Abstract
Background and aims
The symptom-based diagnostic criteria for irritable bowel syndrome (IBS) have recently been revised in the Rome IV consensus. On the other hand, with rising public awareness of IBS, self-diagnosis and self-management is also increasing. We compared the prevalence and impact of Rome IV-based IBS vs self-diagnosed IBS in the general population.
Methods
An internet panel filled out an online survey on bowel symptoms and their impact on health care utilization and daily activities.
Results
A representative internet panel of 1012 individuals completed the online survey. Bowel symptoms were present in 68.6% of the population. Of these, 21% consulted a physician for these symptoms in the last year and 42% earlier. Rome IV IBS criteria were fulfilled by 5.5%, and these were younger and more likely to be female. In this subset, 37% had consulted a physician for IBS symptoms in the preceding year and 29% had done so earlier. A colonoscopy had been performed in 22%. Based on a brief description, 17.6% of the population self-identified as suffering from IBS (p < 0.001 compared to Rome IV IBS prevalence), and these were more likely to be female. Concordance with the Rome IV criteria was only 25%, but except for a lower reporting of pain, the symptom pattern, severity, impact on daily life, inability to work and health care utilization were similar to the Rome IV group. A total of 134 days of absence from work were attributed to bowel symptoms in those self-reporting with IBS.
Conclusion
In the general population, bowel symptoms are highly prevalent, and the self-reported “IBS” is three times more prevalent than according to Rome IV criteria. Self-reported IBS is associated with a similar impact on health care utilization and quality of life but a higher impact on absence from work.
Keywords: Epidemiology, health care resource utilization, irritable bowel syndrome, medication use, sick leave
Key summary
The Rome criteria for diagnosing irritable bowel syndrome (IBS) were recently updated in the Rome IV consensus.
The epidemiology of Rome IV-diagnosed IBS compared to self-reported IBS is unknown.
In the general population, self-reported IBS was three times more prevalent than IBS by Rome IV criteria.
The impact of self-reported IBS was at least comparable to that of Rome IV IBS, suggesting that these criteria may be too restrictive.
Introduction
Irritable bowel syndrome (IBS) is a functional gastrointestinal condition characterized by the association of abdominal pain or discomfort with changes in stool frequency or consistency, in the absence of organic disease explaining the symptoms.1–5IBS is a major cause of visits to general practitioners, gastroenterologists and internists. Because it has considerable socioeconomic consequences, knowledge of its prevalence and impact is important for health care planning in each country.
As IBS is a condition without diagnostic or monitoring biomarkers, patients’ symptom reporting is essential for making a diagnosis. Several symptom-based diagnostic criteria have been proposed to diagnose IBS. The first were the Manning criteria, named after the first author of the study demonstrating that abdominal pain relief by bowel movements, change of stool form and frequency with onset of pain, and visible and feeling of abdominal distension were more common in IBS as compared to organic patients.1These were soon followed by the Rome criteria, which were based on a consensus by a group of experts.2–4The Rome III criteria were published in 2006 and defined IBS as the presence of pain or discomfort in the lower abdomen, associated with (altered) defecation, present for more than six months, and not explained by underlying organic disease.4Most recently, the Rome IV criteria required pain and did not consider discomfort as sufficient for diagnosing IBS.5
Previous studies have reported a prevalence of IBS ranging between 3% and 22% in the community with wide variations between countries.6It has been argued that the large variations in IBS prevalence across studies are due to the use of different diagnostic criteria.6,7Only one previous study, using the Rome II criteria and a telephone survey, has reported on the prevalence of IBS in the general population in Belgium.8
In primary care, where most patients with IBS are diagnosed and managed, physicians rarely use the Rome criteria.9,10Instead, they use a simple definition, based on the longstanding presence of abdominal pain or discomfort associated with altered bowel habits.9,10Awareness of bowel symptoms and IBS in the public have increased steadily over time through activities such as World IBS Day, articles in the lay press, appearance in movies and interest in dietary measures, among others.11–13
The aim of the present study was to evaluate the prevalence of bowel symptoms, IBS according to the Rome IV criteria and self-reported IBS symptoms in the Belgian general population. A second aim was to evaluate in the same population the personal and health economic impact of these conditions.
