Abstract
Objective. To characterize how virtual reality (VR) has been and is being used in pharmacy education, and evaluate the projected utility of VR technology in pharmacy education in the future.
Findings. Virtual reality technology has been used in pharmacy education for many years to provide engaging learning experiences. Although these learning experiences were not available in the three-dimensional digital environments provided by current VR, they demonstrated improvements in learning. Recent technological advancements have substantially increased the potential usefulness of VR for pharmacy education by providing immersive educational activities that mimic real world experiences to reinforce didactic and laboratory concepts. Virtual reality training that uses head-mounted displays is just beginning in pharmacy education, but more educational VR programs are becoming available. Further research will be necessary to fully understand the potential impact of VR on pharmacy education.
Summary. Virtual reality technology can provide an immersive and interactive learning environment, overcoming many of the early challenges faced by instructors who used virtual activities for pharmacy education. With further technological and software development, VR has the potential to become an integral part of pharmacy education.
Keywords: virtual reality, immersive, technology, active learning, augmented reality
INTRODUCTION
Over the past few decades, instructional technology has progressed from chalkboards to computer-based slideshows and beyond; however, the format of pharmacy classes has been slower to evolve. No matter what technology has been available, pharmacy education typically involves an instructor standing at the front of a large classroom, delivering content, hoping to impart knowledge. Low classroom attendance is likely multifactorial; however, there is some evidence to suggest that increasingly poor attendance is supported by lecture and lecture content being accessible through digital means.1-3 As qualitative and quantitative evidence has proven that active learning is more effective than passive learning, instructors are now seeking alternative pedagogies to lectures.4-6 Providing alternatives to lectures appears to be particularly important for 21st century students, who prefer more independent, task-based learning strategies and the integration of technology.7 To address the learning needs of today’s student, educators have begun to adapt their teaching styles to engage learners through the use of active-learning and through incorporation of educational technology.8,9 In everyday practice, pharmacists use problem-solving skills to address numerous patient care issues. The Accreditation Council for Pharmacy Education (ACPE) emphasizes that pharmacy programs provide students with the knowledge, skills, and abilities to provide patient-centered care and solve problems.10 Therefore, pharmacy students must be provided ample opportunities to hone their skills. Practice experiences are arguably the best way to prepare students for a career in pharmacy. However, practice experiences involve challenges such as securing enough sites for all students and ensuring that all students have equivalent experiences. One mechanism developed to provide students with mock experiences are simulations incorporated into the didactic curriculum. Simulations may involve anything from a prepared scenario with actors to using simulation dummies. Active-learning simulations are beneficial to learning, and can even increase students’ empathy for patients.11 However, simulations typically require extensive planning and tend to be resource intensive, with mannequins being costly and scenario simulations requiring a high ratio of instructors to students.12,13
Despite these challenges, educators strive to provide students with the best learning experiences. One emerging technology that is showing promise in not only engaging the learner but also in overcoming current obstacles is VR. The purpose of this manuscript is to evaluate the past, present, and future of VR as a tool in pharmacy education.
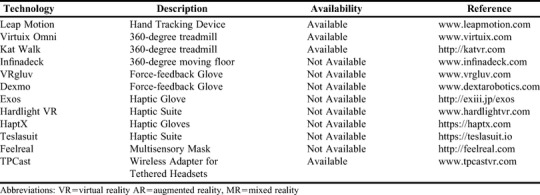
The definition of VR has evolved over time, resulting in some confusion in the literature. The current definition of VR is understood as “an artificial environment which is experienced through sensory stimuli (such as sights and sounds) provided by a computer and in which one's actions partially determine what happens in the environment.”14 This definition can be applied to many different types of activities, but modern VR typically refers to experiences that take place while wearing head-mounted displays or headsets. The terms augmented reality (AR) and “mixed reality” (MR) are both essentially varying degrees of VR. Virtual reality can be defined as any immersive simulated reality, and most often refers to a “complete” virtual experience. Google Cardboard (Google LLC, Mountain View, CA), Google Daydream (Google LLC, Mountain View, CA), Oculus Rift (Facebook Technologies, LLC, Menlo Park, CA), and HTC Vive (HTC, Bellevue, WA) are headsets that are used primarily for VR.15-17 Augmented reality and mixed reality are often confused and used interchangeably. While AR typically refers to a computer-generated overlay on the real world,18 the overlay does not necessarily interact with the real world. Google Glass (Google LLC, Mountain View, CA) is an early example of AR.19 Mixed reality involves a computer-generated overlay that interacts with the real world.18 The Microsoft HoloLens (Microsoft, Redmond, WA) is a promising example of MR, although it is not yet widely available.20 The subtle differences between VR, AR, and MR are summarized in Table 1. Virtual reality is far more advanced in its development than AR and MR, but all three have the potential to positively impact education. Types of VR, AR, and MR headsets and various accessories are listed in Tables 2 and 3, respectively.
Table 1.
Definitions of Virtual Reality, Augmented Reality, and Mixed Reality
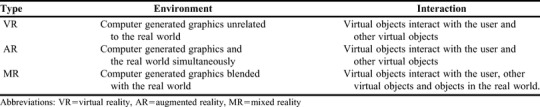
Table 2.
