Abstract
Background
Currently, cardiovascular disease (CVD) is widely acknowledged to be the first leading cause of fatality in the world with 31% of all deaths worldwide and is predicted to remain as such in 2030. Furthermore, CVD is also a major cause of morbidity in adults worldwide. Among these diseases, the coronary artery disease (CAD) is the most common cause, accounting for over 40% of CVD deaths. Despite a decline in mortality rates, the consequences of more effective preventive and management programs, the burden of CAD remains significant. Indeed, the rise in the prevalence of modifiable risk factors due to changes in lifestyle and health behaviors has further increased the burden of this epidemic. Our objective was to evaluate the hospital burden of CAD via MI trends and Percutaneous Coronary Intervention (PCI) in the French Prospective Payment System (PPS).
Methods
MI/PCI were identified in the national PPS database from 2009 to 2014 for patients aged 20 to 99, living in metropolitan France. We examined hospitalisation, readmission and mortality trends using standardised rates.
Results
Over the six-year period, we identified 678,021 patients, representing 900,121 stays of which, 215,224 had a MI and a PCI. Admission trends increased by nearly 25%. Acute MI cases increased every year, with an alarming increase in women, and more specifically in young women. Men were 3 times more hospitalised than women, who were older. A North-South divide was noted. Twenty seven percent of patients experienced readmission within 1 month. Trajectories of care were significantly different by sex and age. Overall in-hospital death was 3.3%, decreasing by 15% during the period. The highest adjusted mortality rates were observed for inpatients aged <40 or >80.
Conclusion
We outlined the public health burden of this condition and the importance of improving the trajectories of care as an aid for better care.
Introduction
Around the world, cardiovascular disease (CVD) is recognized as the leading cause of death (accounting for approximately 31% of all deaths worldwide) and is predicted to remain as such in 2030 [1]. Moreover, this is reinforced with by the World Health Organization (WHO), which forecasts an 11% increase in the burden of CVD by 2030, bringing the worldwide number of myocardial infarctions (MI) and stroke to approximately 36.2 million [2]. In addition, CVD was also a major cause of morbidity in adults worldwide during the 20th century. Today, people with MI have a risk of recurrence and/or development of coronary heart disease-related conditions six times higher than those with no history of MI [3]. Among these diseases, the coronary artery disease (CAD) is the most common cause, accounting for more than 40% of CVD deaths (Source WHO). Despite improvements in care, CAD remain among the top causes of disease, disability and death worldwide leading to a high consumption of health resources [4].
In France, in 2012, the crude hospitalization rates for ischaemic heart disease, acute coronary syndromes and MI were 33.9, 18.8 and 9.4 per 104, respectively [5]. In 2011, standardized mortality rates in ischaemic heart disease were evaluated at 4.8 per 104 [5]. Local and regional or even national analyses from register data, like WHO-MONICA Project, highlighted a decline of these rates in the ten last years [6–9]. However, they also showed a societal change placing women on equal terms with men for risk of MI occurrence and mortality. In parallel, a study related to the economical burden of MI after a first episode underlined that the cost of health care following a MI, has been multiplied by three over the last decade [10].
As MI treatment is performed in a health facility, it is possible to trace the patient pathways through the national hospital Prospective Payment System (PPS), using comprehensive hospital databases, regularly collected for billing purposes. Although these data are sometimes criticised due to inaccuracy and lack of completeness [11, 12], they are increasingly used for epidemiological studies [13]. Moreover, in France, the gradual increase in fee-for-service has enhanced the coding quality [14]. Our objective was to evaluate the hospital burden of CAD through the MI, Percutaneous Coronary Interventions (PCI), and other ischaemic heart diseases (OIHD) annual trends as well as the related costs using the French PPS data over a six-year period.
Materials and methods
Materials
The Agence Technique de l’Information Sur l’Hospitalisation (ATIH) waived the need for consent according to the Enforcement (decree No. 94-666). Since 1996, all French hospitals caring for medical and surgical patients have submitted anonymized patient data to the French Hospital Discharge Database (FHDD). Each discharge summary submitted to the FHDD is linked to a national grouping algorithm leading to a French diagnosis related group [15]; thereby allowing patient comorbidities to be recorded and linked [16]. The study was conducted according to the approval given by the ATIH. Authorization was also obtained from the Commission Nationale de l’Informatique et des Libertés (agreement No. 1375062). The data provided were de-identified.
MI/PCI case identification algorithm in the FHDD
Usually, authors identify acute ischaemic heart events by the principal discharge diagnosis code of acute coronary syndrome using the International Classification of Diseases Tenth Revision (ICD-10) codes [17–20]. The sensitivity has been evaluated to be around 76% [21]. We added criterion based on Percutaneous Coronary Intervention (PCI) (see S1 Table). The list of ICD-10 codes as well as those of the French Common Classification of Medical Procedures (CCMP) [22] used to detect a MI are referenced in S1 Table. The international definition of MI is based on the elevation of troponin, but there is no straightforward translation of the definition into ICD-10 codes. ST-elevation MI (STEMI) is the default for unspecified term “acute MI” (AMI) and Non-ST-elevation MI (NSTEMI) requires more documentation such as the procedures peformed. Thus, ICD-10 codes are insufficient to distinguish the type of MI (STEMI or NSTEMI) [23]. Consequently, we will differentiate AMI coded by I21, which corresponds to the acute type 1 MI (Q-wave, STEMI, NSTEMI) versus the other ischaemic heart diseases (OIHD), I22 to I24 ICD-10 codes, and the PCIs as well, presented in S1 Table.
Inclusion criteria
We used the identification algorithm described above to select hospital stays between March 1, 2009, and December 31, 2014, in metropolitan France for all patients aged 20 to 99, and living in metropolitan France. Datamanagement was performed to validate that hospital stays were consistent particularly in terms of gender, age and death.
Non-inclusion criteria
We did not include patients aged < 20, patients living in French overseas territories and ACS occurring during a hospital stay.
Statistical analysis
We analysed the data according to first admission during the observation period, as well as hospitalisations, readmissions and in-hospital deaths by type of condition. We compared the AMI, OIHD and PCI only groups, as well as the AMI and non-AMI groups (combining OIHD and PCI only). In some cases, we also presented the results in the general case (MI/PCI) without distinguishing between groups.
Primary and associated diagnoses
We assessed incident cases according to the first diagnosis (AMI, OIHD, or PCI only) through the study period from 2010 to 2014. We calculated the global variation rate over the study period by taking into account every annual variation rate. We considered data according to sex. We estimated the average population as of 1st January of each year from data provided by the National Institute for Statistics and Economic Studies (https://www.insee.fr/fr/information/2008354). We then assessed standardised rates on age and sex using the direct standardisation method. The structure of the French metropolitan population of the current year was the reference. We analysed the health of the studied population by investigating their hospitalisation history and related diagnoses based on criteria used in Elixhauser score [24].
Burden and trends of MI/PCI hospitalisations
Specific annual hospitalisation rates were determined by reporting the number of hospitalisations in a given year to the average population by age group and sex for the same year. We assessed standardised rates with the same method as described above. Rates were examined by departments. We compared length of stays according to demographic and diagnosis criteria. The evolution of economic burden was estimated by calculating the hospitalisation costs based on the tariffs provided by the Ministry of Health. We used the Chi-squared test, Student test or ANOVA, as appropriate, to look for between-group statistical differences.
Since our objective was to evaluate the health care burden associated with MI/PCI, in this report the statistical unit was the stay, and we took into account all stays without distinguishing first episode from recurrences.
Burden and trends of MI/PCI readmissions
We considered readmission for an MI diagnosis or a PCI (see S1 Table). Readmission rates following an initial event (MI or PCI) were analysed using a Kaplan-Meier model according to demographic characteristics. Subgroups were compared with a log-rank test. We estimated duration until readmission. We performed the analysis of the principal diagnosis sequences in order to describe the care pathways and compare difference between groups with the Levene test [25].
Burden of in-hospital mortality
We reported the numbers of in-hospital deaths and estimated the mortality rates (gross and standardised) by age and sex, in relationship with the target population. Since the cause of death is not known from these data, this analysis was done in the general MI/PCI case without distinguishing the AMI and non-AMI groups.
All analyses were performed using R software [26] and Microsoft SQL Server Management Studio, version 10.0.1600.22.
Results
We identified 900,121 stays representing 678,021 patients with MI during the study period. Nearly 45% of patients presented with AMI and 7% were OIHD. The remaining 48% of patients, they had a PCI (S1 Fig). Angioplasty was performed in 72% of AMI and 60% OIHD patients, respectively.
Primary and associated diagnoses
Incidence case
Table 1 present the evolution of incident cases from 2010 to 2014. The distribution of incident cases by type of principal diagnosis showed an increase in AMI between 2010 and 2014 for both men and women. In contrast, the number of incident cases decreased for OIHD. About seventy percent of incident AMI cases and eighty percent of incident PCI cases were men.
