Abstract
Background
Despite clear evidence demonstrating the influence of social determinants on health, whether and how clinicians should address these determinants remain unclear. We aimed to understand primary care clinicians’ experiences of administering a social needs screening instrument.
Methods
Using a prospective, observational design, we identified patients living in communities with lower education and income seen by 17 clinicians from 12 practices in northern Virginia. Before office visits, patients completed social needs surveys, which probed about their quality of life, education, housing, finances, substance use, transportation, social connections, physical activity, and food access. Clinicians then reviewed the completed surveys with patients. Concurrently, clinicians participated in a series of learning collaboratives to consider how to address social needs as part of care and completed diary entries about how knowing the patient’s social needs influenced care after seeing each patient.
Results
Out of a total of 123 patients, 106 (86%) reported a social need. Excluding physical activity, 71% reported a social need, although only 3% wanted help. Clinicians reported that knowing the patient had a social need changed care delivery in 23% of patients and helped improve interactions with and knowledge of the patient in 53%. Clinicians reported that assessing social needs is difficult and resource intensive and that there were insufficient resources to help patients with identified needs.
Conclusions
Clinicians reported that knowing patients’ social needs changed what they did and improved communication for many patients. However, more evidence is needed regarding the benefit of social needs screening in primary care before widespread implementation. (J Am Board Fam Med 2018; 31:351–363.)
Keywords: Needs Assessment, Primary Health Care, Prospective Studies, Quality of Life, Surveys and Questionnaires, Virginia
Social determinants of health (SDH) have a demonstrable influence on health outcomes.1–6 Defined as the nonclinical factors that affect health, SDH includes personal resources, such as education and income, and social environments in which people grow up, live, and work.7 Growing research is showing that SDH plays a far greater role on health outcomes than medical care.8–13 However, the majority of resources in the United States is disproportionately spent on direct medical care instead of public health and social determinants.14
The National Academy of Medicine (NAM), the Centers for Medicare and Medicaid Services, and the World Health Organization have called for the integration of primary care and public health to address SDH.15–18 Aiming to provide comprehensive care for individuals, families and communities19, primary care clinicians could potentially play a large role in shaping how SDH are screened for and addressed within health care settings.20–22 The concept of integrating primary care and public health is not new. In the 1940s, community-oriented primary care concepts were developed with this goal of integrating public health with primary care.23–25 However, successful implementation of this integration has not been achieved at scale. To bolster the most recent momentum to address SDH in primary care, NAM released a consensus statement recommending that 12 SDH domains be routinely collected and made available in electronic health records.26,27 The domains include ethnicity/race, tobacco use, alcohol use, residential address, educational attainment, financial resources, stress, depression, physical activity, social isolation, intimate partner violence, and neighborhood median household income.
Several pilot studies have been published to assess how primary care clinicians might collect SDH information. These studies have demonstrated that it is feasible for primary care clinicians to screen for SDH in a variety of primary care settings by using a variety of mechanisms.28–31 However, it is unclear whether knowing the social needs of patients could help clinicians address gaps in care, adapt care for patients, and improve morbidity and mortality. Furthermore, adding more required data collection for primary care clinicians could be burdensome without any benefit32–34 if clinicians are not able to address social needs.35,36 Fundamentally, whether addressing SDH should be within the domain of the health care delivery system remains an unanswered question.21,36
To date, most studies examining SDH screening have taken place in underserved settings.28–30 Although NAM has called for the routine collection of SDH information in clinical practice, concerns have been raised over the burden required, as well as the absence of feasibility assessments or evidence of benefit in more affluent neighborhoods. In a recent editorial, Westfall37 argued that practices in all communities should focus resources on what he calls “cold spots,” or neighborhoods with fewer opportunities. This approach could particularly be useful in more affluent communities. In a parallel study, we demonstrate several means of calculating cold spots within a community38 and then used these definitions to select patients for our intervention in an affluent community.
In our study, we sought to address how primary care clinicians might screen for and consider the impact of SDH by piloting a social needs screening instrument in primary care for patients who might be at greater risk based on geospatial factors. Our objective was to understand primary care clinicians’ experiences with and perspectives on administering the social needs screening instrument, as well as how they might use the information in routine practice.
Methods
Between April 2016 and December 2016, we used a mixed methods design to prospectively evaluate clinicians’ experiences of administering a social needs screening instrument in primary care practices. Clinicians participated in a series of learning collaboratives, while a small subset of their patients completed a social needs survey. The study was approved by the Virginia Commonwealth University Institutional Review Board.
