Abstract
Objective To review research on observed family communication in families with children with chronic illnesses compared with families with healthy, typically developing children, and to integrate findings utilizing a unifying family communication framework. Method Topical review of studies that have directly observed family communication in pediatric populations and included a typically developing comparison group. Results Initial findings from 14 studies with diverse approaches to quantifying observed family communication suggest that families with children with chronic illnesses may demonstrate lower levels of warm and structured communication and higher levels of hostile/intrusive and withdrawn communication compared with families with healthy, typically developing children. Conclusion An integrative framework of family communication may be used in future studies that examine the occurrence, correlates, and mechanisms of family communication in pediatric populations.
Keywords: chronic illness, family functioning, parent–adolescent communication, research design and methods.
Pediatric chronic illness affects 20–30% of families in the United States (van der Lee, Mokkink, Grootenhuis, Heymans, & Offringa, 2007) and represents a significant challenge for these families. While families serve as important resources for children, it is plausible that family processes may be affected by the numerous stressors associated with caring for a child with a chronic illness. One important indicator of a family’s response to these substantial demands is reflected in the nature and quality of communication. Since family communication in pediatric populations was formally identified as a research priority over 30 years ago (Drotar, 1981), the field has made significant advances in methodological assessment through direct observation for a variety of chronic illnesses (Wysocki, 2015).
Family communication has been identified as a correlate of numerous important developmental, psychosocial, and health outcomes, including behavioral autonomy, parental and child distress, and medical adherence (Jaser & Grey, 2010; Stepansky, Roache, Holmbeck, & Shultz, 2009; Wood et al., 2008). Although pediatric illness groups have important differences, they share illness-related stressors that may be associated with common family processes (Cohen et al., 2011). Despite the potential importance of understanding the nature and impact of communication in families with children with chronic illnesses compared to families with typically developing children, findings have not yet been integrated across studies and pediatric diagnoses. Synthesis of findings would afford a broad understanding of differences in communication in these families, and could be leveraged to improve understanding of clinically important correlates of communication and shared points of intervention. However, cross-study comparisons are challenging due to substantial heterogeneity in coding systems.
One way to facilitate comparisons and integrate current knowledge is to apply a unifying family communication framework to synthesize data from diverse observational coding systems. The purpose of this topical review is to provide an overview of how family communication may differ in families of children with chronic health conditions through the application of such a framework. Specifically, we (1) review coding systems used to quantify observed family communication in pediatric samples; (2) present a unifying family communication framework; (3) review findings from a sample of studies that compared communication in families with a child with a chronic illness to families with healthy, typically developing children through the application of this framework; and (4) present considerations for future studies of family communication in pediatric conditions.
Direct Observation of Family Communication in Pediatric Populations
Family communication has overwhelmingly been measured with retrospective, self-report questionnaires (Stamp & Shue, 2013). Yet, the limitations of using self-reports as a single method include problems of limited recall, social desirability, and shared method variance with other constructs of interest (Holmbeck et al., 2002; Stamp & Shue, 2013; Wysocki, 2015). Observational methods allow for a more objective estimate of behaviors, allowing researchers to directly assess specific types of interactions and communication patterns of interest, rather than rely solely on the perceptions of children and parents (Feeney & Noller, 2013; Stamp & Shue, 2013; Wysocki, 2015). There are also limitations of direct observation; even if conducted in the home environment to increase ecological validity, direct measurement of behavior is time-consuming and labor-intensive (Feeney & Noller, 2013; Stamp & Shue, 2013). However, direct observation in psychology research is recognized as an important component of multi-method, evidence-based methodology to assess communication patterns in families (Chorney, McMurtry, Chambers, & Bakeman, 2015; Stamp & Shue, 2013; Wysocki, 2015).
Direct observation of family communication generally involves video-recording one or more semi-structured family interaction tasks in a simulated or natural environment and reviewing and assigning codes using a validated coding system (Chorney et al., 2015). However, there is considerable heterogeneity among observation methods, as specific research questions and feasibility considerations may direct important choices on how researchers observe and code communication. Family communication paradigms vary widely by task structure (e.g., games, discussions) as well as setting (e.g., home, laboratory). However, perhaps the greatest heterogeneity involves the operationalization of family communication through diverse coding procedures. First, coding methods vary by level of measurement, from macro-level systems that take into account frequency, duration, and intensity after viewing an entire sample of behavior (e.g., behavioral control), to micro-level systems that tally the frequency of verbal utterances or behaviors in predetermined categories (e.g., directives). Second, there is variability in whether coding targets the entire family, dyads, or individuals. And third, coding procedures examine different communication patterns depending on the research question and population of interest. As such, synthesis of research in this area has been limited by methodological heterogeneity. For example, previous studies with cystic fibrosis, type 1 diabetes, and asthma samples have used the Mealtime Interaction Coding System (MICS; Dickstein et al., 1994), which emphasizes the importance of transactional patterns in the family system and yields macro-level ratings for overall positive family-level communication. In contrast, several studies with asthma have used the German KPI coding system (Kategoriensystem Fur Partner-Schaftliche Interactions; Hahlweg et al., 1984), which examines dyadic family interactions and yields micro-level scores for parents’ negative verbal behavior (e.g., criticism). These systems are discussed further below.
