Abstract
Background
Sub-Saharan Africa bears a disproportionate burden of mortality from trauma. District hospitals, although not trauma centres, play a critical role in the trauma care system by serving as frontline hospitals. However, the clinical characteristics of patients receiving trauma care in African district hospitals remains under-described and is a barrier to trauma care system development. We aim to describe the burden of trauma at district hospitals by analysing trauma patients at a prototypical district hospital emergency centre.
Methods
An observational study was conducted in August, 2014 at Wesfleur Hospital, a district facility in the Western Cape Province of South Africa. Data were manually collected from a paper registry for all patients visiting the emergency centre. Patients with trauma were selected for further analysis.
Results
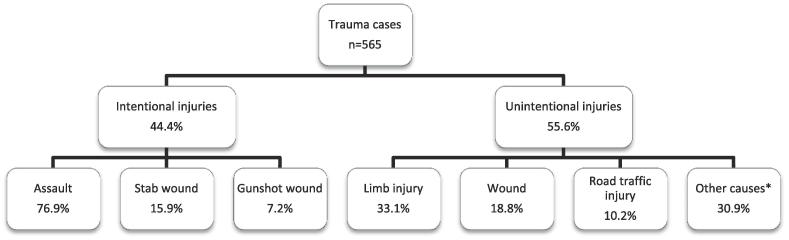
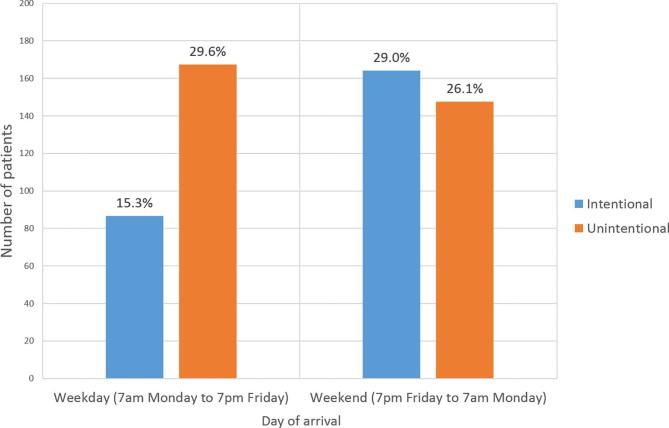
Of 3299 total cases, 565 (17.1%) presented with trauma, of which 348 (61.6%) were male. Of the trauma patients, 256 (47.6%) were ages 18–34 and 298 (52.7%) presented on the weekend. Intentional injuries (assault, stab wounds, and gunshot wounds) represented 251 (44.4%) cases of trauma. There were 314 (55.6%) cases of injuries that were unintentional, including road traffic injuries. There were 144 (60%) intentionally injured patients that arrived overnight (7pm–7am). Patients with intentional injuries were three times more likely to be transferred (to higher levels of care) or admitted than patients with unintentional injuries.
Conclusion
This district hospital emergency centre, with a small complement of non-EM trained physicians and no trauma surgical services, cared for a high volume of trauma with over half presenting on weekends and overnight when personnel are limited. The high volume and rate of admission/ transfer of intentional injuries suggests the need for improving prehospital trauma triage and trauma referrals. The results suggest strengthening trauma care systems at and around this resource-limited district hospital in South Africa may help alleviate the high burden of post-trauma morbidity and mortality.
Keywords: Emergency medical services, Non-accidental injury, Emergency medicine, Trauma system, Unintentional injury
African relevance
-
•
The study provides data regarding patterns of trauma in a typical African setting.
-
•
There is a high burden of intentional injuries at district hospitals in this setting.
-
•
The study suggests opportunities for trauma care system improvement.
-
•
The study suggests the need for improved prehospital trauma triage in this setting.
Introduction
According to the 2015 Global Burden of Disease study, approximately 4.7 million people die each year as a result of trauma, accounting for 8.5% of global deaths [1]. Trauma accounts for 1.7 times the cumulative mortality from malaria, tuberculosis, and HIV/AIDS [2]. In addition, an estimated 973 million people suffer from injuries that warrant urgent or emergent medical attention every year [1]. Significant contributors to the high rate of morbidity and mortality, particularly in low- and middle-income countries (LMICs), are interpersonal violence and road traffic injuries [1], [2]. LMICs account for approximately 90% of all global cases of trauma-related mortality [3]. South Africa, a middle-income country, has a “quadruple burden of disease” consisting of maternal and child health; non-communicable diseases; HIV/AIDS; and violence, injuries, and trauma [4]. In South Africa, major contributors to the burden of trauma include road traffic injuries and interpersonal violence [5], [6]. Further, the South African trauma-related mortality rate is six times the global rate and the road traffic injury rate is double the global average [6].
The aetiology of trauma can be sub-classified on the basis of intentionality, as is done in the Global Burden of Disease Study [1], [7], [8]. Intentional injuries include interpersonal violence, self-inflicted injury, and collective violence [1], [8]. Unintentional injuries include motor vehicle collisions, falls, burn injuries, and drowning [1], [8]. Numerous studies on trauma in sub-Saharan Africa, and specifically South Africa, utilize this convention to organize and describe epidemiological data [9], [10], [11]. South Africa is one of the only countries in the world that has a higher rate of intentional than unintentional injury [6].