Methods
Internet survey methodology
The study used an internet survey (Medistrat internet panel) to collect information of bowel symptoms and their impact in a sample representative of the entire population. This completely anonymous survey was conducted in adults older than 18 years in Dutch and French. The panel was chosen to reflect the composition of the Belgian adult population in terms of province they lived in, age distribution, level of education and employment status. However, the survey was prespecified to recruit a majority of females (62%), taking into account the known imbalance in IBS prevalence with a female majority.6–8The quotum of the filled out questionnaires was intended to match the Belgian population composition. When the profile of a potential participant was completed, this participant no longer had access to the survey. Individuals were given an incentive of being entered in a drawing with the chance of winning a gift voucher. The study was supported by a grant from Menarini Belgium, which otherwise had no input into the study conduct, data analysis and reporting. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki. As this is a fully anonymized internet survey, no ethical approval was needed in agreement with local legislation.
The bowel symptom and impact questionnaire
The questionnaire comprised a part concerning the personal profile of participants (sex, age, weight, height, education, occupation) and a section with specific questions about presence of bowel symptoms, reflecting the Rome IV definitions and criteria. When bowel symptoms were present, the questionnaire asked details about their frequency and their impact, including absence from work, use of medications, doctor consultations and medical examinations. Based on a short description of IBS, resembling the definition used by general practitioners and clinicians (simple definition, based on the long-standing presence of abdominal pain or discomfort associated with altered bowel habits), participants could self-report IBS, and a next section asked those with self-reported IBS questions about bothersomeness of symptoms, lifestyle adjustments, treatment and their perceived efficacy. A final section asked all participants, with and without a diagnosis of IBS, about their knowledge of IBS and the disease perception.
Data collection and analysis
The internet data collection was conducted over the course of a single month. For the data referring to the whole population, prevalence rates were recalculated to reflect the country’s sex distribution (https://www.belgium.be/en/about_belgium/country/Population). The prevalence of gastrointestinal symptoms was assessed, as was the prevalence of self-reported IBS. In the latter subgroup, the concordance with (modified) Rome IV and Rome III criteria was determined, and the pattern and impact of symptoms were compared in the group that did and did not fulfill Rome criteria. Data are presented as mean ± SEM.
Results
Demographic profile of participants
A total of 1012 individuals (mean age of 45.2 ± 0.5 years, 62% female, body mass index of 26.00 ± 0.16 per kg/m2) completed the online survey. Demographic data are summarized in Table 1. The composition of the group matched the population distribution in the Belgian provinces and in terms of educational level and employment status (Table 1), except for the female predominance (62%).
Table 1.
Demographic characteristics of the survey population.
| Sex: female/male | 62%/38% |
|---|---|
| Age range in years | |
| <30 | 20% |
| 30–39 | 28% |
| 40–49 | 24% |
| 50–59 | 17% |
| 60 and older | 21% |
| Composition per province | |
| West Flanders + East Flanders | 27% |
| Antwerp + Limburg | 27% |
| Vlaams Brabant | 6% |
| Brusses + Brabant Wallon | 12% |
| Hainaut + Namur | 16% |
| Liège + Luxembourg | 12% |
| Professional activity | |
| White collar worker | 42% |
| Retired | 20% |
| Blue collar | 11% |
| Unemployed | 8% |
| Houseman/-woman | 7% |
| Student | 5% |
| Self-employed | 1% |
| Other | 6% |
| Education level | |
| Primary school | 6% |
| Lower secondary school | 17% |
| Higher secondary school | 21% |
| Lower technical school | 5% |
| Higher technical school | 14% |
| Higher education outside university | 26% |
| University education | 11% |
Bowel symptoms
Prevalence and type of symptoms
After correction for gender balance, the occurrence of at least one bowel symptom in the previous 12 months was reported by 68.6% of the population (58.7% of the men, and 78.3% of the women, p < 0.0001), and those reporting bowel symptoms were younger (43.2 ± 0.6 vs 50.2 ± 0.9 years, p < 0.001).
