Abstract
In this report, we present the successful treatment of five consecutive cases of premenopausal women suffering from severe menstrual migraine with tokishakuyakusan (TSS). Two patients were complicated by tension‐type headache (TTH), and another patient was by medication overuse headache (MOH). The effects of triptans were limited in all of them. After starting TSS, they showed dramatic improvement in the severity and frequency of their attacks. The patients with TTH and MOH also showed dramatic improvement in their symptoms. TSS could be a promising alternative choice for patients with intractable menstruation–related headaches that are refractory to conventional treatments, including triptans.
Keywords: herbal medicine, intractable headache, menstrual migraine, tokishakuyakusan, triptan
1. INTRODUCTION
Migraine is a disease that presents with relapsing moderate‐to‐severe headaches, mainly seen in young women before menopause. In many patients, migraine attacks are synchronous with the menstrual periods.1 The disease can be treated with preventive medications (eg, calcium channel blockers, beta blockers), combined with medications for pain relief in acute migraine attack (eg, triptans, NSAIDs). However, most of these preventive drugs are counterindicated during pregnancy. A Japanese herbal (kampo) medicine, goshuyuto, is sometimes used to prevent migraine attacks, but it is not always effective as the same with other medications.
Tokishakuyakusan (TSS) is a traditional herbal medicine frequently prescribed to women with dysmenorrhea or menopausal disorder.2 TSS is thought to regulate concentration and cycling of female hormones, and adjust the balance of these hormones.3, 4 From before, the effectiveness of TSS for middle‐aged menopausal or postmenopausal women has been known.5 However, its effectiveness for refractory menstrual migraine in young premenopausal women has not been known yet.
2. CASES
The clinical information of the five consecutive patients with severe intractable menstruation–related headaches is listed in Table 1. All of them were diagnosed with menstrual migraine (attacks between day −2 and +3 of menses for >3 months), with or without tension‐type headache (TTH), by neurologists prior to administration of TSS. All of the patients took triptans or other anti‐headache medications in more than 5 days per month for more than 1 year. At least more than two types of anti‐headache medications were tried before TSS in all of them.
Table 1.
Clinical information of the five patients
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Age at first visit | 24 | 32 | 42 | 48 | 51 |
| Onset age | 15 | 18 | 20 | 17 | 40 |
| Height [cm] | 156.8 | 151.7 | 157.0 | 157.8 | 156.5 |
| Weight [kg] (BMI) | 92.8 (37.7) | 46.7 (20.3) | 64.2 (26.0) | 56.4 (22.6) | 50.6 (20.7) |
| Diagnosis | MM, TTH | MM | MM, TTH, MOH | MM | MM |
| Headache drugs before TSS | SMT, ELT, tizanidine | SMT, NRT, gosyuyuto, loxoprofen | SMT, ASA, eperisone, VPA | SMT, ASA | SMT, tizanidine |
| TSS dosage | 2.5 g TID | 2.5 g TIDa | 2.5 g BID | 2.5 g BID | 2.5 g TID |
| Monthly averaged severity of headache in NRS (0‐10) per attack | |||||
| Before TSS | 9‐10 | 8‐10 | 8‐10 | 8‐10 | 9‐10 |
| 3 mo after TSS | 0‐1 | 0‐1 | 2‐3 | 0 | 5‐6 |
| Frequency of taking anti‐headache medication [times/month] | |||||
| Before TSS | 5‐10 | 5‐10 | 25‐30 | 5‐10 | 5‐10 |
| 3 mo after TSS | 0 | 0 | 3‐4 | 0 | 3‐4 |
Abbreviations: ASA, acetylsalicylic acid; BID, twice daily; BMI, body mass index; ELT, eletriptan; MM, menstrual migraine; MOH, medication overuse headache; NRS, numerical rating scale; NRT, naratriptan; SMT, sumatriptan succinate; TID, three times daily; TSS, Tokisyakuyakusan (Japanese) or Dang‐Gui‐Shao‐Yao‐San (Chinese); TTH, tension‐type headache; VPA, valproic acid. [Correction added on 4 April 2019, after first online publication: Table 1 has been added.]
Case 2 took TSS only around her menstrual periods.
The severity of their headaches was assessed using the numerical rating scale (NRS), from 0 (no pain) to 10 (the strongest pain). They were administered TSS extract granules (Tsumura and Co., Tokyo, Japan) for their chronic fatigue, and its effectiveness for headache was not expected at first. Neurological examinations revealed no abnormal findings in all five patients. Brain MRI studies revealed several white matter lesions (WML) related to migraine in one patient (Case 3), but showed normal findings in the others. Headache diary was used in all patients to subjectively record the nature and course of their headaches. As for their past medical history, Case 5 had suffered from long‐standing iron deficiency anemia with menorrhagia, but others had no mentionable past medical history.