Government hospitals in South Africa are classified as district (level 1), regional (level 2), and tertiary hospitals (level 3) [12]. While some larger district hospitals in urban areas have emergency medicine specialists, rural district hospitals are run by Family Physicians, and offer a 24-hour emergency centre (EC), general outpatient clinics, non-specialized inpatient wards, and basic diagnostic and therapeutic services [12]. Rural district hospitals lack trauma surgical services and other medical specialty services [12]. This is consistent with district hospitals in other countries across sub-Saharan Africa [13], [14]. District hospital ECs are frontline facilities – they serve as the entry point into the healthcare system for a significant portion of the South African population, especially since regional and tertiary hospitals are often located far away [15].
A portion of patients that present to district hospitals in South Africa are referred to secondary or tertiary hospitals in order to receive necessary specialist care, surgery, intensive care, or special tests not available at the referring facility [16]. The Western Cape Government Emergency Medical Services (EMS) system is staffed by basic through advanced Life Support practitioners [16]. The direct trauma transfer policy issued by the Western Cape Government provides specific criteria for inter-facility patient transfers from district hospitals to higher levels of care, including criteria in which EMS practitioners may bypass district hospitals and go directly to a trauma centre [17]. The trauma referral criterion in place also specifies situations in which “stop and intervene” measures must be performed at the nearest hospital prior to inter-facility transfer [17].
Across much of sub-Saharan Africa, patients with emergency medical and traumatic conditions are often limited in their ability to directly access higher level hospitals, partly due to patient transportation barriers, limited prehospital emergency medical services, and ineffective referral practices [18], [19], [20]. Patient transportation barriers are a problem due to limited access to rapid transport, potentially high transportation costs, and large distances to the nearest healthcare facility [21]. Referral practices in some areas are challenged by inefficient referral practices, fragmented systems for referrals, and limited communication infrastructure [22]. A combination of patient and health system factors contribute to an undue burden of trauma at district level hospitals across sub-Saharan Africa [23].
Elucidating the epidemiology of acute conditions, including trauma, was deemed a research priority by the World Health Organization (WHO) and the African Federation for Emergency Medicine [24]. While several studies have researched the epidemiology of trauma presenting to EC at South African tertiary hospitals, limited data are available regarding trauma care at frontline district level hospitals [9], [10], [25], [26], [27]. The paucity of data in South Africa and sub-Saharan Africa hampers advocacy, strategic development, and resource allocation for delivery of effective trauma care at the district level. The overarching aim of this study is to describe the burden of trauma at a South African district hospital.
Methods
This study was a subset of a larger prospective observational study exploring the South African Emergency First Aid Responder (EFAR) program, a volunteer, layperson prehospital emergency care system [28], [29], [30]. The objective of the overarching study was to assess whether the novel EFAR program was an effective component of the local emergency care system and contributed to improved outcomes in Atlantis, Western Cape Province, South Africa [31]. Data for the larger study were prospectively collected over the course of approximately six consecutive months from EFAR patient care forms, METRO EMS patient care report forms, and local hospital EC charts. The data collected from the Wesfleur Hospital EC in Atlantis, South Africa were used in this smaller observational study.
This 31-bed district level hospital located in the Western Cape Province serves a low-income, peri-urban population of approximately 250 000 [32]. Wesfleur Hospital is approximately 50 km from the nearest tertiary care or trauma centre, Groote Schuur Hospital. The government ambulance system (Western Cape Government Health, Emergency Medical Services – EMS) provides the local prehospital care and inter-hospital emergency transport. Wesfleur Hospital has a 24-hour EC staffed by nurses and a small complement of non-EM trained physicians. The EC has an estimated annual volume of 36 000 cases, of which at least 10% or 3 600 arrive by EMS. The EC uses nurse-driven triage (the South African Triage Scale [SATS]), and – at the time of the study – had 4 beds and several chair stretchers. SATS is a validated measure of clinical urgency, and emergency care resources required, based on physiologic parameters and clinical discriminators which prioritizes patients into one of four colours ranging from green (low acuity) to red (emergent) [33]. During the study period in 2014, for the day shift (7am to 7pm) there were usually two non-specialist emergency doctors and a small complement of non-emergency trained nurses. During the night shift (7pm to 7am), there was often one physician and a smaller group of non-emergency trained nurses. Trauma care capabilities in the EC include endotracheal intubation and ventilation, central line access, blood transfusion, and basic fracture management. During the study period, the hospital had inpatient services but lacked trauma surgical services.
The larger EFAR study was conducted between August 1, 2014 and February 10, 2015. This smaller observational study used data collected at Wesfleur Hospital between August 1 and August 31, 2014. EC nurses recorded data on every patient that presented to the Wesfleur Hospital EC in a handwritten registry. The EC registry included data on patients’ medical record number, date and time of arrival, age, sex, chief complaint, SATS acuity, and disposition. EC triage nurses collected data 24 h per day, 7 days per week. Due to pre-existing ethics and institutional approvals, only logbook data for the month of August, 2014 were made available for use in our study. As part of the EFAR study, patients presenting by EMS were matched to the registry book using the daily EMS transport record in order to calculate the admission and transfer rate of EMS transported patients. Data, excluding personal identifiers were manually entered into a Microsoft Excel spreadsheet Version 14.0.7188 (Microsoft Corporation, Redmond, Washington, USA). Each patient encounter was assigned a unique study number.
