Abstract
Purpose: To determine whether the use of social media is useful in improving compliance and follow-up attendance among patients wearing retainers after orthodontic treatment.
Patients and methods: Sixty post-orthodontic patients (aged 16–19 years), randomized in two groups: follow-up supported by participation in WhatsApp chat group (SG), and Control Group (CG). All patients were scheduled for quarterly check-ups for monitoring of orthodontic stability by measurement of intercanine width at the beginning of the study (t0) and every 4 months t1, t2, t3) for 1 year of observation. Patients in the SG additionally participated in a WhatsApp chat group, where they would send, on a weekly basis, snapshots showing his/her occlusion. Every month, the orthodontist acting as the moderator awarded the best five snapshots by publishing a ranking in the chat.
Results: Participants in the SG featured smaller changes from the intercanine widths at baseline (at debonding) compared to the CG patients at all times during 1 year of follow-up. Follow-up attendance was regular in both groups in the first 8 months of follow-up. After that, patient compliance decreased in the CG, with eight patients missing check-up appointments.
Conclusion: Engaging adolescent patients directly through WhatsApp activity seems to increase regularity in wearing removable retainers, attendance to follow-up schedule, and yield better long-term outcome in terms of orthodontic stability and compliance.
Keywords: apps, technologies, orthodontics relapse, orthodontic compliance, patient compliance, young patients
Introduction
Success of orthodontic treatments involving removable retainers heavily relies on patient compliance, and presents an increased risk of relapse over the long-term. Indeed, aside from the few weeks before and after visits in which compliance is highest, patient engagement tends to fade over time.1 One of the main issues with long-term treatments in adolescents is the lack of immediate reward and the difficulty in envisioning the final result. The day-to-day effect of wearing the retainers – or of not wearing them – is not immediately visible and, therefore, leads patients to underestimate the consequences of scarce adherence to post-treatment indications on the long-term. While this is also true for adults who actively seek orthodontic treatment (but are not highly motivated to stick to the treatment strategy), this aspect is further enhanced by the lack of motivation among adolescent patients, who are often not an active part of the initial decision of wearing bracket appliances.2–4
Several studies in the literature have addressed the issue of patient compliance and strategies to obtain the best engagement of patients.2,3,5–9 In the last decades, there has been a large adoption of focus groups, motivational interviewing, and patient education, which nowadays are being further implemented through their use via social media, phone-apps, and content sharing (visuals, graphics, real-time texting).3,5,8,10
In 2016 we tested the use of a Whatsapp chat-room to monitor oral hygiene among patients wearing fixed multi-bracket appliances, boosting their compliance through the sharing of selfies and information on dental health among participants. The experiment provided encouraging results in terms of a reduction of white spots, plaque index, gingival index, and caries.6 Hence, we were interested in evaluating whether a similar application in post-orthodontic patients (passing from fixed to removable retainers) could also help reduce relapse and increase compliance among these subjects.
The primary objectives of the study were to (i) assess differences in relapse rate (defined as any change in orthondontic stability) between patients supported through a motivational approach and engaged in the chat-room interaction compared to a control group, and (ii) assess patient compliance (to both retainer wearing and visit attendance), participation, and feasibility of the proposal.
Materials and methods
This study enrolled 60 adolescent patients aged 16–19 years (average 17.5 years) at the end of non-extraction orthodontic multibrackets treatment performed for class I malocclusion with minimal or moderate crowding according to Little’s Index, and recruited between 2012 and 2014.11 Inclusion criteria were to be the owner of a smartphone, be able to access the internet on a daily basis, be treated with fixed orthodontic appliance Victory braces (MBT prescription, 0.022-inch slot, 3M Unitek, Milan, Italy) for class I malocclusion with minimal or moderate crowding, and Caucasian; whereas exclusion criteria were the presence of a significant medical history, restrictive dietary regimen (which has been shown in the literature to affect long-term compliance), deleterious habits (eg, nail biting, objects biting, cheek/lip biting), difficulties in reading or speaking the national language.12
Intervention
At the end of active orthodontic treatment all patients were instructed on wearing upper and lower retainers (Hawley retainer) for a total of 8 hours/day or more. They also received instructions on the management of retainers (cleaning, storage, etc.), and were invited to attend follow-up visits every 4 months throughout the observation period, starting from the delivery day (t0) of retainer.
