Abstract
Outer membrane vesicle (OMV)- based vaccines have been used to provide strain-specific protection against capsular group B Neisseria meningitidis infections, but the full breadth of the immune response against the components of the OMV has not been established. Sera from adults vaccinated with an OMV vaccine were used to screen 91 outer membrane proteins (OMPs) incorporated in an antigen microarray panel. Antigen-specific IgG levels were quantified pre-vaccination, and after 12 and 18 weeks. These results were compared with IgG levels from mice vaccinated with the same OMV vaccine. The repertoires of highly responding antigens in humans and mice overlapped, but were not identical. The highest responding antigens to human IgG comprised four integral OMPs (PorA, PorB, OpcA and PilQ), a protein which promotes the stability of PorA and PorB (RmpM) and two lipoproteins (BamC and GNA1162). These observations will assist in evaluating the role of minor antigen components within OMVs in providing protection against meningococcal infection. In addition, the relative dominance of responses to integral OMPs in humans emphasizes the importance of this subclass and points to the value of maintaining conformational epitopes from integral membrane proteins in vaccine formulations.
Subject terms: Lipoproteins, Protein vaccines, Bacteriology, Protein vaccines
Introduction
Neisseria meningitidis is the causative pathogen of meningococcal meningitis and septicaemia. More than 90% of the cases of invasive disease worldwide are caused by six capsular groups, A, B, C, W, X, and Y1. Vaccines based on capsular polysaccharide (CPS) have been effective in preventing and controlling outbreaks of disease attributed to capsular groups A, C, Y and W for many years, and several pentavalent X-polysaccharide-containing vaccines are in development in India. Unfortunately, although capsular group B N. meningitidis (NmB) organisms contribute to most disease cases recorded in developed countries2, there are safety concerns about the use of capsular group B CPS, as it shares similarities to polysialic acid-containing structures in human foetal brain tissue3,4. Outer membrane vesicles (OMVs), which are derived from meningococcal growth cultures by detergent extraction, have been used successfully as vaccines to control clonal outbreaks of NmB infection5–7. However, the sequence hypervariability of several NmB OMPs has hampered the development of a universal vaccine using a single OMV. The protection induced by OMV vaccines is largely directed at the hypervariable PorA antigen, the most abundant protein in OMVs8. There is therefore a need to identify other vaccine candidates that are more conserved and can also provide protection against NmB infections. Proteomic analyses of OMVs have identified well over 100 different protein components, including a large number of integral outer membrane proteins (iOMPs) which, for the purposes of this paper, we define as proteins where the polypeptide chain completely spans the outer membrane at least once9,10. iOMPs generally form membrane-spanning β-barrel folds and several crystal structures are known for meningococcal proteins11–14.
The implementation of reverse vaccinology (RV) has driven the development of 4C-MenB (tradename Bexsero®), a vaccine which comprises recombinant protein antigens in combination with an OMV component15. RV is a multistep process, starting with bioinformatic prediction of surface-expressed proteins, followed by their individual expression and evaluation of immunogenicity in a suitable vaccination model16. However, iOMPs were excluded during the selection process, presumably due to challenges associated with protein expression and folding into their native three-dimensional structures17,18. Clinical trials with the 4C-MenB vaccine showed that inclusion of OMVs from a single strain improved the protection conferred by the recombinant antigens (NadA, NHBA, fHbp, GNA2091 and GNA1030)19–23. These observations point to the potential importance of other OMPs, including iOMPs, in helping to confer protection.
Protein microarrays provide a high throughput platform for the identification of protein-protein interactions24. Screening using antisera derived from vaccinees can be used to identify potential vaccine antigens, as well as diagnostic markers25,26. In order to carry out such a screen, a complete library of component antigens is ideally required. It is, however, very difficult in practical terms to obtain a comprehensive library of proteins, due to the challenges associated with protein expression and ensuring correct protein folding. Some researchers have used high throughput in vitro transcription and translation (IVTT) methods, where proteins are produced in situ, in a cell-free system. This approach is simple, fast and convenient for expressing toxic proteins: it has been used in the profiling of immune responses to infection and identification of diagnostic markers, for example25–28. However, IVTT has some drawbacks: first, there is a need to standardize the amount and homogeneity of the protein in each sample, which can be difficult. Second, many longer polypeptide chains do not express well and formation of multimers is difficult to verify. Finally, proteins need to be folded into their native conformation to preserve conformational epitopes and, again, this can be difficult to verify directly.
In previous work Steller et al. adopted a different approach, by individually expressing and purifying 67 out of 102 phase-variable NmB antigens in recombinant form and using them to create a microarray which was then screened against antisera obtained from meningitis and sepsis patients29. However, purification of iOMPs was carried out under denaturing conditions and hence the conformational epitopes from these proteins were lost: for example, only one out of 20 patient sera tested was reactive against PorA. Here we designed a panel of 91 OMPs, including iOMPs, which have been identified as potential vaccine candidates and are also OMV components10,15. The antisera used were derived from a Phase I study using an OMV preparation from a modified NmB strain H44/76, termed MenPF-1, in which the fetA promoter was modified to ensure constitutive expression of the iron transporter FetA8,30,31. This work represents the most comprehensive attempt yet to compare the immunogenicity of OMP components of an N. meningitidis OMV vaccine in humans and mice. The results highlight the shortcomings of murine antibody responses as predictors of the human immune response and have value in helping to refine the components of meningococcal vaccines in development.
Results
Design and manufacture of the meningococcal antigen microarray
Information was used from previous proteomics and FACS analysis to identify OMV component proteins as potential targets for inclusion in the microarray10,15,32,33. In addition, other protein antigens were considered which, on the basis of more recent work, justified their inclusion (eg Adhesin Complex Protein)34. The sequences of individual open reading frames (ORFs) were searched against the Protein Data Bank, to extract information from homologs about domain structure and optimal expression strategies (eg selection of N- and C-termini to allow isolation of specific domains if expression of the entire protein was likely to prove challenging). The selected antigens covered a diverse range of biological functions, including adhesion, transport and immuno-modulation (Table 1). Not all proteins were necessarily predicted to be surface-exposed; some periplasmic proteins were included because they were present in OMV preparations and potentially could elicit an immunogenic response. In addition, we carried out a separate proteomic analysis on the OMV preparation using multidimensional LC-MS/MS peptide sequencing and searching of the N. meningitidis serogroup B/serotype 15 (strain H44/76) FASTA database. A total of 557 proteins were identified which confirmed the presence of key OMPs in the OMV preparation, including those identified as major responding antigens (Supplementary Table S1).
Table 1.
Classification of purified meningococcal OMP antigens based on their biological functions.
| Functiona | Total | Solubleb | Refolded | Foldedc | Unfolded | |
|---|---|---|---|---|---|---|
| 1 | Adhesion | 9 | 5 | 4 | 9 | 0 |
| 2 | Redox homeostasis | 6 | 6 | 0 | 5 | 1 |
| 3 | Lysozyme inhibition | 2 | 2 | 0 | 2 | 0 |
| 4 | Peptidoglycan binding | 2 | 2 | 0 | 2 | 0 |
| 5 | OM assembly | 6 | 2 | 4 | 6 | 0 |
| 6 | Protein folding | 7 | 7 | 0 | 7 | 0 |
| 7 | Metabolism | 3 | 3 | 0 | 2 | 1 |
| 8 | Unknown function | 4 | 2 | 2 | 3 | 1 |
| 9 | Protein assembly | 1 | 1 | 0 | 0 | 1 |
| 10 | Peptidoglycan synthesis | 4 | 3 | 1 | 4 | 0 |
| 11 | Immunomodulation | 4 | 1 | 3 | 4 | 0 |
| 12 | OM stability | 1 | 1 | 0 | 1 | 0 |
| 13 | Macromolecular transport | 17 | 5 | 12 | 14 | 3 |
| 14 | Micromolecular transport | 25 | 16 | 9 | 22 | 3 |
| 91 | 56 | 35 | 81 | 10 |
aFunctional classification of selected proteins was carried out based on entries in the Pfam database75.
bProteins were classified as soluble or refolded based on their solubility after initial cell disruption.
cBased on thermal fluorescence denaturation profile.
The overall strategy adopted for fabrication of the microarray is shown in Fig. 1. Soluble proteins were expressed and purified by metal chelate affinity chromatography, followed by size exclusion chromatography (SEC). Predicted iOMPs were expressed without their signal sequences, which led to formation of inclusion bodies: they were re-solubilized in urea and refolded by rapid dilution into buffer containing detergent before purification by the same processes. During purification by SEC, we observed that some proteins eluted in more than one oligomeric state (eg monomers and dimers); they were collected separately to determine the contribution of oligomerization to the immune response, bringing the total of separate antigens on the array to 91. More details on the individual proteins are given in Supplementary Table S2.
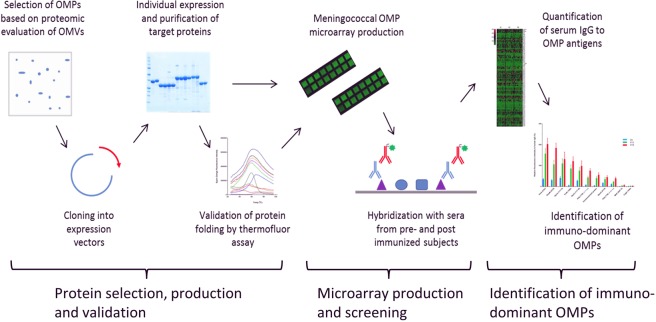
Figure 1.
Work flow for identification of immuno-dominant OMPs. Our strategy is divided into three main steps, namely protein selection, production and validation of expression and folding; protein microarray production and screening and quantification of sero-reactivity and identification of immuno-dominant OMPs.