Table 1. Annual incident numbers and standardised rates of hospitalised patients from 2010 to 2014 in metropolitan France for the first admission with the overall rate evolution.
AMI: Acute Myocardial Infarction (ICD-10 code: I21)—OIHD: Other Ischaemic Heart Diseases (ICD-10 codes: I22 to I24)—PCI only i.e without AMI or OIHD.
| 2010 | 2011 | 2012 | 2013 | 2014 | Global rate (%) |
|
|---|---|---|---|---|---|---|
| Number of patients* | ||||||
| AMI | ||||||
| Men | 34,557 | 34,672 | 36,451 | 37,053 | 37,881 | 9.6 |
| Women | 16,358 | 16,238 | 16,640 | 16,408 | 17,086 | 4.5 |
| OIHD | ||||||
| Men | 5,813 | 6,393 | 5,734 | 5,618 | 5,074 | -12.7 |
| Women | 2,278 | 2,414 | 2,191 | 2,040 | 1,923 | -15.5 |
| PCI only | ||||||
| Men | 51,135 | 49,466 | 51,095 | 51,410 | 54,636 | 6.8 |
| Women | 15,569 | 15,439 | 15,969 | 15,907 | 17,162 | 10.2 |
| Global | 115,570 | 113,043 | 115,223 | 114,270 | 118,418 | 2.4 |
| Incident hospitalisation standardised rates* (per 104) | ||||||
| AMI | ||||||
| Men | 15.3 | 15.3 | 16.0 | 16.2 | 16.4 | 7.1 |
| Women | 6.6 | 6.5 | 6.6 | 6.5 | 6.7 | 1.5 |
| OIHD | ||||||
| Men | 2.6 | 2.8 | 2.5 | 2.5 | 2.2 | -15.4 |
| Women | 0.9 | 0.1 | 0.9 | 0.8 | 0.8 | -11.1 |
| PCI only | ||||||
| Men | 22.7 | 21.8 | 22.4 | 22.4 | 23.7 | 4.4 |
| Women | 6.3 | 6.2 | 6.4 | 6.3 | 6.8 | 7.8 |
| Global | 24.4 | 23.7 | 24.1 | 23.7 | 24.5 | 0.4 |
* First admission in French metropolitan population.
Related diagnoses
Hypertension, congestive heart failure and cardiac arrhythmia were among the most common comorbid conditions in both men and women. However, considering the age group, the most common comorbid condition was hypertension (see Table 2). We found high proportions in diabetes and obesity. There were significant proportions of diabetes and obesity. In addition, alcohol abuse affected about 7% of men up to 65 years old. Among the most common comorbidities included depression in women, weight loss and renal failure in the elderly, and solid tumor without metastasis in men >65 years old.
Table 2. Medical conditions of the population by sex and age group over 2009-2014.
| <45 years | 45-65 years | 65-85 years | >85 years | |||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | |
| Medical conditions | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Congestive heart failure | 6,041 (24.2) | 1,328 (26.0) | 65,006 (31.2) | 12,587 (30.1) | 102,816 (44.8) | 45,585 (44.9) | 18,568 (63.6) | 22,953 (78.7) |
| Cardiac arrhythmia | 3,534 (14.2) | 770 (15.1) | 36,270 (17.4) | 6,572 (15.7) | 81,434 (35.5) | 33,798 (33.3) | 16,320 (55.9) | 18,044 (61.8) |
| Valvular disease | 276 (1.1) | 102 (2.0) | 3,617 (1.7) | 866 (2.1) | 10,618 (4.6) | 4,990 (4.9) | 2,138 (7.3) | 2,151 (7.4) |
| Pulmonary circulation disorders | 217 (0.9) | 96 (1.9) | 3,383 (1.6) | 966 (2.3) | 9,698 (4.2) | 5,892 (5.8) | 2,277 (7.8) | 3,053 (10.5) |
| Peripheral vascular disorder | 2,131 (8.5) | 508 (10.0) | 34,069 (16.4) | 6,055 (14.5) | 56,336 (24.6) | 18,606 (18.3) | 7,154 (24.5) | 6,218 (21.3) |
| Hypertension (uncomplicated) | 6,134 (24.6) | 1,498 (29.4) | 100,056 (48.1) | 22,197 (53.1) | 154,307 (67.3) | 72,952 (71.8) | 20,547 (70.4) | 27,306 (93.6) |
| Hypertension (complicated) | 430 (1.7) | 132 (2.6) | 6,878 (3.3) | 1,818 (4.4) | 15,475 (6.7) | 8,512 (8.4) | 2,897 (9.9) | 4,048 (13.9) |
| Paralysis | 236 (1.0) | 71 (1.4) | 2,905 (1.4) | 623 (1.5) | 6,237 (2.7) | 3,010 (3.0) | 1,099 (3.8) | 1,562 (5.4) |
| Other neurologic disorders | 623 (2.5) | 192 (3.8) | 5,462 (2.6) | 1,260 (3.0) | 11,127 (4.9) | 5,342 (5.3) | 2,163 (7.4) | 2,703 (9.3) |
| Chronic pulmonary diseases | 852 (3.4) | 342 (6.7) | 16,915 (8.1) | 4,048 (9.7) | 31,998 (14.0) | 10,532 (10.4) | 4,580 (15.7) | 3,652 (12.5) |
| Diabetes | 1,786 (7.2) | 562 (11.0) | 36,196 (17.4) | 8,456 (20.2) | 58,751 (25.6) | 25,878 (25.5) | 5,631 (19.3) | 6,789 (23.3) |
| Hypothyroidism | 200 (0.8) | 225 (4.4) | 3,431 (1.7) | 3,460 (8.3) | 7,661 (3.3) | 12,335 (12.1) | 1,471 (5.0) | 4,309 (14.8) |
| Renal failure | 468 (1.9) | 143 (2.8) | 8,079 (3.9) | 1,929 (4.6) | 30,467 (13.3) | 12,762 (12.6) | 8,209 (28.1) | 8,015 (27.5) |
| Liver disease | 485 (1.9) | 101 (2.0) | 5,205 (2.5) | 935 (2.2) | 5,088 (2.2) | 1,895 (1.9) | 429 (1.5) | 438 (1.5) |
| Peptic ulcer disease (excluding bleeding) | 118 (0.5) | 18 (0.4) | 1,666 (0.8) | 322 (0.8) | 2,485 (1.1) | 1,058 (1.0) | 322 (1.1) | 303 (1.0) |
| AIDS/HIV infection | 189 (0.8) | 42 (0.8) | 1070 (0.5) | 114 (0.3) | 246 (0.1) | 27 (0.03) | 7 (0.02) | 1 (0.0) |
| Lymphoma | 89 (0.4) | 32 (0.6) | 884 (0.4) | 185 (0.4) | 1,986 (0.9) | 745 (0.7) | 273 (0.9) | 247 (0.9) |
| Metastatic cancer | 71 (0.3) | 52 (1.0) | 3,702 (1.8) | 895 (2.1) | 7,781 (3.4) | 2,492 (2.5) | 864 (3.0) | 641 (2.2) |
| Solid Tumor without metastasis | 223 (0.9) | 117 (2.3) | 10,394 (5.0) | 2,178 (5.2) | 27,014 (11.8) | 7,157 (7.0) | 3,884 (13.3) | 2,240 (7.7) |
| Rheumatoid arthritis/collagen vascular diseases | 155 (0.6) | 128 (2.5) | 1,796 (0.9) | 936 (2.2) | 3,318 (1.5) | 2,785 (2.7) | 432 (1.5) | 801 (2.7) |
| Coagulopathy | 327 (1.3) | 152 (3.0) | 3,367 (1.6) | 732 (1.8) | 7,711 (3.4) | 2,782 (2.7) | 1,352 (4.6) | 1,209 (4.1) |
| Obesity | 4,636 (18.6) | 1,169 (23.0) | 42,342 (20.3) | 10,415 (24.9) | 41,686 (18.2) | 20,289 (20.0) | 2,279 (7.8) | 2,995 (10.3) |
| Weight loss | 340 (1.4) | 142 (2.9) | 5,402 (2.6) | 1,371 (3.3) | 16,077 (7.0) | 9,944 (9.8) | 5,079 (17.4) | 8,382 (28.7) |
| Fluid and electrolyte disorders | 805 (3.2) | 269 (5.3) | 9,469 (4.6) | 2,540 (6.1) | 22,455 (9.8) | 13,381 (13.2) | 5,624 (19.3) | 8,517 (29.2) |
| Blood loss anemia | 106 (0.4) | 103 (2.0) | 2,110 (1.0) | 698 (1.7) | 6,280 (2.7) | 3,544 (3.5) | 1,346 (4.6) | 1,861 (6.4) |
| Deficiency anemia | 210 (0.8) | 221 (4.3) | 3,710 (1.8) | 1,531 (3.7) | 11,280 (4.9) | 7,599 (7.5) | 2,629 (9.0) | 4,048 (13.9) |
| Alcohol abuse | 1,909 (7.7) | 242 (4.7) | 15,115 (7.3) | 1,707 (4.1) | 8,375 (3.7) | 1,393 (1.4) | 397 (1.4) | 164 (0.6) |
| Drug abuse | 918 (3.7) | 103 (2.0) | 1,092 (0.5) | 174 (0.4) | 261 (0.1) | 171 (0.2) | 32 (0.1) | 53 (0.2) |
| Psychoses | 239 (1.0) | 30 (0.6) | 1,011 (0.5) | 280 (0.7) | 834 (0.4) | 739 (0.7) | 125 (0.4) | 269 (0.9) |
| Depression | 1,013 (4.1) | 474 (9.3) | 7,853 (3.8) | 3,840 (9.2) | 8,576 (3.7) | 9,478 (9.3) | 1,814 (6.2) | 4,214 (14.4) |
On average, comorbid conditions were more frequent in women (3.5) than in men (3.0). Moreover, 11.5% of men (vs 7% of women) did not have comorbidity. Patients having more than 4 comorbidities were 34% in men and 43% in women. The more the patient is older the more comorbid conditions he has (on average 1.7 for the <45 years old versus 4.1 for the >85 years old). Of note, 27% and 3.5% of the <45 years old and the >85 years old, respectively did not have comorbidity. More than half of the <45 years old had more than 4 related diagnoses compared to the <45 years old.