Examples and Specifications of Virtual Reality, Augmented Reality, and Mixed Reality Headsets
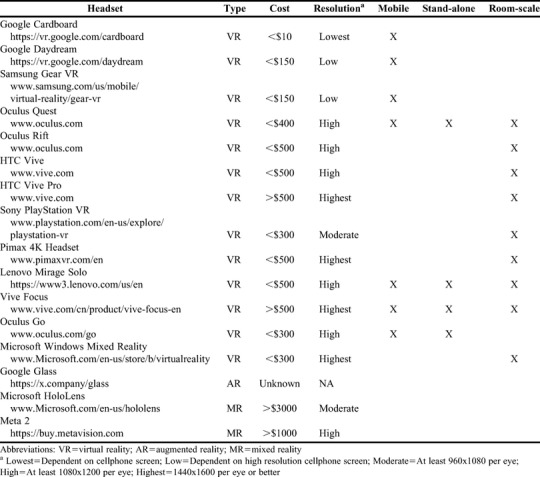
Table 3.
Examples of Accessory Technology for Virtual Reality, Augmented Reality, and Mixed Reality
METHODS
A literature search was conducted for this review using PubMed, Scopus, ERIC, Google, and Google Scholar. Terms searched for included “virtual reality,” “augmented reality” “mixed reality,” and “pharmacy education.” The search was limited to articles describing either the use of head-mounted displays or virtual activities in pharmacy education. Websites for the manufacturers of head-mounted displays were reviewed for technical specifications. Additionally, websites for VR, AR, and MR software were evaluated for educational content.
RESULTS
The History of Virtual Learning in Pharmacy Education
Prior to the advances in immersive technology that resulted in the use of head-mounted displays for VR experiences, educators were already leveraging other types of virtual activity to improve learning. Simulations, two-dimensional virtual world platforms, patient cases, and three-dimensional (3D) modeling have all demonstrated benefits in pharmacy education.13,21-23 Simulation mannequins can be somewhat realistic and responsive and have been used to assess student competencies in patient safety, assessment, ethical, professional and legal behaviors, and patient counseling and virtual patient cases.24-26 Unfortunately, the cost of mannequins, the required ratio of teachers to students, and the realism necessary to conduct accurate patient assessments can be prohibitive. Second Life (Linden Lab, San Francisco, CA) is a two-dimensional (2D) virtual world platform that was popular in education five to 10 years ago. Second Life was used successfully in the development of virtual pharmacy school classrooms with limited content and used as an alternative to teaching classes face-to-face. Second Life was also used to develop a virtual pharmaceutical science (compounding) laboratory with the objective of creating problem-based educational modules.22,27,28 The use of virtual worlds such as those created in Second Life declined as a teaching tool from 2010 to 2015.29 The decrease in use of virtual worlds in pharmacy education may have been because of the high level of expertise required to design activities in the platform and a lack of technological and funding support.29 Virtual reality has been used to teach drug-receptor interactions in 3D as opposed to a traditional lecture with 2D graphics. Students who learned in a 3D space did significantly better on an examination than their 2D graphics counterparts did.21 Similarly, drug design (eg, protein-ligand binding) can be evaluated in VR at the molecular level.30 This type of activity can significantly impact pharmacy education courses in drug development, medicinal chemistry, and pharmacology. Virtual reality was also explored for a virtual community pharmacy experience.31 This virtual community pharmacy experience was developed to assist pharmacists in designing their own pharmacy building and layout, but could be modified for students to learn about interacting with patients within a community pharmacy without compromising real patient care. Lastly, Fox and Felkey discussed using VR for pharmacy patient education to increase a patients’ knowledge about their health and medications.32 In their study, pharmacists provided patients with counseling on how to administer medications and offered an opportunity to administer medications in a virtual world. Pharmacists were also able to conduct teach-back sessions with patients to explain and demonstrate what they had learned.32
Although there were some challenges to overcome, such as virtual media being limited to flat, two-dimensional screens, past use of VR technology in pharmacy education demonstrated some success.13,21–23 Twenty-first century developments in the quality of VR technology have further enhanced pharmacy-related VR educational experiences.