Setting and Participants
Seventeen primary care clinicians from 12 practices in Northern Virginia within one health system participated. The practices function independently for staffing, clinical, and business activities, but they do share an electronic health record and collaborate for population management activities, including work through an accountable care organization and a centralized care management team that clinicians can refer patients to for additional help. Located within a 45-mile radius, the practices mainly care for patients in Fairfax, Loudoun, Prince William, Fauquier, and Arlington counties. These counties collectively have among the highest average income within the United States.39 The practices jointly serve a patient population that is predominantly commercially insured (96.0%), generally more affluent, and speak English as their preferred language (84.9%). To recruit clinicians, we emailed all primary care clinicians from the 12 practices.
Intervention
Using Esri ArcMap 10.3.1, we geocoded all patients seen in the participating practices in the past year to their census tract of residence based on their reported residential address. We then identified all regional census tracts in the lowest quartile of life expectancy, poverty, education, and a validated social deprivation index (SDI), which we defined as “cold spots.” Life expectancy data were extracted from the Virginia Department of Health, Division of Vital Records40, whereas poverty, education, and SDI were measured using the 2010 American Community Survey data.41 We assessed poverty by calculating the percentage of the population earning less than 200% of the federal poverty level and assessed low educational attainment by the percentage who have not received a high school diploma or passed the General Education Development test. Our selected SDI, which is scored from 0 to 100 with higher numbers indicating higher deprivation, is a composite measure of social and material deprivation, which includes education, crowding, transportation, employment, poverty, housing, and family structure.42 This methodology and its limitations are further described in an article by Liaw et al.38
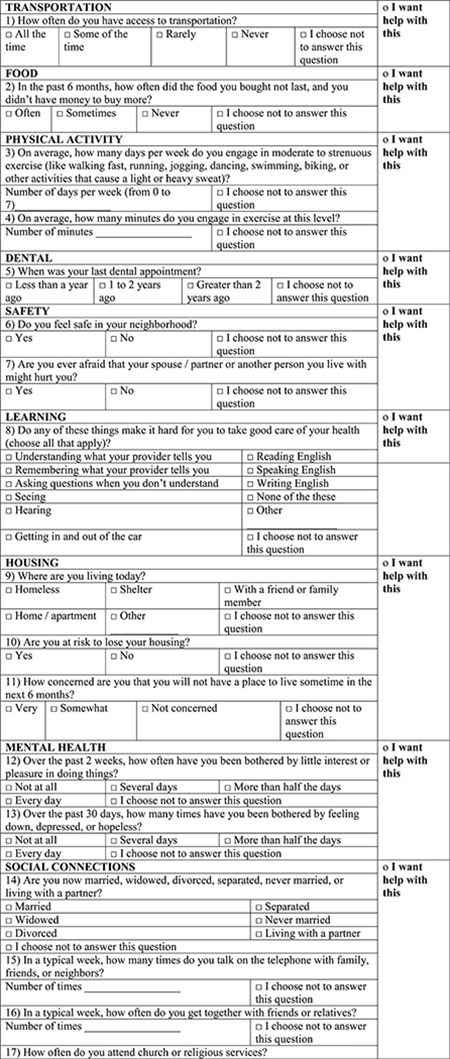
If a patient living in a cold spot had an appointment with 1 of the 17 participating clinicians, we administered a social needs survey to the patient during his or her scheduled visit before seeing the clinician. We continued to identify patients for clinicians until 10 patients were reached or the end of our study period. We excluded patients who were under the age of 18 years and who were unable to read English. Adapted from NAM’s social needs measures27 and supplemented with additional questions from the Hennepin County Lifestyle survey43, the patient survey included questions on transportation, food access, physical activity, dental health, safety, education, housing, mental health, social connections, substance use, finances, employment, and overall quality of life (see Appendix A). In addition to answering questions to assess whether patients had a social need in each specific domain, patients were also asked whether or not they wanted help with each domain. The completed survey was then reviewed with the clinician during their visit.
Clinicians then completed a structured diary entry for each patient who completed the social needs survey. Collected on-line within a week after the clinical encounter with each patient to limit recall bias, the diary entry included both closed-ended and open-ended prompts that queried about changes in care and knowledge of the patient as a result of the social needs survey and experiences of collecting the survey and addressing needs from the survey (see Appendix B for survey).
