Abstract
Objective: To study the general efficacy of hydromorphone as a systemic analgesic in postoperative pain management following single-port video-assisted thoracoscopic surgery (VATS) and to explore the optimal administration regimen.
Methods: A prospective, randomized, double-blind study was designed and conducted in a tertiary hospital. In total, 157 valid patients undergoing single-port VATS were randomly allocated into three groups. A total of 53 patients received morphine bolus only for postoperative analgesia (Group Mb); 51 patients received a hydromorphone background infusion plus bolus (Group Hb + i), and 53 patients received a hydromorphone bolus only (Group Hb). The primary outcomes were patient-reported static and dynamic pain levels; the secondary outcomes included side effects, sleep quality, and recovery indexes.
Results: Patients in Group Hb + i experienced lower pain intensity (approximately 10 out of 100 on the visual analog scale) in both static pain and dynamic pain in the days following surgery (P<0.01), better sleep quality during the first night only (P=0.002), and a higher satisfaction level than those in the other two groups (P=0.006). A comparison of these variables in Group Mb and Group Hb resulted in no significant differences. Lastly, side effects and recovery indexes remained the same among bolus-only groups and bolus-plus-background-infusion groups.
Conclusion: There is no advantage to administering hydromorphone over morphine using bolus only mode. Within 24 h after surgery, a background infusion should be considered as a part of a standard protocol for patient-controlled intravenous analgesia. At 24 h after surgery, the background infusion should be adjusted in accordance with patient preferences and pain intensity.
Keywords: morphine, background infusion, sleep quality, patient satisfaction
Introduction
According to 2018 global cancer statistics, new lung cancer cases reached 11.6% of the total number of cancer cases, and relevant deaths accounted for 18.4% of all deaths caused by cancer, and the same trend was observed in China.1,2 Surgery is the primary option for lung cancer treatment at the early and middle stages. Even though several minimally invasive surgical methods, such as single-port video-assisted thoracoscopic surgery (VATS), have been introduced, many patients still suffer moderate to severe pain postoperatively.3–5 Until now, there has been no standardized protocol for postoperative pain management for single-port VATS.6
A multimodal analgesia regimen is preferred, combining loco-regional analgesia and systemic analgesia to enhance pain relief and reduce side effects.7–9 Intercostal nerve block is an alternative regional anesthesia that is effective for up to 16 h and could reduce analgesic consumption during the first 24 h after surgery instead of thoracic epidural analgesia (TEA) or thoracic paravertebral block, which demonstrate various limitations including the challenge of placing a thoracic epidural catheter, the extra care services required, and possible complications.10–13 Patient-controlled intravenous analgesia (PCIA) is a personalized strategy involving various opioids that allows patients to administer analgesics as needed, and has been demonstrated to be effective for postoperative pain management as TEA under diverse conditions.14–18
Hydromorphone, widely used in the US and Europe, a hydrogenated ketone of morphine, is approximately five to 10 times stronger than its precursor, and has been available in the Chinese medical market for only a few years.19–22 The physicochemical properties (predominantly involving µ-receptors) and metabolites (mainly hydromorphone-3-glucoronide with no analgesic effects) of hydromorphone may lead to fewer side effects when compared with some other opioids commonly used such as morphine, while the analgesic effects remain the same. However, there is a paucity of clinical research studies exploring the optimal PCIA delivery of hydromorphone. In existing clinical trials, most PCIA protocols did not take body weight into account and were fixed for bolus and continuous infusion settings.23–26 Furthermore, there is a lack of studies on the efficacy of hydromorphone in PCIA electrical pumps for patients undergoing single-port VATS.
We have conducted this prospective, randomized controlled trial to investigate the analgesic effect of hydromorphone when used as a systemic analgesic following single-port VATS and to explore the optimal administration regimen.
Methods
Ethics approval and participation consent
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, Zhejiang, China (Ethical number: 2018[014]) and the protocol was registered in the ClinicalTrials.gov registry (NCT03648008). All subjects signed informed consent documents before enrollment. Our study was conducted in accordance with the Declaration of Helsinki.
Sample size calculation
The sample size was pre-calculated using PASS 11 (NCSS Inc., Kaysville, UT, USA) based on the following assumptions: based on related studies, a minimal equivalence of 10 and a standard deviation (SD) of 10 on the Visual Analogue Scale (VAS) were considered as statistically significant changes. The sample size for each group was 57 with α=0.05 (two-sided hypothesis), β=0.80, and a 10% drop-out rate.