Advancements in Immersive VR Technology
Participants’ ability to immerse themselves in VR activities depends on the sense of presence that the experience affords. According to Slater, the sense of presence in a virtual world is dependent on two primary components: place illusion and plausibility illusion.33 Place illusion describes how much a person believes that they are in the virtual world, in other words, immersion. Plausibility illusion describes how much a person believes that what is happening in the virtual world is real.33 Both of these components are necessary to provide a sense of presence in a virtual world. 33 Place illusion can be achieved with high quality computer-generated visual information and accurate head and movement tracking. 33 Recent advances in video card technology have allowed for the development of VR headsets with high-quality visual displays. Accurate tracking technology has also been developed that allows headsets to recognize the six degrees of freedom required for “room-scale VR.” To enable room-scale VR, headsets must recognize the rotation of the head in all three directions (tilting forwards and backwards, rotating left to right, and tilting sideways), and movement across all three planes (moving forwards and backwards, left and right, up and down). Room-scale VR allows a person to move around the virtual space in the same way as the real world, and thus greatly adds to immersion. Tracking technology, combined with high quality visual displays, have allowed the current generation of VR headsets to provide VR experiences that are far more immersive than previous technology.34 Plausibility illusion is a far more complicated component of presence to measure.33 In one study, a variety of different measures, including participants’ survey responses, skin conductance responses, electrocardiograms, and skin temperature were used to assess plausibility illusion.33 This study demonstrated that “full body tracking” was one of the most important factors associated with depth of presence.33,35 Development in plausibility illusion is still ongoing, with the introduction of such devices as haptic gloves and body suits (Table 1). Even without achieving strong plausibility illusion, advances in visual display and head-tracking technology have provided highly immersive experiences and a strong sense of presence in VR that were never previously possible.35
Potential Uses of VR Technology in Pharmacy Education
Active engagement has become widely acknowledged as an important element of the learning process.5,6,36,37 Historically, lecture-based curricula generally encourages passive student engagement. However, instructors are transitioning in their role from a “sage on the stage,” where the teacher is delivering content at the front of the classroom, to a “guide on the side,” where teachers facilitate learning instead.38 The “guide on the side” posturing is readily seen in active-learning pedagogies such as problem-based learning (PBL) and team-based learning (TBL), which are becoming more popular as evidenced by increased use in universities, specifically in healthcare education.38-40 Both PBL and TBL have demonstrated benefits by promoting critical thinking, problem solving, communication, teamwork, and creativity.41,42 These pedagogies help students to learn theory but do not always provide the opportunity for students to apply what they have learned to real-world scenarios. There is evidence to suggest that increased use of appropriate educational technology coupled with decreased faculty-student interaction improves student academic achievement.5 Additionally, student enrollment in distance education has increased for 14 years in a row. In 2016, 31.6% of students enrolled in higher education were taking at least one distance-learning course.43 These distance-learning courses make it difficult to provide practical experiences unless students have required on-campus sessions. For example, many distance-learning science courses require that students attend on-campus laboratory classes.44 Despite these challenges, providing students with opportunities to put theory into practice is essential to many professions. Virtual reality may offer solutions to many of these problems. Headsets are less expensive than specialized equipment and can simulate any environment, negating the need to buy specialized equipment for each discipline. For example, a single VR system could provide a pharmacy dispensing experience for one group of students and a surgical simulation for the next. Large class size may still be challenging in VR, but the reduced cost of equipment may mean that more simulations can be made available to more students at one time. This would allow instructors to run several simulations simultaneously to accommodate larger classes. For distance-learning students, VR could provide hands-on experiences similar to those experienced by students attending classes on campus. In fact, Immersive VR Education, Ltd, are developing a VR educational platform that will enable students and instructors to meet in a virtual classroom from any location.45 Virtual reality may allow distance-learning courses to one day be almost identical to face-to face classes. Oculus recently announced a new headset that will provide room-scale experiences without the need of a computer.46,47 At only $399, this could provide an affordable means for students to learn in VR without any complex set up.47
In addition to making it easier to implement hands-on learning activities, VR can augment education by providing experiences that are not feasible in the real world, which may be especially useful for disciplines where learning from one’s mistakes has unacceptable consequences. For example, students in health care professions cannot put patients at risk in order to learn from their mistakes. Being able to make mistakes while learning and not suffer consequences allows students to look at a situation from different perspectives, identify flaws in their thinking, and uncover assumptions.48,49 Virtual reality simulations provide the opportunity for students not only to learn from their mistakes, but also to receive feedback from instructors, reflect on those mistakes, and try again. This may be particularly useful for pharmacy students learning about patient safety, critical care, medication errors, and having difficult conversations. Some topics are difficult to conceptualize, even with videos and animations. The interactive 3D environment afforded by VR can provide different perspectives that may make difficult topics easier to understand. For example, a recently developed VR application, 4D Toys (Marc Ten Bosch, USA), allows users to interact with theoretical four-dimensional objects from a three-dimensional perspective. The 4D toys application provides a fun and unique way to learn about a difficult concept. There are many topics in the pharmacy curriculum where difficult concepts could be made easier through VR. For example, students could follow the journey of a drug through the human body to learn about pharmacokinetics. Finally, some topics are tedious and/or boring for students to learn. VR can add an element of fun through interactivity or even gamification.50 For example, memorizing the brand and generic names of drugs could be developed into a game to increase engagement.46
Previous research into VR as a medium for health education primarily focused on surgical simulation and anatomical visualization.51-54 Gautier and colleagues designed a game using the Oculus Rift to simulate obstetrical emergencies.51 Although not yet tested with students, the obstetrical emergencies game was intended to teach common gynecological pathologies through various virtual scenarios. Moro and colleagues found that in addition to VR and AR being as effective as tablet-based technology (ie, the use of iPads or Android tablets) for teaching anatomy, they also increased student engagement, interactivity, and enjoyment.53 These successful examples of using VR to teach anatomy to medical students could also be applied to pharmacy education. Thus far, only a handful of educational VR programs, such as The BodyVR (The Body VR, New York, NY), Engage (VR Education Holdings PLC, Waterford City, Ireland), and Human Anatomy VR (Virtual Medicine, s. r. o., Slovakia), have been developed. Pharmacy students need to practice communicating with the healthcare team and with patients and their relatives. Virtual reality can offer students an opportunity to practice communication, perhaps through use of a virtual patient that can make adaptive responses to each choice as students work through the patient care process.55 Virtual reality applications that simulate various patient experiences could be used to build empathy before students interact with patients. In a pilot study, a VR simulation movie that demonstrated dementia through the eyes of a patient was found to provide insight and understanding to caregivers.56 Similar activities could be used to allow students to see what it is like to be a patient. BodyVR provides a journey through a blood vessel and into a cell during a viral infection. Similar types of activities could be developed such as following the journey of a drug through the body on the anatomical, cellular, and molecular level to see where drugs are distributed, how they affect various organs, structural changes to the drug during its journey, metabolism, and elimination. Virtual reality is also proving to be useful in patient care by providing opportunities to understand patients, helping patients overcome phobias, distracting patients from pain, and motivating patients to change their lifestyle.57-62 Collectively, these studies indicate that VR may become commonplace in healthcare regardless of its use in health professions education.
