Abstract
For over a century, research on psychopathology has focused on categorical diagnoses. Although this work has produced major discoveries, growing evidence points to the superiority of a dimensional approach to the science of mental illness. Here we outline one such dimensional system—the Hierarchical Taxonomy of Psychopathology (HiTOP)—that is based on empirical patterns of psychological symptom co-occurrence. We highlight key ways in which this framework can advance mental health research, and we provide some heuristics for using HiTOP to test theories of psychopathology. We then review emerging evidence that supports the value of a hierarchical, dimensional model of mental illness across diverse research areas in psychological science. These new data suggest that the HiTOP system has the potential to accelerate and improve research on mental health problems as well as efforts to more effectively assess, prevent, and treat mental illness.
Keywords: mental illness, nosology, individual differences, transdiagnostic, Hierarchical Taxonomy of Psychopathology (HiTOP), ICD, DSM, RDoC
Dating back to Kraepelin and other early nosologists, research on psychopathology has been framed around mental disorder categories (e.g., What biological malfunctions typify generalized anxiety disorder? How does antisocial personality disorder disrupt close relationships?). This paradigm has produced valuable insights into the nature and origins of psychiatric problems. Yet there is now abundant evidence that categorical approaches to mental illness are hindering scientific progress. Grounded in decades of research, an alternate framework has emerged that characterizes psychopathology using empirically derived dimensions that cut across the boundaries of traditional diagnoses. Recent efforts by a consortium of researchers to review and integrate findings relevant to this framework have given rise to a proposed consensus dimensional system, the Hierarchical Taxonomy of Psychopathology (HiTOP1; Kotov et al., 2017).
Here, we first summarize the rationale behind dimensional rubrics for mental illness and briefly sketch the topography of the HiTOP system (for detailed reviews, see Kotov et al., 2017, Krueger et al., in press). Second, we explain how HiTOP can be used to improve research practices and theory testing. Third, we review new evidence for the utility of HiTOP dimensions across various research contexts, from developmental psychology to neuroscience. Finally, we offer some practical recommendations for conducting HiTOP-informed research.
A Brief History of HiTOP
Mental illness is a leading burden on public health resources and the global economy (DiLuca & Olesen, 2014; Vos et al., 2016). Recent decades have witnessed the development of improved social science methodologies and powerful new tools for quantifying variation in the genome and brain, leading to initial optimism that psychopathology might be more readily explained and objectively defined (e.g., Hyman, 2007). Yet, billions of dollars of research have failed to yield much in the way of new cures, objective assays, or other major breakthroughs (Shackman & Fox, 2018).
A growing number of clinical practitioners and researchers—including the architects of the National Institute of Mental Health Research Domain Criteria (RDoC)—have concluded that this past underperformance reflects problems with categorical diagnoses, rather than any intrinsic limitation of prevailing approaches to understanding risk factors and treatment methods (Gordon & Redish, 2016). Categorical diagnoses—such as those codified in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD)—pose several well-documented barriers to discovering the nature and origins of psychopathology, including pervasive comorbidity, low symptom specificity, marked diagnostic heterogeneity, and poor reliability (Clark, Cuthbert, Lewis-Fernández, Narrow, & Reed, 2017; Helzer et al., 2009; Markon, Chmielewski, & Miller, 2011; Regier et al., 2013). Regarding reliability, for instance, DSM-5 field trials found that approximately 40% of diagnoses examined did not reach the cutoff for acceptable inter-rater agreement (Regier et al., 2013). Attesting to symptom profile heterogeneity in DSM, there are over 600,000 symptom presentations that satisfy diagnostic criteria for DSM-5 posttraumatic stress disorder (Galatzer-Levy & Bryant, 2013).
Addressing these problems requires a fundamentally different approach. HiTOP—like other dimensional proposals, such as RDoC (e.g., Brown & Barlow, 2009; Cuthbert & Insel, 2013)—focuses on continuously distributed traits theorized to form the scaffolding for psychopathology. In the tradition of early factor analyses of disorder signs and symptoms in adults (e.g., Eysenck, 1944; Lorr et al., 1963; Tellegen, 1985) and children (e.g., Achenbach, 1966; Achenbach, Howell, Quay, Conners, & Bates, 1991), more recent quantitative analysis of psychological symptom co-occurrence has established a reproducible set of dimensions theorized to reflect the natural structure of psychological problems (Kotov et al., 2017).
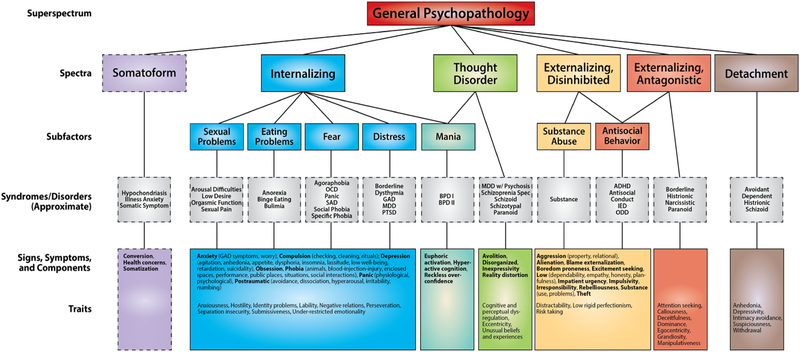
Figure 1 provides a simplified schematic depiction of HiTOP, which features broad, heterogeneous constructs near the top of the model and specific, homogeneous dimensions near the bottom. HiTOP accounts for diagnostic comorbidity by positing dimensions (e.g., internalizing) that span multiple DSM diagnostic categories, and it also models diagnostic heterogeneity by specifying fine-grain processes (e.g., worry, panic) that constitute the building blocks of mental illness. Indeed, profiles of narrow symptom dimensions (e.g., low well-being, suicidality, situational fears) explain variation on broad dimensions (e.g., elevated internalizing) in more detail.
Figure 1.
Hierarchical Taxonomy of Psychopathology (HiTOP) consortium working model. Constructs higher in the figure are broader and more general, whereas constructs lower in the figure are narrower and more specific. Dashed lines denote provisional elements requiring further study. At the lowest level of the hierarchy (i.e., traits and symptom components), for heuristic purposes, conceptually related signs and symptoms (e.g., Phobia) are indicated in bold, with specific manifestations indicated in parentheses. Abbreviations—ADHD: attention-deficit/hyperactivity disorder; GAD: generalized anxiety disorder; IED: intermittent explosive disorder; MDD: major depressive disorder; OCD: obsessive-compulsive disorder; ODD: oppositional defiant disorder; SAD: separation anxiety disorder; PD: personality disorder; PTSD: post-traumatic stress disorder.
HiTOP is an evolving model. An international group of researchers has assembled to investigate this structure and update it as informed by new data (Krueger et al., in press).2 (The HiTOP consortium will publish revisions to the model, as new research findings accumulate, on its website.) Indeed, the explicit goal of the HiTOP project is to follow the evidence. The system is open for any type of revision that is supported by sufficient evidence; its core assumption is that a more valid nosology can be developed based on the empirical pattern of clustering among psychopathology phenotypes (i.e., symptoms and maladaptive traits).
Refining this dimensional model is a key priority, but it is only one step in the evolution of HiTOP. Another key priority is to use HiTOP to improve and accelerate research focused on mental health and illness. As described in detail below, HiTOP has the potential to advance theories of psychopathology and make mental health research more efficient and informative.