Criteria for inclusion and exclusion
The day before surgery, an investigator assessed patients in accordance with the criteria for inclusion and exclusion (Table 1) and confirmed patient willingness to participate in the study after the investigator fully informed the patient about the study goals and design.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Willing participants and signed informed consent Age ≤70 years and age ≥18 ASA I–III Selective operation with single port VATS (unilateral pulmonary wedge resection, segmentectomy, lobectomy, or pneumonectomy) |
History of mental illness, or chronic pain, or alcohol drug abuse, or long-term use of analgesics, sedative drugs, antidepressant drugs, antianxiety drugs, NSAIDs drugs |
| Remarkably abnormal liver and/or kidney function (more than two times of the normal index) | |
| History of abnormal anesthesia progress. Sedatives, analgesics, antiemetic drugs and anti-pruritic drugs used within 24 h prior to the operation | |
| Allergy to related opioid drugs | |
| Monoamine oxidase inhibitors, antidepressants, or antiepileptic drugs administered within 15 days prior to surgery | |
| Communication disorder | |
| Women during pregnancy or lactation Unsuitable for clinical study for other reasons |
Randomization and blinding
Upon receiving written consent, patients were instructed on how to use the VAS (0=no pain to 100=intense pain) to describe the pain they were experiencing. Each patient was randomized into one of the three groups (Group Mb, Group Hb + i, and Group Hb) with an allocation ratio of 1:1:1, using a random, computer-generated table (Table 2). All patients, surgeons, nurses, and data collectors participating in the study were blinded until the final data analysis.
Table 2.
PCIA protocol for groups
| Analgesic | Group Mb | Group Hb + i | Group Hb |
|---|---|---|---|
| Morphine | Hydromorphone | Hydromorphone | |
| Background infusion | 0 | 0.002 mg*kg−1h−1 | 0 |
| Bolus | 0.015 mg*kg−1 | 0.002 mg*kg−1 | 0.002 mg*kg−1 |
| Lockout interval | 8 min | 10 min | 8 min |
To test the pharmacological impact of hydromorphone, two background infusion conditions were compared: 0.002 mg*kg−1h−1 hydromorphone or none. The bolus setting was maintained at 0.002 mg*kg−1, but the lockout interval differed from 10 min to 8 min in order to balance the maximum opioid usage per hour. In the control group, morphine was used in the PCIA pump (bolus 0.015 mg*kg−1, lockout interval 8 min) in the ratio 7.5:1 to hydromorphone.
Anesthesia protocol
All patients avoided preoperative usage of pain medication. In the operation theatre, patients received general anesthesia under standard protocol, which did not include hydromorphone or morphine. Specifically, general anesthesia was induced using midazolam (0.2 mg*kg−1), sufentanil (10 μg*kg−1), and etomidate (0.3 mg*kg−1). Cisatracurium besilate (0.15 mg*kg−1) was administered to induce neuromuscular blockade for tracheal intubation. Anesthesia was continuously maintained using sevoflurane, propofol, and sufentanil. Cisatracurium was used as needed. During the surgery, standardized monitoring and a bispectral index were applied. Central venous catheterization (CVC) and an A-line were implemented for each patient. After surgery, patients were transferred to the postanesthesia care unit (PACU) where their vital signs were continuously monitored. Each subject was extubated and discharged from the PACU when their vital signs stabilized.
Surgical protocol
All 157 patients underwent single-port VATS performed by one attending surgeon. To initiate the single-port VATS, an incision (approximately 3 cm) was made at the fifth intercostal space at the anterior axillary line. The incision was protected using a plastic wound protector. The periosteum and rib were not retracted, the latissimus dorsi muscle was left intact, and the serratus anterior muscle was split apart. Through the single port protector, a 10-mm 30-degree thoracoscope was inserted at the posterior side and two thoracoscopic instruments were inserted from the anterior side into the chest cavity. An endoscopic stapling method was implemented to perform lesion excision and fissure fusion to minimize air leakage. During the surgery, the surgeon was careful not to move the instrument to extreme angles and did not use metallic retraction in order to lessen the risk of crushing intercostal nerves. At the end of the operation, one chest tube and one central venous catheter were separately placed through the incision and the posterior costophrenic angle for drainage.
Postoperative pain and side effect management
Before closure of the thoracic incision, the surgeons performed a three-site intercostal nerve block with 0.75% 10 mL ropivacaine using a thoracoscope. At the end of surgery, pentazocine (5 mg) and tropisetron (5 mg) were administered by the anesthetist. Immediately after surgery, a PCIA pump was connected to the CVC, with different drugs and settings based on the experimental group. In the case of PCIA analgesic failure (VAS constantly >40), dynastat (40 mg) was administered as an alternative rescue method. Tropisetron (5 mg) or palonosetron (0.25 mg) were administered to combat postoperative nausea and vomiting (PONV).
Follow-up and data collection
During the preoperative interview, demographic characteristics, educational background, work type, history of cigarette smoking and alcohol consumption, and preoperative sleep quality were recorded. Intraoperative parameters including surgery type and duration, anesthesia duration, lymphadenectomy, adhesion loosening, and pathologic diagnosis were recorded. VAS at rest was recorded 0.5 h after extubation. After the patients were moved to the thoracic surgery ward, VAS at rest and during coughing were recorded each morning (8 a.m.) and evening (8 p.m.) for the first 3 days or until discharge from hospital.
The primary outcomes were pain intensity assessed by the VAS at rest (static pain) and during coughing (dynamic pain). Secondary outcomes included bolus frequency, analgesic rescue, nausea, vomiting, antiemetic rescue, postoperative sleep quality, cacation within two days, out-of-bed activity, chest tube extubation, hospital day after surgery and patient satisfaction. Before discharge, patients were asked about the degree of satisfaction with their pain management experience (Bad, Fair, Good, or Excellent). The postoperative follow-up was conducted by an investigator who was unaware of which group an individual belonged to.