Although diverse in scientific aims and methodology, there is a growing body of research that has sampled and quantified broad patterns of family communication in a variety of pediatric illnesses (e.g., asthma, epilepsy, cystic fibrosis, spina bifida, type 1 diabetes) to answer a key research question: Is family communication different in families with a chronically ill child? Studies using single cohort designs are important for understanding communication patterns surrounding illness-specific health behaviors (e.g., during medical tasks) and variability and correlates within a population of families faced with a specific chronic health condition. However, critical for this topical review, case-controlled research designs allow researchers to directly evaluate whether broad areas of family communication (e.g., warmth) occur at different frequencies and intensities in families with children with chronic illnesses compared to those with typically developing children. Although methodological heterogeneity in studies to date presents a challenge to compare across studies and pediatric illnesses, integrating findings within a unifying framework of family communication allows for a general synthesis of research findings, and is the first step toward providing an important reference point for future research on communication patterns in families with children with pediatric illnesses.
Applying a Unifying Framework of Family Communication
Family communication is broadly defined as the process through which “each member of the family engages in communicative behavior and exchanges verbal and nonverbal messages and information with other family members” (Stamp, 2004, p.18). While researchers have traditionally described family communication as positive or negative, several comprehensive communication models have brought greater detail to observational research in families. Stafford (2013) highlighted several common themes in these models of family communication that evoke dimensions of warmth and control. This includes circumplex models of family functioning (Beveridge & Berg, 2007; Kiesler, 1996; Olson Russell, & Sprenkle, 1989); models of family communication environments that consider flexibility and cohesion (Fitzpatrick & Marshall, 1996; Koerner & Fitzpatrick, 2013); and those that emphasize autonomy and self-determination, especially in the context of adolescent development (Allen, Hauser, Bell, & Connor, 1994; Ryan & Deci, 2000). Frameworks that draw on warmth and control have roots in Baumrind’s (1968) seminal model of parenting styles, in which the most adaptive, authoritative parenting encompasses both warmth and support as well as developmentally appropriate control and boundaries. Baumrind’s model has also influenced pediatric studies examining parenting style specifically (Butler, Skinner, Gelfand, Berg, & Wiebe, 2007; Olvera & Power, 2010). The communication framework outlined here, however, differs from Baumrind’s original model and can be considered a synthesis of previous models of family communication (Stafford, 2013).
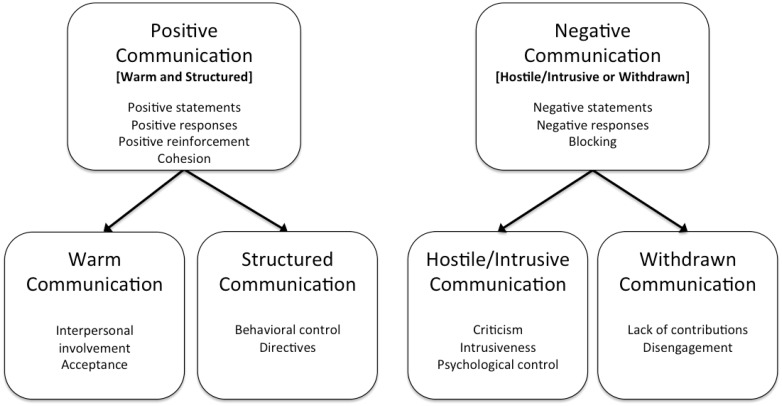
A framework that draws on warmth and control allows for the examination of more specific categories of positive and negative communication, such that positive communication involves high levels of both warm and structured interaction patterns, whereas overall negative communication involves high levels of either hostile/intrusive or withdrawn patterns (Figure 1). Specifically, warm communication includes expression of positive affect, sensitivity, and support, whereas structured communication includes positive reinforcement, adaptation of rules, and guidance (Fitness & Duffied, 2004; Koerner & Fitzpatrick, 2013; Stafford, 2013). In contrast, hostile/intrusive communication involves restrictive, over-controlled, and critical family interactions, while withdrawn communication involves disengaged and uninvolved interactions (Blechman, 1990; Fitness, 2013; Koerner & Fitzpatrick, 2013; Stafford, 2013). Hostile/intrusive communication involves excessive structure with a lack of warmth, whereas withdrawn communication represents a lack of warmth and structure.
Figure 1.
Framework of family communication in families affected by childhood chronic illness.
Literature Search
Consistent with the goals of a topical review, this paper was intended to explore the utility of a model of family communication by identifying findings from studies using codes that fit within this framework. However, a comprehensive systematic review of this literature was beyond the scope of the current review. To this end, 14 studies were identified that met the following criteria: use of direct observation; pediatric chronic illness (van der Lee et al., 2007) and healthy, typically developing comparison groups; and coding schemes consistent with this framework. Studies were identified from the literature through electronic databases (Psycinfo, Google Scholar) and relevant pediatric psychology journals. Search terms were: (specific disease [e.g., asthma] OR chronic illness OR pediatric) and (narrative OR illness narrative OR observation OR observed OR family functioning OR communication OR interaction) and (children OR adolescents). Time limits were not imposed simply because there were so few studies that undertook direct observation of family communication with healthy, typically developing controls. Searches were supplemented with studies cited by articles obtained and with articles already known to the authors. All 14 studies matched comparison groups on child age and at least one other demographic variable (e.g., gender, race/ethnicity, family income).
Applying this framework to pediatric studies required identifying individual codes from separate systems and placing them within the four categories used here. Regardless of how studies operationalized codes (macro vs. micro; family- or parent-level), similar codes were categorized based on the definitions of warm, structured, hostile/intrusive, or withdrawn communication (25% were double-coded and agreement was 90%). The purpose of this initial review is not to exhaustively categorize previous studies but to provide an initial summary of findings to guide future research in direct observation of family communication in pediatrics.