To encourage participation and provide positive reinforcement, patients in the study group (SG) were further engaged in a WhatsApp chat group moderated by one of the authors of this study who was not involved in measurements. Participants were asked to create a fictional nickname and take part in a competition, the “Relapse Game”, by sharing a selfie of their teeth on a weekly basis showing the state of orthodontic stability. Pictures had to show open mouth with upper and lower jaw, as shown by the orthodontist at t0. Text and emoticons could also be used to interact with other members of the chat, while identifying elements such as names and photos with recognizing traits were not allowed in order to preserve privacy. It was explained to patients that scores were given based on timeliness and quality of close-up over a 1-month period. The first Saturday of every month the moderator evaluated the patients’ selfies and published a ranking of the five best participants of the month. No accessory text or comments were added. The pictures were assessed on a qualitative basis, to evaluate participation, and were not used for any quantitative measurements for instability.
Patients in the control group were scheduled for check-up visits from visit to visit, with the same frequency (every 4 months), without reminders or other types of interaction.
Endpoints and measurements
The main outcome in this study was occurrence of relapse event (yes/no), rate, and mean values. Accordingly, the monitoring throughout the follow-up was based on mandibular intercanine width (distance between cusp tip points of the right and left canines), which is the main parameter for orthodontic stability.13–17
A precision impression (AquasilTM Soft Putty, Dentsply, USA) was taken on a quarterly basis at each appointment: ie, at the end of treatment and beginning of the survey (t0); 4 (t1), 8 (t2), and 12 (t3) months after brace removal (ie, the end of our survey).
For each dental cast obtained from the impressions, lower intercanine width was measured with digital caliper by the same blinded operator. The mandibular intercanine width was measured as the straight-line distance between the heights of the incisal edge of the central lobe of each mandibular permanent canine.18 Each measurement was carried out three times (at 15 minute intervals) and values were used to obtain the mean value. The examiner was the same for all measurements and was blinded to both the name of patient and the group to which the patient belonged.
The relapse, where present, was detected at each time range, by subtracting the value of t1 from t0 (Delta 0–1), t2 from t1 (Delta 1–2), and t3 from t2 (Delta 2–3). A positive figure (+) indicated a decrease in width, while a negative figure (−) indicated a gain in width.19
Ethical considerations
The study protocol had been previously approved by the review board of the Dental School of Brescia. All patients/parents provided written informed consent for participation.
Statistical analysis
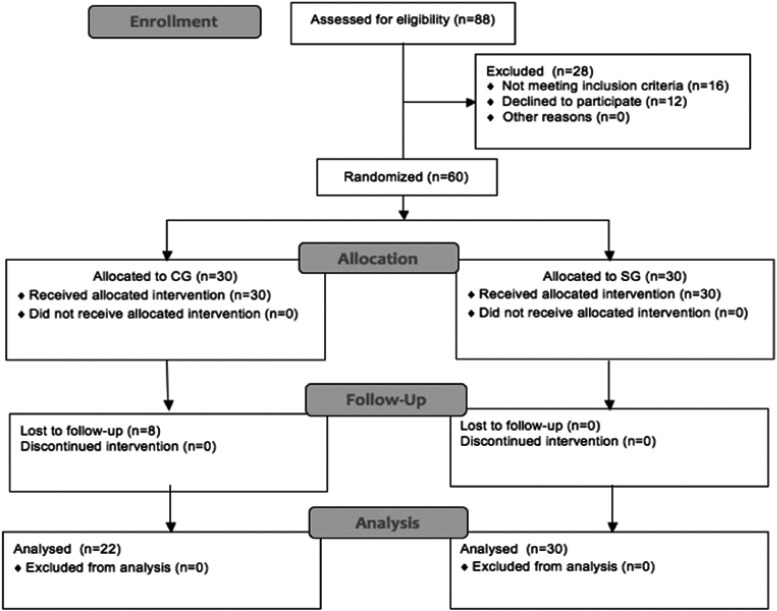
A stratified randomization list was produced by an external office taking into account baseline Little irregularity index value, in order to guarantee inter-groups homogeneity (Figure 1). Sample size was calculated as described elsewhere.6
Figure 1.
Patients allocation flow-chart.
Abbreviations: CG, control group; SG, study group.
Normal distribution of data collected has been tested with Shapiro-Wilk test. Variance homogeneity was tested by Levene test. Intra-group and inter-groups differences at different time-points (Delta 0–1, Delta 1–2, Delta 2–3) were, respectively, assessed by Friedman’s test (P-value≤0.05) and Mann-Whitney test.6 Analyses were performed using SPSS 16 software (SPSS Inc., Chicago, IL, USA).
