Abstract
Cancer of unknown primary origin (CUP) which is usually diagnosed based on the histological type of metastatic site has marked heterogeneous characteristics. Sarcomatoid carcinoma defined as CUP has not been reported according to our literature survey. A 59-year-old man presented with enlarged multiple thoracic lymph nodes, huge splenomegaly and nodules in left temporal lobe of the brain. The histopathological diagnosis of lymph node and spleen was sarcomatoid carcinoma. However, all extensive diagnostic examinations could not detect a site of primary origin. The laboratory data showed marked leukocytosis with increased serum granulocyte colony-stimulating factor (G-CSF). Therefore, the patient was finally diagnosed of CUP of sarcomatoid carcinoma producing G-CSF. After gamma knife treatment for brain metastases, two regimens of taxan-based chemotherapy (carboplatin and paclitaxel, gemcitabine and docetaxel) were administered, with no effect but further tumor progression. Splenectomy for avoiding splenic rupture was performed. As the third line chemotherapy, the combination consisting of doxorubicin and ifosfamide was administered and showed a good therapeutic effect and normalized white blood cell count and serum G-CSF level. He achieved complete remission after three cycles. Herein we present an extremely rare case of CUP of sarcomatoid carcinoma producing G-CSF. Our case suggests the importance of chemotherapy including doxorubicin and ifosfamide, and multimodal therapeutic strategy for this aggressive disease.
Keywords: Cancer of unknown primary origin, Sarcomatoid carcinoma, Granulocyte colony-stimulating factor, Doxorubicin, Ifosfamide
Introduction
Cancer of unknown primary origin (CUP) accounts for 3–5 % of all malignant neoplasms [1]. The prognosis is poor with short median survival of 6–7 months due to refractory to various chemotherapies. About sixty percent of CUP cases are histologically well or moderately differentiated adenocarcinoma [2]. According to our literature survey, sarcomatoid carcinoma as CUP has never been reported. This histological type usually occurs in diverse sites of the body such as lung or colon, which is characterized by an extremely aggressive clinical course. On the other hand, granulocyte colony-stimulating factor (G-CSF) producing cancer is also thought to be detected at an advanced stage associated with an extremely poor prognosis [3, 4]. We describe an extremely rare case of CUP of sarcomatoid carcinoma producing G-CSF, who dramatically responded to the treatment consisting of doxorubicin (DOX) and ifosfamide (IFO).
Case report
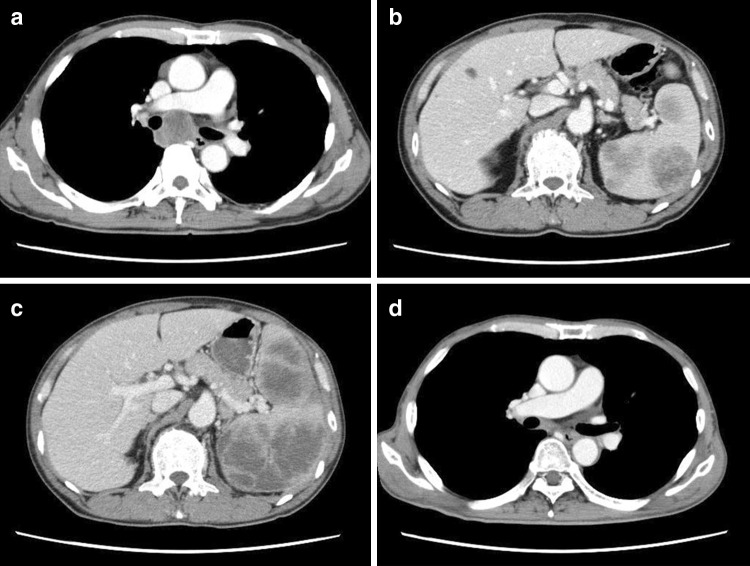
A 59-year-old man visited his primary physician because of hypochondriac pain for more than 1 month. As leukocytosis of 24,000/μl without any signs of infection was observed, he was transferred to our hospital for further medical work-up in May 2013. His past medical history was unremarkable. The only positive finding on his physical examination was mild splenomegaly palpable 2 cm below left costal margin. The laboratory findings were as follows: white blood cell count of 49,900/μl with 84.0 % neutrophils, a red blood cell count of 393 × 104/μl, and a platelet count of 34.4 × 104/μl. C-reactive protein level was 2.7 mg/dl. Serum levels of carcinoembryonic antigen, squamous cell carcinoma antigen, CYFRA and neuron-specific enolase were 2.1 ng/ml (normal range <0.5 ng/ml), 19.4 ng/ml (normal range <1.5 ng/ml), 35.0 ng/ml (normal range <2.0 ng/ml) and 37.9 ng/ml (normal range <16.3 ng/ml), respectively. A bone marrow examination revealed a hypercellular