Abstract
Purpose:
This study describes a novel surgical technique of fibrin glue-assisted retinopexy for rhegmatogenous retinal detachment (GuARD) without oil or gas tamponade after pars plana vitrectomy (PPV).
Methods:
This pilot clinical trial included five eyes of five patients with rhegmatogenous retinal detachments (RD). A complete PPV was done in all cases followed by fluid–air exchange, laser photocoagulation around the break/s, and application of 0.1–0.2 mL of fibrin glue. No air, long-acting gas or silicone oil was used subsequently. No specific postoperative positioning was prescribed. The primary outcome measure was efficacy of the procedure defined as successful anatomical retinal reattachment. Secondary outcome measures were postoperative improvement in best corrected visual acuity (BCVA) and complications.
Results:
The median age of patients was 55 (range: 36–61 years) years and median duration of symptoms was 15 (range: 7–60) days. All eyes were pseudophakic, four eyes had inferior and one eye had total RD. Successful retinal reattachment was achieved in all (100%) cases and was maintained at the end of 3–8 months of follow-up. The median BCVA improved from 20/100 preoperatively to 20/80 at 1-week and 20/50 at 1-month postoperatively. None of the eyes had any postoperative complications such as elevated intraocular pressures or unexpected inflammation.
Conclusion:
The findings of this study suggest that GuARD is a promising technique for treatment of rhegmatogenous RD that may allow early visual recovery while avoiding the problems of gas or oil tamponade and obviating the need of postoperative positioning.
Keywords: Fibrin glue, retinal detachment surgery, rhegmatogenous retinal detachment
The commonly used modalities for management of rhegmatogenous retinal detachments (RD) are scleral buckling (SB), pars plana vitrectomy (PPV), pneumatic retinopexy, or a combination of the above techniques. Recent studies reported a primary retinal reattachment rate of more than 90% in uncomplicated RD with both SB and PPV.[1] The “scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment (SPR) study” showed that PPV had higher anatomical success rates in pseudophakic eyes, whereas SB had better visual improvement rates in phakic eyes.[2] There has been an increase in the popularity of PPV for management of RD in recent years owing to technical advancements in small gauge instrumentations and newer and better wide angled imaging systems.[3,4]
The PPV approach for rhegmatogenous RD repair, however, suffers from a few inherent disadvantages which stem from the necessity for endotamponade with either silicone oil or long-acting gasses. Most importantly, silicone oil and gas tamponade are also associated with complications like secondary glaucoma.[5] The silicone study showed that chronic postoperative elevated intraocular pressure (IOP) was seen in both the gas and silicone oil groups.[5] While removal of silicone oil is associated with an increased risk of redetachment, chronic retention leads to emulsification, increased rate of cataract formation and corneal changes.[6,7,8] Moreover, retinal support with both forms of tamponade is usually insufficient in cases with inferior retinal breaks, even with strict postoperative positioning.[9,10] Proper positioning itself is challenging in the elderly and in patients with spinal disorders and gas tamponades can also lead to restriction in air travel.
In this study, the authors hypothesized that retinal tamponade with long-acting gases or silicone oil and their associated limitations could be circumvented by a temporary tamponading agent localized to the area of the retinal break. Fibrin glue emerged as the likely candidate since its efficacy and safety as an ocular tissue sealant had been established not only in ocular surface procedures, but also in scleral fixation of intraocular lenses and even in surgeries for optic disc pit associated macular detachments.[11,12,13,14,15] This study describes the initial clinical results of a novel surgical technique of fibrin glue-assisted retinopexy for rhegmatogenous retinal detachment (GuARD) that obviates the need for oil or gas tamponade after PPV.
Methods
Study design, duration, location and participants
This was a prospective noncomparative consecutive case series of adult patients with unilateral rhegmatogenous RD who underwent the GuARD procedure between 1st March to 12th September 2018. The study was prospectively approved by the institutional review board and informed written consent was obtained from all patients and the study adhered to the tenets of Declaration of Helsinki. All patients underwent a comprehensive ophthalmic examination and the following exclusion criteria were applied before selecting patients for this novel procedure: a) children b) cases with: any previous retinal surgery, giant retinal tears, proliferative vitreoretinopathy (PVR) grade C or more, associated vitreous hemorrhage, associated choroidal detachment, associated with retinal breaks in multiple quadrants and macular holes.
