The discovery in 1959 that metformin (dimethylbiguanide) lowers blood glucose levels in people with type 2 diabetes (1) has been a major boon for millions with this common metabolic disorder. Metformin is currently also being studied as a therapeutic agent for managing other serious maladies, such as fatty liver disease, cardiovascular disorders, and cancer.
Given its current and potential therapeutic uses, one might think that metformin's mode of action is well understood, as it is for other important drugs, including the anticancer agent Taxol, the analgesic aspirin, and the antidepressant fluoxetine (Prozac). Quite surprisingly, however, metformin's exact molecular mechanism remains a mystery.
This is not for lack of trying. The following relates an ongoing journey to discovering how metformin works, including two seminal studies published in the Journal of Biological Chemistry, now recognized as Classics (2, 3).
In 2000, El-Mir and colleagues (2) reported that metformin inhibits respiratory complex I in the mitochondria of liver cells (hepatocytes). This finding suggested that the authors had hit the bullseye of metformin's molecular target. However, there was a wrinkle; “metformin's effects on complex I were indirect,” says Eric Fontaine, one of the researchers involved in this work and now at Université Grenoble Alpes in France.
This indirect effect decreased cellular respiration and was highly specific, solely affecting mitochondrial complex I—but only in intact hepatocytes. “If we put metformin into isolated mitochondria, we did not observe an inhibition of complex I,” says Fontaine. The reason for this finding remains unclear, but metformin's indirect effect has been reproduced by the authors of the El-Mir paper and also by other labs.
Later studies have reported that metformin directly inhibits complex I in isolated mitochondria, Fontaine says, but only in state 3 of complex I, when ATP is produced, a state that the El-Mir study did not examine. However, the metformin concentrations required to directly affect complex I activity are consistently higher than those yielding the indirect effect. This suggests that the two effects are not linked. In any case, confusion about metformin's effect(s) on complex I persists in the literature to this day and will likely be resolved only after metformin's molecular target(s) is pinpointed.
Shortly after publication of the El-Mir et al. study, another clue to metformin's cellular target came to light in a 2001 paper (4), reporting that metformin activates AMP-activated protein kinase (AMPK). Zhou et al. found that metformin-induced AMPK activation suppresses glucose production in the liver and also promotes glucose uptake into skeletal muscle. The study represented an important advance, according to David Carling, senior author of the second JBC Classics paper published in 2002 (3). However, Carling also notes that “it wasn't clear how metformin was causing AMPK to be activated, what the molecular mechanisms were,” providing an opportunity for his lab, which had a long track record of studying AMPK.
Metformin's effect on AMPK intrigued Carling because “AMPK acts as a very important, perhaps the most important energy sensor, within mammalian cells.” Having previously developed a skeletal muscle cell line called H-2Kb that provided a reliable model to study AMPK in muscle cells, Carling and his group were ideally positioned to take the next steps to look at AMPK's role in mediating metformin's effects. “The first thing was that we got really good [AMPK] activation in this cell line, so that was brilliant. We were able to confirm and reproduce that metformin really did give a very robust activation of AMPK.”
This was no small feat; metformin fails to get into cells that lack a specific transporter, organic cation transporter 1 (OCT1). This technical detail wasn't common knowledge at the time and may still bedevil research on metformin's effects in cells. What's more, the H-2Kb cells, unlike some commonly used cell lines, express high levels of an upstream kinase, liver kinase B1 (LKB1), that phosphorylates and activates AMPK. “The hindsight is that [the cells] were able to take up metformin, and they expressed the upstream kinase that is required for activation of AMPK in response to metformin,” says Carling.
With all these then unknown factors in fortuitous alignment, Carling's research team set out to test whether metformin and another antidiabetic drug, rosiglitazone, activate AMPK by increasing the AMP:ATP ratio, a well-known AMPK inducer. The authors first demonstrated that rosiglitazone also activates AMPK, a finding not previously reported, and that it does so by dramatically increasing the AMP:ATP ratio. Surprisingly, however, metformin apparently did not change the ratio to any measurable extent. This was an interesting finding, prompting the authors to conclude that rosiglitazone and metformin activate AMPK via distinct routes.
But there was a hitch to that conclusion—thanks to greater refinements in analytical methods, additional studies have shown that AMPK is sensitive even to very small changes in the AMP:ATP ratio. So small, in fact, that Carling and his team could not appreciate these changes with the tools in hand. “We did not have sensitive enough methods available for detecting very small changes in AMP,” Carling says. So even though metformin is much less potent than rosiglitazone in increasing the AMP:ATP ratio, both appear to activate AMPK through the same general mechanism. “It's been an interesting journey for the AMPK field to realize that the levels of change in the nucleotides that you need are incredibly subtle,” Carling concludes.
In an ironic twist, later studies have shown that AMPK is, in fact, activated via two separate routes: one through AMP:ATP ratio–stimulated phosphorylation by the upstream kinase LKB1 and another via calcium-induced phosphorylation by another enzyme, calcium/calmodulin-dependent kinase kinase 2 (CAMKK2). “It turns out there are two distinct pathways, just not the ones that we thought,” says Carling.
One detail that has become very clear through both Carling's work on AMPK and that of El-Mir et al. on complex I is that metformin profoundly alters cellular energetics. “I think there are a lot of knock-on effects that interfere with complex I,” says Carling, perhaps explaining why it's been so hard to pin down metformin's direct target (Fig. 1). But metformin's elusive activity in the lab, owing to its relatively weak effects on the AMP:ATP ratio and its impaired uptake into some cells, might be why it continues to be an efficient and well-tolerated antidiabetic drug. “The fact that it is a fairly poor drug turns out to be its strength—it's very unusual,” notes Carling. “I think metformin is a great example of why you shouldn't get too hung up with mechanism [when you start] to test whether a drug is effective.”