marrow with a marked predominance of myeloid cells. No apparent infiltration of abnormal cells was detected in his bone marrow by microscopic examination and flow cytometry, and chromosome analysis (G-band) showed a normal male karyotype. Computed tomography (CT) scan of the whole body revealed enlarged lymph nodes in the right supraclavicular fossae and mediastinum, and splenomegaly with multiple masses (Fig. 1a, b). A fluorodeoxyglucose/positron emission tomography (FDG/PET) scan revealed uptake in many enlarged lymph nodes, tumor site in spleen and the 4th lumbar vertebra (Fig. 2a). Brain magnetic resonance imaging (MRI) revealed brain metastasis in the left temporal lobe. But these extensive diagnostic examinations above were not able to detect a primary site of the lesion. The histopathological examination of mediastinal lymphadenopathy showed proliferation of atypical large cells (Fig. 3a). These tumor cells were polygonal, ovoid, or spindle-like shape and had large irregular-shaped nuclei with prominent nucleoli. Giant cells with bizarre nuclei and multiple nuclei were also observed. These findings indicated the features of sarcomatoid carcinoma. Immunohistochemically, tumor cells were positive for pan-cytokeratin (AE1/AE3), cytokeratin 7 and vimentin (Fig. 3b, c), and were negative for cytokeratin 20, TTF-1, synaptophysin, and chromogranin A, CD3, CD20, and HMB45. In addition, from the results of elevation of number of neutrophils and no obvious focuses of infection, we suspected that this tumor produced G-CSF. The serum level was elevated up to 584 pg/ml (normal range <30 pg/ml) and immunohistochemical examination showed positive staining for G-CSF in the cytoplasm of the tumour cells (Fig. 3d). On the basis of all above findings, he was diagnosed of CUP of sarcomatoid carcinoma producing G-CSF.
Fig. 1.
Radiological findings. Computed tomography (CT) images on admission showing mediastinal lymphadenopathy (a) and multiple masses in the spleen (b). CT image after carboplatin and paclitaxel chemotherapy showing marked progression of splenomegaly (c). CT image after doxorubicin and ifosfamide chemotherapy showing disappearance of mediastinal lymphadenopathy (d)
Fig. 2.

Fluorodeoxyglucose/positron emission tomography (FDG/PET) imagings. FDG/PET scan before treatment shows increased uptake of FDG in many lymphadenopathy (maximum standardized uptake value, SUVmax, is 16.3), tumor sites in spleen and throughout the bone marrow (a). After doxorubicin and ifosfamide chemotherapy, FDG/PET scan shows markedly decreased FDG uptake (b)
Fig. 3.
Histological findings of the biopsy specimens (objective magnification, ×20). Hematoxylin and eosin staining shows polygonal, ovoid, or spindle-like tumor cells including large irregular-shaped nuclei with prominent nucleoli (a). Immunohistochemical stainings show positivity for pan-cytokeratin (AE1/AE3) (b), vimentin (c) and G-CSF (d)
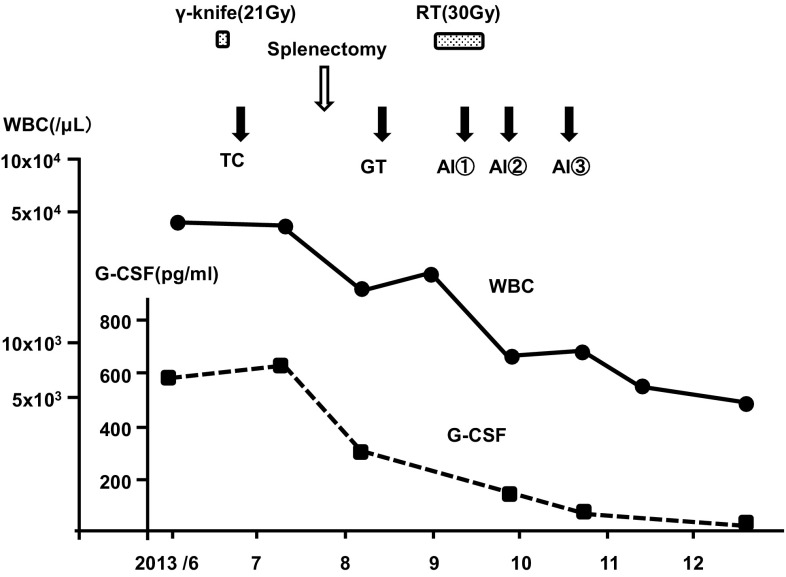
Initially, he was treated with gamma knife of 21 Gy for brain metastases found in the left temporal lobe. Then he underwent TC regimen consisting of carboplatin (AUC: 6, on day 1) and paclitaxel (200 mg/m2, on day 1). However, he had severe left hypochondriac pain after one cycle TC regimen and CT scan showed marked progression of splenomegaly (Fig. 1c). He underwent splenectomy for avoiding splenic rupture. As shown in Fig. 4, his white blood cell count and serum level of G-CSF after splenectomy had decreased from 42,500 to 19,300/μl, and from 698 to 347 pg/ml, respectively. As the 2nd line chemotherapy, a combination of gemcitabine (900 mg/m2, on days 1 