Technological Advances That May Impact Pharmacy Education
The impact of VR technology on health professions education will largely depend on future technological advancements, and we are just beginning to see the considerable potential of VR in pharmacy education.63 For the most part, room-scale VR experiences involve being tethered to a computer. The attached wire can interfere with the user’s immersion and present a potential tripping hazard. Add-on equipment for VR headsets is now available that allows wireless room-scale VR with minimal latency, allowing a high-quality untethered VR experience. Standalone room-scale VR headsets were released in early 2019.64,65 Stand-alone room-scale VR headsets negate the need for an expensive computer and include “inside-out” tracking. Inside-out tracking involves the headset tracking what is around the user, rather than stationary “lighthouses” (sensors) tracking the headset within a predetermined zone. A potential benefit of inside-out tracking is that it could allow multiple VR headsets in any given space, which would make it easier for students to work together on VR problems in the same physical space without the risk of collision. Additionally, these types of headsets require less technical expertise to set up. Also, they will be more “plug-and-play,” which could reduce the level of apprehension instructors may feel about setting up VR equipment. Anticipated standalone headsets will not require cellphones, which would ensure that all devices are of the same quality. Because a separate computer would not be needed, these standalone headsets will likely be less expensive.
One of the most beneficial technological advancements in VR for pharmacy students will be the ability to feel their environment. Haptic gloves will enable students to feel the drugs that they are dispensing, and also provide opportunities to conduct patient assessments. Imagine how beneficial it would be for a student to be able to feel the heart rate of a patient, conduct a diabetic foot examination, or even teach a patient how to properly use their point-of-care device from half a world away. Additionally, VR technology can be used to train students in sterile compounding, which can address the limitations in resources currently needed.66 There are no haptic gloves currently available, but several are under development (Table 1).67,68 Virtual reality headsets are also being improved, having higher resolution screens and wider fields of view.69 Comfortable, ergonomic, and lighter headsets are still under development.
Lastly, AR and MR are also in simultaneous development. Augmented reality is starting to gain traction because of its ability to enhance content. For example, drug companies are exploring AR to provide more in-depth drug information not only to physicians but also to patients by moving their mobile device over an image.70,71 Pharmacy Times has developed an AR application that allows readers to scan pages that have an AR symbol with their cellphone to reveal extra content.72 Augmented reality and MR may be particularly useful in pharmacy practice and education. A study using Google Glass and another using Microsoft HoloLens found both AR and MR to be beneficial during surgical procedures.73,74 In these two studies, the surgeon was able to see the actual surgery and relevant patient information, such as medical history.73,74 The same technology could be used by pharmacists while preparing prescription medications. For example, a pharmacist could use AR to access drug information while verifying or checking a prescription. In France, AR glasses have been used in a hospital pharmacy to prepare injectable medications.75 The AR glasses were used to display instructions for preparation of the medications with the goal of reducing medication errors related to not having access to information while preparing the drugs. With further technological advancements, AR could become an extremely useful tool, both for pharmacy practice and pharmacy education.76
Limitations of VR Technology
Although it may be tempting to dive into VR and all that it has to offer, there are limitations to consider. One of the biggest problems with VR is that wearing a VR headset for prolonged periods is uncomfortable. This is due to several factors, such as headset weight and size, pixilated visual displays, heat generation from the headset, and the required connectivity to a computer. Virtual reality sickness is a possibility for many people. Although not fully understood, simulator sickness seems to occur when there is a discrepancy between visual information informing the body of movement and proprioception. Symptoms of virtual reality sickness include nausea, cold sweating, and pallor.77 Ensuring that there is alignment between visual information on movement and actual movement appears to minimize the likelihood of VR sickness.78 Use of VR sickness detection methods may also help developers to identify and correct problems that could cause VR sickness during the development of VR applications.77,79 Desensitization is possible with even the most high-intensity VR experiences (eg, rollercoaster simulations) with repeated exposure,77 and therefore may become less of a problem with continued VR exposure. Current headsets primarily rely on visual information to provide a sense of realism, which does not provide a fully immersive experience and may exclude users who are visually impaired.
Cost may be a problem, depending on the type and quality of the equipment. A VR-ready desktop computer costs a minimum of $650 and a laptop costs a minimum of $700. Headsets that provide room-scale experiences range from $200 to $1,400. Although still relatively expensive, the cost of VR equipment, including headsets and computers, has significantly decreased since 2017. With the release of newer technology, a low-end, room-scale VR set-up should become more affordable. However, if an institution were to purchase enough VR set-ups for all students, it could still be extremely expensive. Headsets that require a cellphone and recognize head movements but not body movements provide a less expensive alternative to room-scale VR systems. For example, a Google Cardboard costs as little as $5, but would require all students to have their own smart phone and the experience would be less immersive than that when using a room-scale VR.