Findings for Positive, Warm, and Structured Communication
Table I highlights findings from studies with codes that could be classified within the broad category of positive communication because they include elements of both warm and structured communication. This includes Family Positive Statements (Carlson et al., 1994), Positive Responses (Chavez & Buriel, 1988), Family Communication (Janicke et al., 2005; Mitchell et al., 2004; Piazza-Waggoner et al., 2008; Spieth et al., 2001), Family Cohesion (Holmbeck et al., 2002), and Parent Positive Reinforcement (Siniatchkin et al., 2003). For example, the Family Communication code draws on positive affect, inclusion of family members, and clarity of messages, while the Positive Reinforcement code similarly taps expression of positive emotions, compliments, and support (Table I). In six of the eight studies highlighted in this section, including three studies with three different cystic fibrosis samples, one study with type 1 diabetes, one study with spina bifida, and one study with epilepsy, families demonstrated significantly lower levels of positive communication than healthy controls (one study found no difference and the other found a difference in the opposite direction; Table I).
Table I.
Communication in Families With a Child With a Chronic Illness Compared With Families of Healthy Children: Previous Findings for Positive, Warm, Structured, Negative, Hostile/Intrusive, and Withdrawn Patterns
| Study | Illness | Age | N | Observation task(s) | Coding system | Code and unit of analysis | Macro/ Micro | Effect | Finding |
|---|---|---|---|---|---|---|---|---|---|
| Positive communication (warm and structured) | |||||||||
| Carlson, Gesten, McIver, DeClue, & Malone et al., 1994 | T1D | 8–12 years | 20 per group | 3 problem-solving tasks: plan a weekend, discuss a problem identified by the family, diabetes-specific problem | Communication Coding System (COM; Carlson et al., 1994) | Family positive statements | Micro | − | Diabetes group significantly higher than TD group: F(1,38) = 4.18, p < .05 |
| Chavez & Buriel, 1988 | Epilepsy | 4–10 years | 29 epilepsy 24 healthy controls | Structured bean bag toss | McClintock & Moore (1981) coding system | Maternal positive responses | Micro | + | Epilepsy group significantly lower than TD group: F(2, 71) = 4.88, p < .01; post hoc test significant at p < .05 |
| Holmbeck Coakley, Hommeyer, Shapera, & Westhoven, 2002 | SB | 8–9 years | 68 per group | 3: unfamiliar board game, conflict task, structured family interaction task | Johnson & Holmbeck (1995) global coding system | Family cohesion | Macro | + | SB group significantly lower than TD group: F(1, 128) = 4.28, p < .05 |
| Janicke, Mitchell, , & Stark, 2005 | CF | 5–12 years | 28 per group | Family mealtime | MICS (Dickstein et al., 1994) | Family communication | Macro | + | CF group significantly lower than TD group: F(1, 54) = 13.86, p < .001 |
| Mitchell , Powers, Byars, Dickstein, & Stark, 2004 | CF | 7–35 months | 29 per group | Family mealtime | MICS (Dickstein et al., 1994) | Family communication | Macro | + | CF group significantly lower than TD group: F(1,64) = 4.06, p < .05 (ES d = 0.83) |
| Piazza-Wagoner et al., 2008 | T1D | 2–8 years | 33 per group | Family mealtime | MICS (Dickstein et al., 1994) | Family communication | Macro | + | T1D group significantly lower than TD group: t(64) = -2.0, p < .001 |
| Siniatchkin et al., 2003 | Asthma | M = 11 years(range un-known) | 20 per group | Puzzle task | Munich Training Model (MTM; Innerhofer, 1977) | Parent positive reinforcement | Micro | × | No significant difference between groups: (no other information provided) |
| Spieth et al., 2001 | CF | 2–6 years | 29 per group | Family mealtime | Mealtime Interaction Coding System (MICS; Dickstein et al., 1994) | Family communication | Macro | + | CF group significantly lower than TD group: F(1,56) = 10.26, p = .002 |
| Warm communication | |||||||||
| Janicke et al., 2005 | CF | 5–12 years | 28 per group | Family mealtime | MICS (Dickstein et al., 1994) | Family interpersonal involvement | Macro | + | CF group significantly lower than TD group: F(1, 54) = 15.96, p < .001 |
| Lennon , Murray, Bechtel, & Holmbeck, 2015 | SB | 5 Time Points (T1: 8–9 years; T5: 16–17 years) | 68 SB and 68 healthy controls (at T1) | 3: unfamiliar board game, conflict task, structured family interaction task | Johnson & Holmbeck (1995) global coding system | Parental acceptance | Macro | × | No significant difference between groups: (no other information provided) |
| Mitchell et al., 2004 | CF | 7–35 months | 29 per group | Family mealtime | MICS (Dickstein et al., 1994) | Family interpersonal involvement | Macro | + | CF group significantly lower than TD group: F(1,64) = 6.97, p = .01 (ES d = 0.81) |
| Piazza-Waggoner et al., 2008 | T1D | 2–8 years | 33 per group | Family mealtime | MICS (Dickstein et al., 1994) | Family interpersonal involvement | Macro | × | No significant difference between groups: (no other information provided) |