Burden and trends of MI/PCI hospitalisations
Annual numbers
Table 1 shows that, on average, women were older than men. The variation rate between 2009 and 2014 displayed an increase in the average age in men and, conversely, a decrease in women.
The hospitalisation trends from 2009 to 2014 grew steadily with a sharp increase between 2009 and 2010. Table 3 indicates annual numbers and rates by sex. From 2009 to 2014, between 120,000 and 169,000 annual hospitalisations for MI/PCI were recorded, representing between 101,000 and 140,000 patients per year. Around two-thirds of hospitalisations were in public hospitals. The distribution of stays by type of principal diagnosis showed an increase in AMI between 2009 and 2014 for both men and women. In contrast, the number of stays decreased for OIHD.
Table 3. Annual numbers and standardised rates of hospitalised patients from 2009 to 2014 in metropolitan France.
AMI: Acute Myocardial Infarction (ICD-10 code: I21)—OIHD: Other Ischaemic Heart Diseases (ICD-10 codes: I22 to I24)—PCI only i.e without AMI or OIHD.
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Global rate(%) |
|
|---|---|---|---|---|---|---|---|
| Number of patients | |||||||
| AMI | |||||||
| Men | 28,628 | 35,096 | 35,432 | 37,624 | 38,509 | 39 643 | 38.6 |
| Women | 13,493 | 16,587 | 16,613 | 17,113 | 17,030 | 17,791 | 31.9 |
| OIHD | |||||||
| Men | 5,645 | 5,955 | 6,644 | 6,027 | 5,960 | 5,410 | -4.1 |
| Women | 2,273 | 2,325 | 2,473 | 2,266 | 2,114 | 1,994 | -12.2 |
| PCI only | |||||||
| Men | 44,102 | 54,209 | 54,361 | 57,493 | 59,097 | 64,286 | 45.9 |
| Women | 13,548 | 16,378 | 16,666 | 17,573 | 17,866 | 19,591 | 44.7 |
| Global | 101,497 | 122,688 | 124,002 | 129,552 | 131,623 | 139,286 | 37.3 |
| Mean age | |||||||
| AMI | |||||||
| Men | 64.1 | 63.9 | 63.9 | 63.9 | 64.0 | 64.1 | -0.1 |
| Women | 74.5 | 74.6 | 74.2 | 74.2 | 73.9 | 73.9 | -0.9 |
| OIHD | |||||||
| Men | 66.0 | 66.0 | 66.0 | 66.4 | 66.4 | 66.8 | 1.4 |
| Women | 72.9 | 73.4 | 72.5 | 72.7 | 72.9 | 73.1 | 0.5 |
| PCI only | |||||||
| Men | 65.7 | 65.8 | 66.0 | 66.1 | 66.3 | 66.6 | 1.3 |
| Women | 71.3 | 71.7 | 71.5 | 71.7 | 71.7 | 71.9 | 0.7 |
| Global | 67.3 | 67.4 | 67.3 | 67.4 | 67.5 | 67.8 | 0.6 |
| Number of stays | |||||||
| AMI | |||||||
| Men | 33,585 | 41,072 | 41,095 | 43,352 | 44,209 | 45,585 | 35.8 |
| Women | 15,601 | 19,175 | 19,009 | 19,556 | 19,441 | 20,337 | 30.6 |
| OIHD | |||||||
| Men | 6,129 | 6,358 | 7,177 | 6,494 | 6,580 | 5,886 | -3.9 |
| Women | 2,402 | 2,430 | 2,609 | 2,372 | 2,258 | 2,140 | -10.8 |
| PCI only | |||||||
| Men | 48,497 | 60,352 | 60,752 | 64,664 | 66,632 | 72,476 | 49.4 |
| Women | 10,144 | 11,767 | 13,234 | 12,924 | 13,181 | 14,653 | 47.1 |
| Global | 120,960 | 147,407 | 148,929 | 155,810 | 158,863 | 168,152 | 39 |
| Hospitalisation standardised rates* (per 104) | |||||||
| AMI | |||||||
| Men | 15.0 | 18.2 | 18.1 | 19.0 | 19.3 | 19.8 | 32.1 |
| Women | 6.3 | 7.7 | 7.6 | 7.8 | 7.7 | 8.0 | 26.9 |
| OIHD | |||||||
| Men | 2.7 | 2.8 | 3.2 | 2.9 | 2.9 | 2.6 | -3.7 |
| Women | 1.0 | 1.0 | 1.0 | 0.9 | 0.9 | 0.8 | -20 |
| PCI only | |||||||
| Men | 21.7 | 26.8 | 26.8 | 28.4 | 29.1 | 31.5 | 45.2 |
| Women | 6.0 | 7.3 | 7.3 | 7.7 | 7.8 | 8.6 | 43.5 |
| Global | 25.7 | 31.1 | 31.3 | 32.5 | 33 | 34.7 | 35.4 |
* French metropolitan population.
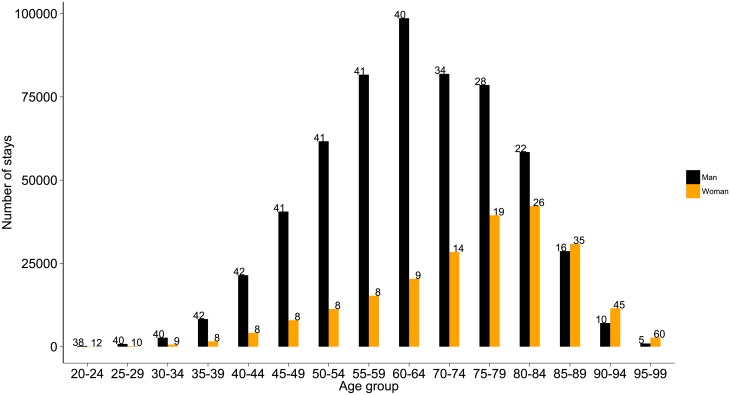
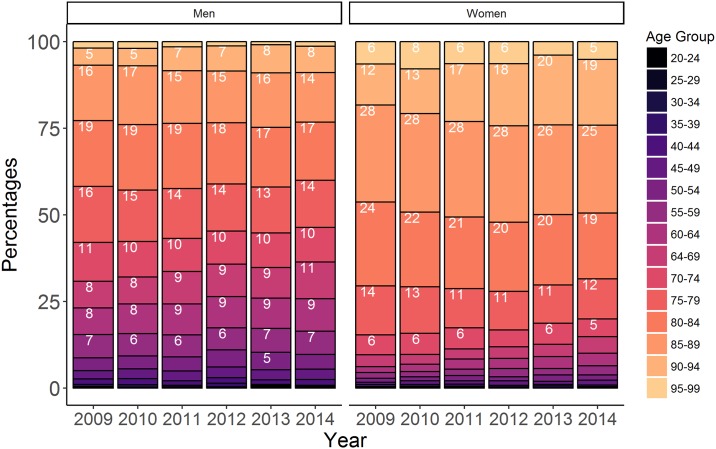
When all ages were combined, men’s stays accounted for about three-quarters of all hospitalisations; the sex distribution differed across age groups (see Fig 1). Among the 25-64 year group, hospitalisations occurred 4.5 times more frequently in men than in women. For the 80-84 year old patients, the differences according to sex were lower: 26% in women and 22% in men. From the age of 85, hospital stays for MI/PCI were more common in women than in men.
