‐theses online service Searched via: http://ethos.bl.uk/ Searched on: Monday June 4th 2018 ((anorexia) and (family)) Open Access Theses and Dissertations Searched via: https://oatd.org Searched on: Monday June 4th 2018 ((anorexia) and (family)) Dissertations and theses database Searched via: ProQuest Searched on: Monday June 4th 2018 ((anorexia) and (family))
3. Trial Registries
ICTRP Searched via: http://apps.who.int/trialsearch/default.aspx Searched on: Monday June 4th 2018 Search terms: ((anorexia) and (family)) Clinical Trials.Gov Searched via: https://www.clinicaltrials.gov/ Searched on: Monday June 4th 2018 Search terms: ((anorexia) and (family))
Data and analyses
Comparison 1. Family therapy approaches vs standard care/treatment as usual.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 2 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 3.50 [1.49, 8.23] |
| 1.1 family‐based therapy | 1 | 41 | Risk Ratio (M‐H, Random, 95% CI) | 6.91 [0.95, 50.35] |
| 1.2 other | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [1.16, 7.73] |
| 2 Remission long‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 General Functioning | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Other | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Dropouts during therapy | 3 | 137 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.44, 2.34] |
| 4.1 systems family therapy | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.11, 2.96] |
| 4.2 family‐based therapy | 1 | 41 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.29, 4.51] |
| 4.3 Other | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.33, 5.45] |
| 5 Eating disorder psychopathology post‐intervention | 2 | 109 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.49, 0.27] |
| 5.1 other | 2 | 109 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.49, 0.27] |
| 6 Weight (BMI) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Other | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Relapse during treatment | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.37, 1.15] |
| 7.1 family‐based therapy | 1 | 41 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.14, 1.89] |
| 7.2 Other | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.37, 1.30] |
Comparison 2. Family therapy approaches vs psychological interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 7 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.89, 1.67] |
| 1.1 family‐based therapy | 7 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.89, 1.67] |
| 2 Remission short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Remission long‐term follow‐up | 6 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.28] |
| 3.1 family‐based therapy | 6 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.28] |
| 4 Dropouts during treatment | 6 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.46, 2.78] |
| 4.1 family‐based therapy | 6 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.46, 2.78] |
| 5 Eating disorder psychopathology post‐intervention | 7 | 262 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.32, 0.66] |
| 5.1 family‐based therapy | 6 | 212 | Std. Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.32, 0.83] |
| 5.2 other | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.78, 0.35] |
| 6 Eating disorder psychopathology short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Eating disorder psychopathology long‐term follow‐up | 6 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.50, 0.47] |
| 7.1 family based therapy | 6 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.50, 0.47] |
| 8 Weight (BMI, BMI%ile, %ABW) post‐intervention | 6 | 210 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [0.01, 0.63] |
| 8.1 family‐based therapy | 6 | 210 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [0.01, 0.63] |
| 9 Weight (BMI%ile) short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Weight (BMI, BMI%ile, %ABW) long‐term follow‐up | 6 | 198 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.16, 0.45] |
| 10.1 family‐based therapy | 6 | 198 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.16, 0.45] |
| 11 Relapse during treatment | 4 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.54, 2.08] |
| 11.1 family‐based therapy | 4 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.54, 2.08] |
| 12 Relapse long‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 12.1 Family based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Family therapy approaches vs educational interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission long‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 other | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Family therapy approaches short‐term vs family therapy approaches long‐term.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission long‐term follow‐up (mean 3.96 years) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Return to functioning (school or work) follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Dropouts during therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Eating disorder psychopathology long‐term follow‐up (EDE) note large dropout | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Weight (BMI) post‐intervention | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Weight (BMI) follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Relapse during treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Family therapy approaches conjoint vs family therapy approaches separated.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 family‐based therapy | 2 | 134 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.38, 0.83] |
| 2 Remission short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Remission long‐term follow‐up | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 family‐based therapy | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.67, 1.09] |
| 4 Dropouts during therapy | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 family‐based therapy | 2 | 134 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.60, 2.68] |
| 5 Dropouts during follow‐up (5 years) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Eating disorder psychopathology post‐intervention (EAT) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 family‐based therapy | 2 | 58 | Mean Difference (IV, Random, 95% CI) | ‐1.85 [‐10.01, 6.31] |
| 7 Eating disorder psychopathology follow‐up (EAT) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Eating disorder psychopathology post‐intervention (MR) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 family‐based therapy | 2 | 58 | Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.95, 0.03] |
| 9 Eating disorder psychopathology post‐intervention (EDI) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Eating disorder psychopathology follow‐up (EDI) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Eating disorder psychopathology post‐intervention (EDE) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Eating disorder psychopathology short‐term follow‐up (EDE) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 family based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Eating disorder psychopathology long‐term follow‐up (EDE) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Weight (%Median BMI) post‐intervention | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Weight (%Median BMI) short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Weight (%Median BMI) long‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Weight (%ABW) post‐intervention | 2 | 58 | Mean Difference (IV, Random, 95% CI) | ‐2.75 [‐18.50, 13.00] |
| 17.1 family‐based therapy | 2 | 58 | Mean Difference (IV, Random, 95% CI) | ‐2.75 [‐18.50, 13.00] |
| 18 Weight (%ABW) follow‐up (5 years) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Relapse post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 19.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Relapse follow‐up (5 years) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 20.1 familybased therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 6. Family therapy approaches vs family therapy approaches plus meal.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 family‐based therapy | 2 | 35 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.23, 2.10] |
| 2 Remission short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Remission long‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 family‐based therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Family function post‐intervention Family Health Scale | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Dropouts | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 family‐based therapy | 2 | 35 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.02, 6.86] |
| 6 Eating disorder psychopathology post‐intervention (MR) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 family‐based therapy | 2 | 35 | Mean Difference (IV, Random, 95% CI) | 0.54 [‐0.78, 1.85] |
| 7 Eating disorder psychopathology short‐term follow‐up (MR) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 family based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Eating disorder psychopathology long‐term follow‐up (MR) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Weight (BMI, EBW%) post‐intervention | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 family‐based therapy | 2 | 35 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.85, 0.48] |
| 10 Weight (EBW%) short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Weight (BMI) long‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 family‐based therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 7. Individual family therapy approaches vs group family therapy approaches.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Family function post‐intervention (carers' LEE) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Family function follow‐up (carers' LEE) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Dropouts | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Eating disorder psychopathology post‐intervention (SEED‐AN) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Eating disorder psychopathology follow‐up (SEED‐AN) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Weight (BMI) post‐intervention | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 Weight (BMI) follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 8. Family‐based therapy vs systemic family therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Remission short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Dropouts during therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 9. Inpatient family therapy approaches vs day‐patient family therapy approaches.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Dropouts | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Eating disorder psychopathology short‐term follow‐up (EDI) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Weight (%EBW) short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Relapse at short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 10. Family‐based therapy vs family‐based therapy plus parent coaching.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Dropouts | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Eating disorder psychopathology post‐intervention (EDE) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Weight (BMI) post‐intervention | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 11. Family‐based therapy plus medical stabilisation vs family‐based therapy plus weight restoration.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Remission short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Remission long‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Dropouts | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Eating disorder psychopathology (EDE) long‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Weight (%EBW change) long‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 Relapse at long‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 12. Family‐based therapy vs family‐based therapy plus consultation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 13. Family therapy approaches vs standard care/treatment as usual (subgroup by age).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention (subgroup by age) | 2 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 3.50 [1.49, 8.23] |
| 1.1 Adult | 2 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 3.50 [1.49, 8.23] |
| 2 Remission long‐term follow‐up | 1 | 41 | Risk Ratio (M‐H, Random, 95% CI) | 6.09 [0.33, 110.84] |
| 2.1 Adult | 1 | 41 | Risk Ratio (M‐H, Random, 95% CI) | 6.09 [0.33, 110.84] |
| 3 General Functioning | 1 | 59 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.62, 1.62] |
| 3.1 Adolescent | 1 | 59 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.62, 1.62] |
| 4 Dropouts during therapy | 3 | 137 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.44, 2.34] |
| 4.1 Adult | 1 | 41 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.29, 4.51] |
| 4.2 Adolescent | 2 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.32, 2.71] |
| 5 Eating disorder psychopathology post‐intervention | 2 | 109 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.49, 0.27] |
| 5.1 Adult | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.86, 0.28] |
| 5.2 Adolescent | 1 | 59 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.48, 0.54] |
| 6 Weight (BMI) | 1 | 59 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.75, 1.55] |
| 6.1 Adolescent | 1 | 59 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.75, 1.55] |
| 7 Relapse during treatment | 2 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.37, 1.15] |
| 7.1 Adult | 1 | 41 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.14, 1.89] |
| 7.2 Adolescent | 1 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.37, 1.30] |
13.1. Analysis.
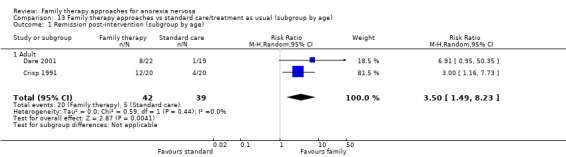
Comparison 13 Family therapy approaches vs standard care/treatment as usual (subgroup by age), Outcome 1 Remission post‐intervention (subgroup by age).
13.2. Analysis.
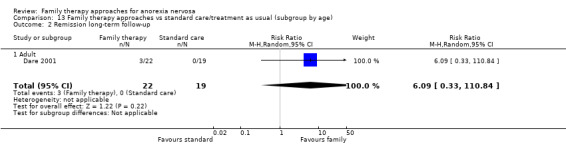
Comparison 13 Family therapy approaches vs standard care/treatment as usual (subgroup by age), Outcome 2 Remission long‐term follow‐up.
13.3. Analysis.
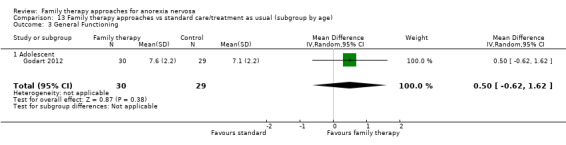
Comparison 13 Family therapy approaches vs standard care/treatment as usual (subgroup by age), Outcome 3 General Functioning.
13.6. Analysis.
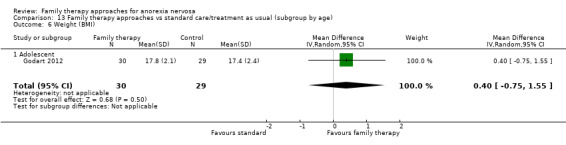
Comparison 13 Family therapy approaches vs standard care/treatment as usual (subgroup by age), Outcome 6 Weight (BMI).
Comparison 14. Family therapy approaches vs psychological interventions (sugroup by age).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Remission post‐intervention | 7 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.89, 1.67] |
| 1.1 Adult | 3 | 76 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.38, 2.07] |
| 1.2 Adolescent | 4 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.87, 1.92] |
| 2 Remission short‐term follow‐up | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.94, 1.44] |
| 2.1 Adolescent | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.94, 1.44] |
| 3 Remission long‐term follow‐up | 6 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.28] |
| 3.1 Adult (note russell is 5 year) | 2 | 33 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.39, 1.21] |
| 3.2 Adolescent | 4 | 167 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.95, 1.34] |
| 4 Dropouts during treatment | 6 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.46, 2.78] |
| 4.1 Adult | 3 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [0.44, 4.70] |
| 4.2 Adolescent | 3 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.18, 3.91] |
| 5 Eating disorder psychopathology post‐intervention | 7 | 262 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.32, 0.66] |
| 5.1 Adult | 3 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.70, 0.34] |
| 5.2 Adolescent | 4 | 177 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [‐0.28, 1.17] |
| 6 Eating disorder psychopathology short‐term follow‐up (Lock 2010‐EDE) | 1 | 89 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.69, 0.23] |
| 6.1 Adolescent | 1 | 89 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.69, 0.23] |
| 7 Eating disorder psychopathology long‐term follow‐up | 6 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.50, 0.47] |
| 7.1 Adult | 2 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.78, 0.65] |
| 7.2 Adolescent | 4 | 165 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.35, 0.68] |
| 8 Weight (BMI, BMI%ile, %ABW) post‐intervention | 6 | 210 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [0.01, 0.63] |
| 8.1 Adult | 2 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐1.10, 0.56] |
| 8.2 Adolescent | 4 | 178 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.14, 0.74] |
| 9 Weight (BMI%ile) short‐term follow‐up | 1 | 89 | Mean Difference (IV, Random, 95% CI) | 2.30 [‐7.28, 11.88] |
| 9.1 Adolescent | 1 | 89 | Mean Difference (IV, Random, 95% CI) | 2.30 [‐7.28, 11.88] |
| 10 Weight (BMI, BMI%ile, %ABW) long‐term follow‐up | 6 | 198 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.16, 0.45] |
| 10.1 Adult | 2 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.21, 0.21] |
| 10.2 Adolescent | 4 | 166 | Std. Mean Difference (IV, Random, 95% CI) | 0.27 [‐0.04, 0.57] |
| 11 Relapse during treatment | 4 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.54, 2.08] |
| 11.1 Adult | 3 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.44, 2.44] |
| 11.2 Adolescent | 1 | 21 | Risk Ratio (M‐H, Random, 95% CI) | 1.1 [0.37, 3.27] |
| 12 Relapse long‐term follow‐up | 1 | 77 | Risk Ratio (M‐H, Random, 95% CI) | 2.49 [0.55, 11.21] |
| 12.1 Adolescent | 1 | 77 | Risk Ratio (M‐H, Random, 95% CI) | 2.49 [0.55, 11.21] |
14.2. Analysis.
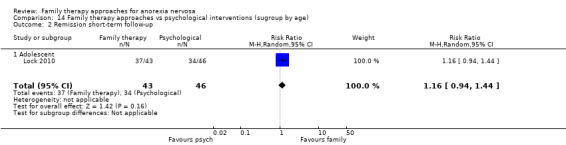
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 2 Remission short‐term follow‐up.
14.6. Analysis.
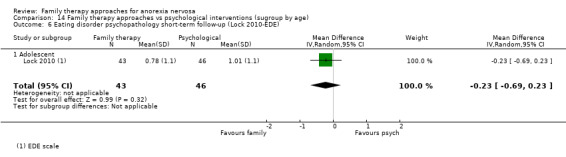
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 6 Eating disorder psychopathology short‐term follow‐up (Lock 2010‐EDE).
14.9. Analysis.
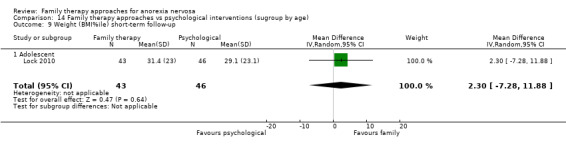
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 9 Weight (BMI%ile) short‐term follow‐up.
14.12. Analysis.
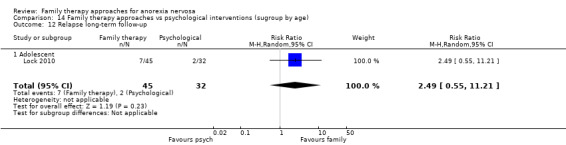
Comparison 14 Family therapy approaches vs psychological interventions (sugroup by age), Outcome 12 Relapse long‐term follow‐up.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Agras 2014.
| Methods | RCT | |
| Participants | Country: USA
Diagnostic tool: DSM‐IV except for the amenorrhoea criterion and with up to 87% of their IBW
No. screened: 564
No. randomised: Total: 164; FBT: 82; SyFT 82
No. started trial: FBT 78; SyFT 80
No. dropped out during intervention: Total: 40; FBT: 20; SyFT 20
No. dropped out during follow‐up: No detail
No. analysed (observed case): Total: 158; FBT: 78; SyTF 80 Mean age in years (SD): Total: 15.3 (1.8); FBT: 15.1 (1.7), SyFT: 15.6 (1.8) Age range in years: Total: Between ages 12 ‐18 Gender %: Total female 89.2%; FBT 85.9%; SyTF 92.5% Subtype purging %: No detail Subtype restricting %: No detail Age of onset: No detail Duration of illness: Total 13.5 (13.9) moths; FBT:11.6 (9.8); SyFT:15.4 (16.9) Baseline weight: Total: mean IBW 81.9%; FBT: 82.2% (3.8); SyFT: 81.7% (3.7) Baseline BMI: No detail Baseline eating disorder scale score: Total: No detail; FBT: 1.6 (1.3) EDE; SyFT: 1.9 (1.5) EDE Baseline eating disorder scale score: Total: No detail; FBT: 10.7 (8.0) Yale‐Brown‐Cornell Eating Disorder Scale; SyFT: 12.1 (8.4) Yale‐Brown‐Cornell Eating Disorder Scale Comorbidity: Total: Dep ‐ 25.3%, Anx ‐ 10.8%, OCD ‐ 11.4 %, Other ‐ 10.1%; FBT: Dep ‐ 25.6%, Anx ‐ 14.1%, OCD ‐ 10.2%, Other ‐ 9.0%; SyFT: Dep ‐ 25.0%, Anx ‐ 7.5%, OCD ‐ 12.5 %, Other ‐ 11.2% Details on living arrangements: No detail Family education/employment/income: No detail Recruitment strategy: 6 clinical sites experienced in the treatment of AN, 1 site had difficulty with recruitment and was replaced by another site Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatient
Training/qualification of care provider(s): Yes: 26 therapists were doctorate‐ or masters‐level psychologists, psychiatrists, or social workers; mean of 6 years’ experience in the treatment of adolescent AN
Treatment manual: Yes, both treatments
Supervision of treatment: Therapists were trained in separate workshops for each treatment and then completed treatment for 2 cases with supervision from experts in each type of family therapy (JL for FBT and ED for SyFT). Supervision of therapists continued at weekly intervals throughout the treatment phase and were provided centrally by the data and co‐ordinating centre and at the site level by a trained supervisor, with each treatment supervised separately. Elements of supervision included listening to therapy tapes, case discussions focusing on the process of treatment, behavioural rehearsal, and treatment planning
Adherence to treatment: Yes: Fidelity to each treatment was assessed at 1 of the sites by 6 raters with a graduate degree in psychology or social work and experience in treating eating disorders. Raters were trained in 1 of the 2 treatments by reading the manual and viewing tapes of the training workshop for clinicians and were also trained in the application of the appropriate fidelity instrument for which reliability was established. Each site provided 4 videotapes per family randomly sampled from each of the following blocks of sessions: 1 to 4, 5 to 8, 9 to 12, and 13 to 16. A total of 421 therapy tapes were audited (210 FBT and 211 SyFT). The overall mean scores for fidelity were FBT 4.15 (0.94) and SyFT 4.38 (0.48) on a 0 to 6 scale
Intervention group 1
Description: Family‐based therapy Length: 60 min, 16 sessions over 9 months Intervention group 2 Description: Systemic family therapy There is no family meal or specific emphasis on normalisation of eating or weight, although if the family raises this issue, the therapist will help them address it Length: 60 min, 16 sessions over 9 months |
|
| Outcomes |
Eating psychopathology EDE Yale‐Brown‐Cornell EDS Behavioural indices Remission (defined as achieving a minimum of 95% of the IBW) Ideal body weight % (IBW) General psychopathology and obsessionality BDI STAI Child Yale‐Brown Obsessive Compulsive Scale Rosenberg self‐esteem scale Global pathology and interpersonal functioning Quality of Life and Enjoyment Scale (short form) |
|
| Notes | The study was supported in part by the following grants from the National Instituteof Mental Health: 1UO1 MH076290 (Dr Agras), MH076254 (Dr Brandt), MH 076251 (Dr Halmi), MH076250 (Dr Johnson), MH 076255 (Dr Wilfley), and076252 (Dr Woodside). Standard deviations often not reported so data for eating disorder psychopathology and weight could not be used |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised within sites to 1 of the 2 family therapies using a computer‐generated programme |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded to the treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Results for all participants who began treatment reported |
| Selective reporting (reporting bias) | Unclear risk | All measures appear to have been reported on; but in many cases the SDs were not reported |
| Other bias | Unclear risk |
|
Ball 2004.
| Methods | RCT | |
| Participants | Country: Australia
Diagnostic tool: DSM‐IV modified to also include participants with < 90% ABW
No. screened: No detail
No. randomised: Total: 25; BFT: 12; CBT: 13
No. started trial: No detail
No. dropped out during intervention: Total: 7; BFT: 3; CBT: 4
No. dropped out during follow‐up: No detail
No. analysed (observed case): BFT: 9; CBT: 9 Mean age in years (SD): BFT: 17.58 (3.37); CBT: 18.45 (2.57) Age range in years: Total: 13 ‐ 23 (totals only provided) Gender %: 100% female Subtype purging %: Total: 36% (N 9); BFT: 25% (N 3); CBT: 46.2% (N 6) Subtype restricting %: Total: 64% (N 16); BFT: 75% (N 9); CBT: 53.8 % (N 7) Age of onset: No detail Duration of illness: No detail Baseline weight: No detail Baseline BMI: BFT: 16.45 (0.85); CBT: 16.06 (1.58) Baseline eating disorder scale score (EDE): BFT: 2.00 (0.2); CBT: 2.05 (0.26) Baseline eating disorder scale score (MRS): BFT: 6.09 (1.51); CBT: 5.94 (1.07) Baseline purging: No detail Comorbidity: No detail Details on living arrangements: Total: All “currently living with their family” (pg. 305) Family education/employment/income: No detail Recruitment strategy: Patients evaluated at eating disorder unit Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatient Training/qualification of care provider(s): Yes: 6 female clinical psychologists with post‐graduate qualifications in CBT and eating disorders ‐ therapist crossed across treatments Treatment manual: No: No for CBT; unclear for BFT “based on a number of behavioural interventions described by Robin 1989. Supervision of treatment: No detail Adherence to treatment: No detail Intervention group 1 Description: Behavioural family therapy Behavioural family therapy (Robin 1989), plus 4 nutritional counselling sessions Length: 25 sessions of 1 hour duration over 12 months Intervention group 2 Description: Individual Cognitive Behavioural Therapy Based on Garner 1982, therapy to address maladaptive core beliefs often associated with feelings of failure and inadequacy. Plus 4 nutritional counselling sessions Length: 25 sessions of 1 hour duration over 12 months | |
| Outcomes |
Eating psychopathology
EDE (Cooper 1987a; Cooper 1987b)
Scales of Body Dissatisfaction, EDI (Garner 1983)
Anorectic Behaviour Observation Scale (Vandereycken 1992)
Behavioural indices
Weight, BMI
Menstruation
Good outcome/intermediate outcome/poor outcome General psychopathology Depression (Beck 1961) STAI (Speilberger 1970) Obsessionality Perfectionism Scale from the EDE (Cooper 1987a; Cooper 1987b) Global pathology and interpersonal functioning State Self Esteem Scale (Heatherton 1991) Family functioning Eating Conflict Scale of the IBC (Robin 1989) (Prinz 1978) |
|
| Notes | Included in family therapy vs individual psychological intervention Family therapy categorised as family‐based therapy Funded by: Prince Henry Hospital Coast Centenary Grant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk |
|
Besharat 2001.
| Methods | RCT | |
| Participants | Country: Not reported in paper (author affiliation listed as Iran; personal correspondence revealed study undertaken in the UK)
Diagnostic tool: DSM‐IV and ICD‐10
No. screened: No detail
No. randomised: 58 (although the results of 62 participants are reported)
No. started trial: No detail
No. dropped out during intervention: No detail
No. dropped out during follow‐up:
No. analysed (observed case): 62 (despite 58 being included in study) Mean age in years (SD): Total: 26.1 (6.6) Age range in years: Total: No detail Gender %: No detail Subtype purging %: No detail Subtype restricting %: No detail Age of onset: Total: No detail Duration of illness: No detail Baseline weight: The ABW, expressed as a percentage of the mean population weight matched for age and height, for the entire sample was 71.8 kg (7.8%) Baseline BMI: No detail Baseline eating disorder scale score: No detail Baseline eating disorder scale score: No detail Baseline purging: No detail Comorbidity: No detail (although must be BN as mixed sample) Details on living arrangements: In 53.3% the family composition was dual‐parental, composed of mother, father and participant, while 26.6% were single‐parent families, mainly mother and the participant, and 20% were marital families, husband and wife Family education/employment/income: Recruitment strategy: No detail Exclusion criteria: No detail |
|
| Interventions | Setting of care: No detail
Training/qualification of care provider(s): No detail
Treatment manual: No detail
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Family therapy No further details Length: Up to 1 year Intervention group 2 Description: Supportive therapy No further details Length: Up to 1 year Intervention group 3 Description: Individual focal psychoanalytic psychotherapy No further details Length: Up to 1 year Intervention group 4 Description: Cognitive analytic therapy No further details Length: Up to 1 year |
|
| Outcomes | Standardised clinical family interview expressed emotion Morgan‐Russell outcome assessment |
|
| Notes | The results from the studies are only reported as group totals for AN versus BN participants. No information is provided for study outcomes by treatment group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants described as "randomly assigned" in abstract. No further details |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 58 study participants are described in the abstract. However, outcomes for 62 participants are reported in Table 1 |
| Selective reporting (reporting bias) | High risk | No results from the actual RCT for therapy outcomes reported by intervention group. Outcomes only reported by AN vs BN and pre‐intervention Expressed Emotion results |
| Other bias | Unclear risk | No useable data |
Crisp 1991.
| Methods | RCT | |
| Participants | Country: UK
Diagnostic tool: DSM‐IIIR
No. screened: No detail
No. randomised: 90: Inpatient (includes FT): 30; Outpatient (includes FT): 20; Outpatient group: 20; Assessment only: 20
No. started trial: 73: Inpatient (includes FT): 18; Outpatient (includes FT): 18; Outpatient group: 17 (1 died); Assessment only: 20
No dropped out during intervention: (not fully reported): Outpatient (includes FT): 3 (attended 5 sessions or fewer); Assessment only: 14 dropped out in the sense that they sought treatment elsewhere
No. analysed: 90 (LOCF): Inpatient (includes FT): 30; Outpatient (includes FT): 20; Outpatient group: 20; Assessment only: 20
Mean age in years (SD): Total: 22: Inpatient (includes FT): 23.2 (4.9); Outpatient (includes FT): 21.2 (5.1); Outpatient group: 19.7 (2.6); Assessment only: 21.9 (4.5)
Age range in years: Total: 20 ‐ 23 (not given by group) Note ‐ the review authors note that this age range is inconsistent with the mean ages provided per treatment group (i.e. outpatient group mean is stated as 19.7).