HiTOP as a Psychopathology Research Framework
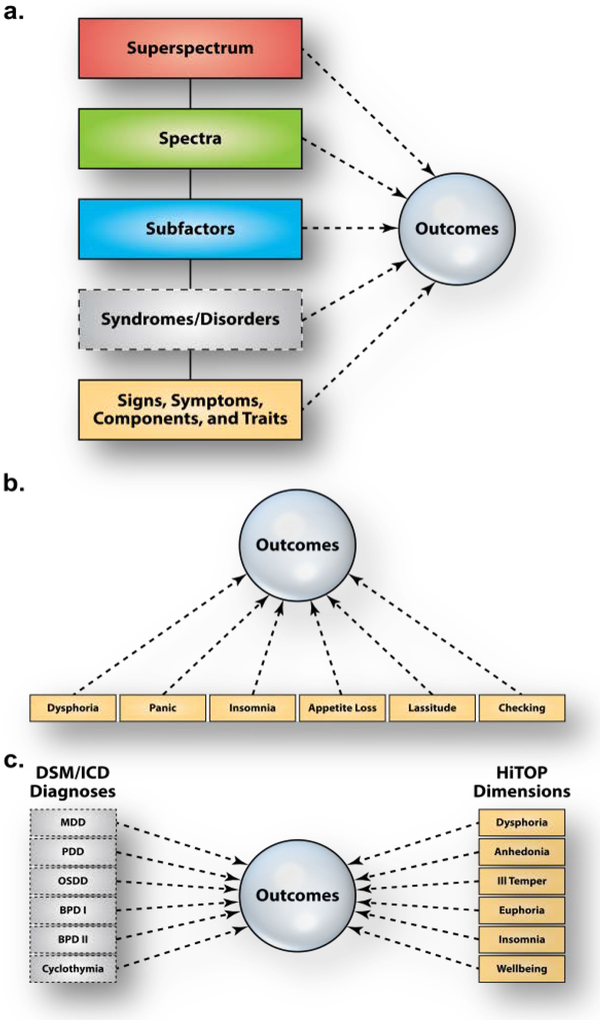
A distinguishing feature of HiTOP is its hierarchical organization (Figure 1). Various processes—some specific, others quite broad—are potentially implicated in the origins and consequences of psychological problems across the lifespan (Forbes, Tackett, Markon, & Krueger, 2016). The hierarchical structure implies that any cause or outcome of mental illness could emerge because of its effects on broad higher order dimensions, the syndromes, or specific lower order dimensions (Figure 2). Take trauma, for example. Suppose that research based on the HiTOP framework establishes that trauma exposure better predicts variation in the internalizing spectrum than in its constituent syndromes (e.g., depression, posttraumatic distress). How would this result change our conceptualization of this research area? It would call for an expansion of our etiological models of posttraumatic distress to focus on the broad internalizing spectrum, including psychobiological processes shared by the mood and anxiety disorders. We might advise a moratorium on research studies that examine only one DSM disorder in relation to trauma exposure; instead, for maximum efficiency, we would consider various aspects of the internalizing spectrum (e.g., worry, rituals, insomnia, irritability) as outcomes simultaneously in research studies. Additionally, when making policy decisions regarding prevention and intervention resources, we might prioritize screening trauma-exposed individuals for the full range of internalizing problems, not just posttraumatic stress disorder. In sum, thinking hierarchically about mental illness can promote more efficient research practices and more nuanced theory.
Figure 2.
Conceptual diagrams of three possible HiTOP research designs. (A) Comparing the predictive validity across HiTOP levels. (B) Comparing predictive validity within a HiTOP level. (C) Comparing the predictive validity of categorical diagnoses to HiTOP dimensions. Abbreviations—BPD I: bipolar I disorder; BPD II: bipolar II disorder; MDD: major depressive disorder; OSDD: other specified depressive disorder; PDD: persistent depressive disorder.
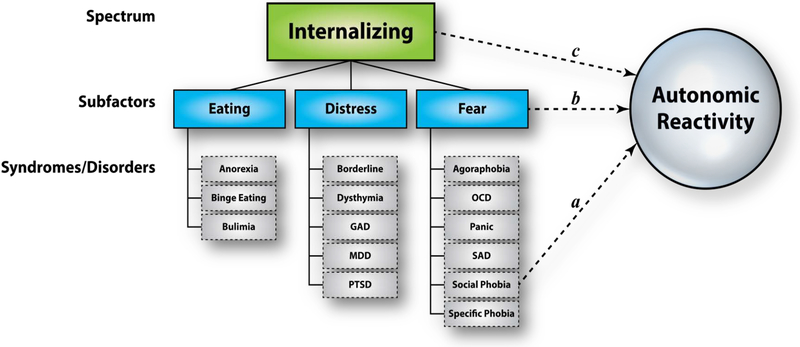
To illustrate these points, we now consider a more detailed example of putting HiTOP into practice (Figure 3). For ease of presentation, DSM diagnoses comprise the basic units of assessment.3 A subset of HiTOP constructs are involved (listed in order of increasing granularity): the internalizing spectrum; fear, distress, and eating pathology subfactors; and their component syndromes (e.g., binge eating disorder, agoraphobia). These constructs serve as the predictor variables here.
Figure 3.
Heuristic model of the internalizing domain in relation to autonomic reactivity to a laboratory challenge. Paths a, b, and c represent regressions of the outcome on dimensions at different levels of the hierarchical model. See the main text for details.
For this example, we consider a test of an autonomic stress reactivity theory of social phobia. The outcome of interest is skin conductance level during an impromptu speech delivered to a group of impassive confederates. The researchers’ theory—which, like many others in psychopathology research, pertains to one particular categorical disorder—dictates that predictive path a in Figure 3 should eclipse the others: the social phobia diagnosis should be specifically associated with exaggerated autonomic reactivity in this evaluative social context. Alternatively, one could reasonably expect that excessive autonomic reactivity is a more general characteristic of fear disorders (e.g., social phobia, panic disorder, agoraphobia), as compared to distress or eating pathology syndromes. In that case, path b should surpass the others in terms of variance explained. Finally, given evidence linking the full complement of anxiety and depressive disorders to stress responsivity, it is possible that reactivity is best captured at the spectrum level. In this last scenario, path c should predominate.
This heuristic illustrates that examining the validity of any DSM diagnosis in isolation—a conventional research strategy—is unnecessarily limiting. A zero-order association between a DSM diagnosis and some outcome could reflect one (or more) qualitatively distinct pathways (in our example, paths a, b, or c in Figure 3). Hierarchical frameworks, like HiTOP, provide a ready means of quantitatively comparing these alternatives. If, in our example, the effect for path a is comparatively small, the research team will know to revise the “autonomic arousal theory of social phobia” to encompass fear-based or internalizing disorders more generally.
We supplement this case study with a real-world example of theory building driven by HiTOP. The stress generation theory posits that individuals with DSM major depression encounter more stressful life events—including ones they have had a role in creating (e.g., romantic relationship dissolution, school expulsion)—than non-depressed counterparts (Hammen, 1991). Indeed, there is evidence that depression prospectively predicts stress exposure. But more recent work suggests that this effect is not specific to depression. In fact, stress generation appears to be a general feature of the internalizing disorders and dispositional negativity (Liu & Alloy, 2010). Consistent with this hypothesis, Conway and colleagues demonstrated that the internalizing spectrum, externalizing spectrum, and DSM major depression all contributed to the prediction of future stress exposure when considered simultaneously (cf. Figure 3; Conway, Hammen, & Brennan, 2012). Interestingly, panic disorder had an inverse effect on stress occurrence after adjusting for the transdiagnostic dimensions. The authors labeled this novel association a “stress inhibition” effect.
These findings prompted a reformulation of stress generation theory. First, stress generation processes are now hypothesized to operate across a range of internalizing and externalizing syndromes, not just DSM major depression. Second, the HiTOP-consistent analysis pointed to a role for depression-specific pathology in predicting stressful events above and beyond the effects of the internalizing spectrum (i.e., incremental validity). Theorists can use that result to consider the specific portions of DSM major depression that increase the likelihood of encountering significant stressors. Third, this work highlights the need to understand more fully the stress inhibiting consequences of panic symptoms, a signal that was not detectable when analyzing DSM diagnoses only.
Up to this point, we have considered how a hierarchical approach—that is, comparing pathways to and from dimensions at different levels of HiTOP—can advance our understanding of psychopathology. Although this approach has been the most common application of HiTOP, it is not the only one. Some researchers have used HiTOP to dissect DSM diagnoses into components and compare their criterion validity (e.g., Simms, Grös, Watson, & O’Hara, 2008) (Figure 2b). For example, panic disorder could be decomposed into physiological (e.g., tachycardia, choking sensations) and psychological symptoms (e.g., thoughts of dying or going crazy). The predictive validity of these two symptom domains could then be compared in relation to a clinical outcome of interest (e.g., emergency room visits). Other researchers have evaluated the joint predictive power of sets of HiTOP dimensions above and beyond the corresponding DSM-5 diagnosis (see Waszczuk, Kotov, et al., 2017; Waszczuk, Zimmerman, et al., 2017). This approach explicitly compares the explanatory potential of dimensional versus categorical approaches to psychopathology (Figure 2c).
Investigators are beginning to use these research strategies to reevaluate existing theories and findings through a HiTOP lens. In the sections that follow, we describe studies that have approached etiological and clinical outcome research from a HiTOP perspective as a way of selectively illustrating its utility.
Etiological Research from a HiTOP Perspective
Quantitative and Molecular Genetics.
Twin studies find that some HiTOP dimensions are underpinned by distinct genetic liability factors, suggesting that the phenotypic and genetic structures of psychopathology may be closely aligned (e.g., Lahey, Krueger, Rathouz, Waldman, & Zald, 2017; Røysamb et al., 2011). For example, twin research has documented an overarching genetic liability factor that resembles a general factor of psychopathology (Pettersson, Larsson, & Lichtenstein, 2016). This general factor (see the top level of Figure 1) was first described in phenotypic analyses (Lahey et al., 2012) and was termed the “p-factor” as a counterpart to the g-factor in the intelligence literature (Caspi et al., 2014; Caspi & Moffitt, 2018). Consistent with the broad intercorrelations among higher order spectra in psychometric studies, there is growing evidence that common genetic vulnerabilities underlie a general (i.e., transdiagnostic) risk for psychopathology (Selzam, Coleman, Moffitt, Caspi, & Plomin, 2018; Waszczuk et al., 2018).