Surgical technique
All the surgeries were performed under local anesthesia by a single surgeon (MT) with a vitrectomy system (Constellation, Alcon Laboratories Inc., Fort Worth, TX, USA) and a noncontact wide viewing system (Resight 700, Carl Zeiss Meditec AG, Jena, Germany). A standard 25-gauge meticulous and complete PPV was done and no vitreous was left adherent at the site of the retinal breaks. This was followed by a fluid–air exchange and subretinal fluid was removed to reattach the retina using a flute needle and to ensure that the surface of the retina was completely dry. The retinal breaks were treated with laser photocoagulation. Using a 1 mL syringe 0.1 to 0.2 mL of fibrin glue (TISSEEL Kit, Baxter AG, Vienna, Austria) was then slowly injected over the retinal breaks [Fig. 1] to cover them. After waiting for 5 min, to allow the glue to form a thick fibrin clot which covered the retinal break, the air was removed from the globe and exchanged with balanced salt solution (Surgical Video, Supplementary Information). No migration or displacement of glue was noted at the end of the procedure. Neither was air, long-standing gas, or silicone oil tamponade used nor were patients instructed to observe any specific postoperative head positioning.
Figure 1.
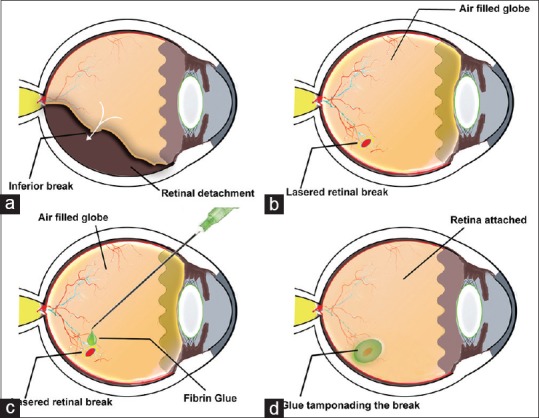
Schematic representation of the surgical technique of glue-assisted retinopexy for rhegmatogenous retinal detachments (GuARD). (a) Representative depiction of inferior retinal detachment with inferior break. (b) After pars-plana vitrectomy and fluid–air exchange the subretinal fluid is drained internally using a flute needle; the retina is settled, and the break is subsequently lasered. (c) In an air-filled eye, 0.1–0.2 mL of fibrin glue is injected and applied over the break. (d) Subsequently at the end of the surgery, air is replaced by balanced salt solution and the retina is left attached with a clot of fibrin covering the break
Postoperative follow-up and medical regimen
All patients were examined postoperatively at 1-day, 1-week, 2-weeks, and 1-month postoperatively. The postoperative evaluations included measurement of the best-corrected visual acuity (BCVA) and intraocular pressure (IOP) and fundus photography at all visits. An optical coherence tomography (OCT) evaluation was done at 1 month and then at all subsequent visits. Besides this electroretinography was done for all patients at 1-month visit.
Outcome measures
The primary outcome measure was efficacy of the procedure defined as successful anatomical retinal reattachment. Secondary outcome measures were postoperative improvement in BCVA and complications.
Statistical analysis
Since this was a small noncomparative case series of five cases, descriptive statistics using median, range, and percentages were used and 95% confidence intervals (CI) were mentioned wherever it was appropriate.
Results
Patient characteristics
The demographics, baseline clinical characteristics, and outcomes of the five patients are summarized in Table 1. The median age of patients was 55 (range: 36–61 years) years and median duration of symptoms was 15 (range: 7–60) days. All eyes were pseudophakic with a posterior chamber intraocular lens (IOL) in four and anterior chamber IOL in one case. There were four cases of inferior and one case of total RD, with the macula involved in all cases.
Table 1.
Baseline clinical characteristics of patients and outcomes of glue-assisted retinopexy for rhegmatogenous retinal detachment (GuARD)
| Age (years) | Duration of symptoms (days) | Eye | Lens status | RD Type | No. of Retinal Breaks | Pre- operative BCVA | Post-operative BCVA (1 week) | Post-operative BCVA (1 month) | Anatomical Outcome | Duration of follow-up (in months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 56 | 7 | Left | PCIOL | Inferior | 1 | 20/80 | 20/80 | 20/30 | Success | 8 |
| 36 | 60 | Left | PCIOL | Inferior | 3 | 20/100 | 20/80 | 20/80 | Success | 8 |
| 61 | 15 | Right | ACIOL | Total | 3 | 20/100 | 20/50 | 20/50 | Success | 7 |
| 45 | 25 | Left | PCIOL | Inferior | 1 | 20/160 | 20/50 | 20/50 | Success | 4 |
| 55 | 15 | Left | PCIOL | Inferior | 3 | 20/50 | 20/50 | 20/30 | Success | 3 |
No=Number; RD=Retinal detachment; BCVA=Best corrected visual acuity
Outcomes
Successful retinal reattachment was achieved in all (100%) cases and was maintained at the end of 3–8 months of follow-up. The median BCVA improved from 20/100 preoperatively to 20/80 at 1-week and 20/50 at 1-month postoperatively. Typically, a clump of fibrin glue was present overlying the break at 1-day which reduced in size considerably by 1-week and had completely dissolved at 2-weeks [Fig. 2]. Neither was subretinal migration noted nor was any glue residue seen at the site of the breaks in the long term [Fig. 3].