Gender: All female participants
Subtype: No detail
Age of onset in years (SD): Inpatient (includes FT): 19.8 (4.7); Outpatient (includes FT): 18.4 (3.9); Outpatient group: 17.4 (3.9); Assessment only: 17.4 (3.2)
Duration of illness in months (SD): Total: 39; range 4 ‐ 107 months; Inpatient (includes FT): 41.0 (30.17); Outpatient (includes FT): 33.4 (25.9); Outpatient group: 27.5 (25.8); Assessment only: 53.5 (52.9)
Baseline weight in kgs: Inpatient (includes FT): 40.8 (6.1); Outpatient (includes FT): 40.3 (3.8); Outpatient group: 40.2 (6.0); Assessment only: 41.0 (6.1)
Baseline deviation below MMPW % (SD): Inpatient (includes FT): 28.0 (9.4); Outpatient (includes FT): 26.5 (6.9); Outpatient group: 26.2 (8.7); Assessment only: 25.0 (8.5)
Baseline BMI: Inpatient (includes FT): 15.3; Outpatient (includes FT): 15.5; Outpatient group: 15.5; Assessment only: 15.7
Baseline eating disorder scale score (MRS): Inpatient (includes FT): 3.5 (0.2); Outpatient (includes FT): 3.9 (0.3); Outpatient group: 3.8 (0.4); Assessment only: 3.5 (0.3)
Baseline purging ("usually vomiting"): Inpatient (includes FT): 5; Outpatient (includes FT): 5; Outpatient group: 5; Assessment only: 7
Baseline Purging ("usually bulimic"): Inpatient (includes FT): 3; Outpatient (includes FT): 2; Outpatient group: 5; Assessment only: 3
Comorbidity: No details
Details on living arrangements: No details
Family education/employment/income: No details
Recruitment strategy: Not stated other than “successive referrals” to treatment centre Exclusion criteria:
|
|
| Interventions | Setting of care: Inpatient and outpatient
Training/qualification of care provider(s): Paper states ‘trained and experienced’ no other details
Treatment manual: No detail
Supervision of treatment: No detail
Adherence to treatment: No detail Intervention group 1 Description: Outpatient individual therapy and family therapy 12 outpatient sessions including individual work which nearly always but to a variable extent included some family work (more with the younger participants). Family work emphasised establishment of boundaries, and addressing issues such as enmeshment, conflict avoidance (e.g. non‐communication) and attempted solving of family problems. Dietary counselling also included. Length: Several months Intervention group 2 Description: Outpatient group therapy for participants and outpatient group therapy for parents 10 outpatient psychotherapy group meetings for the individual and 10 group meetings for parents separately. Issues addressed included conflict avoidance, sense of self, family relationships, identification of moods, meaning of weight and shape, management of impulse, communication and relationship skills, with parents additionally addressing support of each other in managing shared problems and difficulties over autonomy as well as parental discord and lifestyle issues. Dietary counselling also included Length: 10 sessions Intervention group 3 Description: Inpatient treatment Inpatient stay of several months including weight restoration with weekly individual therapy, family therapy, group therapy, dietary counselling and occupational therapy using psychodrama and projective art techniques. Followed by 12 sessions of outpatient treatment involving both the participant and the family Length: Several months of inpatient plus outpatient treatment over several months Intervention group 4 Description: 'One off' ‐ no further treatment Referred back to their family doctor or local consultant who received a detailed report of the assessment with advice on further management. “of those in option 4, 6 had no treatment of any kind, six had inpatient treatment, 5 had outpatient hospital treatment and 3 had very regular contact with GP. 6 patients spent almost the entire year in treatment” (pg. 329 Crisp 1991) Length: 'one off' |
|
| Outcomes |
Eating psychopathology
Morgan Russell Assessment Schedule (Morgan 1988) Behavioural indices Well: weight within 15% MMPW; regular menstruation; normal eating Almost well: weight risen to above 85% of MMPW , menstruation returned (but not necessarily regular); aspects of abnormal eating may remain Significantly better: Weight risen to within 85% or still less but risen by 10%, and/or menstruation absent or sporadic; aspects of abnormal eating may remain No change: Weight less than 85% MMPW and/or increased by < 10% and/or menstruation absent or sporadic; abnormal eating Worse: weight loss has occurred or score lower on the Morgan Russell score; amenorrhoea still present |
|
| Notes | Included in family therapy vs standard care/treatment as usual Family therapy categorised as other Also included in family therapy vs individual psychological intervention Family therapy categorised as other Funded by: Marks and Spencer plc, St George’s Hospital Special Trustees and Worshipful Company of Grocers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail : Methods paper pg. 446 “ treatment option drawn by random allocation” with no other statement |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | At 12 months "patients were seen by one of the team uninvolved in the treatment programs and as far as possibly unaware of the treatment allocation" but the methods paper (Gowers) states it was "not possible for the interviewer to be blind to the treatment given" pg. 453 |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were followed up regardless of compliance with treatment. Analysis included all 90 participants who were randomised |
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk |
|
Dare 2001.
| Methods | RCT | |
| Participants | Country: UK Diagnostic tool: DSM‐IV No. screened: No detail No. randomised: Total : 84: Psychoanalytic psychotherapy: 21; Family therapy: 22; Cognitive analytic therapy: 22; Routine treatment: 19 No. started trial: No detail No. dropped out during intervention: Total : 30: Psychoanalytic psychotherapy: 9; Family therapy: 6; Cognitive analytic therapy: 9; Routine treatment: 6; “4 failed to attend the first treatment session. 6 dropped out within the first two months and a further 19 dropped out during the later stages of treatment” (pg. 218). This adds up to 29 ‐ but they stated 54 completed from 84 randomised ‐ these numbers do not match with the numbers for each group. Number dropped out during follow‐up: No detail Number analysed (LOCF): Total : 84; Psychoanalytic psychotherapy: 21; Family therapy: 22; Cognitive analytic therapy: 22; Routine treatment: 19 Number analysed (observed case): Total : 54; Psychoanalytic psychotherapy: 12; Family therapy: 16; Cognitive analytic therapy: 13; Routine treatment: 13 Mean age (SD) in years: Total : 26.3 (6.7); Psychoanalytic psychotherapy: 26.7(6.4); Family therapy: 26.6 (7.6); Cognitive analytic therapy: 27.2 (7.6); Routine treatment: 24.3 (4.5) Age range: No detail Gender %: Total: 2% male (all in the family therapy group): 98% female Subtype: No detail Age of onset in years: Total : 19.0 (5.3); Psychoanalytic psychotherapy: 18.8 (4.2); Family therapy: 20.5 (7.5); Cognitive analytic therapy: 19.9 (4.1); Routine treatment: 16.6 (4.1) Duration of illness in years: Total : 6.3 years (5.9); 79% had received previous treatment (43% of these as inpatients and 19% requiring multiple admissions); Psychoanalytic psychotherapy: 6.7 (5.9) (71% had received previous treatment ‐ 24% as inpatient); Family therapy: 5.8 (4.9) (82% had received previous treatment ‐ 55% as inpatient); Cognitive analytic therapy: 6.7 (7.6) (77% received previous treatment ‐ 36% as inpatient); Routine treatment: 6.1 (5.0) (84% had received previous treatment ‐ 58% as inpatient) Baseline weight in kgs:Total: 41.1 (5.1) ‐ mean average body weight for height (74.3%); Psychoanalytic psychotherapy: 40.8 (4.6) mean average body weight for height (72.8%); Family therapy: 41.0 (6.2) mean average body weight for height (72.8%); Cognitive analytic therapy: 41.9 (4.6) mean average body weight for height (77.3%); Routine treatment: 40.6 (5.2) mean average body weight for height (73.9%) Baseline BMI: Total : 15.4 (1.6); Psychoanalytic psychotherapy: 15.0 (1.6); Family therapy: 15.2 (1.5); Cognitive analytic therapy: 16.0 (1.7); Routine treatment: 15.3 (1.6) Baseline eating disorder scale score (MRS):Total: 5.5 (1.4) Baseline purging % (vomiting daily or at least weekly):Total : 36% Daily only 13%; Psychoanalytic psychotherapy: 15% Daily only 19%; Family therapy: 14% Daily only 9%; Cognitive analytic therapy: 28% Daily only 27%; Routine treatment: 37% Daily only 11% Comorbidity: No detail Details on living arrangements (lived with their parents or another family member): Total : 50%; Psychoanalytic psychotherapy: 52%; Family therapy:59%; Cognitive analytic therapy: 41%; Routine treatment: 47% Details on living arrangements : 24% lived with a marital or common law partner and 26% alone; Psychoanalytic psychotherapy: 14% cohabiting; 33% alone; Family therapy: 27% cohabiting; 14% alone; Cognitive analytic therapy: 32% cohabiting; 27% alone; Routine treatment: 21% cohabiting; 32% alone Family education/employment/income: No detail Recruitment strategy: Sequential referrals to the outpatient eating‐disorder service Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatient Training/qualification of care provider(s): Yes: A psychologist, doctor and a social worker with training in family therapy Treatment manual: No Supervision of treatment: Yes: Bi‐weekly 90 minute group format Adherence to treatment: No detail Intervention group 1 Description: Family‐based therapy Described as 'Family Therapy' in report. Phase 1 focused on the family control of refeeding but participants took an active role to oppose the anorexic eating habits Length: Mean of 13.6 sessions of 1 hour to 1 hour 15 minutes sessions between once a week and once every 3 weeks Intervention group 2 Description: Focal psychoanalytic psychotherapy Non‐directive with no advice given about AN or symptom management but addresses: a) conscious and unconscious meanings of the symptom in terms of the participants' history and their experience with their family, b) the effects of the symptom and its influence on the participants current relationship, and c) the manifestation of those influences in the relationship with the therapist Length: Planned once a week for a year but mean of 24.9 sessions of 50 minute duration Intervention group 3 Description: Cognitive analytic therapy Participants are helped to evolve a formal mapped‐out structure of the place of the anorexia in their experience of themselves and their early and current relationships Length: Planned weekly sessions for 20 weeks then monthly for 3 months but mean number of 12.9 sessions of 50 minute duration Intervention group 4 Description: Routine treatment Included low contact, outpatient management with provision of information and encouragement Length: Planned to be a low‐contact intervention with mean 10.9 sessions of 30 minute duration over approximately 1 year | |
| Outcomes | Eating psychopathology Morgan Russell Assessment Schedule (Morgan 1988) Behavioural indices BMI Recovered: weight > 85% ABW; menstruation returned, no bulimic symptoms Significantly improved: weight > 85% of ABW but amenorrhoea persists and/or occasional bulimic symptoms (< weekly) Improved: weight > 75% ABW and 10% weight gain and/or regular bulimic symptoms (weekly) Poor: weight < 75% ABW or weight gain < 10% or frequent bulimic symptoms (daily) | |
| Notes | Included in family therapy vs standard care/treatment as usual Family therapy categorised as family‐based therapy Also included in family therapy vs individual psychological intervention Family therapy categorised as family‐based therapy Personal communication stated that the cause of death of the participant who died in the routine group was not available in research files Funded by: Leverhulme Foundation and the Mental Health Research Fund | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “a stratified randomisation procedure...the minimization method (Pocock 1982) was used to control for age of onset and the duration of the illness.” Pg. 216 Personal communication stated that stratified randomisation with minimisation was used to control for age of onset, duration of illness, marital status, and presence of symptoms. If minimisation resulted in a tie, a random sequence had been generated by computer and was used. |
| Allocation concealment (selection bias) | Low risk | Quote: "sealed envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: “the follow‐up research clinician was not blind to treatment” pg. 216 |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk |
|
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Unclear risk |
|
Eisler 2000.
| Methods | RCT | |
| Participants | Country: UK Diagnostic tool: DSM‐IV or ICD 10 No. screened: 57 No. randomised: 40: Conjoint FT:19; Separated FT:21 No. started trial: No details No. dropped out during intervention: 4 (not given by group) No. dropped out during follow‐up: No follow‐up data collected, just end of treatment No. analysed: 40 (LOCF): Conjoint FT: 19; Separated FT: 21 Mean age in years (SD): Total: 15.5 (1.6); Conjoint FT: 15.5; Separated FT: 15.5 Age range in years: Total: 11.5 ‐ 17.8 (not given by group) Gender: 1 male : 39 female (not given by group) Subtype: No details Age of onset in years: Total: 14.5 (1.6) (range 10.6 ‐ 17.0); Conjoint FT: 14.4; Separated FT: 14.5 Duration of illness in months: Total: 12.9 (9.4) months (range 2 ‐ 36 months); Conjoint FT: 13.9; Separated FT: 12.0 Baseline weight in kgs: Total: 40.0 (6.4) kgs (range 28 ‐ 53 kg); Conjoint FT: 39.3 kg; Separated FT: 40.7 kg Baseline ABW: Total: 74.3 (9.8) % (range 50.0% ‐ 95%); Conjoint FT: 72.2%; Separated FT: 76.2% Baseline BMI: No details Baseline eating disorder scale score: EDI: 56.2 (33.9) (not given by group); EAT: 47.7 (25.7) (not given by group) Baseline purging (bulimic symptoms > weekly): Total: 25: Conjoint FT: 31.6; Separated FT: 19.0 Comorbidity: No details Details on living arrangements: Total: nuclear 70%; adoptive 5%; single 10%; reconstituted 15%: Conjoint FT: nuclear 63.3%; adoptive 5.3%; single 10.5%; reconstituted 21.1%: Separated FT: nuclear 76.2%; adoptive 4.8%; single 9.5%; reconstituted 9.5% Family education/employment/income: Total: I ‐ II 65%; III ‐ V 22.5%; VI ‐ VIII 12.5 %: Conjoint FT: I ‐ II 63.2%; III ‐ V 15.8%; VI ‐ VIII 21.0 %; Separated FT: I ‐ II 66.7%; III ‐ V 28.6%; VI ‐ VIII 5.8% Recruitment strategy: Consecutive referrals of adolescents to the eating disorders service at the Maudsely hospital Exclusion criteria: No details | |
| Interventions | Setting of care: Outpatient Training/qualification of care provider(s): No details Treatment manual: No Supervision of treatment: Yes Adherence to treatment: No Intervention group 1 Description: Conjoint family therapy Family‐based therapy with the whole family required to attend every session Length: 1 year Intervention group 2 Description: Separated family therapy Family‐based therapy but the parents are seen separately from the young person with AN. Therapy with the young person consists of supportive educational therapy Length: 1 year | |
| Outcomes | Eating psychopathology Morgan Russell Assessment Schedule (Morgan 1988) EDI (Garner 1983) EAT (Garner 1979) Behavioural indices Kilograms/% of AWB/BMI Good outcome/Intermediate outcome/poor outcome Analogous rating to score for the presence of bingeing, vomiting, laxative abuse, depression, obsessional symptoms, and psychosomatic tension General psychopathology Mood ‐ Short Mood and Feeling Questionnaire (Angold 1995) Obsessionality (Hodgson 1977) Global pathology and interpersonal functioning Self‐Esteem RSE Scale (RSE) (Rosenberg 1965) Family Functioning SCFI (Kinston 1984) Expressed emotions (ratings from video (Leff 1985)) FACES III (Olson 1979; Olson 1985) | |
| Notes | Included in conjoint family therapy vs separated family therapy comparison Family therapy in both cases categorised as family‐based therapy Funded by: Medical research Council, Greek Ministry of Health | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “randomly assigned”, “using a stratified design controlling for levels of critical comments using the Expressed Emotion index” ‐ stated in abstract Quote: “randomised controlled trial” pg. 728, no other statement Personal communication stated that stratified randomisation was undertaken, taking into account parental criticism with the random‐number sequence generated by computer |
| Allocation concealment (selection bias) | Low risk | Personal communication stated that sealed envelopes were opened after consent to the study was obtained |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: “assessments conducted by a research psychiatrist who was independent of the treatment team and interviewed patients and their family and administered self report questionnaires”. Unclear if 'independent' means blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk |
|
Espina 2000.
| Methods | RCT | |
| Participants | Country: Spain Diagnostic tool: DSM‐IV No. screened: No details No. randomised: Family therapy: 44; Group Therapy: 27 No. started trial: No details No. dropped out during intervention: Family therapy: 9; Group Therapy: 2 No. dropped out during follow‐up: No details No. analysed: No details NOTE: for this study most data are not given in totals by intervention group but by subgroup: Group 1: Anorexia Restricting (FT); Group 2: Anorexia Purging (FT); Group 3: Anorexia Purging (GT). There was also a bulimia nervosa subgroup but data for them are not provided. Mean age in years (SD): Family therapy: Anorexia Restricting 18.66 (3.99); Anorexia Purging 19.17 (4.09); Group Therapy: Anorexia Purging 20.30 (6.41) Age range: No detail Gender %: Family therapy: Anorexia Restricting Male 7.1%; Female 92.9%; Anorexia Purging Male 0%; Female 100%, Group therapy: Anorexia Purging Male 0%; Female 100% Subtype: In the family therapy 14 are of the restricting type, 12 are of the purging type; In the group therapy group 100% are of the purging type Age of onset in years: Family therapy: Anorexia Restricting 15.64 (2.9); Anorexia Purging 16.08 (2.64); Group therapy: Anorexia Purging 16.6 (3.17) Duration of illness in months: Family therapy: Anorexia Restricting 33.59 months (30.88); Anorexia Purging 34.92 months (20.08); Group therapy: Anorexia Purging 35.80 months (37.41) Baseline weight: No detail Baseline BMI (% of those less than 17.5):Family therapy: Anorexia Restricting 35.7%; Anorexia Purging 41.7%; Group therapy: Anorexia Purging 40% Baseline eating disorder scale score: No detail Baseline purging: No detail Comorbidity: No detail Details on living arrangements: No detail Family education/employment/income: No detail Recruitment strategy: No detail Exclusion criteria: No detail |
|
| Interventions | Setting of care: Outpatient Training/qualification of care provider(s): Unclear Treatment manual: Unclear Supervision of treatment: Unclear Adherence to treatment: Unclear Intervention group 1 Description: Systemic family therapy (Selvini 1978; Minuchin 1974; Minuchin 1978) Length: Unclear Intervention group 2 Description: Patient support group + group therapy Length: Unclear | |
| Outcomes | Eating psychopathology EDI (Garner 1983; Garner 1991) EAT (Garner 1979) Anorectic Behavior Observation Scale (Vandereycken 1992) Body Shape Questionnaire (Cooper 1987a; Cooper 1987b) Bulimic Investigatory Test Edinburg (Henderson 1987) Behavioural indices BMI Menstruation General Psychopathology BPRS‐E (Lukoff 1986) SCL‐90‐R (Derogatis 1992) Depression BDI (Beck 1961) Self Anxiety Scale (Zung 1971) Global pathology and interpersonal functioning Social Adjustment Scale (Weissman 1976) | |
| Notes | Foreign‐language article, partially translated only. Included in family therapy vs standard care/treatment as usual Family therapy categorised as Systemic family therapy Funded by: University of the Basque Country (Spain) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail: Stated ‘random allocation’ with no detail |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Outcome assessors blind to treatment allocation” |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No detail on dropouts. No ITT analysis. |
| Selective reporting (reporting bias) | Unclear risk | Authors report that they collected data on both dropouts and eating disorder psychopathology, but the data are not reported in a format that is useable for analysis |
| Other bias | Unclear risk |
|
Geist 2000.
| Methods | RCT | |
| Participants | Country: Canada
Diagnostic tool: DSM‐IV; but current weight < 90% IBW and self‐imposed food restriction
No. screened: 120
No. randomised: Total: 25; Family therapy: 12; Family Group Psychoeducation: 13
No. started trial: No detail
No. dropped out during intervention: No detail
No. dropped out during follow‐up: No detail
No. analysed (unclear if Observed Case or LOCF): Total: 25; Family therapy: 12; Family group psychoeducation: 13
Mean age in years (SD): Family therapy: 14.3 (1.5); Family group psychoeducation: 14.9 (1.7)
Age range: Total: 12 ‐ 17.3
Gender %: Total: 0% male: 100% female
Subtype: No detail
Age of onset: No detail
Duration of illness: No detail
Baseline weight in kgs (SD): Family therapy: 41.1 (7.0); Family group psychoeducation: 41.1 (6.3)
Baseline BMI: No detail
Baseline eating disorder scale score (EDI drive for thinness): Family therapy: 11.1 (5.8); Family group psychoeducation: 13.7 (6.2)
Baseline eating disorder scale score (EDI body dissatisfaction): Family therapy: 9.1 (6.6); Family group psychoeducation: 11.0 (5.0)
Baseline eating disorder scale score (EDI bulimia): Family therapy: 1.2 (1.3); Family group psychoeducation: 1.9 (1.6)
Baseline purging: No detail
Comorbidity: No detail
Details on living arrangements: No detail
Family education/employment/income: No detail
Recruitment strategy: “Assessed and admitted to the inpatient program” Exclusion criteria:
|
|
| Interventions | Setting of care: Initially inpatients at screening ‐ once medically stable and met their weight goals ‐ discharged to outpatient clinic for remainder of therapy
Training/qualification of care provider(s): Family therapy: 2 social workers, 1 psychiatrist ‐ with 4 to 10 years experience with family therapy and AN; Family Group Psychoeducation: 2 dieticians, occupational therapist and psychiatric nurse ‐ with 2 to 6 years experience working with adolescent with eating disorders
Treatment manual: No detail
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Family therapy
In the context of standard medical and psychosocial intervention, the main objective of family work was to facilitate the young person with AN to take an active role in the management of the disorder, support weight restoration and normalisation of eating behaviour through direct and open communication within the family. Attempts were made to distinguish the eating disorder symptoms from normal adolescent behaviour and expected parent‐adolescent conflict with efforts made to support the development of adolescent autonomy and maturation with an accommodating family
Length: 4 months Intervention group 2 Description: Family psychoeducation Education to support attitudinal and behaviour change for both the family and young person with AN Length: 4 months |
|
| Outcomes |
Eating psychopathology
EDI‐2 (Garner 1991)
DICA (Welner 1987)
Behavioural indices
BMI
Menstruation
General Psychopathology
Depression CDI (Kovacs 1992)
SCL‐90‐R (Derogatis 1992)
Family Functioning Family functioning (Skinner 1991) |
|
| Notes | Included in family therapy vs educational intervention Family therapy categorised as other Funded by: Physician Services Inc, grant # NIF94‐606 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: “not all parents completed the general or dyadic measures of the FAM‐II” ‐ results not analysed; no other statement as to why the data were missing. Unclear if ITT analysis undertaken |
| Selective reporting (reporting bias) | Low risk | Nothing noted |
| Other bias | Unclear risk | Small trial |
Godart 2012.