From a development perspective, there is limited pharmacy-related educational content available. Hiring developers is expensive and building their own content is not feasible for most educators. Current platforms that help the nondeveloper to create content include Anyland (Philipp Lenssen and Scott Lowe, Germany and UK) and High Fidelity (High Fidelity Inc., San Francisco, CA).80,81 The game development platform, Unreal Engine 4 (Epic Games Inc., Cary, NC),82 has an option to build VR content from within VR, but this may still be challenging for non-developers. Engage from VR Education Holdings promises to allow educators to add their own 3D models, slides, and environments to VR, and has the potential to be user friendly for nondevelopers.83 These tools may eventually enable anyone to build their own content, but for now, a basic level of programming expertise is required to build content. Finally, there is often reluctance on the part of both students and educators to try new technology. Students may readily embrace VR, but it may be more challenging for instructors to become comfortable with the technology, particularly because there are few ways for non-experts to develop VR content. Convincing administrators to invest resources in VR may be even more difficult. To overcome these obstacles, research will be needed to demonstrate the positive benefits that VR can provide for education.
There are also psychosocial considerations that could limit the adoption and usefulness of VR in pharmacy education. Addiction to video games (gaming disorder), has now been included in the 11th revision of the International Classification of Diseases published by the World Health Organization.84 Virtual reality may have the potential for similar addictive tendencies, and some students may need to avoid this type of platform. Development of stronger communication skills is becoming more important in pharmacy education and in health education in general. There is the potential that the VR setting may be detrimental to the development of these skills. Shy students often prefer electronic media to communicate with their peers as it provides them with a sense of anonymity and privacy. Students who learn communication skills in VR may not be able to cope when face-to-face with a real person, and in extreme cases this may cause a person to feel completely disconnected from themselves and the real world. Alternatively, students who would otherwise avoid face-to-face interaction may be more likely to communicate with their peers in VR. More research in this area is necessary to fully understand the psychosocial implications of using VR for education.
Augmented reality and MR are in their early stages of development, which limits their usefulness. Headsets for AR and MR are large and heavy, with a limited battery life and cables that may interfere with function.85 The field of view of MR and AR headsets is limited, which can reduce immersion.86
CONCLUSION
In this review, we discussed the utility of VR in the context of pharmacy education, including a discussion of previous iterations of VR technology, how recent progress in VR technology may benefit pharmacy education, and what we may see in the next decade of VR technology. Earlier versions of VR have been used to provide pharmacy students with active-learning opportunities for many years. However, until recently technology has been restricted to two-dimensional computer screens, expensive simulation mannequins, and static paper-based cases. The latest VR technology involves head-mounted displays that provide interactive 360o environments. This is a crucial step forward in the utility of VR for pharmacy education, as the 360o environment allows for experiences that can immerse the learner in active learning scenarios that would not be otherwise possible. The authors of this manuscript anticipate that the integration of VR into pharmacy education will initially involve instructors occasionally using the technology to demonstrate challenging concepts. Virtual reality environments could be used to provide high-fidelity pharmacy simulations, field trips through the human body, and even opportunities to learn from mistakes, which is usually not feasible with real patients. The full extent to which VR will be used in the pharmacy curriculum is not yet clear and dependent on the development of appropriate software, but early opportunities may involve experiential and laboratory simulation. Widespread adoption of VR for use in pharmacy education will be dependent on overcoming comfort issues, high cost, and the limited educational content available. With more research and development, particularly software development, VR has the potential to become an integral part of pharmacy education.
ACKNOWLEDGEMENTS
The authors would like to thank Ms. Rebecca Fernandez for conducting literature searches.
REFERENCES
- 1.Bati AH, Mandiracioglu A, Orgun F, Govsa F. Why do students miss lectures? A study of lecture attendance amongst students of health science. Nurse Educ Today. 2013;33(6):596–601. doi: 10.1016/j.nedt.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 2.Bukoye OT, Shegunshi A. Impact of engaging teaching model (ETM) on students attendance. Cogent Education. 2016;3(1) [Google Scholar]
- 3.Kottasz R. Reasons for student non-attendance at lectures and tutorials: an analysis. Investigations in University Teaching and Learning. 2005;2(2):5–16. [Google Scholar]
- 4.Michael J. Where’s the evidence that active learning works? Adv Physiol Educ. 2006;30(4):159–167. doi: 10.1152/advan.00053.2006. [DOI] [PubMed] [Google Scholar]
- 5.Zhuang W, Xiao Q. Facilitate active learning: the role of perceived benefits of using technology. Journal of Education for Business. 2018;93(3):88–96. [Google Scholar]
- 6.Maarek J-M. Benefits of active learning embedded in online content material supporting a flipped classroom. Proceedings fo the ASEE Annual Conference & Exposition. 2018:1–10. [Google Scholar]
- 7.Shatto B, Erwin K. Teaching millennials and generation Z: bridging the generational divide. Creat Nurs. 2017;23(1):24–28. doi: 10.1891/1078-4535.23.1.24. [DOI] [PubMed] [Google Scholar]
- 8.Association of American Colleges & Universities. The Rise of Active Learning: Findings from the HERI Survey on Teaching Strategies of Undergraduate Faculty. 2014. https://www.aacu.org/aacu-news/newsletter/rise-active-learning-findings-heri-survey-teaching-strategies-undergraduate Accessed October 16, 2018.