At a lower level of the hierarchy, genetic influences operating at the level of spectra have also been identified. For example, anxiety and depressive disorders appear to substantially share a common genetic diathesis, whereas antisocial behavior and substance use conditions share a distinct substrate (Kendler & Myers, 2014). Also, there is a consistent, but underdeveloped, line of twin research that provides biometric support for the genetic coherence of the thought disorder and detachment spectra (Livesley, Jang, & Vernon, 1998; Tarbox & Pogue-Geile, 2011). Further attesting to the hierarchical structure of genetic risk, distinct genetic influences have been identified for the distress and fear subfactors of the internalizing spectrum (Waszczuk, Zavos, Gregory, & Eley, 2014). Finally, twin research shows that narrow psychiatric syndromes—and even certain symptom components within them—might possess unique genetic underpinnings alongside the genetic vulnerability shared with other psychiatric conditions more broadly (e.g., Kendler, Aggen, & Neale, 2013; Rosenström et al., 2017). Overall, although these specific genetic factors often are comparatively small, they provide etiological support for a hierarchical conceptualization of psychopathology. A key challenge for future research will be to evaluate more comprehensive versions of the HiTOP model in adequately powered, genetically informative samples (e.g., twin, GWAS).
Emerging cross-disorder molecular genetic studies also suggest that genetic influences operate across diagnostic boundaries (Smoller et al., in press). For example, a recent meta-analysis of genome-wide association studies (GWAS) of DSM generalized anxiety disorder, panic, agoraphobia, social anxiety, and specific phobia identified common variants associated with a higher order anxiety factor, consistent with the HiTOP fear subfactor (Otowa et al., 2016). Other work reveals moderate (38%) single nucleotide polymorphism (SNP)-based heritability of the p-factor, indicating that common SNPs are associated with a general psychopathology factor in childhood (Neumann et al., 2016). Beyond these broader spectra, several molecular genetic studies have focused on constructs at the subordinate level of the HiTOP hierarchy, partly to reduce phenotypic heterogeneity and amplify genetic signals. For example, one GWAS investigated a narrowly defined phenotype of mood instability, which led to a discovery of four new genetic variants implicated in mood disorders (Ward et al., 2017). Together, these emerging results suggest that it will be possible to identify specific genetic variants at different levels of HiTOP hierarchy, with some influencing nonspecific psychopathology risk and others conferring risk for individual spectra, subfactors, or even symptoms (e.g., anhedonia). In contrast, traditional case-control designs and even studies focused on pairs of disorders are incapable of untangling such hierarchical effects. In short, HiTOP promises to provide a more effective framework for discovering the genetic underpinnings of mental illness, although further empirical evidence and replications of any specific molecular genetic findings are, of course, needed.
Neurobiology.
Paralleling the genetics literature, there is growing evidence that many measures of brain structure and function do not respect the boundaries implied by traditional DSM/ICD diagnoses. There are no clear-cut depression or schizophrenia “centers” in the brain (e.g., Sprooten et al., 2017). Instead, associations between the brain and mental illness often show one-to-many or many-to-many relations (i.e., multifinality; Zald & Lahey, 2017). Heightened amygdala reactivity, for example, has been shown to confer risk for the future emergence of mood and anxiety symptoms, posttraumatic distress, and alcohol abuse (e.g., McLaughlin et al., 2014; Swartz, Knodt, Radtke, & Hariri, 2015). The internalizing and externalizing spectra are both associated with altered maturation of subcortical structures in late childhood (Muetzel et al., 2018). In some cases, these relations have been shown to reflect specific symptoms that cut across DSM’s categorical diagnoses. For instance, anhedonia is a central feature of both mood and thought disorders in DSM, and dimensional measures of anhedonia have been linked to aberrant ventral striatum function (i.e., activity and functional connectivity) in several large-scale, mixed-diagnosis studies (Sharma et al., 2017; Stringaris et al. 2015).
Evidence of one-to-many relations is not limited to the neuroimaging literature. The P3 event-related potential (ERP), for example, has been linked to a variety of externalizing disorders and to dimensional measures of externalizing (Iacono, Malone & McGue, 2003; Patrick et al., 2006). Cross-sectional and prospective studies have linked the error-related negativity (ERN) to a variety of DSM anxiety disorders, to the development of internalizing symptoms, and to dimensional measures of anxiety (Cavanagh & Shackman, 2015; Meyer, 2017).
Although the neural bases of the p-factor remain far from clear, recent neuroimaging research has begun to reveal some neural systems with conspicuously similar (i.e., transdiagnostic) features. In a recent meta-analysis, McTeague and colleagues (2017) identified a pattern of aberrant activation shared by the major mental disorders. When performing standard cognitive control tasks (e.g., Go/No-Go, Stroop), patients diagnosed with DSM anxiety disorders, bipolar disorder, depression, schizophrenia, or substance abuse all exhibited reduced activation in parts of the so-called salience network, including regions of the cingulate, insular, and prefrontal cortices. Applying a similar approach to voxel-by-voxel measures of brain structure, Goodkind and colleagues (2015) identified a neighboring set of regions in the midcingulate and insular cortices showing a common pattern of cortical atrophy across patients diagnosed with a range of DSM disorders (anxiety, bipolar disorder, depression, obsessive-compulsive, and schizophrenia). Few disorder-specific effects were detected in either of these large meta-analyses.
More recent imaging research has begun to adopt the kinds of analytic tools widely used in psychometric and genetic studies of psychopathology, enabling a direct comparison of different levels of HiTOP (cf. Figure 2a) and new clues about the neural bases of the p-factor. Using data acquired from the Philadelphia Neurodevelopmental Cohort, Shanmugan and colleagues (2016) identified the p-factor and four nested sub-dimensions (antisocial behavior, distress, fear, and psychosis; cf. Figure 1, subfactor level). Higher levels of the p-factor were associated with reduced activation and aberrant multivoxel patterns of activity in the salience network (cingulate and insular cortices) during the performance of the n-back task, a widely used measure of working memory capacity and executive function. After accounting for the phenotypic variance explained by the p-factor, the antisocial, distress, and psychosis dimensions were each associated with additional subfactor-specific alterations in task-evoked activation (e.g., psychosis was uniquely associated with hypoactivation of the dorsolateral prefrontal cortex). Using the same sample, Kaczkurkin and colleagues (in press) found an analogous pattern of results with measures of resting activity. These observations converge with the meta-analytic results discussed above (Goodkind et al., 2015; McTeague et al., 2017) and reinforce the idea that a circuit centered on the cingulate cortex underlies a range of common psychiatric symptoms and syndromes. Still, it is implausible that this circuit will completely explain a phenotype as broad as the p-factor. Indeed, other correlates are rapidly emerging (Romer et al., 2018; Sato et al., 2016; Snyder, Hankin, Sandman, Head, & Davis, 2017).
Collectively, these results highlight the value of the HiTOP framework for organizing neuroscience and other kinds of biological research. Adopting a hierarchical dimensional approach makes it possible to dissect brain structure and function quantitatively, facilitating the discovery of features that are common to many or all of the common mental disorders, those that are particular to specific spectra and syndromes, and those that underlie key transdiagnostic symptoms—a level of insight not afforded by RDoC or traditional diagnosis-centered nosologies.
Environmental Risk.
Stressful environments are intimately intertwined with risk for mental illness. For decades, researchers have proposed theories about the connections between stressors and specific diagnoses (e.g., loss and DSM major depression). Yet it is clear that most stressors are non-specific and confer increased risk for diverse psychopathologies (McLaughlin, 2016). Socioeconomic adversity, discrimination, harsh parenting, bullying, and trauma all increase the likelihood of developing psychiatric illness (Caspi & Moffitt, in press; Lehavot & Simoni, 2011; Wiggins, Mitchell, Hyde, & Monk, 2015). This lack of specificity raises the possibility that many stressors act on illness processes that are shared across entire subfactors (e.g., distress, antisocial behavior), spectra (e.g., internalizing), or even super-spectra. Investigators can use HiTOP to identify the level or levels where stressful environments exert their effects.
Childhood maltreatment represents an instructive case because it has potent and non-specific relations with future psychopathology (Green et al., 2010). Several studies have used a hierarchical approach to assess the relative importance of higher order (i.e., transdiagnostic) versus diagnosis-specific pathways from early maltreatment to mental disorders in adulthood. Leveraging interview-based diagnoses and retrospective reports of childhood maltreatment collected as part of the National Epidemiological Survey on Alcohol and Related Conditions (n > 34,000), Keyes and colleagues observed strong relations between childhood maltreatment and the internalizing and externalizing spectra (cf. path c in Figure 3), but not specific diagnoses (cf. path a in Figure 3) (Keyes et al., 2012). In other words, the marked impact of childhood maltreatment on adult psychopathology was fully mediated by the transdiagnostic spectra. Similar findings emerged in a community sample of over 2,000 youth enriched for exposure to maltreatment (Vachon, Krueger, Rogosch, & Cicchetti, 2015; see also Conway, Raposa, Hammen, & Brennan, 2018; Lahey et al., 2012; Meyers et al., 2015; Sunderland et al., 2016).
