Abstract
Squamous cell carcinoma of the prostate is a rare tumor. It has been typically described as an aggressive cancer, with a median survival time of 14 months. We present a case of locally advanced squamous cell carcinoma of the prostate with a regional lymph node metastasis. The patient received a novel combination chemotherapy regimen, docetaxel, cisplatin, and 5-fluorouracil, with radiotherapy to the whole pelvis and prostate. He was subsequently treated with seven courses of docetaxel, cisplatin, and 5-fluorouracil chemotherapy without any severe adverse events. We identified a 60.1 % reduction in the prostatic tumor, and the lymph node metastasis was shrunk after chemotherapy. A needle biopsy of the prostate after chemotherapy revealed no malignancy. No recurrence has been observed for 24 months. A combination of docetaxel, cisplatin, and 5-fluorouracil chemotherapy and radiotherapy might be an effective therapy for squamous cell carcinoma of the prostate.
Keywords: Squamous cell carcinoma, Prostate, Docetaxel, Cisplatin, Fluorouracil
Introduction
Squamous cell carcinoma (SCC) of the prostate is a rare tumor, and accounts for 0.5–1 % of all prostate carcinomas [1]. Therefore, information regarding clinical presentation, diagnostic workup, treatment, and prognosis has been gathered via anecdotal descriptions. Presenting symptoms can range from lower urinary tract symptoms (i.e., obstructive) to bony metastases. It has typically been described as an aggressive cancer, with a median post-diagnosis survival of approximately 14 months [2]. No definitive treatment exists, although various approaches, including surgical intervention, multimodal chemotherapy, and radiation therapy have been implemented without durable response. We report on a patient with the SCC of the prostate that responded well to a novel combination chemotherapy and radiotherapy. At the 24-month follow-up, the patient has not any evidence of recurrence.
Case report
A 55-year-old man visited our hospital with a chief complaint of micturition pain and macrohematuria. He had been treated with an alpha-1 blocker due to a benign prostatic hyperplasia diagnosis several months prior. The surface of the prostate was irregular on rectal examination. An abdominal ultrasound showed prostate enlargement, with an estimated prostate size of 84.4 cc. Urinalysis revealed pyuria, and urinary cytology revealed SCC. Cystoscopy and urethroscpy showed no malignant mass within the bladder and the urethra. Although the prostate-specific antigen (PSA) was within normal range (0.31 ng/mL), we performed a prostate needle biopsy. The histological examination demonstrated nests and sheets of moderately differentiated squamous carcinomatous cells characterized by intercellular bridges (Fig. 1). There were focal areas with the evidence of individual keratinization. No squamous metaplasia, transitional cell, or adenocarcinomatous components were observed. Plasma SCC was 25.7 ng/mL (normal: <1.5 ng/mL). Computed tomography (CT) showed an irregularly enlarged prostate, compressing the base of the bladder and disrupting the prostatic anatomy. We also detected an enlarged lymph node of the left obturator nerve. On T2 weighted magnetic resonance imaging (MRI), prostate tumor showed heterogeneous with high signal intensity. On dynamic contrast-enhanced MRI, prostate tumor showed increased vascularity on the peripheral lesion, on the other hand decreased vascularity on the inside lesion which suggested necrosis of the cancer. On FDG-PET/CT, SUV max was 29.3 in prostate tumor and 8.9 in the enlarged lymph node of the left obturator nerve. We diagnosed the patient with the primary SCC of the prostate (cT3bN1M0). The patient received chemotherapy consisting of seven cycles of DCF chemotherapy (5-fluorouracil 600 mg/m2 of body-surface area per day administered as a continuous 24-h infusion for days 1–5, docetaxel 50 mg/m2 on day 2, followed by intravenous cisplatin 60 mg/m2 on day 2, every 4 weeks) combined with external beam radiotherapy (total: 64 Gy) to the whole pelvis and prostate. He tolerated the chemotherapy and radiotherapy well. A significant reduction of the prostate tumor (Fig. 2a, b) and the lymph node (Fig. 3a, b) was detected, and the plasma SCC became normal after chemo-radiotherapy. A subsequent prostate biopsy revealed no malignancy. This patient did not hope to receive prostatectomy. Therefore, we are checking urine cytology, enhanced CT, and plasma SCC every 3 months. At the 24-month follow-up, he had no evidence of the disease.
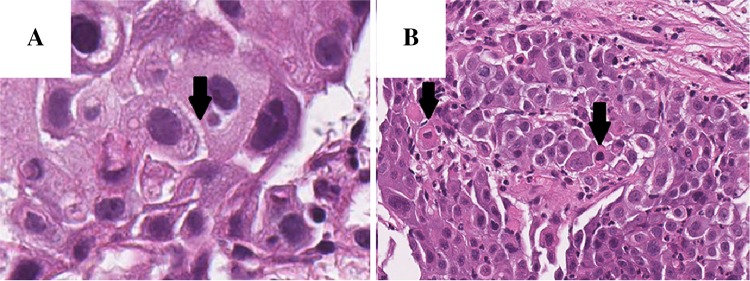
Fig. 1.
Histological finding of the prostate tissue revealed well-differentiated squamous cell carcinoma with intracytoplasmic keratinization, clearly defined intercellular bridges (a), and individual keratinization (b). Hematoxylin and eosin stain
Fig. 2.
Pelvic CT image showed an irregularly enlarged prostate, compressing the base of the bladder and disrupting the prostatic anatomy before therapy (a). After seven cycles of DCF chemotherapy with radiotherapy, the prostate tumor had shrunk (b)
Fig. 3.