The clinicians also participated concurrently in a series of 4 learning collaboratives in which participants not only provided feedback about their experiences and perspectives but also learned about social needs screening from the facilitator and from other learning collaborative members.44–46 In addition to the 17 clinicians, 3 patient representatives from the practices’ existing patient advisory council, 3 selected patients living in cold spots, 3 practice administrators, and 6 population health managers were divided into 3 groups based on geographic location of the practice to participate in these learning collaboratives. During these collaboratives, we shared health outcomes data from cold spots to elicit reactions and obtained feedback on ways to collect the social needs surveys. The first 2 collaboratives occurred before fielding the social needs survey so that clinicians shared their beliefs about the value of collecting SDH and provided suggestions to each other on ways to collect and address SDH as part of their care. In the last 2 collaboratives, which occurred after fielding the survey, clinicians shared experiences of collecting the survey and addressing identified needs from the survey. They also provided suggestions on how SDH might be integrated into primary care in the future.
We did not offer any financial incentives to study practices, participating clinicians, or patients completing surveys.
Data Collection
We used 3 sources for outcomes: learning collaborative transcripts, clinician diary entries, and patient social needs surveys. Learning collaboratives were recorded, transcribed, and coded. Clinician diary entries were reviewed and coded. The social needs surveys that were completed by the patients were also collected.
Statistical Analysis
We used descriptive statistics to calculate percentages and counts from closed-ended questions from the clinician diary entries. We also calculated percentages and counts of domains in which patients identified social needs and for which patients asked for assistance. The software Stata 14.2 was used for all analyses.
Qualitative Analysis
Three reviewers (ST, WL, and AK) used a template approach, which involves the directed coding of collected qualitative material based on a code manual47, to capture facilitators, barriers, and suggestions to improve collection of social needs and address identified social needs. The 2 learning collaboratives that occurred before the survey administration and the 2 that occurred after the survey administration were included in the analysis; this allowed for comparison of pre-survey and postsurvey administration views from clinicians. Two reviewers coded each transcript independently. Merged data were reviewed for discrepancies in coding and discussed by all 3 reviewers until reaching a consensus. Themes were then identified, with each theme’s strength demonstrated by consistency of expression, frequency of associated coding instances, and participant agreement.
Results
Seventeen clinicians participated and 100% completed the study. A total of 215 eligible patients in the care of the 17 clinicians were identified. Of these, 123 patients completed the social needs survey and reviewed the results with their clinician. Of the 92 who did not participate, 22 declined, 13 did not show up for their appointment, 23 canceled their appointment, 18 did not participate due to clinic logistics (eg, time constraints, misplaced survey, and neglected to administer), 1 was not able to read in English, and 15 did not participate for other unknown reasons.
Social Needs Survey
The social needs survey is provided in Table 1. We found that 86.2% of patients screened positive in at least 1 of the 16 domains. However, only 3.3% of patients wanted help in any domains. The most common domains for positive screens were physical activity (53.0%), dental (25.2%), and alcohol use (14.6%). When we excluded physical activity, 70.7% of patients screened positive in at least 1 domain and 3.3% wanted help in any domain. The least common domains for positive screens were social connections (1.6%), safety (2.4%), and education (2.4%). There was a significant range in how often patients wanted help when they screened positive with 100% of patients screening positive for safety asking for help but only 3.0% of patients screening positive for physical activity asking for help.
Table 1.
Patient Responses to Social Needs Survey (n = 123)
| Domain | Descriptor of Positive Screen | Percentage with Positive Screen | Percentage Asking for Help |
|---|---|---|---|
| Physical activity | Less than 150 minutes of strenuous exercise per week | 53.0 | 1.6 |
| Dental | Last dental appointment ≥1 year ago | 25.2 | 1.6 |
| Alcohol use | AUDIT-C* score ≥3 in women or ≥4 in men | 14.6 | 0.8 |
| Overall health | Self-rated health as “fair” or “poor”† | 13.0 | 0.0 |
| Tobacco use | Current use of cigarettes | 12.2 | 0.8 |
| Finances | Lack of medical insurance, concern for losing medical insurance, or problems paying for medications, clinic visits or supplies | 11.4 | 0.0 |
| Work | Currently unemployed, receiving disability, or other government assistance | 11.4 | 0.0 |
| Learning | Problems with understanding, remembering, seeing, hearing, and English literacy | 10.6 | 0.8 |
| Mental health | PHQ-2‡ score ≥3 | 10.6 | 0.8 |
| Food | Insufficient food and lack of money to buy more | 7.3 | 1.6 |
| Drugs | Any use of illicit drugs or prescription drugs for nonmedical purposes | 7.3 | 0.0 |
| Transportation | Problems with access to transportation | 4.9 | 0.8 |
| Housing | Currently homeless or living in shelter; currently at risk of losing housing; or concern that will lose housing in next 6 months | 4.1 | 0.8 |
| Education | Did not complete high school | 2.4 | 1.6 |
| Safety | Feeling unsafe in neighborhood or concern that spouse/partner might hurt them | 2.4 | 2.4 |
| Social connections | Limited interaction with family, friends, and neighbors | 1.6 | 0.8 |
| Overall with at least one domain | 86.2 | 3.3 | |
| Overall with at least one domain with physical activity excluded | 70.7 | 3.3 |
Note: see Appendix A for full social needs survey.