Figure 2.
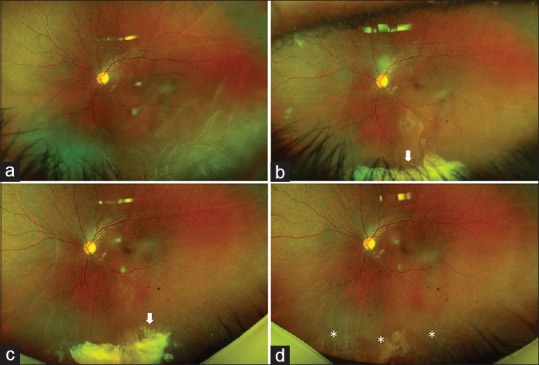
Early clinical course of glue-assisted retinopexy for rhegmatogenous retinal detachment (GuARD). (a) Fundus photograph of the left eye of a 36-year-old male patient with inferior retinal detachment. (b) Same eye on first postoperative day with attached retina and fibrin clot covering the inferior retinal breaks (white bold arrow); (c) At 1-week, the inferior fibrin clot over the breaks is still visible but has decreased in size; (d) At 2-weeks the fibrin clot has completely disappeared and the lasered inferior breaks are now visible (white asterisks). The visual acuity improved from 20/100, preoperatively to 20/80 at 6 months
Figure 3.
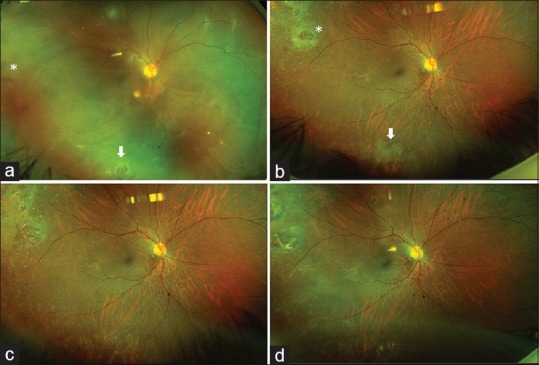
Long-term clinical course of glue-assisted retinopexy for rhegmatogenous retinal detachment (GuARD). (a) Fundus photograph of the right eye of a 61-year-old male patient with total retinal detachment with inferior horse-shoe tear (bold white arrow) and two additional retinal breaks temporally. Fibrin glue was used for tamponading all the breaks (b) Same eye at 1-month postoperative visit with attached retina and lasered inferior (white bold arrow) and temporal retinal breaks (white asterisk); (c) At 3-months and 6-months (d) postoperatively, the retina remained attached and the visual acuity improved from 20/100 to 20/30 at 6-months
Complications
No eye had any increase in postoperative inflammation. None of the eyes had an elevation of intraocular pressure at any of the visits. Two cases showed cystoid macular changes on OCT at 1-month visit which was treated with topical Nepafenac eyedrops and showed resolution by 2-month visit. Electroretinography was done for all eyes at 1 month visit and there was no significant increase in implicit times, “a” and “b” wave amplitudes, or b/a ratios.
Discussion
In this study, the authors investigated the suitability of fibrin glue as a local tamponading agent after PPV in RD surgery. The initial results of this pilot study indicate that air, long-acting gas, and silicone oil tamponade may be avoidable with the use of the novel GuARD technique. This approach will be advantageous in many ways, including but not restricted to early visual recovery, no risk of secondary glaucoma or corneal endothelial damage and obviation of postoperative head positioning. The American Society of Retina Specialists 2015 Global Trends in Retina survey revealed that 63–87% of the respondents preferred PPV for treating pseudophakic superior as well as inferior RD.[16] Thus, for those cases of uncomplicated RD where PPV is preferred over SB, GuARD can evolve as an useful alternative to gas or silicone oil tamponade.