Patients of all ages in our Wesfleur Hospital database with trauma (penetrating, blunt, burns, and drowning) were selected for further analysis. Other non-forceful injury mechanisms (e.g. poisoning, envenomation, and drug overdoses) were excluded. Patients that left the EC without completing triage were excluded from the study.
To discover patients with trauma within the entire Wesfleur Hospital EC population of patients, a previously described classification system was used to organize chief complaints into primary categories of “medical”, “injury”, “OBGYN”, “psychiatric”, and “miscellaneous” [34]. Each chief complaint was then further normalized into a standardized (secondary) list of chief complaints. Data were descriptively analysed and odds ratios for patients requiring admission or transfer were calculated. Ethical approval for this study was obtained in South Africa (University of Cape Town HREC ref: 636/2014) and from the USA (Colorado Multiple Institutional Review Board protocol #14-0051).
Of the 3 299 total cases, 1 589 (48.2%) were male, and the mean age 33.1 years (range: 0–89.3). The most frequent SATS colour for all patients was yellow (1 417 cases, 43.0%), and the most frequent SATS colour for trauma patients was also yellow (368 cases, 65.1%) (Table 1). 2 389 (72.4%) patients were discharged, 249 (7.5%) patients were admitted/transferred to higher level of care or died, and 278 (8.4%) patients had missing disposition data (Table 1).
Table 1.
Frequency table of study population.
| Population Characteristics | |||
|---|---|---|---|
| % of all patients (N = 3299) | % of Trauma Patients (N = 565) | ||
| Sex | Male | 48.2 | 61.6 |
| Female | 51.0 | 37.3 | |
| Missing Data | 0.8 | 1.1 | |
| Age | <18 | 23.5 | 22.5 |
| 18–34 | 31.5 | 46.7 | |
| 35–59 | 32.0 | 24.4 | |
| >60 | 11.1 | 4.6 | |
| Missing Data | 1.9 | 1.8 | |
| SATS Score | Green | 16.5 | 13.3 |
| Yellow | 43.0 | 65.1 | |
| Orange | 20.3 | 11.3 | |
| Red | 0.5 | 1.1 | |
| Blue | 0.3 | 0.0 | |
| Missing Data | 19.4 | 9.2 | |
| Disposition | Discharged | 72.4 | 80.9 |
| Admitted | 5.1 | 2.7 | |
| Transferred | 1.9 | 3.5 | |
| Abscond | 11.6 | 6.0 | |
| Death | 0.5 | 0.0 | |
| Missing Data | 8.5 | 6.9 | |
Of the 565 (17.1% of total cases) trauma cases, 348 (61.6%) were male. Trauma patients had a mean age of 28.5 years (range: 0.4–87.8), with 256 (46.7%) between 18–34 years of age (Table 2). 63% of assaults, 72% of gunshot wounds, 66% of stab wounds, and 65% of motor vehicle collisions were patients between 18–34 years old. Trauma accounted for 19.1% of total EC cases after omitting the 347 cases with missing chief complaints.
Table 2.
Frequency of sex, age, South African Triage Scale scores and outcomes in intentional and unintentional trauma cases.
| Intentional |
Unintentional |
Chi Square Test | ||||
|---|---|---|---|---|---|---|
| Cases | Percentage | Cases | Percentage | |||
| Sex | Male | 154 | 61.4 | 194 | 61.8 | 4.5977 (p = 0.03) |
| Female | 93 | 37.1 | 118 | 37.6 | 2.962 (p = 0.09) | |
| Missing | 4 | 1.6 | 2 | 0.6 | 0.667 (p = 0.41) | |
| Age | <18 | 26 | 10.4 | 101 | 32.2 | 44.291 (p < 0.001) |
| 18–34 | 152 | 60.6 | 104 | 33.1 | 9.000 (p < 0.01) | |
| 35–59 | 67 | 26.7 | 80 | 25.5 | 1.150 (p = 0.28) | |
| >60 | 2 | 0.8 | 23 | 7.3 | 17.640 (p < 0.001) | |
| Missing | 4 | 1.6 | 6 | 1.9 | 0.400 (p = 0.53) | |
| South African Triage Scale Score | Red | 5 | 2.0 | 1 | 0.3 | 2.667 (p = 0.10) |
| Orange | 27 | 10.8 | 37 | 11.8 | 1.563 (p = 0.21) | |
| Yellow | 156 | 62.2 | 212 | 67.5 | 8.522 (p < 0.01) | |
| Green | 43 | 17.1 | 32 | 10.2 | 1.613 (p = 0.20) | |
| Missing | 20 | 8.0 | 32 | 10.2 | 2.769 (p = 0.10) | |
| Disposition | Admitted | 13 | 5.2 | 2 | 0.6 | 8.067 (p < 0.01) |
| Transferred | 12 | 4.8 | 8 | 2.5 | 0.800 (p = 0.37) | |
| Discharged | 194 | 77.3 | 263 | 83.8 | 10.418 (p = 0.001) | |
| Abscond | 19 | 7.6 | 15 | 4.8 | 0.471 (p = 0.49) | |
| Missing | 13 | 5.2 | 26 | 8.3 | 4.333 (p = 0.04) | |
| Total | 251 | 44.4 | 314 | 55.6 | 7.025 (p = 0.01) | |
Trauma cases were divided into two groups based on intentionality (Fig. 1). Intentional injuries (i.e. blunt assault, stab wounds, and gunshot wounds) accounted for 251 (44.4%), while unintentional injuries (e.g. road traffic injuries) accounted for 314 (55.6%) of the trauma cases (Fig. 1). Subgroup analysis by individual mechanisms of injury is not presented here due to the relatively small sample sizes of gunshot wounds and stab wounds in our study population. A temporal breakdown of injury visits (by time of day, and day of week) is demonstrated in Fig. 2, in which 298 (52.7%) patients presented on the weekend. In addition, 144 (60%) of intentionally injured patients arrived overnight (7pm-7am) while 191 (63%) of unintentionally injured patients arrived during the day (7am-7pm).
