Watch a video presentation of this article
Abbreviations
- FHVP
free hepatic vein pressure
- HVPG
hepatic venous pressure gradient
- NCPH
noncirrhotic portal hypertension
- WHVP
wedged hepatic vein pressure
Portal hypertension is a clinical syndrome characterized by splenomegaly, ascites, gastrointestinal varices, and encephalopathy and is defined by a hepatic vein pressure gradient (HVPG) exceeding 5 mm Hg.1 Portal hypertension is the major cause of severe complications and death in patients with cirrhosis.1 Portal hypertension also can develop in the absence of cirrhosis under the condition called noncirrhotic portal hypertension (NCPH). In both cirrhotic portal hypertension and NCPH, the goal is to diagnose and characterize the severity of portal hypertension to minimize potentially severe and deadly complications. The intention of this review is to provide an overview of the approach to the diagnosis of portal hypertension. However, to understand the diagnosis and management of portal hypertension, it is essential to understand the underlying pathophysiological and etiological features.
Portal Hypertension and Related Hemodynamic Factors
In cirrhotic and most noncirrhotic cases of portal hypertension, portal hypertension results from changes in portal resistance in combination with changes in portal inflow. The portal vein pressure is a product of the portal blood flow volume and the resistance to flow as defined by an application of Ohm's law:
Because of its invasive nature, the direct measurement of the portal pressure is not routine. As a less invasive and indirect measure, the hepatic venous pressure gradient (HVPG) is considered the best surrogate indicator of portal hypertension in cirrhosis and has been found to carry independent prognostic value for many of the complications of portal hypertension (Fig. 1).2 HVPG can be calculated by the subtraction of the wedged hepatic vein pressure (WHVP) from the free hepatic vein pressure (FHVP):
Figure 1.
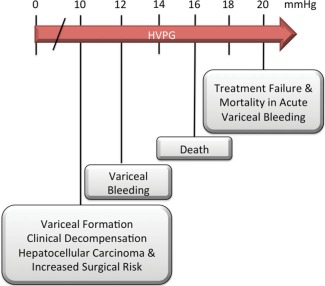
Diagram showing the risks associated with increased HVPG.
This indirect method of portal pressure measurement is performed with fluoroscopy, can be completed in approximately 10 to 30 minutes, and is safe, reproducible, and accurate (with certain exceptions described later).3
Evaluation of Portal Hypertension
The diagnosis of portal hypertension can be made in several ways. Clinically, patients with cirrhosis can be diagnosed with portal hypertension by the presence of ascites, varices, or both. Imaging studies such as Doppler ultrasonography, computed tomography, and magnetic resonance imaging also can aid in diagnosing portal hypertension and in defining portal vein anatomical features. Findings suggestive of portal hypertension include splenomegaly, portal vein dilation, portal vein occlusion, collateral vessel formation, declining platelet counts, and ascites with a serum‐ascites‐albumin gradient of 1.1 g/dL or more. However, these methods do not perform well in identifying subclinical portal hypertension, delineating the type of portal hypertension, or quantifying the extent of portal hypertension. Figure 2 provides an algorithm for the evaluation of portal hypertension. Novel techniques such as transient elastography are promising but as yet are unproven for routine clinical use.1
Figure 2.
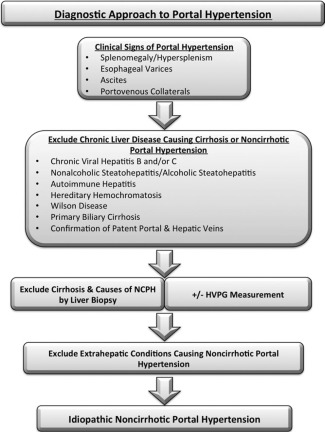
Algorithm showing the diagnostic approach to portal hypertension.
The range of HVPG measurements can provide clinically useful information in terms of the prognosis related to portal hypertension and its complications (Fig. 1).4, 5, 6, 7, 8 In normal healthy individuals, HVPG ranges from 2 to 5 mm Hg. An HVPG greater than or equal to 6 mm Hg constitutes portal hypertension, and an HVPG greater than or equal to 10 mm Hg constitutes clinically significant portal hypertension. An HVPG greater than or equal to 10 mm Hg can predict the clinical course of patients with cirrhosis, including the development of portal hypertension–related complications and an increased mortality rate.4, 5, 6, 7, 8
Although single HVPG measurements are useful in staging and predicting the course of both compensated and decompensated cirrhosis, HVPG also has usefulness in other measures of liver disease. First, HVPG can help to define the type of portal hypertension (as discussed later), which is useful in suspected cases of NCPH. A limitation is that HVPG is not elevated in all cases of NCPH, such as those resulting from prehepatic and presinusoidal causes (Fig. 2 and Table 1). Second, repeat HVPG measurements can help to monitor patients for the progression of liver disease and to assess response to pharmacotherapy. The limitations of this procedure include the need for local expertise and adherence to guidelines to ensure reliable and reproducible measurements as well as the invasive nature of the procedure. Another benefit of the procedure is the ability to couple it with other transjugular studies, such as transjugular liver biopsy and right heart catheterization.
Table 1.