In RD surgeries, tamponade agents are used to provide surface tension across retinal breaks in order to prevents further fluid flow into the subretinal space until the effect of retinopexy (photocoagulation or cryopexy) becomes permanent.[17] It has also been shown that adhesion strength of almost 95% is achieved at 18 hours after laser photocoagulation and the maximum strength is reached on day 5 (approximately 230% of normal).[18,19] As shown in this pilot study and in previous studies using fibrin glue for optic disc pits, the glue appears to stay in place for 1–2 weeks.[11,12] Therefore, it's reasonable to assume that a fibrin plug can safely and adequately cover the bare retinal breaks until the retinopexy effect becomes permanent. Haruta et al. had earlier tried using Seprafilm Adhesion Barrier (Sanofi, Bridgewater, NJ, USA), a bioresorbable translucent membrane comprising sodium hyaluronate and carboxymethylcellulose to patch retinal breaks.[20] However, Haruta et al. found it difficult to ensure safe and effective delivery of the Seprafilm sheet into the eye and the study was limited to retinal tears that could be covered with 5 × 2 mm sheets of Seprafilm. Since fibrin glue is injected in liquid form and gels as the two components interact, size of the retinal break or its location should not be limiting factors. Fibrin glue has been described earlier in the management of optic disc pit-associated macular detachments.[11,12] None of these studies reported any toxicity of fibrin glue. Like in this current study, fibrin glue was also not found to have any toxic effects on retinal function or structure in a rabbit model.[13]
Unlike anterior segment surgeons, fibrin glue is not commonly used by vitreoretinal specialists. Therefore, it may be useful to highlight some of the technical aspects of using fibrin glue, particularly in the context of intraocular retinal application. It's best to avoid the DUPLOJECT injector as the glue tends to gel within the 25-g needle and block it. Ideally, one should prepare the two components (sealer protein and thrombin solutions) of the glue separately in 1 mL insulin syringes. The thrombin solution is less viscous and tends to squirt leading to spillage, which can cause a larger clot than required. This can be avoided by first making the needle fluid free and discarding a small amount externally before introducing the needle through the vitrectomy port. Otherwise, the excessive clot can be trimmed with the vitrectomy cutter. It's also advisable to apply the more viscous sealer protein solution first and then applying the thrombin solution as it tends to gel as soon as there is contact and there is no excessive spillage beyond the area of the retinal break.
This was a small pilot-trial and encouraged by the initial results the authors are now designing a larger randomized controlled trial to compare the speed of visual recovery between GuARD technique and perfluoropropane gas tamponade in eyes with uncomplicated RD. At this point in time the authors have no personal experience of using this approach in complicated RD and standard PPV with silicone oil or gas tamponade will continue to be the author's primary preference in these cases until they gain more experience with the technique. The authors also feel that this technique may not be replicable in complicated RDs, in cases with advanced PVR changes and RD with multiple breaks in different quadrants. The authors also accept the limitation of a small sample size and absence of a control group, since this was a pilot-study of a novel surgical technique to simply establish proof-of-concept.
Conclusion
In conclusion, the authors studied the role of a novel surgical technique of fibrin glue assisted localized tamponade for retinal breaks and found that GuARD is a promising technique for the treatment of uncomplicated rhegmatogenous RD that allows early visual recovery while avoiding the usual problems of gas or oil tamponade and obviating the need of postoperative positioning.
Financial support and sponsorship
Hyderabad Eye Research Foundation (HERF).