The HiTOP framework has also been used to understand the influence of chronic stressors in adulthood (Snyder, Young, & Hankin, 2017). For instance, Rodriguez-Seijas et al. (2015) recently showed that racial discrimination has strong associations with the internalizing and externalizing spectra (cf. path c in Figure 3) in a nationally representative sample of over 5,000 Black Americans. For most disorders, the pathway from discrimination to particular DSM diagnoses (e.g., ADHD, social phobia) was largely explained by its impact on higher order spectra. In a few cases, discrimination was directly associated with specific diagnoses (e.g., alcohol use disorder). These effects make it clear that multiple pathways from environmental adversity to psychopathology are possible—some centered on transdiagnostic spectra, others on more specific syndromes—with important implications for efforts to develop more effective and efficient strategies for preventing and treating mental illness.
Clinical Outcome Research from a HiTOP Perspective
Like etiological factors, clinical outcomes often reflect a mixture of specific and transdiagnostic effects and, as a result, are better aligned with HiTOP than traditional diagnostic systems, like DSM or ICD.
Prognosis.
Clinicians and researchers often seek to forecast the onset or recurrence of psychological problems based on diagnostic and symptom data (e.g., Morey et al., 2012). The HiTOP system has the potential to streamline this prognostic decision-making. For instance, using data gleaned from the World Mental Health Surveys (N > 20,000), Kessler et al. (2011) examined the prognostic value of 18 DSM-IV disorders in predicting new onsets of subsequent diagnoses. They found that the vast majority of the development of categorical diagnoses arising at later time points was attributable to variation on internalizing and externalizing dimensions earlier in life (for similar results, see Eaton et al., 2013). This result suggests that higher order dimensions can often provide a more efficient means of predicting the natural course of mental illness (see also Kotov, Perlman, Gamez, & Watson, 2015; Olino et al., in press).
Suicide.
The HiTOP framework has also proven useful for optimizing suicide prediction. Tools for forecasting suicide are often based on the presence or absence of specific diagnoses (e.g., bipolar disorder, borderline personality disorder). But recent large-scale studies have consistently shown that the predictive power of DSM diagnoses pales in comparison to that of higher order dimensions. For instance, in the NESARC sample described earlier, the distress subfactor (Figure 1) explained ~34% of the variance in suicide attempt history. In contrast, the top-performing DSM diagnoses only accounted for ~1% (Eaton et al., 2013; see also Naragon-Gainey & Watson, 2011; Sunderland & Slade, 2015). These kinds of observations indicate that suicide risk is better conceptualized at the level of spectra, not syndromes, contrary to standard research and clinical practices.
Impairment.
Psychosocial impairment is typically a core feature of contemporary definitions of psychopathology, and it often persists long after acute symptoms have abated. Understanding impairment is important for prioritizing scarce resources. But is impairment better explained and, more importantly, predicted by DSM/ICD diagnoses or transdiagnostic dimensions? Using data from the Collaborative Longitudinal Personality Disorders Study (N = 668), Morey et al. (2012) found that maladaptive personality traits were twice as effective at predicting patients’ functional impairment across a decade-long follow-up, when compared to traditional diagnoses (cf. Figure 2c). Likewise, Forbush and colleagues demonstrated that higher order dimensions explain 68% of the variance in impairment in a sample of eating disorder patients (Forbush et al., 2017). In contrast, DSM anxiety, depression, and eating disorder diagnoses collectively explained only 11%. In the area of psychosis, van Os and colleagues (1999) compared the predictive power of five dimensions versus eight DSM diagnoses in a large longitudinal sample across 20 distinct psychosocial outcomes (e.g., disability, unemployment, cognitive impairment, and suicide). For every outcome with a clear difference in predictive validity, dimensions outperformed diagnoses.
Waszczuk, Kotov, et al. (2017) reported similar results in two samples evaluated with the Interview for Mood and Anxiety Symptoms (IMAS), which assesses the lower order components of emotional pathology (e.g., lassitude, obsessions). These dimensions explained nearly two times more variance in functional impairment compared to DSM diagnoses. Moreover, DSM diagnoses did not show any incremental power over the dimensional scores—a particularly striking result given that impairment is part of the DSM diagnostic criteria but not directly captured by IMAS scores (cf. Figure 2c). In sum, this line of research suggests that transdiagnostic dimensions of the kinds embodied in HiTOP have superior prognostic value—both concurrently and prospectively—for psychosocial impairment (see also Jonas & Markon, 2013; Markon, 2010; South, Krueger, & Iacono, 2011).
Summary
Traditionally, theoretical models of the causes and consequences of psychiatric problems have been framed around diagnoses. New research highlights the importance of extending this focus to encompass transdiagnostic dimensions, including both narrowly defined symptoms and traits (e.g., anhedonia) and broader clusters of psychological conditions (e.g., internalizing spectrum). In contrast to other classification systems (e.g., DSM) and unlike RDoC, HiTOP provides a convenient framework for directly testing the relative importance of symptom components, syndromes, spectra, and super-spectra (e.g., p-factor) for the emergence and treatment of psychopathology (Figure 1). The evidence reviewed here suggests that in many cases mental illness is better conceptualized in terms of transdiagnostic dimensions.
HiTOP: A Practical Guide
A primary objective of this review is to provide investigators with some practical recommendations for incorporating HiTOP into their research. Here we outline design, assessment, and analytic strategies that follow from the theory and available data underpinning HiTOP.
Design.
Historically, the lion’s share of clinical research has been conducted using traditional case-control designs, in which participants meeting criteria for a particular diagnosis are compared to a group free of that disorder or perhaps any mental illness. This approach is generally inconsistent with a dimensional perspective on psychopathology. There is compelling evidence that mental illness is continuously distributed in the population, without the gaps or “zones of discontinuity” expected of categorical illnesses (Krueger et al., in press; although for a different perspective see Borsboom et al., 2016). These observations indicate that artificially separating cases from non-cases leads to an appreciable loss of information (Markon et al., 2011), consistent with more general recommendations to avoid post hoc dichotomization (e.g., median splits) of continuous constructs (Preacher, Rucker, MacCallum, & Nicewander, 2005).
The case-control strategy also ignores the issue of diagnostic comorbidity. The ubiquitous co-occurrence of disorders makes it extremely difficult to establish discriminant validity for most categorical syndromes. In practical terms, any distinction between, say, DSM panic disorder patients and healthy controls in a particular study may not be a unique characteristic of panic disorder. It could instead reflect the influence of a higher order dimension, such as the HiTOP fear subfactor, that permeates multiple diagnoses (e.g., panic disorder, agoraphobia, social anxiety disorder, and specific phobia). By disregarding the symptom overlap among clusters of related conditions, the case-control design is bound to underestimate the breadth of psychopathology associated with a given clinical outcome.
From an efficiency standpoint, recruiting on the basis of particular diagnoses creates a fragmented scientific record. The traditional approach of studying one disorder in relation to one outcome has spawned many insular journals, societies, and scholarly sub-communities (“silos”). This convention belies the commonalities among disorders and has led to piecemeal progress. For example, the initial phases of psychiatric genetic research were oriented around specific diagnoses. There were separate studies focused on the molecular genetic origins of obsessive-compulsive disorder, generalized anxiety disorder, posttraumatic stress disorder, and so on. Analogously, there are voluminous literatures on childhood maltreatment in relation to various individual syndromes. These lines of research have consumed considerable resources, but they have revealed few (if any) replicable one-to-one associations between risks and disorders. A more parsimonious and efficient approach is to recruit participants on the basis of a particular psychopathological dimension (e.g., antisocial behavior, excitement seeking), either sampling to ensure adequate representation of all ranges of this dimension, or recruiting at random from the population of interest (e.g., community, students, or outpatients) to provide a representative sample.4 Then, as was the case for our fictional study of autonomic disruptions in social phobia, the effects of both general and more specific dimensions of psychopathology can be compared empirically. Thinking broadly, such a strategy promises to facilitate more cumulative, rapid progress in developing etiological models for a wide range of psychological conditions.
It merits comment that some of these recommendations can be addressed after the fact. Many of the analyses that we have reviewed were carried out using datasets that were not assembled with HiTOP in mind. However, these projects have generally included a thorough assessment of psychopathology outcomes, which can serve as building blocks for quantitative investigations of symptom or syndrome co-occurrence via factor analysis or related techniques. For example, there have been several studies of the correlates (e.g., demographic features, racial discrimination, childhood maltreatment) of higher order dimensions versus syndromes in epidemiological studies, such as the National Comorbidity Survey-Replication and NESARC (e.g., Eaton et al., 2013; Keyes et al., 2012; Slade, 2007). Investigators have also taken advantage of comprehensive psychopathology assessments in longitudinal cohort studies—such as the Dunedin Multidisciplinary Health and Development Study and the Pittsburgh Girls Study—to examine the temporal course and longitudinal correlates of HiTOP dimensions (e.g., Krueger et al., 1998; Lahey et al., 2015; McElroy, Belsky, Carragher, Fearon, & Patalay, in press). These cohort studies are particularly valuable for theory building because they tend to have rich assessments of validators (etiological factors, clinical outcomes; e.g., Caspi et al., 2014).