AUDIT-C is a 3-item validated alcohol screening tool that helps identify persons with hazardous drinking or active alcohol use disorders.
options for health ranking including Excellent, Very Good, Good, Fair and Poor.
PHQ-2, the Patient Health Questionnaire-2, is a validated depression screening tool, which inquires about frequency of depressed mood and anhedonia over the past 2 weeks.
Clinician Experiences
Clinicians reported in their postencounter diary entries that the social needs survey helped change care in 22.5% of encounters (Table 2). Ways that the social needs survey changed care included providing more exercise and dietary counseling, helping address financial barriers to medications and being mindful of medication costs when prescribing, addressing behavioral health issues, and helping with transportation to access clinical services. Furthermore, clinicians reported that in 52.5% of encounters, the social needs survey helped them know the patient better (Table 2). Specifically, clinicians reported they were able to better understand their patients’ finances, relationships with family and friends, beliefs and values, and behavioral health needs.
Table 2.
Clinician Diary Responses About Using the Social Needs Survey (n = 123)
| Positive Response (%) | Neutral (%) | Negative Response (%) | |
|---|---|---|---|
| Information from social needs survey helped during encounter | 33.9 | 64.4 | 1.7 |
| Knowing patient lives in “cold spot” helped during the encounter | 33.3 | 63.3 | 3.3 |
| Social needs suarvey helped change care* | 22.5 | N/A | 77.5 |
| Social needs survey helped me know patient better | 52.5 | 40.8 | 6.7 |
Note: see Appendix B for clinician diary response prompts.
for this question, clinicians were not given a neutral response option.
The themes and findings from our series of 4 learning collaboratives are shown in Table 3. Specifically, although some clinicians expressed skepticism about the value of collecting SDH information before administering the social needs surveys to patients, clinicians identified value in improving interactions with patients and knowledge of their patients after the surveys were administered. For example, one clinician said the following: “It is a reminder that […] our patients have lives outside of just the medicine that we give them.” Others discussed specific examples of how they changed their care and interactions: “I took extra time asking her about barriers” and “I was less inclined to assume she did not care about her health.”
Table 3.
Themes from Clinician Perspectives Identified in Learning Collaboratives and Clinician Diaries
| Themes | Findings | Example Quotations |
|---|---|---|
| The act of assessing social needs is difficult and resource intensive | Screening is less beneficial for patients that you know well Patients may be hesitant to share needs |
“Some of the folks I have known for 20 plus years, so there wasn’t a lot that could surprise me.” “The patient was very reluctant to complete the survey. He did not report any social needs for any topic and did not ask for help with any topics. However, I actually suspect that the patient has a number of social needs. Talking about the responses made me think he had a number of needs but was embarrassed to mention them.” “I think there’s a lot of pride too. Like I had one patient that looked at the survey and he figured out pretty quick what it was and then he just didn’t want to do it.” |
| Patients who need help do not come in for visits | “It’s important to mention that the people who really need it may not be the ones who are actually coming in.” | |
| The information is overwhelming for physicians | “And I think it does get a bit overwhelming to think about having that burden. I mean as a family practitioner, we already do so much in terms of looking at the whole person, but it just adds another dimension but I don’t know how well, right now, we are equipped to deal with.” “We’re doing too many things. We have too much to do. We have too little time.” |
|
| Few resources exist to help patients with social needs | Providers want to address social needs but lack agency with respect to addressing social needs | “Our resources as a practice are limited because we can’t be paying for rides for patients. We can’t be, you know, doing some of these things. So really we have to think about what we really want to accomplish with this.” |
| Clinicians are not aware of community resources | “One problem is we don’t know what resources are even in our community, most of us.” “There’s so much that’s out there that I never stumble upon until like I have one patient who has this one resource that I end up using. It would be helpful just to know what all is there, you know?” |
|
| Practices lack adequate support to address social needs | “It doesn’t do you much good in a system to identify issues or problems if the system doesn’t have any way to address them.” | |
| Screening for social needs did not seem to help with social service delivery, but it did help clinicians to know their patients and seems to change clinician-patient interactions |
May change how clinician interacts with patient | “The patient had a new diagnosis of diabetes and told me she did not go to the diabetes education classes because they were $250 per class. With the survey, my reaction was more understanding and I was less inclined to assume she did not care about her health.” “My patient had a mammogram ordered from wellness visit last year but never had it done. Knowing she was from a resource poor area, I took extra time asking her about barriers that would prohibit her from getting this done this year.” |