- 9.Nicol AA, Owens SM, Le Coze SS, MacIntyre A, Eastwood C. Comparison of high-technology active learning and low-technology active learning classrooms. Active Learning in Higher Education. 2017:146978741773117. [Google Scholar]
- 10. Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree “Standards 2016.” 2015.
- 11.Whitley HP. Active-learning diabetes simulation in an advanced pharmacy practice experience to develop patient empathy. Am. J. Pharm. Educ. 2012;76(10):Article 203. doi: 10.5688/ajpe7610203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shin S, Park J-H, Kim J-H. Effectiveness of patient simulation in nursing education: meta-analysis. Nurse Educ. Today. 2015;35(1):176–182. doi: 10.1016/j.nedt.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Ray SM, Wylie DR, Shaun Rowe A, Heidel E, Franks AS. Pharmacy student knowledge retention after completing either a simulated or written patient case. Am. J. Pharm. Educ. 2012;76(5):Article 86. doi: 10.5688/ajpe76586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merriam-Webster Virtual Reality. https://www.merriam-webster.com/dictionary/ virtual%20reality Accessed December 19, 2017.
- 15.VIVE. Discover Virtual Reality Beyond Imagination. https://www.vive.com/us/. Accessed October 17, 2018.
- 16.Oculus. https://www.oculus.com/ Accessed October 18, 2018.
- 17. Google Cardboard – Google VR. https://vr.google.com/cardboard/. Accessed October 18, 2018.
- 18. Foundry. VR? AR? MR? Sorry, I’m confused. 2016. https://www.foundry.com/industries/virtual-reality/vr-mr-ar-confused. Accessed October 15, 2018.
- 19.Glass. https://x.company/glass Accessed October 16, 2018.
- 20.HoloLens Microsoft. The leader in mixed reality technology. https://www.microsoft.com/en-us/hololens Accessed October 17, 2018.
- 21.Richardson A, Bracegirdle L, McLachlan SIH, Chapman SR. Use of a three-dimensional virtual environment to teach drug-receptor interactions. Am J Pharm Educ. 2013;77(1):Article 11. doi: 10.5688/ajpe77111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Veronin MA, Daniels L, Demps E. Pharmacy cases in Second Life: an elective course. Adv. Med. Educ. Pract. 2012;3:105–112. doi: 10.2147/AMEP.S35358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3):Article 48. doi: 10.5688/aj700348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vyas D, Bray BS, Wilson MN. Use of simulation-based teaching methodologies in US colleges and schools of pharmacy. Am J Pharm Educ. 2013;77(3):Article 53. doi: 10.5688/ajpe77353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cendan J, Lok B. The use of virtual patients in medical school curricula. Adv Physiol Educ. 2012;36(1):48–53. doi: 10.1152/advan.00054.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryall T, Judd BK, Gordon CJ. Simulation-based assessments in health professional education: a systematic review. J Multidiscip Healthc. 2016;9:69–82. doi: 10.2147/JMDH.S92695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pharmatopia@Nottingham - Second Life - YouTube. https://www.youtube.com/watch?v=rpVv8zMYVRM Accessed January 13, 2018.
- 28. Pharmatopia - Faculty of Pharmacy and Pharmaceutical Sciences. https://www.monash.edu/pharm/innovative-learning/technologies/pharmatopia. Accessed January 13, 2018.
- 29.Gregory S, Scutter S, Jacka L, McDonald M, Farley H, Newman C. Barriers and enablers to the use of virtual worlds in higher education: an exploration of educator perceptions, attitudes and experiences. J Educ Tech & Soc. 2015;18(1):3–12. [Google Scholar]
- 30.Norrby M, Grebner C, Eriksson J, Boström J. Molecular rift: virtual reality for drug designers. J Chem Inf Model. 2015;55(11):2475–2484. doi: 10.1021/acs.jcim.5b00544. [DOI] [PubMed] [Google Scholar]
- 31.Mobach MP. The transformation of pharmacy concepts into building and organization. Pharm World Sci. 2005;27(4):329–338. doi: 10.1007/s11096-005-7111-x. [DOI] [PubMed] [Google Scholar]
- 32.Fox BI, Felkey BG. Virtual reality and pharmacy: opportunities and challenges. Hosp Pharm. 2017;52(2):160–161. doi: 10.1310/hpj5202-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Slater M. Place illusion and plausibility can lead to realistic behaviour in immersive virtual environments. Philos. Trans. R. Soc. Lond. B, Biol. Sci. 2009;364(1535):3549–3557. doi: 10.1098/rstb.2009.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Packet39. 3DOF, 6DOF, RoomScale VR, 360 Video and everything in between. 2018. https://packet39.com/blog/2018/02/25/3dof-6dof-roomscale-vr-360-video-and-everything-in-between/. Accessed October 25, 2018.
- 35. Skarbez RT. Plausibility illusion in virtual environments. 2016.