Studies need not have especially large samples or wide-ranging assessment batteries (e.g., “big data”) to take advantage of the HiTOP framework. Often, dimensional measures of psychopathology can be integrated into typical (in terms of resources and sample size) study designs. Take, for example, the fictional study of autonomic reactivity described earlier. We described a scenario in which diagnoses were the basic units of mental illness and were used to infer standing on the next higher-level dimensions (i.e., the subfactor and spectrum levels). However, analogous tests could be carried out if researchers administered a self-report questionnaire assessing both the broad and specific features of the internalizing domain, such as the Inventory of Depression and Anxiety Symptoms (Watson et al., 2012). For instance, the effect of lower order symptom components (e.g., lassitude, obsessions; cf. Figure 3 path c) on autonomic reactivity could be compared to the effect of a higher-level (e.g., spectrum) dimension (e.g., dysphoria; cf. Figure 3 path a). We expect that, in most research situations, moderately sized samples would suffice to precisely gauge these effects. More generally, we expect that empirically derived, dimensional measures of mental illness can be integrated effectively into most standard research designs. Along those lines, we plan to publish a series of “worked examples” on the HiTOP consortium website that illustrate the methodological and data analytic steps—including relevant materials, data, and code—in typical studies that apply the HiTOP framework.
Assessment.
Although assessing multiple syndromic or symptom constructs in the same study represents an improvement over “one disorder, one outcome” designs, there are limitations to this approach. DSM/ICD diagnoses and many symptom measures are notoriously heterogeneous, meaning they are composed of multiple lower order dimensions of psychopathology. For instance, many common depressive symptom scales include not only cognitive and vegetative symptoms, which arguably have separate etiologies and correlates, but also include anxiety symptoms (e.g., Fried, 2017). Thus, a more optimal approach is to forego traditional diagnostic constructs in favor of assessing lower order dimensions of pathology (e.g., the symptom component level of Figure 1). This strategy maximizes the precision of the dimensions that can be examined, improving our ability to “carve nature at its joints.”
Consequently, we recommend using assessment instruments that measure both higher and lower order dimensions of psychopathology. A number of such measures are reviewed in Kotov et al. (2017). No omnibus inventory yet exists that covers the entirety of the HiTOP framework, although our consortium is currently developing one. Instead, there are many existing measures that assess specific aspects (e.g., component/trait, syndrome, and subfactor levels) of the HiTOP model (see https://psychology.unt.edu/hitop). Researchers can use these measures to perform a complete assessment of one spectrum (e.g., antagonistic externalizing) or several (e.g., antagonistic externalizing, disinhibited externalizing, thought disorder). The list of measures is expected to continue evolving, and researchers can refer to the HiTOP website to access the latest inventories, including a forthcoming comprehensive measure of the full HiTOP model, as currently constituted. At present, most facets of the HiTOP structure can be assessed economically with questionnaire measures that are available in self- and informant-report versions. Structured and semi-structured interview approaches can also be used, assuming they allow for dimensional scoring. Of course, for such assessments to be compatible with HiTOP, they may need to be modified to eliminate “skip rules” (e.g., if neither significant depressed mood or anhedonia is endorsed, some interview procedures automatically exit the major depression section) and hierarchical decision rules (e.g., DSM-IV stipulated that generalized anxiety disorder could not be diagnosed if it presented only in the context of a co-occurring depressive disorder) in order to collect all symptom data. Overriding these rules permits assessment of the full clinical picture.
Analysis.
There are several different ways for investigators to test the association of dimensional constructs with outcomes of interest. Expertise with latent variable modeling is not a prerequisite. Many popular measurement tools (e.g., the Child Behavior Checklist; Achenbach, 1991) include a combination of broad (e.g., externalizing) and narrow (e.g., aggression) dimensions. Connections of these scales with background characteristics or clinical outcomes could then be contrasted using standard regression approaches.
In the case of large samples, it is possible to use latent variable modeling to empirically extract the relevant dimensions. Exploratory factor analysis (EFA) is an atheoretical approach to determining the appropriate number and nature of latent dimensions undergirding psychological problems. In many common statistical packages, it is possible to perform an EFA and then extract factor scores—values that represent a person’s standing on a latent dimension—that can be used as variables in standard regression or analysis of variance procedures (although this procedure has some drawbacks; e.g., Devlieger, Mayer, & Rosseel, 2016). Confirmatory factor analysis, a hypothesis-driven approach in which the researcher specifies the relations of symptom or diagnostic constructs to latent dimensions, is another common approach. Finally, Goldberg’s (2006) approach of using a series of factor analyses to explicate a hierarchical factor structure, by proceeding from higher (broader) to lower (narrower) levels of specificity (termed the “bass-ackwards” method), can be useful in extracting HiTOP dimensions from symptom- or diagnostic-level data.
Future Challenges
There are clear and compelling scientific reasons to adopt HiTOP-style approaches to understanding psychopathology. But it is equally clear that additional work will be required to refine this framework and determine its optimal role in mental illness research. Uncertainties remain about several architectural elements of HiTOP. Additional research is needed to incorporate psychiatric problems not currently included in HiTOP (e.g., autism spectrum disorder and other neurodevelopmental conditions) and to validate the placement of domains of psychopathology that have received limited attention in structural studies (e.g., lower order dimensions of mania as components of internalizing versus thought disorder). At the spectrum level, data are particularly limited for HiTOP’s somatoform and detachment dimensions. Further, continued research is needed on possible latent taxa, as opposed to dimensions, involved in mental illness. Taxometric research has favored dimensions over categories for every HiTOP construct that has been examined to date; however, in theory, “zones of discontinuity” could emerge and would therefore merit inclusion in the HiTOP model. For example, deviation on multiple dimensions may yield discontinuous cutpoints (cf. Kim & Eaton, 2017). In short, the HiTOP framework is a work in progress and researchers are encouraged to consult the consortium website for updates or to apply for membership in the consortium and contribute to improving the model.
Moving forward, we also need to examine carefully the use and interpretation of factor analysis with respect to HiTOP. There are questions about whether the theoretical constructs outlined in HiTOP satisfy assumptions of the common factor model (e.g., van Bork, Epskamp, Rhemtulla, Borsboom, & van der Maas, 2017; see also Borsboom, Mellenbergh, & van Heerden, 2003). For instance, are the factors (e.g., fear, detachment) naturally occurring phenomena that directly cause variation in their indicators (e.g., panic, social phobia)? Or are the HiTOP factors simply useful—and, to some extent, artificial—summaries of symptom covariation (see Jonas & Markon, 2016)? We note that although factor analysis has proved to be a useful tool in this area of research, HiTOP outcomes need not be represented by latent variables; it is possible to operationalize them directly using questionnaire and interview measures of the types mentioned earlier, although every specific measure has strengths, weakness, and a particular range of applicability, so it will be important not to equate measures with constructs.
Additional work will also be required to better understand the degree to which HiTOP is compatible with network models and the RDoC framework (e.g., Clark et al., 2017; Fried & Cramer, 2017). Network models conventionally assume that psychopathology does not reflect latent traits; psychological syndromes instead arise from a chain reaction of symptoms activating one another (e.g., Cramer, Waldorp, van der Maas, & Borsboom, 2010). A common example is that a constellation of depression symptoms might coalesce not because of the guiding influence of an unobserved, unitary depression dimension, but rather due to a “snowballing” sequence of symptom development (e.g., insomnia → fatigue, fatigue → concentration problems, and so on). The purpose of the network model is to discern these hypothesized causal pathways among symptoms. In contrast, HiTOP aims to identify replicable clusters of symptoms that have shared risk factors and outcomes. Both perspectives can be useful for understanding the nature of psychopathology and are not necessarily mutually exclusive (e.g., Fried & Cramer, 2017).
Like HiTOP, the National Institute of Mental Health’s RDoC initiative deconstructs psychopathology into more basic units that cut across traditional diagnoses (Table 1). However, its primary focus is on fundamental biobehavioral processes (e.g., reward, anxiety), especially those conserved across species, that are disrupted in mental illness (Clark et al., 2017). This approach has gained traction in biological psychology and psychiatry as an alternative to DSM diagnoses, but its utility for other areas of research may be more limited because RDoC does not specifically model the observable signs and symptoms of mental illness that are the subject of most theories of psychopathology. That is, it does not include detailed representations of clinical phenotypes (e.g., aggression, narcissism, emotional lability) that are common targets in research on organizations, close relationships, social groups, aging, psychotherapy, and many other fields wherein the prevailing theoretical models have little (or no) biological emphasis.
Table 1.