Fig. 1.
Flowchart of study data analysis. Intentional and unintentional injury cases were selected for further analysis from the total trauma population of 565.
Fig. 2.
Trauma cases by time of day and day of week.
Patients with intentional injuries were triaged as SATS green or yellow in 199 (38.8% of total) cases, and high acuity (SATS score of orange or red) in 32 (6.2%) cases. Patients with unintentional injuries were triaged as green or yellow in 244 (47.6%) cases, and high acuity in 38 (7.4%) cases (Table 2).
After omitting cases with missing dispositions, patients were transferred to higher levels of care or admitted in 7.1% of trauma cases. Overall, patients with intentional injuries were 3.2 times more likely to be transferred to higher levels of care or admitted than those with unintentional injuries (OR 3.2; 95% CI 1.5–7.0). Higher acuity trauma patients were 9.05 times more likely (OR 9.05; 95% CI 4.2–19.5) to be admitted or transferred than those with lower acuity (Table 2). Patients that arrived via EMS were 2.68 times more likely to be admitted or transferred than patients that presented directly to the EC (OR 2.68; 95% CI 1.04–6.920).
Discussion
Between 1990 and 2013, injury disability adjusted life years (DALY) globally declined by 30.9%. However, Africa is one of the few exceptions to this significant reduction; southern Africa experienced up to a 10% increase in DALY, for both intentional and unintentional injuries [1]. While the global DALY rate for interpersonal violence decreased by 19.1%, there was up to a 50% rise in southern Africa [1]. When rapid urbanization and growth in motorization outpace infrastructural development and levels of law enforcement, the trauma burden grows [6], [35]. District hospitals, like Wesfleur, serve as the entry point to the healthcare system and play an increasingly critical role in the care of trauma.
This South African district hospital EC, with a small complement of non-EM trained physicians and no trauma surgical services, cared for a relatively high absolute number of trauma (565 total) cases in one month. By comparison, several tertiary centres serving much larger urban areas in Malawi, Botswana, Kenya, Rwanda, and Zambia are reported to care for smaller monthly number of trauma cases [9], [36], [37], [38], [39], [40]. Wesfleur Hospital was the only major health facility serving a population of about one-quarter million people, which may explain the relatively high absolute monthly case load of trauma. If the proportion of trauma cases is considered, Wesfleur Hospital’s proportion of trauma (19.1%) was relatively consistent with prior studies conducted at other sub-Saharan Africa district hospitals [23], [43], [44], [45], [46]. The high trauma caseload at Wesfleur Hospital, similar to other African settings, reinforces the need to strengthen capacity of the local trauma care system, especially given the severity of injuries at Wesfleur. Potential solutions may include task-shifting to improve trauma provider staffing, improved EC capacity and services, and general strengthening of the regional trauma care system [41], [42].
Our data found that a higher proportion of young males presented with trauma than any other demographic, particularly from interpersonal violence (62% male, 48% of trauma occurred in those aged 18 – 34, 44.4% of trauma cases were intentional injuries). These findings are consistent with prior studies in the region [2], [47], [48]. A study at Groote Schuur Hospital, a tertiary centre 50-km away in Cape Town, found that males were 2.2 times more likely to present with violent trauma than females [9]. A study in Lusaka, Zambia found that trauma patients had a median age of 24 and 71.8% were male [40]. A study utilizing a hospital based surveillance system in the KwaZulu-Natal province of South Africa found that interpersonal violence accounted for 45% of total trauma cases, which was identical to the rate at Wesfleur Hospital [48]. Ours and others’ data demonstrate that economically productive members of African societies have a high rate of trauma, potentially resulting in lost income. Additional economic cost also comes in the form of healthcare expenses and wages lost due to post-injury long-term morbidity.
Over half of the trauma patients presented on the weekend. A majority of intentional injuries presented during the nights, while a majority of unintentional injuries presented during the day. Not only is this district-level hospital providing care for a high volume of trauma cases, but the most severely injured and high-risk trauma patients are presenting at times when personnel are most scarce. These findings are consistent with prior studies in the region [9], [10], [46], [49]. Increased attention to staffing and resource needs during times of high patient volume or acuity is essential to addressing the needs of any EC population. At times of low staffing, increased utilization of telemedicine communication with a trauma expert may help improve trauma care outcomes.
