Burkholderia pseudomallei is the causative agent of melioidosis. This condition most often presents as pneumonia and bacteremia, with mortality rates of 9% to 70%.
KEYWORDS: Burkholderia pseudomallei, matrix-assisted laser desorption ionization, melioidosis, diagnostics, mass spectrometer
ABSTRACT
Burkholderia pseudomallei is the causative agent of melioidosis. This condition most often presents as pneumonia and bacteremia, with mortality rates of 9% to 70%. Therefore, early identification of this organism may aid in directing appropriate management. This study aimed to use the Vitek matrix-assisted laser desorption ionization–time of flight mass spectrometer to create a spectrum for the rapid identification of B. pseudomallei. Spectra from 85 isolate cultures were acquired using the Vitek mass spectrometer research mode. A SuperSpectrum was created using peak matching and subsequently activated for analysis of organism identification. All 85 isolates were correctly identified as B. pseudomallei. A total of 899 spectra were analyzed and demonstrated a specificity of 99.8%. Eighty-one clinical isolates were used, of which 10 were neuromelioidosis, and no discernible spectrum difference was appreciated. Spectrum acquisition from a single spot was only successful in 374/899 (41%) of isolates. This increased to 100% when 3 spots of the same extract were analyzed. The Vitek mass spectrometer can be used for the rapid identification of B. pseudomallei with a high level of specificity.
INTRODUCTION
The genus Burkholderia contains 50 species. Among these, only B. mallei, B. pseudomallei, B. cepacia complex, B. thailandensis, and B. gladioli are generally recognized as human pathogens (1). These organisms utilize aerobic respiration, are non-spore-forming Gram-negative bacilli, and with the exception of B. mallei, are all motile (1).
B. pseudomallei is the causative agent of melioidosis in both animals and humans. It is a saprophytic organism found predominantly in moist soil and water (2, 3). Infection is often associated with an inoculating injury or the inhalation of aerosolized bacteria, which appears to occur more frequently in the wet season or severe weather events such as tropical storms (4–7). The most common presentation of melioidosis is community-acquired pneumonia and bacteremia (5, 8).
Melioidosis is predominantly a disease of the subtropical and tropical regions, endemic largely in northern Australia and South East Asia, including but not limited to Thailand, Vietnam, Laos, Cambodia, Malaysia, Indonesia, Singapore, Papua New Guinea, and the Indian subcontinent (9). The incidence appears to be increasing, and although overall mortality appears to be improving in Australia, mortality rates range from 14% to as high as 42.5% in Northeast Thailand (4, 10). Current estimates suggest 165,000 cases of melioidosis and 89,000 resultant deaths worldwide per year (11).
The identification of B. pseudomallei has been an ongoing challenge since its initial description. Apart from colonial morphology recognition and simple bench tests, more robust specific phenotypic characteristics have been utilized. An analytical profile index (API), specifically the bioMérieux API 20NE (bioMérieux, Marcy-l’Etoile, France) is used as an adjunct to the diagnosis. Unfortunately, this method, with a turnaround time of approximately 48 h, has demonstrated a 31% misidentification of B. pseudomallei in one study and a range of 37% to 99% in others (1, 12). Automated colorimetric-based identification such as Vitek-2 has an improved accuracy; however, it too has a wide margin of error with 63% to 81% accuracy (13). An indirect diagnosis by using serology is an alternative if no microbiological specimens are available or positive. However, serology is less useful in areas of endemicity, as it will not be able to differentiate exposure, past, chronic, or active infection. The indirect hemagglutination assay (IHA) test is performed using an antigen from strains of B. pseudomallei sensitized to sheep cells and utilizes unsensitized cells as a control (1). Notably, the combination of IHA and IgM enzyme-linked immunosorbent assay (ELISA) in the diagnosis of acute melioidosis in an area of endemicity demonstrated a sensitivity of 100% and specificity of 95.4%; however, the performance of this test is variable in a low prevalence setting (14). The development of a lateral flow assay which detects capsular polysaccharide via a monoclonal antibody has a reported sensitivity of 99% and specificity of 100% when used on turbid blood cultures (15, 16). The test is easy to perform, relatively inexpensive, and may be a promising rapid diagnostic tool (16). PCR testing of clinical isolates in B. pseudomallei culture-positive patients has demonstrated 100% sensitivity and specificity on wound swabs, abscess aspirates, urine, and sputum (17). Notably, the sensitivity of this assay on blood samples ranged from 17% to 74% depending on features of septic shock and likely reflects a constraint in the limit of detection (17, 18). Currently, a major reason for the poor uptake of molecular testing appears to be a limited availability of real-time PCR instrumentation in diagnostic laboratories.
Matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) is a rapid identification system which is widely used in diagnostic microbiology laboratories. The benefits of this method include a short analysis time and high sensitivity and specificity, as well as limited technical and training requirements (19–21). Two commercially available MALDI-TOF MS instruments, namely, the Bruker Microflex Biotyper (Bruker Daltonik GmbH, Bremen, Germany) and bioMérieux Vitek MS (bioMérieux, Marcy-l'Etoile, France), have been approved for clinical use. Neither system’s standard diagnostic database includes the reference spectra required for identification of B. pseudomallei by MALDI-TOF MS (22, 23). The standard Vitek MS in vitro diagnostic (IVD) database can identify the organism to the genus but not species level (24). This is of limited use, as it is not uncommon for B. pseudomallei to be misidentified as B. cepacia by phenotypic methods. The Vitek MS research use only (RUO) database does include B. pseudomallei spectra, but it is not FDA approved nor has it been evaluated in a clinical context (25). Using the Bruker standard database, the result may only be accurate to the genus level or the isolate may be misidentified as B. thailandensis. On this platform, the security-relevant library, which includes potential agents of bioterrorism, can identify B. pseudomallei (25–27). In-house Bruker MS reference libraries have been created and found to be accurate in the identification of B. pseudomallei from both primary isolates and directly from blood cultures (28, 29). This study demonstrated a potential workflow that would decrease the time to identification by up to 24 h. There is no current standard for the minimum number of isolates or strains required for the creation of in-house spectra; however, there is evidence to suggest that 10 or more reference spectra correlate with the greatest identification accuracy (30). A potential drawback to the use of MALDI-TOF MS is the requirement for organism inactivation. Multiple methods have been proposed, including 70% ethanol, formic acid, trifluoroacetic acid, gamma irradiation, centrifugation, and filtration, with various results (31, 32). One study reported a 100% reduction in viable organisms treated with on-plate 70% formic acid (33).
Given the nature of the infection and high mortality rate, a rapid diagnosis is imperative to enable appropriate directed therapy (4, 8). This study aimed to use the Vitek MS RUO mode to create a spectrum for the rapid identification of B. pseudomallei.
MATERIALS AND METHODS
The study was performed at the Townsville Hospital, a 600-bed tertiary care center in North Queensland, Australia. Approval for this study was obtained from the Townsville Hospital and Health Service Human Research Ethics Committee (HREC/18/QTHS/3). Isolates of B. pseudomallei were obtained from the department of microbiology’s stored collection of over 250 clinical isolates, collected from 1990 to 2017. Due to the potential diversity of different B. pseudomallei proteomes, 40 random isolates were initially chosen for analysis. All handling of preinactivated isolates occurred in a physical containment (PC) level 3 laboratory. Each isolate was initially plated onto Ashdown’s agar (ASH) to ensure pure growth. Subsequently, the cultured organism was plated in duplicates on horse blood agar (HBA), chocolate agar (CHOC), and ASH (bioMérieux, Marcy-l'Etoile, France). Each isolate was then incubated at 35°C in both O2 and CO2 environments. Additionally, 24- and 48-h colony growth of each isolate was analyzed.
To minimize the potential risk of laboratory-acquired infection and to maximize protein extraction, the Vitek Mycobacterium/Nocardia kit was used for isolate inactivation and extraction according to the manufacturer’s instructions. A 1-µl volume of each extracted sample was placed on a target spot on the MALDI-TOF MS acquisition plate. After air drying, 1 µl of α-cyano-4-hydroxycinnamic acid (CHCA) matrix was added to the spot and allowed to crystallize prior to spectrum acquisition. Spectrum acquisition was performed in RUO mode utilizing the Shimadzu Biotech MALDI-MS application (Shimadzu Biotech, Kyoto, Japan). Each isolate from each growth condition was analyzed at least once, totaling a minimum of 12 spectra per isolate. These spectra were then imported into the research database. Data analysis and SuperSpectrum creation were performed using the SARAMIS (Spectral Archive and Microbial Identification System) v4.12 application (bioMérieux, Marcy-l'Etoile, France). Additionally, 8 isolates of B. thailandensis were used to create a B. thailandensis SuperSpectrum using the aforementioned methodology, with the aim of excluding overlapping mass/charge peaks from the B. pseudomallei SuperSpectrum to improve the specificity of identification. Once activation occurred, known isolates were run through the Vitek MS RUO mode and compared to the newly created B. pseudomallei SuperSpectrum to assess the accuracy of identification.