To evaluate the degree of folding of each purified antigen, we used the measurement of fluorescence of Sypro Orange dye, as a function of temperature: this is a widely used and convenient method which lends itself to high throughput applications35. An example is shown in Supplementary Fig. S1; a peak in the first derivative change in fluorescence with temperature is indicative of an unfolding event. In this example, Neisserial surface protein A (NspA), an iOMP, shows a transition corresponding to the melting temperature at approximately 60 °C, compared with the IgA-specific endopeptidase sample, which shows no transition feature. Of the 91 NmB OMPs in the array, 81 (~90%) gave evidence of folded structure by this criterion. Human and mouse IgG, and Epstein-Barr nuclear antigen 1 (EBNA-1) were included on the array as controls36. Interference arising from antibody binding to traces of contaminant proteins was eliminated by addition of an E. coli soluble lysate and a membrane–enriched extract during primary antibody hybridization37. Microarray glass slides coated with porous nitrocellulose (Grace Biolabs) were used to immobilize the proteins on the slide. The nitrocellulose membrane is porous and captures proteins within its fibrous matrix. This approach offers optimal binding capacity, retains protein conformation and provides longer shelf-life stability38,39. For refolded proteins such as iOMPs, which do not adhere optimally on glass slides, this approach was most suitable for immobilization. The proteins were printed using a non-contact, on-the-fly technology which offers more advantages over contact printing, such as high precision, excellent spot morphology and also avoids protein damage during the contact printing40. Preliminary screening with anti-histidine primary antibodies showed excellent reproducibility within replicate spots and between different miniarrays. All protein spots demonstrated a good morphology and consistency, with no merging.
Identification of antigens providing strongest IgG reactivity in human and murine antisera after OMV vaccination
Serum samples obtained from immunized mice or adult human participants of an OMV vaccine phase I trial were used to probe the microarray slides. The human antisera were obtained from a previous study: high (50 μg OMV protein) or low (25 μg OMV protein) dose vaccine was given every 8 weeks and serum samples collected 4 weeks after each vaccination30. Serum samples used in this study were collected at the following time-points: pre-vaccination (T0), post-second (T12) and post-third vaccinations (T20), 12 and 20 weeks post-vaccination respectively. The mouse antisera are from the terminal bleed of 10 BALB/c mice after two inoculations (3 weeks apart) with 2.5 μg OMV protein8. Protein spots were hybridized with sera from pre- and post-vaccination samples and bound IgG antibodies were detected by the fluorescence signal intensity. Given that all OMPs were printed at the same concentration and most (~88%) retained their native conformation, differences in signal intensity are attributable to the concentration of specific IgG antibodies in the serum. Examples of sample data for human and mouse sera are shown in Fig. 2- the increase in IgG reactivity following inoculation is readily apparent.
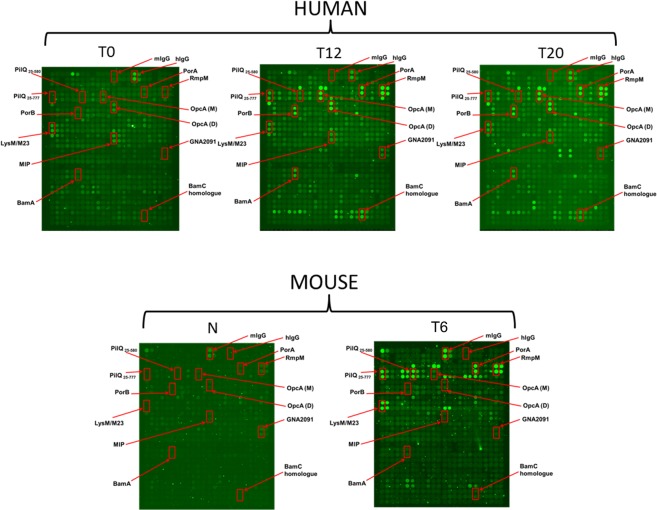
Figure 2.
Exemplar raw data microarrays of human or mouse IgG seroreactivity. The microarrays were hybridized with human or mouse sera and developed for total IgG. T0 or naïve (N) represents pre-vaccination serum, T12 and T20 represent post-vaccination collection the 12 and 20 week time points respectively from the human high dose vaccinees while T6 represents terminal bleed from vaccinated mice after 2 doses. Spots representing highly immunogenic proteins in human or mouse sera are blocked in red. Duplicate spots are shown; the third replicate spot is not in close proximity to the first two spots.
The serum IgG reactivity for both human high dose and mouse OMV vaccinations to individual purified protein antigens are summarised as a heat map in Fig. 3. IgG responses were highly variable between individuals, with some human vaccinees showing strong reaction against specific antigens at T0, as well as T12 and T20. Similar results were obtained for sera from the human low dose group, but were generally subject to more variation and are omitted here. Only a minority of antigens, at the top of the heat map, appeared to consistently stimulate a response at T12 and T20, relative to T0, in most human vaccine recipients. Understandably, the responses in mice were more consistent, with fewer instances of individual animals reacting against a particular antigen. The LysM/M23 domain protein maintained a consistently high reactivity before and after vaccination which could originate from non-specific cross-reactivity.
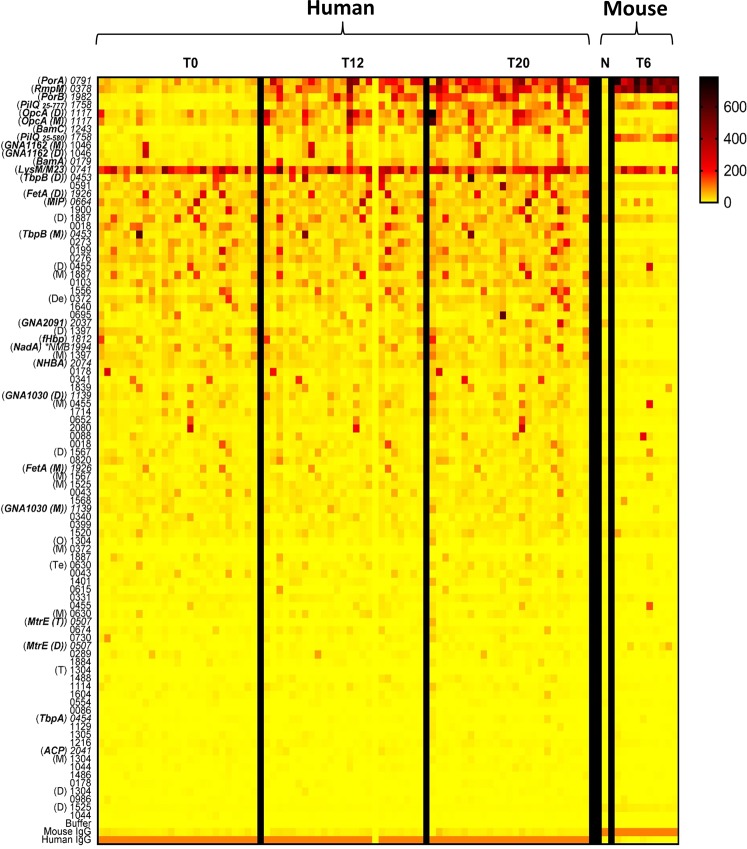
Figure 3.
IgG seroreactivity of immuno-dominant OMPs at different vaccination time points. Reactivity of immunogenic proteins to pre- (T0 or N) and post-vaccination (T12 or T20) sera from 25 human vaccinees and 10 mice (T6) are quantified and represented as a heat map. The colour blocks represent the fluorescence signal intensity for reactivity against total IgG antibodies in serum. Antigens are ranked according to magnitude of difference between human T20 and T0. PilQ25–777 represents the full length protein while PilQ25–580 is missing the C-domain. Proteins are represented as the last 4 digits of their gene numbers (NMBH4476_), letters represent the oligomeric state (M, monomer; D, dimer; T, trimer; Te, tetramer; O, octamer; De, decamer). *NMB 1994 (NadA) is not expressed in strain H44/76 and was obtained from MC58 strain. More details on the individual proteins are given in Supplementary Table S2.
The major IgG reactive antigens for human and mouse antisera are summarised in Table 2. We identified seven different proteins for human and four for mouse which showed increases (p < 0.05) in IgG reactivity after vaccination. All identified highly sero-reactive OMPs retained folded characteristics, as judged by the Thermofluor assay (Supplementary Fig. S2). Of the seven antigens reactive against human antisera, four are iOMPs; of the remaining three, two are lipoproteins (GNA1162 and BamC) and the remaining antigen has a role in stabilising PorA/PorB trimers (RmpM41). Fewer antigens were identified from the mouse antisera, possibly because there were fewer individual serum samples and/or the mice are from an inbred strain; LysM/M23 is listed in Table 2 because it met the criteria for inclusion but, as noted above, it consistently showed a high background. Several antigens appear more than once in the list, either as a consequence of being in a different engineered form (PilQ) or oligomeric state (eg OpcA). Despite the high abundance of the PorB porin in the OMV preparation, it did not appear to elicit high IgG levels in mice, perhaps arising from different immunogenic responses in mice and humans. Although we did record IgG reactivity against FetA in some human antisera, responses were generally weak, even though the parent strain for the OMV preparation was engineered to over-express the iron transporter30.
Table 2.