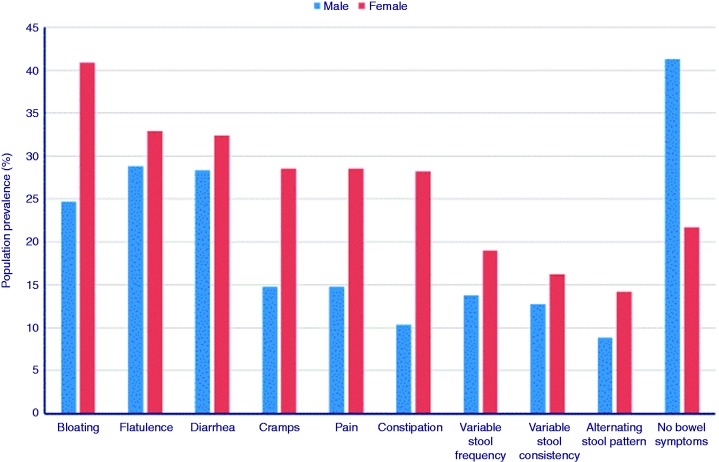
On average, 2.1 ± 0.1 symptoms were reported per participant. Of these, bloating, diarrhea, flatulence, abdominal cramps, pain and constipation were the most frequently reported, with markedly higher prevalence in women for most symptoms (Figure 1). Of the participants reporting at least one symptom, 77.2% reported that the symptoms improved with defecation or evacuation of gas.
Figure 1.
Prevalence of bowel symptoms as reported by the general population in men and women.
Of participants with bowel symptoms, 56.3% and 36.4% respectively reported symptom occurrence at least three days per month or at least one day per week in the last three months.4,5,14Twelve percent reported that symptom occurrence was daily.
Impact of bowel symptoms on daily life and health care utilization
Individuals reporting bowel symptoms were more likely to be working (53.4% vs 43.7%, p = 0.006) and less likely to be retired (15.0% vs 30.5%, p < 0.001). Of the participants with at least one bowel symptom who were working or studying, 13.4% reported absence from work because of these symptoms over the last year. Twenty-one percent of participants reporting at least one symptom consulted a medical doctor for these symptoms during the preceding 12 months. This was the general practitioner in 82% of cases and one or more specialists in 32% of cases, with a mean of 2.6 ± 0.4 consultations per individual. Of the participants with at least one bowel symptom, 28.2% and 44.3% respectively reported undergoing a colonoscopy or radiological examination because of their bowel symptoms in the last 12 months.
Of those with symptoms not consulting a physician over the last 12 months, 41% had consulted a physician for these symptoms in the past. Of those with symptoms who had never consulted a physician, 26% indicated that the symptoms were not severe enough, 21% reported spontaneous disappearance of the symptoms and 13% indicated they had identified the cause (food, stress, menstruation, etc.).
Diagnosis in case of medical consulting
The participants who consulted a medical doctor received a diagnosis suggestive of bowel disease in 28% (IBS 8%, diverticular disease 3%, hypersensitive intestine, hypoactive intestine, intestinal colic, long intestine, … ). Other diagnoses were made in 12% of the participants, including Crohn disease (n = 5) and intestinal cancer (n = 2). Forty-two percent of those consulting a physician for bowel symptoms did not receive a clear diagnosis.
Disease perception of IBS
Forty-eight percent of the 1012 participants were familiar with the term “irritable bowel syndrome” or related terms used in clinical practice such as “spastic colon” or “nervous colon,” and of these 27% defined themselves as being affected by this disorder (see below). Of the participants, 39% were aware of IBS symptoms (pain, cramps, disordered bowel habit, and so on), while 22% had no concept of IBS. Eighteen percent attributed IBS symptoms to stress, 11% to food and 8% to a sensitive bowel.
Seventy-eight percent of participants considered “irritable bowel syndrome” a true disease; paradoxically this was only 56% in those who defined themselves as suffering from this disorder (see below). Fifty-one percent of participants considered “irritable bowel syndrome” as severe or quite severe, while 37% considered it “not really severe.”
IBS according to the Rome IV criteria
After correction for gender balance, 5.5% of the Belgian population fulfilled the Rome IV diagnostic criteria for IBS (Table 2). Those with Rome IV IBS tended to be female (7.0% of women vs 3.9% of men, p = 0.05) and younger (42.4 ± 1.9 vs 45.4 ± 0.5 years), but the latter did not reach significance (p = 0.1). In these Rome IV IBS participants, diarrhea was present in 37%, constipation in 34% and alternating stool pattern in 28%. Figure 2summarizes the symptom prevalence in individuals fulfilling the Rome IV IBS criteria. Daily occurrence of symptoms was reported by 37% of these participants. Sixty-three percent of these individuals were employed, and only 8% reported absence from work because of IBS symptoms, leading to only 14 days of absence from work because of bowel symptoms in those fulfilling Rome IV criteria.