RESULTS
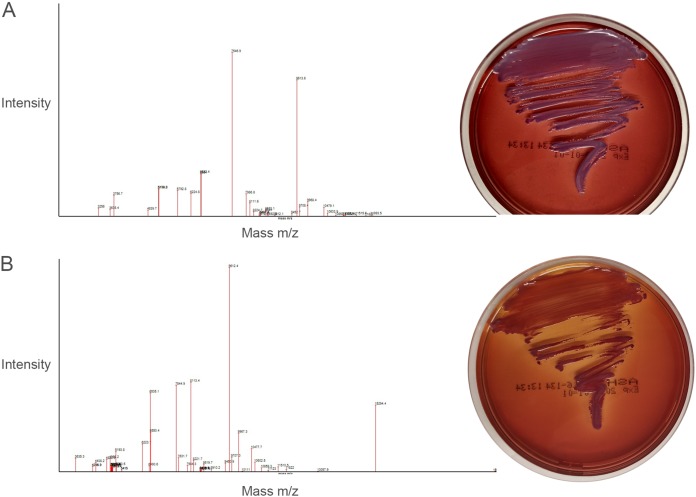
A total of 568 spectra were created using 40 isolates. Of the 40 isolates, 36 were from clinical samples, 2 were American Type Culture Collection (ATCC) strains (ATCC 23343 and ATCC 4846), 1 was a National Collection of Type Culture (NCTC) strain (NCTC 13178), and 1 was a Western Australian Culture Collections (WACC) strain (WACC 236/91). A comparison between isolates demonstrated a diversity of both phenotypes and spectra with regard to peaks and intensity (Fig. 1).
FIG 1.
Phenotypic and spectrum comparison between two American Type Culture Collection (ATCC) strains. (A) ATCC 4846; (B) ATCC 23343. Organisms were cultured for 48 h at 35°C in 5% CO2 on Ashdown agar.
There was also substantial intraisolate spectrum variability. This variability did not appear to be specifically influenced by the incubation period, O2 and CO2 culture environment, or HBA, CHOC, and ASH media.
Following completion and activation of the SuperSpectrum, the original 40 isolates were rerun, and 32/40 (80%) were identified as B. pseudomallei. There were no incorrect organism identifications, as the 8 isolates that were not identified had no genus nor species reported. The specificity of the B. pseudomallei SuperSpectrum was assessed by comparing it to the SuperSpectrum of all organisms in the bioMérieux database (bioMérieux, Marcy-l’Etoile, France). Additionally, 8 B. thailandensis isolates were prepared, and 220 spectra were acquired with the creation of a B. thailandensis SuperSpectrum. None of the spectra were identified as B. pseudomallei.
In an attempt to improve the sensitivity of B. pseudomallei identification, additional isolates were used to create a second SuperSpectrum. As the initially acquired spectra did not demonstrate substantial variability with regard to culture conditions, an additional 45 isolates were cultured on HBA in 5% CO2 for 24 h, and then spectra were acquired from colonies performed as per the aforementioned methodology. An additional 286 spectra from these 45 isolates were added to the original data. A new SuperSpectrum using 854 spectra was subsequently created with the aim of improving organism identification. With the additional spectrum acquisitions, a total of 899 spectra were acquired from 85 isolates.
An assessment of the new SuperSpectrum demonstrated correct identification of all 85 (100%) B. pseudomallei isolates; however, spectrum acquisition from a single spot was only successful in 374/899 (41%) of isolates. This increased to 100% when 3 spots of the same extract were analyzed. Identification accuracy scores for B. pseudomallei isolates ranged from 75.4% to 99.9%. There were only 2 (0.2%) misidentifications when comparing all 899 B. pseudomallei spectra to the Vitek MS IVD database. Of these misidentifications, one spectrum was identified as Yersinia species with a 78% identification score, the second was Proteus mirabilis with a score of 75%. Therefore, the specificity for identifying B. pseudomallei from a matched spectrum was 99.8%.