| Spieth et al., 2001 | CF | 2–6 years | 29 per group | Family mealtime | MICS (Dickstein et al., 1994) | Family interpersonal involvement | Macro | + | CF group significantly lower than TD group: F(1,56) = 16.56, p = .002 |
| Structured communication | |||||||||
| Chavez & Buriel, 1988 | Epilepsy | 4–10 years | 29 epilepsy 24 healthy controls | Structured bean bag toss | McClintock & Moore (1981) coding system | Maternal verbal directives | Micro | + | Epilepsy group significantly lower than TD group: F(2,71) = 4.86, p < .01 |
| Lennon et al., 2015 | SB | 5 Time Points (T1: 8–9 years; T5: 16–17 years) | 68 SB and 68 healthy controls (at T1) | 3: unfamiliar board game, conflict task, structured family interaction task | Johnson & Holmbeck (1995) global coding system | Mother and father behavioral control | Macro | -,× | SB group significantly higher than TD group on maternal but not paternal behavioral control at T3 (10–13 yrs), T4 (14–15 yrs, and T5 (16–17 yrs): F's = 7.12, 7.10, and 8.34 (respectively), p's < .05 |
| Negative communication (hostile/intrusive or withdrawn) | |||||||||
| Carlson et al., 1994 | T1D | 8–12 years | 20 per group | 3 Problem solving tasks: plan a weekend, discuss a family problem, diabetes specific problem | COM (Carlson et al., 1994) | Family negative statements | Micro | × | No significant difference between groups: (no other information) |
| Chavez & Buriel, 1988 | Epilepsy | 4–10 years | 29 epilepsy 24 healthy controls | Structured bean bag toss | McClintock & Moore (1981) coding system | Maternal negative responses | Micro | + | Epilepsy group significantly higher than TD group: F(2, 71) = 7.69, p < .01 |
| Siniatchkin et al., 2003 | Asthma | M = 11 Years (range unknown) | 20 per group | Puzzle task | MTM (Innerhofer, 1977) | Parent Blocking | Micro | + | Asthma group significantly higher than TD group: (statistics not reported; χ2 < .05) |
| Hostile/intrusive communication | |||||||||
| Hermanns, Florin, Dietrich, Rieger, & Hahlweg, 1989 | Asthma | 7–13 years | 25 asthma 25 healthy | Problem discussion and resolution | KPI Interaction Coding System (Hahlweg et al., 1984) | Maternal criticism | Micro | + | Asthma group significantly higher than TD group: t(37) = 2.61, p < .05 |
| Lennon et al., 2015 | SB | 5 Time Points (T1: 8–9 years; T5: 16–17 years) | 68 SB and 68 healthy controls (at T1, ages 8–9) | 3: unfamiliar board game, conflict task, structured family interaction task | Johnson & Holmbeck (1995) global coding system | Mother and father Psychological control | Macro | +,× | SB group significantly higher than TD group on maternal but not paternal psychological control at T1 (8–9 years): F(3, 127) = 3.39, p < .05 |
| Schöbinger, Florin, Zimmer, Lindemann, & Winter, 1992 | Asthma | 6–13 years | 24 asthma 22 healthy | Problem discussion and resolution | KPI Interaction Coding System (Hahlweg et al., 1984) | Paternal criticism | Macro | + | Asthma group significantly higher than TD group: F(1,44) = 33.68, p < 0.001 (ES d = 1.72) |
| Schöbinger, Florin, Reichbauer, Lindemann, & Zimmer, 1993 | Asthma | 6–13 years | 24 asthma 23 healthy | Problem discussion and resolution | KPI Interaction Coding System (Hahlweg et al., 1984) | Maternal criticism | Micro | + | Asthma group significantly higher than TD group: F(1,44) = 17.0, p < .0001 (ES d = 1.39) |
| Tuminello, Holmbeck, & Olson, 2012 | SB | 14–15 years | 61 SB, 65 control | 2: unfamiliar board game and conflict task | Johnson & Holmbeck (1995) global coding system | Mother and father intrusiveness | Macro | +,+ | SB group significantly higher than TD group on maternal and paternal intrusiveness: t(105) = 4.21, p < .001; t(71) = 3.20, p = .00 |
| Withdrawn communication | |||||||||
| Lennon et al., 2015 | SB | 5 Time Points (T1: 8–9 years; T5: 16–17 yrs) | 68 SB and 68 healthy controls (at T1) | 3: unfamiliar board game, conflict task, structured family interaction task | Johnson & Holmbeck (1995) global coding system | Child positive engagement (reverse) | Macro | + | SB group significantly lower child engagement than TD group at every time point: F's ranged 40.98–4.60, p's < .05 |
| Seiffge-Krenke, 2002 | T1D | 12–16 years | 58 T1D, 76 control | Plan a fictitious 3-week vacation together | Condon, Cooper, & Grotevant (1983) coding system | Father contributions (reverse) | Micro | + | T1D group significantly lower father involvement than TD group: F's ranged 1.88–3.71, p's < .05 |
Note. SB = spina bifida; T1D = type 1 diabetes; TD = typically developing; ES = effect size in Cohen’s d.
Unit of analysis: Family = both parent and child contributions taken into account for scoring; Mother/Maternal = only mother’s contributions taken into account for scoring; Father/Paternal = only father’s contributions taken into account for scoring.
+Significant finding such that chronic illness group demonstrates lower positive or higher negative communication.
−Significant finding such that chronic illness group demonstrates higher positive or lower negative communication.
×No significant difference between groups.