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.ijo.in
References
- 1.Adelman RA, Parnes AJ, Ducournau D. Strategy for the management of uncomplicated retinal detachments: The European vitreo-retinal society retinal detachment study report 1. Ophthalmology. 2013;20:1804–08. doi: 10.1016/j.ophtha.2013.01.070. [DOI] [PubMed] [Google Scholar]
- 2.Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers RD, Foerster MH, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: A prospective randomized multicenter clinical study. Ophthalmology. 2007;114:2142–54. doi: 10.1016/j.ophtha.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz SG, Flynn HW. Pars plana vitrectomy for primary rhegmatogenous retinal detachment. Clin Ophthalmol. 2008;2:57–63. doi: 10.2147/opth.s1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chong DY, Fuller DG. The declining use of scleral buckling with vitrectomy for primary retinal detachments. Arch Ophthalmol. 2010;128:1206–7. doi: 10.1001/archophthalmol.2010.190. [DOI] [PubMed] [Google Scholar]
- 5.Barr CC, Lai MY, Lean JS, Linton KL, Trese M, Abrams G, et al. Postoperative intraocular pressure abnormalities in the silicone study. Silicone study report 4. Ophthalmology. 1993;100:1629–35. doi: 10.1016/s0161-6420(93)31425-9. [DOI] [PubMed] [Google Scholar]
- 6.Toklu Y, Cakmak HB, Ergun SB, Yorgun MA, Simsek S. Time course of silicone oil emulsification. Retina. 2012;32:2039–44. doi: 10.1097/IAE.0b013e3182561f98. [DOI] [PubMed] [Google Scholar]
- 7.Abrams GW, Azen SP, Barr CC, Lai MY, Hutton WL, Trese MT, et al. The incidence of corneal abnormalities in the Silicone study. Silicone study report 7. Arch Ophthalmol. 1995;113:764–9. doi: 10.1001/archopht.1995.01100060090039. [DOI] [PubMed] [Google Scholar]
- 8.Federman JL, Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology. 1988;95:870–87. doi: 10.1016/s0161-6420(88)33080-0. [DOI] [PubMed] [Google Scholar]
- 9.Fawcett IM, Williams RL, Wong D. Contact angles of substances used for internal tamponade in retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol. 1994;232:438–44. doi: 10.1007/BF00186587. [DOI] [PubMed] [Google Scholar]
- 10.Williams R, Wong D. The influence of explants on the physical efficiency of tamponade agents. Graefes Arch Clin Exp Ophthalmol. 1999;237:870–4. doi: 10.1007/s004170050325. [DOI] [PubMed] [Google Scholar]
- 11.Al Sabti K, Kumar N, Chow DR, Kapusta MA. Management of optic disc pit-associated macular detachment with tisseel® fibrin sealant. Retin Cases Brief Rep. 2008;2:274–7. doi: 10.1097/ICB.0b013e3180eaa21b. [DOI] [PubMed] [Google Scholar]
- 12.Kumar N, Al Sabti K. Optic disc pit maculopathy treated with vitrectomy, internal limiting membrane peeling, and gas tamponade: A report of two cases. Eur J Ophthalmol. 2009;19:897–72. doi: 10.1177/112067210901900537. [DOI] [PubMed] [Google Scholar]
- 13.Coleman DJ, Lucas BC, Fleischman JA, Dennis PH, Jr, Chang S, Iwamoto T, et al. A biologic tissue adhesive for vitreoretinal surgery. Retina. 1988;8:250–6. doi: 10.1097/00006982-198808040-00006. [DOI] [PubMed] [Google Scholar]
- 14.Balakrishnan D, Mukundaprasad V, Jalali S, Pappuru RR. Comparative Study on surgical outcomes of glued intraocular lens and sutured scleral fixated intraocular lens implantation. Semin Ophthalmol. 2018;33:576–80. doi: 10.1080/08820538.2017.1346132. [DOI] [PubMed] [Google Scholar]
- 15.Basu S, Surekha SP, Shanbhag SS, Kethri AR, Singh V, Sangwan VS. Simple limbal epithelial transplantation: Long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns. Ophthalmology. 2016;123:1000–10. doi: 10.1016/j.ophtha.2015.12.042. [DOI] [PubMed] [Google Scholar]
- 16.Rezaei KA, Stone TW. Global trends in retina. American Society of Retina Specialists. Available from: https://www.asrs.org/contentdocuments/2015_global_trends_comprehensivepostmtg.pdf .
- 17.Regillo CD, Tornambe PE. Primary retinal detachment repair. In: Regillo CD, Brown GC, Flynn HW Jr, editors. Vitreoretinal Disease: The Essentials. 1st ed. New York: Thieme; 1998. pp. 631–46. [Google Scholar]
- 18.Zauberman H. Tensile strength of chorioretinallesions produced by photocoagulation, diathermy, and cryopexy. Br J Ophthalmol. 1969;53:749–52. doi: 10.1136/bjo.53.11.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation. Ophthalmology. 1988;95:1385–138. doi: 10.1016/s0161-6420(88)33000-9. [DOI] [PubMed] [Google Scholar]
- 20.Haruta M, Arai M, Sueda J, Hirose T, Yamakawa R. Patching retinal breaks with Seprafilm for treating retinal detachments in humans: 9 years of follow-up. Eye. 2017;31:776–80. doi: 10.1038/eye.2016.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