Fig 1. Distribution of hospital stays by sex and age group.
Numbers indicate the standardised percentages.
Standardised rates by sex and age
As reported in Table 3, overall hospitalisation rates were significantly different (p < 2.2e-16) according to sex (39.4 per 104 men and 13.3 per 104 women). The AMI trend grew over the study period: 15 per 104 in 2009 to 19.8 per 104 in 2014 for men and 6.3 per 104 to 8 per 104 for women. The average rate over the entire study period was 23.7 per 104 inhabitants per year.
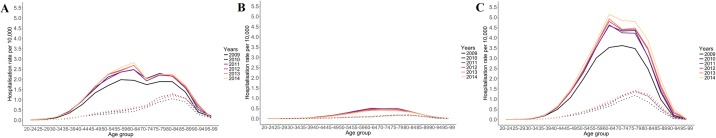
When age was taken into account, there were still differences according to sex (Fig 2). As seen in Table 3, the rates were higher for PCI only, then AMI and OIHD. In women, the rates were systematically lower than the rates in men from the age of 30. For men, hospitalisation rates increased with age, peaking at 5, 2.5 and 0.5 per 104 for PCI only, AMI and OIHD, respectively. in the 60-64 and 75-79 age groups, respectively. Between the ages of 60 and 70, rates decreased, except for PCI only in 2009 where the rate remained constant. For women, hospitalisation rates increased with age, peaking at 1 for AMI/PCI and at 0.15 for OIHD, respectively in the 75-84 year age group. As expected, beyond 90 years old, hospitalisation rates declined.
Fig 2. Hospitalisation rates per 104 by age group and sex (dotted line for women and solid line for men) according to year.
(A) Hospitalisation for AMI (ICD-10 code: I21). (B) Hospitalisation for OIHD (ICD-10 codes: I22 to I24). (C) Hospitalisation for PCI only i.e without AMI or OIHD.
Standardised rates by region and by sex
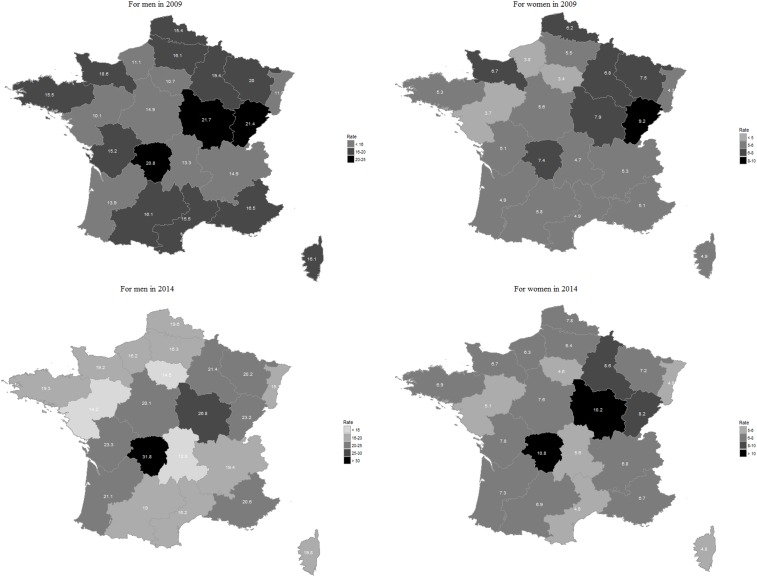
We compared results for hospitalisation standardised rates per 104 inhabitants between 2009 and 2014 according to sex and region for AMI (Fig 3 and S2 Table).
Fig 3. AMI hospitalisation standardised rates per 104 inhabitants, by region and sex, in 2009 and 2014.
For men, the average national standardised rates were 15.5 and 19.6 per 104 respectively in 2009 and 2014. Per region, rates varied from 10.1 per 104 in the Pays de Loire in 2009, to 31.8 per 104 in Limousin, in 2014. The greatest increase of rates was noted in Poitou-Charentes (34.8%) and in Limousin (34.6%), but these regions had low population variation rates. The lowest change rate (-3.9) was detected in Auvergne.
For women, the average national standardised rates were 5.6 and 6.9 per 104 in 2009 and 2014, respectively. In 2009, rates varied from 3.4 per 104 in Ile de France to 10.8 per 104 in the Limousin region in 2014. Changes in percentages of standardised rates between 2009 and 2014 were greatest for the regions of Haute-Normandie (39.8%) and Poitou-Charentes (34.2%), while the growth rate of the population between 2009 and 2014 was 0.3% and 0.4%, respectively. However, the lowest population change rate -13% was observed in Franche-Comté, the population of which increased by 1.3% over the six-year study period.
Standardised rates for non-AMI hospitalisations are presented in S2 Fig. The highest rates are observed in the southern and northeastern regions, regardless of the year and gender.
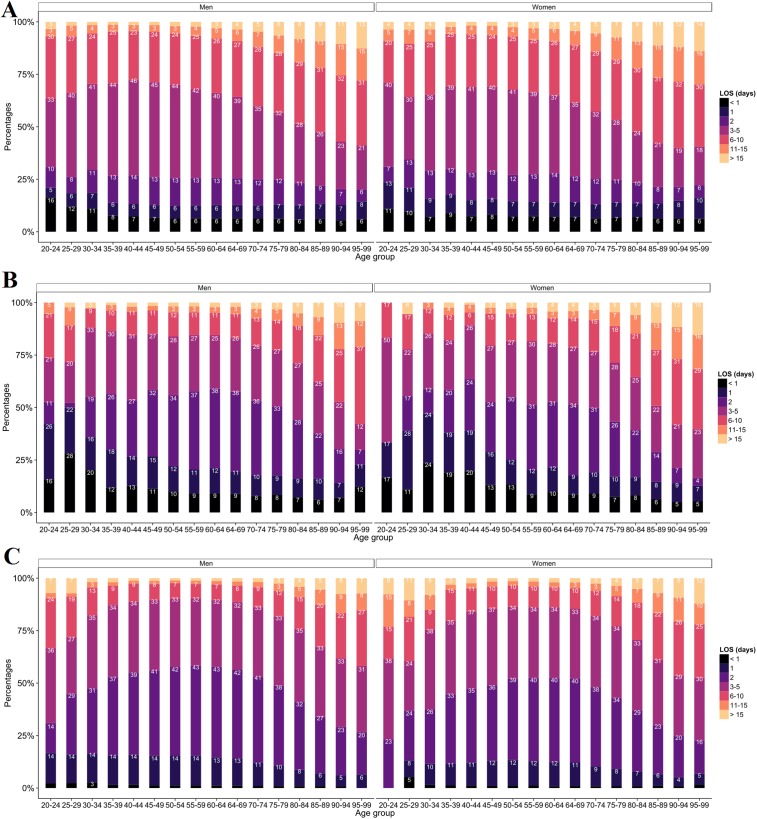
Length of hospital stay
Most stays for AMI lasted less than 6 days (Fig 4A). In AMI, the lengths of stay (LOS) were quite similar between men and women. However, longer stays were generally observed among men. For OIHD (Fig 4B), the proportion of 2-day stays was higher for women than for men except for 25-29 years old. In PCI only stays, (Fig 4C), we observed a high proportion of long stays (> 11 days) among women less than 35 years old. In addition, among women aged 35 to 80, the proportion of 2-day stays remained relatively constant (around 10%).
Fig 4. Distribution of length of stay (LOS) according to sex and age groups.
(A) Hospitalisation for AMI (ICD-10 code: I21). (B) Hospitalisation for OIHD (ICD-10 codes: I22 to I24). (C) Hospitalisation for PCI only i.e without AMI or OIHD.
In all cases combined, the LOS varied substantially: 3.7% of stays lasted less than 1 day, 9.4% lasted 1 day, whereas the 2 and 3-5 days concerned 27.4% and 33.5% of hospital stays, respectively. Only 3.5% of hospitalisations lasted more than 15 days. The LOS increased with age. The average LOS in the 20-24, 55-59 and +90 year of age groups was 5, 3 and 7 days, respectively. Stays of 11-15 days represented 4% of stays for the 20-24 years group, and 16% of stays for the 95-99. In 2014, the average of AMI LOS was 5.7 days, and was significatively lower (p < 9.8e-13) than in 2009 (6.0).
Hospital costs
The evolution of hospital costs over the observation period is presented in Table 4. In line with the evolution of the number of stays and patients (Table 3), there is a constant increase in direct costs from 2009 to 2014, except for OIHD, with a rate of change of about 42%. In contrast, for OIHD, we observed a decrease of about 3%. In France, the economic burden of CAD was € 3.65 billion in 2009 compared with € 5.08 billion in 2014.