Results
The total study population (n=60) consisted of 24 males and 36 females, and was divided into two homogeneous groups (Table 1). Ten patients did not participate because of parent’s refusal, and two did not use smartphones. While all patients of the SG took part in the chat-room weekly, shared their snapshots regularly, and attended scheduled check-ups for the entire observation period, eight of 30 control group (CG) patients discontinued visits after 8 months from the beginning of the follow-up.
Table 1.
Demographic variables
| Variable | SG (n=30) | CG (n=30) |
|---|---|---|
| Female, n | 20 | 16 |
| Age, years mean (±SD) | 17.2 (±1.03) | 17.8 (±1.06) |
| Caucasian (%) | 100 | 100 |
| Intercanine width (mm) (±SD) | 25.34 (±0.33) | 25.84 (±1.76) |
Abbreviations: CG, control group; N, overall number of patients per group; SG, study group.
In SG patients, intercanine width decreased by 0.017 mm from t0 to t1, 0.133 mm from t1 to t2, and 0.177 mm from t2 to t3. In the CG patients intercanine width decreased by 0.097 mm from t0to t1, 0.795 mm from t1 to t2, and 0.412 mm from t2 to t3. The cumulative observed decreasing of this width from t0 to t4 was 0.327 mm in the SG , whereas in the CG it was 1.304 mm.
Differences in intercanine widths in each group at different time points were found to be statistically significant (P≤0.05) (Table 2), as well as differences in intercanine widths between two groups (P≤0.05) (Table 3). Descriptive statistical analysis shows the extent of these differences (Table 4).
Table 2.
Intra-group differences in intercanine width (Friedman test)
| CG | ||
|---|---|---|
| Delta 0–1 | Delta 1–2 | Delta 2–3 |
| *** | *** | *** |
| SG | ||
| Delta 0–1 | Delta 1–2 | Delta 2–3 |
| *** | *** | *** |
Notes: t0=at baseline; t1=after 4 months; t2=after 8 months; t3=after 12 months. Delta 0–1=difference between t0 and t1, Delta 1–2=difference between t1 and t2, Delta 2–3=difference between t2 and t3, ***P<0.001.
Abbreviations: CG, control group; SG, study group.
Table 3.
Inter-groups differences in intercanine width (Mann-Whitney test)
| SG vs CG | |
|---|---|
| Delta 0–1 | *** |
| Delta 1–2 | *** |
| Delta 2–3 | *** |
Notes: t0=at baseline; t1=after 4 months; t2=after 8 months; t3=after 12 months. Delta0–1=difference between t0 and t1, Delta1–2=difference between t1 and t2, Delta2–3=difference between t2 and t3, ***P<0.001.
Abbreviations: CG, control group; SG, study group.
Table 4.
Mean (mm) and SD of intercanine width decrease at different Delta
| CG | SG | |
|---|---|---|
| Delta 0–1 | 0.097 (0.096) | 0.017 (0.042) |
| Delta 1–2 | 0.795 (0.249) | 0.133 (0.087) |
| Delta 2–3 | 0.412* (0.418*) | 0.177 (0.084) |
Notes: t0=at baseline; t1=after 4 months; t2=after 8 months; t3=after 12 months. Delta 0–1=difference between t0 and t1, Delta 1–2=difference between t1 and t2, Delta 2–3=difference between t2 and t3, *values calculated on 22 patients.
Abbreviations: CG, control group; SG, study group.
Patient chat participation was 100% and constant throughout the observation period. In addition to selfies, members also used text messaging and emoticons. No patient blocked or withdrew from the chat.
Discussion
The present work aimed to evaluate whether engagement of adolescent patients in social media activity (namely WhatsApp) could increase compliance in wearing retainers, follow-up attendance, and ultimately reduce the occurrence and degree of relapse. In designing the study, the main endpoint selected for monitoring orthodontic stability was intercanine width. Despite a number of other parameters being described in the literature,13–15 we chose this one in consideration of its widespread use throughout practices and rapid calculation, which would allow it to be more easily exported to other settings.
In consideration of the many variables affecting changes in intercanine width and dental arch, we chose patients belonging to the same ethnic group. Moreover, during the orthodontic treatment for all patients, proper dental arch shapes were chosen as close as possible to the patient’s natural shape, in order to reduce potential relapse.20 Measurements of intercanine widths were carried out every 4 months, with changes being reported as a partial relapse for every time-point.