and 8) and docetaxel (75 mg/m2, on day 8) therapy (GT regimen) was administered, with no effect but further lower back pain due to tumor progression. He was treated with radiation therapy of 30 Gy to the 4th lumbar vertebra. As he strongly hoped for further chemotherapy and his performance status was 1, a combination chemotherapy consisting of DOX (30 mg/m2, days 1–2) and IFO (2 g/m2, days 1–3) (AI regimen) was started as the third line. His tumor dramatically regressed during short time, and CT scan and FDG/PET scan showed that he achieved a complete remission (CR) after three cycles of AI regimen (Fig. 1d, b). His white blood cell count and the level of G-CSF were decreased to 4,900/μl, and to the normal range, namely, 22.0 pg/ml, respectively (Fig. 4). He lived his daily life, being followed up alive in state of CR, in April 2014.
Fig. 4.
Clinical course and changes in white blood cell (WBC) count and level of granulocyte colony-stimulating factor (G-CSF). The WBC count and the level of G-CSF decreased to the normal range after treatment with AI regimen. (G-CSF normal range: <30 pg/ml) RT radiation therapy, TC carboplatin and paclitaxel regimen, GT gemcitabine and docetaxel regimen, AI doxorubicin and ifosfamide regimen
Discussion
To our knowledge, this is the first report of sarcomatoid carcinoma producing G-CSF defined as CUP with successful result of DOX and IFO chemotherapy. Sarcomatoid carcinoma has been reported in a variety of organs and an extremely rare clinical entity. It is histologically characterized by a combination of carcinomous and sarcomatous components. In general, the prognosis is poor [5–7]. Recently, GT regimen has been evaluated in a variety of malignancies such as non-small lung cancer or soft tissue sarcoma (STS) [8, 9]. The tumors had sarcomatous components and we presumed that GT regimen might yield clinical benefit. Therefore, we used GT regimen as second-line chemotherapy after TC regimen that is known to be active in the treatment for patients with CUP. These combination regimens unfortunately had not responded and tumor progressed. Lee et al. [10] described that MAID regimen (mesna, DOX, IFO and dacarbazine) which was established for the treatment of advanced STS might be an active combination for pleomorphic carcinoma/sarcomatoid carcinoma. But MAID regimen has more side-effects such as severe myelosuppression or chemotherapy-induced nausea/vomiting than AI regimen (DOX and IFO). Given that the aim of 3rd line chemotherapy was palliation for our patient, it was of major importance that drug side-effects did not overweigh the potential benefits of chemotherapy. DOX and IFO remain the backbone of chemotherapy in patients with STS [11], therefore, we chose AI regimen. Our case and Lee’s report may indicate that the anticancer drugs of DOX and IFO have an important role in the treatment of sarcomatoid carcinoma. For high-grade STS a randomized Phase II/III trial of chemotherapy with AI regimen versus GT regimen was recently planned by Japan Clinical Oncology Group Study (JCOG) [12]. Therefore, such a clinical study like Phase I/II trial of AI regimen may be carried out for sarcomatoid carcinoma referring to this JCOG trial.
In addition, important characteristic of the present case was that the tumor produced G-CSF. Many G-CSF producing tumors are generally considered to be biologically highly malignant due to autocrine and/or paracrine mechanism [13]. Therefore, early diagnosis and multimodal therapy are needed. In the present case, splenectomy was performed after only one cycle chemotherapy, thereby leading to the later treatment.