2.1. Case 1
When she first visited our hospital at the age of 24, her symptoms fulfilled both code 1.1 “migraine without aura” and code 2.3 “chronic tension‐type headache” of the International Classification of Headache Disorders‐3 beta version (ICHD‐3β).6 Triptans were largely ineffective by the time she consulted us. Within a month from starting TSS at 7.5 mg/day for her chronic fatigue, her headache, together with the fatigue and TTH‐related symptoms, swiftly disappeared and she discontinued using triptans.
2.2. Case 2
She was 32 years old when she first visited our hospital. Her clinical course is shown in Figure 1. Her symptoms gravely deteriorated after she experienced a spontaneous abortion at age 31. After this event, her headaches were extremely acute and caused her ADL to be severely compromised. The effectiveness of triptans or NSAIDs was limited and short‐lived. Gosyuyuto was also tried, but was totally ineffective. When she first visited our hospital, her symptoms fulfilled the ICHD‐3β code 1.2.1.1 “typical aura with headache”.6 Low‐dose estrogen‐progestin therapy and female hormone injections were tried and were effective to some extent, but their effects lasted no more than 2‐3 weeks. By this time, triptans, goshuyuto, or NSAIDs had also become ineffective. Within 2 weeks from starting TSS, her headache dramatically disappeared and she no more required any anti‐headache medications.
Figure 1.
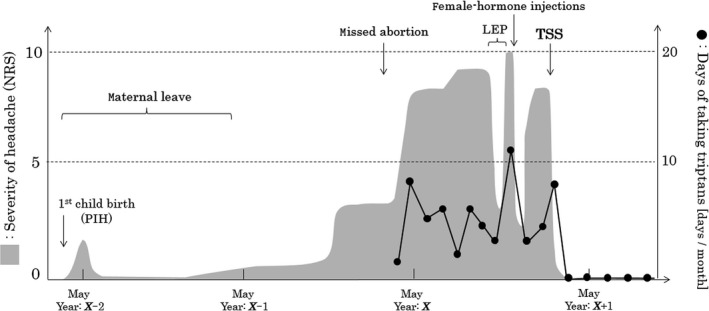
Strength of headache and the frequency of taking triptans in Case 2. An association between the headache and female hormones was apparent from the shown clinical course. NRS, numerical rating scale for pain; PIH, pregnancy‐induced hypertension; LEP, low‐dose estrogen‐progestin; TSS, tokishakuyakusan
2.3. Case 3
She had suffered from migraines since the age of 20 and gradually developed symptoms suggestive of TTH. Triptans were effective at first, but their effectiveness gradually decreased, and she discontinued them because of their side effects. Valproic acid as a preventive therapy was totally ineffective. In her thirties, administration of NSAIDs (ibuprofen) became frequent, almost every day without drug holiday. When she first visited our hospital at the age of 42, her symptoms fulfilled the ICHD‐3β code 1.1 “migraine without aura,” code 2.3 “chronic tension‐type headache,” and code 8.2 “medication‐overuse headache”.6 Brain MRI revealed several WML possibly related to migraine. Within a month from starting TSS, her headache was gradually alleviated and the frequency of taking headache drugs also decreased.
2.4. Case 4
She was 48 years old when she first visited our hospital. She had suffered from chronic headache since the age of 17, but she had never consulted a doctor and chose to use over‐the‐counter drugs. Her symptoms fulfilled ICHD‐3β code 1.1 “migraine without aura”.6 She refused to take allopathic preventive drug and pain‐relief medications but agreed to take herbal medicines. She was administered TSS at 5.0 mg/day. Within a month, her headache disappeared and she did not require any further medication.
2.5. Case 5
She had suffered from menstrual migraine since the age of 40. She did not wish to become pregnant, but she refused to take any preventive medications recommended by the previous doctor and continued to take triptans as needed. When she consulted with us at the age of 51, her symptoms fulfilled ICHD‐3β code 1.2.1.1 “typical aura with headache”.6 She was administered TSS at 7.5 mg/day. Within several months, her headache was alleviated and the frequency with which she took triptans also decreased.