| Methods | RCT | |
| Participants | Country: France
Diagnostic tool: DSM‐ IV
No. screened: 116
No. randomised: Total: 60; TAU + FT: 30; TAU: 30
No. started trial: Total: 58; TAU + FT: 29; TAU: 29
No. dropped out during intervention: Total: Total: 5; TAU + FT: 3; TAU: 2
No. dropped out during follow‐up: Total: 1; TAU + FT: 0; TAU: 1
No. analysed (observed case): Total: 59; TAU + FT: 29; TAU: 30 Mean age in years (SD): Total; 16.6 (1.6); TAU + FT: 16.4 (1.7); TAU: 16.6 (1.7) Age range in years: Total: 16.6 (1.6) years; TAU + FT: 17.3 (1.3); TAU: 16.9 (3.1) Gender %: Female 100% Subtype purging %: Total: 13.3% (8/60); TAU + FT: 16.7% (5/3); TAU: 10% (3/30) Subtype restricting %: No detail Age of onset: Total 14.8 (1.6); TAU + FT: 14.7 (1.7); TAU 15.0 (1.5) Duration of illness: Total: 16.6 (6.8) months; TAU + FT: 17.1 (8.3) months; TAU: 16.1 (5.2) months Baseline weight: Total: 83.6 (5.2) ABW% (at inclusion), 77.8 (8.9) EBW%, 42.9 (7.3) kgs; TAU + FT:83.9 (5.6) ABW%, 75.7 (7.2) EBW%, 43.7 (5.9) kgs; TAU: 83.3 (5.0) ABW%, 80.1 (10.3) EBW%, 42.0 (8.8) kgs Baseline BMI: Total: 16.9 (1.1); TAU + FT: 17.0 (1.2); TAU: 16.9 (1.0) Baseline eating disorder scale score: Total: 60.7 (35.1) EDI; TAU + FT: 61.3 (36.2) EDI; TAU: 60.2 (34.6) EDI Baseline purging: Total: 13.3% (8/60); TAU + FT: 16.7% (5/3); TAU: 10% (3/30) Comorbidity: "The two groups were comparable in terms of comorbid mood and anxiety disorders (i.e., major depressive disorder, social phobia, panic disorder, agoraphobia, obsessive compulsive disorder, post traumatic stress disorder; details available on request from the authors)." Pg 4 Details on living arrangements: Total: 9 (15%) not intact family status Family education/employment/income: No detail Recruitment strategy: AN hospitalised inpatients Exclusion criteria:
|
|
| Interventions | Setting of care: Inpatient and outpatient
Training/qualification of care provider(s): The psychiatrist and psychologist involved in the study had > 4 years of experience in the outpatient care of AN adolescents
Treatment manual: Unclear for TAU, states manual not used for FT component
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Treatment as usual + family therapy Family therapy sessions targeting intra‐familial dynamics, but not eating disorder symptoms Length: 18 months, length and number of sessions unclear (Mean FT sessions attended 11.8, SD 5.7) Intervention group 2 Description: Treatment as usual Consisted in ambulatory care initiated before hospital discharge and was tailored according to the mental and physical state of the participant. It included individual consultations, regular interviews involving the parents, and, if required, individual psychotherapy with another therapist. At each appointment, the psychiatrist conducted clinical investigation of the participant’s mental state, eating habits, medical condition, and psychosocial environment. In addition, the psychiatrist provided support, co‐ordinated services (e.g. general practitioner, psychotherapist, dietician or nutritionist, social worker, and school), prescribed medication as necessary, and offered parental support and guidance regarding conflicts they had with their daughter. Parents were advised to be supportive but to leave decisions about food to the adolescent and to discuss the difficulties they observed not directly with their daughter during or after the meal, but at the time of the consultations with the psychiatrist and their daughter. In addition, nutritional/dietetic advice was provided to the participants who were not gaining weight or not gaining sufficient weight Length: 18 months, length and number of sessions unclear (Mean TAU sessions attended 27.2, SD 12.7) |
|
| Outcomes |
Eating psychopathology MRS Outcome measures EDI Behavioural indices BMI Amenorrhea Rehospitalisation (psychiatric or for AN) Global pathology and interpersonal functioning GOAS SAS: Social Adjustment Scale |
|
| Notes | Funded by: The study was funded by the Projet Hospitalier de Recherche Clinique (CRC‐ PHRC, 1997, AOM97133 AP‐HP French Ministry of Health); and promoted by Assistance Publique des Hôpitaux de Paris (AP‐HP). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation to 1 of the 2 parallel treatment groups (30 in each) was performed using the SPSS randomisation program (FC). The 2 groups were randomised by blocks of 30 |
| Allocation concealment (selection bias) | Low risk | The result was issued to participants in a sealed envelope at inclusion by the psychiatrist in charge of signing the consent form |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Some missing data, up to 18% of total sample (e.g. at 6‐month follow‐up), ITT analysis and LOCF analysis undertaken. |
| Selective reporting (reporting bias) | High risk | MINI reportedly administered at intake and end of treatment, but not reported at end of treatment. Data at 6 and 12 months not reported |
| Other bias | Unclear risk |
|
Hall 1987.
| Methods | RCT | |
| Participants | Country: United Kingdom Diagnostic tool: ‘primary anorexia nervosa’; criteria not stated No. screened: No detail No. randomised: Individual and family: 15; Dietetic advice: 15 No. started trial: Individual and family, Dietetic advice: no detail No. dropped out during intervention: Individual and family: 1; Dietetic advice: 4 No. dropped out during follow‐up: Individual and family: 0; Dietetic advice: 0 No. analysed (LOCF): Individual and family: 15; Dietetic advice: 15 Number analysed (OC): Individual and family: 15; Dietetic advice: 15 Mean age in years (SD): Individual and family: 19.55; Dietetic advice:19.57 Age range in years: Total: 13 ‐ 27; Individual and family: 14 ‐ 25; Dietetic advice: 13 ‐ 27 Gender %: All female Subtype: No detail Age of onset in years: Individual and family: 17.07 (range 12 ‐ 21); Dietetic advice: 17.53 (range 12 ‐ 25) Duration of illness: Total : 6 to 72 months; Individual and family: 29.7 months (10 had received previous treatment), Dietetic advice: 24.5 months (8 had received previous treatment) Baseline weight in kgs: Total : < 85% of MMPW with amenorrhoea; Individual and family: 41.00 (mean 25.35% below ABW); Dietetic advice: 39.54 (mean 28.16% below ABW) Baseline BMI: Individual and family: 15.7; Dietetic advice: 15.00 Baseline eating disorder scale score: Individual and family: mean desired body weight 42.7 kg; Dietetic advice: mean desired body weight 44.2 kg Baseline purging: No detail Comorbidity: No detail Details on living arrangements: No detail Family education/employment/income:Total : social classes I ‐ III Recruitment strategy: Consecutive referrals to 1 of the study authors; mostly referred by general practitioner Exclusion criteria: No detail | |
| Interventions | Setting of care: Outpatient Training/qualification of care provider(s): Unclear: “therapists was trained and experienced in these therapeutic approaches” p. 186, no other statement Treatment manual: No: “proportions of individual psychodynamic therapy and family therapy depended on clinical judgment” pg. 186 Supervision of treatment: No detail Adherence to treatment: No detail Intervention group 1 Description: Combined individual and family psychotherapy Focus on the role of AN in relationship of the participant with her family and others with efforts made to change those aspects of relationship that stifled participant's development and maintained AN, especially over‐protectedness, conflict avoidance enmeshment and distancing within the family. Broad goals to encourage participant development both within and separately from the family and to promote insight Length: 12 sessions Intervention group 2 Description: Dietary advice Length: 12 sessions | |
| Outcomes | Eating psychopathology CCEI (Crown 1979) Morgan Russell Assessment Schedule (Morgan 1988) Global score calculated from the mean of these Behavioural indices Scores for body weight and menstrual function calculated from CCEI | |
| Notes | Included in family therapy vs educational intervention Family therapy categorised as other Funded by: No detail | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “one year after the assessment interview, all the subjects were interviewed by an assessor who was blind to the treatment allocated” pg. 186 |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Numbers of dropouts described. No details on why participants did not complete treatment. ITT analysis undertaken |
| Selective reporting (reporting bias) | High risk | Authors report that they collected data on eating disorder psychopathology, but the data are not reported in a format that is useable for analysis. No reporting on eating behaviour outcomes i.e. restricting, purging behaviours No useable data |
| Other bias | High risk |
|
Herpertz‐Dahlmann 2014.
| Methods | Randomised non‐inferiority trial | |
| Participants | Country: Germany
Diagnostic tool: DSM‐ IV
No. screened: 660
No. randomised: Total: 176
No. started trial: Total: 172; IP: 85; DP: 87
No. dropped out during intervention: Total: 29; IP: 10; DP: 19
No, dropped out during follow‐up: Total: 11; IP: 10; DP: 1
No. analysed (observed case): Differing N for various outcomes Mean age in years (SD): IP: 15·2 (1·5); DP: 15·3 (1·5) Age range in years: No detail Gender %: Female 100% Subtype purging %: No detail Subtype restricting %: No detail Age of onset: No detail Duration of illness (weeks): IP: 53·7 (39·6); DP: 42·4 (33·1) Baseline weight: No detail Baseline BMI: IP: 15·1 (1·2); DP: 14·9 (1·5) Baseline eating disorder scale score (MRAOS): IP 5·0 (1·7); DP: 5·6 (1·7) Baseline eating disorder scale score (EDI‐II Global Score): IP: 272·5 (59·4); DP: 248·8 (58·2) Baseline purging: No detail Comorbidity (Any): IP: 33 (44%); DP: 28 (38%), Affective, Anxiety, Obsessive Compulsive and Attention Deficit Hyperactivity Disorders Details on living arrangements: No detail Family education/employment/income: No detail Recruitment strategy: Multi‐site: 6 centres in Germany Exclusion criteria:
|
|
| Interventions | Setting of care: Inpatient and outpatient
Training/qualification of care provider(s): No detail
Treatment manual: No detail
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Inpatient therapy
Admission to IP for medical observation or stabilisation during the first 3 weeks of the study. Multimodal multidisciplinary treatment programme based on weight restoration, nutritional counselling, CBT, and family therapy but undertaken in inpatient setting Length: Mean 14.6 weeks Intervention group 2 Description: Day patient therapy Admission to IP for medical observation or stabilisation during the first 3 weeks of the study. Multimodal multidisciplinary treatment programme based on weight restoration, nutritional counselling, CBT, and family therapy but undertaken in day‐patient setting Length: Mean 16.5 weeks |
|
| Outcomes |
Eating psychopathology Morgan Russell Outcome Scales (MRAOS) Eating Disorders Inventory (EDI‐II) Global Score Behavioural indices BMI Number of eating disorder readmissions Costs, loss to follow‐up General Psychopathology and Obsessionality Brief Symptom Inventory |
|
| Notes | The differences between the IP and DP are unclear. It is not clearly stated how the treatments differed beyond the initial 3 week IP admission. Descriptions for discharge criteria and interventions appear to be the same. The family therapy component is not described. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequence to randomly assign participants to continued IP or DP after 3 weeks of inpatient care |
| Allocation concealment (selection bias) | High risk | Patients and therapists could not be masked to treatment allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessors were initially masked but some participants inadvertently revealed their treatment allocation; masking was maintained for the primary outcome of BMI |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Differences in numbers at post‐intervention analysis and 12‐month follow‐up. Fewer participants included in post‐intervention analysis compared to follow‐up. Modified ITT analysis reported. There is an imbalance in the missing data across conditions (i.e. missing data from 10 participants in inpatient condition and only missing data from 1 in day patient condition). |
| Selective reporting (reporting bias) | Low risk | Outcomes appear to have been reported |
Herscovici 2017.
| Methods | RCT | |
| Participants | Country: Argentina
Diagnostic tool: Great Ormond Street operational definition of AN (Bryant‐Waugh 2000). The entire sample would have met current DSM V diagnostic criteria
No. screened: Total: 38
No. randomised: Total: 23
No. started trial: 23
No. dropped out during intervention: 2
No. dropped out during follow‐up: No detail
No. analysed (observed case): Total: 23; FT: 12; FTFM: 11 Mean age in years (SD): Total: 17.1 (2.3) Age range in years: Total: No detail Gender %: No detail Subtype purging %: Total: 35; FT: 25; FTFM 45 Subtype restricting %: No detail Age of onset: No detail Duration of illness: Total: 21.5 (14.3) months; FT: 21.1 (12.0) months; FTFM: 21.9 (11.9); Range: 8.5 ‐ 36 months Baseline weight: Most were severely underweight (21/23 had < 85% EBW), no further detail Baseline BMI: No detail Baseline eating disorder scale score: Total: 7.0 (3.0) EDI‐2 Global Score; FT: 5.2 (SD, 2.1) EDI‐2 GS; 9.1 (2.7) EDI‐2 GS Baseline eating disorder scale score: No detail Baseline purging: No detail Comorbidity: FT: 51.4 (6.5) GSI of SCL90‐R; 62.5 (11.1) GSI of SCL90‐R Details on living arrangements: All residing at home with 1 or both parents as per inclusion criteria. Total: Intact 13 (57%), Blended 1 ( 4%), Divorced 6 (26%), Single 3 (13%); FT: Intact 6 (50%), Blended 1 ( 8%), Divorced 5 (42%), Single 0 ( 0%); FTFM: Intact 7 (64%), Blended 0 ( 0%), Divorced 1 ( 9%), Single 3 (27%) Family education/employment/income: Total: Socioeconmic level: Lower 3 (13%), Middle 10 (44%), Upper Middle 3 (13%), Upper 7 (30%); FT: Lower 1 (8%), Middle 4 (33.%), Upper Middle 2 (17%), Upper 5 (42%); FTFM: Lower 2 (18%), Middle 6 (55%), Upper Middle 1 ( 9%), Upper 2 (18%) Recruitment strategy: Methods of recruitment of participants included: (i) agreements with eating disorder hospital services; (ii) informative presentations for parents at schools; and (iii) public service announcements in the media. 70 telephone inquiries were screened to determine eligibility. Following this, 38 adolescents and their families were scheduled for assessment at the Universidad del Salvador (supplementaries), although paper states they were from the clinician's private practice. Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatient
Training/qualification of care provider(s): Family therapist
Treatment manual: No detail
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Family‐based therapy
Maudsley Approach. Length: Mean 14 sessions (range 10 ‐ 19) Intervention group 2 Description: Family‐based therapy + family meal As above, with family meal included Length: Mean 18 sessions (range 14 ‐ 25) but 1 participant received more, 90 minute sessions, 6 months |
|
| Outcomes |
Eating psychopathology EDI‐2 MRGAS Behavioural indices Weight recovery Amenorrhea General Psychopathology and Obsessionality SCL‐90 |
|
| Notes | Funded by: no details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequence |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | < 10% missing data; but despite reports that data was missing, these participants appear to have been included in the analysis. Thus it is unclear if LOCF analysis was undertaken, but not stated |
| Selective reporting (reporting bias) | Low risk | All measures appear to be reported across paper and supplementary tables |
| Other bias | Unclear risk |
|
Le Grange 1992.
| Methods | RCT | |
| Participants | Country: United Kingdom
Diagnostic tool: DSM‐III‐R
No. screened: No detail
No. randomised: Total: 18
No. started trial: No detail
No. dropped out during intervention: No detail
No. dropped out during follow‐up: No detail
No. analysed: Total: 18, Mean age in years (SD):, Total: 15.33 (1.81)
Age range: Total: 12 ‐ 17 years
Gender %: Total: 2 male; 16 female
Subtype: No details
Age of onset: No details
Duration of illness: Total: 13.7 months; SD: 8.83 (not stated if treated or untreated)
Baseline weight: Total: ABW 77.9%, SD 7.62; Family therapy: ABW 75.9% SD 8.8; Family counselling: ABW 80.5 SD 5.3
Baseline BMI: No details
Baseline eating disorder scale score (EAT): Family therapy: 36.9 (27.6); Family counselling: 35.3 (22.8)
Baseline eating disorder scale score (MRS): Family therapy: 3.9 (1.7); Family counselling: 4.8 (1.5)
Baseline purging: No details
Comorbidity: States that those with co‐morbidity were excluded
Details on living arrangements: No details
Family education/employment/income: No details
Recruitment strategy: Referral to the Dept of Children and Adolescents at the Bethlem and Maudsley Hospital
Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatient Training/qualification of care provider(s): Yes: 2 Clinical psychologists, 1 psychiatrist, 1 social worker, all experienced in working with families and with treating AN, within this context Treatment manual: No detail Supervision of treatment: Yes: “regularly by consultant psychiatrist and family therapist" Adherence to treatment: No detail Intervention group 1 Description: Conjoint family therapy Family‐based therapy with the whole family required to attend every session Length: 6 months Intervention group 2 Description: Family counselling/ separated family therapy Family‐based therapy, but the parents are seen separately from the young person with AN. Therapy with the young person consists of supportive educational therapy Length: 6 months | |
| Outcomes | Eating psychopathology Morgan Russell Assessment Schedule (Morgan 1988) EAT (Garner 1979) Behavioural indices Weight, height, menstruation Good/intermediate/poor outcome on MR scales Global pathology and interpersonal functioning Self‐esteem RSE (Rosenberg 1965) Family Functioning SCFI (Kingston 1984; Kingston 1988) Expressed emotions (ratings from video, Vaughn 1976) FACES III (Olson 1979; Olson 1985) | |
| Notes | Included in conjoint family therapy vs separated family therapy comparison Family therapy in both cases categorised as family‐based therapy. Personal communication stated this is a small pilot study with no other data apart from what were published. Funded by: No details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Personal communication stated a random number sequence was used |
| Allocation concealment (selection bias) | Low risk | Personal communication stated sealed envelopes were used |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
|
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk |
|
Le Grange 2016.
| Methods | RCT | |
| Participants | Country: Australia
Diagnostic tool: DSM‐IV criteria for AN (excluding amenorrhoea). Given the anticipated publication of the DSM‐5 during the study, with its proposed deletion of the weight cut‐off for AN, inclusion criteria for weight was ≤90% median BMI for adolescents ≤75th percentile for height, and <95% median BMI for adolescents ≥75th percentile for height No. screened: 269 clinic assessment, 196 screened by interview No. randomised: Total: 107; FBT: 55; PFT: 52 No. started trial: 107 No. dropped out during intervention: Total: 17; FBT: 9; PFT: 7 + excluded from analysis: 1 No. dropped out during follow‐up: Total: 19; FBT 9 (with another 15 only partial assessments); PFT: 10 (with another 10 only partial assessments) No. analysed (observed case): Total: 106; FBT: 55; PFT: 51, ITT Mean age in years (SD): Total: 15.5 (1.5); FBT: 15.4 (1.3); PFT 15.7 (1.6) Age range in years: Total: 15.5 (1.5); FBT: 15.4 (1.3); PFT: 15.7 (1.6) Gender % female: Total: 87.7; FBT: 89.1; PFT: 86.3 Subtype purging %: No detail Subtype restricting %: No detail Age of onset: No detail Duration of illness: Mean months (SD) Total: 10.5 (8.8); FBT: 11.0 (9.4); PFT: 10.0 (8.1) Baseline weight: Total: No detail Baseline BMI Mean (SD): Total: 16.5 (1.3); FBT: 16.3 (1.2); PFT: 16.7 (1.4) Baseline eating disorder scale score: EDE Globabl Total: 2.15 (1.68); FBT: 2.20 (1.81); PFT: 2.09 (1.54) Baseline purging: Total: No detail Comorbidity Mood Disorder %: Total: ; FBT: 16.4; PFT: 29.4 Comorbidity Anxiety Disorder %: Total: 22.6; FBT: 21.8; PFT: 23.5 Comorbidity OCD% : Total: 5.7; FBT : 3.6; PFT: 7.8 Comorbidity Behavioural Disorder %: Total: 1.9; FBT: 3.6; PFT: 0.0 Comorbidity suicide or self‐harm risk %: Total: 10.4; FBT: 12.7; PFT: 7.8 Details on living arrangements ‐ "intact family" %: Total: 63.2; FBT: 61.8; PFT: 64.7 Family education/employment/income, University degree mother %: Total: 37.8; FBT: 43.1; PFT: 31.9 Family education/employment/income, University degree father %: Total: 38.2; FBT: 40.0; PFT: 36.1 Recruitment strategy: All patients who presented to the specialist clinic during the recruitment period (July 2010 to July 2014) were assessed for eligibility. Exclusion criteria:
Must also be: living with at least 1 parent available to undertake treatment; and English proficiency by adolescents and parents at the sixth‐grade level |
|
| Interventions | Setting of care: Outpatient
Training/qualification of care provider(s): "Therapist", no further details
Treatment manual: Yes
Supervision of treatment: Weekly supervision in both treatments
Adherence to treatment: All treatment sessions for which consent has been provided are audio recorded Randomly‐selected recordings are reviewed by author DLG throughout the trial. No further detail
Intervention group 1
Description: Family‐based therapy (FBT) Includes the entire family in treatment sessions, and a family meal Length: 18 sessions over 6 months. 10 minutes for participant weigh‐in with therapist + 50‐minute therapy session for family Intervention group 2 Description: Parent‐focused treatment (PFT) An adaptation of FBT, but parents are seen separately from client (other than first and last sessions) and there is no family meal Length: 18 sessions over 6 months. 15‐minute sessions with nurse for client, 50‐minute sessions with therapist for parents |
|
| Outcomes |
Eating psychopathology EDE global, restraint, eating concerns, weight concerns, shape concerns Behavioural indices Recovery ‐ defined as: 95% mBMI and a global EDE score within 1 SD of community norms % median BMI Days drive exercise General Psychopathology and Obsessionality Child Depression Inventory Global pathology and interpersonal functioning Rosenberg self‐esteem scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An off‐site biostatistician (RC) generated a randomisation schedule that was stratified by eating disorder severity (low versus high) |
| Allocation concealment (selection bias) | Low risk | The randomisation schedule is only accessible by designated staff members at the Royal Children’s Hospital who are independent of the Eating Disorders Programme team including the research team |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Independent and trained assessors, who were not involved in treatment delivery, administered all assessments. No details provided about whether or not they were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Missing data for continuous outcome measures at EOT and follow‐up were imputed using multiple imputation based on fully conditional Markov chain Monte Carlo modelling. The final analyses were based on the pooled results of 5 separate imputations. Treatment groups were then compared separately at EOT and at 6‐ and 12‐ month follow‐up using a general linear model for symmetric continuous outcomes, or a generalized linear model for non symmetric data. Covariates for all models included baseline observation, sex, age at baseline, and illness severity. Sensitivity analyses were conducted using maximum likelihood imputation and last observation carried forward, with results compared across the 3 methods" pg 687. |
| Selective reporting (reporting bias) | High risk | The following measures stated to have been administered, but not reported on, individually, only as results in moderator analyses: Children’s Yale–Brown Obsessive Compulsive Scale (CY‐BOCS),29 Yale–Brown–Cornell Eating Disorder Scale (YBC‐EDS), Mini International Neuropsychiatric Interview for Children and Adolescents (MINI‐Kid),31 Symptom Checklist‐90–Revised (SCL‐90‐R),32 Five Minute Speech Sample (FMSS), Therapy Suitability and Patient Expectancy (TSPE), Helping Relationship Questionnaire (HRQ), Parents Versus Anorexia (PVA),36 Positive and Negative Affect Scale–Expanded (PANAS‐X), Borderline Personality Questionnaire (BPQ), and the Family Environment Scale (FES) |
| Other bias | Unclear risk | Trial conducted by the developers FBT therapy treatment Funded by: Baker Foundation |
Li 2006.
| Methods | RCT | |
| Participants | Country: China
Diagnostic tool: Chinese Classification of Mental Disorders (CCMD‐3) criteria for AN
No. screened: No detail
No. randomised: No detail
No. started trial: No detail
No. dropped out during intervention: No detail
No. dropped out during follow‐up: No detail
No. analysed (observed case): Total: 42; FT + DT: 21; DT: 21 Mean age in years (SD): Total: 41.3 (18.5); FT + DT: 40.1 (20.3); DT: 38.7 (20.5) Age range in years: Total: No detail Gender %: No detail Subtype purging %: 42 Subtype restricting %: No detail Age of onset: No detail Duration of illness: FT + DT: 5.6 (2.4); DT: 5.4 (3.0) Baseline weight: FT + DT: 34.8 (2.8); DT: 34.8 (2.9) Baseline BMI: No detail Baseline eating disorder scale score: No detail Baseline eating disorder scale score: No detail Baseline purging: No detail Comorbidity, HAMD: FT + DT: 29.2 (4.7); DT: 29.0 (4.9) Details on living arrangements: No detail Family education/employment/income: No detail Recruitment strategy: Recruited from inpatients, no further information Exclusion criteria:
|
|
| Interventions | Setting of care: Inpatient and 1‐year follow‐up as outpatient after discharge Training/qualification of care provider(s): Professionally‐trained psychiatrists Treatment manual: Unclear. "The treatment was structured", no further information Supervision of treatment: No detail Adherence to treatment: This was assessed, but results not reported Intervention group 1 Description: Family therapy + drug therapy: Citalopram (20 mg ‐ 60 mg/day) Length: 60 min, 6 sessions on average; 12 weeks Intervention group 2 Description: Drug therapy: Citalopram (20 mg ‐ 60 mg/day) Length: 12 weeks | |
| Outcomes |
Behavioural indices
Weight Relapse General Psychopathology and Obsessionality HAMD (Hamilton 1960) |
|
| Notes | Foreign‐language article. Screened and data extracted by researcher outside of the main review team. Data extracted by only 1 researcher | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were randomised according to the order of their hospital admission, no further information about randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No detail |
| Selective reporting (reporting bias) | High risk | The paper describes a method, LOWE, to judge the efficacy of the treatment but the results are not reported. Interview records and other psychiatric evaluation results not reported at baseline. Additional medicine used for sleeping disorders was not reported. No useable data |
| Other bias | Low risk | |
Lock 2005.