Partial List of Causes of Intrahepatic Portal Hypertension
| Presinusoidal | Sinusoidal | Postsinusoidal |
|---|---|---|
| Developmental abnormalities | Cirrhosis | Veno‐occlusive disease |
| Idiopathic NCPH | Amyloid or light‐chain deposition in space of Disse | Central venopathy |
| Biliary diseases | Early noncirrhotic alcoholic liver disease | Primary vascular malignancy |
| Intrahepatic malignant occlusion of the portal vein | Fibrosis of space of Disse | |
| Granulomatous lesions | Infiltrative diseases | |
| Hepatoportal sclerosis | ||
| Nodular regenerative hyperplasia |
This table was adapted with permission from Hepatology.9
Causes of Portal Hypertension
Cirrhosis
Cirrhosis is the end stage of most chronic liver diseases, and portal hypertension is often the earliest and major result of cirrhosis. Portal hypertension in cirrhosis results from 3 mechanisms. The first mechanism is a fixed component that results in mechanical obstruction from fibrosis and compression by regenerative nodules. The second mechanism, which accounts for 20% to 30% of increased intrahepatic resistance, is a functional component that results from the active contraction of vascular smooth muscle cells and activated stellate cells.1 The third mechanism is an increased portal blood flow due to increased mesenteric arterial vasodilation.
Noncirrhotic Portal Hypertension
Portal hypertension also can develop in the absence of cirrhosis and is then called NCPH. In contrast to cirrhotic portal hypertension, NCPH is characterized by well‐preserved hepatic synthetic function with less frequent occurrences of ascites or hepatic encephalopathy.
Worldwide, the most common cause of NCPH is schistosomiasis.9 NCPH often is the result of problems at different levels of the hepatic circulation and can be classified as prehepatic, intrahepatic, and posthepatic portal hypertension (Fig. 3). The diagnostic algorithm shown in Fig. 2 may aid in the evaluation of NCPH.
Figure 3.
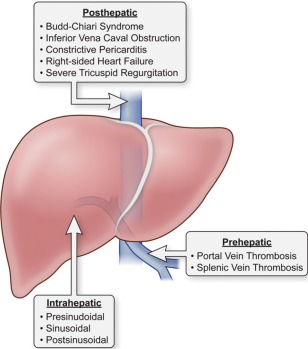
Diagram showing an abbreviated list of prehepatic, intrahepatic, and posthepatic causes of portal hypertension.
Conclusions
Portal hypertension and its related consequences are the leading causes of illness and death in patients with advanced liver disease. The goals of the evaluation of patients with portal hypertension are to determine the cause, to measure the severity, to reduce the complications of portal hypertension, and ultimately improve patient survival.
Acknowledgments
Because of the limited space for this review, we have been unable to refer to many excellent articles that have furthered the field with respect to the assessment of portal hypertension. We thank these authors for their contributions and apologize for our inability to mention them directly in this review. We also thank Dr. Yaron Rotman for a critical review of the manuscript.
This study was supported by the Intramural Research Programs of the National Institute of Diabetes & Digestive & Kidney Diseases, National Institutes of Health, Bethesda, MD.
Potential conflict of interest: Nothing to report.
References
- 1. Sanyal AJ, Bosch J, Blei A, Arroyo V. Portal hypertension and its complications. Gastroenterology 2008;134:1715–1728. [DOI] [PubMed] [Google Scholar]
- 2. Castera L, Pinzani M, Bosch J. Noninvasive evaluation of portal hypertension using transient elastography. J Hepatol 2012;56:696–703. [DOI] [PubMed] [Google Scholar]
- 3. Thabut D, Moreau R, Lebrec D. Noninvasive assessment of portal hypertension in patients with cirrhosis. Hepatology 2011;53:683–694. [DOI] [PubMed] [Google Scholar]
- 4. Monescillo A, Martinez‐Lagares F, Ruiz‐del‐Arbol L, Sierra A, Guevara C, Jiménez E, et al. Influence of portal hypertension and its early decompression by TIPS placement on the outcome of variceal bleeding. Hepatology 2004;40:793–801. [DOI] [PubMed] [Google Scholar]
- 5. Garcia‐Tsao G, Groszmann RJ, Fisher RL, Conn HO, Atterbury CE, Glickman M. Portal pressure, presence of gastroesophageal varices and variceal bleeding. Hepatology 1985;5:419–424. [DOI] [PubMed] [Google Scholar]
- 6. Bruix J, Castells A, Bosch J, Feu F, Fuster J, Garcia‐Pagan JC, et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 1996;111:1018–1022. [DOI] [PubMed] [Google Scholar]
- 7. Ripoll C, Groszmann R, Garcia‐Tsao G, Grace N, Burroughs A, Planas R, et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 2007;133:481–488. [DOI] [PubMed] [Google Scholar]
- 8. Ripoll C, Groszmann RJ, Garcia‐Tsao G, Bosch J, Grace N, Burroughs A, et al. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. J Hepatol 2009;50:923–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schouten JN, Garcia‐Pagan JC, Valla DC, Janssen HL. Idiopathic noncirrhotic portal hypertension. Hepatology 2011;54:1071–1081. [DOI] [PubMed] [Google Scholar]