Statistical analysis
Based on the variable distribution type, variables with normal and abnormal distributions are presented as mean (SD) and median (range or IQR), respectively. For a comparison of pain levels between the three groups during the postoperative period, a repeated measure analysis of variance (ANOVA) test was used. The distributions of patient characteristics and other variables among Group Mb, Group Hb + i, and Group Hb were compared using an ANOVA for continuous variables, the Pearson chi-square test or Fisher’s exact test for categorical variables, and the Kruskal–Wallis test for abnormally distributed variables. The Least Significant Difference (LSD) test was used for posthoc analysis. P<0.05 was considered to indicate a significant difference. All statistical analyses were performed using SPSS version 23.0 (SPSS Inc., Chicago, IL, USA).
Results
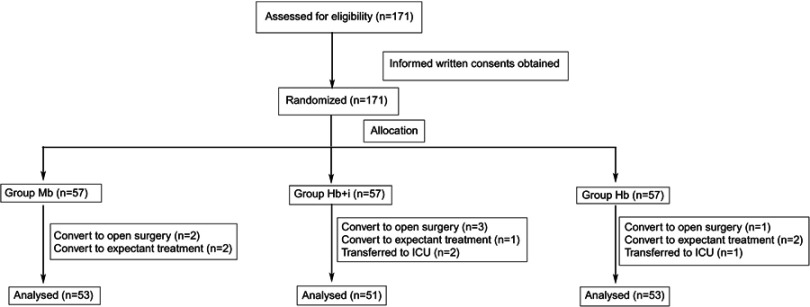
From May to September 2018, a total of 171 patients voluntarily consented to participate in this study and were randomly allocated to one of the three groups (Figure 1). A total of 14 patients were withdrawn because of conversion to open surgery, expectant treatment, or transfer to the intensive care unit after surgery. Therefore, data from 157 patients were used in the final analysis, as shown in Figure 1.
Figure 1.
Study flow diagram.
There were no significant differences between the three groups in terms of age, gender, weight, body mass index, history of cigarette smoking, history of alcohol consumption, education level, work type, preoperative stage sleep quality, surgical type, lymphadenectomy, adhesion loosening, pathologic diagnosis, baseline VAS (0.5 h after extubation), surgical duration, and anesthesia duration (Tables 3 and 4).
Table 3.
Distribution of sociodemographic characteristics between groups
| Variables | Group | P-value | ||
|---|---|---|---|---|
| Group Mb (n=53) | Group Hb + i (n=51) | Group Hb (n=53) | ||
| Age (y) (mean ± SD) | 58.28±8.28 | 58.08±7.89 | 58.11±8.30 | 0.99 |
| Sex | 1.00 | |||
| Female | 27 (50.9%) | 26 (51.0%) | 27 (50.9%) | |
| Male | 26 (49.1%) | 25 (49.0%) | 26 (49.1%) | |
| Weight (mean ± SD) | 61.15±10.28 | 61.94±8.97 | 61.08±11.85 | 0.90 |
| BMI (mean ± SD) | 22.59±3.03 | 23.02±2.64 | 22.67±3.00 | 0.73 |
| History of cigarette smoking | 0.22 | |||
| Yes | 10 (18.9%) | 17 (33.3%) | 12 (22.6%) | |
| No | 43 (81.1%) | 34 (66.7%) | 41 (77.4%) | |
| History of alcohol consumption | 0.45 | |||
| Yes | 10 (18.9%) | 10 (19.6%) | 15 (28.3%) | |
| No | 43 (81.1%) | 41 (80.4%) | 38 (71.7%) | |
| Educational level | 0.50 | |||
| Low | 22 (41.5%) | 19 (37.3%) | 22 (41.5%) | |
| Medium | 19 (35.8%) | 26 (51.0%) | 22 (41.5%) | |
| High | 12 (22.6%) | 6 (11.8%) | 9 (17.0%) | |
| Work type | 0.40 | |||
| Manual labor | 21 (39.6%) | 24 (47.1%) | 18 (34.0%) | |
| Knowledge work | 32 (60.4%) | 27 (52.9%) | 35 (66.0%) | |
| Sleep quality | 0.66 | |||
| Poor | 6 (11.3%) | 11 (21.6%) | 7 (13.2%) | |
| Fair | 20 (37.7%) | 18 (35.3%) | 21 (39.6%) | |
| Good | 27 (50.9%) | 22 (43.1%) | 25 (47.2%) | |
Note: P<0.05 indicated a significant difference.
Table 4.