Our data found that patients with intentional injuries were about three times more likely to be admitted or transferred to higher levels of care than patients with unintentional injuries. The high rate of admissions and transfers amongst trauma patients at Wesfleur Hospital (7.1%) was found to be either consistent with, or slightly lower than, prior studies at other sub-Saharan African district hospitals [44], [45], [50]. In addition, higher acuity trauma patients were about nine times more likely to be admitted or transferred. Patients that arrived at the Wesfleur EC via EMS were more than twice as likely to be admitted or transferred as patients that did not arrive by EMS. This finding is consistent with others, including a study from the Ashanti Region of Ghana [18]. Although our study sample contained a small number of cases resulting in death, the high admission and transfer rate suggests a large amount of morbidity and health system resource utilization resulting from trauma.
The high rate of admission or transfer amongst EMS-transported patients may indicate a need to enforce the Western Cape Government’s EMS direct trauma transfer criteria (which allows adult major trauma to safely bypass lower levels of care) [17]. The transfer criteria also specifies situations in which “stop and intervene” measures (i.e. intubation, placement of chest tube, etc.) must be performed at the nearest hospital [17]. According to the policy, for example, patients with severe head injuries, polytrauma, or those in shock from a penetrating chest injury may be transferred directly to a trauma facility with trauma surgical capabilities or relevant diagnostic equipment, like a CT scanner [17]. A study in the Western Cape Province that analysed patient transfers from district to tertiary hospitals found that trauma accounted for 46% of referrals, of which head injuries accounted for 58% [16]. Further data collection is necessary to determine if the criteria are being appropriately applied to head injury and patients in traumatic shock. Additionally, improved capacity to execute ambulance transfers for rapid inter-facility transfers could be useful, especially for severe trauma patients who self-present to Wesfleur Hospital.
The high rate of admission and transfer at Wesfleur Hospital suggests a possible lack of adherence to the direct trauma transfer criteria by Western Cape Province EMS providers. Studies at Level 2 and 3 Trauma Centres in high income countries have shown that tiered trauma systems provide earlier access to the appropriate level of care for moderate and minor trauma at local facilities [51]. Studies have demonstrated that tiered trauma systems, equipped with suitable prehospital emergency care and effective triage, decrease mortality by taking severely injured patients directly to the most appropriate initial level of care [52], [53], [54], [55], [56], [57]. A study in the KwaZulu-Natal Province of South Africa analysing trauma referrals to a tertiary hospital found that the direct trauma transfer policy that allowed bypassing of lower levels of care was underutilized, in which 88% of accepted referrals were admitted as inter-hospital transfers [58]. The results suggest the need to further educate regional EMS providers to correctly identify major trauma patients, especially if they do not require immediate intubation, ventilation, or urgent surgery, and refer these patients directly to a tertiary hospital [58]. The large volume of high acuity and intentional trauma cases at Wesfleur Hospital that are admitted or transferred to higher levels of care similarly suggests the need to reinforce the trauma transfer criteria in the Western Cape Province. This expanded education of providers and reinforcement of established criteria has been previously achieved in other trauma systems in LMICs [59], [60]. Further research is needed to analyse adherence of EMS providers to the direct trauma transfer criteria.
The high volume of trauma cases, particularly among young males, is similar to other African data and concerning. Public health experts suggest rates of interpersonal violence in South Africa, and much of sub-Saharan Africa, may be reduced by increasing employment, reducing income inequality, limiting access to weapons, and reducing alcohol and drug abuse [61]. A prior study at a Cape Town hospital found that approximately 47% of trauma patients were under the influence of alcohol, of which 87% had some form of interpersonal violence ensuing [46]. The 2010 Global Burden of Disease study found that alcohol was the leading risk factor for trauma in South Africa. Development of educational programs targeting young males that advocate against alcohol abuse and challenge socio-cultural practices that promote violent behaviours may help reduce this burden of trauma [9].
This study has several limitations. Patient data were manually entered into a handwritten logbook by triage nurses, resulting in 40 undecipherable cases (1.2% of total cases) due to illegible handwriting. In addition, data fields were occasionally left incomplete by triage nurses, resulting in missing data. We believe the effect of this missing data to be minimal, particularly since the results were consistent with the results of similar prior studies [9], [36], [37], [38], [39], [40], [48]. Additionally, EC data were collected during the month of August 2014, possibly resulting in missed seasonal variations in trauma. Furthermore, it is difficult to extrapolate findings from one month of data from one health facility, suggesting the need for further larger trauma epidemiologic and outcomes research. Additionally, the handwritten registry of chief complaints did not specify the anatomic locations of gunshot wounds and stab wounds, which would likely have impacted the acuity and disposition of these trauma patients. Lastly, there were limited data recorded on the resources consumed during trauma care - these data could be used to better prepare similar district hospitals for trauma care.
Conclusion
This observational study conducted at a single district hospital provides insightful data regarding patterns of trauma in a district hospital in a southern African setting. The high burden of intentional injuries at district hospitals, particularly amongst young males that frequently present during times when personnel are scarce, suggests specific opportunities for trauma care system improvement and public health prevention in this region. In addition, the high rate of admission and transfer for intentional injuries, and higher acuity trauma, suggest the need for improved prehospital trauma destination selection. Further data collection is still needed at district level hospital ECs across sub-Saharan Africa to strengthen the evidence for improved trauma care at these critical frontline facilities.
Acknowledgments
Acknowledgements
We would like to thank the medical records and EC staff at Wesfleur Hospital, including Dr. Godwana and Dr. Okwuosa, for their efforts to support this work. We also acknowledge and thank the leadership and administration of Wesfleur Hospital for their collaboration and permissions to conduct this study. We would like to also thank the Emergency Medicine Foundation and the Carnegie Corporation of New York for funding that supported this research.