Table 4. Estimated hospital costs* (€ billion) of AMI, OIHD and PCI only admissions in France from 2009 to 2014 with the overall evolution rate.
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Global rate (%) |
|
|---|---|---|---|---|---|---|---|
| AMI | 1.43 | 1.79 | 1.81 | 1.96 | 1.95 | 2.03 | 41.8 |
| OIHD | 0.22 | 0.22 | 0.25 | 0.22 | 0.23 | 0.21 | -3.3 |
| PCI only | 2.01 | 2.42 | 2.45 | 2.62 | 2.62 | 2.85 | 41.7 |
* hospital costs were estimated using hospital tariffs.
Burden and trends of MI/PCI readmissions
Readmission rates
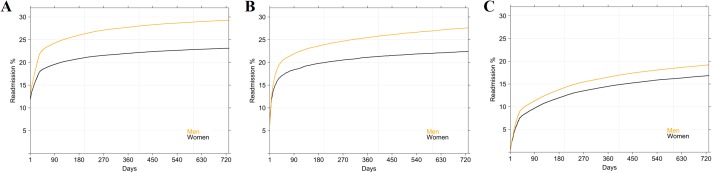
The median number of readmissions was one; 78% were readmitted twice, 18% thrice and 4% four fold or more. Men were significantly more readmitted than women (p < 2.2e-16) whatever the reason of first admission (Fig 5). Readmission rates were different according to the reason of first admission: rates were higher for AMI, then OIHD and PCI only. For instance, when first admission was AMI, the readmission rates by sex varied between 17 and 21% at month 1, between 20 and 24% at month 3, between 21 and 26% at month 6, between 22 and 28% at year 1 and between 23 and 29% at year 2.
Fig 5. Readmission rates: Kaplan-Meier analysis by sex.
(A) When first admission was AMI (ICD-10 code: I21). (B) When first admission was OIHD (ICD-10 codes: I22 to I24). (C) When first admission was PCI only i.e without AMI or OIHD.
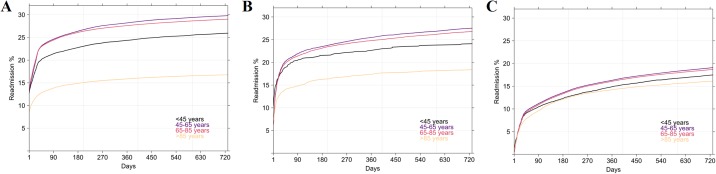
Fig 6 shows the readmission rates by age. Patients over 85 years had significantly lower readmission rates (p < 2.2e-16) whatever the reason of first admission. However, this observation is more important when AMI was the first admission than PCI only for example. Besides, The gap between the readmission rates of the 45-65 age group and the over 85 age group was larger for AMIs than for non-AMIs. AMI readmission rates by age ranged between 12 and 21% at month 1, between 14 and 25% at month 3, between 15 and 26% at month 6, between 15 and 27% at month 9, between 16 and 28% at year 1 and between 17 and 30% at year 2. As in Fig 5, readmission rates were higher for AMI, then OIHD and PCI only.
Fig 6. Readmission rates: Kaplan-Meier analysis by age group.
(A) When first admission was AMI (ICD-10 code: I21). (B) When first admission was OIHD (ICD-10 codes: I22 to I24). (C) When first admission was PCI only i.e without AMI or OIHD.
Readmission time
Analysing only readmissions, the average number of hospital stays during the 2009-2014 period was 2.3 (95% confidence interval [CI]: 2.29-2.32) with a significant difference (p < 2.2e-16) between men and women. Among patients who where rehospitalised, some (41,224 women and 129,677 men) were hospitalised several times in the six-year period, representing a total of 353,970 stays (85,867 for women and 268,112 for men). The median time until rehospitalisation with I21 ICD-10 code as primary diagnosis, was 41 days (average 208 days (95% CI: 206-212). Among rehospitalised patients, it occurred within three months in half of all cases. The readmission time was significantly different (p < 6.25e-06) between men and women, occurring on average 11 days later in men. The median readmission time was three months for both groups.
Table 5 summarises readmission times according to sex in AMI and non-AMI. For AMI, a relapse occurred within 48 hours, more often for women (6.2%) than for men (4.8%). A readmission was observed beyond six months in 38.2% of cases (38.4% for men vs. 37.6% for women). For non-AMI, the percentages of readmissions within 3 days are low (less than 2%). Beyond 6 months, there is readmission in about 2 out of 5 cases.
Table 5. Distribution of readmission times according to sex during the first year.
| AMI | non-AMI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Total | Men | Women | Total | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| <24h | 1,078 | 2.91 | 445 | 4.19 | 1,523 | 3.19 | 209 | 0.26 | 80 | 0.42 | 289 | 0.29 |
| 24h | 294 | 0.79 | 93 | 0.88 | 387 | 0.81 | 309 | 0.39 | 77 | 0.40 | 386 | 0.39 |
| 24-48h | 39 | 1.05 | 117 | 1.10 | 508 | 1.07 | 689 | 0.87 | 169 | 0.88 | 858 | 0.87 |
| 2-3 days | 412 | 1.11 | 136 | 1.28 | 548 | 1.15 | 928 | 1.18 | 213 | 1.11 | 1141 | 1.16 |
| 3-7 days | 2,031 | 5.48 | 592 | 5.57 | 2,623 | 5.50 | 5,077 | 6.43 | 1,048 | 5.45 | 6,125 | 6.24 |
| 7-15 days | 4,389 | 11.84 | 1,172 | 11.03 | 5,561 | 11.66 | 7,785 | 9.87 | 1,808 | 9.40 | 9,593 | 9.78 |
| 15-30 days | 7,573 | 20.43 | 1,951 | 18.37 | 9,524 | 19.97 | 9,572 | 12.13 | 2,228 | 11.59 | 11,800 | 12.02 |
| 1-3 months | 6 448 | 17.39 | 1,892 | 17.81 | 8,340 | 17.49 | 10,871 | 13.78 | 2,865 | 14.90 | 13,736 | 14.00 |
| 3-6 months | 3,745 | 10.10 | 1,162 | 10.94 | 4,907 | 10.29 | 9,670 | 12.25 | 2,577 | 13.41 | 12,247 | 12.48 |
| 6-12 months | 3,886 | 10.48 | 1,122 | 10.56 | 5,008 | 10.50 | 11,434 | 14.49 | 2,934 | 15.26 | 14,368 | 14.64 |
| >1 year | 6,826 | 18.41 | 1,939 | 18.26 | 8,765 | 18.38 | 22,367 | 28.34 | 5,225 | 27.18 | 27,592 | 28.12 |
| Total | 37,073 | 99.99 | 10,621 | 99.99 | 4,694 | 100 | 78,911 | 99.99 | 19,224 | 100 | 98,135 | 99.99 |
Regional disparities
We compared readmission rates at 3 months, 9 months and one year for AMI and non-AMI (S3 Fig). There is a little asymmetry; readmission rates according to region are different according to the sex. Men rates were higher than women, particularly in AMI readmissions. In addition we observed a North-South readmission divide, except Burgundy.
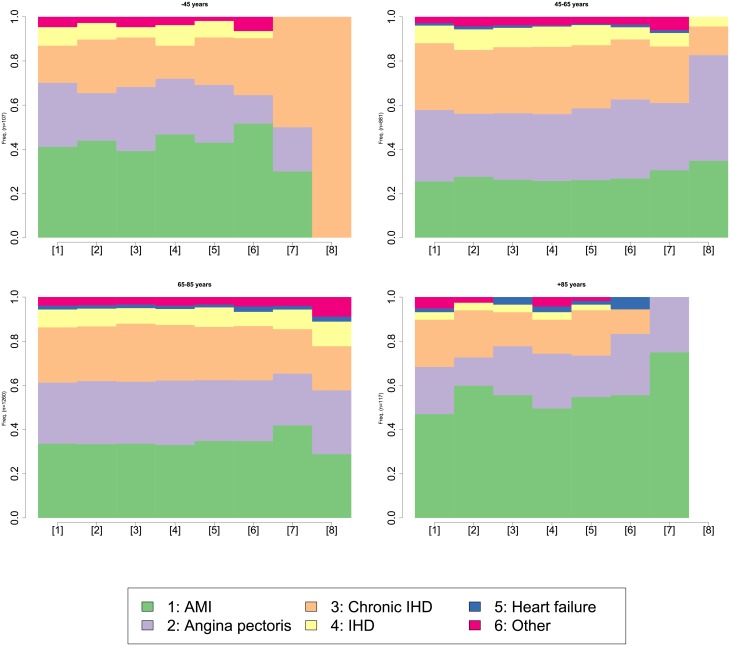
Description of care pathways according to hospital diagnosis
Sequences of events were analysed by sex and age. Data were separated according to length of sequences (i.e. number of hospitalisations in the study period for a given patient). The first analysis carried out on short length sequences (less than 5 events) did not highlighted between-group differences. A further analysis carried out on long sequences (at least 5 events, and less than 8 events) gave different results. Trajectories were significantly different by sex (p < 0.01) but also by age (p < 0.02). The chronogram, displayed in Fig 7, is a status distribution plot. It represents the general patterns of the whole set of sequences by age group. Fig 7 shows jumps in the sequence of the principal diagnosis distributions, more specifically between the <45 and the 45-65 year group and between the >85 and 65-85 year group from the sixth event onward. AMI was more frequent in women but also in the <45 and the >85 years, irrespective of sex.