| May increase clinician awareness | “It’s a reminder that our patients, in filling out these surveys and learning more about them, that our patients have lives outside of just the medicine that we give them.” | |
| May not change practice | “I don’t think that other than maybe a little bit of insight making me think about those community factors more than I would if I hadn’t had the survey to look at […] I haven’t changed anything.” | |
| Screening for social needs can cause harms | “Does it make a difference that I’m actually surveying these people? Am I doing this for naught? And I guess that would be another…what’s the outcome going to do? Because I always want to do good. I took an oath to do no harm.” | |
| More evidence is needed about how to collect social needs, how to help address social needs, and the impact on health | Some clinicians questioned if health care system is the right place to address social needs | “For at least social needs, I would think the doctor is a small little isolated part that could be addressed by a bigger system […] it seems like there’s probably a better structure to gather the data to identify what the needs are and to actually address the needs that is probably not the doctor’s office.” “We’re not asking the right questions. It makes me think well, gosh, what would be the right questions to ask to identify things that the doctor might be able to help with.” |
| More evidence is needed about whether addressing social needs improves health outcomes | “I think the bottom line is: Does it improve social or health outcome? I mean that’s what we want to know the answer to. Is investing your time and doing these things, does it pay off? Does it actually help the patient? It would be nice to see data that shows that it does.” | |
| Clinicians have ideas about how to address social needs better | “Maybe a print-out of the basic resources in there that we could just easily pick up.” “What about group sessions that we would hold here for people with similar county, in the same county, and similar issues and we could talk to them all at one time? I mean some people may be embarrassed /by this but then also they could support each other.” |
However, there remained concern that screening for social needs might not change practice significantly and whether or not the health care system is the right place to address social needs. For example, one clinician stated that “For at least social needs, I would think the doctor is a small little isolated part” and indicated concern that clinicians might be held responsible for one more metric. Clinicians also identified concerns about being overwhelmed with too much information and administrative burden. Furthermore, they were concerned about the lack of resources to address any identified needs.
When completing the learning collaborative series, clinicians indicated interest in further exploring how social needs screening might be more broadly applied. They indicated interest in finding out whether or not addressing social needs might improve health outcomes and spent significant amounts of the time during the learning collaborative brainstorming ways to better address identified social needs.
Discussion
Although prior studies have examined the feasibility of screening for social needs in primary care practices, our study adds to the literature by examining primary care clinicians’ experiences of collecting SDH information. Through diary entries and learning collaboratives, clinicians reported that knowing patients’ social needs changed what they did and improved communication for a substantial number of patients. Because primary care values patient relationships and continuity of care, screening for social needs may play a role not only in helping address the social needs of patients but also in building the patient-clinician relationship. Improvement in both of these areas may in turn be able to reduce the disparities that are found in patients who come from these cold spot neighborhoods.37 Furthermore, whereas other studies have focused on social needs screening in underserved communities, our study was able to demonstrate substantial social needs in a subset of a population in an affluent community. This may make the case for screening a subset of patients for social needs in affluent communities.
However, significant work needs to be done before the dissemination and implementation of social needs screening. Clinicians in our study spoke about the need for more meaningful resources to address social needs, more education on how to best address social needs, and the need for collaborations with community partners to adequately address social needs. Creating these resources and community-clinical partnerships will take substantial work and time; clinicians will need to be supported in these activities if they are to be expected to screen for and address social needs within their practices.
Interestingly, whereas 70.7% of patients screened positive for at least one social need (excluding physical activity), only 3.3% asked for help for a social need. It would likely be overwhelming for primary care clinicians to address social needs in more than half of their patients; however, clinicians could potentially focus on the smaller proportion of patients who sought help with their social needs within the subset of patients identified as living in a cold spot. This approach might make addressing social needs more manageable for primary care clinicians and likely more successful if resources were targeted toward patients who sought help from their clinicians and lived within cold spot communities. Clinicians could then focus on developing resources and community-clinical partnerships in domains where their patients are more likely to seek help.