Prominent mental illness frameworks
| DSM | HiTOP | RDoC | |
|---|---|---|---|
| Empirical foundation | Historically was based on clinical heuristics; recent revisions are guided by systematic review of research evidence | Data driven; observed clustering of psychopathology signs and symptoms | Expert workgroup interpretation of research evidence |
| Structure | Signs and symptoms are organized into diagnoses, which are in turn grouped into chapters on the basis of shared phenomenology and/or presumed etiology; some disorders include subtypes | Hierarchical system of broad constructs near the top and homogeneous symptom components near the bottom | Five domains of functioning (e.g., negative valence) each divided into 3 to 6 constructs (e.g., acute threat); domains encompass 7 units of analysis, from molecules to verbal report |
| Dimensional vs categorical | Predominantly categorical, but contains optional dimensional elements for screening and diagnosis, such as the Alternative Model for Personality Disorder | Dimensional, but able to incorporate categories (“taxa”) if empirically warranted | Explicitly focused on dimensional processes |
| Timeframe for clinical implementation | Widely used | Able to guide assessment and treatment, but currently not disseminated widely for direct clinical application | Limited prospects for clinical applications in near-term (e.g., assessment, treatment, communication) |
| Etiology | Diagnosis generally is based on observed signs and symptoms, not putative causes (posttraumatic stress disorder is an exception) | Model structure depends on observed (phenotypic) clustering—not necessarily etiological coherence—of clinical problems; model dimensions can be validated with respect to putative etiological factors | Conceptualizes clinical problems as “brain disorders”; neurobiological correlates of mental illness are emphasized |
Note. DSM = Diagnostic and Statistical Manual of Mental Disorders; HiTOP = Hierarchical Taxonomy of Psychopathology; RDoC = Research Domain Criteria.
A complementary nosological framework is needed to link the basic science discoveries spurred by RDoC—and similar NIH initiatives, such as the National Institute of Alcohol Abuse and Alcoholism’s Addictions Neuroclinical Assessment and the National Institute of Drug Abuse’s Phenotyping Assessments Battery—to the signs and symptoms that lead people to seek treatment. HiTOP, which provides a clear and comprehensive system of clinical phenotypes, offers such a bridge. Research that integrates these dimensional frameworks has the potential to make RDoC clinically relevant and to provide important insights into the biological bases of the dimensions embodied in the HiTOP framework.
Whereas RDoC proponents acknowledge that it is unlikely to have much applied clinical value in the near-term, HiTOP is poised for clinical implementation. HiTOP encapsulates clinical problems that practitioners are familiar with and routinely encounter. Existing questionnaire and interview measures that capture HiTOP dimensions can be administered to patients or other informants (Kotov et al., 2017). Normative data are available for many measures and will continue to accrue (e.g., Stasik-O’Brien et al., in press). Clinicians can use dimensional scores to compare patients’ scores to clinical cutoffs or other norms to inform decisions about prognosis and treatment (see Ruggero et al., 2018). Moreover, dimensional measures are more useful for monitoring treatment progress than are categorical diagnoses because they tend to be more sensitive to change while also yielding more reliable change indices (e.g., Kraemer, Noda, & O’Hara, 2004). One of the most important challenges for the future will be to gather appropriate normative data for more instruments and refine their use in clinical assessment and treatment planning.
The hierarchical structure of HiTOP implies that targeting higher order dimensions, like the internalizing spectrum, may cause therapeutic effects to percolate across multiple DSM conditions, augmenting the efficiency of psychological treatment. For example, the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (Barlow et al., 2014) was developed to act on common temperamental processes theorized to lie at the core of internalizing problems. Rather than using separate protocols to treat individual diagnoses, such as major depression and generalized anxiety disorder, the Unified Protocol uses cognitive-behavioral strategies to reduce negative emotionality and increase positive emotionality, traits thought to maintain anxiety and depression over time, and there is emerging evidence that such transdiagnostic psychotherapies can be as effective as traditional (i.e., diagnosis-specific) treatments (Barlow et al., 2017). Practitioners can apply the Unified Protocol to a diverse set of anxiety and depressive conditions, streamlining the training process and minimizing barriers to dissemination, as compared to standard training models that involve learning a separate treatment framework for each disorder (Steele et al., 2018). The policy of using one psychological treatment for various conditions is analogous to standard prescription practices for psychiatric medications, which often work across—and in many cases have regulatory approval for treatment of—multiple diagnoses.
The most important avenue for future empirical work, in our view, is continued validation research into the utility (for research and theory building) of the dimensions that make up the HiTOP model. In particular, validation studies to date have been mostly limited to the spectrum level (e.g., correlates of internalizing, disinhibited externalizing), and criterion-validity research is needed at other levels of the hierarchy. Also, existing research has largely relied on snapshots of symptoms and syndromes without modeling illness course. Longitudinal studies that are designed to examine the correlates and structure of HiTOP dimensions in diverse samples across the lifespan are a pressing priority (cf. Lahey et al., 2015; Wright, Hopwood, Skodol, & Morey, 2016), as is research on the short-term dynamics of psychopathology symptoms (e.g., Wright & Simms, 2016). Although research has supported the invariance of the internalizing and externalizing spectra across gender, developmental stages, and various racial, ethnic, and cultural groups (see Rodriguez-Seijas et al., 2015), investigation of other HiTOP dimensions with regard to aging, culture, context, and so forth will be important.
Conclusion
There is compelling evidence that the nature of psychopathology is dimensional and hierarchical, with many studies indicating that genes, neurobiology, and clinical outcomes align with this new conceptualization. We recommend a shift in mental health research practices to match the HiTOP model. This emerging system has the potential to (i) expand existing theories and generate new hypotheses; (ii) unify unnecessarily fragmented empirical literatures; (iii) increase the utility of classification systems for both basic and applied research; and (iv) establish novel phenotypes that explain the etiology of psychological problems and serve as more efficient assessment and treatment targets. Although many important challenges remain, HiTOP has the potential to transform research practices for the better and accelerate theory development across diverse areas of psychological science.
Acknowledgments:
This paper was organized by members of the HiTOP Consortium, a grassroots organization open to all qualified investigators (https://medicine.stonybrookmedicine.edu/HITOP/).
Footnotes
Footnotes
Unlike DSM and ICD workgroups, HiTOP membership has developed organically rather than through selection. The consortium was founded by Roman Kotov, Robert Krueger, and David Watson, who invited all scientists with significant publication records on quantitative mental-health nosologies to join the consortium. As the consortium grew and gained greater recognition, scientists began contacting the consortium offering to contribute their effort.
We emphasize, however, that it is optimal from a HiTOP perspective to orient data collection around more homogeneous signs and symptoms of mental disorder (e.g., Markon, 2010; Waszczuk, Kotov, Ruggero, Gamez, & Watson, 2017).
Incidentally, this is roughly the same recruitment strategy recommended under the RDoC framework.