The isolates used were reviewed with regard to the clinical source of infection. Of 81 clinical isolates, 27/81 were from pulmonary foci, 13/81 were from an unknown focus, 10/81 from the central nervous system (CNS), 7/81 from joints, 5/81 from skin and soft tissues, 4/81 from lymph nodes, 4/81 from urine, 3/81 from prostates, 3/81 from osteomyelitis, 3/81 from bacteremia, 1/81 from a liver abscess, and 1/81 from a psoas abscess. There was no correlation between spectrum identification and the infection source.
After completion of the evaluation of B. pseudomallei identification by the newly created SuperSpectrum, a secondary analysis of spectra was performed in order to compare isolates associated with CNS and non-CNS infections. In total, 10 isolates were from patients with CNS melioidosis. A SuperSpectrum using these isolates was created in order to ascertain the most common mass peaks. In total, 47 peaks were found to have adequate reproducibility between spectra. There were no outlying peaks in the CNS SuperSpectrum that could be used to rapidly differentiate isolates that may have a CNS preponderance.
DISCUSSION
Previous methods of B. pseudomallei identification have been plagued by inaccuracy, prolonged turnaround time, and cost (1, 12, 26, 34). Mass spectrometry identification of organisms has increased over time and is now a standard in many laboratories worldwide. Although the initial equipment cost may be high, the laboratory savings for organism identification has been reported at greater than 50% compared to that with conventional methods (35–37). Additionally, specific identification turnaround time for B. pseudomallei may be improved by 16 to 24 h given the current method involves phenotypic analysis. This improved time to diagnosis may improve antimicrobial stewardship and patient outcomes.
This study demonstrates that bioMérieux Vitek MS (bioMérieux, Marcy-l'Etoile, France) can be used for the rapid identification of B. pseudomallei. While the use of 40 isolates to create the first SuperSpectrum resulted in 80% isolate identification, the addition of 45 isolates resulted in 100% identification with 99.8% specificity. This information supports the fact that B. pseudomallei is phenotypically diverse and, as such, may have a broad potential proteome structure. Our results are surprising with regard to specificity. Previous reports have suggested misidentification with B. thailandensis, which was not reproduced in our data. Notably, identification was performed using the Bruker Biotyper MALDI-TOF MS (Bruker Daltonics, Bremen, Germany) instrument (23, 26).
There are several limitations in this study. The current methodology resulted in a low reproducibility of only 41%. Specifically, a single 1-µl spot of the extracted isolate produced inconsistent spectrum results. However, assessing three or more 1-µl spots from the same extract produced 100% identification. This may be due to an imperfect ability to accurately and repeatedly measure the exact volume of colony used in the inactivation-extraction process. It has been reported in other settings that the volume of extraction agents may be adjusted depending on pellet size (38). Arguably, this may be less rigorous than creating a more accurate initial volume, as determining the pellet size accurately would be challenging. The authors acknowledge that performing a spectral analysis in triplicates is not standard practice. However, the additional time and cost in this setting would be of negligible practical consequence and would improve identification to 100% while maintaining a 0.2% false-positive rate. Another limitation of this study is that a B. mallei SuperSpectrum was not created to compare to that of B. pseudomallei, as previous data suggest that these species may be misidentified (22). However, given that B. mallei is a much rarer cause of human disease, this omission may be of limited clinical relevance (1, 39). The authors acknowledge that no specific phenotypic or genetic testing was performed, nor environmental isolates included; therefore, we cannot confirm the diversity of the isolates used. However, the use of 81 clinical isolates representing an array of clinical syndromes may obviate this limitation.
In conclusion, the Vitek MS RUO can be used for the rapid identification of B. pseudomallei and will now be considered a supplementary tool in our laboratory workflow. Further research is required with regard to improving the reproducibility of spectrum acquisition and identification. Additionally, this creates the scope to assess the performance of the new SuperSpectrum in identifying B. pseudomallei directly from positive blood culture.