Limitations
There are several limitations to our study. First, our clinician sample may not be representative of all primary care clinicians, but rather biased by self-selection to participate among clinicians more interested in addressing SDH. Second, selection bias may exist from our patient sample for 3 reasons: (1) the cold-spotting methodology used may have excluded patients who did not live in a cold spot who have social needs, (2) patients who could not read English were excluded, and (3) patients who did not show up for their visit were excluded. However, it may be the case that in most primary care practices, it would not be practical to initially target interventions to address social needs in patients who do not come for appointments. Third, we had a limited sample size from clinics within one health system. Although our study demonstrated that there is value in screening for social needs even in an affluent population, it may not be representative of clinician experiences in other settings and may not represent the proportion of patients with social needs in other settings. Furthermore, different health care settings may have different resource availability. Fourth, although our social needs survey (Appendix A) is derived from NAM’s social needs measures and the Hennepin County Lifestyle Survey, it is not a validated instrument. Fifth, because this study focused on the experiences of clinicians screening for social needs, our sample of patients is small and may limit findings from the patient responses on the social needs survey.
Conclusions
Our study suggests that clinicians may find value in screening for and addressing social determinants of health in their practice. Finding out about patients’ social needs may not only change care but also may help improve the patient-clinician relationship. However, before social needs screening is widely implemented, more work is needed to develop resources for primary care clinicians to address identified social needs, particularly those with which patients ask for help. Future studies are also needed to assess the health benefits of social needs screening in primary care before widespread implementation. If these associations are found, there are potentially significant implications on how primary care clinicians could address SDH in their practices.
Acknowledgments
We thank Jené Grandmont, David Grolling, Camille Hochheimer, Jennifer Rankin, and Roy Sabo for their work geocoding patient addresses and identifying cold spots.
Funding: UL1TR000058 from the National Center for Advancing Translational Sciences and the CCTR Endowment Fund of Virginia Commonwealth University.
Appendix A: Social Needs Survey
 |
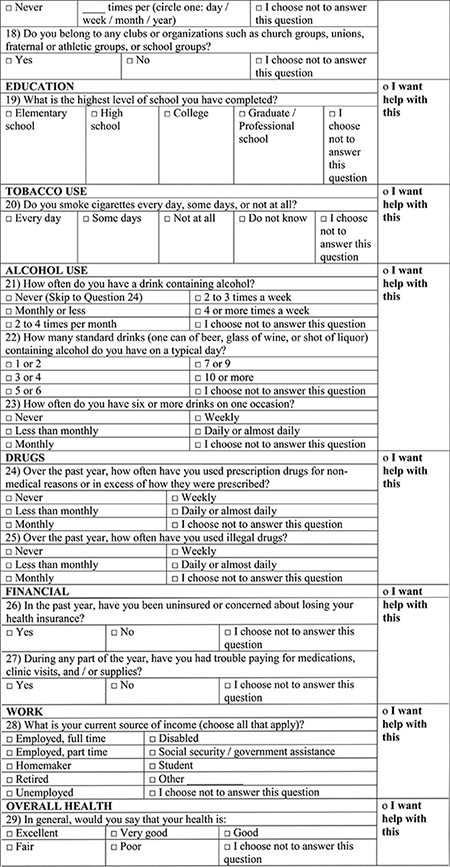 |
Appendix B: Postencounter Clinician Diary Entry Questions
| 1. Did you review the social needs survey completed by the patient? |
| ○ Yes |
| ○ No |
| ○ Did not receive the social needs survey |
| 2. How much did the information from the social needs survey help or distract you during the encounter? |
| ○ Helped a lot |
| ○ Helped somewhat |
| ○ Neither helped nor distracted |
| ○ Distracted somewhat |
| ○ Distracted a lot |
| 3. How much did knowing that your patient lives in a resource poor community help or distract you during the encounter? |
| ○ Helped a lot |
| ○ Helped somewhat |
| ○ Neither helped nor distracted |
| ○ Distracted somewhat |
| ○ Distracted a lot |
| 4. As a result of having this additional information, how much did you change the care you delivered (consider the language used, time spent, follow up planned, tests ordered, medications prescribed, referrals made, etc.)? |
| ○ I changed my care a lot |
| ○ I changed my care somewhat |
| ○ I did not change my care at all |
| 5. How did your care change (consider both positive and negative changes)? |
| 6. What additional community or social information would have helped you? |
| 7. What additional support would help you better address community or social needs? |
| 8. I know my patient better as a result of having this additional information. |
| ○ Strongly disagree |
| ○ Slightly disagree |
| ○ Neutral |
| ○ Slightly agree |
| ○ Strongly agree |
| 9. What did you learn about your patient that you did not already know? |
Footnotes
Conflict of interest: none declared.