Distribution of clinical characteristics between groups
| Variables | Group | P-value | ||
|---|---|---|---|---|
| Group Mb (n=53) | Group Hb + i (n=51) | Group Hb (n=53) | ||
| Surgery time (median [IQR]) | 90 (62.5–105) | 80 (65–95) | 85 (60–115) | 0.63 |
| Anesthesia time (median [IQR]) | 115 (92.5–135) | 100 (85–15) | 115 (82.5–140) | 0.53 |
| Surgery type | 0.77 | |||
| Wedge resection | 12 (22.6%) | 8 (15.7%) | 8 (15.1%) | |
| Segmentectomy | 8 (15.1%) | 6 (11.8%) | 6 (11.3%) | |
| Lobectomy | 33 (62.3%) | 37 (72.5%) | 38 (71.7%) | |
| Pneumonectomy | 0 | 0 | 1 (1.9%) | |
| Lymph node dissection | 0.11 | |||
| Yes | 41 (77.4%) | 47 (92.2%) | 46 (86.8%) | |
| No | 12 (22.6%) | 4 (7.8%) | 7 (13.2%) | |
| Adhesion loosening | 0.86 | |||
| Yes | 26 (49.1%) | 25 (49.0%) | 29 (54.7%) | |
| No | 27 (50.9%) | 26 (51.0%) | 24 (45.3%) | |
| Pathologic diagnosis | 0.29 | |||
| Malignant | 45 (84.9%) | 48 (94.1%) | 49 (92.5%) | |
| Benign | 8 (15.1%) | 3 (5.9%) | 4 (7.5%) | |
| VAS at rest (0.5 h after extubation) | 0 (0–23.5) | 0 (0–17.0) | 0 (0–20.0) | 0.98 |
Note: P<0.05 indicated a significant difference.
Assessment of postoperative pain and analgesia
A total of 33% of patients returned to the recovery ward around or after 8 p.m. and 24% of patients were discharged from the hospital on the second day after surgery. To preserve the integrity of the data, the following time points were discarded: 8 p.m. on the day of surgery and 8 p.m. on the second day after surgery. Therefore, data at three time points were collected: 8 a.m. and 8 p.m. on the first day postsurgery, and 8 a.m. on the second day postsurgery.
As shown in Table 4, at 0.5 h after tracheal extubation, there was no significant difference in VAS at rest between the three groups (P=0.98). At the aforementioned three time points, VAS at rest or during coughing were all lowest in Group Hb + i (P<0.001). The time effect was independent among the three groups (P<0.001) and the interaction effect with analgesic drugs was non-existent (P=0.140 and 0.854, respectively) (Table 5). Table 6 summarizes the usage of bolus and analgesic rescue. Patients randomized into Group Hb + i consumed the lowest number of boluses compared with patients in Group Mb and Group Hb at all three follow-up time points (P=0.044, 0.008, and 0.036, sequentially). However, there was no significant difference in analgesic rescue among the three groups (P=0.37, 0.59, and 0.09, sequentially) (Table 6).
Table 5.
Postoperative patient pain between groups
| Variables | Group | P-value | ||||
|---|---|---|---|---|---|---|
| Group Mb (n=53) | Group Hb + i (n=51) | Group Hb (n=53) | Group effect | Time effect | Interaction effect | |
| VAS at rest | <0.001 | <0.001 | 0.140 | |||
| 8 a.m. 1st day postsurgery | 26.0±15.6 | 17.1±12.1*# | 29.5±16.1 | |||
| 8 p.m. 1st day postsurgery | 15.2±12.5 | 7.7±9.3*# | 19.0±14.4 | |||
| 8 a.m. 2nd day postsurgery | 7.7±9.3 | 3.9±7.0*# | 10.3±10.5 | |||
| VAS on cough | <0.001 | <0.001 | 0.854 | |||
| 8 a.m. 1st day postsurgery | 52.2±14.9 | 42.8±15.2*# | 55.1±15.0 | |||
| 8 p.m. 1st day postsurgery | 42.3±13.7 | 33.8±10.9*# | 45.5±14.0 | |||
| 8 a.m. 2nd day postsurgery | 36.0±13.9 | 25.4±10.3*# | 36.5±14.1 | |||
Notes: *P<0.05 in comparison with Group Mb; #P<0.05 in comparison with Group Hb. P<0.05 indicated a significant difference.
Table 6.
Analgesic use between groups
| Variables | Group | P-value | ||
|---|---|---|---|---|
| Group Mb (n=53) | Group Hb + i (n=51) | Group Hb (n=53) | ||
| Bolus frequency | ||||
| 8 a.m. 1st day postsurgery | 2 (1–4) | 1 (0–3) | 3 (1–4) | 0.044 |
| 8 p.m. 1st day postsurgery | 3 (2–5) | 1 (0–3)* | 3 (1–4.75) | 0.008 |
| 8 a.m. 2nd day postsurgery | 1 (0–3) | 0 (0–2)* | 1 (0–2.5) | 0.036 |
| Analgesic rescue | ||||
| 8 a.m. 1st day postsurgery | 0.37 | |||
| Yes | 18 (34.0%) | 11 (21.6%) | 14 (26.4%) | |
| No | 35 (66.0%) | 40 (78.4%) | 39 (73.6%) | |
| 8 p.m. 1st day postsurgery | 0.59 | |||
| Yes | 22 (42.3%) | 26 (51.0%) | 27 (51.9%) | |
| No | 30 (57.7%) | 25 (49.0%) | 25 (48.1%) | |
| 8 a.m. 2nd day postsurgery | 0.09 | |||
| Yes | 10 (19.2%) | 11 (21.6%) | 19 (36.5%) | |
| No | 42 (80.8%) | 40 (78.4%) | 33 (63.5%) | |
Notes: *P<0.05 in comparison with Group Mb. P<0.05 indicated a significant difference.