| Methods | RCT | |
| Participants | Country: USA
Diagnostic tool: DSM‐IV, with some partially weight‐restored participants included, and requirement of only 1 instead of 3 missed menstrual periods
No. screened: 241
No. randomised: 86, Short‐term FT: 44; Long‐term FT: 42
No. started trial: No details
No. dropped out during intervention: Total: 9; Short‐term FT: 2; Long‐term FT: 7
No. dropped out during follow‐up: Total: 8; Short‐term FT: 5; Long‐term FT: 3
No. analysed: Total: 86 (at 6 and 12 months) (LOCF); Short‐term FT: 44; Long‐term FT: 42
Short‐term FT: OC BMI 37; EDE20 at 12 months
Long‐term FT: OC BMI 34; EDE15 at 12 months
Mean age (SD): Short‐term FT: 15.2 (1.6) years; Long‐term FT: 15.2 (1.7) years
Age range in years: 12 ‐ 18 (not given by group)
Gender: Total: 9 male: 77 female; Short‐term FT: 5 (11%):39 (89%); Long‐term FT: 4 (9%):38 (91%)
Subtype: Short‐term FT: purging (7) 16%; restricting (37) 84%; Long‐term FT: purging (9) 21%; restricting (33) 79%
Age of onset: No details
Duration of illness: Total : 30% had been previously hospitalised but not stated by group whether treated or untreated; Short‐term FT: 11.3 (10.4) months; Long‐term FT: 12.0 (9.9) months
Baseline weight (SD): Short‐term FT: 44.6 (5.5) kg; Long‐term FT: 46.7 (7.2) kg
Baseline BMI: Total: 17.1 (1.4); Short‐term FT: 17.0 (1.3); Long‐term FT: 17.3 (1.5)
Baseline eating disorder scale score (EDE eating concern): Short‐term FT: 1.35 (1.13); Long‐term FT: 1.04 (1.33)
Baseline eating disorder scale score (EDE restraint): Short‐term FT: 2.76 (1.97); Long‐term FT: 2.64 (1.96)
Baseline eating disorder scale score (EDE shape concerns): Short‐term FT: 2.61 (1.73); Long‐term FT: 2.41 (1.67)
Baseline eating disorder scale score (EDE weight concern): Short‐term FT: 2.32 (1.51); Long‐term FT: 1.96 (1.52)
Baseline purging: No details
Comorbidity: Total: 36% (n = 31) had any psychiatric illness; 24% (n = 21) had MDD or DYS; 14% (n = 12) had anxiety disorder; 5% (n = 4) other
Details on living arrangement: Short‐term FT: living in an ‘intact family’ 82% (n = 36); Long‐term FT: living in an ‘intact family’ 74% (n = 31)
Family education/employment/income: Short‐term FT: 9% < 50 K; 33% 50 ‐ 100 K; 57% > 100 K; Long‐term FT: 10% < 50 K; 43% 50 ‐100 K; 48%, > 100 K
Recruitment strategy: Recruited by referral from paediatricians and therapists to a specialty evaluation clinic for child and adolescent eating disorders
Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatient, with some hospitalised before treatment
Training/qualification of care provider(s): Yes: 3 Masters Level psychologists, 1 child/adolescent psychiatrist
Treatment manual: Yes: “therapists were all trained in the manual based version of family based treatment"
Supervision of treatment: Yes: Weekly supervision
Adherence to treatment: Unclear: “a manual based form of family based treatment was used” pg. 667(Lock 2006)
Intervention group 1
Description: Short‐term family therapy
Family‐based therapy but consisting of only Phase 1 and 2 (refeeding and problem‐solving for issues that interfere with refeeding)
Length; 6 months
Intervention group 2
Description: Family‐based therapy Labelled 'Long Term Family Therapy' in report. Consists of Phases 1, 2 and 3 Length: 12 months |
|
| Outcomes | Eating psychopathology EDE (Cooper 1987a; Cooper 1987b) Behavioural indices BMI Menstruation General Psychopathology and Obsessionality Schedule for Affective Disorders and Schizophrenia for School‐Aged Children (Kaufman 1997) YBC‐ED scale (Sunday 1995) Global pathology and interpersonal functioning Child Behaviour Checklist; Youth Self Report Checklist (Achenbach 1991) Family Functioning Family Environment Scale | |
| Notes | Included in short family therapy vs long family therapy comparison Family therapy in both cases categorised as family‐based therapy Funded by: NIH Career Development Award | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “randomised subjects were stratified...by duration of illness”; “ within each stratum using the Efron biased coin procedures by a research assistant not involved in assessments” pg. 634 |
| Allocation concealment (selection bias) | Unclear risk | Quote: “randomised by a research assistant not involved in assessment to either a short or long term treatment” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “assessments were conducted by trained assessors who were not involved with the treatment of patients‐not told which group that the patient was randomised to for treatment” pg. 634 |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | High risk |
|
| Other bias | Low risk | No other problems noted |
Lock 2010.
| Methods | RCT | |
| Participants | Country: USA
Diagnostic tool: DSM‐IV criteria for AN excluding the amenorrhoea criterion
No. screened: telephone screening N = 331, invited for an assessment interview N = 175 (53%)
No. randomised: Total: 121; FBT: 61; AFT: 60
No. started trial: FBT: 57; AFT: 59
No. dropped out during intervention: Total: 12; FBT: 9; AFT: 3
No. dropped out during follow‐up: 6 months; FBT: 18; AFT: 14; 12 months: FBT:17; AFT: 11
No. analysed (observed case): FBT end of treatment: 50; FBT 6 months: 44; FBT 12 months: 45; AFT end of treatment: 49; 6 months: 47; 12 months: 49 Mean age in years (SD): Total: 14.4 (1.6) years; FBT: 14.1 (1.7); AFT: 14.7(1.5) Age range in years: Not stated, but needed to be between 12 and 18 years (inclusion criteria) Gender %: No detail Subtype purging %: 17.4% (n = 21) "Binge‐purge" subtype Subtype restricting %: No detail Age of onset: No detail Duration of illness: Total: 11.3 (8.6) months; FBT: 12.3 (8.5) months; AFT: 10.3 (8.7) months Baseline weight Mean IBW%: 82 Baseline BMI: 16.1 (1.1) Baseline eating disorder scale score EDE: Total: 1.77 (1.45); FBT: 1.5 (1.3): AFT: 2.1 (1.3) Baseline purging: No detail Comorbidity: Approximately ¼ of participants (24.5%, n = 29) met criteria for a current comorbid psychiatric disorder, as assessed by the Schedule for Affective Disorders and Schizophrenia for School‐Aged Children. FBT: 20% with psych comorbidity; AFT: 32% with psychiatric co‐morbidity Details on living arrangements: 79% were from intact families. All participants lived at home or with legal guardian. Family education/employment/income, parental education mean years (SD): FBT: 17.0 (3.1); AFT: 17.1 (2.6) Recruitment strategy: Participants were recruited by advertising to clinicians, organisations, and clinics treating eating disorders. After telephone screening (N = 331) to determine eligibility, 175 (53%) were invited for an assessment interview Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatients, but hospitalisation allowed if required on medical grounds
Training/qualification of care provider(s): PhD psychologists and 2 child psychiatrists
Treatment manual: "use of manualised treatments", no further information
Supervision of treatment: Weekly
Adherence to treatment: Unclear. Therapists treated 3 pilot cases satisfactorily with each treatment prior to treating randomised cases. No details about monitoring treatment adherence during trial
Intervention group 1
Description: Family‐based therapy Length: 60 mins, 24 sessions (24 hours), 12 months Intervention group 2 Description: Adolescent‐focused therapy (AFT) Participants learn to identify and define their emotions and later to tolerate affective states rather than numbing themselves with starvation. Originally described by Robin 1999 as ego‐oriented individual therapy Length: 32 x 45‐minute sessions (24 hours), 12 months |
|
| Outcomes |
Eating psychopathology
EDE, version 12.0
Behavioural indices
Remission: those who achieved 95% IBW, adjusted for age, sex, and height, and total EDE score within 1 SD of normal
Relapse BMI, BMI % for age and sex and percentage EBW (% EBM), IBW Family Functioning McMaster FAD |
|
| Notes | Funded by: Stanford University and National Institute of Mental Health (NIMH) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed separately for each site by a biostatistician in the Data and Co‐ordinating Center under independent management from either intervention site. The Efron biased coin design was used to balance treatment within sites. Participants were stratified within sites based on current use of psychiatric medication |
| Allocation concealment (selection bias) | Low risk | See above: Randomisation was performed separately for each site by a biostatistician in the Data and Co‐ordinating Center under independent management from either intervention site. This can be considered sufficient for a low risk of bias for randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "independent assessors", no further detail |
| Incomplete outcome data (attrition bias) All outcomes | High risk | > 29.5% data missing for some outcome/follow‐up measures, paper states "Intent‐to‐treat mixed‐effects modelling used all available data", but analysis appears to have been observed case in some instances |
| Selective reporting (reporting bias) | Low risk | Results from all measures appear to have been reported |
| Other bias | Unclear risk | Researchers involved in the trial also developed the intervention. |
Lock 2015.
| Methods | RCT (unbalanced design) | |
| Participants | Country: Not reported (author affiliation listed as USA)
Diagnostic tool: DSM‐IV TR criteria for AN,except for the amenorrhoea requirement
No. screened: 70
No. randomised: Total: 45; FBT: 10; FBT/IPC: 35
No. started trial: No detail
No. dropped out during intervention: Total: 9; FBT: 2; FBT/IPC: 7
No. dropped out during follow‐up: No detail
No. analysed (observed case): Unclear, no detail Mean age in years (SD): FBT: 14.3 (1.5); FBT/IPC: 14.6 (1.4) Age range in years: No detail Gender % female: FBT: 90; FBT/IPC: 92.07 Subtype purging %: No detail Subtype restricting %: No detail Age of onset: No detail Duration of illness, months: Total:12.6 (13.7) Baseline weight: No detail Baseline BMI : FBT: 16.1 (1.1); FBT/IPC: 16.2 (0.9) Baseline eating disorder scale score Global EDE: FBT: 1.8 (1.6); FBT/IPC: 1.9 (1.5) Baseline purging: No detail Comorbidity (depression, anxiety, obsessive compulsive, panic, phobia, adjustment disorders): FBT 30%; FBT/ICP: 52.4% Details on living arrangements, intact family: FBT: 80%; FBT/IPC: 85.3% Family education/employment/income: No detail Recruitment strategy: No detail Exclusion criteria:
|
|
| Interventions | Setting of care: Outpatient
Training/qualification of care provider(s): No detail
Treatment manual: Yes for FBT, unclear for FBT/IPC
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Family‐based therapy (FBT) Includes a family meal Length: Sessions: Mean (SD) 12.9 (3.6); 6 months (target: 15 sessions over 6 months) Intervention group 2 Description: Family‐based therapy + intensive family coaching (FBT + IPC) In the adaptive treatment arm, FBT/IPC+ provides 3 sessions of IPC added to standard FBT focused on meal time coaching for families whose child had not gained 2.3 kg (4.8 lbs) by session 4. The first of these sessions (new session 5) is a family session designed to present the failure in sufficient weight gain by this point as a crisis and strives to reinvigorate the family to make definitive behavioural changes to support weight restoration. Following this session (new session 6), a session with the parents only is held to identify what impediments the parents perceive might be interfering with successful re‐feeding. Finally, a second family meal (new session 7) is held which includes direct coaching by the therapist to help address the specific challenges identified during the meeting with the parents alone. Following these 3 sessions, the treatment resumes the regular course of standard FBT. Participants in this arm who did gain 2.3 kg by session 4 did not receive the IPC sessions. Length: Sessions: Mean (SD) 13.9 (4.3); 6 months (target: 18 sessions over 6 months) |
|
| Outcomes |
Eating psychopathology EDE Global Score Behavioural indices Recovery (% EBW > 95) Weight BMI General Psychopathology and Obsessionality CYBOCS YBCEDS Total BDI (RSE HRQ Global pathology and interpersonal functioning TSPE |
|
| Notes | Funded by: NIMH to Dr. Lock (PI) R34‐MH09349303, Dr. Le Grange (PI) R34‐MH093768, and Dr. Agras, (co‐PI), R34‐MH09349303 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome data reported for all randomised participants (unclear if ITT or observed case outcome data used) |
| Selective reporting (reporting bias) | High risk | Parents Versus Anorexia Nervosa Scale, PvAn, not reported for all groups at end of treatment, Schedule for Affective Disorders and Schizophrenia for School‐Aged Children (6 ‐ 18 years) ‐ Present and Lifetime Version (K‐SADS‐PL) not reported at end of treatment. Family income data discussed but not reported |
| Other bias | Unclear risk | Unbalanced randomised design N = 10 in FBT; N = 35 in FBT/IPC (but N = 23 in FBT/IPC had only FBT, e.g. FBT/IPC‐; N = 12 in FBT/IPC had FBT and IPC, e.g. FBT/IPC+) |
Madden 2015.
| Methods | RCT | |
| Participants | Country: Australia
Diagnostic tool: DSM‐IV diagnosis of AN Total: ; MS + FBT: ; WR + FBT: No. screened: 266 No. randomised: Total: 82; MS + FBT: 41; WR + FBT: 41 No. started trial: MS + FBT: 40; WR + FBT: 38 No. dropped out during intervention: Total: 9; MS + FBT: 4; WR + FBT:5 No. dropped out during follow‐up: Total: 5; MS + FBT: 0; WR + FBT:5 No. analysed (observed case): Variable by outcome measure and follow‐up time Mean age in years (SD): Total: 14.89 (1.46); MS + FBT: 14.89 (1.36); WR + FBT: 14.88 (1.56) Age range in years: No detail, but inclusion criteria 12 to 18 years Gender % female: Total: 95.1; MS + FBT: 95.1; WR + FBT:95.1 Subtype purging %: Total: 30.51; MS + FBT: 29.27; WR + FBT: 31.73 Subtype restricting %: Total: 69.50; MS + FBT: 70.73; WR + FBT: 68.32 Age of onset: No detail Duration of illness: Total: 7.62 (6.16) months; MS + FBT: 7.39 (5.42) months; WR + FBT: 7.85 (6.89) months Baseline weight: Total: 78.26 (6.35) %EBW; MS + FBT: 77.28 (6.67) % EBW; WR + FBT: 79.25 (5.95) % EBW Baseline BMI: No detail Baseline eating disorder scale score, EDE total: Total: 3.07 (1.12); MS + FBT: 2.95 (1.14); WR + FBT: 3.19 (1.11) Baseline purging: See purging subtype above Comorbidity: Psychological feature: MS + FBT Mean (SD), WR + FBT mean (SD), Total Mean (SD) Depression features: 13 (31.7), 13 (31.7), 26 (31.7) Self‐harm/suicidality: 14 (34.2), 15 (36.6), 29 (35.8) Anxiety features: (34.2), 18 (43.9), 32 (39.0) OCD: 6 (14.6), 9 (22.0), 15 (18.3) PTSD/trauma/grief: 8 (19.5), 6 (14.6), 14 (17.1) Developmental/intellectual concerns: 2 (4.9), 5 (12.2), 7 (8.5) RCADS: Depression: 58.12 (15.51), 56.80 (14.86), 57.46 (15.11) RCADS: Anxiety: 49.15 (12.47), 52.78 (14.28), 50.96 (13.45) ChOCI‐R: Frequency of obsessions: 16.56 (3.75), 18.02 (6.26), 17.29 (5.18) Details on living arrangements, single parent %: Total: 26.8; MS + FBT: 29.3; WR + FBT: 24.4 Family education/employment/income: No detail Recruitment strategy: 266 consecutive eating disorder admissions to 2 specialist paediatric medical units Exclusion criteria:
|
|
| Interventions | Setting of care: Inpatient and outpatient
Training/qualification of care provider(s): 3 psychologists and a social worker trained in the FBT model
Treatment manual: FBT component of both treatments manualised
Supervision of treatment: Weekly individual and group supervision was provided by 2 experienced FBT therapists (AW and PR) with over 5 years of experience in FBT
Adherence to treatment: Where consent was provided (89% of families), treatment sessions were recorded on digital video and a random sample of 5% of these sessions were assessed for treatment fidelity by 1 of the authors of the FBT manual (DLG). No information provided about the level of adherence to treatment
Intervention group 1
Description: Medical stablisation + family‐based therapy (MS + FBT) MS: All participants were re‐fed using a standardised protocol starting with 24 – 72 hours of continuous nasogastric feeds (ceased with daytime medical stability) followed by a combination of nocturnal nasogastric feeds and supported meals aiming for a total caloric intake of between 2400 and 3000 kcal/day. The amount and duration of nasogastric feeding was determined by markers of medical instability for a minimum of 14 days. Total caloric intake was based on a rate of weight gain of 1 kg/week (Kohn 2011). Participants in the MS arm were subsequently discharged to outpatient FBT if they had no markers of medical instability for 72 hours after nasogastric feeds were ceased Length: Mean sessions (SD) 24.25 (8.51), 24.25 (hours), maximum of 12 months Intervention group 2 Description: Weight restoration + family‐based therapy (WR + FBT) WR: All participants were re‐fed using a standardised protocol starting with 24 – 72 hours of continuous nasogastric feeds (ceased with daytime medical stability) followed by a combination of nocturnal nasogastric feeds and supported meals aiming for a total caloric intake of between 2400 and 3000 kcal/day. The amount and duration of nasogastric feeding was determined by markers of medical instability for a minimum of 14 days. Total caloric intake was based on a rate of weight gain of 1 kg/week (Kohn 2011). Participants in the WR arm continued in hospital on supported meals without nasogastric feeding once they had no markers of medical instability for 72 hours, until they reached 90% EBW before discharge to outpatient FBT Length: Mean sessions (SD) 31.30 (12.60), 31.30 hours, maximum of 12 months |
|
| Outcomes |
Eating psychopathology EDE Global score Behavioural indices Number of days of hospitalisation, following initial admission, used by the12‐month follow‐up Total number of hospital days used by the 12‐month follow‐up and the percentage of participants at full remission as defined by an EBW > 95% and an EDE global score within 1 SD of expected norms. Partial remission was also examined as defined by weight > 85% of EBW % EBW |
|
| Notes | Funded by: National Health and Medical Research Council (NHMRC) of Australia (Grant ID 457235). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised in clusters of 6 using a block size of 2. Each new cluster was randomised through a blind random binary list created by an external statistician |
| Allocation concealment (selection bias) | High risk | Although the use of clusters unblinded recruitment staff to the group status of participants, this design was chosen to prevent potential problems of dropout if participants from different groups were treated alongside one another in hospital and became dissatisfied with their allocation. Participants and families were blind to treatment assignment prior to randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A clinical psychologist blind to treatment assignment conducted all baseline interviews and collected questionnaires at assessment time points |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Some missing outcome data and appear to have used observed case in the analysis |
| Selective reporting (reporting bias) | High risk | A number of measures not reported at EOT, e.g. RCADS, ChOCI‐R, RSES |
| Other bias | Unclear risk |
|
Onnis 2012.
| Methods | RCT | |
| Participants | Country: Italy
Diagnostic tool: DSM‐IV‐TR
No. screened: No detail
No. randomised: Total: 28 (16 BN, 12 AN); SFT:14 (AN + BN; MNT:14 (AN + BN)
No. started trial: Done
No dropped out during intervention: Done
No dropped out during follow‐up: Done
No. analysed (observed case): Done Mean age in years (SD): SFT: 18; MNT: 19.3 Age range in years: Total: Done Gender %: Female 100% Subtype purging %: No detail Subtype restricting %: No detail Age of onset: Done Duration of illness: SFT: 1.8 years; MNT: 2.1 years Baseline weight: SFT: 39.7; MNT: 36.4 Baseline BMI: SFT: 14.5; MNT: 14.2 Baseline eating disorder scale score: EDI ‐ No detail Baseline purging: No detail Comorbidity: Done Details on living arrangements: Done Family education/employment/income: SFT: 1 upper‐middle, 3 middle, 2 lower‐middle SES; MNT: 1 upper‐middle, 3 middle, 2 lower‐middle Recruitment strategy: Recrutied from non‐hospitalised patients connected to the Service for Eating Disorders of the Department of Neuropsychiatic Sciences for Child Development Exclusion criteria: Unclear |
|
| Interventions | Setting of care: Outpatient
Training/qualification of care provider(s): No detail
Treatment manual: No detail
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Minuchin's structural family therapy
Length: 20 ‐ 25 sessions (over 12 months; 1 session every 2 weeks)
Intervention group 2
Description: Treatment as usual Comprised Medical Nutritional Therapy and "possibly supported by psychiatric counselling" (pg. 40) Length: No detail |
|
| Outcomes |
Eating psychopathology
EDI EAT ‐ Data not reported Behavioural indices BMI Family Functioning Unclear |
|
| Notes | Mixed AN and BN sample. Based on the following quote "subdivided, with a randomisation distribution, into two homogeneous, experimental and control groups, of 14 patients each" (pg 40), we made the assumption that the 4:3 distribution (16 BN:12 AN) at inclusion was replicated in the experimental and control conditions (8 BN:6 AN per condition) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... the patients were randomly assigned to the two experimental and control groups." No further detail. |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Some separated AN and BN data reported, and some conjoint. SDs not reported |
| Selective reporting (reporting bias) | High risk | Not all measures have been reported (e.g. EAT). Unclear presentation of data. No useable data. |
Rausch Herscovici 2006.
| Methods | RCT | |
| Participants | Country: Argentina Diagnostic tool: Diagnostic criteria of “Great Ormond St” pg. 10 No. screened: No detail No. randomised: No detail No. started trial: No detail No. dropped out during intervention: No detail No. dropped out during follow‐up: No detail No. analysed: No detail Mean age in years (SD): No detail Total: 17.49 (2.08): Family therapy: 17.35 (2.79); Family therapy plus meal: (17.63 (1.30) Age range in years: Intake criteria were 12 ‐ 20, no other detail Gender %: Total: 8.3% (1) male; 97.79% (11) female; No detail by group Subtype: Total: 1 out of total were purging subtype; 8 out of total were restricting. No detail by group Age of onset: Total : 15.33 (2.42); Family therapy: 15.16 (3.18); Family therapy plus meal: 15.5 (1.64) Duration of illness (months): Total : 20.6 (12.73); Family therapy: 22.33 (12.79); Family therapy plus meal: 19.00 (13.65) Baseline weight in kgs (SD): Total : 43.18 (8.56); Family therapy: 41.58 (9.51); Family therapy plus meal: 44.77 (8.05) Baseline BMI:Total: 16.23 (1.92); Family therapy: 16.23 (2.57); Family therapy plus meal: 16.22 (1.23) Baseline eating disorder scale score: No detail Baseline purging: No detail Comorbidity: No detail Details on living arrangements: No detail Family education/employment/income: No detail Recruitment strategy:Subjects admitted to a clinic and subsequently discharged Exclusion criteria: No detail | |
| Interventions | Setting of care: Outpatient
Training/qualification of care provider(s): No detail
Treatment manual: No detail
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Family‐based therapy
Length: No details
Intervention group 2
Description: Family‐based therapy + meal Labelled 'Family Meal Intervention' in report Length: No details |
|
| Outcomes |
Eating psychopathology
MRS (Morgan 1988);
EAT (Garner 1979)
EDI‐II (Garner 1983)
Behavioural indices
Weight BMI General Psychopathology and Obsessionality SCL‐90‐R, BDI‐II Family Functioning ESF (Family Health Scale) |
|
| Notes | Foreign‐language article, partially translated only Included in family therapy vs family therapy plus meal comparison Family therapy in both cases categorised as family‐based therapy Funded by: No detail | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Outcome assessors blind to allocation" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk |
|
| Selective reporting (reporting bias) | Unclear risk |
|
| Other bias | Unclear risk | Data extracted by Spanish‐speaking colleague who was not part of the main review team |
Rhodes 2008.
| Methods | RCT | |
| Participants | Country: United Kingdom
Diagnostic tool: DSM‐IV TR diagnosis of AN
No. screened: No detail
No. randomised: Total: 20
No. started trial:
No. dropped out during intervention: Total: "13.3% of data was missing due to dropout from treatment"
No. dropped out during follow‐up: No detail
No. analysed (observed case): No detail Mean age in years (SD): Total: 14; FBT: 14.3; FBT + PPC 13.7 Age range in years: Total: 12.2 ‐ 16.1; FBT: 13.1 ‐ 16.1; FBT + PPC: 12.2 ‐ 15.9 Gender %: Female 100% Subtype purging %: No detail Subtype restricting %: No detail Age of onset: Duration of illness: Total: < 6 months = 9; 6 ‐ 12 months = 10; > 12 months = 1; FBT: < 6 months = 5; 6 ‐ 12 months = 4; > 12 months = 1; FBT + PPC: < 6 months = 4; 6 ‐ 12 months = 6; > 12 months = 0 Baseline weight: Total: %IBW 81.21; FBT: %IBW 83.85; FBT + PPC: %IBW 81.21 Baseline BMI: No detail Baseline eating disorder scale score: No detail Baseline eating disorder scale score: No detail Baseline purging: No detail Comorbidity: Total: Depression = 3; OCD = 5; FBT: Depression = 2; OCD = 3; FBT + PPC: Depression = 1; OCD = 2 Details on living arrangements: Total: Intact family: 12; lived with sole parent (and no contact with other biological parent): 2 ; 2 lived with 1 custodial parent and had fortnightly contact with other parent; FBT: Intact: 8; separated (both parents): 0; separated (1 parent): 2; FBT + PPC: Intact: 4; separated (both): 2; separated (1): 4 Family education/employment/income: No detail Recruitment strategy: Patients admitted to hospital via casualty, presenting with protein calorie malnutrition and associated medical compromise. Exclusion criteria: No detail |
|
| Interventions | Setting of care: Outpatient (all participants had previously been admitted to hospital via casualty)
Training/qualification of care provider(s): All therapists conducting these interviews had extensive experience, both in the Maudsley model (mean = 33 months) and generic family therapy (mean = 49 months). Specific training was also provided for the consultations (training was 3 hours, followed a structured interview protocol and included role plays)
Treatment manual: Yes
Supervision of treatment: No detail
Adherence to treatment: No detail
Intervention group 1
Description: Family‐based therapy (FBT)
Maudsley approach. Length: 60 mins , 20 sessions. 20 hours. Duration (e.g. months, not reported) Intervention group 2 Description: FBT + parent‐to‐parent consultation (FBT + PPC) The technique of "parent to parent consultation" is derived from narrative therapy and involves a joint interview with new parents and parents who have completed treatment. New parents listen as the therapist interviews graduated parents, with the aim of circulating liberative stories. PPC is a practice that has the capacity to build solidarity between parents rather than explore and resolve any unique family dysfunction Length: 60 mins, 20 FBT session + 60 mins PPC (+ 10 minutes for parents to talk at the end without therapist present). 21 hours. Duration (e.g. months, not reported) |
|
| Outcomes | Eating psychopathology Morgan–Russell categories (Morgan 1975) Behavioural indices % IBW General Psychopathology and Obsessionality Patient distress was measured using the DASS Family Functioning Parental efficacy was measured using the Parent versus Anorexia Scale (PVA) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A list of random numbers was generated using SPSS random‐number generation process |
| Allocation concealment (selection bias) | Low risk | Therapists were given a sealed envelope containing the group allocations at week 1 of treatment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 types of missing data: 1) participants engaged in treatment but temporarily unable or unwilling to complete valid measures: 3.6% (out of 501 observations 2) participants who dropped out of treatment, make an overt decision to stop responding to measures or complete treatment in less than 20 sessions. 38% missing for this reason; 13.3 % due to dropout from treatment, 11.3 % due to completion of treatment and 13.4% due to decision to stop responding to measures. 1) first type of missing data: LOCF 2) second type: analysis was restricted to 6 sessions after the consultation, resulting in a decrease in percentage of missing data in the poor outcome category, from 48% to 9.5%. This was seen as appropriate, given the analysis aimed to isolate any immediate effects of parent‐to‐parent consultations between sessions 3 and 5. Second, the remaining missing data were replaced by calculating the average score on all measures for each session |
| Selective reporting (reporting bias) | High risk | Parental efficacy measured using the PVA and depression/anxiety measured using the DASS were administered weekly for all parents, but not reported |
| Other bias | Unclear risk | Small trial |
Robin 1999.