Contributor Information
Sebastian T. Tong, Virginia Commonwealth University, Richmond, VA.
Winston R. Liaw, The Robert Graham Center, Washington D.C.; University of Texas Health Science Center at Houston
Paulette Lail Kashiri, Virginia Commonwealth University, Richmond, VA.
James Pecsok, Virginia Commonwealth University, Richmond, VA.
Julia Rozman, Virginia Commonwealth University, Richmond, VA.
Andrew W. Bazemore, Virginia Commonwealth University, Richmond, VA; The Robert Graham Center, Washington D.C..
Alex H. Krist, Virginia Commonwealth University, Richmond, VA.
References
- 1.Galea S, Vlahov D. Social determinants and the health of drug users: Socioeconomic status, homelessness, and incarceration. Public Health Rep 2002; 117:S135–S145. [PMC free article] [PubMed] [Google Scholar]
- 2.Galobardes B, Smith GD, Jeffreys M, McCarron P.Childhood socioeconomic circumstances predict specific causes of death in adulthood: The Glasgow student cohort study. J Epidemiol Community Health 2006;60:527–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009;6: e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammig O, Bauer GF. The social gradient in work and health: A cross-sectional study exploring the relationship between working conditions and health inequalities. BMC Public Health 2013;13:1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krieger N, Kosheleva A, Waterman PD, Chen JT, Beckfield J, Kiang MV. 50-year trends in US socioeconomic inequalities in health: US-born black and white Americans, 1959–2008. Int J Epidemiol 2014; 43:1294–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA 2004;291:1238–45. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. What are social determinants of health? 2012. Available from: http://www.who.int/social_determinants/sdh_definition/en/. Accessed June 20, 2017.
- 8.Woolf SH, Johnson RE, Phillips RL Jr., Philipsen M. Giving everyone the health of the educated: an examination of whether social change would save more lives than medical advances. Am J Public Health 2007;97:679–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galea S, Tracy M, Hoggatt KJ, Dimaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health 2011;101: 1456–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schoeni RF, Dow WH, Miller WD, Pamuk ER. The economic value of improving the health of disadvantaged Americans. Am J of Prev Med 2018;40: S67–S72. [DOI] [PubMed] [Google Scholar]
- 11.Barnard LS, Wexler DJ, DeWalt D, Berkowitz SA. Material need support interventions for diabetes prevention and control: a systematic review. Curr Diab Rep 2015;15:2. [DOI] [PubMed] [Google Scholar]
- 12.Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: Food insecurity, cost-related medication underuse, and unmet needs. Am J Med 2014;127:303–10. [DOI] [PubMed] [Google Scholar]
- 13.Patel MR, Piette JD, Resnicow K, Kowalski-Dobson T, Heisler M. Social determinants of health, cost-related nonadherence, and cost-reducing behaviors among adults with diabetes: Findings from the National Health Interview Survey. Med Care 2016;54: 796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA 2016;316:2627–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Committee on Integrating Primary Care and Public Health. Primary care and public health: Exploring integration to improve population health. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 16.Commission on Social Determinants of Health. Closing the gap in a generation. Geneva: World Health Organization; 2008. [Google Scholar]
- 17.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities—addressing social needs through Medicare and Medicaid. N Engl J Med 2016;374:8–11. [DOI] [PubMed] [Google Scholar]
- 18.Adler N, Cutler D, Fielding J, et al. Addressing social determinants of health and health disparities: A vital direction for health and health care. Washington, DC: National Academy of Medicine; 2016. [Google Scholar]
- 19.World Health Organization. Declaration of Alma-Ata. Paper presented at: International Conference on Primary Health Care 1978; Alma-Ata, USSR. [Google Scholar]
- 20.Braveman P, Gottlieb L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep 2014;129:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman A Theory vs practice: Should primary care practice take on social determinants of health now? Yes. Ann Fam Med 2016;14:100–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeVoe JE, Bazemore AW, Cottrell EK, et al. Perspectives in primary care: A conceptual framework and path for integrating social determinants of health into primary care practice. Ann Fam Med 2016;14:104–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liaw W, Rankin J, Bazemore AW. Community oriented primary care curriculum. 2016. Available from: http://www.graham-center.org/rgc/maps-data-tools/tools/copc.html. Accessed February 27, 2016.