Fig 7. Cross-sectional distributions of principal diagnosis by age for patients who experienced 4 to 8 hospitalisations during 2009-2014.
Burden of in-hospital mortality
In-hospital mortality by sex and age
Fig 8 represents the proportion of deaths according to age group by sex and year. Over the six-year period, regardless of sex, in-hospital fatalities mostly affected the 80-89 age group with a rate of 20%. In women, the proportion of deaths was higher in the 80-94 age group, with percentages ranging from 19% to 28% depending on the years. Whereas in men, the proportion increased with age and decreased over 90-year old.
Fig 8. Proportion of in-hospital deaths by age group according to sex and year.
For sake of readability, proportions were only displayed for values greater than or equal to 5%.
In-hospital mortality rates
In the years 2009 to 2014, 3.3% (29,728 subjets) of hospitalised patients died with an in-hospital fatality rate ranging from 80 to 95 per 104 hospital stays per year. Thus, every year, between 4,212 and 5,252 people hospitalised with MI/PCI died during their hospital stay. Hospital death decreased significantly by 15% (p < 2.2e-16) during the period from 4,2% in 2009 to 3.6% in 2014. The in-hospital mortality rate was higher among women (between 0.013 and 0.022 per 104 hospitalisations) than among men (0.003 per 104 hospitalisations).
The analysis by age showed higher rates in patients aged less than 35, regardless of sex. The rates decreased until 40 years old, and from the 75-79 age group onwards rates grew exponentially with age.
Discussion
Primary and associated diagnoses
During the five years from 2010 to 2014, the number of incident cases increased regardless of the reason for hospitalisation. However, our study highlights differences according to the diagnosis at first admission during the study period. Indeed, only the incident cases of OIHD observed a decline of about 14%. Unlike PCIs, the increase in AMI incidence was greater among men. There are potential reasons for these findings: a wider access to healthcare from the first MI symptoms through information and awareness campaigns, together with a better dissemination of recommendations published by the French National High Authority for Health since 2007 following the consensus conference of November, 2006 [27]; an increase in MI cases, although the health survey in 2015 found no change in MI cases in the French population from 2000 to 2010 [28]; a slight increase in risk factors was observed, for instance, daily smoking prevalence in France between 2005 and 2010 increased 7% [28]; and finally the definition used in this analysis is less precise than those of the Third Universal Definition of Myocardial Infarction [29].
Globally, our analysis confirmed a preponderance of incident stays for men, already established in the literature [30], almost three times more frequent than in women. The current burden of MI/PCI is influenced by cardiovascular health disparities. The analysis of the health status of the population studied through the comorbidities of the Elixhauser score shows that a significant proportion of the population suffers from cardiovascular disorders, hypertension, obesity and diabetes. This observation, explained by the evolving change in lifestyle (tobacco use, decreased physical activity, and westernization of traditional diets), is worrisome and contributes to the burden of hypertension, an important contributor to CAD [31]. This is how the fight against the progression of the CAD epidemic is deeply linked to that of the progression of obesity and sedentary lifestyle [32]. In addition, modifiable risk factors must be added to that of air pollution. In view of this work, it would be interesting to complete this work by considering the environment aspect with data on air quality measurements [33].
Burden and trends of MI/PCI hospitalisations
During the 2009-2014 period, hospitalisations for MI/PCI represented an annual average of 150,000 stays and an average of about 125,000 patients in health services. We highlighted that the annual hospitalisation trend was globally increasing. Meanwhile, the total number of hospital stays for any reason decreased from 11.96 million in 2009 to 11.31 million in 2014. Therefore, MI/PCI hospital burden has increased over the study period, representing 1% of all stays in 2009 compared to 1.5% in 2014.
Our study reported increasing rates in young women. However, the latter may be driven by the low overall frequency, making a small absolute increase account for a high relative change. We also observed a difference according to age groups: women were affected later in life, together with a higher life expectancy (84.4 years for women vs. 77.7 years for men in 2009, source Insee 2015), and an aging population between 2009 and 2014 (About 57%, source Insee 2016).
In the present data, AMI cases were heterogeneous across the country. High hospitalisation rates in the South were due to elderly population growth in these regions. At a national level, the MONICA project highlighted an MI case geographic disparity worldwide, but also within each country, with a North-South divide [34].
In most cases, the LOS depended on patients’ age and MI complications. We found that for elderly patients the average LOS was seven days, versus three days for patients between 55 and 59 years old. This is consistent with the French average LOS of one week. Early hospital discharge is possible: in an uncomplicated revascularized MI, the vital risk drops significantly at three days [34]. The MI care is different according to countries: it is four weeks in Japan [35], four days in Norway and Denmark, about 10 days in Germany and Greece according to the OECD (Organisation for Economic Co-operation and Development) survey [36].
From an economic point of view, the gross cost of hospitalisation is increasing during the observation period for AMIs and PCIs and decreasing for OIHD in line with hospitalisations trends. The cost of a hospital stay may vary from one patient to another, depending on LOS, age and comorbid conditions. In average, CAD hospital cost was around 4 billion euros [5]. However, since it is difficult to determine the accountability of comorbidities, to refine these results, it would be interesting to take into account both all hospitalisations of patients (not only those related to CAD) but also the outpatient care consumption [37].
Burden and trends of MI/PCI readmissions
In summary, our analysis highlighted several key points which might be helpful in patient care optimisation and healthcare resources allocation. Firstly, readmission for an MI/PCI occurred in 30% of patients and was more frequent in men and in the 65-85 age group. This confirmed the discrepancies in risk linked to sex and age group [38]. Secondly, readmission rates were highest for, in that order, an AMI, an OHID and a PCI, whatever the diagnosis of the first admission. Thirdly, in patients with AMI, 14% were readmitted within the first month and 16% within the following two-to-three months. These results are quite similar to those of one study which established that 20% of patients with a primary MI diagnosis were readmitted or died one month later. Moreover, the analysis of the readmission time revealed that 75% of MI relapse occurred in the year following the primary diagnosis [39]. Fourthly, we highlighted a South-North divide in readmissions. Regional variability in population MI incidence and mortality was ascertained in Spain [40], and in other countries by the WHO-MONICA Project [9]. Besides, a sex discordance between certain regions where hospitalisation rates for men were always higher, as was incidence in females was established. Yet mortality rates were not abnormally elevated, except in Corsica.
As we took into account all readmissions without distinguishing scheduled readmissions (for instance, an angioplasty for another vessel) from those resulting from an evolution of the disease, our analysis has established a consistent readmission burden for MI/PCI for both recurrences and follow-up care after a first episode. Moreover, with regard to care follow-up, the sequence analysis revealed that regardless of the timing of the care pathway, AMI diagnosis was most common in women, but also in the extreme age groups (<45 years and >85 years). Conversely, in the middle age groups, there were more events such as CIHD and IHD. These results are consistent with the US study of readmission rates after AMI by age and sex [38]. In addition, we noticed that some patients had similar pathways. This information could prove invaluable for health planning: adapting the patient’s care pathway or better managing the availability of resources. Based on this observation, we investigate an extension work. We have developed a model to characterize hospital healthcare flows from patient care pathways in order to improve their knowledge in a perspective of possible change in public health policies for the improvement of patient care [41].
Burden of in-hospital mortality
Our findings established a decline in annual mortality rates over the study period. These results are consistent with previous investigations and tend to suggest an improved prognosis for these patients and better management of acute coronary events, as well as risk factors in secondary prevention [5]. The latter might explain the inflation of the economic burden.
Furthermore, our results pinpointed that adjusted mortality rates were higher for inpatients aged less than 40 and more than 80, but a conclusive link with comorbidity could not be found. In fact, administrative data are not designed to explore this question. Death generally occurred during the first hospital admission [42]. Moreover, this risk of death was higher in women. However, women generally suffered MI later than men. Thus, they were older at MI occurrence which may contribute to a higher severity of a subsequent cardiac event.