Dissemination of results
This manuscript has not been published elsewhere and is not under consideration by any other publication. The abstract of this paper was presented at the American College of Emergency Physicians Scientific Assembly in Las Vegas, NV, USA on October 17, 2016.
Author Contribution
Authors contributed as follow to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published: AZ 35%; NM 30%; JD 11%; and KL, SDV, LAW, and AG 6% each. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of Interest
Prof Lee Wallis is an editor of the African Journal of Emergency Medicine. Prof Wallis was not involved in the editorial workflow for this manuscript. The African Journal of Emergency Medicine applies a double blinded process for all manuscript peer reviews. The authors declared no further conflict of interest.
Funding Sources
The Emergency Medicine Foundation awarded us the International Outcomes and Efficacy Research Grant (PI: Corresponding Author, 2014). Funding was also awarded by the Carnegie Corporation of New York to Corresponding Author via the African Diaspora Program Fellowship to support this research (2014-2015). There was no involvement of the study sponsors in the study design; collection, analysis and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2019.01.007.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Haagsma J.A., Graetz N., Bolliger I. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22(1):3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO; Geneva: 2014. Injuries and violence: the facts 2014. http://apps.who.int/iris/bitstream/10665/149798/1/9789241508018_eng.pdf (Accessed 1 May, 2017) [Google Scholar]
- 3.Krug E.G., Sharma G.K., Lozano R. The global burden of injuries. Am J Public Health. 2000;90(4):523–526. doi: 10.2105/ajph.90.4.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coovadia H., Jewkes R., Barron P., Sanders D., McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374(9692):817–834. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- 5.Prinsloo M., Kotzenberg C., Seedat M. Medical Research Council/UNISA Crime, Violence and Injury Lead Programme; Cape Town: 2007. A profile of fatal injuries in South Africa: 7th annual report of the national injury mortality surveillance system 2005. [Google Scholar]
- 6.Norman R., Matzopoulos R., Groenewald P., Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ. 2007;85(9):695–702. doi: 10.2471/BLT.06.037184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray C.J., Lopez A.D. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349(9061):1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 8.Thind A, Hsia R, Mabweijano J, Hicks ER, Zakariah A, Mock CN. Prehospital and emergency care. Disease control priorities, (Volume 1): Essential surgery. 2015:245. [DOI] [PubMed]
- 9.Schuurman N., Cinnamon J., Walker B.B., Fawcett V., Nicol A., Hameed S.M. Intentional injury and violence in Cape Town, South Africa: an epidemiological analysis of trauma admissions data. Glob Health Action. 2015;8(1):27016. doi: 10.3402/gha.v8.27016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pillay K.K., Ross A., Van der Linde S. Trauma unit workload at King Edward VIII Hospital, Durban. KwaZulu-Natal. S Afr Med J. 2012;102(5):307–308. doi: 10.7196/samj.5440. [DOI] [PubMed] [Google Scholar]
- 11.Kobusingye O., Guwatudde D., Lett R. Injury patterns in rural and urban Uganda. Inj Prev. 2001;7(1):46–50. doi: 10.1136/ip.7.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cullinan K. Health services in South Africa: a basic introduction. Health-e News Service. 2006 [Google Scholar]
- 13.English M., Lanata C., Ngugi I., Smith P.C. The district hospital. Disease Control Priorities in Developing Countries. 2006;2:1211–1228. [Google Scholar]
- 14.Gorgen H., Kirsch-Woik T., Schmidt-Ehry B. The District Health System Experiences and Prospects in Africa: manual for public health practitioners. Deutsche Gesellschaft fur. 2004 [Google Scholar]
- 15.District/Provincially Aided Hospitals. Western Cape Government Web site. https://www.westerncape.gov.za/directories/facilities/914 (Accessed May 1, 2017).
- 16.Slabbert J., Smith W. Patient transport from rural to tertiary healthcare centres in the Western Cape: is there room for improvement? Afr J Emerg Med. 2011;1(1):11–16. [Google Scholar]
- 17.Engelbrecht B. Direct transfer of adult major trauma and severe head injury patients. Western Cape Government. Circular H186 of 2013.