| Methods | RCT | |
| Participants | Country: USA Diagnostic tool:DSM‐IIIR No. screened: “approximately 120 telephone enquiries and scheduled 60 for intake interviews” No. randomised: “41 agreed to participate and 4 dropped out, leaving 37 participants”. Does not say when participants dropped out. BFST: 19, EOIT: 18 No. started trial: No detail No. dropped out during intervention: “41 agreed to participate and 4 dropped out, leaving 37 participants”. Does not say when pp dropped out. 7 dropped out ‐ different numbers for different outcomes No. dropped out during follow‐up: “41 agreed to participate and 4 dropped out, leaving 37 participants”. Does not say when pp dropped out No. analysed: Total: 37 (LOCF) BFST: Different N’s for each measure, EOIT: Different N’s for each measure Mean age in years (SD): BFST: 14.9; EOIT: 13.4 Age range in years: Total: 11 ‐ 20 Gender %: Total: 0 male, 37 female; BFST: 0 male, 19 Female; EOIT: 0 male, 18 Female Subtype: No detail Age of onset: No detail Duration of illness: Total: < 12 months Baseline weight: Total: BFST: 86.5 pounds (39.3 kg); EOIT: 86.8 pounds (39.5 kg) Baseline BMI: Total: BFST: 15.0 (1.4), EOIT: 16.3 (2.8) Baseline eating disorder scale score (EAT): BFST: n = 19 32.6 (SD 15.6); EOIT: n = 16 20.6 (SD 15.6) Baseline purging: BFST: 0; EOIT: 0 Comorbidity: Total: 54% mood disorder, 13% anxiety disorder; BFST: BDI score 19.4 (12.3); EOIT: BDI score 11.3 (10.5) Details on living arrangements: Total: All residing at home with 1 or both parents (34 in 2‐parent homes; 3 in single‐mother households) Family education/employment/income (Socioeconomic Status (Hollingshead Four Factor Scale):, BFST: 47.5 (13.6); EOIT: 47.9 (12.0) Recruitment strategy: Investigator’s practice settings, letters sent to physicians, psychologists, clergy, community agencies and schools, public service announcements/media stories, presentations to schools and clinics by the investigators Exclusion criteria: No detail | |
| Interventions | Setting of care: Outpatient treatment provided. Some participants hospitalised with treatment provided as inpatients (11 in the family group and 5 in the individual group) Training/qualification of care provider(s): Yes: 4 doctoral psychologists, 1 masters social worker Treatment manual: Yes Supervision of treatment: No details Adherence to treatment: Yes: All audiotaped and 40 sessions sampled with checklist Intervention group 1 Description: Behavioral family systems Description in the report similar to family‐based therapy including all 3 phases Length: Average 15.9 months Intervention group 2 Description: Ego‐oriented individual therapy Aimed to build ego strength, autonomy and insight. Parents also met with therapists bimonthly Length: Average 15.9 months | |
| Outcomes |
Eating psychopathology
EAT (Garner 1979)
The body shape questionnaire and the dissatisfaction scale of EDI (Garner 1983)
Behavioural indices
BMI
Percentage who reached/exceeded target weight
Menstruation
General psychopathology
BDI (Beck 1961)
Child Behaviour Checklists Internalising Behaviour Problems Score (Achenbach 1991) Global pathology and interpersonal functioning Ego functioning ‐ the ineffectiveness interpersonal distrust and interoceptive awareness scale (Garner 1983). Family functioning General and Eating‐Related Conflict (Robin 1990) Observed family conflict ‐ Interaction Behaviour Code for videotaped interactions (Robin 1989) |
|
| Notes | Included in family therapy vs individual psychological intervention Family therapy categorised as family‐based therapy Funded by: National Institute of Mental Health Grant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Correspondence from author stated "coin tossing" was used |
| Allocation concealment (selection bias) | Unclear risk | Correspondence from author suggested concealment was not possible, but this was followed by a description of blinding |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Correspondence from author stated that this was not possible except for those coding the family interactions. |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk |
|
Russell 1987.
| Methods | RCT | |
| Participants | Country: United Kingdom Diagnostic tool: DSM‐III + extreme self‐induced weight loss, fear of fatness psychopathology, endocrine disorder (amenorrhoea in females, sexual dysfunction in males) No. screened: No detail No. randomised: Total : 80; Family therapy: 41 (includes the BN participants); Individual therapy: 38 (includes the BN participants) No. dropped out after randomisation and before start of trial: Total: Group 1 (AN, onset < 18 onset, < 3 yrs duration): 1a ‐ 0, 1b ‐ 0, Group 2 (AN < 18 onset, > 3 yrs duration): 2a ‐ 1, 2b ‐ 1, Group 3 (AN > 19 onset): 3a ‐ 1, 3b ‐ 0 No. dropped out during intervention (did not receive a year of therapy): Total : 17; Family Therapy (a) Group 1 = 1, Group 2 = 2; Group 3 = 3; Individual therapy (b) Group 1 = 7, Group 2 = 3; Group 3 = 0 No. dropped out during follow‐up: 5 years (total only): 3 died; had data on 77 (63 from clinical interview; 1 telephone interview; 3 returned a questionnaire; indirect information from parents or GP) (for 7 participants who refused 5‐year follow‐up they used 3‐year outcomes) No. analysed: 1 year: Family therapy 5 did not get included in 1‐year analysis; Individual therapy 2 in individual therapy did not get included in 1‐year analysis, 5 years: total 77 NOTE: for this study most data are not given by intervention group but by subgroup: Group 1: AN, onset < 18 onset , < 3 yrs duration; Group 2: AN < 18 onset, > 3 yrs duration; Group 3: AN > 19 onset (Group 4 was made up of participants with BN) Mean age in years (SD): Group 1 (AN, onset < 18 onset,< 3 yrs duration): 16.6 (1.7); Group 2 (AN < 18 onset, > 3 yrs duration): 20.6 (4.0); Group 3 (AN > 19 onset): 27.7 (7.8) Age Range: No details Gender %: Total (including BN group): 9% male; 91% female Subtype: No details Age of onset in years (SD): Group 1 (AN, onset < 18 onset,< 3 yrs duration): 15.3 (1.8); Group 2 (AN < 18 onset, > 3 yrs duration): 14.3 (2.4); Group 3 (AN > 19 onset): 24.6 (5.8) Duration of illness: Group 1: by definition < 3 yrs duration; Group 2: by definition > 3 yrs duration; Group 3: by definition no details Baseline weight (on discharge from inpatient admission): Group 1 (AN, onset < 18 onset, < 3 yrs duration): 88.9 (7.4) ABW%; Group 2 (AN < 18 onset, > 3 yrs duration): 91.4 (5.5) ABW%; Group 3 (AN > 19 onset): 85.8 (7.3) ABW% Paper stated that the participants were generally severe with an average admission weight of 69.9% ABW Baseline BMI: No details Baseline eating disorder scale score: No details Baseline purging: No details Comorbidity: Paper stated “most patients‐complicated by episodes of self harm severe depression or personality disorder” with no other details given Details on living arrangements:Total : 64 single, 8 married, 3 separated/divorced; 60 were living with parents, 12 were living with a spouse or co‐habiting, 8 lived alone Family education/employment/income: No details Recruitment strategy: No details Exclusion criteria: No details | |
| Interventions | Setting of care: Outpatient (following inpatient refeeding for an average of 10.4 weeks) Training/qualification of care provider(s): Yes: 3 social workers and 1 psychologist Treatment manual: No details Supervision of treatment: Yes Adherence to treatment: No details Intervention group 1 Description: Family‐based therapy Length: 1 year from the date of discharge from hospital Intervention group 2 Description: Individual supportive therapy Included supportive problem‐centred counselling, education with elements of cognitive, interpretive and strategic therapy Length: 1 year from the date of discharge from hospital | |
| Outcomes | Eating psychopathology Morgan Russell Assessment Schedule (Morgan 1988) Behavioural indices BMI Menstruation Good outcome/Intermediate outcome/ Poor outcome Need for readmission General psychopathology and Obsessionality CCEI (Crown 1979) | |
| Notes | Included in family therapy vs individual psychological intervention. Family therapy categorised as family‐based therapy Dare 1990 and Russell 1987 refer to the acute study and Eisler 1997 is the follow‐up study. 1‐year follow‐up data are the equivalent to end of treatment 5‐year mortality data are still being checked by authors and will be provided Funded by: Medical Research Council, Britain | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Personal communication stated stratified randomisation by diagnostic and prognostic groups |
| Allocation concealment (selection bias) | Low risk | Personal communication stated sealed envelopes were used |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
|
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | High risk |
|
| Other bias | High risk |
|
1. Search Strings.
| Medline | PsycInfo | Embase |
| 1. exp Eating Disorders/ 2. Anorexia/ or Anorexia Nervosa/ 3. 1 or 2 4. Family Therapy/ 5. family therap$.tw. 6. family based therap$.tw. 7. family‐based therap$.tw. 8. systems therap$.tw. 9. family system$ therap$.tw. 10. family treatment$.tw. 11. family intervention$.tw. 12. or/4‐11 13. 3 and 12 14. clinical trial.pt. 15. clinical trial$.mp. 16. random$.mp. 17. placebo.ti,ab. 18. groups.ti,ab. 19. or/14‐18 20. 13 and 19 |
1. exp Eating Disorders/ 2. Anorexia Nervosa/ 3. 1 or 2 4. Family Therapy/ 5. Family Intervention/ 6. Conjoint Therapy/ 7. family therap$.tw. 8. family based therap$.tw. 9. family‐based therap$.tw. 10. systems therap$.tw. 11. family system$ therap$.tw. 12. family treatment$.tw. 13. family intervention$.tw. 14. conjoint therap$.tw. 15. or/4‐14 16. 3 and 15 17. Clinical Trials/ 18. controlled trial$.tw. 19. (controlled studies or controlled study).tw. 20. random$.tw. 21. Random Sampling/ 22. ((singl$ or doubl$ or trebl$ or tripl$) adj5 (blind$ or dummy or mask$)).tw. 23. placebo$.mp. 24. or/17‐23 25. 16 and 24 |
1. exp Eating Disorders/ 2. Anorexia Nervosa/ 3. 1 or 2 4. Family Therapy/ 5. Family Intervention/ 6. family therap$.tw. 7. family based therap$.tw. 8. family‐based therap$.tw. 9. systems therap$.tw. 10. family system$ therap$.tw. 11. family treatment$.tw. 12. family intervention$.tw. 13. conjoint therap$.tw. 14. or/4‐13 15. exp controlled study/ 16. (controlled trial$ or controlled study or controlled studies).tw. 17. exp clinical trial/ 18. (clinical trial$ or clinical study or clinical studies).tw. 19. random$.tw. 20. single blind procedure/ 21. double blind procedure/ 22. ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$ or dummy)).tw. 23. placebo$.mp. 24. or/15‐23 25. 3 and 4 and 24 |
Russell 1987a.
| Methods | See Russell 1987 | |
| Participants | See Russell 1987 | |
| Interventions | See Russell 1987 | |
| Outcomes | See Russell 1987 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | See Russell 1987 |
| Allocation concealment (selection bias) | Unclear risk | See Russell 1987 |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Russell 1987 |
| Selective reporting (reporting bias) | Unclear risk | See Russell 1987 |
| Other bias | Unclear risk | See Russell 1987 |
Russell 1987b.
| Methods | See Russell 1987 | |
| Participants | See Russell 1987 | |
| Interventions | See Russell 1987 | |
| Outcomes | See Russell 1987 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | See Russell 1987 |
| Allocation concealment (selection bias) | Unclear risk | See Russell 1987 |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Russell 1987 |
| Selective reporting (reporting bias) | Unclear risk | See Russell 1987 |
| Other bias | Unclear risk | See Russell 1987 |
Russell 1987c.
| Methods | See Russell 1987 | |
| Participants | See Russell 1987 | |
| Interventions | See Russell 1987 | |
| Outcomes | See Russell 1987 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | See Russell 1987 |
| Allocation concealment (selection bias) | Unclear risk | See Russell 1987 |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Russell 1987 |
| Selective reporting (reporting bias) | Unclear risk | See Russell 1987 |
| Other bias | Unclear risk | See Russell 1987 |
Whitney 2012.
| Methods | RCT | |
| Participants | Country: UK
Diagnostic tool: DSM‐IV
No. screened: 95
No. randomised: Total: 48; IFW: 23; FDW: 25
No. started trial: No detail
No. dropped out during intervention:Total: 6; IFW: 3; FDW: 3
No. dropped out during follow‐up:Total: 11; IFW: 5; FDW: 6
No. analysed (OC): BMI (long‐term follow‐up), IFW: 21, FDW: 23, SEED AN (long‐term follow‐up), IFW 15, FWD 14, SEED BN (long‐term follow‐up), IFW: 15, FWD: 14, IIP (long‐term follow‐up), IFW: 11, FWD: 14
Mean age in years (SD): Total: 25 (9.15)
Age range: No detail
Gender %: Total: 4% (1) male; 96% (47) female, IFW: 1 male; 22 female, FDW: 0 male; 25 female
Subtype: Total: no specific detail on subtype but text states “the patients primarily had the restricting type of AN. Approximately 20‐25% used vomiting or laxatives, and approximately half reported using excessive exercise”
No detail by group
Age of onset: No detail
Duration of illness (months): Total : 56% had a duration of ± 5 years; 25% had ± 10 years, IFW: range 1 ‐ 20 years, FDW: range <1 ‐ >20 years
Baseline weight: No detail
Baseline BMI: Total : 13.3 (1.6); No detail by group
Baseline eating disorder scale score, IFW: SEED AN 13.3 (1.6), FDW: SEED AN 13.2 (1.5)
Baseline purging (vomiting at least once a day): Total: IFW: 6 (26%), FDW: 4 (16%)
Comorbidity: No detail
Details on living arrangements: Total: IFW: 65% living in family unit (52% parents; 9% spouse; 4% children); FDW: 88% living in family unit (80% parents; 8% spouse; 0% children)
Family education/employment/income: Detail of highest education, occupation, employment status and income/support for participants reported in Table 2
Recruitment strategy: Consecutive referrals to the inpatient eating disorder unit
Exclusion criteria:
|
|
| Interventions | Setting of care: Inpatient Training/qualification of care provider(s): Yes: “six experienced eating disorder therapists from diverse mental health professional backgrounds (e.g. nurses, social workers, and doctors) all with training in family work” pg. 9 Treatment manual: No detail Supervision of treatment: Yes: “All participated in training workshops prior to the commencement of the study with regular supervision throughout the study” pg. 9 Adherence to treatment: Yes: “Typically two therapists were involved in both interventions. The sessions were video‐taped for supervision and to ensure treatment fidelity” pg. 9 Intervention group 1 Description: Specific family therapy Involved 2 phases: 1. engaging family, dispelling myths about AN, reducing parental guilt, instilling confidence in parents that they can help child; 2. problem‐ and symptoms‐oriented focus with emphasis on parental coping strategies, functional analysis of difficulties in managing AN in the home, reduction of hostile, over‐critical or over‐protective interactions Length: 18 hours of treatment in 1 ‐ 2 hour weekly or fortnightly sessions with 3 follow‐up sessions Intervention group 2 Description: Standard family systems therapy Highly structured intervention working with 2 families over 3 days with the aim to promote rapport between families to share difficulties and strengths in managing and including shared meals. Day 1 focus on family difficulties; Day 2 focus on current family functioning and organisation around AN; Day 3 teaching philosophies that underpin health behaviour change Length: 18 hours of treatment over 3 days followed by 3 hour‐long follow‐up sessions | |
| Outcomes | Eating psychopathology SEED (Kordy 2005) Behavioural indices Weight change (BMI) Global pathology and interpersonal functioning Inventory of Interpersonal Problems Family functioning LEE scale Other Measurement at baseline, discharge (mean 5.3 months (6 months for carers)) and at 3‐year follow‐up | |
| Notes | Included in individual family therapy vs group family therapy comparison Family therapy in both cases categorised as other Funded by: Psychiatry Research Trust | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly allocated" pg. 4, no detail |
| Allocation concealment (selection bias) | Low risk | Quote: "the randomisation administrator informed the clinical team of the group assignment. The randomisation sequence had been generated independently from the clinical team and was placed in numbered sealed envelops" pg. 5 |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Therapists and participants cannot be blinded in trials of family‐based therapy |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
|
| Selective reporting (reporting bias) | Low risk |
|
| Other bias | Unclear risk |
|
ABW: average body weight; BFT: behavioural family therapy; BMI: body mass index; BN: bulimia nervosa; BPRS‐E: brief psychiatric rating scale‐expanded; CBT: cognitive behavioural therapy; CCEI: Crown‐Crisp experimental index; CDI: children's depression inventory; CYBOCS: children's Yale‐Brown obsessive‐compulsive scale; DASS: depression, anxiety and stress scale; DICA: diagnostic interview for children and adolescents; DP: day patient; EAT: eating attitudes test; EDE: eating disorder examination; EDI: eating disorder inventory; EDS: eating disorder scale; EFS: family health scale; FAD: family assessment device; FBT: family‐based therapy; GOAS: global outcome assessment scale; IBC: interactive behaviour code; HAMD: Hamilton depression scale; HRQ: helping relationship questionnaire; IBW: ideal body weight; IP: inpatient; ITT: intention‐to‐treat; LOCF: last observation carried forward; MDD: major depressive disorder; MI: motivational interviewing; MMPW: mean matched population weight; MRAOF: Morgan‐Russell outcome scale; MRGAS: Morgan‐Russell global assessment scale; MRS: Morgan Russell scale; OC: observed case; OP: outpatient; PVA: parent versus anorexia; RSE: Rosenberg self‐esteem (scale); SAS: social adjustment scale; SCFI: standardised clinical family interview; SCL‐90‐R: symptom check list‐revised; SD: standard deviation; SEED: short evaluation of eating disorders; STAI: state‐trait anxiety inventory; SyFT: systematic family therapy; TAU: treatment as usual; TSPE: Therapy suitability and patient expectancy; YBCSEDS: Yale‐Brown‐Cornell eating disorder scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Attia 2012 | Not an RCT |
| Buddeberg 1979 | 2 case histories presented |
| Ciao 2015 | Not Anorexia Nervosa |
| Dalle Grave 2010 | Not family therapy, describes but does not report on RCT |
| Fettes 1992 | Not Anorexia Nervosa |
| George 1997 | Not an RCT |
| Gilbert 2008 | Not an RCT |
| Goddard 2013 | Not family therapy |
| Gowers 2010 | Not family therapy |
| Karwautz 2015 | Not family therapy |
| Keshen 2013 | Not family therapy |
| Le Grange 2005a | Not an RCT |
| Loeb 2007 | Not an RCT |
| Perkins 2005 | Not Anorexia Nervosa |
| Reyes‐Rodriguez 2011 | Not Anorexia Nervosa |
| Salbach 2006 | Not an RCT |
| Schmidt 2005 | Not Anorexia Nervosa (participants are carers) |
| Schmidt 2013 | Not family therapy |
| Slagerman 1989 | Not an RCT |
| Spettigue 2015 | Not family therapy |
| Treasure 2006 | Not family therapy |
| Treasure 2007 | Not an RCT |
| Vandereycken 1977 | Not family therapy |
| Vandereycken 1978 | Not family therapy |
| Wallin 2000 | All participants received family therapy and were randomised to receive individual body awareness therapy |
| Whitney 2012b | Not Anorexia Nervosa (participants are carers) |
| Woidislawsky 1996 | Not family therapy. Mixed sample ‐ unable to separate AN data |
Characteristics of studies awaiting assessment [ordered by study ID]
Bulik 2009.
| Methods | Randomised parallel assignment |
| Participants | Inclusion Criteria:
Exclusion Criteria:
|
| Interventions |
Intervention group 1 Description: CBCT. CBCT consists of 1‐hour weekly sessions between a couple and a therapist. In this programme, couples learn about ways to communicate about their relationship in the context of experiencing anorexia nervosa. CBCT focuses on couple‐specific skills such as communication and targets relationship domains such as exercise, body image and sexuality, eating together as a couple, and broader relationship concerns outside of anorexia nervosa Length: 20 weeks Intervention group 2 Description: Family supportive therapy Couples meet once a week for an hour for couples therapy. Family supportive therapy is not manualised and is the standard form of care at the UNC Eating Disorders Programme Length: 20 weeks |
| Outcomes | Not provided |
| Notes | clinicaltrials.gov/show/NCT00928109 |
Dimitropoulos 2014.
| Methods | Randomised parallel assignment |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention group 1 Description: Multi‐family therapy Involves 8 ‐ 10 families who meet as a group with 2 therapists for a duration of 8 x 1½‐hour sessions. Group topics are set and cover material on eating disorder psychoeducation, caregiving styles, meal support and relapse prevention. Length: ˜8 weeks Intervention group 2 Description: Supportive family therapy Families meet independently with a therapist once a week for 1‐hour session of supportive counselling. The length of the therapy and the topics of therapy are decided upon collaboratively with the therapist and the family. Length: ˜10 weeks |
| Outcomes | Primary outcomes: 1. Dropouts 2. Change in weight Secondary outcomes: 1. Change in caregiver functioning |
| Notes | clinicaltrials.gov/show/NCT02106728 [Study results available, July 2016] |
Eisler 2006.
| Methods | Multi‐centre randomised treatment trial |
| Participants | Participants are referred to 5 eating disorder services (South London and Maudsley NHS Trust, St Georges and South West London NHS Trust , Blackwater Valley Primary Health Care Trust, Central & Northwest London Trust, The Child and Adolescent Eating Disorder Service of the Royal Free Hampstead Trust) Inclusion criteria
Exclusion criteria:
|
| Interventions |
Intervention group 1 Description: Inpatient treatment "Inpatient treatment is based around a carefully structured nursing regimen, the main aims of which are: 1. To form a therapeutic alliance 2. To achieve weight restoration Other members of the multidisciplinary team provide additional therapeutic input depending on the needs of individual participants. Participants allocated to inpatient treatment will be admitted to a specialist Eating Disorder Unit for approximately 12 weeks. The actual length of inpatient stay will be determined by the time needed for each individual participant to reach a healthy weight. The study design, however, will limit the length of time from reaching a healthy weight to discharge from hospital to 2 weeks. Following discharge from hospital they will receive regular follow‐up treatment for 6 months for themselves and their families. To ensure continuity of treatment the therapist responsible for the follow‐up treatment will engage the participant and her family during the last 2 weeks of the inpatient stay" (from website: http://www.isrctn.com/ISRCTN11275465). Length: 12 months (inpatient stay plus follow‐up) Intervention group 2 Description: Family‐based therapy Outpatient therapy. "These are mainly conjoint family meetings, although some individual sessions are included where appropriate (particularly with older adolescents at later stages of the treatment)" (from website: http://www.isrctn.com/ISRCTN11275465). Length: 12 months Intervention group 3 Description: Multi‐family day treatment (MFTD) "MFDT is a new treatment programme that has been developed over the past 3 years at the Maudsley Hospital and at the Eating Disorder Service in Dresden. The treatment provides a more intensive form of family intervention than the usual outpatient family therapy, but is conceptually very similar. In common with our outpatient family therapy, MFDT aims to help families rediscover their own resources by emphasising ways in which parents can take control of re‐nutrition. At the same time the families are encouraged to use the group setting to explore how the eating disorder and the interactional patterns in the family have become entangled, making it difficult for the family to follow the normal developmental course of the family life‐cycle. The sharing of experiences and the dynamics of the multiple family group are important components of the treatment. The treatment starts with an intensive one‐week multiple family day programme for up to 6 families and is followed by a further 4 to 5 one‐day meetings at 4‐ to 8‐week intervals. Individual family meetings are scheduled in the intervals between group meetings as needed, with the overall length of treatment for each family being 12 months. A wide range of intervention techniques is used (including group, family, psycho‐educational and creative techniques) with multiple family, parent or adolescent groups as well as individual family meetings. There is also practical input around managing mealtimes and food" (from website: http://www.isrctn.com/ISRCTN11275465). Length: 12 months |
| Outcomes | Primary outcomes: 1. Symptomatic change: a. BMI (kg/m2) b. SEED symptomatology c. EDE d. C‐EDE 2. Health economic costs a. Client service receipt inventory Secondary outcomes: 1. Participants/family satisfaction questionnaire 2. Experience of caregiving |
| Notes | www.controlled‐trials.com (2007) ISRCTN11275465 |
Gore‐Rees 2001.