Most countries referred to nationwide clinical registries to evaluate and forecast trends in MI [7, 43, 44]. AMI mortality rate was assessed at 9.7% in Great Britain with National Institute for Cardiovascular Outcomes Research/Myocardial Ischaemia National Audit Project and CArdiovascular disease research using LInked Bespoke studies and Electronic health Records, at 8.4% in Sweden with Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated Accorded to Recommended Therapies/Register of Information and Knowledge about Swedish Heart Intensive care Admissions, at 10.8% in Germany with hospital data and at 5.3% in France with FAST-MI (French nationwide registry). Nevertheless, health coding systems, MI case identification algorithms and years studied did not allow comparison of the reported rates with our results.
In future work, we plan to elaborate a prognostic model of in-hospital mortality in acute coronary syndrome from patient pathways to predict fatality risk. Indeed, a better knowledge of the relationship between care pathways, associated with chronic conditions and mortality might help to combat this public health issue by reducing CAD mortality burden.
Data completeness
Although we attempted to provide a systematic view in annual MI burden, our investigation underlined limits in data completeness due to the retained choice of the MI case identification algorithm.
Patients with MI not seen by the healthcare providers can be categorised in two groups: 1) Silent MI without health care [45]. The patient are unaware they have had a heart attack since they did not experience the classic symptoms such as chest pain; 2) Sudden cardiac death. Indeed, most of the deaths after MI occurred outside health facilities: of the 33,435 annual deaths (Source Center for Epidemiology on Medical Causes of Death 2013), circa 5,085 deaths occurred during hospitalisation (Source ATIH 2013).
Some patients, out of hospital after emergency services, probably considered the least serious or on the contrary who died in the emergency room, are not recorded in the PPS database. In this instance, confining the analysis to hospitalised MI in PPS gives a homogeneous but partial view of the MI burden.
Several studies compared cardiac registers with medico-economics data. For instance, a MI monitoring study [21] reported a sensitivity rate about 76% and positive predictive value (PPV) of 78% in detecting this pathology with ICD-10 in PPS, regardless of age between 35 and 74, and irrespective of gender. Another study used ICD-10 codes based on data from 2004 to 2008, comparing accuracy in detecting MI between PPS and register obtained sensitivity of 77% and PPV of 69% [20]. At the international level, there is an investigation on validation of identification MI algorithms from electronic healthcare records in different countries using distinctive disease coding system [18]. The identification algorithms based on ICD codes in Italy, Denmark and the Netherlands had a PPV greater than 90%. Moreover, Coloma et al. suggested that using several sources of information offers diverse perspectives and complementary knowledge. For instance, GPs databases when available. Hospital base report information related to care, such as stenting or intraluminal dilatation, was provided in health facilities only.
Conclusion
We quantified the burden of CAD, as opposed to other studies estimating changing trends, this requires taking into account the entire consumption of hospital care. Our findings, based on 900,121 stays representing 678,021 patients with MI/PCI during the study period, showed that the burden of CAD is persisting making it a major public health issue exerting heavy economic costs. Indeed, we underscored a constant increase in AMI and PCI burden meaning rising hospitalisation rates with rising health care costs. In contrast, we observed a decline in OIHD burden. However, mortality rates were decreasing illustrating the medical progress in reducing CVD fatality in recent decades, but also the positive impact of health campaigns to address risk factors such as smoking bans in work and public places [46] and reducing salt intake [47].
Although our results are to be modulated because of the limits in PPS data completeness, these data appears as a complementary approach to follow up the burden of AMI hospitalisations but also for for public health surveillance of several conditions. Moreover, these data can be completed with information collected by the French health insurance system [48] from medico-economic research.
Given the demographic changes (growing population, ageing population…) with the still rising risk factors, the future CAD burden is expecting a further increase. Therefore, it is essential to continue monitoring and measuring the burden of this epidemic in order to measure the impact of anti-development campaigns, as well as to anticipate the real needs for the years in terms of staff and infrastructure.
Supporting information
(PDF)
(PDF)
(TIFF)
(TIFF)
(A) When admission was AMI (ICD-10 code: I21). (B) When admission was non-AMI.
(TIFF)
Acknowledgments
We warmly thank Sarah Kabani for her expert editing of the manuscript.
Data Availability
All relevant data are within the manuscript and its Supporting Information files. The original data source is not accessible because it is protected by data confidentiality. The data is stored by a third party, which delivers the permission to access this data in the same manner as the authors. The authors didn’t have any access privileges that other researchers would not have. The request for data has to be sent to the Système national des données de santé (SNDS). The procedure is clearly described here: https://www.snds.gouv.fr/SNDS/Processus-d-acces-aux-donnees.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006. November;3:e442 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global atlas on cardiovascular disease prevention and control. World Health Organization; World Heart Federation; World Stroke Organization. 2011. Available: http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/
- 3.World Health Organization. Cardiovascular diseases (CVDs) World Health Organization. 2017. Available: http://www.who.int/mediacentre/factsheets/fs317/en/
- 4.World Health Organization. New initiative launched to tackle cardiovascular disease, the world’s number one killer. WHO. 22 Sep 2016. Available: http://www.who.int/cardiovascular_diseases/global-hearts/Global_hearts_initiative/en/
- 5. Tuppin P, Rivière S, Rigault A, Tala S, Drouin J, Pestel L et al. Prevalence and economic burden of cardiovascular diseases in France in 2013 according to the national health insurance scheme database. Archives of Cardiovascular Diseases. 2016:109(6–7):399–411. 10.1016/j.acvd.2016.01.011 [DOI] [PubMed] [Google Scholar]
- 6. Ducimetière P, Ruidavets J-B, Montaye M, Haas B, Yarnell J. Five-year incidence of angina pectoris and other forms of coronary heart disease in healthy men aged 50–59 in France and Northern Ireland: the Prospective Epidemiological Study of Myocardial Infarction (PRIME) study. Int J Epidemiol. 2001;30: 1057–1062. 10.1093/ije/30.5.1057 [DOI] [PubMed] [Google Scholar]
- 7. Puymirat E, Simon T, Cayla G, Cottin Y, Elbaz M, Coste P, et al. Acute myocardial infarction: changes in patient characteristics, management, and 6-Month outcomes over a period of 20 years in the FAST-MI program (French registry of acute ST-elevation or non-ST-elevation myocardial infarction) 1995 to 2015. Circulation. 2017;136: 1908–1919. 10.1161/CIRCULATIONAHA.117.030798 [DOI] [PubMed] [Google Scholar]
- 8. Wagner A, Haas B, Montaye M, Moitry M, Ruidavets JB, Dallongeville J, et al. Trends of in-hospital and out-of-hospital coronary heart disease mortality rates in French registers in the period 2000-2013. Eur Heart J. 2017;38: 4441 10.1093/eurheartj/ehx504.P4441 [DOI] [Google Scholar]
- 9. Thorvaldsen P, Asplund K, Kuulasmaa K, Rajakangas A-M, Schroll M. Stroke incidence, case fatality, and mortality in the WHO MONICA project. Stroke. 1995;26: 361–367. 10.1161/01.STR.26.3.361 [DOI] [PubMed] [Google Scholar]
- 10. Philippe F, Blin P, Bouée S, Laurendeau C, Torreton E, Gourmelin J, et al. Costs of healthcare resource consumption after a myocardial infarction in France: An estimate from a medicoadministrative database (GSB). Int J Cardiol. 2016;219: 387–393.27372604 [Google Scholar]
- 11.Ruch P, Gobeill J, Tbahriti I, Geissbühler A. From episodes of care to diagnosis codes: automatic text categorization for medico-economic encoding. AMIA Annual Symposium Proceedings. 2008. pp. 636–640. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2655971/ [PMC free article] [PubMed]
- 12. Rubbo B, Fitzpatrick NK, Denaxas S, Daskalopoulou M, Yu N, Patel RS, et al. Use of electronic health records to ascertain, validate and phenotype acute myocardial infarction: A systematic review and recommendations. Int J Cardiol. 2015;187: 705–711. 10.1016/j.ijcard.2015.03.075 [DOI] [PubMed] [Google Scholar]
- 13. McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PloS One. 2014;9: e92286 10.1371/journal.pone.0092286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Le Bihan-Benjamin C. L P, Chatelier G. Linking hospital stays in the national PMSI MCO database improved between 2006 and 2009: Analysis and consequences. J Econ Medicale. 2012;30: 17–30. [Google Scholar]
- 15.Agence Technique de l’Information sur l’Hospitalisation. Manuel des GHM—Version définitive 11g. Paris, France: Ministère de la Santé et des Sports; 2015 Jul p. 92. Available: http://www.atih.sante.fr/manuel-des-ghm-version-definitive-11g
- 16. Trombert-Paviot B, Couris CM, Couray-Targe S, Rodrigues JM, Colin C, Schott AM. Quality and usefulness of an anonymous unique personal identifier to link hospital stays recorded in French claims databases. Rev Epidemiol Santé Publique. 2007;55: 203–211. 10.1016/j.respe.2007.01.029 [DOI] [PubMed] [Google Scholar]
- 17. Chevreul K, Prigent A, Durand-Zaleski I, Steg PG. Does lay media ranking of hospitals reflect lower mortality in treating acute myocardial infarction? Arch Cardiovasc Dis. 2012;105: 489–498. 10.1016/j.acvd.2012.05.007 [DOI] [PubMed] [Google Scholar]
- 18. Coloma PM, Valkhoff VE, Mazzaglia G, Nielsson MS, Pedersen L, Molokhia M, et al. Identification of acute myocardial infarction from electronic healthcare records using different disease coding systems: a validation study in three European countries. BMJ Open. 2013;3: e002862 10.1136/bmjopen-2013-002862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Haesebaert J, Termoz A, Polazzi S, Mouchoux C, Mechtouff L, Derex L, et al. Can hospital discharge databases be used to follow ischemic stroke incidence? Stroke. 2013;44: 1770–1774. 10.1161/STROKEAHA.113.001300 [DOI] [PubMed] [Google Scholar]
- 20. Aboa-Eboulé C, Mengue D, Benzenine E, Hommel M, Giroud M, Béjot Y, et al. How accurate is the reporting of stroke in hospital discharge data? A pilot validation study using a population-based stroke registry as control. J Neurol. 2013;260: 605–613. 10.1007/s00415-012-6686-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Peretti C, Bonaldi C. Étalonnage du PMSI MCO pour la surveillance des infarctus du myocarde. Saint-Maurice, France: Institut de veille sanitaire; 2010 p. 24. Available: http://opac.invs.sante.fr/index.php?lvl=notice_display&id=596.