Assessment of PONV and early rehabilitation index
Tables 7 and 8 summarize postoperative complications such as nausea, vomiting, length of stay, postoperative sleep quality, and early rehabilitation indexes. Sleep quality during the first night and patient satisfaction were significantly different among the three groups (P=0.002 and P=0.006), with Group Hb + i performing better than the other two groups. There was no significant difference among the other indexes.
Table 7.
Adverse reaction and sleep quality between groups
| Variables | Group | P-value | ||
|---|---|---|---|---|
| Group Mb (n=53) | Group Hb + i (n=51) | Group Hb (n=53) | ||
| Nausea | ||||
| 8 a.m. 1st day postsurgery | 0.20 | |||
| Yes | 18 (34.0%) | 22 (43.1%) | 14 (26.4%) | |
| No | 35 (66.0%) | 29 (56.9%) | 39 (73.6%) | |
| 8 p.m. 1st day postsurgery | 0.74 | |||
| Yes | 10 (19.2%) | 9 (17.6%) | 7 (13.5%) | |
| No | 42 (80.8%) | 42 (82.4%) | 45 (86.5%) | |
| 8 a.m. 2nd day postsurgery | 0.64 | |||
| Yes | 3 (5.8%) | 4 (7.8%) | 2 (3.8%) | |
| No | 49 (94.2%) | 47 (92.2%) | 50 (96.2%) | |
| Vomiting | ||||
| 8 a.m. 1st day postsurgery | 0.16 | |||
| Yes | 7 (13.2%) | 14 (27.5%) | 9 (17.0%) | |
| No | 46 (86.8%) | 37 (72.5%) | 44 (83.0%) | |
| 8 p.m. 1st day postsurgery | 1.00 | |||
| Yes | 4 (7.7%) | 4 (7.8%) | 4 (7.7%) | |
| No | 48 (92.3%) | 47 (92.2%) | 48 (92.3%) | |
| 8 a.m. 2nd day postsurgery | 0.13 | |||
| Yes | 1 (1.9%) | 3 (5.9%) | 0 | |
| No | 51 (98.1%) | 48 (94.1%) | 52 | |
| Antiemetic rescue | ||||
| 8 a.m. 1st day postsurgery | 0.72 | |||
| Yes | 4 (7.5%) | 4 (7.8%) | 2 (3.8%) | |
| No | 49 (92.5%) | 47 (92.2%) | 51 (96.2%) | |
| 8 p.m. 1st day postsurgery | 0.20 | |||
| Yes | 7 (13.5%) | 9 (17.6%) | 3 (5.8%) | |
| No | 45 (86.5%) | 42 (82.4%) | 49 (94.2%) | |
| 8 a.m. 2nd day postsurgery | 0.51 | |||
| Yes | 3 (5.8%) | 6 (11.8%) | 4 (7.7%) | |
| No | 49 (94.2%) | 45 (88.2%) | 48 (92.3%) | |
| Sleep quality during 1st night | 0.002 | |||
| Poor | 24 (45.3%) | 12 (23.5%)# | 30 (56.6%) | |
| Fair | 24 (45.3%) | 23 (45.1%) | 17 (32.1%) | |
| Good | 5 (9.4%) | 16 (31.4%)*# | 6 (11.3%) | |
| Sleep quality during 2nd night | 0.278 | |||
| Poor | 7 (13.5%) | 3 (5.9%) | 6 (11.5%) | |
| Fair | 20 (38.5%) | 14 (27.5%) | 21 (40.4%) | |
| Good | 25 (48.1%) | 34 (66.7%) | 25 (48.1%) | |
Notes: *P<0.05 in comparison with Group Mb; #P<0.05 in comparison with Group Hb. P<0.05 indicated a significant difference.
Table 8.
Rehabilitation index between groups
| Variables | Group | P-value | ||
|---|---|---|---|---|
| Group Mb (n=53) | Group Hb + i (n=51) | Group Hb (n=53) | ||
| Cacation within 2 days | 0.37 | |||
| Yes | 14 (26.4%) | 11 (21.6%) | 18 (34.0%) | |
| No | 39 (73.6%) | 40 (78.4%) | 35 (66.0%) | |
| Out-of-bed activity | 1.00 | |||
| First day | 50 (94.3%) | 48 (94.1%) | 50 (94.3%) | |
| Second day | 3 (5.7%) | 3 (5.9%) | 3 (5.7%) | |
| Chest tube extubation time | ||||
| First tube | 1 (1–2) | 2 (1–2) | 2 (1–2) | 0.90 |
| Second tube | 3 (2–5) | 3 (2–4) | 3 (2–4) | 0.85 |
| Patient satisfaction | 0.006 | |||
| Bad | 5 (9.4%) | 4 (7.8%) | 9 (17.0%) | |
| Fair | 36 (67.9%) | 21 (41.2%)* | 34 (64.2%) | |
| Good | 11 (20.8%) | 25 (49.0%)*# | 10 (18.9%) | |
| Excellent | 1 (1.9%) | 1 (2.0%) | 0 | |
| Hospital day after surgery | 3 (2–5) | 3 (2–4) | 3 (3–4) | 0.79 |
Notes: *P<0.05 in comparison with Group Mb; #P<0.05 in comparison with Group Hb. P<0.05 indicated a significant difference.