Overall, results for intercanine widths were better among the SG, as well as attendance to follow-up visits, confirming the positive effect of the use of the WhatsApp chat in patient involvement and adherence. In detail, the values collected in both groups were clinically negligible during the first period of observation (t0–t1) and suggested similar compliance among both patient groups. However, variation trends differed within groups results. Intercanine width in SG decreased more slowly in Delta 0–1 and Delta 1–2, and became more evident in Delta 2–3. This might be due to a physiological lack of motivation at the end of follow-up and to a loss of interest in the Relapse Game: despite participation to the chat remaining 100%, we cannot exclude that over the long-term participants wore retainers less than the prescribed time during the day. Meanwhile, values in the CG decreased considerably, immediately after the braces removal up until the first 8 months of observation; then the trend remained steady over time. These data are coherent with literature results that show relapse is greater immediately after the removal of the appliance.13,14
Despite the differences in intercanine widths, no non-scheduled interventions were necessary as the values collected in both group were still considered clinically negligible, in agreement with evidences from literature, and did not undermine the esthetic and functional results of orthodontic therapy.13–15,21
The publication of a monthly ranking score surely reinforced positive feedback and contributed to increasing the higher compliance in the SG.5 Yet, we cannot exclude that the high compliance rate observed could have been to some degree due to the patient’s awareness of being under observation in the chat room and within an orthodontic study. However, the use of emoticons and comments in the chat showed no evidence of a lack of authenticity in communication among members of the chat room. Moreover, although ranking of selfies was qualitative and based on the moderator’s subjective evaluation alone (whereas measurements were done on dental impressions), participants were not aware of this technical aspect, and respected the periodic appointments for sending selfies and follow-up checks. None of the patients withdrew from the chat-room nor missed check-up appointments throughout the follow-up.
A high drop-out rate was noticed in CG patients, probably due to a lack of motivation in check-up appointments. Compliance to attempt visits, especially after 2-years of active orthodontic treatment, might be difficult to maintain in adolescents and patients not too motivated, who could drop out of the follow-up. This means failure of the entire treatment and lack of control of results that could temporally deteriorate and make useless both diagnostic and clinical treatment. Therefore, patients adherence to follow-up might be considered a crucial point indeed during the planning of treatment, in order to assure the best goal and best maintenance of obtained orthodontic results. In this study seven patients of CG quit the study without a strong reason, probably because of lack of motivation; only one of them moved to another city and so his parents could not drive him to check-ups.
We can assume that the drop-out rate observed here, while a limit, did not affect the purpose of the study only because it confirmed the mean on which it was designed, namely the importance of strong engagement in maintenance of compliance. However, a 27% drop-out rate is a great rate and it might affect the statistical power of our study, and, due to this, the present work aimed to be only a pilot study and the authors are well aware that a larger sample is needed in order to obtain stronger results.
Yet, changes in intercanine width also increased among the SG after 8 months into follow-up, coherently to the higher compliance in wearing a device immediately after braces removal and a lower one of over time.3,22
Similar experiences have been published by other authors in reference to oral hygiene. Eppright et al5 proposed a system of active reminders for adolescent patients with full fixed appliances in both arches, by text messaging parents weekly to remind the child of constant oral hygiene. The study by Cozzani et al.9 on oral hygiene among patients beginning fixed orthodontic treatment, proposed text messages within hours after bonding to increase oral hygiene compliance, by offering encouragement and enquiring into patient’s wellbeing. A previous study of ours on adolescents wearing fixed multi-brackets appliances investigated patient compliance and outcome in terms of oral hygiene, engaging patients through the use of a WhatsApp chat-room and sharing of selfies. Findings of such studies were consistent in demonstrating higher patient compliance whenever patients or family were reminded of goals, and actively encouraged through positive feedback.
Compared to the study by Cozzani et al,9 here we directly addressed the patients rather than the parents or tutor. This was a key aspect in the success of the strategy. Because adolescents begin to feel the need for independence from parent supervision and tend to manifest defiance to parental guidance, they are more likely to be responsive when directly addressed by a care provider on a one-to-one basis. Rather than receiving instructions by parents, they are made an active part of the decision process and feel accountable for their perseverance in post-treatment.
Also, compared to text messaging, being part of a chat creates a feeling of belonging and acceptance in a group of peers that are experiencing the common involvement of wearing retainers, which represents a further asset in consideration of the adolescent phase. Nowadays, the involvement on social media is with no doubt the best way to reach adolescents. Sharing of selfies, with the use of emoticons or accessory text and captions, allows individuals to communicate in a creative way; plus the ranking of best weekly pics encourages the young patients to compare their performance and realize how much more effort they need to apply to be at the same level as their chat contacts.