- 22.Mousquès J. Common classification of medical procedures. France: Health Policy Monitor; 2005 Apr p. 8. Report No.: 5. Available: http://www.hpm.org/fr/a5/2.pdf
- 23. Alexandrescu R, Bottle A, Jarman B, Aylin P. Current ICD10 codes are insufficient to clearly distinguish acute myocardial infarction type: a descriptive study. BMC Health Serv Res. 2013;13: 468 10.1186/1472-6963-13-468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical Care. 2009;47(6): 626–633. Available: http://www.jstor.org/stable/40221931. [DOI] [PubMed] [Google Scholar]
- 25. Nordstokke DW, Zumbo BD. A new nonparametric Levene test for equal variances. Psicológica. 2010;31: 401–430. [Google Scholar]
- 26. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. Available: https://www.R-project.org/ [Google Scholar]
- 27. HAS. Prise en charge de l’infarctus du myocarde à la phase aiguë en dehors des services de cardiologie. Presse Médicale. 2007;36: 1029–37. [DOI] [PubMed] [Google Scholar]
- 28.Direction de la recherche des études de l’évaluation et des statistiques (DREES). L’état de santé de la population en France. DREES Éditions; 2015 p. 502. Available: http://www.ladocumentationfrancaise.fr/var/storage/rapports-publics/154000124.pdf
- 29. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33: 2551–2567. 10.1093/eurheartj/ehs184 [DOI] [PubMed] [Google Scholar]
- 30. Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, Simone GD, et al. Heart Disease and Stroke Statistics—2010 Update: A Report From the American Heart Association. Circulation. 2010;121: e46–e215. 10.1161/CIRCULATIONAHA.109.192667 [DOI] [PubMed] [Google Scholar]
- 31. Bonow RO, Smaha LA, Smith SC, Mensah GA, Lenfant C. World Heart Day 2002: The International Burden of Cardiovascular Disease: Responding to the Emerging Global Epidemic. Circulation. 2002;106(13): 1602–1605. 10.1161/01.CIR.0000035036.22612.2B [DOI] [PubMed] [Google Scholar]
- 32. Leong Darryl P, Joseph Philip G, McKee M, Anand Sonia S, Teo Koon K, Schwalm J-D, Yusuf S. Reducing the global burden of cardiovascular disease, Part 2. Circ Res. 2017;121(6):695–710. 10.1161/CIRCRESAHA.117.311849 [DOI] [PubMed] [Google Scholar]
- 33. Feigin V L, Roth G A, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet Neurol. 2016;15: 913–924. 10.1016/S1474-4422(16)30073-4 [DOI] [PubMed] [Google Scholar]
- 34. Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104: 2746–2753. 10.1161/hc4601.099487 [DOI] [PubMed] [Google Scholar]
- 35. Kinjo K, Sato H, Sakata Y, Nakatani D, Mizuno H, Shimizu M, et al. Identification of uncomplicated patients with acute myocardial infarction undergoing percutaneous coronary intervention. Circ J. 2005;69: 1163–1169. 10.1253/circj.69.1163 [DOI] [PubMed] [Google Scholar]
- 36.The Organisation for Economic Co-operation and Development (OECD). Average length of stay in hospitals. Health at a Glance 2015. Éditions OCDE. Paris; 2015. pp. 108–109. Available: 10.1787/health_glance-2015-34-en. [DOI]
- 37. Leal J, Luengo-Fernández R, Gray A, Petersen S, Rayner M. Economic burden of cardiovascular diseases in the enlarged European Union. Eur Heart J. 2006;27(13): 1610–1619. 10.1093/eurheartj/ehi733 [DOI] [PubMed] [Google Scholar]
- 38. Khera R, Jain S, Pandey A, Agusala V, Kumbhani DJ, Das SR, et al. Comparison of readmission rates after acute myocardial infarction in 3 patient age groups (18 to 44, 45 to 64, and ≥65 Years) in the United States. Am J Cardiol. 2017;120: 1761–1767. 10.1016/j.amjcard.2017.07.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Oliver D. Readmission rates reflect how well whole health and social care systems function. BMJ. 2014;348: g1150 10.1136/bmj.g1150 [DOI] [PubMed] [Google Scholar]
- 40. Marrugat J, Elosua R, Aldasoro E, Tormo MJ, Vanaclocha H, Segura A, et al. Regional Variability in Population Acute Myocardial Infarction Cumulative Incidence and Mortality Rates in Spain 1997 and 1998. Eur J Epidemiol. 2004;19: 831–839. 10.1023/B:EJEP.0000040531.77638.17 [DOI] [PubMed] [Google Scholar]
- 41. Pinaire J, Azé J, Bringay S, Poncelet P, Genolini C, Landais P. PaFloChar: an innovating approach to characterise patient flows in myocardial infarction MIE: Medical Informatics Europe. Goteborg, Sweden; 2018. Available: https://hal.archives-ouvertes.fr/hal-01781095 [PubMed] [Google Scholar]
- 42. Asaria P, Elliott P, Douglass M, Obermeyer Z, Soljak M, Majeed A, et al. Acute myocardial infarction hospital admissions and deaths in England: a national follow-back and follow-forward record-linkage study. Lancet Public Health. 2017;2: e191–e201. 10.1016/S2468-2667(17)30032-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Freisinger E, Fuerstenberg T, Malyar NM, Wellmann J, Keil U, Breithardt G, et al. German nationwide data on current trends and management of acute myocardial infarction: discrepancies between trials and real-life. Eur Heart J. 2014;35: 979–988. 10.1093/eurheartj/ehu043 [DOI] [PubMed] [Google Scholar]
- 44. Chung S-C, Sundström J, Gale CP, James S, Deanfield J, Wallentin L, et al. Comparison of hospital variation in acute myocardial infarction care and outcome between Sweden and United Kingdom: population based cohort study using nationwide clinical registries. BMJ. 2015;351: h3913 10.1136/bmj.h3913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Evuru S, Venkata Krishna Rao S. A study of clinical profile of unrecognised myocardial infarction. J Evol Med Dent Sci. 2017;6: 4279–4290. [Google Scholar]
- 46. Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis. J Am Coll Cardiol. 2009;54: 1249–1255. 10.1016/j.jacc.2009.07.022 [DOI] [PubMed] [Google Scholar]
- 47. He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. The Lancet. 2011;378: 380–382. 10.1016/S0140-6736(11)61174-4 [DOI] [PubMed] [Google Scholar]
- 48. Tuppin P, de Roquefeuil L, Weill A, Ricordeau P, Merlière Y. French national health insurance information system and the permanent beneficiaries sample. Rev DÉpidémiologie Santé Publique. 2010;58: 286–290. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(TIFF)
(TIFF)
(A) When admission was AMI (ICD-10 code: I21). (B) When admission was non-AMI.
(TIFF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files. The original data source is not accessible because it is protected by data confidentiality. The data is stored by a third party, which delivers the permission to access this data in the same manner as the authors. The authors didn’t have any access privileges that other researchers would not have. The request for data has to be sent to the Système national des données de santé (SNDS). The procedure is clearly described here: https://www.snds.gouv.fr/SNDS/Processus-d-acces-aux-donnees.