| Methods | Randomisation of cases of anorexia nervosa to receive any of 3 treatments |
| Participants | Anorexia Nervosa |
| Interventions | Inpatient against outpatient treatment |
| Outcomes | Primary Outcomes: Composite clinical measure of physical, social and psychological outcome Secondary Outcomes: Percentage weight for height, family functioning, HoNOSCA score, participant and family acceptability |
| Notes |
Jacobi 2012.
| Methods | Randomised controlled trial of 1 active intervention and 1 control condition |
| Participants | Inclusion criteria:
|
| Interventions |
Intervention group 1 Description: Family‐oriented, internet‐based intervention. The intervention consists of an online programme for parents of adolescent daughters moderated by eating disorder experts (e.g. diploma‐level psychologists). Parents are educated on the danger of AN and the need to intervene to prevent this outcome. In addition, parents are encouraged to take definitive steps to intervene with any weight loss efforts (dieting, diet pills, over‐exercise) in order to prevent the elaboration of these behaviours with an attendant escalation in medical and psychological problems. Additional features are an online discussion group, 2 phone calls to enable individualised feedback on the child's problems with eating, weight and shape, and referral to other resources (self‐help guide,Lock 2004); in‐ or outpatient treatment) if necessary Length: 6 sessions over 6 weeks Control group Description: Non‐intervention control group Length: 'non‐intervention' |
| Outcomes | Primary outcomes: 1. Weight normalisation (changes in BMI) 2. Weight and shape concerns, eating concerns, restraint (restrictive eating): EDE interview Secondary outcomes: 1. Risk status (as described in inclusion criteria, questionnaire) 2. Full or partial AN diagnoses: EDE interview 3. Drive for thinness, body dissatisfaction: EDI‐2 questionnaire 4. Self‐esteem: RSE questionnaire 5. Depression: BDI‐II questionnaire 6. Perfectionism: MPS‐F questionnaire 7. Social adjustment: SAS, German version: Fragebogen zur sozialen Integration, FSI, questionnaire |
| Notes | www.isrctn.com/ISRCTN18614564 |
Le Grange 2005.
| Methods | Participants in this open‐label study will be randomly assigned to 1 of 3 treatment groups. Study visits will occur at baseline, immediately post‐intervention, and again 6 months and 1 year post‐intervention |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention group 1 Description: Family‐based therapy Labelled 'Standard Family Therapy' in report Length: 24 hours over 12 months Intervention group 2 Description: Individual adolescent‐focused therapy An ego‐oriented psychotherapy treatment Length: 24 hours over 12 months Intervention group 3 Description: Specific family therapy (not described in report) Length: 24 hours over 12 months |
| Outcomes | Primary outcomes: 1. Weight (BMI) Secondary outcomes: 1. Changes in weight and shape concerns as measured with EDE subscales |
| Notes | clinicaltrials.gov/show/NCT00183586 |
Lock 2014.
| Methods | Randomised parallel assignment |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention group 1 Description: Family‐based therapy with CRT Length: 15 sessions over 6 months Intervention group 2 Description: Family‐based therapy and art therapy Length: 15 sessions over 6 months |
| Outcomes | Primary outcome measures: 1. Full remission from AN (weight restoration to at least 95% of median body weight) |
| Notes | clinicaltrials.gov/show/NCT02054364 |
Nevonen 2015.
| Methods | Single‐centre randomised control trial |
| Participants | Inclusion criteria:
|
| Interventions |
Intervention group 1 Description: Individual cognitive behavioural therapy (I‐CBT) This intervention aims to target specific factors related to the eating disorder psychopathology that are involved in the development and maintenance of the disorder. The treatment is manual‐based and tailored for each participant for attitudes and behaviours associated with weight, shape and eating control and general psychopathology such as perfectionism, low self‐esteem and interpersonal problems. The treatment consists of sessions divided into 3 phases. Phase 1 focuses on alliance, motivation and treatment formulation. One family session is included for the purpose of educating about eating disorders and its consequences and how the family can support the participant. Phase 2 lasts for a year with 1 session a week targeting the psychopathology of the eating disorder in order to change the dysfunctional thoughts and behaviours related to eating, body image and weight Length: 60 1‐hour sessions over 18 months Intervention group 2 Description: Family‐based therapy Maudsley approach. Length: 40 ninety‐minute sessions over 18 months |
| Outcomes | Primary outcomes: 1. BMI 2. The Rating of Anorexia and Bulimia Interview‐revised version (RAB‐R) is a Swedish semi‐structured interview for clinical and research purposes for a wide range of eating disorder symptoms and related psychopathology through which the patient receives a DSM‐IV diagnosis Secondary outcomes: 1. Eating Disorder Inventory‐3 (EDI‐3) 2. Beck's Depression Inventory (BDI) 3. Family Relation Scale (FARS) 4. Inventory of Interpersonal Problems (IIP) 5. Eating Disorder Expectations and Experiences (EDPEX) 6. Body Shape Questionnaire (BSQ) 7. Treatment credibility 8. Visual Analoge Scale regarding Parental burden (VAS) 9. Rosenber Self‐Esteem Scale (RSE) 10. Treatment Satisfaction Scale (TSS) 11. Background questionnaire |
| Notes | www.isrctn.com/ISRCTN25181390 |
Rugiu 1999.
| Methods | The participants selected for the study were randomly allocated to 2 groups. All patients were given clinical examinations and tests before and after the treatment |
| Participants | Individuals with anorexia nervosa or bulimia |
| Interventions | Family therapy according to a paradoxical approach (elementary Pragmatic Model) and Day Hospital integrated approach |
| Outcomes | The results of follow‐up indicated a greater efficacy of day hospitals in bulimia and family therapy in anorexia |
| Notes | From CCDAN Studies Register |
Zucker 2008.
| Methods | Two‐stage research design. Phase 1 will consist of focus groups comprising members of parent‐training groups. Results from Phase I will be used to improve the intervention. She will then subject the improved intervention to a pilot, pre‐post, randomised design to assess preliminary efficacy in Phase 2. This initial trial will lead to further enhancements of the programme, will define the populations most suited to a group parent‐training model, will permit exploration of potential mechanisms of action, and will highlight additional participant needs for further treatment development. Allocation: Randomised Control: Active control Endpoint classification: Safety/efficacy study Intervention Model: Parallel assignment Masking: Single‐blind (outcomes assessor) Primary Purpose: Treatment |
| Participants | Inclusion Criteria:
Exclusion Criteria:
|
| Interventions |
Intervention group 1 Description: Group parent‐training skills Group for parents that provides psychoeducation for eating disorder and skills in behaviour management, self‐regulation, and emotion regulation Length: not stated Intervention group 2 Description: Family‐based therapy Maudsley approach Length: not stated |
| Outcomes | Primary outcomes: 1. BMI Secondary outcomes: 2. Eating disorder symptoms other than body weight |
| Notes | clinicaltrials.gov/ct2/show/NCT00672906 |
AN: anorexia nervosa; BDI: Beck depression inventory; BMI: body mass index; BSQ: body shape questionnaire; CBCT: cognitive behavioural couple therapy; C‐EDE: children's eating disorder examination; CRT: cognitive remediation therapy; EDE: eating disorder examination; EDI: eating disorder inventory; EDPEX: eating disorder expectations and experience; FARS: family relation scale; FBT: family‐based therapy; IIP: inventory of interpersonal problems; MPS‐F: Frost multidimensional perfectionism scale; RAB‐R: Rating of Anorexia and Bulimia Interview‐revised version; RSE: Rosenberg self‐esteem; SAS: social adjustment scale; SEED: severity of eating disorder; TSS: treatment satisfaction scale; VAS: visual analogue scale;
Characteristics of ongoing studies [ordered by study ID]
Bilyk 2017.
| Trial name or title | Effectiveness of a Cognitive Behavioral Management Pilot Program in a sample of Brazilian adolescents with Anorexia Nervosa |
| Methods | Clinical treatment trial, parallel, open, non‐randomized controlled with two arms. |
| Participants | Adolescents aged 12 to 17 with Anorexia Nervosa with significant weight loss, marked by the decrease of at least a percentile below the expected for the age, based on the body mass index (BMI) curve for age, gender and compared to the patient's weight before disease onset |
| Interventions | Cognitive‐Behavioral Psychotherapy delivered in groups; 24 90‐minute sessions. The patients also received psychiatric, nutritional and family treatment during the 6 months. Comparison group received psychiatric, nutritional and family treatment for 6 months without cognitive behavioral therapy. |
| Outcomes | Weight recovery based on the adequacy or improvement of the percentile expected for the age verified by the growth curve of Body Mass Index for the age of the World Health Organization, associated with decreased symptoms of Eating Disorder evaluated by decreased scores on the Questionnaire of examination for eating disorders applied in the pre‐, post‐intervention and follow‐up. |
| Starting date | 2015‐02‐04 |
| Contact information | bacy@uol.com.br |
| Notes |
Bulik 2012.
| Trial name or title | Enhancing treatment for adult anorexia with a couple‐based approach |
| Methods | Randomised parallel assignment |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention group 1 Description: Uniting Couples in the Treatment of Anorexia Nervosa (UCAN) + Cognitive Behavioural Therapy (CBT) This condition includes 22 UCAN sessions and 22 CBT sessions, totaling 44 psychotherapy sessions. UCAN is a manualised, 22‐session Cognitive Behavioral Couple Therapy (CBCT) intervention that engages the couple to target the core psychopathology of AN and address the uniquely challenging stress that AN places on intimate relationships. The CBT proposed for this study is a 22‐session adaptation of the manualised intervention that has been employed successfully as an outpatient post‐hospitalisation therapy and in an National Institute of Mental Health multi‐site study of fluoxetine with elements from the CBT manual used in McIntosh 2005. Intervention group 2 Description: CBT In this condition, participants will receive a higher "dose" of individual CBT, with 44 total sessions. Our experience with patients in the pilot strongly suggests that a higher dose of CBT will allow for further, fruitful discussion and exploration of key individual issues and is unlikely to be experienced as diluted or a slow approach to treatment. Most of these patients have complicated histories, long‐standing eating disorders, and complex comorbid conditions. |
| Outcomes | Primary outcomes: 1. Change in BMI from baseline through 12 month follow‐up 2. Change in Global EDE Scores from baseline through 12 month follow‐up Secondary outcomes: 1. Dropout (the percentage of individuals who withdrew participation from treatment) 2. Treatment satisfaction scores as measured with the CSQ 3. Relationship satisfaction as measured with the DAS and DAS‐4 (measures extent to which someone is happy in his or her relationship) Other outcomes: 1. Cost effectiveness ratio (= the ratio of the change in costs to incremental benefits of a therapeutic intervention or treatment. It will be calculated using data from the MFED |
| Starting date | July 2012 |
| Contact information | Camden Matherne, Ph.D; ph: 9119‐843‐2483; email: ucan @unc.edu |
| Notes | clinicaltrials.gov/show/NCT01740752 |
Carrot 2017.
| Trial name or title | Family Therapy and Anorexia Nervosa : Which is the Best Approach? (THERAFAMBEST) |
| Methods | Non inferiority randomised trial |
| Participants | 13 to 19 year olds; Anorexia Nervosa according to DSM‐5 criteria |
| Interventions | Multiple Family Therapy (MFT) within a multi‐disciplinary treatment program for Anorexia Nervosa (AN) versus single Systemic Family Therapy (SyFT) |
| Outcomes | Change from baseline Body Mass Index (Weight in KG / Height in m²) at 12 months |
| Starting date | January 8, 2018 |
| Contact information | benjamin.carrot@imm.fr |
| Notes |
Hildebrandt 2016.
| Trial name or title | Reward Systems and Food Avoidance in Eating Disorders |
| Methods | Randomised controlled trial |
| Participants | 12 to 18 year olds; Refusal to maintain greater than minimally low body weight based on BMI for age percentiles and growth trajectories; Clinically significant restriction of food intake on the dietary restraint subscale of the EDE or evidence of persistent food avoidance as reported by patient or guardians |
| Interventions | Interoceptive Exposure (IE) versus Family‐Based Therapy (FBT)) |
| Outcomes | fMRI‐EMG: Change in the emotional responses from facial muscle movements to food pictures and non‐food pictures as measured with the fMRI‐EMG; KCal Intake; Eating Disorder Examination (EDE); Clinical Impairment Assessment; Anxiety Sensitivity Index‐III |
| Starting date | November 2016 |
| Contact information | tom.hildebrandt@mssm.edu; robyn.sysko@mssm.edu |
| Notes |
Lock 2017.
| Trial name or title | Adaptive Treatment for Adolescent Anorexia Nervosa |
| Methods | Randomized controlled trial using an adaptive design |
| Participants | 12 to 18 year olds; living with participants' families; meeting DSM‐5 criteria for AN (both subtypes) except for the amenorrhea requirement; medically stable for outpatient treatment according to the recommended thresholds of the American Academy of Pediatrics and the Society of Adolescent Medicine |
| Interventions | Standard Family Based Treatment (FBT) to adaptive FBT with an Intensive Parental Coaching (IPC) component |
| Outcomes | Estimated Body Weight (EBW) [Time Frame: following 9 months of treatment] |
| Starting date | |
| Contact information | mvierhil@stanford.edu |
| Notes | September 1, 2017 |
McCormack 2014.
| Trial name or title | Know and grow: An investigation into parent and family involvement in eating disorder treatment |
| Methods | Randomised controlled trial |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention group 1 Description: Parent skills training (otherwise known as Collaborative Caring for Loved Ones with an Eating Disorder) This intervention uses parent‐training skills based on motivational interviewing, behavioural analysis, cognitive and interpersonal therapy, dialectical behavioural therapy, problem‐solving skills, and psychoeducation. It is delivered in a group therapeutic workshop face‐to‐face format with mental health practitioner Length: 12 hours of workshop content delivered over 2 consecutive days Intervention group 2 Description: Treatment as usual This means standard treatment at the study site delivered by a multidisciplinary team and includes medical and psychological care and education services Length: not stated |
| Outcomes | Primary outcome measures: 1.Global Eating Disorder Psychopathology using scores on the EDE 2. Child self‐esteem using scores on the RSE scale 3. Family Functioning measured by the Family Assessment Device and the Inventory of Parent and Peer Attachment. Secondary outcome measures: 1. Childhood medical status and measured by BMI, Body fat percentage, mid‐upper arm circumference, ferritin, insulin‐like growth factor and amenorrhoea status (self and parent report) as measured and calculated by paediatrician during medical examination including laboratory blood tests and BODPOD assessments 2. Child levels of depression and anxiety as measured by the Children's Depression Inventory and the Multidimensional Anxiety Scale for Children 3. Carer Distress as measured by the DASS 4. Parent care‐giving burden as measured by the Experience of Care‐giving Inventory 5. Quality of life as measured by the Child Health Questionnaire and the Quality of life Enjoyment and Satisfaction Questionnaire 6. Expressed Emotion as measured by the Family Questionnaire |
| Starting date | February 2015 |
| Contact information | Ms Julie McCormack, Princess Margaret Hospital, Roberts Road, Subiaco 6008 WA, Australia. +61 8 9340 7012. julie.mccormack@health.wa.gov.au |
| Notes |
www.anzctr.org.au/ACTRN12614001296628 2014 |
BMI: body mass index; EDE: eating disorder examination; CBCT: cognitive behavioural couples therapy; CSQ: client satisfaction questionnaire; DASS: depression, anxiety and stress scale; MFED: McKnight follow‐up of eating disorders; RSE: Rosenberg self‐esteem
Differences between protocol and review
There were some changes between the methods undertaken in the original protocol (Fisher 2008), and the original version of the published review (Fisher 2010). The current review has one objective (to evaluate the efficacy of family therapy compared with standard treatment and other treatments in AN). This has been simplified from the four objectives in the previous versions (i.e. 1. To evaluate the efficacy of family therapy compared with standard treatment and other treatments; 2. To investigate the relative efficacy of different forms of family therapy (see section below on 'Types of Interventions'; 3. To investigate the efficacy of family therapy in patients with chronic AN vs non‐chronic AN; 4. To investigate the efficacy of family therapy in adolescents with AN compared to adults with AN). This rationalisation occurred as there were insufficient data in the available studies to investigative the effects of age or of chronicity, effectively in the original review, and similarly in this version. The review authors also decided that the single objective covered the previous second objective, of investigating different forms of family therapy, with analysis of this conducted in the current review.
In the current version of the review we have replaced the term 'cognitive distortion’ with ‘eating disorder psychopathology', to reflect the current terminology in the literature. This assessed variable relates to scores on eating disorder assessment scales and we are of the opinion that ‘eating disorder psychopathology' reflects this more accurately than 'cognitive distortion', as some of the items on these scales do not relate to cognitions but rather to behaviours.
Rates of missing data in the newly‐included studies in this version of the review were lower than in the studies in the original version of the review. Where data directly relevant to the specific outcome measures were reported to have been obtained during the study (based on the outlined methodology) but were not reported, we contacted authors (i.e. Besharat 2001) in an attempt to acquire these data. However, we were unable to obtain the data that related directly to the primary and secondary outcomes of the review.
New Summary of findings tables have been included in this update of the review.
Contributions of authors
All authors were involved in the inclusion/exclusion assessment of studies. CF, SS and KR extracted the information about trials (for the Table of Included Studies) and outcome data and undertook 'Risk of bias' assessment. CF and SH analysed the data, and all authors contributed to the write‐up of the review. All authors contributed to the write‐up of the Discussion and final preparation of the manuscript.
Sources of support
Internal sources
Orygen Youth Health Research Centre funded and supported by The Colonial Foundation, Australia.
External sources
No sources of support supplied
Declarations of interest
Caroline Fisher: None known; Sonja Skocic: None known; Katheleen Rutherford: None known; Sarah Hetrick: None known.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Agras 2014 {published data only}
- Agras WS. Family therapy in the treatment of adolescent anorexia nervosa. NIH CRISP. [CRSREF: 2855946; NIH grant number: 5U01MH076290]
- Agras WS, Lock J, Brandt H, Bryson SW, Dodge E, Halmi KA, et al. Comparison of 2 family therapies for adolescent anorexia nervosa: a randomized parallel trial. JAMA Psychiatry 2014;71(11):1279‐86. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Agras WS, Bryson SW, Brandt H, Halmi KA, Kaye W, et al. Does family‐based treatment reduce the need for hospitalization in adolescent anorexia nervosa?. International Journal of Eating Disorders 2016;49(9):891–4. [DOI: 10.1002/eat.22536] [DOI] [PubMed] [Google Scholar]
- Lock J, Brandt H, Woodside B, Agras S, Halmi WK, Johnson C, et al. Challenges in conducting a multi‐site randomized clinical trial comparing treatments for adolescent anorexia nervosa. International Journal of Eating Disorders 2012;45(2):202‐13. [DOI: 10.1002/eat.20923] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh‐Sharvit S, Arnow KD, Osipov L, Lock JD, Jo B, Pajarito S, et al. Are parental self‐efficacy and family flexibility mediators of treatment for anorexia nervosa?. International Journal of Eating Disorders 2018;51(3):275‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ball 2004 {published data only (unpublished sought but not used)}
- Ball J, Mitchell P. A randomized controlled study of cognitive behaviour therapy and behavioral family therapy for anorexia nervosa patients. Eating Disorders 2004;12(4):303‐14. [DOI] [PubMed] [Google Scholar]
- Ball JR. A controlled evaluation of psychological treatments for anorexia nervosa. (cognitive behavior therapy, behavioral family therapy). Dissertation Abstracts International 1999;59(11‐B):5781. [Google Scholar]
- Ball JR, Mitchell PB, Touyz SW, Griffiths RA, Beumont PJ. Clinical utility of the modified Stroop task as a treatment outcome measure: Questions raised. Clinical Psychologist 2004;8(2):76‐80. [Google Scholar]
Besharat 2001 {published data only (unpublished sought but not used)}
- Besharat MA. The predictive value of family expressed emotion in eating disorders. Iranian Journal of Medical Sciencse 2001;26(3 & 4):110‐5. [Google Scholar]
Crisp 1991 {published data only (unpublished sought but not used)}
- Crisp AH, Norton K, Gowers S, Halek C, Bowyer C, Yeldham D, et al. A controlled study of the effect of therapies aimed at adolescent and family psychopathology in anorexia nervosa. British Journal of Psychiatry 1991;159:325‐33. [DOI] [PubMed] [Google Scholar]
- Gowers S, Norton K, Halek C, Crisp AH. Outcome of outpatient psychotherapy in a random allocation treatment study of anorexia nervosa. International Journal of Eating Disorders 1994;15(2):165‐77. [DOI] [PubMed] [Google Scholar]
- Gowers S, Phil M, Norton K, Yeldham D, Bowyer C, Levett G, et al. The St. George's prospective treatment study of anorexia nervosa: A discussion of methodological problems. International Journal of Eating Disorders 1989;8(4):445‐54. [Google Scholar]
Dare 2001 {published and unpublished data}
- Dare C, Eisler I, Russell G, Treasure J, Dodge L. Psychological therapies for adults with anorexia nervosa: Randomised controlled trial of out‐patient treatments. British Journal of Psychiatry 2001;178(3):216‐21. [DOI] [PubMed] [Google Scholar]
Eisler 2000 {published and unpublished data}
- Dare C, Chania E, Eisler I, Hodes M, Dodge E. The Eating Disorder Inventory as an instrument to explore change in adolescents in family therapy for anorexia nervosa. European Eating Disorders Review 2000;8(5):369‐83. [Google Scholar]
- Eisler I, Dare C, Hodes M, Russell G, Dodge E, Grange D. Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2000;41(6):727‐36. [PubMed] [Google Scholar]
- Eisler I, Simic M, Russell GF, Dare C. A randomised controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa; a five year follow‐up. Journal of Child Psychology and Psychiatry 2007;48(6):552‐60. [DOI] [PubMed] [Google Scholar]
Espina 2000 {published data only (unpublished sought but not used)}
- Espina A, Joaristi L, Ortego MA, Alda IO. Eating disorders, family interventions and changes in MMPI profiles. An exploratory study. Estudios de Psicologia 2003;24(3):359‐75. [Google Scholar]
- Espina EA, Ortego Saenz De Calderon MA, Ochoa De Alda Apellaniz I. A controlled trial of family interventions in eating disorders. Changes in psychopathology and social adjustment. Apuntes de Psicologia 2002;20(1):49‐62. [Google Scholar]
- Espina EA, Ortego Saenz de Cabezon MA, Ochoa de Alda Martinez de Apellaniz I. A controlled trial of family interventions in eating disorders [Un ensayo controlado de intervenciones familiares en trastornos alimetarios]. Anales de Psiquiatria 2000;16(8):322‐36. [Google Scholar]
Geist 2000 {published data only (unpublished sought but not used)}
- Geist R, Heinmaa M, Stephens D, Davis R, Katzman DK. Comparison of family therapy and family group psychoeducation in adolescents with anorexia nervosa. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie 2000;45(2):173‐8. [DOI] [PubMed] [Google Scholar]
Godart 2012 {published data only}
- Duclos J, Dorard G, Curt F, Godart N. Eighteen months predictive factors of anorexia nervosa (AN) outcome: Does the family emotional climate play a role?. 20th World Congress of the International Association for Child and Adolescent Psychiatry and Allied Professions, IACAPAP. Paris, France, 2012.
- Godart N, Berthoz S, Curt F, Perdereau F, Rein Z, Wallier J, et al. A randomized controlled trial of adjunctive family therapy and treatment as usual following inpatient treatment for anorexia nervosa adolescents. PloS One 2012;7(1):e28249. [ISRCTN71142875] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godart N, Radon L, Duclos J, Berthoz S, Perdereau F, Curt F, et al. Quantitative evaluation of the impact of family therapy: A randomized controlled trial comparison of adjunctive family therapy and treatment as usual following inpatient treatment for adolescent anorexia nervosa, a 13 years follow‐up months outcome. 16th International Congress of European Society for Child and Adolescent Psychiatry, ESCAP. Madrid, Spain, 2015.