Adolescence is quite complex, and the doctor–patient relationship can be a determining factor towards success of treatment, as well as parental influence, social standing, education, and others. However, we did not evaluate these aspects as they were beyond the scope of this study, and are extensively discussed elsewhere.2–4,8,23
From a practical point of view, despite the increasing availability of educational apps for patients,24 the WhatsApp chat-room represents a very economical solution to encourage adolescent patients to be actively engaged in their own health treatment and to work towards a goal and keep track of progress. It can be easily adopted by orthodontic practices serving any size of patient basin, without the burden of financial and human resources required to create ad hoc apps. Similarly to the concept of text messaging to reduce no-shows which has now become widespread among orthodontic practices with significant economical returns and more effective management of work flow,25,26 adopting this simple chat-room project can lead to great gains in terms of treatment effectiveness. From the technical point of view, this active engagement increases the likelihood the treatment actually sees a continuity between the “fixed” and “removable” treatment, which will improve final stability on the long-term. From the patient point of view, the chat room represents an extra effort towards a stronger doctor–patient relationship, creating to some degree a “complicity” with the adolescent patient. Lastly, from the parent’s/payer’s point of view this extra service provided is pleasantly welcomed, and further contributes to proving the customer a service of excellence.
Recent meta-analyses examined the association with several demographic clinical and social variables in compliance of adolescents to oral hygiene and retainer treatment,3,9 evidencing the family support, education, and income as determining factors for higher compliance within patient education initiatives. Certainly these are important aspects to consider and would allow one to target patient needs around the individual patient needs. Nonetheless, in the real clinical practice, customization or design of sophisticated web and mobile apps are not feasible. Considering the widespread access to WhatsApp and the degree of young engagement, we believe a more simple approach through a universally accessible tool, like this one, might overcome such socio-demographic barriers and could involve a larger number of people. Although WhatsApp is mostly used across Europe, this concept can certainly be generalized and transposed to similar platforms such as Facebook’s Messenger or Skype which basically offer the same communication tools of image and photo sharing and real-time exchange of chat messages.
Conclusion
This pilot experience documents the higher compliance in wearing post-orthodontic retainers among adolescent patients involved in a social media activity, and ultimately a lower relapse rate and degree of changes in intercanine width. We believe such findings may represent a small contribution for future studies employing intervention mapping approaches, longer follow-up and large scale application.
Disclosure
The present was a spontaneous study and did not receive any external funding. A modified version of the abstract has been presented as a poster at the EOS Congress in Venice in 2015 (April 13–15, 2015) and it received the Francesca Miotti Award for the best clinical poster. The authors have no conflicts of interests in this work.
References
- 1.Al-Moghrabi D, Salazar FC, Pandis N, Fleming PS. Compliance with removable orthodontic appliances and adjuncts: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2017;152:17–32. doi: 10.1016/j.ajodo.2017.03.019 [DOI] [PubMed] [Google Scholar]
- 2.Wong P, Freer TJ. Patients’ attitudes towards compliance with retainer wear. Aust Orthod J. 2005;21:45–53. [PubMed] [Google Scholar]
- 3.Ackerman MB, Thornton B. Posttreatment compliance with removable maxillary retention in a teenage population: a short-term randomized clinical trial. Orthodontics (Chic). 2011;12:22–27. [PubMed] [Google Scholar]