Fewer studies have examined either warm or structured communication separately. Regarding warm communication, Interpersonal Involvement (Janicke et al., 2005; Mitchell et al., 2004; Piazza-Wagoner et al., 2008; Spieth et al., 2001), which draws on empathic involvement from family members, and parental Acceptance (Lennon et al., 2015), which combines individual codes such as listens to others, humor and laughter, open or warm, and supportiveness, both fit in this category. Similarly, maternal Verbal Directives (Chavez & Buriel, 1988), such as instructions and explanation, and parental Behavioral Control (Lennon et al., 2015), tapping parental power and structuring of the task, both represent structured communication, as they examine elements of reinforcement and guidance without either overt negative tone or warmth. Four of five studies in the warm category and one of two studies in the structured category found lower levels compared with controls (Table I).
Findings for Negative, Hostile/Intrusive, and Withdrawn Communication
Table I highlights findings with codes classified as overall negative, capturing hostile/intrusive or withdrawn communication. This includes maternal Negative Responses (Chavez & Buriel, 1988), such as expressions of displeasure with the child; family Negative Statements (Carlson et al., 1994), such as insults, disagreements, refusals, and criticism; and parent Blocking (Siniatchkin et al., 2003), such as criticism, ignoring, and interrupting. Of the three studies in this category, two found higher levels of negative communication in families of children with epilepsy and asthma compared with families of healthy children (Table I).
Regarding hostile/intrusive communication, previous studies in pediatrics have focused on parent-level communication. This includes parent Criticism (Hermanns et al., 1989; Schöbinger Florin, Zimmer, Lindemann, & Winter, 1992; Schöbinger, Florin, Reichbauer, Lindemann, & Zimmer, 1993), including critical comments and accusations; parent Psychological Control (Lennon et al., 2015), including pressuring others to agree, overprotectiveness, and unable to tolerate differences and disagreements; and parent Intrusiveness (Tuminello, Holmbeck, & Olson, 2012), which includes prevention of independent behavior, infantilization, and excessive control. Pediatric studies that have examined withdrawn communication have focused on first coding engagement on a continuum (with high scores indicating greater engagement or involvement), then examining the reverse. For example, Seiffge-Krenke (2002) measured Contributions by fathers, including suggestions, clarifications, and explanations; similarly, Lennon et al. (2015) measured child Positive Engagement, including clarity, listening, involvement, and explanation codes. Across three studies of children with asthma, two of spina bifida, and one of type 1 diabetes, findings indicate significantly higher levels of hostile/intrusive and withdrawn communication compared with controls (Table I).
Summary of Findings Within Framework
Although not completely uniform, these results provide initial evidence that observed communication may differ in families of children with chronic illnesses, such that families demonstrate lower levels of warm and structured communication and higher levels of hostile/intrusive and withdrawn communication compared with healthy controls. Of the 28 effects examined across 14 studies, 20 found poorer communication in families with a child with a chronic illness relative to controls. Most studies are notable for relatively small sample sizes (<30 per group), suggesting that group differences were sufficiently large in magnitude to be detected in studies with relatively low power.
Despite the pattern of effects observed across these 14 studies, a larger body of evidence, with multiple studies in each category, is needed before a future meta-analysis can quantify effects. However, this synthesis is provocative for future research. The above studies included pediatric illnesses that are chronic in nature, requiring careful medical monitoring of often complex medical regimens across the life span (Stark, 2013; Quittner et al., 2008). Potential mechanisms of suboptimal communication may include family-level stress related to disruptions in normal roles and routines, increased financial burdens, parent and child psychological distress, as well as issues surrounding medical adherence and responsibility. A family communication framework that emphasizes dimensions of warmth and control can be used to further examine factors that contribute to impaired family communication.
Limitations
Given the small number of studies reviewed, there are limitations to note. Several studies used codes that fit in multiple categories and were cited more than once (Lennon et al. 2015; Spieth et al., 2001), so these samples had greater influence. There was also considerable variability among studies. Samples included a wide range of ages, from families with toddlers (Spieth et al., 2001) to families with older adolescents (Tuminello et al., 2012). While sampling a wide age range is a strength of the review, more research is needed to explore possible age effects. Race and ethnicity should also be explored further; although Chavez and Buriel (1988) specifically studied Mexican American samples, most studies included samples that were predominantly Caucasian. There was also variability in unit of analysis, as some studies coded the entire family, while others coded a parent or child (Table I). It is possible that different family members may simultaneously engage in different communication patterns such that unit of analysis impacts results; future reviews could parse differences among contributions of each family member or focus on transactional, reciprocal influences (Beveridge & Berg, 2007). Discussion topic also varied between studies, and it is possible that communication patterns differ when discussing illness-specific topics compared with general family discussions (Maharaj, Rodin, Connolly, Olmsted, & Daneman, 2001). Further, not enough studies are included to indicate if communication differs among illness groups.
Due to the small number of studies, we did not include a date limit on literature searches, which introduces potential cohort differences and may have impacted findings, especially given the increase in psychology’s role in pediatric settings. Importantly, studies included in this review were limited to those with healthy, typically developing control groups. This reduced the number of disease groups included in the review (e.g., studies with direct observation in pediatric cancer samples have not yet included healthy controls) and the within-group analyses conducted. Indeed, only four studies in this review examined the relation between communication and health variables and found inconsistent relations between communication and disease severity (Carlson et al., 1994; Hermanns et al., 1989; Schöbinger et al., 1992, 1993) and executive function (Tuminello et al., 2012). A future review could examine the relation between communication and health variables in single samples within this framework. This is an exciting area for future research and is discussed further below.