Hall 1987 {published data only (unpublished sought but not used)}
- Hall A, Crisp AH. Brief psychotherapy in the treatment of anorexia nervosa. Outcome at one year. British Journal of Psychiatry 1987;151:185‐91. [DOI] [PubMed] [Google Scholar]
Herpertz‐Dahlmann 2014 {published data only}
- Herpertz‐Dahlmann B, Schwarte R, Krei M, Egberts K, Warnke A, Wewetzer C, et al. Day‐patient treatment after short inpatient care versus continued inpatient treatment in adolescents with anorexia nervosa (ANDI): a multicentre, randomised, open‐label, non‐inferiority trial. Lancet 2014;383(9924):1222‐9. [DOI] [PubMed] [Google Scholar]
Herscovici 2017 {published data only}
- Herscovici CR, Kovalskys I, Orellana L. An exploratory evaluation of the family meal intervention for adolescent anorexia nervosa. Family Process 2017;56(2):364‐75. [DOI] [PubMed] [Google Scholar]
Le Grange 1992 {published and unpublished data}
- Grange D, Eisler I, Dare C, Hodes M. Evaluation of family therapy in adolescent anorexia nervosa: A pilot study. International Journal of Eating Disorders 1992;12(4):347‐57. [Google Scholar]
Le Grange 2016 {published data only}
- ACTR 12610000216011. A randomised controlled trial of two forms of family‐based treatment and the effect on percent ideal body eeight and eating disorders symptoms in adolescent anorexia nervosa. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=335239 (first received 16 March 2010). [Trial ID ACTRN12610000216011]
- Allan E, Grange D, Sawyer S, McLean L, Hughes E. Parental expressed emotion during two forms of family‐based treatment for adolescent anorexia nervosa. European Eating Disorders Review 2018;26(1):46‐52. [DOI] [PubMed] [Google Scholar]
- Hughes EK, Grange D, Yeo MS, Campbell S, Allan E, Crosby RD, et al. Parent‐focused treatment for adolescent anorexia nervosa: a study protocol of a randomised controlled trial. BMC Psychiatry 2014;14:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes EK, Sawyer S, Court A, Yeo M, Grange D. 20th World Congress of the International Association for Child and Adolescent Psychiatry and Allied Professions. Paris, France, 2012.
- Grange D, Hughes EK, Court A, Yeo M, Crosby RD, Sawyer SM. Randomized clinical trial of parent‐focused treatment and family‐based treatment for adolescent anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry 2016;55(8):683‐92. [ACTRN12610000216011] [DOI] [PubMed] [Google Scholar]
- Murray SB, Pila E, Grange D, Sawyer SM, Hughes EK. Symptom trajectories throughout two family therapy treatments for adolescent anorexia nervosa. International Journal of Eating Disorders 2017;50(11):1323–7. [DOI] [PubMed] [Google Scholar]
Li 2006 {published data only}
- Li Y, Wang J, Ma J. A controlled clinical trial of citalopram and citalopram combined with family therapy in the treatment of anorexia nervosa. Shanghai Archives of Psychiatry 2006;18(3):158‐6. [Google Scholar]
Lock 2005 {published data only (unpublished sought but not used)}
- Grange D, Hoste RR, Lock J, Bryson SW. Parental expressed emotion of adolescents with anorexia nervosa: outcome in family‐based treatment. International Journal of Eating Disorders 2011;44(8):731‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HY, Lock J. Anorexia nervosa in Asian‐American adolescents: Do they differ from their non‐Asian peers. International Journal of Eating Disorders 2007;40(3):227‐31. [DOI] [PubMed] [Google Scholar]
- Lock J, Agras WS, Bryson S, Kraemer HC. A comparison of short‐ and long‐term family therapy for adolescent anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry 2005;44(7):632‐9. [DOI] [PubMed] [Google Scholar]
- Lock J, Couturier J, Agras WS. Comparison of long‐term outcomes in adolescents with anorexia nervosa treated with family therapy. Journal of the American Academy of Child and Adolescent Psychiatry 2006;45(6):666‐72. [DOI] [PubMed] [Google Scholar]
- Lock J, Couturier J, Bryson S, Agras S. Predictors of dropout and remission in family therapy for adolescent anorexia nervosa in a randomized clinical trial. International Journal of Eating Disorders 2006;39(8):639‐47. [DOI] [PubMed] [Google Scholar]
- Pereira T, Lock J, Oggins J. Role of therapeutic alliance in family therapy for adolescent anorexia nervosa. International Journal of Eating Disorders 2006;39(8):677‐84. [DOI] [PubMed] [Google Scholar]
- Utzinger L. Transdiagnostic response to family‐based treatment for eating disorders in adolescents: predictors of outcome. Dissertation Abstracts International: Section b: the Sciences and Engineering 2014; Vol. 74.
Lock 2010 {published data only}
- Accurso EC, Ciao AC, Fitzsimmons‐Craft EE, Lock JD, Grange D. Is weight gain really a catalyst for broader recovery?: The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behaviour Research and Therapy 2014;56:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accurso EC, Fitzsimmons‐Craft EE, Ciao AC, Grange D. From efficacy to effectiveness: Comparing outcomes for youth with anorexia nervosa treated in research trials versus clinical care. Behaviour Research and Therapy 2015;65:36‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownstone L, Anderson K, Beenhakker J, Lock J, Grange D. Recruitment and retention in an adolescent anorexia nervosa treatment trial. International Journal of Eating Disorders 2012;45(6):812‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne CE, Accurso EC, Arnow KD, Lock J, Grange D. An exploratory examination of patient and parental self‐efficacy as predictors of weight gain in adolescents with anorexia nervosa. International Journal of Eating Disorders 2015;48:883‐8. [DOI: 10.1002/eat.22376] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne CE, Kass AE, Accurso EC, Fischer S, O'Brien S, Goodyear A, et al. Overvaluation of shape and weight in adolescents with anorexia nervosa: does shape concern or weight concern matter more for treatment outcome?. Journal of Eating Disorders 2015;3(49):1‐5. [DOI 10.1186/s40337‐015‐0086‐7] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne CE, Wonderlich JA, Curby T, Fischer S, Lock J, Grange D. Using bivariate latent basis growth curve analysis to better understand treatment outcome in youth with anorexia nervosa. European Eating Disorders Review 2018;6(5):483‐8. [DOI] [PubMed] [Google Scholar]
- Ciao AC, Accurso EC, Fitzsimmons‐Craft EE, Lock J, Grange D. Family functioning in two treatments for adolescent anorexia nervosa. International Journal of Eating Disorders 2015;48(1):81‐90. [DOI: 10.1002/eat.22314] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciao AC, Accurso EC, Fitzsimmons‐Craft EE, Lock J, Grange D. Moderators and mediators of remission in family‐based treatment and adolescent focused therapy for anorexia nervosa. Behaviour Research and Therapy 2012;50(2):85‐92. [NCT00149786] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsberg S, Darcy A, Bryson SW, Arnow KD, Datta N, Grange D, et al. Psychological symptoms among parents of adolescents with anorexia nervosa: A descriptive examination of their presence and role in treatment outcome. Journal of Family Therapy 2015;39(4):514‐36. [DOI: 10.1111/1467-6427.12088] [DOI] [Google Scholar]
- Forsberg S, LoTempio E, Bryson S, Fitzpatrick KK, Grange D, Lock J. Parent–therapist alliance in family‐based treatment for adolescents with anorexia nervosa. European Eating Disorders Review 2014;22(1):53‐8. [DOI: 10.1002/erv.2242] [DOI] [PubMed] [Google Scholar]
- Grange D, Accurso EC, Lock J, Agras S, Bryson SW. Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. International Journal of Eating Disorders 2014;47(2):124‐9. [DOI: 10.1002/eat.22221] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grange D, Lock J, Accurso EC, Agras WS, Darcy A, Forsberg S, et al. Relapse from remission at two‐ to four‐year follow‐up in two treatments for adolescent anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry 2014;53(11):1162‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grange D, Lock J, Agras WS, Moye A, Bryson S, Jo B, et al. Moderators and mediators of remission in family‐based treatment and adolescent focused therapy for anorexia nervosa. Behaviour Research and Therapy 2012;50(2):85‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Grange D, Agras WS, Moye A, Bryson SW, Booil J. Randomized clinical trial comparing family‐based treatment with adolescent‐focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry 2010;67(10):1025‐32. [NCT00149786] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00149786. Treatment of adolescents with anorexia nervosa. ClinicalTrials.gov/show/NCT00149786 (first received 8 September 2005). [CRSREF 2855952]
- Rienecke RD, Accurso EC, Lock J, Grange D. Expressed emotion, family functioning, and treatment outcome for adolescents with anorexia nervosa. European Eating Disorders Review 2015;24:43‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles‐Shields C, Lock J, Le Grange, D. The effect of driven exercise on treatment outcomes for adolescents with anorexia and bulimia nervosa. International Journal of Eating Disorders 2015;48(4):392‐6. [DOI] [PubMed] [Google Scholar]
Lock 2015 {published data only}
- Lock J, Grange D, Agras WS, Fitzpatrick KK, Jo B, Accurso E, et al. Can adaptive treatment improve outcomes in family‐based therapy for adolescents with anorexia nervosa? Feasibility and treatment effects of a multi‐site treatment study. Behaviour Research and Therapy 2015;73:90‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Madden 2015 {published data only}
- Madden S, Miskovic‐Wheatley J, Wallis A, Kohn M, Lock J, Grange D, et al. A randomized controlled trial of in‐patient treatment for anorexia nervosa in medically unstable adolescents. Psychological Medicine 2015;45(2):415‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden S, Miskovic‐Wheatley J, Wallis A, Kohn M, Hay P, Touyz S. Early weight gain in family‐based treatment predicts greater weight gain and remission at the end of treatment and remission at 12‐month follow‐up in adolescent anorexia nervosa. International Journal of Eating Disorders 2015;48(7):919‐22. [DOI] [PubMed] [Google Scholar]
- Wallis A. Family Based Treatment for Young People with Severe Anorexia Nervosa: An Investigation of Outcome, Family Functioning and Relationship Change [thesis]. Sydney: University of Sydney, Faculty of Science, School of Psychology, 2017. [Google Scholar]
- Wallis A, Miskovic‐Wheatley J, Madden S, Rhodes P, Crosby RD, Cao L, et al. How does family functioning effect the outcome of family based treatment for adolescents with severe anorexia nervosa?. Journal of Eating Disorders 2017;5:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Onnis 2012 {published data only}
- Onnis L, Barbara E, Bernardini M, Caggese A, Giacomo S, Giambartolomei A, et al. Family relations and eating disorders. The effectiveness of an integrated approach in the treatment of anorexia and bulimia in teenagers: Results of a case‐control systemic research. Eating and Weight Disorders 2012;17(1):e36‐e48. [DOI] [PubMed] [Google Scholar]
Rausch Herscovici 2006 {published data only (unpublished sought but not used)}
- Rausch Herscovici C. Lunch session, weight gain and their interaction with the psychopathology of anorexia nervosa in adolescents. Vertex: Revista Argentina de Psiquiatria 2006;17(65):7‐15. [PubMed] [Google Scholar]
Rhodes 2008 {published data only}
- Rhodes P, Baillee A, Brown J, Madden S. Can parent‐to‐parent consultation improve the effectiveness of the Maudsley model of family‐based treatment for anorexia nervosa? A randomized control trial. Journal of Family Therapy 2008;30(1):96‐108. [Google Scholar]
- Rhodes P, Brown J, Madden S. The Maudsley model of family‐based treatment for anorexia nervosa: a qualitative evaluation of parent‐to‐parent consultation. Journal of Marital and Family Therapy 2009;35(2):181‐92. [DOI] [PubMed] [Google Scholar]
Robin 1999 {published and unpublished data}
- Robin AL. Behavioral family systems therapy for adolescents with anorexia nervosa. In: Kazdin, AE editor(s). Evidence‐based Psychotherapies for Children and Adolescents. New York: Guilford Press, 2003:358‐73. [Google Scholar]
- Robin AL, Siegel P. The limited effectiveness of short‐term therapy for anorexia nervosa. 155th Annual Meeting of the American Psychiatric Association; Philadelphia PA; 18‐23 May 2002. 2002:10C.
- Robin AL, Siegel PT, Koepke T, Moye AW, Tice S. Family therapy versus individual therapy for adolescent females with anorexia nervosa. Journal of Developmental and Behavioral Pediatrics 1994;15(2):111‐6. [PubMed] [Google Scholar]
- Robin AL, Siegel PT, Moye A. Family versus individual therapy for anorexia: Impact on family conflict. International Journal of Eating Disorders 1995;17(4):313‐22. [DOI] [PubMed] [Google Scholar]
- Robin AL, Siegel PT, Moye AW, Gilroy M, Dennis AB, Sikand A. A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry 1999;38(12):1482‐9. [DOI] [PubMed] [Google Scholar]
Russell 1987 {published and unpublished data}
- Dare C, Eisler I, Russell GF, Szmukler GI. The clinical and theoretical impact of a controlled trial of family therapy in anorexia nervosa. Journal of Marital and Family Therapy 1990;16(1):39‐57. [Google Scholar]
- Eisler I [pers comm]. Data sent for post‐intervention outcomes by subgroup [personal communication]. Letter to Caroline Fisher 13 October 2008.
- Eisler I, Dare C, Russell GF, Szmukler G, Grange D, Dodge E. Family and individual therapy in anorexia nervosa. A 5‐year follow‐up. Archives of General Psychiatry 1997;54(11):1025‐30. [DOI] [PubMed] [Google Scholar]
- Hewell K, Hoste RR, Grange D. Recruitment for an adolescent bulimia nervosa treatment study. International Journal of Eating Disorders 2006;39(7):594‐7. [DOI] [PubMed] [Google Scholar]
- Russell GF, Szmukler GI, Dare C, Eisler I. An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Archives of General Psychiatry 1987;44(12):1047‐56. [DOI] [PubMed] [Google Scholar]
- Szmukler GI, Dare C. The Maudsley study of family therapy in anorexia and bulimia nervosa. In: Blake D, Shekter‐Wolfson L editor(s). Family Approaches in Treatment of Eating Disorders. Washington, DC: American Psychiatric Press, 1991:1‐21. [Google Scholar]
Russell 1987a {published and unpublished data}
Russell 1987b {published data only}
Russell 1987c {published data only}
Whitney 2012 {published and unpublished data}
- Todd G, Gavan K, Murphy T. Family work in the treatment of patients with anorexia nervosa. 29th Annual Conference of the British Association for Behavioural and Cognitive Psychotherapies; 20‐23 June 2001, Glasgow UK. 2001.
- Whitney J, Murphy T, Landau S, Gavan K, Todd G, Whitaker W, et al. Exploratory RCT of family day workshops and individual family work as a supplement to inpatient care for anorexia nervosa. International Journal of Eating Disorders 2012;20(2):142‐50. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Attia 2012 {published data only}
- Attia E. In the Clinic. Eating disorders. Annals of Internal Medicine 2012;156(7):1‐16. [DOI] [PubMed] [Google Scholar]
Buddeberg 1979 {published data only}
- Buddeberg B, Buddeberg C. Family therapy of anorexia nervosa. Praxis der Kinderpsychologie und Kinderpsychiatrie 1979;28(2):37‐43. [PubMed] [Google Scholar]
Ciao 2015 {published data only}
- Ciao AC, Accurso EC, Fitzsimmons‐Craft EE, Grange D. Predictors and moderators of psychological changes during the treatment of adolescent bulimia nervosa. Behaviour Research and Therapy 2015;69:48‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dalle Grave 2010 {published data only}
- Dalle Grave R. Inpatient cognitive behavior therapy for severe eating disorders. Psychological Topics 2010;19(2):323‐40. [Google Scholar]
Fettes 1992 {published data only}
- Fettes PA, Peters JM. A meta‐analysis of group treatments for bulimia nervosa. International Journal of Eating Disorders 1992;11(2):97‐110. [Google Scholar]
George 1997 {published data only}
- George L. The psychological characteristics of patients suffering from anorexia nervosa and the nurse’s role in creating a therapeutic relationship. Journal of Advanced Nursing 1997;26:899‐908. [DOI] [PubMed] [Google Scholar]
Gilbert 2008 {published data only}
- Gilbert G. Inpatient treatment equals outpatient treatment for anorexia. Journal of the National Medical Association 2008;100(7):869‐70. [Google Scholar]
Goddard 2013 {published data only}
- Goddard E, Raenker S, Macdonald P, Todd G, Beecham J, Naumann U, et al. Carers' assessment, skills and information sharing: theoretical framework and trial protocol for a randomised controlled trial evaluating the efficacy of a complex intervention for carers of inpatients with anorexia nervosa. European Eating Disorders Review 2013;21(1):60‐71. [DOI] [PubMed] [Google Scholar]
- ISRCTN06149665. A randomised pragmatic trial comparing the cost effectiveness of supplementing standard care with an intervention for carers (Carers Assessment, Skills and Information Sharing [CASIS]) of people with eating disorders. www.isrctn.com/ISRCTN06149665 (first recieved 19 August 2008).
- Macdonald P, Rhind C, Hibbs R, Goddard E, Raenker S, Todd G, et al. Carers' assessment, skills and information sharing (CASIS) trial: A qualitative study of the experiential perspective of caregivers and patients. European Eating Disorders Review 2014;22(6):430‐8. [DOI] [PubMed] [Google Scholar]
- Macdonald P, Rhind C, Hibbs R, Goddard E, Raenker S, Todd G, et al. Carers' assessment, skills and information sharing: Theoretical framework and trial protocol for a randomised controlled trial evaluating the efficacy of a complex intervention for carers of inpatients with anorexia nervosa. European Eating Disorders Review 2013;21(1):60‐71. [DOI] [PubMed] [Google Scholar]
- Macdonald P, Rhind C, Hibbs R, Goddard E, Raenker S, Todd G, et al. Two‐year follow‐up of a pragmatic randomised controlled trial examining the effect of adding a carer's skill training intervention in inpatients with anorexia nervosa. European Eating Disorders Review 2015;24(2):122‐30. [DOI] [PubMed] [Google Scholar]
Gowers 2010 {published data only}
- Byford S, Barrett B, Roberts C, Clark A, Edwards V, Smethurst N, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. British Journal of Psychiatry 2007;191:436‐40. [DOI] [PubMed] [Google Scholar]
- Gowers S. Evidence based decision making in adolescent anorexia nervosa. 33rd Annual Conference of the British Association for Behavioural and Cognitive Psychotherapies, July 21‐23 2005, Canterbury UK. Canterbury, 2005:87.
- Gowers SG, Clark A, Robert C, Griffiths A, Edwards V, Bryan C, et al. Clinical effectiveness of treatments for anorexia nervosa in adolescents: randomised controlled trial. British Journal of Psychiatry 2009;191:427‐35. [DOI] [PubMed] [Google Scholar]
- Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al. A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost‐effectiveness and patient acceptability ‐ The TOuCAN trial. Health Technology Assessment 2010;14(15):1‐98. [DOI] [PubMed] [Google Scholar]
Karwautz 2015 {published data only}
- Karwautz A, Wagner G. Supporting carers of children and adolescents with eating disorders in Austria (SUCCEAT). clinicaltrials.gov/show/NCT02480907 (first received 25 June 2015).
Keshen 2013 {published data only}
- Keshen A. Effectiveness of the ECHOs Approach for Patients With Eating Disorders and Their Carers (ECHO). clinicaltrials.gov/show/NCT01927042 (first received 22 August 2013). [NCT01927042]
Le Grange 2005a {published data only}
- Grange D, Binford R, Loeb KL. Manualized family‐based treatment for anorexia nervosa: A case series. Journal of the American Academy of Child and Adolescent Psychiatry 2005;44(1):41‐6. [DOI] [PubMed] [Google Scholar]
Loeb 2007 {published data only}
- Loeb L, Walsh TB, Lock, J, Grange D, Jones, J, Marcus S, et al. Open trial of family‐based treatment for full and partial anorexia nervosa in adolescence: Evidence of successful dissemination. Journal of the American Academyof Child and Adolescent Psychiatry 2007;46(7):792‐800. [DOI] [PubMed] [Google Scholar]
- NCT00418977. Early identification and treatment of anorexia nervosa. ClinicalTrials.gov/show/NCT00418977 (first received 28 April 2014).
Perkins 2005 {published data only}
- Perkins S, Schmidt U, Eisler I, Treasure J, Yi I, Winn S, et al. Why do adolescents with bulimia nervosa choose not to involve their parents in treatment?. European Child and Adolescent Psychiatry 2005;14(7):376‐85. [DOI] [PubMed] [Google Scholar]
- Schmidt U, Lee S, Beecham J, Perkins S, Treasure J, Yi I, et al. A randomized controlled trial of family therapy and cognitive behavior therapy guided self‐care for adolescents with bulimia nervosa and related disorders. American Journal of Psychiatry 2007;164(4):591‐8. [DOI] [PubMed] [Google Scholar]
Reyes‐Rodriguez 2011 {published data only}
- Reyes‐Rodriguez ML. Engaging Latino families in eating disorders treatment (PAS). ClinicalTrials.gov/show/NCT01470508 (first received 11 November 2011).
Salbach 2006 {published data only}
- Salbach H, Bohnekamp I, Lehmkuhl U, Pfeiffer E, Korte A. Family‐oriented group therapy in the treatment of female patients with anorexia and bulimia nervosa ‐ a pilot study. Zeitschrift fur Kinder‐und Jugendpsychiatrie und Psychotherapie 2006;34:267‐74. [DOI] [PubMed] [Google Scholar]
Schmidt 2005 {published data only}
- Schmidt U. A pilot randomised controlled trial of the CD‐ROM based intervention for carers of people with anorexia nervosa (AN). www.isrctn.com/ISRCTN33652725 (first received 13 May 2005). [DOI: 10.1186/ISRCTN33652725] [DOI]
Schmidt 2013 {published data only}
- Schmidt U, Renwick B, Lose A, Kenyon M, DeJong H, Broadbent H, et al. The MOSAIC study ‐ comparison of the Maudsley Model of Treatment for Adults with Anorexia Nervosa (MANTRA) with Specialist Supportive Clinical Management (SSCM) in outpatients with anorexia nervosa or eating disorder not otherwise specified, anorexia nervosa type: Study protocol for a randomized controlled trial. Trials 2013; Vol. 14, issue 1:160. [DOI] [PMC free article] [PubMed]
Slagerman 1989 {published data only}
- Slagerman M, Yager J. Multiple family group treatment for eating disorders: A short term program. Psychiatric Medicine 1989;7(4):269‐83. [PubMed] [Google Scholar]
Spettigue 2015 {published data only}
- Spettigue W, Maras D, Obeid N, Henderson KA, Buchholz A, Gomez R, et al. A psycho‐education intervention for parents of adolescents with eating disorders: a randomized controlled trial. Eating Disorders 2015;23(1):60‐75. [DOI] [PubMed] [Google Scholar]
Treasure 2006 {published data only}
- Treasure J. Collaborative caring project: working with parents at treatment and secondary prevention of eating disorders. isrctn.com/ISRCTN56376745 (first received 4 October 2005). [DOI: 10.1186/ISRCTN56376745] [DOI]
Treasure 2007 {published data only}
- Treasure J, Sepulveda AR, Whitaker W, Todd G, Lopez C, Whitney J. Collaborative care between professionals and non‐professionals in the management of eating disorders: A description of workshops focused on interpersonal maintaining factors. European Eating Disorders Review 2007;15:24‐34. [DOI] [PubMed] [Google Scholar]
Vandereycken 1977 {published data only}
- Vandereycken W, Pierloot R. Anorexia nervosa: weight recovery with behaviour therapy. Feuillets Psychiatrique de Liege 1977;10:47‐58. [Google Scholar]
Vandereycken 1978 {published data only}
- Vandereycken W, Pieters G. Short‐term weight restoration in anorexia nervosa through operant conditioning. Scandinavian Journal of Behaviour Therapy 1978;7(4):221‐36. [Google Scholar]
Wallin 2000 {published data only}
- Wallin U, Kronovall P, Majewski M. Body awareness therapy in teenage anorexia nervosa: outcome after 2 years. European Eating Disorders Review 2000;8(1):19‐30. [Google Scholar]
Whitney 2012b {published data only}
- Whitney J, Currin L, Murray J, Treasure J. Family work in anorexia nervosa: A qualitative study of carers' experiences of two methods of family intervention. European Eating Disorders Review 2012;20(2):132‐41. [DOI] [PubMed] [Google Scholar]
Woidislawsky 1996 {published data only}
- Woidislawsky R. A comparison of two types of group psychotherapy for eating disordered daughters and their mothers. Dissertation Abstracts International 1996;56(9‐B):5192. [Google Scholar]
References to studies awaiting assessment
Bulik 2009 {published data only}
- Bulik C. UCAN: Uniting Couples in the Treatment of Anorexia Nervosa (UCAN). clinicaltrials.gov/ct2/show/NCT00928109 (first received 25 June 2009).
Dimitropoulos 2014 {published data only}
- Dimitropoulos G. Multi‐family group therapy for adult eating disorders (MFGT). clinicaltrials.gov/show/NCT02106728 (first received 8 April 2014).
Eisler 2006 {published data only}
- Eisler I. A multi‐centre randomised trial of the outcome, acceptability and cost‐effectiveness of family therapy and multi‐family day treatment compared with inpatient care and outpatient family therapy for adolescent anorexia nervosa. www.isrctn.com/ISRCTN11275465 (first received 5 April 2006).