- 18.Mould-Millman C.N.-K., Rominski S., Oteng R. Ambulance or taxi? High acuity prehospital transports in the Ashanti region of Ghana. Afr J Emerg Med. 2014;4(1):8–13. [Google Scholar]
- 19.Mould-Millman N.-K., Rominski S.D., Bogus J., Ginde A.A., Zakariah A.N., Boatemaah C.A. Barriers to accessing emergency medical services in Accra, Ghana: development of a survey instrument and initial application in Ghana. Global Health: Sci Practice. 2015;3(4):577–590. doi: 10.9745/GHSP-D-15-00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mould-Millman N.-K., Dixon J.M., Sefa N., Yancey A., Hollong B.G., Hagahmed M. The state of emergency medical services (EMS) systems in Africa. Prehospital Disaster Med. 2017:1–11. doi: 10.1017/S1049023X17000061. [DOI] [PubMed] [Google Scholar]
- 21.Thaddeus S., Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091–1110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 22.Kobusingye O.C., Hyder A.A., Bishai D., Hicks E.R., Mock C., Joshipura M. Emergency medical systems in low-and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83(8):626–631. [PMC free article] [PubMed] [Google Scholar]
- 23.Hunter L., Lahri S., van Hoving D. Case mix of patients managed in the resuscitation area of a district-level public hospital in Cape Town. Afr J Emerg Med. 2017;7(1):19–23. doi: 10.1016/j.afjem.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds T.A., Calvello E.J., Broccoli M.C., Sawe H.R., Mould-Millman N.-K., Teklu S. AFEM consensus conference 2013 summary: emergency care in Africa-Where are we now? Afr J Emerg Med. 2014;4(3):158–163. [Google Scholar]
- 25.Lewis C., Wood D. Interpersonal violence as a major contributor towards the skewed burden of trauma in KwaZulu-Natal, South Africa. S Afr Med J. 2015;105(10):827–830. doi: 10.7196/SAMJnew.8380. [DOI] [PubMed] [Google Scholar]
- 26.Van Wyk P.S., Jenkins L. The after-hours case mix of patients attending the George Provincial Hospital Emergency Centre. South African Family Practice. 2014;56(4):240–245. [Google Scholar]
- 27.Hodkinson P.W., Wallis L.A. Cross-sectional survey of patients presenting to a South African urban emergency centre. Emerg Med J. 2009;26(9):635–640. doi: 10.1136/emj.2008.063362. [DOI] [PubMed] [Google Scholar]
- 28.Sun J.H., Shing R., Twomey M., Wallis L.A. A strategy to implement and support pre-hospital emergency medical systems in developing, resource-constrained areas of South Africa. Injury. 2014;45(1):31–38. doi: 10.1016/j.injury.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 29.Sun J.H., Wallis L.A. The emergency first aid responder system model: using community members to assist life-threatening emergencies in violent, developing areas of need. Emerg Med J. 2012;29(8):673–678. doi: 10.1136/emermed-2011-200271. [DOI] [PubMed] [Google Scholar]
- 30.Sun J.H., Wallis L.A. Learning and retention of emergency first aid skills in a violent, developing South African township. Emerg Med J. 2012 doi: 10.1136/emermed-2011-200429. emermed-2011-200429. http://dx.doi.org/10.1136/emermed-2011-200429. [DOI] [PubMed] [Google Scholar]
- 31.Mould-Millman N.-K., Dixon J., Holmes J., Crockett D., LeBeau S., De Vries S. 216 EMF Emergency Scene Responses by African Community-Based Emergency First Aid Responders. Ann Emerg Med. 2015;66(4):S80. [Google Scholar]
- 32.Wesfleur Hospital (Atlantis). SAME Foundation Web site. http://www.samefoundation.org.za/wesfleur-hospital-atlantis (Accessed 1 May, 2017).
- 33.Twomey M., Wallis L.A., Thompson M.L., Myers J.E. The South African triage scale (adult version) provides valid acuity ratings when used by doctors and enrolled nursing assistants. Afr J Emerg Med. 2012;2(1):3–12. doi: 10.1016/j.ienj.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 34.Mould-millman N.-k., Raji Z., Rodriguez K., Zaidi A., Dixon J., Patel H. Prehospital care in South Africa: characterizing complaints and response type by Western Cape Ems. Acad Emerg Med. 2016;23:S98. [Google Scholar]
- 35.World Health Organization . WHO; Geneva: 2013. Global status report on road safety 2013. http://www.who.int/iris/bitstream/10665/78256/1/9789241564564_eng.pdf (Accessed 1 May, 2017) [Google Scholar]
- 36.Samuel J.C., Akinkuotu A., Villaveces A., Charles A.G., Lee C.N., Hoffman I.F. Epidemiology of injuries at a tertiary care centre in Malawi. World J Surg. 2009;33(9):1836–1841. doi: 10.1007/s00268-009-0113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chandra A., Mullan P., Ho-Foster A., Langeveldt A., Caruso N., Motsumi J. Epidemiology of patients presenting to the emergency centre of Princess Marina Hospital in Gaborone, Botswana. Afr J Emerg Med. 2014;4(3):109–114. [Google Scholar]
- 38.House D.R., Nyabera S.L., Yusi K., Rusyniak D.E. Descriptive study of an emergency centre in Western Kenya: challenges and opportunities. Afr J Emerg Med. 2014;4(1):19–24. [Google Scholar]
- 39.Mbanjumucyo G., George N., Kearney A., Karim N., Aluisio A.R., Mutabazi Z. Epidemiology of injuries and outcomes among trauma patients receiving prehospital care at a tertiary teaching hospital in Kigali, Rwanda. Afr J Emerg Med. 2016;6(4):191–197. doi: 10.1016/j.afjem.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seidenberg P., Cerwensky K., Brown R.O., Hammond E., Mofu Y., Lungu J. Epidemiology of injuries, outcomes, and hospital resource utilisation at a tertiary teaching hospital in Lusaka, Zambia. Afr J Emerg Med. 2014;4(3):115–122. [Google Scholar]