Conclusions and Future Directions
Findings from this review suggest that comparisons across studies that have taken diverse approaches to quantifying observed family communication are possible with a unifying framework that accommodates multiple coding systems. A future review could use a similar approach to examine studies that used self-report questionnaires of family communication to better understand how findings across methodologies converge or diverge. While studies reviewed here have begun to uncover differences in family communication between chronic illness and typically developing pediatric samples, the next step will be to better understand demographic and illness characteristics of families with suboptimal and optimal communication as well as relations between family communication and child and family functioning. Direct observation is an important methodological approach in the field (Wysocki, 2015), and we highlight several avenues for future research in family communication and the utility of a unifying framework.
First, future studies could examine family and child variables related to family communication within chronic illness samples. These factors may include illness onset (i.e., congenital vs. childhood-onset), severity, child sex or age, family race/ethnicity, and socioeconomic status. Age or developmental stage may be particularly important to consider in the context of family communication. Because normative adolescent strivings for autonomy and control are at odds with dependence imposed by a chronic illness, differences in communication (e.g., greater harsh/intrusive communication in chronic illness samples) may become more pronounced during this developmental period. Longitudinal, case-controlled research will be critical for determining transitional periods when differences in communication are likely to emerge (e.g., adolescence; Lennon et al., 2015).
Second, it will be important to systematically evaluate the relation between family communication patterns and indicators of psychosocial functioning and health (e.g., parent and child distress and medical adherence) within pediatric samples. The communication framework applied here may be helpful to this end. For example, while hostile/intrusive communication has been linked to greater child distress in both pediatric and typically developing samples (Ge, Best, Conger, & Simon, 1996; Holmbeck et al., 2002), these styles of communication may be adaptive, at least in the short term, for helping children achieve medical adherence. In addition, parental distress has been linked to lower levels of warm communication in families of children with asthma and type 1 diabetes (Celano et al., 2008; Jaser & Grey, 2010) and higher levels of hostile/intrusive and withdrawn communication families of children with asthma and cancer (Celano et al., 2008; Murphy et al., in press). Similarly, hostile/intrusive communication has been linked to greater child distress in asthma, type 1 diabetes, and spina bifida samples (Holmbeck et al., 2002; Jaser & Grey, 2010; Wood et al., 2008), and studies suggest that parent communication may mediate the relation between symptoms of parent and child distress (Murphy et al., in press; Wood et al, 2008). Longitudinal research is needed to clarify the direction of the relations between family communication and outcomes over time.
The results of this review also have several important clinical implications. First, clinicians should attend to potentially maladaptive family communication patterns in pediatric populations. In-clinic consultations may involve observing interactions among family members to identify potentially impaired communication patterns (e.g., child appears withdrawn and does not contribute to conversation with caregivers). Because research-validated paradigms of direct observation of families are often too cumbersome for routine clinic visits, a high priority for future research would involve the development and validation of a brief family communication observation checklist to be used during in-clinic consultations. In addition, previous research has indicated that parent–child interaction and behavioral family systems therapies can be applied to specific pediatric populations (e.g., diabetes) to target family communication patterns. These interventions have resulted in significant reductions of negative communication and increases in positive communication and accompanying improvements in health status (Cohen, Heaton, Ginn, & Eyberg, 2011; Wysocki et al., 2008). Given that a range of pediatric illnesses may be at higher risk for impaired family communication, future research may attempt to develop transdiagnostic interventions that can be applied to multiple illness groups. Future theoretically derived research is also needed to understand how family communication can be leveraged to improve adaptation to illness. Interventions that aim to effect changes in outcomes such as medical adherence and child distress should not only target family communication, but track changes in observed family communication in relation to outcomes over time.
In summary, direct observation of family communication in pediatric populations provides a unique window into family processes, as families attempt to adapt to the substantial demands of caring for a child with a chronic illness. Results from this initial topical review, using a unifying framework of family communication, suggest that communication may differ in families of children with chronic illnesses. This framework may be used in future studies that examine mechanisms and consequences of impaired family communication as well as interventions to improve communication and promote adaptation to pediatric chronic illness.
Funding
This work was supported by a grant from the National Cancer Institute (R01CA118332) and a gift from Patricia and Rodes Hart. There are no financial or other relationships that would lead to a conflict of interest.