Discussion
Minimally invasive surgery is preferred for lung diseases because of its potential for reduced trauma and enhanced recovery. However, postoperative pain remains moderate to severe, especially within 48 h after single-port VATS.3–5 PCIA using traditional opioids is an effective therapy for postoperative pain. However, side effects associated with opioids are an issue, especially PONV. Consequently, we aimed to find a more appropriate type of opioid, with better analgesic effects or lower side effects. The current study aimed to verify whether hydromorphone is a better alternative to morphine and determine the optimal administration procedure for hydromorphone in PCIA for postoperative pain management after single-port VATS.
Contrary to our hypothesis, the results indicated that hydromorphone exhibited no noticeable advantage over morphine in terms of pain management and side effects in the bolus only setting. Some of the limitations of the study may underlie these results. First, based on the primary original design and intention of this study and data from manufacturers and other studies, the ratio of morphine to hydromorphone was set at 7.5:1. However, a higher ratio such as 6:1 or 5:1 may be more appropriate to demonstrate the superiority of hydromorphone. Second, adding a morphine background infusion group might have been beneficial in comparing the effectiveness of hydromorphone and morphine with different administration regimens.
As the results show, adding a background infusion of hydromorphone in PCIA may outweigh its disadvantages. Previous studies have suggested that there are no advantages to using a supplemental background infusion for pain relief, and its use could lead to higher incidences of complications.30–36 Contrary to this argument, research conducted by Wang and his colleagues support background-infused analgesics, since higher sedation ratings and fewer side effects were reported after abdominal hysterectomy;37 White also found that a combined background infusion of morphine can provide better pain management, reduce opioid consumption, and minimize complications compared with a PCIA bolus-only protocol following colorectal cancer surgery.38 The discrepancies in background infusion efficacy may be attributed to different surgery types, distinct ethnic groups, and diverse analgesic regimens.
From the second postsurgery night onward, the rest pain in each group was not substantially different, even though there was a statistically significant difference, while the background infusion reduced dynamic pain to some extent (10 out of 100). There were no statistically significant differences in side effects and antiemetic rescue when comparing analgesic treatment with or without background infusion. However, the frequency of PONV in Group Hb + i was relatively higher than in the other two groups, especially at 8 p.m. from the first day and afterwards. The sample size was limited in the current study, and this phenomenon requires further investigation with a larger sample size to determine whether the benefits from background infusion outweigh the side effects beyond 24 h after surgery.
Surgery related pain leads to sleep disruption, which delays postoperative recovery.42–44 The relationships between these factors are intertwined: unsatisfactory sleep may increase sensitivity to pain during the following day, so a higher pain intensity would be experienced and more analgesic medication utilized. Subsequently, sleep quality during the following night would be influenced by daytime pain intensity and analgesic medication.49,50 The patients in Group Hb + i had better sleep quality while experiencing low pain intensity and requiring less extra analgesic rescue to achieve better sleep quality than those in Group Mb and Group Hb during the first night. As time progressed beyond 24 h after surgery, the pain scores were below the desired VAS of approximately 40 and there was no significant difference among the three groups in terms of sleep quality during the second night. This may be attributed to the low-dose background infusion of opioid analgesic that kept the pain under control and facilitated sleep. With better pain management and sleep quality during the first night, patient satisfaction was also significantly higher in Group Hb + i.
The intense pain caused by this type of surgery is normally sustained within 24 h, especially during the first night and the first morning after surgery. As observed during this study, an overwhelming majority of patients undergoing this type of surgery can achieve satisfactory pain relief 24 h after surgery, regardless of the type of intervention used. The observed complications were not significantly higher with background infusion. Also, background infusion did not hinder discharge, extubation of chest tubes, out-of-bed activity, and other postoperative rehabilitation indexes.
Conclusion
The current study suggests that in the bolus only mode, hydromorphone has no advantages over morphine and within 24 h after surgery, a background infusion should be added to the protocol for better sleep quality and pain management. At 24 h after surgery, the bolus-only method should be considered, and the background infusion should be adjusted according to patient demand and pain intensity to avoid unwanted complications.
Acknowledgments
The authors thank Professor Yunxian Yu (Department of Epidemiology & Health Statistics, School of Public Health, School of Medicine, Zhejiang University) for assistance in analyzing the results; Bin Zheng (Department of Surgery, University of Alberta), Wuyi Xia (Department of Anesthesia, David Geffen School of Medicine at UCLA), and Jillian Kobayashi (Department of Anesthesia, David Geffen School of Medicine at UCLA) for assistance in language editing. This study was carried out in and was funded by the Department of Anesthesiology, the Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China. Clinical Trial Number: NCT03648008 https://register.clinicaltrials.gov.
Data sharing
All the data will be available through email by contacting our group and we will provide the data in perpetuity.
Disclosure
All the authors have no conflicts of interest to declare in this work.