Table 2.
Comparison between patients fulfilling Rome IV criteria and the self-reported irritable bowel syndrome (IBS) group.
| IBS according to Rome IV | Self-reported IBS | |
|---|---|---|
| Prevalence | 5.5% | 17.6% |
| Employment state: | ||
| Employed | 63% | 45% |
| Symptoms | ||
| Diarrhea | 37% | 39% |
| Constipation | 34% | 35% |
| Alternating stool pattern | 28% | 28% |
| Abdominal pain | 100% | 48% |
| Bloating | 74% | 65% |
| Abdominal cramps | 69% | 51% |
| Problems with frequency of bowel symptoms | 49% | 27% |
| Problems with consistency of bowel movements | 37% | 24% |
| Impact of symptoms | ||
| Absence from work | 14 days | 134 days |
| Primary care physician | 27% | 82% |
| A specialist | 15% | 39% |
| Colonoscopy | 12% | 11% |
| Radiological examination | 15% | 14% |
| Associated fatigue | 88% | 83% |
| Irritability | 85% | 83% |
| Insomnia | 65% | 66% |
| Anxiety | 69% | 59% |
| Loss of appetite | 69% | 61% |
| Depressive mood | 54% | 54% |
| Shame | 58% | 48% |
| Staying home from social activities | 54% | 50% |
| Anger | 54% | 40% |
| Medication | ||
| Spasmolytic agents | 39% | 36% |
| Antidiarrheal agents | 11% | 27% |
| Analgesics | 43% | 27% |
| Fiber supplements | 21% | 26% |
| Laxatives | 18% | 21% |
| Anxiolytics | 21% | 10% |
| Antidepressants | 4% | 9% |
| Sleeping pills | 7% | 8% |
| Antinauseants | 11% | 4% |
Figure 2.
Prevalence of symptoms in patients fulfilling Rome IV criteria for irritable bowel syndrome (IBS) and in patients with self-reported IBS according to a simple descriptive definition.
Medication use in patients with IBS according to the Rome IV criteria is summarized in Table 2. Most frequently used were analgesics (43%), followed by spasmolytic agents (39%), anxiolytics (21%), fiber supplements (21%), laxatives (18%) and antidiarrheal agents (11%). Table 3reports the percentage of individuals satisfied by treatments for each class of medications. Participants with IBS according to the Rome IV criteria also adjusted their diet by increasing their intake of fiber (43%) and water (50%) and by decreasing the amount of fat (50%). Twenty-one percent of these individuals consumed smaller meal portions, and only 14% had never tried a dietary restriction to avoid their symptoms. Thirty-seven percent had consulted a physician for their IBS symptoms (27% primary care physician and 15% a specialist) over the last year, with an average of 4.1 ± 2.2 doctor visits per patient. Over the last year, colonoscopy was performed in 12% and radiological examination in 15% of those fulfilling Rome IV IBS. Twenty-nine percent had consulted a physician prior to the last year, 20% their primary care physician and 12% a specialist. Radiology and colonoscopy were performed before the last year each in 10%. Those who visited a physician received a diagnosis of IBS in only 26%, and attribution of symptoms to stress in 18%. In the 34% of individuals fulfilling Rome IV IBS criteria who had not consulted a physician, the main reasons for not doing so were self-management (35%), lack of severity (30%), chronic nature of the symptoms (15%), spontaneous improvement (10%) and pregnancy (one participant).
Figure 3.
Impact of symptoms on daily activities reported by subjects with self-reported “IBS”. The numbers represent the percentage of subjects with self-reported IBS indicating a consequence of their symptoms as “occasional” or “frequent”.
Table 3.