References
- Allen J. P., Hauser S. T., Bell K. L., O’connor T. G. (1994). Longitudinal assessment of autonomy and relatedness in adolescent family interactions as predictors of adolescent ego development and self-esteem. Child Development, 65, 179–194. [DOI] [PubMed] [Google Scholar]
- Baumrind D. (1968). Authoritarian vs. authoritative parental control. Adolescence, 3, 255–272. [Google Scholar]
- Beveridge R. M., Berg C. A. (2007). Parent–adolescent collaboration: An interpersonal model for understanding optimal interactions. Clinical Child and Family Psychology Review, 10, 25–52. [DOI] [PubMed] [Google Scholar]
- Blechman E. A. (1990). A new look at emotions and the family: A model of effective family communication In Blechman E. (Ed.), Emotions and the family (pp. 201–224). Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Butler J. M., Skinner M., Gelfand D., Berg C. A., Wiebe D. J. (2007). Maternal parenting style and adjustment in adolescents with type I diabetes. Journal of Pediatric Psychology, 32, 1227–1237. [DOI] [PubMed] [Google Scholar]
- Carlson K. P., Gesten E. L., McIver L. S., DeClue T., Malone J. (1994). Problem solving and adjustment in families of children with diabetes. Children's Health Care, 23, 193–210. [Google Scholar]
- Chorney J. M., McMurtry C. M., Chambers C. T., Bakeman R. (2015). Developing and modifying behavioral coding schemes in pediatric psychology: A practical guide. Journal of Pediatric Psychology, 40(1), 154–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celano M., Bakeman R., Gaytan O., Smith C. O., Koci A., Henderson S. (2008). Caregiver depressive symptoms and observed family interaction in low‐income children with persistent asthma. Family Process, 47, 7–20. [DOI] [PubMed] [Google Scholar]
- Chavez J. M., Buriel R. (1988). Mother-child interactions involving a child with epilepsy: A comparison of immigrant and Native-born Mexican Americans. Journal of Pediatric Psychology, 13, 349–361. [DOI] [PubMed] [Google Scholar]
- Cohen E., Kuo D. Z., Agrawal R., Berry J. G., Bhagat S. K., Simon T. D., Srivastava R. (2011). Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics, 127, 529–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen M. L., Heaton S. C., Ginn N., Eyberg S. M. (2011). Parent–child interaction therapy as a family-oriented approach to behavioral management following pediatric traumatic brain injury: A case report. Journal of Pediatric Psychology, 37, 1–11. [DOI] [PubMed] [Google Scholar]
- Condon S. L., Cooper C. R., Grotevant H. D. (1983). Manual for the analysis of family discourse. Unpublished manuscript, University of Texas at Austin. [Google Scholar]
- Dickstein S., Hayden L. C., Schiller M., Seifer R., San Antonio W. (1994). Providence Family Study mealtime family interaction coding system: Adapted from the McMaster clinical rating scale. East Providence, RI: E. P. Bradley Hospital. [Google Scholar]
- Drotar D. (1981). Psychological perspectives in chronic childhood illness. Journal of Pediatric Psychology, 6, 211–228. [DOI] [PubMed] [Google Scholar]
- Feeney J. A., Noller P. (2013). Perspectives on studying family communication. Multiple methods and multiple sources In Vangelisti A. L. (Ed.), Routledge Handbook of Family Communication (11–28). New York: Routledge. [Google Scholar]
- Fitness J., Duffied J. (2003). Emotion and communication in families In Vangelisti A. L. (Ed.), Handbook of family communication (pp. 473–494). New York, NY: Routledge. [Google Scholar]
- Fitzpatrick M., Marshall L. J. (1996). The effect of family communication environments on children’s social behavior during middle childhood. Communication Research, 23, 379–407. [Google Scholar]
- Ge X., Best K. M., Conger R. D., Simons R. L. (1996). Parenting behaviors and the occurrence and co-occurrence of adolescent depressive symptoms and conduct problems. Developmental Psychology, 32, 717–731. [Google Scholar]
- Hahlweg K., Reisner L., Kohli G., Vollmer M., Schindler L., Revenstorf D. (1984). Kategoriensystem fur partnerschaftliche interaktion [Development and validity of a new system to analyze interpersonal communication] In Hahlweg K., Jacobson N. S. (Eds.), Marital interaction: Analysis and modification (pp. 182–198). New York, NY: Guildford. [Google Scholar]
- Hermanns J., Florin I., Dietrich M., Rieger C., Hahlweg K. (1989). Maternal criticism, mother-child interaction, and bronchial asthma. Journal of Psychosomatic Research, 33, 469–476. [DOI] [PubMed] [Google Scholar]
- Holmbeck G. N., Coakley R. M., Hommeyer J. S., Shapera W. E., Westhoven V. C. (2002). Observed and perceived dyadic and systemic functioning in families of preadolescents with spina bifida. Journal of Pediatric Psychology, 27, 177–189. [DOI] [PubMed] [Google Scholar]
- Innerhofer P. (1997). Das Muünchener Trainingsmodell: Beobachtung, Interaktionsanalyse, Verhaltensänderung. Berlin: Springer Verlag. [Google Scholar]
- Janicke D. M., Mitchell M. J., Stark L. J. (2005). Family functioning in school-age children with cystic fibrosis: An observational assessment of family interactions in the mealtime environment. Journal of Pediatric Psychology, 30, 179–186. [DOI] [PubMed] [Google Scholar]
- Jaser S. S., Grey M. (2010). A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. Journal of Pediatric Psychology, 35, 738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S. Z., Holmbeck G. N. (1995). Manual for OP coding system. Unpublished manual, Loyola University of Chicago. [Google Scholar]
- Kiesler D. J. (1996). Contemporary interpersonal theory and research: Personality, psychopathology, and psychotherapy. New York, NY: John Wiley and Sons. [Google Scholar]
- Koerner A. F., Fitzpatrick M. A. (2013). Communication in intact families In Vangelisti A. L. (Ed.), Routledge handbook of family communication (pp. 129–144). New York, NY: Routledge. [Google Scholar]
- Lennon J. M., Murray C. B., Bechtel C. F., Holmbeck G. N. (2015). Resilience and disruption in observed family interactions in youth with and without Spina Bifida: An eight-year, five-wave longitudinal study. Journal of Pediatric Psychology, 40, 943–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maharaj S., Rodin G., Connolly J., Olmsted M., Daneman D. (2001). Eating problems and the observed quality of mother–daughter interactions among girls with type 1 diabetes. Journal of Consulting and Clinical Psychology, 69, 950.. [PubMed] [Google Scholar]
- McClintock E., Moore J. W. (1981). Interactional styles of immigrant and later generation Mexican American mother-child pairs. Paper presented at the Second Symposium on Chicano Psychology, Riverside, CA.