- 41.Mock C.N., Jurkovich G.J., Arreola-Risa C., Maier R.V. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma Acute Care Surgery. 1998;44(5):804–814. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 42.Gove S., Tamburlini G., Molyneux E., Whitesell P., Campbell H. Development and technical basis of simplified guidelines for emergency triage assessment and treatment in developing countries. Arch Dis Child. 1999;81(6):473–477. doi: 10.1136/adc.81.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Periyanayagam U., Dreifuss B., Hammerstedt H., Chamberlain S., Nelson S., Bosco K.J. Acute care needs in a rural Sub-Saharan African Emergency Centre: a retrospective analysis. Afr J Emerg Med. 2012;2(4):151–158. [Google Scholar]
- 44.Wallis L.A., Twomey M. Workload and casemix in Cape Town emergency departments. S Afr Med J. 2007;97(12):1276–1280. [PubMed] [Google Scholar]
- 45.Marsala J.M., Faye F., BeLue R., Schoeck O. Characterising emergency centre encounters in Mbour, Senegal as emergent-emergency care, emergent-primary care or non-emergent. Afr J Emerg Med. 2017;7(3):124–129. doi: 10.1016/j.afjem.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Govender I., Matzopoulos R., Makanga P., Corrigall J. Piloting a trauma surveillance tool for primary healthcare emergency centres. S Afr Med J. 2012;102(5):303–306. doi: 10.7196/samj.5293. [DOI] [PubMed] [Google Scholar]
- 47.Feigin V. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. https://doi.org/.10.1016/S0140-6736(16)31012-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lutge E., Moodley N., Tefera A., Sartorius B., Hardcastle T., Clarke D. A hospital based surveillance system to assess the burden of trauma in KwaZulu-Natal Province South Africa. Injury. 2016;47(1):135–140. doi: 10.1016/j.injury.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 49.Gallaher J.R., Molyneux E., Charles A.G. Sub-Saharan African hospitals have a unique opportunity to address intentional injury to children. Afr J Emerg Med. 2016;6(2):59–60. doi: 10.1016/j.afjem.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chokotho L., Mulwafu W., Jacobsen K.H., Pandit H., Lavy C. The burden of trauma in four rural district hospitals in Malawi: a retrospective review of medical records. Injury. 2014;45(12):2065–2070. doi: 10.1016/j.injury.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 51.Utter G.H., Maier R.V., Rivara F.P., Mock C.N., Jurkovich G.J., Nathens A.B. Inclusive trauma systems: do they improve triage or outcomes of the severely injured? J Trauma Acute Care Surgery. 2006;60(3):529–537. doi: 10.1097/01.ta.0000204022.36214.9e. [DOI] [PubMed] [Google Scholar]
- 52.Moore L., Hanley J.A., Turgeon A.F., Lavoie A. Evaluation of the long-term trend in mortality from injury in a mature inclusive trauma system. World J Surg. 2010;34(9):2069–2075. doi: 10.1007/s00268-010-0588-z. [DOI] [PubMed] [Google Scholar]
- 53.MacKenzie E.J., Rivara F.P., Jurkovich G.J., Nathens A.B., Frey K.P., Egleston B.L. A national evaluation of the effect of trauma-centre care on mortality. N Engl J Med. 2006;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 54.Nathens A.B., Jurkovich G.J., Rivara F.P., Maier R.V. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma Acute Care Surgery. 2000;48(1):25. doi: 10.1097/00005373-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 55.Jurkovich G.J., Mock C. Systematic review of trauma system effectiveness based on registry comparisons. J Trauma Acute Care Surgery. 1999;47(3):S46–S55. doi: 10.1097/00005373-199909001-00011. [DOI] [PubMed] [Google Scholar]
- 56.Celso B., Tepas J., Langland-Orban B., Pracht E., Papa L., Lottenberg L. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centres following the establishment of trauma systems. J Trauma Acute Care Surgery. 2006;60(2):371–378. doi: 10.1097/01.ta.0000197916.99629.eb. [DOI] [PubMed] [Google Scholar]
- 57.Mullins R.J., Mann N.C. Population-based research assessing the effectiveness of trauma systems. J Trauma Acute Care Surgery. 1999;47(3):S59–S66. doi: 10.1097/00005373-199909001-00013. [DOI] [PubMed] [Google Scholar]
- 58.Hardcastle T.C., Reeds M.G., Muckart D.J.J. Utilisation of a Level 1 Trauma Centre in KwaZulu-Natal: appropriateness of referral determines trauma patient access. World J Surg. 2013;37(7):1544–1549. doi: 10.1007/s00268-012-1890-8. [DOI] [PubMed] [Google Scholar]
- 59.Wisborg T., Murad M.K., Edvardsen O., Husum H. Prehospital trauma system in a low-income country: system maturation and adaptation during 8 years. J Trauma Acute Care Surgery. 2008;64(5):1342–1348. doi: 10.1097/TA.0b013e31812eed4e. [DOI] [PubMed] [Google Scholar]
- 60.Callese T.E., Richards C.T., Shaw P., Schuetz S.J., Paladino L., Issa N. Trauma system development in low-and middle-income countries: a review. J Surgical Res. 2015;193(1):300–307. doi: 10.1016/j.jss.2014.09.040. [DOI] [PubMed] [Google Scholar]
- 61.Matzopoulos R., Bowman B., Mathews S., Myers J. Applying upstream interventions for interpersonal violence prevention: an uphill struggle in low-to middle-income contexts. Health Policy. 2010;97(1):62–70. doi: 10.1016/j.healthpol.2010.03.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.