In conclusion, multimodal therapy with carefully selected chemotherapy, radiation therapy and surgery may produce good outcome.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Fizazi K, Greco FA, Pavlidis N, et al. Cancer of unknown primary site. ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2011;22((Supplement 6)):vi64–vi68. doi: 10.1093/annonc/mdr389. [DOI] [PubMed] [Google Scholar]
- 2.Pavlidis N, Pentheroudakis G. Cancer of unknown primary site. Lancet. 2012;379:1428–1435. doi: 10.1016/S0140-6736(11)61178-1. [DOI] [PubMed] [Google Scholar]
- 3.Yamano T, Morii E, Ikeda J, et al. Granulocyte colony-stimulating factor production and rapid progression of gastric cancer after histological change in the tumor. Jpn J Clin Oncol. 2007;37:793–796. doi: 10.1093/jjco/hym094. [DOI] [PubMed] [Google Scholar]
- 4.Kawaguchi M, Asada Y, Terada T, et al. Aggressive recurrence of cancer as a granulocyte-colony-stimulating factor-producing tumor. Int J Clin Oncol. 2010;15:191–195. doi: 10.1007/s10147-010-0023-3. [DOI] [PubMed] [Google Scholar]
- 5.Bae HM, Min HS, Lee SH, et al. Palliative chemotherapy for pulmonary pleomorphic carcinoma. Lung Cancer. 2007;58:112–115. doi: 10.1016/j.lungcan.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Hong JY, Choi MK, Uhm JE, et al. The role of palliative chemotherapy for advanced pulmonary pleomorphic carcinoma. Med Oncol. 2009;26:287–291. doi: 10.1007/s12032-008-9117-4. [DOI] [PubMed] [Google Scholar]
- 7.Sato S, Koike T, Yamato Y, et al. A case of rapid growing pulmonary carcinosarcoma. Int J Clin Oncol. 2010;15:319–324. doi: 10.1007/s10147-010-0043-z. [DOI] [PubMed] [Google Scholar]
- 8.Georgoulias V, Kouroussis C, Androulakis N, et al. Front-line treatment of advanced non-small cell lung cancer with docetaxel and gemcitabine: a multicenter phase II trial. J Clin Oncol. 1999;17:914–920. doi: 10.1200/JCO.1999.17.3.914. [DOI] [PubMed] [Google Scholar]
- 9.Hensley ML, Maki R, Venkatraman E, et al. Gemcitabine and docetaxel in patients with unresectable leiomyosarcoma: results of a phase II trial. J Clin Oncol. 2002;20:2824–2831. doi: 10.1200/JCO.2002.11.050. [DOI] [PubMed] [Google Scholar]
- 10.Lee KW, Kim YJ, Kim JH, et al. Two consective cases of platinum-refractory pulmonary pleomorphic carcinoma that showed dramatic responses to MAID (Mesna, Doxorubicin, Ifosfamide and Dacarbazine) chemotherapy. Jpn J Clin Oncol. 2011;41:430–433. doi: 10.1093/jjco/hyq180. [DOI] [PubMed] [Google Scholar]
- 11.Worden FP, Taylor JMG, Biermann JS, et al. Randomized phase II evaluation of 6 g/m2 of ifosfamide plus Doxorubicin and granulocyte colony-stimulating factor (G-CSF) compared with 12 g/m2 of ifosfamide plus doxorubicin and G-CSF in the treatment of poor-prognosis soft tissue sarcoma. J Clin Oncol. 2005;23:105–112. doi: 10.1200/JCO.2005.05.108. [DOI] [PubMed] [Google Scholar]
- 12.Kataoka K, Tanaka K, Mizusawa J, et al. A randomized phase II/III trial of perioperative chemotherapy with adriamycin plus ifosfamide versus gemcitabine plus docetaxel for high-grade soft tissue sarcoma: Japan Clinical Oncology Group Study JCOG1306. Jpn J Clin Oncol. 2014;44:765–769. doi: 10.1093/jjco/hyu080. [DOI] [PubMed] [Google Scholar]
- 13.Obermueller E, Vosseler S, Fusenig NE, et al. Cooperative autocrine and paracrine functions of granulocyte colony-stimulating factor and granulocyte-macrophage colony-stimulating factor in the progression of skin carcinoma cells. Cancer Res. 2004;64:7801–7812. doi: 10.1158/0008-5472.CAN-03-3301. [DOI] [PubMed] [Google Scholar]