References
- Achenbach TM (1966). The classification of children’s psychiatric symptoms: A factor-analytic study. Psychological Monographs, 80, 1–37. [DOI] [PubMed] [Google Scholar]
- Achenbach TM (1991). Manual for the child behavior checklist/4–18 and 1991 profile. Burlington: University of Vermont, Department of Psychiatry. [Google Scholar]
- Achenbach TM, Howell CT, Quay HC, Conners CK, & Bates JE (1991). National Survey of problems and competencies among four- to sixteen-year-olds: Parents’ reports for normative and clinical samples. Monographs of the Society for Research in Child Development, 56, 1–131. [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, …, & Cassiello-Robbins C (2017). The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry, 74, 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, & Ellard KK (2014). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2, 344–365. [Google Scholar]
- Borsboom D, Mellenbergh GJ, & Van Heerden J (2003). The theoretical status of latent variables. Psychological Review, 110, 203–219. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Rhemtulla M, Cramer AOJ, van der Maas HLJ, Scheffer M, & Dolan CV (2016). Kinds versus continua: a review of psychometric approaches to uncover the structure of psychiatric constructs. Psychological Medicine, 1–13. [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH (2009). A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment, 21, 256–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (in press). All for one and one for all: Mental disorders in one dimension American Journal of Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh JF, & Shackman AJ (2015). Frontal midline theta reflects anxiety and cognitive control: Meta-analytic evidence. Journal of Physiology, 109, 3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Cuthbert B, Lewis-Fernández R, Narrow WE, & Reed GM (2017). Three Approaches to Understanding and Classifying Mental Disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). Psychological Science in the Public Interest, 18, 72–145. [DOI] [PubMed] [Google Scholar]
- Cramer AO, Waldorp LJ, van der Maas HL, & Borsboom D (2010). Complex realities require complex theories: Refining and extending the network approach to mental disorders. Behavioral and Brain Sciences, 33, 178–193. [Google Scholar]
- Conway CC, Hammen C, & Brennan PA (2012). Expanding stress generation theory: Test of a transdiagnostic model. Journal of Abnormal Psychology, 121, 754–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway CC, Raposa EB, Hammen C, & Brennan PA (2018). Transdiagnostic pathways from early social stress to psychopathology: a 20-year prospective study. Journal of Child Psychology and Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert BN, & Insel TR (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11, 126–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devlieger I, Mayer A, & Rosseel Y (2016). Hypothesis testing using factor score regression: A comparison of four methods. Educational and Psychological Measurement, 76, 741–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLuca M, & Olesen J (2014). The cost of brain diseases: a burden or a challenge?. Neuron, 82, 1205–1208. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Markon KE, Keyes KM, Skodol AE, Wall M, … Grant BF (2013). The structure and predictive validity of the internalizing disorders. Journal of Abnormal Psychology, 122, 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ (1944). Types of personality: a factorial study of seven hundred neurotics. The British Journal of Psychiatry, 90, 851–861. [Google Scholar]
- Forbes MK, Tackett JL, Markon KE, & Krueger RF (2016). Beyond Comorbidity: Toward a dimensional and hierarchal approach to understanding psychopathology across the lifespan. Development and Psychopathology, 28, 971–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbush KT, Hagan KE, Kite BA, Chapa DA, Bohrer BK, & Gould SR (2017). Understanding eating disorders within internalizing psychopathology: A novel transdiagnostic, hierarchical-dimensional model. Comprehensive Psychiatry, 79, 40–52. [DOI] [PubMed] [Google Scholar]
- Fried EI (2017). The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. Journal of Affective Disorders, 208, 191–197. [DOI] [PubMed] [Google Scholar]
- Fried EI, & Cramer AOJ (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science, 12, 999–1020. [DOI] [PubMed] [Google Scholar]
- Goldberg LR (2006). Doing it all bass-ackwards: The development of hierarchical factor structures from the top down. Journal of Research in Personality, 40, 347–358. [Google Scholar]
- Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, …, Etkin A (2015). Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry, 72, 305–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon JA, & Redish AD (2016). On the cusp. Current challenges and promises in psychiatry In Redish AD & Gordon JA (Eds.), Computational psychiatry: New perspectives on mental illness (pp. 3–14). Cambridge, MA: MIT Press. [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67, 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C (1991). Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology, 100, 555–561. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, & McGue M (2003). Substance use disorders, externalizing psychopathology, and P300 event-related potential amplitude. International Journal of Psychophysiology, 48, 147–178. [DOI] [PubMed] [Google Scholar]
- Hyman SE (2007). Can neuroscience be integrated into the DSM-V?. Nature Reviews Neuroscience, 8, 725–732. [DOI] [PubMed] [Google Scholar]
- Jonas KG, & Markon KE (2013). A model of psychosis and its relationship with impairment. Social Psychiatry and Psychiatric Epidemiology, 48, 1367–1375. [DOI] [PubMed] [Google Scholar]
- Jonas KG, & Markon KE (2016). A descriptivist approach to trait conceptualization and inference. Psychological Review, 123, 90–96. [DOI] [PubMed] [Google Scholar]
- Kaczkurkin AN, Moore TM, Calkins ME, Ciric R, Detre JA, Elliott MA, … & Ruparel K (in press). Common and dissociable regional cerebral blood flow differences associate with dimensions of psychopathology across categorical diagnoses Molecular Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, & Neale MC (2013). Evidence for multiple genetic factors underlying DSM-IV criteria for major depression. JAMA Psychiatry, 70, 599–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, & Myers J (2014). The boundaries of the internalizing and externalizing genetic spectra in men and women. Psychological Medicine, 44, 647–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, & Zaslavsky AM (2011). The role of latent internalizing and externalizing predispositions in accounting for the development of comorbidity among common mental disorders. Current Opinion in Psychiatry, 24, 307–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, & Eaton NR (2017). A hierarchical integration of person-centered comorbidity models: structure, stability, and transition over time. Clinical Psychological Science, 5, 595–612. [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, & Hasin DS (2012). Childhood maltreatment and the structure of common psychiatric disorders. The British Journal of Psychiatry, 200, 107–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … & Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. [DOI] [PubMed] [Google Scholar]
- Kotov R, Perlman G, Gámez W, & Watson D (2015). The structure and short-term stability of the emotional disorders: a dimensional approach. Psychological Medicine, 45, 1687–1698. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Noda A, & O’Hara R (2004). Categorical versus dimensional approaches to diagnosis: methodological challenges. Journal of Psychiatric Research, 38, 17–25. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, & Silva PA (1998). The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology, 107, 216–227. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Kotov R, Watson D, Forbes MK, Eaton NR, Ruggero CJ, … Zimmermann J (in press). Progress in achieving quantitative classification of psychopathology World Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, & Rathouz PJ (2012). Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology, 121, 971–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143, 142–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Keenan K, Stepp SD, Loeber R, & Hipwell AE (2015). Criterion validity of the general factor of psychopathology in a prospective study of girls. Journal of Child Psychology and Psychiatry, 4, 415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79, 159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL, & Vernon PA (1998). Phenotypic and genetic structure of traits delineating personality disorder. Archives of General Psychiatry, 55, 941–948. [DOI] [PubMed] [Google Scholar]
- Liu RT, & Alloy LB (2010). Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review, 30, 582–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorr M, Klett CJ, & McNair DM (1963). Syndromes of psychosis. New York, NY: Pergamon Press. [Google Scholar]
- Markon KE (2010). Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological Medicine, 40, 273–288. [DOI] [PubMed] [Google Scholar]
- Markon KE, Chmielewski M, & Miller CJ (2011). The reliability and validity of discrete and continuous measures of psychopathology: a quantitative review. Psychological Bulletin, 137, 856. [DOI] [PubMed] [Google Scholar]
- McElroy E, Belsky J, Carragher N, Fearon RMP, & Patalay P (in press). Developmental stability of general and specific factors of psychopathology from early childhood through adolescence: Dynamic mutualism or p-differentiation?. Journal of Child Psychology and Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Zhang Y, Miller MB, Basu S, Vrieze S, Hicks B, … & Iacono WG (2013). A genome-wide association study of behavioral disinhibition. Behavior Genetics, 43, 363–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA (2016). Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child & Adolescent Psychology, 45, 361–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Busso DS, Duys A, Green JG, Alves S, Way M, & Sheridan MA (2014). Amygdala response to negative stimuli predicts PTSD symptom onset following a terrorist attack. Depression and Anxiety, 31, 834–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTeague LM, Huemer J, Carreon DM, Jiang Y, Eickhoff SB, & Etkin A (2017). Identification of common neural circuit disruptions in cognitive control across psychiatric disorders. American Journal of Psychiatry, 174, 676–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer A (2017). A biomarker of anxiety in children and adolescents: A review focusing on the error-related negativity (ERN) and anxiety across development. Developmental Cognitive Neuroscience, 27, 58–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers JL, Lowe SR, Eaton NR, Krueger R, Grant BF, & Hasin D (2015). Childhood maltreatment, 9/11 exposure, and latent dimensions of psychopathology: A test of stress sensitization. Journal of Psychiatric Research, 68, 337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE (1993). Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychological Review, 100, 674. [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ, Markowitz JC, Gunderson JG, Grilo CM, McGlashan TH, … Skodol AE (2012). Comparison of alternative models for personality disorders, II: 6-, 8- and 10-year follow-up. Psychological Medicine, 42, 1705–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muetzel RL, Blanken LM, van der Ende J, El Marroun H, Shaw P, Sudre G, … & White T (2018). Tracking brain development and dimensional psychiatric symptoms in children: A longitudinal population-based neuroimaging study. American Journal of Psychiatry, 1, 54–62. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, & Watson D (2011). The anxiety disorders and suicidal ideation: accounting for co-morbidity via underlying personality traits. Psychological Medicine, 41, 1437–1447. [DOI] [PubMed] [Google Scholar]