3. DISCUSSIONS
Five premenopausal patients who suffered from severe menstruation‐related headaches were successfully treated with TSS. All of the five patients had shown limited responses to one or more triptans before starting TSS. As shown in Table 1, the severity and frequency of their menstruation‐related headaches dramatically decreased within 1 month after starting TSS. Additional pain‐relief medications were not necessary in three of the five patients (Cases 1, 2, and 4). The effectiveness of TSS persisted for more than 6 months without any apparent side effects and the effects continued even after ceasing administration of the drug in one patient (Case 2). The BMI may not be an appropriate predictor for judging the indication of TSS.
TSS has been widely used in the field of gynecology, targeting diseases such as ovarian dysfunction, ovulation disorders, dysmenorrhea, infertility, and menopausal disorders.7, 8 TSS is believed to function by increasing the secretion of estrogen and progesterone from the ovary, possibly by activating the hypothalamic‐pituitary‐gonadal axis (HPG axis).3, 4
Herbal medicines are reasonable alternative treatments for migraine with the drug prices lower than triptans. As described in the introduction, there are herbal medicines other than TSS that can be used for headache. One of the candidates is gosyuyuto, but it is used for frequent headache with nausea and cold feeling, which were not apparent in the presented cases. Another candidate would be chotosan, but it is mainly used for headache in the morning. Meanwhile, TSS is usually used for headache accompanied by menstrual conditions; thus, TSS seems to have advantages for the presented five cases among these medicines.
As for the timing of starting TSS in patients with triptan‐resistant menstrual migraine, many neurologists usually try to use at least two or three triptans (ie, serotonin 5‐HT 1B/1D receptor agonists) before making diagnosis as being triptan‐resistant. Thus, the timing of starting TSS for symptoms with the indication of TSS in patients with menstrual migraine, with or without the intention to expect therapeutic effects even to the headache, would be ideal after trying more than two types of triptans.
As a conclusion, TSS could be a useful alternative treatment for premenopausal women suffering from severe intractable menstruation–related headaches.
CONFLICTS OF INTEREST
ST, MO, AK, and TI belong to the department of kampo medicine in Tohoku University Hospital, which receives grant from Tsumura and Co., Tokyo, Japan.
Akaishi T, Takayama S, Ohsawa M, et al. Successful treatment of intractable menstrual migraine with the traditional herbal medicine tokishakuyakusan. J Gen Fam Med. 2019;20:118–121. 10.1002/jgf2.242
REFERENCES
- 1. Kornstein SG, Parker AJ. Menstrual migraines: etiology, treatment, and relationship to premenstrual syndrome. Curr Opin Obstet Gynecol. 1997;9(3):154–9. [PubMed] [Google Scholar]
- 2. Pan JC, Tsai YT, Lai JN, Fang RC, Yeh CH. The traditional Chinese medicine prescription pattern of patients with primary dysmenorrhea in Taiwan: a large‐scale cross sectional survey. J Ethnopharmacol. 2014;152(2):314–9. [DOI] [PubMed] [Google Scholar]
- 3. Koyama T, Hagino N, Cothron AW, Saito M. Effect of toki‐shakuyaku‐san on ovulation induced by human menopausal gonadotropin in rats. Am J Chin Med. 1988;16(3–4):169–72. [DOI] [PubMed] [Google Scholar]
- 4. Irahara M, Yasui T, Tezuka M, Ushigoe K, Yamano S, Kamada M, et al. Evidence that Toki‐shakuyaku‐san and its ingredients enhance the secretion of a cytokine‐induced neutrophil chemoattractant (CINC/gro) in the ovulatory process. Methods Find Exp Clin Pharmacol. 2000;22(10):725–30. [DOI] [PubMed] [Google Scholar]
- 5. Terauchi M, Hiramitsu S, Akiyoshi M, Owa Y, Kato K, Obayashi S, et al. Effects of the kampo formula tokishakuyakusan on headaches and concomitant depression in middle‐aged women. Evidence‐based complementary and alternative medicine : eCAM. 2014;2014:593560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. The International Classification of Headache Disorders . 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. [DOI] [PubMed] [Google Scholar]
- 7. Enomoto K, Higashida H, Maeno T. Effects of toki‐shakuyaku‐san (Tsumura TJ‐23) on electrical activity in neuroblastoma cells and frog neuromuscular junctions. Neurosci Res. 1992;15(1–2):81–9. [DOI] [PubMed] [Google Scholar]
- 8. Proctor ML, Farquhar CM. Dysmenorrhoea. BMJ Clin Evid. 2007;2007:????–????. [PMC free article] [PubMed] [Google Scholar]