Reported benefit of medication use in individuals with irritable bowel syndrome (IBS) according to Rome IV criteria, self-reported “IBS” and formally diagnosed IBS.
| Proportion reporting good or very good response | Rome IV IBS | Self-reported IBS | Formally diagnosed |
|---|---|---|---|
| Spasmolytics | 81% | 84% | 75% |
| Antidiarrheals | 67% | 89% | 100% |
| Analgesics | 67% | 72% | 69% |
| Fiber supplements | 71% | 77% | 73% |
| Laxatives | 80% | 71% | 71% |
| Anxiolytics | 51% | 65% | 75% |
| Antidepressants | Insufficient data | 60% | 60% |
Self-reported IBS
These data are reported in the online supplement.
Discussion
Although the epidemiology of IBS has been the topic of several studies and reviews, only few data are available for Belgium.6–8In the present paper, we conducted a population-based internet survey of the prevalence and impact of bowel symptoms of IBS according to the Rome IV definition and of self-reported IBS in the Belgian general population.5,9,10,15The present survey used an internet panel that accurately mirrored the composition of the Belgian population in terms of demographic, language, geographic, education and employment characteristics.
As expected, bowel symptoms in the preceding year were extremely prevalent in the general population, with 68.6% of the population reporting such symptoms above the Rome consensus-based threshold over the last year. The prevalence of bowel symptoms was significantly higher in women and was associated with younger age. Most participants reported several coexisting bowel symptoms, and the majority reported experiencing symptoms at least several times per month. Diarrhea was the second most prevalent symptom, and constipation was much less frequently reported. This is at variance with earlier surveys showing similar prevalence of both stool types in the general population.8,9,16
Next, the survey addressed the impact of bowel symptoms in the general population. This part of the study revealed a high health economic impact, with absence from work for bowel symptoms during the last year in 13%, and high rates of doctor visits (21% in the last year and 42% prior to the last year) and additional diagnostic investigations. A surprisingly high proportion of those consulting a physician (42%) did not receive a formal diagnosis. When a diagnosis was given, it indicated functional bowel disorders, especially IBS, in the majority of cases.
In the internet survey, we also determined the prevalence of bowel symptoms in general and IBS, as defined by Rome IV, in Belgium, and the prevalence of self-reported IBS using a clinically used descriptive definition.
Applying the Rome IV criteria, 5.5% of the general population fulfilled IBS diagnostic criteria. This number is comparable to early reports of Rome IV IBS population prevalence studies conducted in the United States, United Kingdom (UK) and Canada.17
The presence of IBS had a relevant impact in terms of ability to work and health care utilization. Reports on individuals with IBS coming to medical attention indicate that the Rome IV criteria select a smaller patient group with more severe severity and impact.14,18In the present general population study, self-reported IBS, largely based on more historical diagnostic criteria, was three times more prevalent (17.6% of the population) and, while it was not dominated by the presence of abdominal pain, was associated with a similar major impact on quality of life, ability to work and health care utilization. This is in line with previous reports of higher prevalence of IBS-like symptoms, with only a proportion of patients fulfilling the duration, frequency and severity criteria that are required to fulfill Rome definitions.9,15This type of simpler definition is probably used in clinical practice, where many patients are diagnosed with IBS who do not fulfill strict criteria.9,11,18The findings suggest that the Rome IV criteria identify IBS patients with pain as a predominant symptom, but those fulfilling older diagnostic criteria, which also takes discomfort into account, seem to be similarly affected. The present study confirmed that the Rome IV definition is more restrictive, as it identified far fewer individuals compared to the self-reported IBS group; however, we did not confirm that those identified by the Rome IV criteria are more severely affected. Whether the more restrictive Rome IV definition identifies a more homogeneous group of patients and improves treatment outcome remains to be determined in outcome studies.
Self-reported IBS sufferers identified both stress and dietary factors as triggers for symptom exacerbations, and this is also in line with previous reports.19,20,26In those self-defining as suffering from “IBS,” the symptoms had a major impact on daily functioning through physical impairment (fatigue, loss of appetite), emotional impairment (anxiety, depression and shame) and inability to work or socialize. Participants with self-reported IBS attributed more anxiety, depression and fatigue to their IBS than those fulfilling the Rome IV criteria, suggesting that this group may have more psychosocial comorbidity. These findings are in line with other patient and population surveys confirming that although benign in nature, the impact of IBS on patients is often major.21,22,27Similar to the Rome IV–positive patients, only a minority had received a formal IBS diagnosis even when they had consulted a physician for their symptoms.