Enlarged lymph node of the left obturator nerve was detected before chemo-radiotherapy (a). Significant reduction of the lymph node was observed after chemo-radiotherapy (b)
Discussion
The primary SCC of the prostate is a rare pathological entity. It appears to be a highly aggressive tumor with a poor long-term outcome. As for clinical markers, the squamous variant typically does not result in elevated levels of PAP or PSA. In addition, bone metastases have an osteolytic appearance rather than the osteoblastic appearance seen in adenocarcinoma.1 In a review of the scientific literature, patients with the SCC of the prostate ranged in age from 42 to 85 years with presenting symptoms, including LUTS, acute urinary retention, and urinary tract infection [3]. In the past, various therapeutic modalities, including surgery, hormonal therapy, and irradiation, have proven to be ineffective in treating this malignancy [4]. However, new chemotherapeutic agents used alone or in combination with surgical and/or radiation therapies have recently demonstrated some promise in the treatment of the SCC of the prostate. Several drugs have been employed, mainly based on the experience with epithelial tumors located at other anatomical sites, such as the head and neck, esophagus, and lung.
Several reports have indicated that combination chemotherapy based on cisplatin and radiation may be effective on the SCC of the prostate. Munoz and colleagues showed a 60-month survival using a multimodal approach in a patient presenting with extracapsular disease. Their patient underwent three courses of chemotherapy with cisplatin (CDDP; 75 mg/m2) on day 1 and continuous infusion with 5-fluorouracil (5-FU; 750 mg/m2) on days 1–5. This was followed by a full course of radiation therapy using a linear accelerator (19 MV photons) with a conventional four-field box technique up to 46 Gy to the pelvis with a 20 Gy boost dose to the prostate bed and 6 Gy to the prostate gland [5]. Another promising outcome using multimodal therapy from Uchibayashi and coauthors resulted in a 21-month survival in a patient with organ-confined disease. This patient received 54 Gy of radiotherapy to his pelvis and intravenous (IV) administration of bleomycin (45 mg) with intra-arterial administration of cisplatin [6]. Okada et al. treated a patient with T3N1M0 disease with 50 Gy LINAC radiation to the pelvis, and a boost to the prostate 10 Gy along with two cycles of chemotherapy (IV injection of peplomycin, 15 mg, weekly up to 150 mg, and CDDP, 80 mg/m2, every fourth week) [7]. However, no definitive chemotherapy regimen for prostate SCC has not been established.
Recently, it has been reported that the docetaxel, cisplatin, and 5-fluorouracil (DCF) therapy extended survival as compared with that by the standard CF therapy for head and neck cancer [8]. We expected a similar equivalent curative effect on the SCC of the prostate, and planned a combination of DCF chemotherapy with radiotherapy to the whole pelvis and prostate. Since a previous study reported that combined docetaxel with CDDP chemotherapy (75 mg/m2 docetaxel and 75 mg/m2 cisplatin every 3 weeks) for androgen-independent prostate cancer caused severe (grade 3–4) neutropenia and severe nonhematological toxicities, including vomiting, diarrhea, neuropathy, and fatigue [9], our regimen reduced the concentration of docetaxel and CDDP with a dosage interval of 4 weeks. Our patient only had Grade 2 neutropenia and anorexia.
To our knowledge, the use of combined docetaxel, cisplatin, and 5-FU to treat the SCC of the prostate has not been previously reported. Based on the good response rate and excellent tolerance of this regimen in our patient, further investigation using DCF chemotherapy should be undertaken. Our case has suggested that a combination of chemotherapy consisting of DCF and radiation may be an effective treatment for the SCC of the prostate.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
References
- 1.Mott LJ. Squamous cell carcinoma of the prostate: report of 2 cases and review of the literature. J Urol. 1979;121:833–835. doi: 10.1016/s0022-5347(17)57013-5. [DOI] [PubMed] [Google Scholar]
- 2.Moskovitz B, Munichor M, Bolkier M, et al. Squamous cell carcinoma of the prostate. Urol Int. 1993;51:181–183. doi: 10.1159/000282540. [DOI] [PubMed] [Google Scholar]
- 3.Malik RD, Dakwar G, Hardee ME, et al. Squamous cell carcinoma of the prostate. Rev Urol. 2011;13:56–60. [PMC free article] [PubMed] [Google Scholar]
- 4.Sarma DP, Weilbaecher TG, Moon TD. Squamous cell carcinoma of prostate. Urology. 1991;37:260–262. doi: 10.1016/0090-4295(91)80299-M. [DOI] [PubMed] [Google Scholar]
- 5.Munoz F, Franco P, Ciammella P, et al. Squamous cell carcinoma of the prostate: long-term survival after combined chemo-radiation. Radiat Oncol. 2007;2:15. doi: 10.1186/1748-717X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uchibayashi T, Hisazumi H, Hasegawa M, et al. Squamous cell carcinoma of the prostate. Scand J Urol Nephrol. 1997;31:223–224. doi: 10.3109/00365599709070338. [DOI] [PubMed] [Google Scholar]
- 7.Okada E, Kamizaki H. Primary squamous cell carcinoma of the prostate. Int J Urol. 2000;7:347–350. doi: 10.1046/j.1442-2042.2000.00204.x. [DOI] [PubMed] [Google Scholar]
- 8.Lorch JH, Goloubeva O, Haddad RI, et al. Induction chemotherapy with cisplatin and fluorouracil alone or in combination with docetaxel in locally advanced squamous-cell cancer of the head and neck: long-term results of the TAX 324 randomised phase 3 trial. Lancet Oncol. 2011;12:153–159. doi: 10.1016/S1470-2045(10)70279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Culine S, El-Demery M, Lamy PJ, et al. Docetaxel and cisplatin in patients with metastatic androgen independent prostate cancer and circulating neuroendocrine markers. J Urol. 2007;178:844–848. doi: 10.1016/j.juro.2007.05.044. [DOI] [PubMed] [Google Scholar]