- 24.Mullan F, Epstein L. Community-oriented primary care: New relevance in a changing world. Am J Public Health 2002;92:1748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Institute of Medicine Division of Health Care Services. Community-oriented primary care: A practical assessment. Washington, DC: National Academies Press; 1984. [Google Scholar]
- 26.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: The accountable health communities screening tool. Washington, DC; 2017. [Google Scholar]
- 27.Institute of Medicine. Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 28.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics 2015;135: e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Byhoff E, Cohen AJ, Hamati MC, Tatko J, Davis MM, Tipirneni R. Screening for social determinants of health in Michigan health centers. J Am Board Fam Med 2017;30:418–27. [DOI] [PubMed] [Google Scholar]
- 30.Page-Reeves J, Kaufman W, Bleecker M, et al. Addressing social determinants of health in a clinic setting: The WellRx pilot in Albuquerque, New Mexico. J Am Board Fam Med 2016;29:414–8. [DOI] [PubMed] [Google Scholar]
- 31.Klein MD, Kahn RS, Baker RC, Fink EE, Parrish DS, White DC. Training in social determinants of health in primary care: Does it change resident behavior? Acad Pediatr 2011;11:387–93. [DOI] [PubMed] [Google Scholar]
- 32.Erickson SM, Rockwern B, Koltov M, McLean RM.Putting patients first by reducing administrative tasks in health care: A position paper of the American College of Physicians. Ann Intern Med 2017;166: 659–61. [DOI] [PubMed] [Google Scholar]
- 33.Christino MA, Matson AP, Fischer SA, Reinert SE, DiGiovanni CW, Fadale PD. Paperwork versus patient care: a nationwide survey of residents’ perceptions of clinical documentation requirements and patient care. J Grad Med Educ 2013;5:600–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siegler JE, Patel NN, Dine CJ. Prioritizing paperwork over patient care: Why Can’t we do both? J Grad Med Educ 2015;7:16–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baum FE, Legge DG, Freeman T, Lawless A, Labonté R, Jolley GM. The potential for multi-disciplinary primary health care services to take action on the social determinants of health: actions and constraints. BMC Public Health 2013;13:460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Solberg LI. Theory vs practice: Should primary care practice take on social determinants of health bow? No. Ann Fam Med 2016;14:102–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Westfall JM. Cold-Spotting: Linking primary care and public health to create communities of solution. J Am Board Fam Med 2013;26:239–40. [DOI] [PubMed] [Google Scholar]
- 38.Liaw W, Krist A, Tong S, et al. Are cold spots associated with worse clinical outcomes? J Am Board Fam Med. In press. [Google Scholar]
- 39.United States Census Bureau. Northern Virginia dominates list of highest-income counties, Census Bureau Reports. 2013. Available from: https://www.census.gov/newsroom/press-releases/2013/cb13-214.html. Accessed Aug 1, 2017.
- 40.Virginia Department of Health. Division of Vital Records. 2017. Available from: http://www.vdh.virginia.gov/vital-records/. Accessed Jul 31, 2017.
- 41.United States Census Bureau. American Community Survey. 2016. Available from: https://www.census.gov/programs-surveys/acs/. Accessed Jul 31, 2017.
- 42.Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res 2013;48:539–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sandberg SF, Erikson C, Owen R, et al. Hennepin Health: A safety-net accountable care organization for the expanded Medicaid population. Health Aff (Millwood) 2014;33:1975–84. [DOI] [PubMed] [Google Scholar]
- 44.Contandriopoulos D, Lemire M, Denis JL, Tremblay E. Knowledge exchange processes in organizations and policy arenas: A narrative systematic review of the literature. Milbank Q 2010;88:444–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Agency for Healthcare Research and Quality. Establishing an AHRQ learning collaborative, a white paper. 2014. Available from: http://www.ahrq.gov/research/findings/final-reports/learningcollab/index.html.
- 46.Institute for Healthcare Improvement. The break-through series: IHI’s collaborative model for achieving breakthrough improvement. Boston: Institute for Healthcare Improvement; 2003. [Google Scholar]
- 47.Crabtree B, Miller W. Using codes and code manuals: A template organizing style of interpretation In: Crabtree B, Miller W, editors. Doing qualitative research. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc; 1999. [Google Scholar]