- Mitchell M. J., Powers S. W., Byars K. C., Dickstein S., Stark L. J. (2004). Family functioning in young children with cystic fibrosis: Observations. Of Interactions at Mealtime. Journal of Developmental & Behavioral Pediatrics, 25, 335–346. [DOI] [PubMed] [Google Scholar]
- Murphy L. K., Rodriguez E., Saylor M., Dunn M., Gerhardt C. A., Vannatta K., Saylor M., Compas B. E. (in press). Longitudinal associations among maternal communication and adolescent posttraumatic stress symptoms after cancer. Psychooncology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson D., Russel C. S., Sprenkle D. J. (Eds.) (1989). Circumplex model: Systematic assessment and treatment of families. Binghamton, NY: Hawthorne Press. [Google Scholar]
- Olvera N., Power T. G. (2010). Brief report: Parenting styles and obesity in Mexican American children: A longitudinal study. Journal of Pediatric Psychology, 35, 243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza-Waggoner C., Modi A. C., Powers S. W., Williams L. B., Dolan L. M., Patton S. R. (2008). Observational assessment of family functioning in families with children who have type 1 diabetes mellitus. Journal of Developmental and Behavioral Pediatrics, 29, 101–105. [DOI] [PubMed] [Google Scholar]
- Quittner A. L., Modi A. C., Lemanek K. L., Ievers-Landis C. E., Rapoff M. A. (2008). Evidence-based assessment of adherence to medical treatments in pediatric psychology. Journal of Pediatric Psychology, 33(9), 916–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan R. M., Deci E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55, 68.. [DOI] [PubMed] [Google Scholar]
- Schöbinger R., Florin I., Reichbauer M., Lindemann H., Zimmer C. (1993). Childhood asthma: Mothers' affective attitude, mother-child interaction and children's compliance with medical requirements. Journal of Psychosomatic Research, 37, 697–707. [DOI] [PubMed] [Google Scholar]
- Schöbinger R., Florin I., Zimmer C., Lindemann H., Winter H. (1992). Childhood asthma: Paternal critical attitude and father-child interaction. Journal of Psychosomatic Research, 36, 743–750. [DOI] [PubMed] [Google Scholar]
- Seiffge-Krenke I. (2002). “Come on, say something, dad!”: Communication and coping in fathers of diabetic adolescents. Journal of Pediatric Psychology, 27, 439–450. [DOI] [PubMed] [Google Scholar]
- Siniatchkin M., Kirsch E., Arslan S., Stegemann S., Gerber W. D., Stephani U. (2003). Migraine and asthma in childhood: Evidence for specific asymmetric parent–child interactions in migraine and asthma families. Cephalalgia, 23, 790–802. [DOI] [PubMed] [Google Scholar]
- Spieth L., Stark L., Mitchell M., Schiller M., Cohen L., Mulvihill M., Hovell M. F. (2001). Observational assessment of family functioning at mealtime in preschool children with cystic fibrosis. Journal of Pediatric Psychology, 26, 215–224. [DOI] [PubMed] [Google Scholar]
- Stafford L. (2013). Parent and sibling interactions during middle childhood In Vangelisti A. L. (Ed.), Routledge handbook of family communication (pp. 256–270). New York, NY: Routledge. [Google Scholar]
- Stamp G. H. (2004). Theories of family relationships and a family relationships theoretical model In Vangelisti A. L. (Ed.), Handbook of family communication (pp. 1–30). New York, NY: Routledge. [Google Scholar]
- Stamp G. H., Shue C. K. (2013). Twenty years of family research published in communication journals: A review of the perspectives, theories, concepts, and contests In Vangelisti A. L. (Ed.), Routledge handbook of family communication (pp. 11–28). New York, NY: Routledge. [Google Scholar]
- Stark L. J. (2013). Introduction to the special issue on adherence in pediatric medical conditions. Journal of Pediatric Psychology, 38(6), 589–594. [DOI] [PubMed] [Google Scholar]
- Stepansky M. A., Roache C. R., Holmbeck G. N., Schultz K. (2009). Medical adherence in young adolescents with spina bifida: Longitudinal associations with family functioning. Journal of Pediatric Psychology, 35, 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuminello E. R., Holmbeck G. N., Olson R. (2012). Executive functions in adolescents with spina bifida: Relations with autonomy development and parental intrusiveness. Child Neuropsychology, 18, 105–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Lee J. H., Mokkink L. B., Grootenhuis M. A., Heymans H. S., Offringa M. (2007). Definitions and measurement of chronic health conditions in childhood: A systematic review. JAMA, 297, 2741–2751. [DOI] [PubMed] [Google Scholar]
- Wood B. L., Lim J., Miller B. D., Cheah P., Zwetsch T., Ramesh S., Simmens S. (2008). Testing the biobehavioral family model in pediatric asthma: Pathways of effect. Family Process, 47, 21–40. [DOI] [PubMed] [Google Scholar]
- Wysocki T. (2015). Introduction to the special issue: Direct observation in pediatric psychology research. Journal of Pediatric Psychology, 40, 1–7. [DOI] [PubMed] [Google Scholar]
- Wysocki T., Harris M. A., Buckloh L. M., Mertlich D., Lochrie A. S., Taylor A., Sadler M., White N. H. (2008). Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behavior Therapy, 39, 33–46. [DOI] [PubMed] [Google Scholar]