- 4.Mirzakouchaki B, Shirazi S, Sharghi R, Shirazi S. Assessment of factors affecting adolescent patients’ compliance with Hawley and Vacuum formed retainers. J Clin Diagnostic Res. 2016;10:ZC24–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eppright M, Shroff B, Best AM, Barcoma E, Lindauer SJ. Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod. 2014;84:208–213. doi: 10.2319/062813-481.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zotti F, Dalessandri D, Salgarello S, et al. Usefulness of an app in improving oral hygiene compliance in adolescent orthodontic patients. Angle Orthod. 2016;86:101–107. doi: 10.2319/010915-19.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowen TB, Rinchuse DJ, Zullo T, DeMaria ME. The influence of text messaging on oral hygiene effectiveness. Angle Orthod. 2015;85:543–548. doi: 10.2319/071514-495.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mas FG, Plass J, Kane WM, Papenfuss RL. Health education and multimedia learning: connecting theory and practice (Part 2). Health Promot Pract. 2003;4:464–469. doi: 10.1177/1524839903255411 [DOI] [PubMed] [Google Scholar]
- 9.Cozzani M, Ragazzini G, Delucchi A, et al. Oral hygiene compliance in orthodontic patients: a randomized controlled study on the effects of a post-treatment communication. Prog Orthod. 2016;17:41. doi: 10.1186/s40510-016-0154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheerman JFM, van Meijel B, van Empelen P, et al. Study protocol of a randomized controlled trial to test the effect of a smartphone application on oral-health behavior and oral hygiene in adolescents with fixed orthodontic appliances. BMC Oral Health. 2018;18:19. doi: 10.1186/s12903-018-0507-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–563. [DOI] [PubMed] [Google Scholar]
- 12.Laffranchi L, Zotti F, Bonetti S, Dalessandri D, Fontana P. Oral implications of the vegan diet: observational study. Minerva Stomatol. 2010;59:583–59s. [PubMed] [Google Scholar]
- 13.Olive RJ, Basford KE. A longitudinal index study of orthodontic stability and relapse. Aust Orthod J. 2003;19:47–55. [PubMed] [Google Scholar]
- 14.Josell SD. Tooth stabilization for orthodontic retention. Dent Clin North Am. 1999;43:151–165s. [PubMed] [Google Scholar]
- 15.Steinnes J, Johnsen G, Kerosuo H. Stability of orthodontic treatment outcome in relation to retention status: an 8-year follow-up. Am J Orthod Dentofac Orthop. 2017;151:1027–1033. doi: 10.1016/j.ajodo.2016.10.032 [DOI] [PubMed] [Google Scholar]
- 16.Ward DE, Workman J, Brown R, Richmond S. Changes in arch width. A 20-year longitudinal study of orthodontic treatment. Angle Orthod. 2006;76:6–1s. doi: 10.1043/0003-3219(2006)076[0006:CIAW]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 17.Motamedi AK, Dadgar S, Teimouri F, Aslani F. Stability of changes in mandibular intermolar and intercuspid distances following orthodontic treatment. Dent Res J (Isfahan). 2015;12:71s–75s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Erdinc AE, Nanda RS, Işıksal E. Relapse of anterior crowding in patients treated with extraction and nonextraction of premolars. Am J Orthod Dentofac Orthop. 2006;129(6):775–784. doi: 10.1016/j.ajodo.2006.02.022 [DOI] [PubMed] [Google Scholar]
- 19.Kahl-Nieke B, Fischbach H, Schwarze CW. Post-retention crowding and incisor irregularity: a long-term follow-up evaluation of stability and relapse. Br J Orthod. 1995;22:249–257. [DOI] [PubMed] [Google Scholar]
- 20.Fleming PS, Dibiase AT, Lee RT. Arch form and dimensional changes in orthodontics. Prog Orthod. 2008;9:66–73. [PubMed] [Google Scholar]
- 21.Littlewood SJ, Kandasamy S, Huang G. Retention and relapse in clinical practice. Aust Dent J. 2017;62(Suppl 1):51–57. doi: 10.1111/adj.12475 [DOI] [PubMed] [Google Scholar]
- 22.Schott TC, Schlipf C, Glasl B, Schwarzer CL, Weber J, Ludwig B. Quantification of patient compliance with Hawley retainers and removable functional appliances during the retention phase. Am J Orthod Dentofacial Orthop. 2013;144:533–540. doi: 10.1016/j.ajodo.2013.04.020 [DOI] [PubMed] [Google Scholar]
- 23.Mas FGS, Plass J, Kane WM, Papenfuss RL. Health Education and. multimedia learning: educational psychology and health behavior theory (Part 1). Health Promot Pract. 2003;4:288–292s. doi: 10.1177/1524839903004003013 [DOI] [PubMed] [Google Scholar]
- 24.Baheti MJ, Toshniwal N. Orthodontic apps at fingertips. Prog Orthod. 2014;15:36s. doi: 10.1186/s40510-014-0036-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Almog DM, Devries JA, Borrelli JA, Kopycka-Kedzierawski DT. The reduction of broken appointment rates through an automated appointment confirmation system. J Dent Educ. 2003;67:1016–1022. [PubMed] [Google Scholar]
- 26.Car J, Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments In: Car J, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons Ltd; 2012:CD007458. [DOI] [PubMed] [Google Scholar]