- Eisler I, Simic M, Hodsoll J, Asen E, Berelowitz M, Connan F, et al. A pragmatic randomised multi‐centre trial of multifamily and single family therapy for adolescent anorexia nervosa. BMC Psychiatry 2016;16(1):422. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gore‐Rees 2001 {published data only}
- Gore‐Rees, P. A randomised controlled multicentre treatment of adolescent anorexia nervosa including assessment of cost and patient acceptability. National Research Register [Archived].
Jacobi 2012 {published data only}
- Jacobi C. Early detection and intervention of anorexia nervosa in adolescent girls: a randomized controlled trial comparing a family‐oriented, internet‐based intervention with a control group without intervention. www.isrctn.com/ISRCTN18614564 (first received 6 January 2012).
Le Grange 2005 {published data only}
- Grange D. Treatment for adolescent anorexia nervosa. clinicaltrials.gov/ct2/show/NCT00183586 (first received 16 September 2005). [NCT00183586]
Lock 2014 {published data only}
- Lock J. Feasibility of combining family and cognitive therapy to prevent chronic anorexia. clinicaltrials.gov/ct2/show/NCT02054364 (first received 4 February 2014).
- Lock J, Fitzpatrick KK, Agras WS, Weinbach N, Jo B. Feasibility study combining art therapy or cognitive remediation therapy with family‐based treatment for adolescent anorexia nervosa. European Eating Disorders Review 2018;26(1):62‐8. [DOI: 10.1002/erv.2571] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nevonen 2015 {published data only}
- Nevonen L. The Gothenburg anorexia nervosa treatment study. www.isrctn.com/ISRCTN25181390 (first received 21 July 2015).
Rugiu 1999 {published data only}
- Santoni Rugiu A, Giacomo P, Calo P, Giacomo A, Catucci A, Viola G. A comparison of family therapy and day hospital integrated treatment in anorexia and bulimia nervosa. Current Opinion in Psychiatry 1999;12(Suppl 1):335. [Google Scholar]
Zucker 2008 {published data only}
- Zucker NL. Group parent training for adolescent eating disorders (GPT‐AN). clinicaltrials.gov/ct2/show/NCT00672906 (first received 6 May 2008).
References to ongoing studies
Bilyk 2017 {published data only}
- Bilyk BF. Effectiveness of a cognitive behavioral management pilot program in a sample of Brazilian adolescents with anorexia vervosa [Efetividade de um programa piloto de tratamento cognitivo comportamental em uma amostra de adolescentes brasileiros com anorexia nervosa]. www.ensaiosclinicos.gov.br/rg/RBR‐4dpths/ (first received 14 September 2017). [Trial ID: U1111‐1202‐0493]
Bulik 2012 {published data only}
- Bulik C, Baucom D. UNCAN2: Enhancing treatment for adult anorexia with a couple‐based approach. clinicaltrials.gov/show/NCT01740752 (first received 4 December 2012).
Carrot 2017 {unpublished data only}
- Carrot B. Family therapy and anorexia nervosa : Which is the best approach? (THERAFAMBEST). clinicaltrials.gov/ct2/show/NCT03350594 (first received 22 November 2017).
Hildebrandt 2016 {unpublished data only}
- Hildebrandt T. Reward systems and food avoidance in eating disorders. clinicaltrials.gov/ct2/show/NCT02795455 (first received 10 June 2016).
Lock 2017 {unpublished data only}
- Lock JD. Adaptive treatment for adolescent anorexia nervosa. clinicaltrials.gov/ct2/show/NCT03097874 (first received 31 March 2017).
McCormack 2014 {published data only}
- McCormack J. Know and grow: An investigation into parent and family involvement in eating disorder treatment. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12614001296628 (first received 12 November 2014). [U1111‐1163‐9479]
Additional references
Achenbach 1991
- Achenbach T. Manual for the Youth Self‐Report and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry, 1991. [Google Scholar]
Angold 1995
- Angold A, Costello EJ, Messer SC, Pickles A. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research 1995;5(4):237‐249. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV). 4th Edition. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
APA 2013
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM‐5. 5th Edition. Washington, D.C.: American Psychiatric Association, 2013. [APA (2013); APA, 2013] [Google Scholar]
Beck 1961
- Beck AT, Warn CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561‐71. [DOI] [PubMed] [Google Scholar]
Berkman 2006
- Berkman ND, Bulik CM, Brownley KA, Lohr KN, Sedway JA, Rooks A, et al. Management of Eating Disorders. Evidence Report/Technology Assessment No. 135. (Prepared by the RTI International‐University of North Carolina Evidence‐Based Practice Center under Contract No. 290‐02‐0016.). Rockville, MD: Agency for Healthcare Research and Quality, 2006. [Google Scholar]
Berkman 2007
- Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: a systematic review of the literature. International Journal of Eating Disorders 2007;40(4):293‐309. [DOI] [PubMed] [Google Scholar]
Bryant‐Waugh 2000
- Bryant‐Waugh R. Overview of the eating disorders. In: Lask B, Bryant‐Waugh R editor(s). Anorexia nervosa and related eating disorders in childhood and adolescence. 2nd Edition. East Sussex, UK: Psychology Press, 2000:27–40. [Google Scholar]
Bulik 2007
- Bulik CM, Berkman ND, Brownley KA, Sedway JA, Lohr KN. Anorexia nervosa treatment: a systematic review of randomized controlled trials. International Journal of Eating Disorders 2007;40(4):310‐20. [DOI] [PubMed] [Google Scholar]
Carter 2011
- Carter FA, Jordan J, McIntosh VV, Luty SE, McKenzie JM, Frampton CM, et al. The long‐term efficacy of three psychotherapies for anorexia nervisa: A randomised controlled trial. International Journal of Eating Disorders 2011;44(7):647‐54. [DOI] [PubMed] [Google Scholar]
Cerniglia 2017
- Cerniglia L, Cimino S, Tafa M, Marzilli E, Ballarotto G, Bracaglia F. Family profiles in eating disorders: family functioning and psychopathology. Psychology Research and Behavior Management 2017;10:305‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Claudino 2006
- Claudino AM, Hay P, Lima MS, Bacaltchuk J, Schmidt U, Treasure J. Antidepressants for anorexia nervosa. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD004365.pub2] [DOI] [PubMed] [Google Scholar]
Cole 1988
- Cole JD, Kazarian SS. The level of expressed emotion scale: A new measure of expressed emotion. Journal of Clinical Psychology 1988;44:392‐7. [DOI] [PubMed] [Google Scholar]
Cooper 1987a
- Cooper PJ, Taylor MJ, Cooper Z, Fairburn CG. The development and validation of the Body Shape Questionniare. International Journal of Eating Disorders 1987; Vol. 6:485‐94.
Cooper 1987b
- Cooper Z, Fairburn CG. The Eating Disorders Examination: a semi‐structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders 1987; Vol. 6:1‐8.
Court 2008
Couturier 2013
- Couturier J, Kimber M, Szatmar P. Efficacy of family‐based treatment for adolescents with eating disorders: A systematic review and meta‐analysis. International Journal of Eating Disorders 2013;46(1):3‐11. [DOI] [PubMed] [Google Scholar]
Crown 1979
- Crown S, Crisp AH. Crown‐Crisp Experiential Index. London: Hodder and Stoughton, 1979. [Google Scholar]
Culbert 2015
- Culbert KM, Racine SE, Klump KL. Research Review: What we have learned about the causes of eating disorders – a synthesis of sociocultural, psychological, and biological research. The Journal of Child Psychology and Psychiatry 2015;56(11):1141‐64. [DOI] [PubMed] [Google Scholar]
Dare 1990
- Dare C, Eisler I, Russell GF, Szmukler GI. The clinical and theoretical impact of a controlled trial of family therapy in anorexia nervosa. Journal of Marital and Family Therapy 1990;16(1):39‐57. [Google Scholar]
Derogatis 1992
- Derogatis LR. SCL‐90‐R: Administration, Scoring & Procedures Manual‐II, for the R (Revised) Version and Other Instruments of the Psychopathology Rating Scale Series. 2nd Edition. Towson: Clinical Psychometric Research, Inc, 1992. [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7:177‐88. [DOI] [PubMed] [Google Scholar]
Eisler 1997
- Eisler I, Dare C, Russell GF, Szmukler G, Grange D, Dodge E. Family and individual therapy in anorexia nervosa. A 5‐year follow‐up. Archives of General Psychiatry 1997;54(11):1025‐30. [DOI] [PubMed] [Google Scholar]
Eisler 2005
- Eisler I. The empirical and theoretical base of family therapy and multiple family day therapy for adolescent anorexia nervosa. Journal of Family Therapy 2005;27:104‐31. [Google Scholar]
Eisler 2008
- Eisler I [pers comm]. Data sent for post‐intervention outcomes by subgroup. Letter to Caroline Fisher (sent 13 October 2008).
Fairburn 2003
- Fairburn CG, Harrison PJ. Eating disorders. Lancet 2003;361:407‐16. [DOI] [PubMed] [Google Scholar]
Fichter 2006
- Fichter MM, Quadflieg N, Hedlund S. Twelve‐year course and outcome predictors of anorexia nervosa. International Journal of Eating Disorders 2006;39(2):87‐100. [DOI] [PubMed] [Google Scholar]
Garner 1979
Garner 1982
- Garner DM, Bemis KM. A cognitive‐behavioral approach to anorexia nervosa. Cognitive Therapy and Research 1982;6:123‐50. [Google Scholar]
Garner 1983
- Garner DM, Olmstead MP, Polivy K. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders 1983; Vol. 2:15.
Garner 1991
- Garner DM. Eating Disorders Inventory‐2: Professional Manual. Odessa, FL: Psychological Assessment Resources, 1991. [Google Scholar]
Guyatt 1998
- Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS. Interpreting treatment effects in randomised trials. BMJ 1998;316(7132):690–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology Neurosurgery and Psychiatry 1960;23:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harris 1998
- Harris EC, Barraclough B. Excess mortality of mental disorder. British Journal of Psychiatry 1998;173:11‐53. [DOI] [PubMed] [Google Scholar]
Hay 2013
- Hay P. A systmatic review of evidence for psychological treatments in eating disorders: 2005–2012. International Journal of Eating Disorders 2013;46(5):462‐469. [DOI] [PubMed] [Google Scholar]
Hay 2015
- Hay P, Claudino A, Touyz S, Abd Elbaky G. Individual psychological therapy in the outpatient treatment of adults with anorexia nervosa. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD003909.pub2; CD003909. PMID 14583998] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heatherton 1991
- Heatherton TF, Polivy J. Development and validation of a scale for measuring state self‐esteem. Journal of Personality and Social Psychology 1991;60(6):895‐910. [Google Scholar]
Henderson 1987
- Henderson M, Freeman CPL. A Self‐rating Scale for Bulimia the ‘BITE’. The British Journal of Psychiatry 1987;150(1):18‐24. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2016
- Higgins JP, Lasserson T, Chandler J, Tovey D, Churchill R. Methodological Expectations of Cochrane Intervention Reviews. Cochrane: London 2016; Vol. Version 1.02.
Hodgson 1977
- Hodgson RJ, Rachman S. Obsessional‐compulsive complaints. Behavior Research and Therapy 1977;15(5):389‐395. [DOI] [PubMed] [Google Scholar]
Hudson 2007
- Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry 2007;61(3):348‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jeammet 1991
- Jeammet P, Brechon G, Payan C, Gorge A, Fermanian J. The outcome of anorexia nervosa: a prospective study of 129 patients evaluated at least 4 yearsafter their first admission. Psychiatrie de l'Enfant 1991;34(2):381–442. [PubMed] [Google Scholar]
Jewell 2016
- Jewell T, Collyer H, Gardner T, Tchanturia K, Simic M, Fonagy P, et al. Attachment and mentalization and their association with child and adolescent eating pathology: A systematic review. International Journal of Eating Disorders 2016;49(4):354‐73. [DOI] [PubMed] [Google Scholar]
Juni 2001
- Juni P, Altman DG, Egger M. Assessing the quality of controlled clinical trials. BMJ 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Katzman 2005
- Katzman DK. Medical complications in adolescents with anorexia nervosa: A review of the literature. International Journal of Eating Disorders 2005;37 Suppl:s52‐s59. [DOI] [PubMed] [Google Scholar]
Kaufman 1997
- Kaufman J, Birmhaher B, Brent D, Rao U, Flynn C, Morici P, et al. Schedule for affective disorders and schizophrenia for school‐age children‐present and lifetime version (KSADS‐PL: initial reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry 1997; Vol. 36, issue 7:980‐8. [DOI] [PubMed]
Kaye 2000
- Kaye WH, Klump KL, Frank GK, Strober M. Anorexia nervosa and bulimia. Annual Review of Medicine 2000;51:299–313. [DOI] [PubMed] [Google Scholar]
Keel 2008
- Keel PK, Haedt A. Evidence‐based psychosocial treatments for eating problems and eating disorders. Journal of Clinical Child and Adolescent Psychology 2008;37(1):39‐61. [DOI] [PubMed] [Google Scholar]
Kingston 1984
- Kingston W, Loader P. Eliciting whole‐family interaction with a standardized clinical interview. Journal of Family Therapy 1984;6(347‐363). [Google Scholar]
Kingston 1988
- Kingston W. The Family Health Scales for global assessment of family functioning. In: Keller PA, Heyman SR editor(s). Innovations in Clinical Practice: A Source Book. Sarasota, FL: Professional Resource Exchange Inc, 1988:299‐330. [Google Scholar]
Kinston 1984
- Kinston W, Loader P. Eliciting whole‐family interaction with a standardized clinical interview. Journal of Family Therapy 1984; Vol. 6:347‐63.
Kohn 2011
- Kohn M, Madden S, Clarke S. Refeeding in anorexia nervosa: increased safety and efficiency through understanding the pathophysiology of protein calorie malnutrition. Current Opinions in Pediatrics 2011;23:390–394. [DOI] [PubMed] [Google Scholar]
Kordy 2005
- Kordy H. Counting the COST: A European collaboration on the efficacy of psychotherapeutic treatment of patients with eating disorders. European Eating Disorders Review 2005;13:153‐158. [Google Scholar]
Kovacs 1992
- Kovacs M. The Children's Depression Inventory. North Tonawanda, New York: Mental Health Systems, 1992. [Google Scholar]
Le Grange 1999
- Grange D. Family therapy for adolescent anorexia nervosa. Journal of Clinical Psychology 1999;55:727‐40. [DOI] [PubMed] [Google Scholar]
Le Grange 2005b
- Grange D, Lock J. The dearth of psychological treatment studies for anorexia nervosa. International Journal of Eating Disorders 2005;37(2):79‐91. [DOI] [PubMed] [Google Scholar]
Le Grange 2010
- Grange D, Lock J, Loeb K, Nicholls D. Academy for Eating Disorders position paper: The role of the family in eating disorders. International Journal of Eating Disorders 2010;43(1):1‐5. [DOI] [PubMed] [Google Scholar]
Le Grange 2012
- Grange D, Lock J, Agras WS, Moye A, Bryson SW, Jo B, et al. Moderators and mediators of remission in family‐based treatment and adolescent focused therapy for anorexia nervosa. Behaviour Research and Therapy 2012;50(2):85‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Le Grange 2017
- Grange D, Robin AL. Family‐based treatment and behavioual family systems therapy for adolescent easting disorders. In: Weisz JR, Kazdin AE editor(s). Evidence‐Based Psychotherapies for Children and Adolescents. 3rd Edition. Guilford Publications, 2017:308‐24. [Google Scholar]
Leff 1985
- Leff J, Vaughn CE. Expressed Emotion in Families: Its Significance for Mental Illness. New York: Guilford Press, 1985. [Google Scholar]
Lock 2004
- Lock J, Grange D. Help Your Teenager Beat an Eating Disorder. New York, London: Guilford Publications, 2004. [Google Scholar]
Lock 2006
- Lock J, Couturier J, Agras WS. Comparison of long‐term outcomes in adolescents with anorexia nervosa treated with family therapy. Journal of the American Academy of Child and Adolescent Psychiatry 2006;45(6):666‐72. [DOI] [PubMed] [Google Scholar]
Lukoff 1986
- Lukoff D, Nuechterlein KH, Ventura J. Manual for expanded Brief Psychiatric Rating Scale. Schizophrenia Bulletin 1986;12:594–602. [Google Scholar]
Madanes 1981
- Madanes C. Strategic Family Therapy. San Francisco, CA: Jossey‐Bass, 1981. [Google Scholar]
McIntosh 2005
- McIntosh VV, Jordan J, Carter FA, Luty SE, McKenzie JM, Bulik CM, et al. Three psychotherapies for anorexia nervosa: a randomized, controlled trial. Am J Psychiatry. American Journal of Psychiatry 2005;162(4):741‐7. [DOI] [PubMed] [Google Scholar]
Miller‐Day 2006
- Miller‐Day M, Marks JD. Perceptions of communication orientation, perfectionism, and disordered eating behaviours of sons and daughters. Health Communication 2006;19(2):153‐163. [DOI] [PubMed] [Google Scholar]
Minuchin 1974
- Minuchin S. Families and Family Therapy. Cambridge, MA: Harvard University Press, 1974. [Google Scholar]
Minuchin 1975
- Minuchin S, Baker L, Rosman BL, Liebman R, Milman L, Todd TC. A conceptual model of psychosomatic illness: Family organization and family therapy. Archives of General Psychiatry 1975;32:1031‐8. [DOI] [PubMed] [Google Scholar]
Minuchin 1978
- Minuchin S, Rosman BL, Baker L. Psychosomatic families: Anorexia nervosa in context. Vol. viii, Oxford, England: Harvard University Press, 1978. [Google Scholar]
Moos 1994
- Moos R, Moos B. Family Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press, 1994. [Google Scholar]
Morgan 1975
- Morgan HG, Russell GF. Value of family background and clinical features as predictors of long‐term outcome in anorexia nervosa: four‐year follow‐up study of 41 patients. Psychological Medicine 1975;5(4):355‐71. [DOI] [PubMed] [Google Scholar]
Morgan 1988
Mustelin 2016
- Mustelin L, Silén Y, Raevuori A, Hoek HW, Kaprio J, Keski‐Rahkonen A. The DSM‐5 diagnostic criteria for anorexia nervosa may change its population prevalence and prognostic value. Journal of Psychiatric Research 2016;77:85‐91. [Mestelin 2016] [DOI] [PubMed] [Google Scholar]
NICE 2017
- National Institute for Health and Care Excellence. Eating disorders: recognition and treatment. www.nice.org.uk/guidance/ng69/resources/eating‐disorders‐recognition‐and‐treatment‐pdf‐1837582159813 (accessed 23 May 2017). [PubMed]
Olson 1979
Olson 1985
- Olson DH, Portner J, Lavee Y. FACES‐III. Minnesota: Family Social Science: University of Minnesota, 1985. [Google Scholar]
Pingani 2012
- Pingani L, Catellani S, Arnone F, Bernardis E, Vinci V, Ziosi G, et al. Predictors of dropout from in‐patient treatment of eating disorders:An Italian experience. Eating and Weight Disorders 2012;17(4):290‐7. [DOI] [PubMed] [Google Scholar]
Prinz 1978
- Prinz RJ, Kent RN. Recording parent‐adolescent interactions without the use of frequency or interval by interval coding. Behavior Therapy 1978;9(602‐604). [Google Scholar]
Robin 1989
- Robin AL, Foster SL. Negotiating Parent‐Adolescent Conflict: A Behavioural‐Family Systems Approach. New York: Guilford, 1989. [Google Scholar]
Robin 1990
- Robin AL, Koepke T, Moye A. Multidimensional assessment of parent‐adolescent relations. Psychological Assessment: Journal of Consulting and Clinical Psychology 1990; Vol. 2:451‐9.
Robin 1994
- Robin AL, Siegel PT, Koepke T, Moye AW, Tice S. Family therapy versus individual therapy for adolescent females with anorexia nervosa. Journal of Development and Behavioral Pediatrics 1994;15(2):111‐6. [PubMed] [Google Scholar]
Robin 1995
- Robin AL, Siegel PT, Moye A. Family versus individual therapy for anorexia: impact on family conflict. International Journal of Eating Disorders 1995;17(4):313‐22. [DOI] [PubMed] [Google Scholar]
Rosenberg 1965
- Rosenberg M. Society and the adolescent self‐image. Princeton, NJ: Princeton University Press, 1965. [Google Scholar]
Sawyer 2018
- Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child and Adolescent Health 2018;2(3):223‐8. [DOI] [PubMed] [Google Scholar]
Selvini 1978
- Selvini Palazzoli M, Boscolo L, Cecchin G, Prata G. Paradox and Counterparadox. New York: Aronson, 1978. [Google Scholar]
Simic 2018
- Simic M, Eisler I. Maudsley Family Therapy for Eating Disorders. In: Lebow J, Chambers A, Breunlin D editor(s). Encyclopedia of Couple and Family Therapy. Switzerland: Springer, Cham, 2018. [online ISBN 978‐3‐319‐15877‐8; print ISBN 978‐3‐319‐49423‐4; print and eBook ISBN 978‐3‐319‐49424‐1] [Google Scholar]
Skinner 1991
- Skinner HA, Steinhauer PD, Santa‐Barbara J. The Family Assessment Measure. Toronto: Multi‐Health Systems, 1991. [Google Scholar]
Smink 2014
- Smink R, Hoeken D, Oldehinkel AJ, Hoek HW. Prevalence and severity of DSM‐5 eating disorders in a community cohort of adolescents. International Journal of Eating Disorders 2014;47(6):610‐9. [DOI] [PubMed] [Google Scholar]
Soenens 2008
- Soenens B, Vansteenkiste M, Vandereycken W, Luyten P, Sierens E, Goossens L. Perceived parental psychological control and eating‐disordered symptoms: Maladaptive perfectionism as a possible intervening variable. Journal of Nervous and Mental Disease 2008;196(2):144‐52. [DOI] [PubMed] [Google Scholar]
Speilberger 1970
- Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State‐Trait Anxiety Inventory.. Palo Alto: Consulting Psychologists Press, 1970. [Google Scholar]
Sullivan 1995
- Sullivan PF. Mortality in anorexia nervosa. American Journal of Psychiatry 1995;152(7):1073‐4. [DOI] [PubMed] [Google Scholar]
Sunday 1995
Tolkien II Team 2006
- Tolkien II Team. A Needs‐Based, Costed, Stepped Care Model for Mental Health Services. Sydney: World Health Organization Collaborating Centre for Classification in Mental Health. Competitive Edge Graphics, 2006. [Google Scholar]
Touyz 2013
- Touyz S, Grange D, Lacey H, Hay P, Smith R, Maguire S, et al. Treating severe and enduring anorexia nervosa: A randomized controlled trial. Psychological Medicine 2013;43(12):2502‐11. [DOI] [PubMed] [Google Scholar]
Touyz 2015
- Touyz S, Grange D, Lacey H, Hay P, Smith R, Maguire S, et al. Treating severe and enduring anorexia nervosa: a randomized controlled trial. European Psychiatry 2015;30:357. [DOI] [PubMed] [Google Scholar]
Vandereycken 1992
Vaughn 1976
Wade 2000
- Wade TD, Bulik CM, Neale M, Kendler KS. Anorexia nervosa and major depression: shared genetic and environmental risk factors. American Journal of Psychiatry 2000;157(3):469‐71. [DOI] [PubMed] [Google Scholar]
Weissman 1976
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self‐report. Archives of General Psychiatry 1976;33(9):1111‐1115. [DOI] [PubMed] [Google Scholar]
Welner 1987
- Welner Z, Reich W, Herjanic B, Jung KG, Amado H. Reliability, validity, and parent‐child agreement studies of the Diagnostic Interview for Children and Adolescents (DICA). Journal of the American Academy of Child & Adolescent Psychiatry 1987;26(5):649‐653. [DOI] [PubMed] [Google Scholar]
Whitney 2005
- Whitney J, Eisler I. Theoretical and empirical models around caring for someone with an eating disorder: the reorganisation of family life and inter‐personal maintenance factors. Journal of Mental Health 2005;6:575‐85. [Google Scholar]
WHO 1992
- World Health Organization. The 10th Revision of the International Classification of Diseases and Related Health Problems (ICD‐10); www.who.int/classifications/apps/icd/icd10online/. World Health Organization, 1992. [Google Scholar]
Zipfel 2003
- Zipfel S, Lowe B, Herzog W. Medical complications. In: Treasure J, Schmidt U editor(s). Handbook of Eating Disorders. Chichester, UK: John Wiley & Sons Ltd, 2003:191‐206. [Google Scholar]
Zung 1971
- Zung WW. A rating instrument for anxiety disorders. Psychosomatics 1971;12(6):371‐379. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Fisher 2008
- Fisher CA, Rushford N, Hetrick SE. Family therapy for anorexia nervosa. Cochrane Database of Systematic Reviews 2008, Issue 2008. [DOI: 10.1002/14651858.CD004780] [DOI] [PubMed] [Google Scholar]
Fisher 2010
- Fisher CA, Hetrick SE, Rushford N. Family Therapy for Anorexica Nervosa. Cochrane Database of Systematic Reviews 2010, Issue 6. [DOI: 10.1002/14651858.CD004780.pub2] [DOI] [PubMed] [Google Scholar]
Fisher 2018
- Fisher CA, Skocic S, Rutherford KA, Hetrick SE. Family therapy approaches for anorexia nervosa. Cochrane Database of Systematic Reviews 2018, Issue 10. [DOI: 10.1002/14651858.CD004780.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]