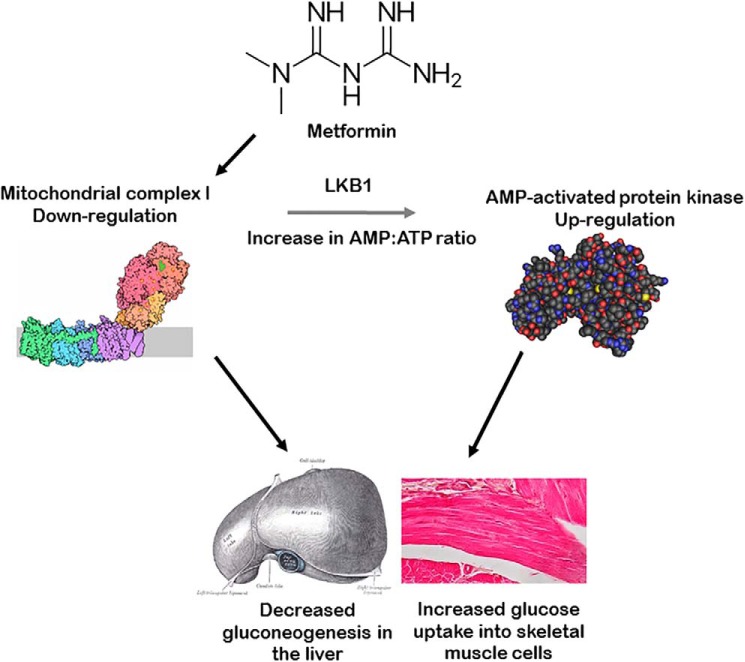
Figure 1.
Metformin down-regulates mitochondrial complex I activity in intact liver cells and stimulates AMPK activity in muscle cells. As shown by El-Mir et al. (2), hepatocytes exposed to millimolar concentrations of metformin have lower activity of complex I. This effect is indirect because it manifests only in intact cells and not in isolated mitochondria or permeabilized hepatocytes. As reported by Fryer and colleagues (3), treating muscle cells with metformin up-regulates AMPK, presumably via liver kinase B1 (LKB1), indicating an indirect effect of metformin on AMPK. Although metformin's direct molecular target remains unknown to date, metformin's effect on complex I likely affects cellular bioenergetics, resulting in knock-on effects, such as an increase in the AMP:ATP ratio, which, in turn, stimulates AMPK activity (as indicated by the gray arrow). Additional studies have shown that metformin decreases liver gluconeogenesis and increases insulin-mediated glucose uptake into skeletal muscle cells. Images of metformin, mitochondrial complex I, AMPK, liver, and skeletal muscle are from Wikimedia, used under Creative Commons.
This hasn't stopped scientists' search for metformin's direct target(s). The hope is that unraveling how metformin works could lead to its improvement to more efficiently manage diabetes or cancers that have emerged as potential targets of metformin-based therapies. Recent advances such as cryo-EM have enabled detailed structural studies of larger protein complexes, including complex I. Carling predicts that we may now be much closer to finding out whether or how metformin interacts with complex I or other cellular structures. “[Complex I] is an obvious one to do,” he says. Perhaps the long journey to solving the mystery of metformin's direct target will soon come to an end.
Sadly, three of the scientists who made major contributions to the findings related here have since died: Mohamad-Yehia El-Mir and Xavier Leverve, first and senior authors, respectively, of the El-Mir et al. paper, and Lee Fryer, first author of the study by the Carling group.
Fontaine worked closely with El-Mir for about two years and remembers him as a great friend and colleague. Fontaine fondly recalls that Leverve was a very inspiring mentor. “He was a fantastic man—very, very charismatic. Everybody who met him wanted to work with him.” He suspects that Leverve's training and experience as a physician working in an intensive care unit (ICU) probably had spurred his advisor's interest in bioenergetics, leading him to study complex I and the compounds acting on it. “He had a very open mind from the clinic, especially in the ICU, where there is a kind of energy failure during a septic shock,” Fontaine says.
Although Carling very much appreciates that his lab's work has been nominated as a JBC Classic, he also notes, “It's a great shame that Lee is not around to see this recognition. Lee was a very productive scientist and had a big impact on my laboratory. It's such a pity that he is no longer around to contribute to science.”
Footnotes
Ruma Banerjee nominated these papers as Classics.
References
- 1. Sterne J. (1959) Treatment of diabetes mellitus with N,N-dimethylguanylguanidine (LA. 6023, glucophage). Therapie 14, 625–630 [PubMed] [Google Scholar]
- 2. El-Mir M. Y., Nogueira V., Fontaine E., Avéret N., Rigoulet M., and Leverve X. (2000) Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I. J. Biol. Chem. 275, 223–228 10.1074/jbc.275.1.223 [DOI] [PubMed] [Google Scholar]
- 3. Fryer L. G., Parbu-Patel A., and Carling D. (2002) The anti-diabetic drugs rosiglitazone and metformin stimulate AMP-activated protein kinase through distinct signaling pathways. J. Biol. Chem. 277, 25226–25232 10.1074/jbc.M202489200 [DOI] [PubMed] [Google Scholar]
- 4. Zhou G., Myers R., Li Y., Chen Y., Shen X., Fenyk-Melody J., Wu M., Ventre J., Doebber T., Fujii N., Musi N., Hirshman M. F., Goodyear L. J., and Moller D. E. (2001) Role of AMP-activated protein kinase in mechanism of metformin action. J. Clin. Invest. 108, 1167–1174 10.1172/JCI13505 [DOI] [PMC free article] [PubMed] [Google Scholar]