Major IgG reactive antigens to human and mouse antisera following administration of MenPF-1 OMV vaccinea.
| NMBH4476b | Folded | iOMP? | Relative abundance in OMVc | IgG reactivityd | p-valuee | |
|---|---|---|---|---|---|---|
| Human | ||||||
| PorA | 0791 | YES | YES | 12,840 | 166 ± 27 | 5.93 × 10−7 |
| RmpM | 0378 | YES | NO | 1,970 | 149 ± 21 | 3.01 × 10−8 |
| PorB | 1982 | YES | YES | 13,870 | 114 ± 21 | 2.00 × 10−6 |
| PilQ25–777 | 1758 | YES | YES | 850 | 68 ± 9 | 2.73 × 10−9 |
| OpcA (Df) | 1117 | YES | YES | 1,230 | 87 ± 26 | 1.42 × 10−3 |
| OpcA (Mf) | 1117 | YES | YES | 1,230 | 68 ± 20 | 1.94 × 10−3 |
| BamC | 1243 | YES | NO | 340 | 53 ± 10 | 7.00 × 10−6 |
| PilQ25–580 | 1758 | YES | YES | 850 | 29 ± 5 | 7.00 × 10−3 |
| GNA1162 (M) | 1046 | YES | NO | 180 | 14.8 ± 4.5 | 1.6 × 10−2 |
| GNA1162 (D) | 1046 | YES | NO | 180 | 14.1 ± 3.8 | 4.82 × 10−3 |
| Mouse | ||||||
| PorA | 0791 | YES | YES | 12,840 | 509 ± 46 | 2.00 × 10−6 |
| RmpM | 0378 | YES | NO | 1,970 | 434 ± 17 | 2.75 × 10−8 |
| LysM/M23 | 0741 | YES | NO | NDg | 187 ± 33 | 3.54 × 10−4 |
| PilQ25–580 | 1758 | YES | YES | 850 | 106 ± 16 | 1.92 × 10−4 |
| PilQ25–777 | 1758 | YES | YES | 850 | 114 ± 17 | 1.53 × 10−4 |
aMajor reactive antigens are defined as p < 0.05.
bProteins are represented as the last 4 digits of their NCBI protein accession number or gene numbers (NMBH4476_).
cValue represents the relative protein abundance in OMV as estimated by mass spectrometry.
dDifference in total IgG sero-reactivity between human pre-vaccination (T0) and post-3-vaccination (T20) sera or mouse naïve (N) and post-2-vaccination (T6) sera. The reactivity is given as arbitrary fluorescence measurement ± standard error.
eIgG reactivities at 0, 12 and 20 weeks were analysed for differences using one-way repeated measures ANOVA with Greenhouse-Greisser correction. For the mouse sera, p-values were determined by two-tailed T-test.
fM, monomer; D, dimer or multimer.
gNot detected.
As the strongest mean magnitude responses were observed at T20, we represented the enhanced IgG responses to individual antigens by calculating the increased relative response from T0 to T20. Seventy antigens showed an enhanced IgG reactivity (value ≥ 3) in more than one human vaccinee. Table 3 shows a summary for the seven major sero-reactive antigens identified in Table 2. Several of the highly responding antigens have been reported previously as capable of eliciting serum bactericidal activity and most are subject to some degree of phase or antigenic variation. More than 80% of recipients showed at least a 3-fold increase in IgG against PorA, PorB and the full length PilQ25–777 secretin. We identified NMBH4476_1243 as a homolog of BamC, which forms part of the outer membrane protein BAM assembly complex42,43: it showed an increase in IgG levels by a factor of at least 3 in 14 out of 25 recipients (56%). Other antigens induced a lower frequency of positive responses, specifically RmpM, the iOMP adhesin OpcA and a lipoprotein (GNA1162).
Table 3.
Summary of individual vaccinee responses to antigens with high IgG reactivities.
| Protein name | Gene namea | Functionb | Individual vaccinee response to MenPF-1 OMV vaccinec | SBA?e | Variabilityf | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | P | A | ||||
| PorA | 0791 | Transport | <3 | 8 | 6 | 5 | 11 | 5 | 4 | 5 | 7 | 10 | 4 | 6 | <3 | 27 | 10 | 5 | 6 | 7 | <3 | 6 | 14 | 8 | 4 | 5 | 4 | YES76 | YES77 | YES78 |
| RmpM | 0378 | OM stability | 4 | 7 | 5 | <3 | 3 | 9 | <3 | 8 | 13 | 16 | 5 | 4 | 3 | 19 | 15 | 5 | <3 | 4 | 6 | 7 | 7 | 8 | 15 | <3 | 3 | YES56 | NO79 | NO80 |
| PorB | 1982 | Transport | 5 | 13 | 29 | 18 | 16 | 12 | — | — | 6 | — | 19 | 47 | 107 | 95 | — | 42 | 38 | 195 | 9 | — | 76 | 8 | 30 | 10 | <3 | YES81 | NO82 | YES83 |
| PilQ25–777 | 1758 | Type IV pilus formation | 0 | 27 | 8 | 7 | 13 | 14 | 4 | 15 | 14 | 93 | 5 | 9 | 18 | — | — | 7 | 29 | 21 | 12 | <3 | 5 | 3 | 14 | 13 | 3 | YES63 | NO79 | NO84 |
| OpcA (D) | 1117 | Adhesion | 4 | 5 | <3 | 5 | <3 | 3 | 3 | <3 | 3 | <3 | <3 | 4 | <3 | 7 | 3 | 9 | <3 | 5 | <3 | <3 | <3 | 3 | <3 | <3 | <3 | YES85 | YES86 | NO87 |
| OpcA (M) | 1117 | Adhesion | 6 | 6 | <3 | 3 | <3 | 5 | <3 | <3 | 4 | <3 | 4 | 3 | <3 | 9 | 4 | 6 | <3 | 3 | <3 | <3 | 4 | 3 | <3 | <3 | 3 | YES85 | YES86 | NO87 |
| BamC | 1243 | Protein assembly | — | — | 18 | <3 | 24 | — | — | 41 | 13 | 95 | <3 | <3 | 13 | 91 | 5 | — | — | 109 | 21 | 32 | — | — | 112 | 13 | 4 | YES43 | NO43 | NO43 |
| PilQ25–580 | 1758 | Type IV pilus formation | 3 | 5 | 4 | 3 | <3 | 3 | 3 | <3 | 11 | 10 | <3 | 4 | 5 | 43 | 3 | 4 | 6 | 5 | 3 | <3 | 4 | 3 | 4 | <3 | <3 | YES63 | NO79 | NO84 |
| GNA1162 (M) | 1046 | Unknown | 3 | 5 | <3 | <3 | <3 | <3 | <3 | <3 | <3 | <3 | <3 | 3 | <3 | 5 | <3 | <3 | <3 | <3 | 3 | <3 | 6 | 3 | 4 | <3 | <3 | — | — | — |
| GNA1162 (D) | 1046 | Unknown | <3 | <3 | <3 | <3 | <3 | 3 | <3 | <3 | <3 | <3 | <3 | 3 | <3 | 5 | <3 | <3 | <3 | <3 | <3 | <3 | 5 | 4 | <3 | <3 | <3 | — | — | — |
aProteins are listed as the last 4 digits of their NCBI protein accession number or gene numbers (NMBH4476_).
bProtein function is detailed based on previous experimental findings or predictions from the Pfam database75.
cValues represent the proportional increase in serum reactivity to antigen i.e. (fluorescence value at T20)/(fluorescence value at T0). Where the T0 value was very low or zero, the cell is left blank.
ePublished Serum Bactericidal Assay to a homolog.
fPhase (P) and antigenic (A) variability of antigens.
gM, monomer; D, dimer.
Analysis of sequence conservation of selected antigens
PorA and PorB, are major meningococcal surface antigens, and are subject to a high degree of sequence variation, principally within the surface-exposed loop regions, probably as a result of immune selection pressure44,45. The degree of sequence variation within the other antigens in Table 1 and how it maps onto three-dimensional structure has been less well studied, however. OpcA is an iOMP with 10 membrane-spanning β-strands which is subject to much less sequence variation and has been advocated previously as a potentially valuable vaccine component13,46,47. We therefore set out to analyse the relationship between sequence and structure for the other antigens identified in Table 2.
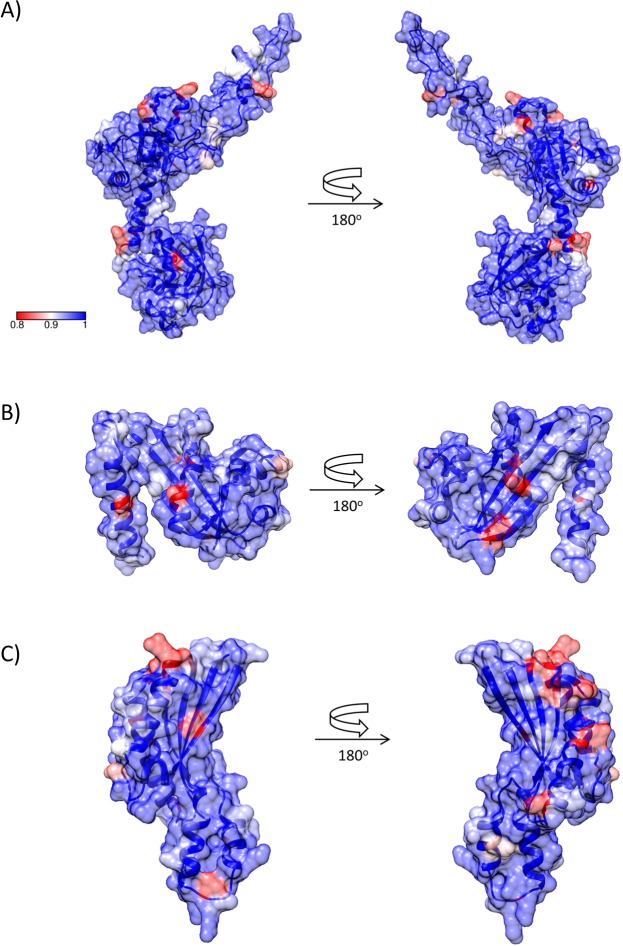
BamC, GNA1162 and RmpM do not contain membrane-spanning β-strands and consist of α/β globular domain structures41,42,48. Using all available allele sequences from the Neisseria PubMLST databank49, sequence variation was mapped onto the crystal structures of GNA116248 and RmpM50, and a molecular model of BamC, derived from the crystal structure of the BamACDE complex from E. coli42. Sequence variation was limited, with relatively few residues showing conservation of 80% or less (Fig. 4). There were no noticeable ‘hotspots’ of variation, with the possible exception of RmpM, which showed a marginally greater distribution at one end of the α/β domain (Fig. 4C).