References
- 1.Chen W, Sun K, Zheng R, et al. Cancer incidence and mortality in China, 2014. Chin J Cancer Res. 2018;30:1–12. doi: 10.21147/j.issn.1000-9604.2018.01.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 3.Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: a propensity-matched comparative analysis. J Thorac Dis. 2016;8:2872–2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med. 2015;3:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirai K Takeuchi S and Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomesdagger. Eur J Cardiothorac Surg. 2016;49(Suppl 1):i37–i41. doi: 10.1093/ejcts/ezv320 [DOI] [PubMed] [Google Scholar]
- 6.Holbek BL, Horsleben Petersen R, Kehlet H, et al. Fast-track video-assisted thoracoscopic surgery: future challenges. Scand Cardiovasc J. 2016;50:78–82. doi: 10.3109/14017431.2015.1114665 [DOI] [PubMed] [Google Scholar]
- 7.Wick EC Grant MC and Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152:691–697. doi: 10.1001/jamasurg.2017.0898 [DOI] [PubMed] [Google Scholar]
- 8.Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the american pain society, the american society of regional anesthesia and pain medicine, and the American society of anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016;17:131–157. doi: 10.1016/j.jpain.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 9.Savoia G, Alampi D, Amantea B, et al. Postoperative pain treatment SIAARTI recommendations 2010. Short version. Minerva Anestesiol. 2010;76:657–667. [PubMed] [Google Scholar]
- 10.Pace MM, Sharma B, Anderson-Dam J, et al. Ultrasound-guided thoracic paravertebral blockade: a retrospective study of the incidence of complications. Anesth Analg. 2016;122:1186–1191. doi: 10.1213/ANE.0000000000001117 [DOI] [PubMed] [Google Scholar]
- 11.Kelly ME, Mc Nicholas D, Killen J, et al. Thoracic paravertebral blockade in breast surgery: is pneumothorax an appreciable concern? A review of over 1000 cases. Breast J. 2018;24:23–27. doi: 10.1111/tbj.12831 [DOI] [PubMed] [Google Scholar]
- 12.Piccioni F, Colombo J, Fumagalli L, et al. Inadvertent high central neuraxial block and possible total spinal anaesthesia occurring after nerve stimulation guided thoracic paravertebral block. Anaesth Intensive Care. 2014;42:270–271. [PubMed] [Google Scholar]
- 13.Yamauchi Y, Isaka M, Ando K, et al. Continuous paravertebral block using a thoracoscopic catheter-insertion technique for postoperative pain after thoracotomy: a retrospective case-control study. J Cardiothorac Surg. 2017;12:5. doi: 10.1186/s13019-017-0566-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butkovic D, Kralik S, Matolic M, et al. Postoperative analgesia with intravenous fentanyl PCA vs epidural block after thoracoscopic pectus excavatum repair in children. Br J Anaesth. 2007;98:677–681. doi: 10.1093/bja/aem055 [DOI] [PubMed] [Google Scholar]
- 15.Yie JC, Yang JT, Wu CY, et al. Patient-controlled analgesia (PCA) following video-assisted thoracoscopic lobectomy: comparison of epidural PCA and intravenous PCA. Acta Anaesthesiol Taiwan. 2012;50:92–95. doi: 10.1016/j.aat.2012.08.004 [DOI] [PubMed] [Google Scholar]
- 16.Kim JA, Kim TH, Yang M, et al. Is intravenous patient controlled analgesia enough for pain control in patients who underwent thoracoscopy? J Korean Med Sci. 2009;24:930–935. doi: 10.3346/jkms.2009.24.5.930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant RP, Dolman JF, Harper JA, et al. Patient-controlled lumbar epidural fentanyl compared with patient-controlled intravenous fentanyl for post-thoracotomy pain. Can J Anaesth. 1992;39:214–219. doi: 10.1007/BF03008779 [DOI] [PubMed] [Google Scholar]
- 18.Hiro K, Sugiyama T, Kurata M, et al. Postoperative analgesia for video-assisted thoracoscopic surgery–continuous intravenous infusion of fentanyl combined with intercostal nerve block v.s. Continuous epidural analgesia. Masui. Jpn J Anesthesiology. 2016;65:114–118. [PubMed] [Google Scholar]
- 19.Mahler DL, Forrest WH Jr. Relative analgesic potencies of morphine and hydromorphone in postoperative pain. Anesthesiology. 1975;42:602–607. [DOI] [PubMed] [Google Scholar]
- 20.Hill JL, Zacny JP. Comparing the subjective, psychomotor, and physiological effects of intravenous hydromorphone and morphine in healthy volunteers. Psychopharmacology (Berl). 2000;152:31–39. [DOI] [PubMed] [Google Scholar]
- 21.Lawlor P, Turner K, Hanson J, et al. Dose ratio between morphine and hydromorphone in patients with cancer pain: a retrospective study. Pain. 1997;72:79–85. [DOI] [PubMed] [Google Scholar]
- 22.Hong D, Flood P, Diaz G. The side effects of morphine and hydromorphone patient-controlled analgesia. Anesth Analg. 2008;107:1384–1389. doi: 10.1213/ane.0b013e3181823efb [DOI] [PubMed] [Google Scholar]