- Neumann A, Pappa I, Lahey BB, Verhulst FC, Medina-Gomez C, Jaddoe VW, … & Tiemeier H (2016). Single nucleotide polymorphism heritability of a general psychopathology factor in children. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 1038–1045. [DOI] [PubMed] [Google Scholar]
- Olino TM, Bufferd SJ, Dougherty LR, Dyson MW, Carlson GA, & Klein DN (in press). The development of latent dimensions of psychopathology across early childhood: stability of dimensions and moderators of change. Journal of Abnormal Child Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otowa T, Hek K, Lee M, Byrne EM, Mirza SS, Nivard MG, … & Fanous A (2016). Meta-analysis of genome-wide association studies of anxiety disorders. Molecular psychiatry, 21, 1391–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Bernat EM, Malone SM, Iacono WG, Krueger RF, & McGue M (2006). P300 amplitude as an indicator of externalizing in adolescent males. Psychophysiology, 43, 84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, & Hajcak G (2016). RDoC: Translating promise into progress. Psychophysiology, 53, 415–424. [DOI] [PubMed] [Google Scholar]
- Pettersson E, Larsson H, & Lichtenstein P (2016). Common psychiatric disorders share the same genetic origin: A multivariate sibling study of the Swedish population. Molecular Psychiatry, 21, 717–721. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, MacCallum RC, & Nicewander WA (2005). Use of the extreme groups approach: A critical reexamination and new recommendations. Psychological Methods, 10, 178–192. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Clarke DE, Kraemer HC, Kuramoto SJ, Kuhl EA, & Kupfer DJ (2013). DSM-5 field trials in the United States and Canada, Part II: Test-retest reliability of selected categorical diagnoses. The American Journal of Psychiatry, 170, 59–70. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, Stohl M, Mauro PM, & Hasin DS (2017). Mental disorder comorbidity and treatment utilization. Comprehensive Psychiatry, 79, 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Stohl M, Hasin DS, & Eaton NR (2015). Transdiagnostic factors and mediation of the relationship between perceived racial discrimination and mental disorders. Journal of the American Medical Association Psychiatry, 72, 706–713. [DOI] [PubMed] [Google Scholar]
- Romer AL, Knodt AR, Houts R, Brigidi BD, Moffitt TE, Caspi A, & Hariri AR (2018). Structural alterations within cerebellar circuitry are associated with general liability for common mental disorders. Molecular Psychiatry, 23, 1084–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenström T, Ystrom E, Torvik FA, Czajkowski NO, Gillespie NA, Aggen SH, … Reichborn-Kjennerud T (2017). Genetic and environmental structure of DSM-IV criteria for antisocial personality disorder: A twin study. Behavior Genetics, 47, 265–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Røysamb E, Kendler KS, Tambs K, Ørstavik RE, Neale MC, Aggen SH, … & Reichborn-Kjennerud T (2011). The joint structure of DSM-IV Axis I and Axis II disorders. Journal of Abnormal Psychology, 120, 198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggero C (2018, August 18). Integrating a Dimensional, Hierarchical Taxonomy of Psychopathology into Clinical Practice. Retrieved from psyarxiv.com/r2jt6 [Google Scholar]
- Sato JR, Salum GA, Gadelha A, Crossley N, Vieira G, Manfro GG, … Hoexter MQ (2016). Default mode network maturation and psychopathology in children and adolescents. Journal of Child Psychology and Psychiatry, 57, 55–64. [DOI] [PubMed] [Google Scholar]
- Selzam S, Coleman JR, Moffitt TE, Caspi A, & Plomin R (2018). A polygenic p factor for major psychiatric disorders. bioRxiv, 287987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shackman AJ, & Fox AS (2018). Getting serious about variation: Lessons for clinical neuroscience (A commentary on ‘The myth of optimality in clinical neuroscience’). Trends in Cognitive Sciences, 22, 368–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanmugan S, Wolf DH, Calkins ME, Moore TM, Ruparel K, Hopson RD, … & Gennatas ED (2016). Common and dissociable mechanisms of executive system dysfunction across psychiatric disorders in youth. American Journal of Psychiatry, 173, 517–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Wolf DH, Ciric R, Kable JW, Moore TM, Vandekar SN, … & Elliott MA (2017). Common dimensional reward deficits across mood and psychotic disorders: a connectome-wide association study. American Journal of Psychiatry, 174, 657–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simms LJ, Grös DF, Watson D, & O’Hara MW (2008). Parsing the general and specific components of depression and anxiety with bifactor modeling. Depression and Anxiety, 25, 34–46. [DOI] [PubMed] [Google Scholar]
- Slade T (2007). The descriptive epidemiology of internalizing and externalizing psychiatric dimensions. Social Psychiatry and Psychiatric Epidemiology, 42, 554–560. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Andreassen OA, Edenberg HJ, Faraone SV, Glatt SJ, & Kendler KS (2018). Psychiatric genetics and the structure of psychopathology. Molecular Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Hankin BL, Sandman CA, Head K, & Davis EP (2017). Distinct patterns of reduced prefrontal and limbic gray matter volume in childhood general and internalizing psychopathology. Clinical Psychological Science, 5, 1001–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017). Chronic stress exposure and generation are related to the p-factor and externalizing specific psychopathology in youth. Journal of Clinical Child and Adolescent Psychology, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South SC, Krueger RF, & Iacono WG (2011). Understanding general and specific connections between psychopathology and marital distress: A model based approach. Journal of Abnormal Psychology, 120, 935–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprooten E, Rasgon A, Goodman M, Carlin A, Leibu E, Lee WH, & Frangou S (2017). Addressing reverse inference in psychiatric neuroimaging: Meta-analyses of task-related brain activation in common mental disorders. Human Brain Mapping, 38, 1846–1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasik-O’Brien SM, Brock RL, Chmielewski M, Naragon-Gainey K, Koffel E, McDade-Montez E, … & Watson D (in press). Clinical utility of the Inventory of Depression and Anxiety Symptoms (IDAS). Assessment. 10.1177/1073191118790036 [DOI] [PubMed] [Google Scholar]
- Steele SJ, Farchione TJ, Cassiello-Robbins C, Ametaj A, Sbi S, Sauer-Zavala S, & Barlow DH (2018). Efficacy of the Unified Protocol for transdiagnostic treatment of comorbid psychopathology accompanying emotional disorders compared to treatments targeting single disorders. Journal of Psychiatric Research, 104, 211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Vidal-Ribas Belil P, Artiges E, Lemaitre H, Gollier-Briant F, Wolke S, … & Fadai T (2015). The brain’s response to reward anticipation and depression in adolescence: dimensionality, specificity, and longitudinal predictions in a community-based sample. American Journal of Psychiatry, 172, 1215–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunderland M, Carragher N, Chapman C, Mills K, Teesson M, Lockwood E, … & Slade T (2016). The shared and specific relationships between exposure to potentially traumatic events and transdiagnostic dimensions of psychopathology. Journal of Anxiety Disorders, 38, 102–109. [DOI] [PubMed] [Google Scholar]
- Sunderland M, & Slade T (2015). The relationship between internalizing psychopathology and suicidality, treatment seeking, and disability in the Australian population. Journal of Affective Disorders, 171, 6–12. [DOI] [PubMed] [Google Scholar]
- Swartz JR, Knodt AR, Radtke SR, & Hariri AR (2015). A neural biomarker of psychological vulnerability to future life stress. Neuron, 85, 505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarbox SI, & Pogue-Geile MF (2011). A multivariate perspective on schizotypy and familial association with schizophrenia: a review. Clinical Psychology Review, 31, 1169–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellegen A (1985). Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report In Tuma AH & Maser JD (Eds.), Anxiety and the anxiety disorders (pp. 681–706). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, & Cicchetti D (2015). Assessment of the harmful psychiatric and behavioral effects of different forms of child maltreatment. JAMA Psychiatry, 72, 1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Bork R, Epskamp S, Rhemtulla M, Borsboom D, & van der Maas HL (2017). What is the p-factor of psychopathology? Some risks of general factor modeling. Theory & Psychology, 27, 759–773. [Google Scholar]
- van Os J, Gilvarry C, Bale R, Van Horn E, Tattan T, & White I (1999). A comparison of the utility of dimensional and categorical representations of psychosis. Psychological Medicine, 29, 595–606. [DOI] [PubMed] [Google Scholar]
- Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, … & Coggeshall M (2016). Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet, 388, 1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward J, Strawbridge R, Graham N, Bailey M, Freguson A, Lyall D, … & Pell J (2017). Genome-Wide Analysis Of 113,968 Individuals In UK Biobank Identifies Four Loci Associated With Mood Instability. bioRxiv, 117796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waszczuk M (2018, August 28). Redefining phenotypes to advance psychiatric genetics: Implications from the hierarchical taxonomy of psychopathology. 10.31234/osf.io/sf46g [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waszczuk MA, Kotov R, Ruggero C, Gamez W, & Watson D (2017). Hierarchical structure of emotional disorders: From individual symptoms to the spectrum. Journal of Abnormal Psychology, 126, 613. [DOI] [PubMed] [Google Scholar]
- Waszczuk MA, Zavos HMS, Gregory AM, & Eley TC (2014). The phenotypic and genetic structure of depression and anxiety disorder symptoms in childhood, adolescence, and young adulthood. JAMA Psychiatry, 71, 905–916. [DOI] [PubMed] [Google Scholar]
- Waszczuk MA, Zimmerman M, Ruggero C, Li K, MacNamara A, Weinberg A, … & Kotov R (2017). What do clinicians treat: Diagnoses or symptoms? The incremental validity of a symptom-based, dimensional characterization of emotional disorders in predicting medication prescription patterns. Comprehensive Psychiatry, 79, 80–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins JL, Mitchell C, Hyde LW, & Monk CS (2015). Identifying early pathways of risk and resilience: The codevelopment of internalizing and externalizing symptoms and the role of harsh parenting. Development and Psychopathology, 27, 1295–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AG, Hopwood CJ, Skodol AE, & Morey LC (2016). Longitudinal validation of general and specific structural features of personality pathology. Journal of Abnormal Psychology, 125, 1120–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zald DH, & Lahey BB (2017). Implications of the hierarchical structure of psychopathology for psychiatric neuroimaging. Biological Psychiatry, 2, 310–317. [DOI] [PMC free article] [PubMed] [Google Scholar]