Figure 4.
Structures and sequence variation of N. meningitidis BamC, GNA1162 and RmpM. (A) BamC. The model for BamC was generated using SWISS-MODEL71, based on PDB accession 5D0Q. (B) GNA1162 (PDB accession 4HRV). (C) RmpM (PDB accession 1R1M). Figures were generated using CONSURF72 and CHIMERA73. Surfaces are coloured by sequence conservation, from 80% or lower (red), through 90% (white) to 100% (blue).
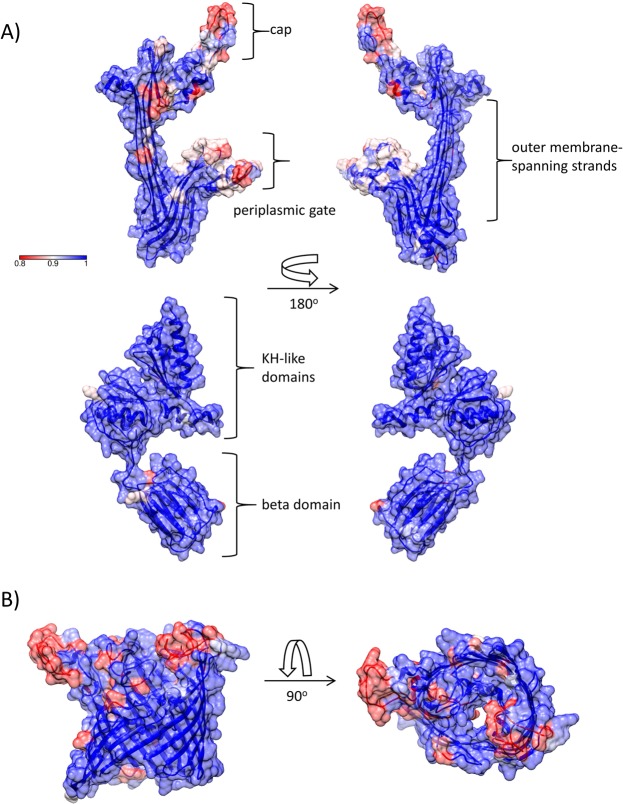
In contrast, the PilQ secretin adopts a complex, multidomain oligomeric assembly which spans the outer membrane and part of the periplasm. Using recent structures derived from related secretins51, a model for the transmembrane portion of PilQ was generated; a previous NMR study generated structural models for the KH-like α/β domains and β domain which constitute the portion within the periplasm52. Sequence variation mapped to two parts of the transmembrane region, specifically the cap and periplasmic gate, which closes off the internal chamber within the oligomer51 (Fig. 5A). Sequence variation within the periplasmic domains was much more limited and not concentrated into any specific region. As a basis for comparison, we conducted a similar analysis on PorA, where antigenic variation has been studied in more detail. Sequence variation is concentrated into the surface-exposed loop regions, particularly loops 1 and 4 (Fig. 5B). This suggests that IgG recognition of PilQ is also concentrated into peptide sequences within the cap and periplasmic gate structures, an observation which could be of value in development of vaccines incorporating PilQ antigens.
Figure 5.
Structures and sequence variation of N. meningitidis PilQ and PorA. (A) PilQ. Upper panel: outer membrane-spanning domain; lower panel: periplasmic domains. The model for the membrane-spanning domain was generated by I-TASSER74 using multiple templates. The periplasmic domain was based on PDB accession 4AV2. (B) PorA. The model for PorA was generated using SWISS-MODEL71, based on PDB accession 3A2S.
Discussion
OMV-based vaccines have been widely used since the 1970s, with reported efficacies above 70%53. A major limitation, however, is that protection against heterologous strains is limited54. This can be attributed, at least in part, to antigenic variation within the major outer membrane protein antigen, PorA44. However, OMVs represent a complex mixture of different antigens, several of which could assist in providing protection. For example, a study of antibody responses to an OMV vaccine based on strain H44/76 showed that the iOMP OpcA also made a contribution to bactericidal activity55. More generally, identification of the additional antigens which are at least able to elicit IgG responses will be valuable in identifying what further protective antigens there are in OMVs. The fact that we identify PorA as the most reactive antigen is to be expected, and provides an encouraging validation of our approach (Table 2). This was not the case with a similar antigen microarray study which used iOMPs in a denatured state29; this emphasises the importance of maintaining conformational epitopes in microarray screens.
Although our microarray contained over 90 proteins, only about 10% gave IgG responses in the human vaccinees which we could assign as significant. That is not to say that other proteins, or indeed non-protein components, do not play a role in providing protection in some vaccine individuals. It does suggest, however, that a panel of judiciously chosen antigens might be able to provide a level of protection similar to an OMV preparation, at least as far as the protein components of OMVs are concerned. Interestingly, we find that four out of the seven responding antigens in humans are iOMPs (Table 2). This observation poses a challenge for the development of antigen microarrays- iOMPs tend to be more difficult to isolate in their native conformational states than their soluble counterparts. Here, we used a generalized refolding protocol which was successful previously11–13, although it is imperfect: we have not been able to develop a refolding protocol which successfully reconstitutes the dodecameric PilQ assembly, for example. PilQ is a member of the secretin family, a group of iOMPs which are challenging to isolate and study51. The fact that our recombinant PilQ sample shows a well-defined peak in the Sypro Orange fluorescence assay suggests that some conformational epitopes are retained, however (Supplementary Fig. S2). This assay is a relatively crude measure of the folded state but provides a guide. Inevitably, protein antigen microarrays will be incomplete, to the extent that they omit proteins which are difficult to express, purify or reconstitute into their native conformations. Nevertheless, the fact that we identified several iOMPs (Table 2) suggests that we have been able to overcome these obstacles, at least to some extent.
The highest IgG responses observed in this study were directed against PorA, PorB and RmpM, which are thought to form a complex in vivo41. PorA and PorB form β-barrel structures, characteristic of bacterial porins, with surface-exposed loop regions44. RmpM, however, consists of a flexible N-terminal region and a C-terminal domain which binds to peptidoglycan41,56. The N-terminal region binds to PorA and PorB on the periplasmic side of the barrel41,57- this model suggests that no part of RmpM is surface-exposed in intact bacteria. This proposition is supported by earlier work which showed that antibodies derived from human OMV vaccinees reacted against segments of the protein which were not exposed in intact bacteria56. An obvious explanation is that portions of RmpM become exposed during OMV manufacture, which can stimulate an IgG response but, if correct, these epitopes are unlikely to be effective in providing protection.
An unanticipated outcome of this study was the identification of two lipoproteins which have received relatively little attention previously as potential meningococcal vaccine components. BamC is part of the BamABCDE (BAM) complex, which promotes insertion and folding of β-barrel iOMPs into the outer membrane58. Some components are dispensable for function in some organisms- BamE is not necessary for viability in N. gonorrhoeae, for example59. Delgado et al. identified NMBH4476_1243 (NCBI accession number) as a homolog of BamC from E. coli43. They showed that mice immunized with the BamC lipoprotein reconstituted into liposomes produced bactericidal antibodies which conferred protection in an infant rat model43. However, recent structural studies on the E. coli BAM complex suggest that BamC is likely located in the periplasm42. We also found sero-reactivity against BamA, although whether it appeared as meeting the significance criterion for inclusion in Table 2 depended on the statistical test employed. BamA is the key iOMP component of the BAM complex and the crystal structure of BamA from N. gonorrhoeae shows several external loop regions which could interact with antibody60. Further, a reverse vaccinology strategy applied to search for potential gonococcal vaccine candidates from naturally released gonococcal OMVs identified a BamA homolog which induced bactericidal antibodies61. BAM complex proteins are therefore worthy of further consideration as potential meningococcal vaccine components.
GNA1162 was originally identified as a potential meningococcal vaccine component using a reverse vaccinology approach16; FACS analysis suggested that it was surface-exposed, although serum bactericidal activity was weak (1/4). The crystal structure of GNA1162 has been determined, but there are few details available on its function: structural similarities were identified with TolB and LptE, suggestive of a role in transport or translocation48. Using the sequences from the Neisseria PubMLST databank49, we identified 426 alleles but, overall, a high degree of sequence conservation, with only a few residues exhibiting less than 80% sequence conservation (Fig. 4B). Given the strong IgG response to GNA1162 (Table 2), it may be worth revisiting the use of this lipoprotein as a useful vaccine component.
Antigens derived from the PilQ secretin also featured in the list of proteins reacting strongly against IgG from humans and mice (Table 2). PilQ forms a cage-like dodecameric assembly which spans the outer membrane and part of the periplasm52,62. It is a member of the secretin family of outer membrane proteins, and forms a large pore in the membrane for the passage of the assembled type IV pilus. Two PilQ constructs were used: one, PilQ25–777, constitutes the mature protein, whereas PilQ25–580 covers just the predicted periplasmic domains and omits the C-terminal, membrane-spanning region. Our findings are consistent with previous research which demonstrated that a 406–777 residue fragment of PilQ is both antigenic in mice and the antisera generated were bactericidal63.