- 23.Yang Y, Wu J, Li H, et al. Prospective investigation of intravenous patient-controlled analgesia with hydromorphone or sufentanil: impact on mood, opioid adverse effects, and recovery. BMC Anesthesiol. 2018;18:37. doi: 10.1186/s12871-018-0540-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nedeljkovic SS, Correll DJ, Bao X, et al. Randomised, double-blind, parallel group, placebo-controlled study to evaluate the analgesic efficacy and safety of VVZ-149 injections for postoperative pain following laparoscopic colorectal surgery. BMJ Open. 2017;7:e011035. doi: 10.1136/bmjopen-2016-011035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu S, Carpenter RL, Mulroy MF, et al. Intravenous versus epidural administration of hydromorphone. Effects on analgesia and recovery after radical retropubic prostatectomy. Anesthesiology. 1995;82:682–688. [DOI] [PubMed] [Google Scholar]
- 26.Bell JG, Shaffer LE, Schrickel-Feller T. Randomized trial comparing 3 methods of postoperative analgesia in gynecology patients: patient-controlled intravenous, scheduled intravenous, and scheduled subcutaneous. Am J Obstet Gynecol. 2007;197(472):e1–e7. doi: 10.1016/j.ajog.2007.03.039 [DOI] [PubMed] [Google Scholar]
- 30.Chen WH, Liu K, Tan PH, et al. Effects of postoperative background PCA morphine infusion on pain management and related side effects in patients undergoing abdominal hysterectomy. J Clin Anesth. 2011;23:124–129. doi: 10.1016/j.jclinane.2010.08.008 [DOI] [PubMed] [Google Scholar]
- 31.Mackie AM, Bc C, Hf H. Adolescents use patient-controlled analgesia effectively for relief from prolonged oropharyngeal mucositis pain. Pain. 1991;46:265–269. [DOI] [PubMed] [Google Scholar]
- 32.Parker RK, Holtmann B, Pf W. Effects of a nighttime opioid infusion with PCA therapy on patient comfort and analgesic requirements after abdominal hysterectomy. Anesthesiology. 1992;76:362–367. [DOI] [PubMed] [Google Scholar]
- 33.White PF, Parker RK. Is the risk of using a “basal” infusion with patient-controlled analgesia therapy justified? Anesthesiology. 1992;76:489. doi: 10.1097/00000542-199203000-00043 [DOI] [PubMed] [Google Scholar]
- 34.Doyle E, Robinson D, Ns M. Comparison of patient-controlled analgesia with and without a background infusion after lower abdominal surgery in children. Br J Anaesth. 1993;71:670–673. [DOI] [PubMed] [Google Scholar]
- 35.Morad A, Winters B, Stevens R, et al. The efficacy of intravenous patient-controlled analgesia after intracranial surgery of the posterior fossa: a prospective, randomized controlled trial. Anesth Analg. 2012;114:416–423. doi: 10.1213/ANE.0b013e31823f0c5a [DOI] [PubMed] [Google Scholar]
- 36.van Beers EJ, van Tuijn CF, Nieuwkerk PT, et al. Patient-controlled analgesia versus continuous infusion of morphine during vaso-occlusive crisis in sickle cell disease, a randomized controlled trial. Am J Hematol. 2007;82:955–960. doi: 10.1002/ajh.20944 [DOI] [PubMed] [Google Scholar]
- 37.Wang F, Shen X, Liu Y, et al. Continuous infusion of butorphanol combined with intravenous morphine patient-controlled analgesia after total abdominal hysterectomy: a randomized, double-blind controlled trial. Eur J Anaesthesiol. 2009;26:28–34. doi: 10.1097/EJA.0b013e32831a6aa2 [DOI] [PubMed] [Google Scholar]
- 38.White I, Ghinea R, Avital S, et al. Morphine at “sub-analgesic” background infusion rate plus low-dose PCA bolus control pain better and is as safe as twice a bolus-only PCA regimen: a randomized, double blind study. Pharmacol Res. 2012;66:185–191. doi: 10.1016/j.phrs.2012.03.016 [DOI] [PubMed] [Google Scholar]
- 42.Dette F, Cassel W, Urban F, et al. Occurrence of rapid eye movement sleep deprivation after surgery under regional anesthesia. Anesth Analg. 2013;116:939–943. doi: 10.1213/ANE.0b013e3182860e58 [DOI] [PubMed] [Google Scholar]
- 43.Kjolhede P, Langstrom P, Nilsson P, et al. The impact of quality of sleep on recovery from fast-track abdominal hysterectomy. J Clin Sleep Med. 2012;8:395–402. doi: 10.5664/jcsm.2032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fernandes NM, Nield LE, Popel N, et al. Symptoms of disturbed sleep predict major adverse cardiac events after percutaneous coronary intervention. Can J Cardiol. 2014;30:118–124. doi: 10.1016/j.cjca.2013.07.009 [DOI] [PubMed] [Google Scholar]
- 49.Raymond I, Ancoli-Israel S, Choiniere M. Sleep disturbances, pain and analgesia in adults hospitalized for burn injuries. Sleep Med. 2004;5:551–559. doi: 10.1016/j.sleep.2004.07.007 [DOI] [PubMed] [Google Scholar]
- 50.Raymond I, Nielsen TA, Lavigne G, et al. Quality of sleep and its daily relationship to pain intensity in hospitalized adult burn patients. Pain. 2001;92:381–388. [DOI] [PubMed] [Google Scholar]