ACKNOWLEDGMENTS
We thank Snehal Anuj and bioMérieux Australia, as well as The Townsville Hospital Pathology Queensland staff for their patience and assistance during this study.
REFERENCES
- 1.LiPuma JJ, Currie BJ, Peacock SJ, Vandamme P. 2015. Burkholderia, Stenotrophomonas, Ralstonia, Cupriavidus, Pandoraea, Brevundimonas, Comamonas, Delftia, and Acidovorax, p 791–812. In Jorgensen JH, Pfaller MA, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW. (ed), Manual of clinical microbiology, 11 ed ASM Press, Washington, DC. [Google Scholar]
- 2.Currie BJ, Jacups SP, Cheng AC, Fisher DA, Anstey NM, Huffam SE, Krause VL. 2004. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop Med Int Health 9:1167–1174. doi: 10.1111/j.1365-3156.2004.01328.x. [DOI] [PubMed] [Google Scholar]
- 3.Vuddhakul V, Tharavichitkul P, Na-Ngam N, Jitsurong S, Kunthawa B, Noimay P, Noimay P, Binla A, Thamlikitkul V. 1999. Epidemiology of Burkholderia pseudomallei in Thailand. Am J Trop Med Hyg 60:458–461. doi: 10.4269/ajtmh.1999.60.458. [DOI] [PubMed] [Google Scholar]
- 4.Currie BJ, Ward L, Cheng AC. 2010. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl Trop Dis 4:e900. doi: 10.1371/journal.pntd.0000900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng AC, Currie BJ. 2005. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Currie BJ, Price EP, Mayo M, Kaestli M, Theobald V, Harrington I, Harrington G, Sarovich DS. 2015. Use of whole-genome sequencing to link Burkholderia pseudomallei from air sampling to mediastinal melioidosis, Australia. Emerg Infect Dis 21:2052–2054. doi: 10.3201/eid2111.141802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen P-S, Chen Y-S, Lin H-H, Liu P-J, Ni W-F, Hsueh P-T, Liang S-H, Chen C, Chen Y-L. 2015. Airborne transmission of melioidosis to humans from environmental aerosols contaminated with B. pseudomallei. PLoS Negl Trop Dis 9:e0003834. doi: 10.1371/journal.pntd.0003834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stewart JD, Smith S, Binotto E, McBride WJ, Currie BJ, Hanson J. 2017. The epidemiology and clinical features of melioidosis in Far North Queensland: implications for patient management. PLoS Negl Trop Dis 11:e0005411. doi: 10.1371/journal.pntd.0005411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Currie BJ, Dance DAB, Cheng AC. 2008. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg 102:S1–S4. doi: 10.1016/S0035-9203(08)70002-6. [DOI] [PubMed] [Google Scholar]
- 10.Limmathurotsakul D, Wongratanacheewin S, Teerawattanasook N, Wongsuvan G, Chaisuksant S, Chetchotisakd P, Chaowagul W, Day NPJ, Peacock SJ. 2010. Increasing incidence of human melioidosis in northeast Thailand. Am J Trop Med Hyg 82:1113–1117. doi: 10.4269/ajtmh.2010.10-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Limmathurotsakul D, Golding N, Dance DA, Messina JP, Pigott DM, Moyes CL, Rolim DB, Bertherat E, Day NP, Peacock SJ, Hay SI. 2016. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol 1:15008. doi: 10.1038/nmicrobiol.2015.8. [DOI] [PubMed] [Google Scholar]
- 12.Glass MB, Popovic T. 2005. Preliminary evaluation of the API 20NE and RapID NF Plus systems for rapid identification of Burkholderia pseudomallei and B. mallei. J Clin Microbiol 43:479–483. doi: 10.1128/JCM.43.1.479-483.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zong Z, Wang X, Deng Y, Zhou T. 2012. Misidentification of Burkholderia pseudomallei as Burkholderia cepacia by the VITEK 2 system. J Med Microbiol 61:1483–1484. doi: 10.1099/jmm.0.041525-0. [DOI] [PubMed] [Google Scholar]