Recent structural work on related secretins enabled us to construct models for the membrane-spanning and periplasmic PilQ domains. Modelling of the C-terminal region, which is the most conserved part of the multimer, enables us to identify which regions might potentially be surface-exposed (Fig. 5A). Mapping of the sequences from 992 alleles identified two ‘hotspots’ of variation within the cap and periplasmic gate regions; much less variation was seen within the periplasmic domains. One explanation for the higher sequence variation observed within these regions is that they are subject to immune selection pressure, in a similar fashion to PorA (Fig. 5B). Such a conclusion should be treated with caution, however: further evidence is required, such as the mapping of epitopes recognised by neutralising antibodies to these regions. Both the cap and periplasmic gate structures would be displaced on passage of an assembled pilus fibre (6–7 nm in diameter)64, and it is possible that this could accentuate external exposure of these parts of the secretin.
Two vaccines, 4C-MenB65 and rLP208666, have been licensed for use against capsular group B meningococcal disease. 4C-MenB is a four component vaccine which contains two fusion recombinant proteins, NHBA-GNA1030 and fHbp-GNA2091, in combination with the adhesin NadA and a detergent-extracted OMV preparation derived from strain NZ98/254 (New Zealand). rLP2086 comprises two recombinant lipidated variants of fHbp (factor H binding protein), which has been a major focus of meningococcal vaccine antigen development67. Although these antigens were included in our protein microarray library, none showed an increased response after MenPF-1 vaccination, probably because they are present at low levels in the OMV preparation.
In summary, this work has shown that minor OMV antigens can elicit significant levels of IgG response and are therefore worthy of consideration as components in future vaccines.
Methods
MenPF-1 OMV vaccine
MenPF-1 vaccine is an OMV-based vaccine produced at Norwegian Institute of Public Health, (NIPH) from a genetically modified capsular Neisseria meningitidis capsular group B (NmB) strain H44/76 characterised as B:15: P1.7,16: F3-3:ST-32. The strain was genetically modified by replacing the wild-type fetA promoter, whose expression is dependent on iron concentration in the growth medium, with a porA promoter sequence to produce a modified meningococcal strain H44/76 which constitutively expresses FetA and retains wild-type expression of PorA8,31. The MenPF-1 vaccine consists of detergent-derived OMVs formulated with aluminium hydroxide, sucrose and water to contain 25 μg OMV proteins per 0.5 ml vial30.
Serum samples from pre-clinical and clinical trials with MenPF-1 OMV vaccine
For this study, 10 C57BL/6 mice (female, 18–22 g) were immunised subcutaneously with 2 doses of 2.5 μg MenPF-1 vaccine. Each dose was 3 weeks apart and the terminal bleeds, collected 3 weeks after the second dose, were used for microarray analysis. This dosage and schedule had previously been shown to induce the production of PorA- and FetA-specific IgG responses8. All procedures were performed in accordance with the terms of the UK Home Office Animals Act Project License. Procedures were approved by the University of Oxford Animal Care and Ethical Review Committee.
Pre-clinical and Phase 1 clinical immunogenicity studies on MenPF-1 were carried out in mice and adult humans as described8,30. 52 volunteers (male and female, 18–50 yrs) were split equally into 2 dose groups to receive 25 μg of MenPF-1 vaccine in one group and 50 μg in the other. Three doses of vaccine were administered by intra-muscular injection 8 weeks apart and serum samples were collected 4 weeks after each dose30. Samples used for this study were pre-vaccination (T0), 12 (T12) and 20 (T20) weeks post-vaccination respectively. Ethical approval for the study was granted by NRES Oxford A (12/SC/0023) and the trial was registered with clinicaltrials.gov and EudraCT (NCT01640652 and 2012-001046-17 respectively). It was conducted in accordance with the principles of the Declaration of Helsinki (2008) and the International Conference on Harmonization (ICH) Good Clinical Practices standards.
Protein characterization using multidimensional LC-MS/MS
The proteomics experiments were performed using a non-clinical GMP batch of MenPF vaccine (lot number FMOX1102) formulated with 3% sucrose to a final protein concentration of 0.05 mg/mL and Al(OH)3 concentration 3.3 mg/mL (~aluminium content of 1.15 mg/mL)8. The solution containing 600 µL of vaccine sample; 400 µL of 1 M tetraethylammonium bromide was added to a 1 mg RapiGest bottle (Waters, UK) and incubated at 100 °C for 5 min. When it reached ambient temperature (22 °C), the solution was transferred to a 20 µg trypsin bottle (Promega, UK) and placed at 37 °C overnight. The digestion was terminated and the RapiGest was disintegrated by addition of 5 µL trifluoroacetic acid and incubated at 22 °C for 30 min. The digest (~1 mL) was dried down under vaccum (using a Speedvac) to ~70 µL. Multidimensional LC-MS/MS was carried out according the method described by Chan et al.68. The 12 fractions collected by high pH RP-HPLC separation were each subjected to 240-min LC-MS/MS peptide sequencing using a MS system (Thermo Scientific) equipped with a nano-electrospray ion source and two mass detectors, linear trap (LTQ) and Orbitrap, coupled with an Ultimate 3000 nano-LC system. Data analysis including mass spectra processing and database searching was carried out using the Thermo Proteome Discoverer 1.4, with built-in Sequest (Thermo Scientific). Initial mass tolerances for protein identification by MS were set to 10 ppm. Up to two missed tryptic cleavages were considered and methionine oxidation was set as dynamic modification. Peptide sequences by MS/MS were only included when correlation scores were greater than 1.5, 2 or 2.2 for charge states 1, 2 and 3, respectively. An unambiguous identification was considered when at least two unique peptides matched to the protein. The protein FASTA databases were downloaded from www.uniprot.org, release 2014_07 including the complete entries from MenB H44/76 strain.
Cloning, expression and purification of meningococcal OMPs
The open reading frames (ORFs) of selected OMPs of NmB strain were cloned into pOPINF and pOPINE plasmid vectors using a high-throughput In-Fusion™ cloning method developed by the Oxford Protein Production Facility (OPPF). The pOPINF plasmid encodes N-terminal hexa-histidine (His) tagged proteins while the pOPINE plasmid encodes C- terminal His tagged proteins69. The ORFs of gene encoding proteins were engineered to improve their solubility and expression. The gene sequences encoding mature NHBA, and NadA proteins, were synthesized in vitro (GeneArt, Invitrogen) and optimised for expression in E. coli. Synthesized genes were then cloned into pET22b(+) plasmid (Novagen) vector in between the NdeI and XhoI restriction sites to generate C-terminal hexa-histidine tagged proteins. All recombinant plasmids generated were sequenced (GATC Biotech) and confirmed with reference to the nucleotide database at the National Centre for Biotechnology Information70.
Recombinant plasmids were transformed into XL-10 Gold ultra-competent E. coli cells (Stratagene) for plasmid amplification and subsequently into BL21 (DE3) competent E. coli cells (New England Biolabs) for protein expression. Cultured cells were grown in terrific broth and induced at A600 (absorbance at 600 nm) of 0.8 by adding isopropyl-β-1-D-thiogalactopyranoside (IPTG; Sigma-Aldrich) to a final concentration of 0.5 mM for overnight expression at 16 °C.
1 mL aliquots of pre- and post-induction cell cultures were collected to assess the expression of target protein and its cellular location. Cells were pelleted by centrifugation at 16,000 × g for 5 min and subsequently, re-suspended in 500 μL of lysis buffer (50 mM HEPES-NaOH pH 7.5; 200 mM NaCl; 5% glycerol; 25 mM EDTA). The expression of target protein in total cell extract and soluble supernatant fractions from pre- and post-IPTG induction samples was analysed by SDS-PAGE. Proteins present in both total extract and supernatant fractions were regarded as soluble proteins and purified from the supernatant fraction. Proteins that were present only in the total extract samples were recovered from inclusion bodies (IBs). They were solubilised using urea and subsequently refolded using a protocol described previously11.
All solubilized target proteins were subject to sequential chromatographic steps for purification as described previously11,34. In brief, target proteins were purified with nickel iminodiacetic acid resin (Generon) using 50 mM HEPES pH7.5, 200 mM NaCl, 500 mM imidazole and 0.05% Glycerol for soluble proteins and 20 mM Tris-HCl pH 7.9; 0.5 M NaCl; 0.1% (v/v) LDAO 500 mM imidazole for refolded proteins. All eluents were analysed using 12% w/v SDS-PAGE (Invitrogen); fractions with target protein were pooled for further purification and concentrated using centrifugal concentrators (Sartorius) at 6,000 × g. To determine their oligomeric state, purified proteins were passed through a size exclusion chromatography column (Superdex S-75 or S-200 Hi-Load 16/60 column; GE Healthcare) on an AKTA-FPLC system (GE Healthcare). Column buffers used were 25 mM HEPES pH 7.5, 150 mM NaCl for soluble proteins and 20 mM Tris-HCl pH 7.9; 0.1 M NaCl; 0.1% (v/v) LDAO for refolded proteins. Eluted protein samples were analysed for purity by SDS-PAGE, and concentrated with Vivaspin® centrifugal concentrators (Sartorius). All purified OMPs were concentrated to 5–10 mg/ml, protein concentration estimated from absorbance at 280 nm and stored at −80 °C prior to microarray printing.