- 36.King A. From sage on the stage to guide on the side. College Teaching. 1993;41(1):30–35. [Google Scholar]
- 37.Lujan HL, DiCarlo SE. Too much teaching, not enough learning: what is the solution? Adv Physiol Educ. 2006;30(1):17–22. doi: 10.1152/advan.00061.2005. [DOI] [PubMed] [Google Scholar]
- 38.Baylor College of Medicine A Comparison between Three Modes of Instruction. 2002. https://www2.kumc.edu/PDFATraining/Admin/documents/Bonaminio%202.16.07%20comparison%20btwn%20lecture%20-%20pbl%20-%20team%20learning%20v2.pdf. Accessed October 25, 2018.
- 39.Allen RE, Copeland J, Franks AS, et al. Team-based learning in US colleges and schools of pharmacy. Am J Pharm Educ. 2013;77(6) doi: 10.5688/ajpe776115. Article 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burgess A, Bleasel J, Haq I, et al. Team-based learning (TBL) in the medical curriculum: better than PBL? BMC Med. Educ. 2017;17(1):243. doi: 10.1186/s12909-017-1068-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Phungsuk R, Viriyavejakul C, Ratanaolarn T. Development of a problem-based learning model via a virtual learning environment. Kasetsart Journal of Social Sciences. 2017 [Google Scholar]
- 42.Ofstad W, Brunner LJ. Team-based learning in pharmacy education. Am J Pharm Educ. 2013;77(4):Article 70. doi: 10.5688/ajpe77470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Seaman JE, Allen IE, Seaman J. Grade Increase: Tracking Distance Education in the United States. Babson Survey Research Group; 2018. [Google Scholar]
- 44.Smith GG, Passmore D, Faught T. The challenges of online nursing education. The Internet and Higher Education. 2009;12(2):98–103. [Google Scholar]
- 45.Engage Education Platform | Immersive VR Education. http://immersivevreducation.com/engage-education-platform/ Accessed December 19, 2017.
- 46.Shawaqfeh MS. Gamification as a learning method in pharmacy education. J Pharma Care Health Sys. 2015;s2 [Google Scholar]
- 47. Oculus. Oculus Quest. https://www.oculus.com/quest/. Accessed October 21, 2018.
- 48.Lundquist R. Critical thinking and the art of making good mistakes. Teaching in Higher Education. 1999;4(4):523–530. [Google Scholar]
- 49.Hemming HE. Encouraging critical thinking: “but ...what does that mean? McGill Journal of Education/Revue des sciences de l’éducation de McGill. 2000 [Google Scholar]
- 50. UPwork. Virtual Reality and Gamification: Two Biggest Trends in EdTech. https://www.upwork.com/hiring/for-clients/virtual-reality-gamification-edtech-trends/. Accessed October 21, 2018.
- 51.Jean Dit Gautier E, Bot-Robin V, Libessart A, Doucède G, Cosson M, Rubod C. Design of a serious game for handling obstetrical emergencies. JMIR Serious Games. 2016;4(2):e21. doi: 10.2196/games.5526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ros M, Trives JV, Lonjon N. From stereoscopic recording to virtual reality headsets: Designing a new way to learn surgery. Neurochirurgie. 2017;63(1):1–5. doi: 10.1016/j.neuchi.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 53.Moro C, Štromberga Z, Raikos A, Stirling A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ. 2017;10(6):549–559. doi: 10.1002/ase.1696. [DOI] [PubMed] [Google Scholar]
- 54.Messier E, Wilcox J, Dawson-Elli A, Diaz G, Linte CA. An interactive 3D virtual anatomy puzzle for learning and simulation - initial demonstration and evaluation. Stud Health Technol Inform. 2016;220:233–240. [PubMed] [Google Scholar]
- 55. Virtual Reality Is A Growing Reality In Health Care. https://www.forbes.com/sites/brucelee/2017/08/28/virtual-reality-vr-is-a-growing-reality-in-health-care/#6a04d1d48380. Accessed January 14, 2018.
- 56.Wijma EM, Veerbeek MA, Prins M, Pot AM, Willemse BM. A virtual reality intervention to improve the understanding and empathy for people with dementia in informal caregivers: results of a pilot study. Aging Ment. Health. 2017:1–9. doi: 10.1080/13607863.2017.1348470. [DOI] [PubMed] [Google Scholar]
- 57.Miloff A, Lindner P, Hamilton W, Reuterskiöld L, Andersson G, Carlbring P. Single-session gamified virtual reality exposure therapy for spider phobia vs. traditional exposure therapy: study protocol for a randomized controlled non-inferiority trial. Trials. 2016;17:60. doi: 10.1186/s13063-016-1171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tong X, Gromala D, Gupta D, Squire P. Usability comparisons of head-mounted vs. stereoscopic desktop displays in a virtual reality environment with pain patients. Stud Health Technol Inform. 2016;220:424–431. [PubMed] [Google Scholar]
- 59.Hoffman HG, Meyer WJ, Ramirez M, et al. Feasibility of articulated arm mounted Oculus Rift Virtual Reality goggles for adjunctive pain control during occupational therapy in pediatric burn patients. Cyberpsychol Behav Soc Netw. 2014;17(6):397–401. doi: 10.1089/cyber.2014.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hoffman HG, Garcia-Palacios A, Kapa V, Beecher J, Sharar SR. Immersive virtual reality for reducing experimental ischemic pain. Int. J. Hum. Comput. Interact. 2003;15(3):469–486. [Google Scholar]
- 61.Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev. 2010;30(8):1011–1018. doi: 10.1016/j.cpr.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 62.Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clin J Pain. 2009;25(9):815–826. doi: 10.1097/AJP.0b013e3181aaa909. [DOI] [PubMed] [Google Scholar]
- 63. Best Ways to Use Virtual and Augmented Reality for Pharma Viseven. https://viseven.com/news/best-ways-use-virtual-augmented-reality-pharma. Accessed January 13, 2018.