- 14.Kunakorn M, Boonma P, Khupulsup K, Petchclai B. 1990. Enzyme-linked immunosorbent assay for immunoglobulin M specific antibody for the diagnosis of melioidosis. J Clin Microbiol 28:1249–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Houghton RL, Reed DE, Hubbard MA, Dillon MJ, Chen H, Currie BJ, Mayo M, Sarovich DS, Theobald V, Limmathurotsakul D, Wongsuvan G, Chantratita N, Peacock SJ, Hoffmaster AR, Duval B, Brett PJ, Burtnick MN, AuCoin DP. 2014. Development of a prototype lateral flow immunoassay (LFI) for the rapid diagnosis of melioidosis. PLoS Negl Trop Dis 8:e2727. doi: 10.1371/journal.pntd.0002727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woods KL, Boutthasavong L, NicFhogartaigh C, Lee SJ, Davong V, AuCoin DP, Dance DAB. 2018. Evaluation of a rapid diagnostic test for detection of Burkholderia pseudomallei in the Lao People's Democratic Republic. J Clin Microbiol 56:e02002-17. doi: 10.1128/JCM.02002-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meumann EM, Novak RT, Gal D, Kaestli ME, Mayo M, Hanson JP, Spencer E, Glass MB, Gee JE, Wilkins PP, Currie BJ. 2006. Clinical evaluation of a type III secretion system real-time PCR assay for diagnosing melioidosis. J Clin Microbiol 44:3028–3030. doi: 10.1128/JCM.00913-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Novak RT, Glass MB, Gee JE, Gal D, Mayo MJ, Currie BJ, Wilkins PP. 2006. Development and evaluation of a real-time PCR assay targeting the type III secretion system of Burkholderia pseudomallei. J Clin Microbiol 44:85–90. doi: 10.1128/JCM.44.1.85-90.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Welker M, Moore ER. 2011. Applications of whole-cell matrix-assisted laser-desorption/ionization time-of-flight mass spectrometry in systematic microbiology. Syst Appl Microbiol 34:2–11. doi: 10.1016/j.syapm.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Krásný L, Hynek R, Hochel I. 2013. Identification of bacteria using mass spectrometry techniques. Int J Mass Spectrom 353:67–79. doi: 10.1016/j.ijms.2013.04.016. [DOI] [Google Scholar]
- 21.Holland RD, Wilkes JG, Rafii F, Sutherland JB, Persons CC, Voorhees KJ, Lay JO Jr. 1996. Rapid identification of intact whole bacteria based on spectral patterns using matrix-assisted laser desorption/ionization with time-of-flight mass spectrometry. Rapid Commun Mass Spectrom 10:1227–1232. doi:. [DOI] [PubMed] [Google Scholar]
- 22.Karger A, Stock R, Ziller M, Elschner MC, Bettin B, Melzer F, Maier T, Kostrzewa M, Scholz HC, Neubauer H, Tomaso H. 2012. Rapid identification of Burkholderia mallei and Burkholderia pseudomallei by intact cell matrix-assisted laser desorption/ionisation mass spectrometric typing. BMC Microbiol 12:229. doi: 10.1186/1471-2180-12-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang H, Chen YL, Teng SH, Xu ZP, Xu YC, Hsueh PR. 2016. Evaluation of the Bruker Biotyper matrix-assisted laser desorption/ionization time-of-flight mass spectrometry system for identification of clinical and environmental isolates of Burkholderia pseudomallei. Front Microbiol 7:415. doi: 10.3389/fmicb.2016.00415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luo Y, Siu GK, Yeung AS, Chen JH, Ho PL, Leung KW, Tsang JL, Cheng VC, Guo L, Yang J, Ye L, Yam WC. 2015. Performance of the Vitek MS matrix-assisted laser desorption ionization-time of flight mass spectrometry system for rapid bacterial identification in two diagnostic centres in China. J Med Microbiol 64:18–24. doi: 10.1099/jmm.0.080317-0. [DOI] [PubMed] [Google Scholar]
- 25.Dingle TC, Butler-Wu SM, Abbott AN. 2014. Accidental exposure to Burkholderia pseudomallei in the laboratory in the era of matrix-assisted laser desorption ionization–time of flight mass spectrometry. J Clin Microbiol 52:3490–3491. doi: 10.1128/JCM.01238-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walewski V, Mechai F, Billard-Pomares T, Juguet W, Jaureguy F, Picard B, Tandjaoui-Lambiotte Y, Carbonnelle E, Bouchaud O. 2016. MALDI-TOF MS contribution to diagnosis of melioidosis in a nonendemic country in three French travellers. New Microbes New Infect 12:31–34. doi: 10.1016/j.nmni.