Protein folding fluorescence temperature ramp assay
20 µL of each purified OMP was prepared at 25 µg/ml and 1x SYPRO® orange dye (Sigma) in appropriate buffer (25 mM HEPES-NaOH pH 7.5 and 150 mM NaCl for soluble proteins and 20 mM Tris-HCl pH 7.9, 0.5 M NaCl and 0.1% LDAO for refolded proteins). Samples were transferred to MicroAmp® Fast Optical 96 well reaction plates (Applied Biosystems) and sealed. The assay was conducted in a StepOne® Real Time PCR System (Life Technologies). Samples were heated from 25 to 95 °C at a rate of 1 °C/min. Fluorescence intensities were measured with excitation and emission wavelengths of 575/602 nm respectively. Samples were recorded in triplicate. Control wells consisting of buffer and dye only was used to normalise the fluorescence intensities for each protein. A reference ovalbumin protein sample was used as a positive control.
Antigen microarray fabrication
The meningococcal protein microarray slides were custom-made by Arrayjet Limited, UK. Recombinant meningococcal protein samples were printed from 384 well plates containing 10 µL of each OMPs diluted to 1 µg/µL with Arrayjet printing buffer® (Arrayjet). Control spots consisted of a) monoclonal mouse and human IgG were prepared at a concentration of 0.3 µg/µL b) purified E. coli soluble lysate, E. coli IB extracts c) purified EBNA-1 viral protein at 0.1 µg/µL d) Arrayjet printing buffer® control spots. Two drops of 100 pL were arrayed per spot onto ONCYTE® SuperNOVA nitrocellulose coated glass slides (Grace Bio-Labs). The spot distance was set as 190 μm in the vertical and horizontal directions. Each microarray slide consisted of 16 identical blocks with each miniarray containing 91 OMP preparations and 5 control samples in triplicate. Printing was carried out at 18 °C and 50% relative humidity; arrayed protein slides were air-dried overnight at 4 °C and stored at −20 °C until used.
Validation of protein spots on microarray slide
Protein spots were assessed for spot quality, circularity and consistency by using mouse monoclonal anti-tetra-histidine IgG antibody (Qiagen) to detect hexa-histidine tagged OMPs. Preliminary experiments with mouse and human sera showed that 1:125 dilutions of serum produced the best signal without significant background. Anti-mouse IgG Alexa Fluor 555 secondary antibody (Molecular Probes) was used to detect bound antibodies. Signal intensities were quantified and normalised against background using the GenePix® Pro 7 Microarray Image Analysis software (Molecular Devices).
Microarray Immunogenicity probing
The Proplate® Multi-Array Slide System (Grace BioLabs) was used to create 16 leak-proof minipads on the meningococcal protein microarray slides; one minipad was used per serum sample. Minipads were blocked with 300 µL of 3% bovine serum albumin (Thermo Fisher) in Phosphate Buffered Saline (PBS) for 1 hr at room temperature. Addition of E. coli soluble lysate and inclusion body extracts to the serum sample were used to reduce non-specific recognition of E. coli proteins. 300 µl of 1:125 diluted serum in PBS supplemented with 10% w/v E. coli lysate (5 mg/mL) and IB extracts (5 mg/mL) were added per well and slides were incubated overnight at 4 °C under gentle agitation. After washing twice with 250 µL PBS-T (0.05% Tween-20) and once in PBS, for 10 min each time, slides were incubated in the dark with 300 µL of 1:1000 diluted anti-human or anti-mouse IgG Alexa Flour 555 secondary antibody (Molecular Probes), diluted in PBS, for 2 hr at 25 °C under gentle agitation. Wash steps were repeated as described above in the dark, then slides were rinsed in de-ionized water and dried by centrifugation at 200 × g for 2 min. Slides were scanned in a Gene Pix Pro 4200A microarray scanner (Molecular Devices) with the photo multiplier tube set to 100% for 532 nm wavelength and image analysis and data quantification was carried out using GenePix Pro 7 Microarray Image Analysis software (Molecular Devices).
Data and statistical analysis
Microarray spot intensities were quantified using GenePix Pro 7 Microarray Image Analysis software (Molecular Devices) which utilises automatic background subtraction for each spot. The spot intensities for each protein were recorded in triplicate, arithmetic means determined and spot intensities for buffer-only-controls subtracted. To determine the increase in IgG reactivity for a particular antigen as shown in Table 2, the corrected value obtained from serum collected before immunization was subtracted from the same value obtained from serum after immunization (eg T20-T0 for human sera). A two-tailed T-test was used to calculate p-values and test for significance between doses per protein.
Supplementary information
Acknowledgements
A.M.A. was the recipient of TETFund (Nigeria), while C.M.C. was a recipient of Taiwan Bio-Development Foundation and The MOE (Taiwan) Technologies Incubation Scholarship. The MenPF-1 Phase I trial was funded by a Wellcome Trust Strategic Translation Award (Award number: 082102/Z/07/A). RJO LEB and JEN acknowledge support from the UK Medical Research Council (MR/K018779/1). We thank Angela Thistlethwaite for laboratory assistance and Saloni Sonawala (Arrayjet Ltd) for her help with the microarray printing. CR and AJP are Jenner investigators.
Author Contributions
A.M.A. and C.M.C. performed research; J.P.D. and A.J.P. designed research; L.M., C.D., H.C. and C.S.R. provided serum samples; L.E.B., J.E.N. and R.J.O. assisted with protein expression; J.X.W. performed proteomics on OMV; A.M.A., C.M.C. and J.P.D. analysed the data and wrote the paper. All authors revised the manuscript.
Competing Interests
There was no involvement of any commercial organization in this study. J.P.D. is in receipt of funds from GlaxoSmithKline for vaccine research. He does not receive any personal payments from them or honoraria. A.J.P. has previously conducted clinical trials on behalf of Oxford University funded by manufacturers of meningococcal vaccines including Novartis Vaccines, GlaxoSmithKline, Pfizer and Sanofi Pasteur. He does not receive any personal payments from them nor travel reimbursement or honoraria. His department has received unrestricted educational grants from vaccine manufacturers for organisation of courses and symposia. A.J.P. has previously been named on patents in the field of group B meningococcal vaccines. All the other authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Amaka M. Awanye and Chun-Mien Chang contributed equally.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-43139-0.
References
- 1.Tzeng YL, Stephens DS. Epidemiology and pathogenesis of Neisseria meningitidis. Microb. Infect. 2000;2:687–700. doi: 10.1016/S1286-4579(00)00356-7. [DOI] [PubMed] [Google Scholar]
- 2.Andrews SM, Pollard AJ. A vaccine against serogroup B Neisseria meningitidis: Dealing with uncertainty. Lancet Infect. Dis. 2014;14:426–434. doi: 10.1016/S1473-3099(13)70341-4. [DOI] [PubMed] [Google Scholar]
- 3.Finne J, Leinonen M, Makela PH. Antigenic similarities between brain components and bacteria causing meningitis. Implications for vaccine development and pathogenesis. Lancet. 1983;2:355–357. doi: 10.1016/s0140-6736(83)90340-9. [DOI] [PubMed] [Google Scholar]
- 4.Swartley JS, et al. Capsule switching of Neisseria meningitidis. Proc. Natl. Acad. Sci. USA. 1997;94:271–276. doi: 10.1073/pnas.94.1.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boslego J, et al. Efficacy, safety, and immunogenicity of a meningococcal group B (15:P1.3) outer membrane protein vaccine in Iquique, Chile. Chilean National Committee for Meningococcal Disease. Vaccine. 1995;13:821–829. doi: 10.1016/0264-410X(94)00037-N. [DOI] [PubMed] [Google Scholar]
- 6.Wedege E, Hoiby EA, Rosenqvist E, Bjune G. Immune responses against major outer membrane antigens of Neisseria meningitidis in vaccinees and controls who contracted meningococcal disease during the Norwegian serogroup B protection trial. Infect. Immun. 1998;66:3223–3231. doi: 10.1128/iai.66.7.3223-3231.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Milagres LG, Gorla MC, Rebelo MC, Barroso DE. Bactericidal antibody response to Neisseria meningitidis serogroup B in patients with bacterial meningitis: effect of immunization with an outer membrane protein vaccine. FEMS Immunol. Med. Microbiol. 2000;28:319–327. doi: 10.1111/j.1574-695X.2000.tb01493.x. [DOI] [PubMed] [Google Scholar]
- 8.Norheim G, et al. An OMV Vaccine Derived from a Capsular Group B Meningococcus with Constitutive FetA Expression: Preclinical Evaluation of Immunogenicity and Toxicity. PLoS One. 2015;10:e0134353. doi: 10.1371/pone.0134353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lappann M, Otto A, Becher D, Vogel U. Comparative proteome analysis of spontaneous outer membrane vesicles and purified outer membranes of Neisseria meningitidis. J. Bacteriol. 2013;195:4425–4435. doi: 10.1128/JB.00625-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrari Germano, Garaguso Ignazio, Adu-Bobie Jeannette, Doro Francesco, Taddei Anna Rita, Biolchi Alessia, Brunelli Brunella, Giuliani Marzia Monica, Pizza Mariagrazia, Norais Nathalie, Grandi Guido. Outer membrane vesicles from group BNeisseria meningitidis Δgna33 mutant: Proteomic and immunological comparison with detergent-derived outer membrane vesicles. PROTEOMICS. 2006;6(6):1856–1866. doi: 10.1002/pmic.200500164. [DOI] [PubMed] [Google Scholar]