- 64. Lenovo. Introducing the New Lenovo Mirage Solo with Daydream. http://blog.lenovo.com/en/blog/cut-the-cables-and-immerse-yourself-in-virtual-reality-like-never-before-wi. Accessed January 22, 2018.
- 65.VIVE Blog. Vive Announces Vive Wave Open Platform and Vive Focus, Its Standalone VR device For China. https://blog.vive.com/us/2017/11/13/vive-developers-conference-beijing-2017/ Accessed January 21, 2018.
- 66. Learning Technologies Lab – University of Pittsburgh School of Computing & Information. http://learningtechlab.pitt.edu/. Accessed January 29, 2018.
- 67. VRgluv – Force Feedback Gloves for Virtual Reality. https://vrgluv.com/. Accessed January 29, 2018.
- 68. HaptX. Haptic gloves for VR training, simulation, and entertainment. https://haptx.com/. Accessed January 29, 2018.
- 69. 8K – Pimax Technology (Shanghai) Co., Ltd. https://www.pimaxvr.com/en/8k/#page1. Accessed January 29, 2018.
- 70. Augmented Reality In Healthcare Will Be Revolutionary - The Medical Futurist. http://medicalfuturist.com/augmented-reality-in-healthcare-will-be-revolutionary/. Accessed January 13, 2018.
- 71.Ferrone M, Kebodeaux C, Fitzgerald J, Holle L. Implementation of a virtual dispensing simulator to support US pharmacy education. Curr Pharm Teach Learn. 2017;9(4):511–520. doi: 10.1016/j.cptl.2017.03.018. [DOI] [PubMed] [Google Scholar]
- 72. Pharmacy Times. AR. http://www.pharmacytimes.com/ar. Accessed January 13, 2018.
- 73.Qian L, Barthel A, Johnson A, et al. Comparison of optical see-through head-mounted displays for surgical interventions with object-anchored 2D-display. Int J Comput Assist Radiol Surg. 2017;12(6):901–910. doi: 10.1007/s11548-017-1564-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Golab MR, Breedon PJ, Vloeberghs M. A wearable headset for monitoring electromyography responses within spinal surgery. Eur. Spine J. 2016;25(10):3214–3219. doi: 10.1007/s00586-016-4626-x. [DOI] [PubMed] [Google Scholar]
- 75.Orthman SB, Foinard A, Herbommez P, et al. Augmented reality for risks management in injectable drugs preparation in hospital pharmacy. Groupe d’Evaluation et de Recherche sur la Protection en Atmosphere Controlee. https://www.gerpac.eu/augmented-reality-for-risks-management-in-injectable-drugs-preparation-in-hospital-pharmacy. Accessed April 4, 2018.
- 76.Akçayır M, Akçayır G. Advantages and challenges associated with augmented reality for education: a systematic review of the literature. Educational Research Review. 2017;20:1–11. [Google Scholar]
- 77.Gavgani AM, Nesbitt KV, Blackmore KL, Nalivaiko E. Profiling subjective symptoms and autonomic changes associated with cybersickness. Auton Neurosci. 2017;203:41–50. doi: 10.1016/j.autneu.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 78. How to Avoid the Effect of Motion Sickness in VR - VRScout. https://vrscout.com/news/avoid-motion-sickness-developing-for-vr/. Accessed December 19, 2017.
- 79. Nakagawa C. Toward the detection of the onset of virtual reality sickness by autonomic indices. In: 2015 IEEE 4th Global Conference on Consumer Electronics (GCCE). IEEE; 2015:662-663. doi:10.1109/GCCE.2015.7398740.
- 80. SteamVR. Anyland. http://anyland.com/. Accessed January 29, 2018.
- 81.Henrich J. High fidelity. Science. 2017;356(6340):810. doi: 10.1126/science.aan2473. [DOI] [PubMed] [Google Scholar]
- 82. Unreal Engine VR Mode: Unreal Engine. https://docs.unrealengine.com/latest/INT/Engine/Editor/VR/. Accessed January 29, 2018.
- 83. VR Education Holdings. Virtual Reality Education, Training, Simulation, Learning. http://www.vreducationholdings.com/. Accessed October 21, 2018.
- 84. World Health Organization. Gaming disorder. 2018. http://www.who.int/features/qa/gaming-disorder/en/. Accessed October 21, 2018.
- 85.Khor WS, Baker B, Amin K, Chan A, Patel K, Wong J. Augmented and virtual reality in surgery-the digital surgical environment: applications, limitations and legal pitfalls. Ann Transl Med. 2016;4(23):454. doi: 10.21037/atm.2016.12.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Mashable. The worst thing about Microsoft HoloLens is still its field of view. 2018. https://mashable.com/2018/05/08/microsoft-hololens-field-of-view-big-weakness/#erGV9iZRagqs. Accessed October 21, 2018.