Self-reporting as IBS was associated with a high rate of medication usage (1.6 drugs per participant on average), which was evaluated as having a favorable impact on symptoms by more than 70%. While the rate of medication usage is in line with other surveys, the reported treatment satisfaction is high compared to the often perceived limited impact of traditional treatments on IBS symptoms.23,24Individuals fulfilling Rome IV criteria were most frequently treated with analgesics, whereas self-reported IBS was most frequently treated with spasmolytics and antidiarrheal agents. This treatment profile is in line with the focus of Rome IV on pain as a cardinal symptom.5In addition, 77% of IBS sufferers used dietary adjustments to control symptoms of IBS, but these did not correspond to established dietary interventions for IBS, such as a diet low in fermentable oligo-, di- and polysaccharides and polyols, or the UK’s National Institute for Clinical Excellence IBS diet.24,25Finally, the majority of IBS sufferers and nonsufferers alike in this survey identified IBS as a condition worthy of medical attention and expressed a need for more information regarding this disease.
One of the limitations of the current study is its setup as an online survey that is based on participant self-reporting. Furthermore, these participants received an incentive. On the other hand, this approach allows researchers to reach a big sample size, representative of the general population, in a short period of time. Furthermore, the nature of the aim of the survey (bowel symptoms) was not revealed before participants started filling it out. Owing to the limited number of questions, the survey was short to complete, especially for those without or with only few bowel symptoms.
In summary, an internet-based survey regarding bowel symptoms, the prevalence of IBS according to the Rome IV criteria, and the impact of self-reported IBS was conducted in 1012 members of the Belgian adult population. The occurrence of bowel symptoms was highly prevalent and most of the symptoms were more likely in women and the younger population. Nevertheless, only 5.5% of the population fulfilled the Rome IV IBS diagnostic criteria. After reading the descriptive definition of IBS, 17.6% noted that they suffered from IBS. Those with self-reported IBS reported a similar impact of their symptoms on health care utilization and quality of life and a higher impact on work absence.
Supplemental Material
Supplemental Material for Prevalence and impact of self-reported irritable bowel symptoms in the general population by K Van den Houte, F Carbone, J Pannemans, M Corsetti, B Fischler, H Piessevaux and J Tack in United European Gastroenterology Journal
Declaration of conflicting interests
This study was supported by a grant from Menarini Pharmaceuticals Belgium.
Ethics approval
This study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki. As this is a fully anonymized internet survey, no ethical approval was needed in agreement with local legislation.
Funding
This work was supported by a Methusalem grant from Leuven University to Jan Tack and by a research grant from Menarini Belgium.
Informed consent
Consent was not required as this was an anonymous survey conducted in adults.
References
- 1.Manning AP, Thompson WG, Heaton KW, et al. Towards positive diagnosis of the irritable bowel. Br Med J 1978; 2: 653–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson WG, Creed F, Drossman DA, et al. Functional bowel disorders and chronic functional abdominal pain. Gastroenterol Int 1992; 5: 75–91. [Google Scholar]
- 3.Thompson WG, Longstreth GF, Drossman DA, et al. Functional bowel disorders and functional abdominal pain. Gut 1999; 45(Suppl 2): II43–II47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology 2006; 130: 1480–1491. [DOI] [PubMed] [Google Scholar]
- 5.Lacy B, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology 2016; 150: 1393–1407.e5. [DOI] [PubMed] [Google Scholar]
- 6.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clin Gastroenterol Hepatol 2012; 10: 712–721. [DOI] [PubMed] [Google Scholar]
- 7.Sperber AD, Dumitrascu D, Fukudo S, et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: A Rome Foundation working team literature review. Gut 2017; 66: 1075–1082. [DOI] [PubMed] [Google Scholar]