- 11.Saleem M, Moore J, Derrick JP. Expression, purification, and crystallization of neisserial outer membrane proteins. Methods Mol. Biol. 2012;799:91–106. doi: 10.1007/978-1-61779-346-2_6. [DOI] [PubMed] [Google Scholar]
- 12.Saleem M, et al. Refolding, purification and crystallization of the FrpB outer membrane iron transporter from Neisseria meningitidis. Acta Crystallogr. F. 2012;68:231–235. doi: 10.1107/S1744309111056028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prince SM, Achtman M, Derrick JP. Crystal structure of the OpcA integral membrane adhesin from Neisseria meningitidis. Proc. Natl. Acad. Sci. USA. 2002;99:3417–3421. doi: 10.1073/pnas.062630899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanabe M, Nimigean CM, Iverson TM. Structural basis for solute transport, nucleotide regulation, and immunological recognition of Neisseria meningitidis PorB. Proc. Natl. Acad. Sci. USA. 2010;107:6811–6816. doi: 10.1073/pnas.0912115107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Serruto D, Bottomley MJ, Ram S, Giuliani MM, Rappuoli R. The new multicomponent vaccine against meningococcal serogroup B, 4CMenB: immunological, functional and structural characterization of the antigens. Vaccine. 2012;30(Suppl 2):B87–97. doi: 10.1016/j.vaccine.2012.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pizza M, et al. Identification of vaccine candidates against serogroup B meningococcus by whole-genome sequencing. Science. 2000;287:1816–1820. doi: 10.1126/science.287.5459.1816. [DOI] [PubMed] [Google Scholar]
- 17.Poolman J, Berthet FX. Alternative vaccine strategies to prevent serogroup B meningococcal diseases. Vaccine. 2001;20:S24–S26. doi: 10.1016/S0264-410X(01)00283-3. [DOI] [PubMed] [Google Scholar]
- 18.Kelly DF, Rappuoli R. Reverse vaccinology and vaccines for serogroup B Neisseria meningitidis. Adv. Exp. Med. Biol. 2005;568:217–223. doi: 10.1007/0-387-25342-4_15. [DOI] [PubMed] [Google Scholar]
- 19.Giuliani MM, et al. A universal vaccine for serogroup B meningococcus. Proc. Natl. Acad. Sci. USA. 2006;103:10834–10839. doi: 10.1073/pnas.0603940103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Findlow J, et al. Multicenter, open-label, randomized phase II controlled trial of an investigational recombinant Meningococcal serogroup B vaccine with and without outer membrane vesicles, administered in infancy. Clin. Infect. Dis. 2010;51:1127–1137. doi: 10.1086/656741. [DOI] [PubMed] [Google Scholar]
- 21.Gossger N, et al. Immunogenicity and Tolerability of Recombinant Serogroup B Meningococcal Vaccine Administered With or Without Routine Infant Vaccinations According to Different Immunization Schedules A Randomized Controlled Trial. J. Am. Med. Assoc. 2012;307:573–582. doi: 10.1001/jama.2012.85. [DOI] [PubMed] [Google Scholar]
- 22.Santolaya MaE, et al. Immunogenicity and tolerability of a multicomponent meningococcal serogroup B (4CMenB) vaccine in healthy adolescents in Chile: A phase 2b/3 randomised, observer-blind, placebo-controlled study. The Lancet. 2012;379:617–624. doi: 10.1016/S0140-6736(11)61713-3. [DOI] [PubMed] [Google Scholar]
- 23.Toneatto D, et al. Early clinical experience with a candidate meningococcal B recombinant vaccine (rMenB) in healthy adults. Hum Vaccines. 2011;7:781–791. doi: 10.4161/hv.7.7.15997. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez LC. Protein microarrays, biosensors, and cell-based methods for secretome-wide extracellular protein-protein interaction mapping. Methods. 2012;57:448–458. doi: 10.1016/j.ymeth.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Davies DH, et al. Profiling the humoral immune response to infection by using proteome microarrays: high-throughput vaccine and diagnostic antigen discovery. Proc. Natl. Acad. Sci. USA. 2005;102:547–552. doi: 10.1073/pnas.0408782102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liang, L. et al. Immune profiling with a Salmonella Typhi antigen microarray identifies new diagnostic biomarkers of human typhoid. Scientific Reports3, 10.1038/srep01043 (2013). [DOI] [PMC free article] [PubMed]
- 27.Felgner PL, et al. A Burkholderia pseudomallei protein microarray reveals serodiagnostic and cross-reactive antigens. Proc. Natl. Acad. Sci. USA. 2009;106:13499–13504. doi: 10.1073/pnas.0812080106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vigil A, et al. Profiling the humoral immune response of acute and chronic Q fever by protein microarray. Mol. Cell. Proteomics. 2011;10(M110):006304. doi: 10.1074/mcp.M110.006304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steller S, et al. Bacterial protein microarrays for identification of new potential diagnostic markers for Neisseria meningitidis infections. Proteomics. 2005;5:2048–2055. doi: 10.1002/pmic.200401097. [DOI] [PubMed] [Google Scholar]
- 30.Marsay L, et al. A novel meningococcal outer membrane vesicle vaccine with constitutive expression of FetA: A phase I clinical trial. J. Infect. 2015;71:326–337. doi: 10.1016/j.jinf.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanders H, et al. FetA Antibodies Induced by an Outer Membrane Vesicle Vaccine Derived from a Serogroup B Meningococcal Isolate with Constitutive FetA Expression. PLoS One. 2015;10:e0140345. doi: 10.1371/pone.0140345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uli L, et al. Outer membrane vesicles of the VA-MENGOC-BC (R) vaccine against serogroup B of Neisseria meningitidis: Analysis of protein components by two-dimensional gel electrophoresis and mass spectrometry. Proteomics. 2006;6:3389–3399. doi: 10.1002/pmic.200500502. [DOI] [PubMed] [Google Scholar]
- 33.Vipond C, et al. Proteomic analysis of a meningococcal outer membrane vesicle vaccine prepared from the group B strain NZ98/254. Proteomics. 2006;6:3400–3413. doi: 10.1002/pmic.200500821. [DOI] [PubMed] [Google Scholar]
- 34.Humbert MV, Awanye AM, Lian L-Y, Derrick JP, Christodoulides M. Structure of the Neisseria Adhesin Complex Protein (ACP) and its role as a novel lysozyme inhibitor. PLoS Path. 2017;13:e1006448. doi: 10.1371/ppat.1006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huynh K, Partch CL. Analysis of Protein Stability and Ligand Interactions by Thermal Shift Assay. Current Protocols in Protein Science. 2015;79:28.29.21–28.29.14. doi: 10.1002/0471140864.ps2809s79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramachandran N, et al. Tracking humoral responses using self assembling protein microarrays. Proteom Clin Appl. 2008;2:1518–1527. doi: 10.1002/prca.200800034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J, et al. A versatile protein microarray platform enabling antibody profiling against denatured proteins. Proteom Clin Appl. 2013;7:378–783. doi: 10.1002/prca.201200062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grainger DW, Greef CH, Gong P, Lochhead MJ. Current microarray surface chemistries. Methods Mol. Biol. 2007;381:37–57. doi: 10.1007/978-1-59745-303-5_2. [DOI] [PubMed] [Google Scholar]
- 39.Henkel S, Wellhausen R, Woitalla D, Marcus K, May C. Epitope Mapping Using Peptide Microarray in Autoantibody Profiling. Methods Mol. Biol. 2016;1368:209–924. doi: 10.1007/978-1-4939-3136-1_15. [DOI] [PubMed] [Google Scholar]
- 40.McWilliam I, Chong Kwan M, Hall D. Inkjet printing for the production of protein microarrays. Methods Mol. Biol. 2011;785:345–361. doi: 10.1007/978-1-61779-286-1_23. [DOI] [PubMed] [Google Scholar]
- 41.Maharjan S, et al. Dissection of the function of the RmpM periplasmic protein from Neisseria meningitidis. Microbiology. 2016;162:364–375. doi: 10.1099/mic.0.000227. [DOI] [PubMed] [Google Scholar]
- 42.Gu YH, et al. Structural basis of outer membrane protein insertion by the BAM complex. Nature. 2016;531:64–69. doi: 10.1038/nature17199. [DOI] [PubMed] [Google Scholar]
- 43.Delgado M, et al. Lipoprotein NMB0928 from Neisseria meningitidis serogroup B as a novel vaccine candidate. Vaccine. 2007;25:8420–8431. doi: 10.1016/j.vaccine.2007.09.053. [DOI] [PubMed] [Google Scholar]
- 44.Derrick JP, Urwin R, Suker J, Feavers IM, Maiden MCJ. Structural and evolutionary inference from molecular variation in Neisseria porins. Infect. Immun. 1999;67:2406–2413. doi: 10.1128/iai.67.5.2406-2413.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bennett JS, Callaghan MJ, Derrick JP, Maiden MCJ. Variation in the Neisseria lactamica porin, and its relationship to meningococcal PorB. Microbiology-(UK) 2008;154:1525–1534. doi: 10.1099/mic.0.2007/015479-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Andreae CA, Sessions RB, Virji M, Hill DJ. Bioinformatic analysis of meningococcal Msf and Opc to inform vaccine antigen design. PLoS One. 2018;13:21. doi: 10.1371/journal.pone.0193940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jolley KA, Appleby L, Wright JC, Christodoulides M, Heckels JE. Immunization with recombinant opc outer membrane protein from Neisseria meningitidis: Influence of sequence variation and levels of expression on the bactericidal immune response against meningococci. Infect. Immun. 2001;69:3809–3816. doi: 10.1128/iai.69.6.3809-3816.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cai XY, et al. Structure of Neisseria meningitidis lipoprotein GNA1162. Acta Crystallogr. F-Struct. Biol. Commun. 2013;69:362–368. doi: 10.1107/s1744309113004417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jolley, K. A. & Maiden, M. C. J. BIGSdb: Scalable analysis of bacterial genome variation at the population level. BMC Bioinformatics11, 10.1186/1471-2105-11-595 (2010). [DOI] [PMC free article] [PubMed]