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jang HR, Lee CW, Ok SJ, Kim MJ, Bae MJ, Song S, Yi J, Kim KH. 2015. Melioidosis presenting as a mycotic aneurysm in a Korean patient, diagnosed by 16S rRNA sequencing and matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Int J Infect Dis 38:62–64. doi: 10.1016/j.ijid.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 28.Inglis TJJ, Healy PE, Fremlin LJ, Golledge CL. 2012. Use of matrix-assisted laser desorption/ionization time-of-flight mass spectrometry analysis for rapid confirmation of Burkholderia pseudomallei in septicemic melioidosis. Am J Trop Med Hyg 86:1039–1042. doi: 10.4269/ajtmh.2012.11-0454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suttisunhakul V, Pumpuang A, Ekchariyawat P, Wuthiekanun V, Elrod MG, Turner P, Currie BJ, Phetsouvanh R, Dance DA, Limmathurotsakul D, Peacock SJ, Chantratita N. 2017. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry for the identification of Burkholderia pseudomallei from Asia and Australia and differentiation between Burkholderia species. PLoS One 12:e0175294. doi: 10.1371/journal.pone.0175294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seng P, Drancourt M, Gouriet F, La Scola B, Fournier PE, Rolain JM, Raoult D. 2009. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin Infect Dis 49:543–551. doi: 10.1086/600885. [DOI] [PubMed] [Google Scholar]
- 31.Rudrik JT, Soehnlen MK, Perry MJ, Sullivan MM, Reiter-Kintz W, Lee PA, Pettit D, Tran A, Swaney E. 2017. Safety and accuracy of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of highly pathogenic organisms. J Clin Microbiol 55:3513–3529. doi: 10.1128/JCM.01023-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cunningham SA, Patel R. 2013. Importance of using Bruker's security-relevant library for Biotyper identification of Burkholderia pseudomallei, Brucella species, and Francisella tularensis. J Clin Microbiol 51:1639–1640. doi: 10.1128/JCM.00267-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cunningham SA, Patel R. 2015. Standard matrix-assisted laser desorption ionization-time of flight mass spectrometry reagents may inactivate potentially hazardous bacteria. J Clin Microbiol 53:2788–2789. doi: 10.1128/JCM.00957-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Inglis TJ, Chiang D, Lee GS, Chor-Kiang L. 1998. Potential misidentification of Burkholderia pseudomallei by API 20NE. Pathology 30:62–64. doi: 10.1080/00313029800169685. [DOI] [PubMed] [Google Scholar]
- 35.Patel TS, Kaakeh R, Nagel JL, Newton DW, Stevenson JG. 2017. Cost analysis of implementing matrix-assisted laser desorption ionization–time of flight mass spectrometry plus real-time antimicrobial stewardship intervention for bloodstream infections. J Clin Microbiol 55:60. doi: 10.1128/JCM.01452-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tran A, Alby K, Kerr A, Jones M, Gilligan PH. 2015. Cost savings realized by implementation of routine microbiological identification by matrix-assisted laser desorption ionization–time of flight mass spectrometry. J Clin Microbiol 53:2473–2479. doi: 10.1128/JCM.00833-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ge M-C, Kuo A-J, Liu K-L, Wen Y-H, Chia J-H, Chang P-Y, Lee M-H, Wu T-L, Chang S-C, Lu J-J. 2017. Routine identification of microorganisms by matrix-assisted laser desorption ionization time-of-flight mass spectrometry: success rate, economic analysis, and clinical outcome. J Microbiol Immunol Infect 50:662–668. doi: 10.1016/j.jmii.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 38.Chen JH, Ho PL, Kwan GS, She KK, Siu GK, Cheng VC, Yuen KY, Yam WC. 2013. Direct bacterial identification in positive blood cultures by use of two commercial matrix-assisted laser desorption ionization-time of flight mass spectrometry systems. J Clin Microbiol 51:1733–1739. doi: 10.1128/JCM.03259-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.White NJ. 2003. Meliodosis. Lancet 361:1715–1722. doi: 10.1016/S0140-6736(03)13374-0. [DOI] [PubMed] [Google Scholar]