- 8.Hungin AP, Whorwell PJ, Tack J, et al. The prevalence, patterns and impact of irritable bowel syndrome: An international survey of 40,000 subjects. Aliment Pharmacol Ther 2003; 17: 643–650. [DOI] [PubMed] [Google Scholar]
- 9.Corsetti M, Tack J. Are symptom-based diagnostic criteria for irritable bowel syndrome useful in clinical practice? Digestion 2004; 70: 207–209. [DOI] [PubMed] [Google Scholar]
- 10.Ford A, Moayyedi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol 2009; 104: S1–S35. [DOI] [PubMed] [Google Scholar]
- 11.Hahn BA, Saunders WB, Maier WC. Differences between individuals with self-reported irritable bowel syndrome (IBS) and IBS-like symptoms. Dig Dis Sci 1997; 42: 2585–2590. [DOI] [PubMed] [Google Scholar]
- 12.Sherwin LB. Layperson’s knowledge and perceptions of irritable bowel syndrome as potential barriers to care. J Adv Nurs 2018; 74: 1199–1207. [DOI] [PubMed] [Google Scholar]
- 13.Goodwin L, White PD, Hotopf M, et al. Life course study of the etiology of self-reported irritable bowel syndrome in the 1958 British birth cohort. Psychosom Med 2013; 75: 202–210. [DOI] [PubMed] [Google Scholar]
- 14.Aziz I, Törnblom H, Palsson OS, et al. How the change in IBS criteria from Rome III to Rome IV impacts on clinical characteristics and key pathophysiological factors. Am J Gastroenterol 2018; 113: 1017–1025. [DOI] [PubMed] [Google Scholar]
- 15.Lea R, Hopkins V, Hastleton J, et al. Diagnostic criteria for irritable bowel syndrome: Utility and applicability in clinical practice. Digestion 2004; 70: 210–213. [DOI] [PubMed] [Google Scholar]
- 16.Talley NJ, Zinsmeister AR, Van Dyke C, et al. Epidemiology of colonic symptoms and the irritable bowel syndrome. Gastroenterology 1991; 101: 927–934. [DOI] [PubMed] [Google Scholar]
- 17.Palsson OS, van Tilburg MA, Simrén M, et al. Mo1642 Population prevalence of Rome IV and Rome III irritable bowel syndrome (IBS) in the United States (US), Canada and the United Kingdom (UK). Gastroenterology 2016; 150(Suppl 1): S739–S740. [Google Scholar]
- 18.Vork L, Weerts ZZRM, Mujagic Z, et al. Rome III vs Rome IV criteria for irritable bowel syndrome: A comparison of clinical characteristics in a large cohort study. Neurogastroenterol Motil 2018; 30. [DOI] [PubMed] [Google Scholar]
- 19.O’Mahony SM, Clarke G, Dinan TG, et al. Irritable bowel syndrome and stress-related psychiatric co-morbidities: Focus on early life stress. Handb Exp Pharmacol 2017; 239: 219–246. [DOI] [PubMed] [Google Scholar]
- 20.Eswaran S, Tack J, Chey WD. Food: The forgotten factor in the irritable bowel syndrome. Gastroenterol Clin North Am 2011; 40: 141–162. [DOI] [PubMed] [Google Scholar]
- 21.Tack J, Vanuytsel T, Corsetti M. Modern management of irritable bowel syndrome: More than motility. Dig Dis 2016; 34: 566–573. [DOI] [PubMed] [Google Scholar]
- 22.Moayyedi P, Mearin F, Azpiroz F, et al. Irritable bowel syndrome diagnosis and management: A simplified algorithm for clinical practice. United European Gastroenterol J 2017; 5: 773–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simrén M, Tack J. New treatments and therapeutic targets for IBS and other functional bowel disorders. Nat Rev Gastroenterol Hepatol 2018; 15: 589–605. [DOI] [PubMed] [Google Scholar]
- 24.Halmos EP, Power VA, Shepherd SJ, et al. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology 2014; 146: 67–75. [DOI] [PubMed] [Google Scholar]
- 25.Böhn L, Störsrud S, Liljebo T, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: A randomized controlled trial. Gastroenterology 2015; 149: 1399–1407. [DOI] [PubMed] [Google Scholar]
- 26.Qin HY, Cheng CW, Tang XD, et al. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol 2014; 20: 14126–14131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mönnikes H. Quality of life in patients with irritable bowel syndrome. J Clin Gastroenterol 2011; 45(Suppl): S98–S101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Prevalence and impact of self-reported irritable bowel symptoms in the general population by K Van den Houte, F Carbone, J Pannemans, M Corsetti, B Fischler, H Piessevaux and J Tack in United European Gastroenterology Journal