- 50.Grizot S, Buchanan SK. Structure of the OmpA-like domain of RmpM from Neisseria meningitidis. Mol. Microbiol. 2004;51:1027–1037. doi: 10.1046/j.1365-2958.2003.03903.x. [DOI] [PubMed] [Google Scholar]
- 51.Filloux A, Voulhoux R. Multiple Structures Disclose the Secretins’ Secrets. J. Bacteriol. 2018;200:5. doi: 10.1128/jb.00702-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berry J-L, et al. Structure and Assembly of a Trans-Periplasmic Channel for Type IV Pili in Neisseria meningitidis. PLoS Path. 2012;8:e1002923. doi: 10.1371/journal.ppat.1002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holst J, et al. Vaccines against meningococcal serogroup B disease containing outer membrane vesicles (OMV) Lessons from past programs and implications for the future. Hum Vacc Immunother. 2013;9:1241–1253. doi: 10.4161/hv.24129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tappero JW, et al. Immunogenicity of 2 serogroup B outer-membrane protein meningococcal vaccines - A randomized controlled trial in Chile. J. Am. Med. Assoc. 1999;281:1520–1527. doi: 10.1001/jama.281.16.1520. [DOI] [PubMed] [Google Scholar]
- 55.Rosenqvist E, et al. Human antibody responses to meningococcal outer membrane antigens after 3 doses of the Norwegian Group B meningococcal vaccine. Infect. Immun. 1995;63:4642–4652. doi: 10.1128/iai.63.12.4642-4652.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rosenqvist E, et al. Functional activities and epitope specificity of human and murine antibodies against the class 4 outer membrane protein (Rmp) of Neisseria meningitidis. Infect. Immun. 1999;67:1267–1276. doi: 10.1128/iai.67.3.1267-1276.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zeth K, et al. Structure and function of the PorB porin from disseminating Neisseria gonorrhoeae. Biochem. J. 2013;449:631–642. doi: 10.1042/BJ20121025. [DOI] [PubMed] [Google Scholar]
- 58.Plummer AM, Fleming KG. From Chaperones to the Membrane with a BAM! Trends Biochem. Sci. 2016;41:872–882. doi: 10.1016/j.tibs.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sikora AE, et al. Structural and functional insights into the role of BamD and BamE within the beta-barrel assembly machinery in Neisseria gonorrhoeae. J. Biol. Chem. 2018;293:1106–1119. doi: 10.1074/jbc.RA117.000437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Noinaj N, et al. Structural insight into the biogenesis of beta-barrel membrane proteins. Nature. 2013;501:385–390. doi: 10.1038/nature12521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zielke RA, et al. Proteomics-driven Antigen Discovery for Development of Vaccines Against Gonorrhea. Mol. Cell. Proteomics. 2016;15:2338–2355. doi: 10.1074/mcp.M116.058800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Collins RF, et al. Structure of the Neisseria meningitidis outer membrane PilQ secretin complex at 12 Ångstrom resolution. J. Biol. Chem. 2004;279:39750–39756. doi: 10.1074/jbc.M405971200. [DOI] [PubMed] [Google Scholar]
- 63.Haghi F, Peerayeh SN, Siadat SD, Zeighami H. Recombinant outer membrane secretin PilQ(406-770) as a vaccine candidate for serogroup B Neisseria meningitidis. Vaccine. 2012;30:1710–1714. doi: 10.1016/j.vaccine.2011.12.076. [DOI] [PubMed] [Google Scholar]
- 64.Collins RF, et al. Interaction with type IV pili induces structural changes in the bacterial outer membrane secretin PilQ. J. Biol. Chem. 2005;280:18923–18930. doi: 10.1074/jbc.M411603200. [DOI] [PubMed] [Google Scholar]
- 65.Gorringe Andrew R., Pajón Rolando. Bexsero. Human Vaccines & Immunotherapeutics. 2012;8(2):174–183. doi: 10.4161/hv.18500. [DOI] [PubMed] [Google Scholar]
- 66.Gandhi A, Balmer P, York LJ. Characteristics of a new meningococcal serogroup B vaccine, bivalent rLP2086 (MenB-FHbp; Trumenba (R)) Postgrad. Med. 2016;128:548–556. doi: 10.1080/00325481.2016.1203238. [DOI] [PubMed] [Google Scholar]
- 67.McNeil LK, et al. Role of factor H binding protein in Neisseria meningitidis virulence and its potential as a vaccine candidate to broadly protect against meningococcal disease. Microbiol. Mol. Biol. Rev. 2013;77:234–252. doi: 10.1128/MMBR.00056-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chan W-Y, et al. A Novel, Multiple-Antigen Pneumococcal Vaccine Protects against Lethal Streptococcus pneumoniae Challenge. Infect. Immun. 2019;87:e00846–00818. doi: 10.1128/iai.00846-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bird, L. E. et al. In DNA Cloning and Assembly Methods Vol. 1116 Methods in Molecular Biology (eds Valla, S. & Lale, R.) 209–234 (Humana Press Inc, 2014).
- 70.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. Basic local alignment search tool. J. Mol. Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 71.Waterhouse A, et al. SWISS-MODEL: homology modelling of protein structures and complexes. Nucleic Acids Res. 2018;46:W296–W303. doi: 10.1093/nar/gky427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ashkenazy H, Erez E, Martz E, Pupko T, Ben-Tal N. ConSurf 2010: calculating evolutionary conservation in sequence and structure of proteins and nucleic acids. Nucleic Acids Res. 2010;38:W529–W533. doi: 10.1093/nar/gkq399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pettersen EF, et al. UCSF chimera - A visualization system for exploratory research and analysis. Journal of Computational Chemistry. 2004;25:1605–1612. doi: 10.1002/jcc.20084. [DOI] [PubMed] [Google Scholar]
- 74.Zhang, Y. I-TASSER server for protein 3D structure prediction. BMC Bioinformatics9, 10.1186/1471-2105-9-40 (2008). [DOI] [PMC free article] [PubMed]
- 75.Finn RD, et al. The Pfam protein families database: towards a more sustainable future. Nucleic Acids Res. 2016;44:D279–285. doi: 10.1093/nar/gkv1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cartwright K, et al. Immunogenicity and reactogenicity in UK infants of a novel meningococcal vesicle vaccine containing multiple class 1 (PorA) outer membrane proteins. Vaccine. 1999;17:2612–2619. doi: 10.1016/S0264-410X(99)00044-4. [DOI] [PubMed] [Google Scholar]
- 77.van der Ende A, Hopman CT, Dankert J. Multiple mechanisms of phase variation of PorA in Neisseria meningitidis. Infect. Immun. 2000;68:6685–6690. doi: 10.1128/IAI.68.12.6685-6690.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bart A, Dankert J, van der Ende A. Antigenic variation of the class I outer membrane protein in hyperendemic Neisseria meningitidis strains in the netherlands. Infect. Immun. 1999;67:3842–3846. doi: 10.1128/iai.67.8.3842-3846.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Snyder LA, Butcher SA, Saunders NJ. Comparative whole-genome analyses reveal over 100 putative phase-variable genes in the pathogenic Neisseria spp. Microbiology. 2001;147:2321–2332. doi: 10.1099/00221287-147-8-2321. [DOI] [PubMed] [Google Scholar]
- 80.Klugman KP, Gotschlich EC, Blake MS. Sequence of the structural gene (rmpM) for the class 4 outer membrane protein of Neisseria meningitidis, homology of the protein to gonococcal protein III and Escherichia coli OmpA, and construction of meningococcal strains that lack class 4 protein. Infect. Immun. 1989;57:2066–2071. doi: 10.1128/iai.57.7.2066-2071.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wright JC, Williams JN, Christodoulides M, Heckels JE. Immunization with the recombinant PorB outer membrane protein induces a bactericidal immune response against Neisseria meningitidis. Infect. Immun. 2002;70:4028–4034. doi: 10.1128/IAI.70.8.4028-4034.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Abad R, et al. Sequencing of the porB gene: a step toward a true characterization of Neisseria meningitidis. Clin Vaccine Immunol. 2006;13:1087–1091. doi: 10.1128/CVI.00211-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zapata GA, Vann WF, Rubinstein Y, Frasch CE. Identification of variable region differences in Neisseria meningitidis class 3 protein sequences among five group B serotypes. Mol. Microbiol. 1992;6:3493–3499. doi: 10.1111/j.1365-2958.1992.tb01784.x. [DOI] [PubMed] [Google Scholar]
- 84.Hansen MV, Wilde CE., 3rd Conservation of peptide structure of outer membrane protein-macromolecular complex from Neisseria gonorrhoeae. Infect. Immun. 1984;43:839–845. doi: 10.1128/iai.43.3.839-845.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Keiser PB, et al. A phase 1 study of a group B meningococcal native outer membrane vesicle vaccine made from a strain with deleted lpxL2 and synX and stable expression of opcA. Vaccine. 2010;28:6970–6976. doi: 10.1016/j.vaccine.2010.08.048. [DOI] [PubMed] [Google Scholar]
- 86.Sarkari J, Pandit N, Moxon ER, Achtman M. Variable expression of the Opc outer membrane protein in Neisseria meningitidis is caused by size variation of a promoter containing poly-cytidine. Mol. Microbiol. 1994;13:207–217. doi: 10.1111/j.1365-2958.1994.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 87.Seiler A, Reinhardt R, Sarkari J, Caugant DA, Achtman M. Allelic polymorphism and site-specific recombination in the opc locus of Neisseria meningitidis. Mol. Microbiol. 1996;19:841–856. doi: 10.1046/j.1365-2958.1996.437970.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.