Abstract
Objectives
Blind working (BW) time (time during which vision is not required), the interblink interval (IBI), and subjective symptoms were investigated in workers using visual display terminals (VDTs).
Subjects and Methods
To investigate BW time, 10 VDT users were instructed to close their eyes when this did not interfere with their work. They were video recorded for 60 minutes using a webcam attached to the display on which they were engaged in regular data input tasks, and BW time was measured. The values of the IBI during the final 20 minutes of the BW experiment and during the final 20 minutes of normal working without BW were compared. A questionnaire was administered to investigate subjective symptoms using a visual analogue scale.
Results
The total BW time during the final 20‐minute period was 20.6‐121.0 seconds (1.7%‐10.1%). The mean IBI of 5.5 ± 4.5 seconds during the BW experiment was not significantly different from that of 6.2 ± 5.6 seconds during normal working, and the mean of three IBIs immediately after BW during the BW experiment was 2.7 ± 1.0 seconds, significantly shorter than the 6.2 ± 5.6 seconds during normal working. Dry eye, ocular fatigue, and blurred vision during normal working improved when subjects were engaged in BW.
Conclusions
VDT users could engage in BW during VDT work, the IBI was shorter immediately after BW, and subjective symptoms improved. These results suggest that BW may provide a more effective measure for the management of VDT working time.
Keywords: blind working, eye closure, interblink interval, subjective symptoms, visual display terminals
1. INTRODUCTION
Workers using visual display terminals (VDT) often complain of dry eye,1, 2 ocular fatigue,3, 4 and other ophthalmic symptoms. Visual health surveillance has therefore been considered a key element for the protection of VDT users.5 VDT working time and the management of breaks during VDT work are a major issue in occupational health. In the actual workplace, however, reasons such as being too busy or actually being hesitant to take breaks often make it difficult to take breaks during VDT work. Therefore Anshel6 mentioned the “20‐20‐20 Rule” idea in the 1990's, suggesting taking a 20 seconds break every 20 minutes by looking 20 feet away for preventing and relieving digital eye strain. Nowadays many academic societies such as the American Optometric Association7 and the American Academy of Ophthalmology8 have referred and recommend it for prevention of eye strain. The rule has already been applied in the advanced enterprises of occupational health. The guidelines on VDT work including break times have also been drawn up in many countries9, 10, 11 (Table 1). A long time has passed since these guidelines were formulated, and the past decade has seen a continuous increase in the level of dependency on VDT work in many different professions. VDT working time and the management of breaks during VDT work are thus becoming ever more important, and current measures cannot be described as adequate.
Table 1.
VDT break time guidelines in different countries
| Country | Title | Editor | Last review | Reference |
|---|---|---|---|---|
| Japan | Guidelines for Industrial Health Controls of VDT Operations | Ministry of Health, Labour and Welfare | 2002 | 9 |
| For operators who are involved in operations applicable to “simple input type” and “binding type” of “operation type”; in attachment, one continuous operation time must not exceed 1 hour and a break of 10‐15 min must be established before subsequent continuous operation. In addition, short breaks must be established once or twice within 1 continuous operation time. “Short breaks” are breaks of 1‐2 min during one continuous operation time. | ||||
| United States | Working Safely with Video Display Terminals | Department of Labor | 1997 | 10 |
| We recommend a 10‐min rest break after 2 h of continuous VDT work for operators under moderate visual demands; and a 15‐min rest break after 1 h of continuous VDT work where there is a high visual demand or repetitive work task. | ||||
| United Kingdom | Health and Safety (Display Screen Equipment) Regulations | Health and Safety Executive | 1992 | 11 |
| It is not appropriate to lay down requirements for breaks which apply to all types of work. Short, frequent breaks are more satisfactory than occasional, longer breaks: for example, a 5‐ to 10‐min break after 50‐60 min continuous screen and/or keyboard work is likely to be better than a 15‐min break every 2 h. | ||||
However, there should be periods during VDT work in which workers can perform tasks that do not require the use of sight, such as during intervals between tasks, when switching between screens, or when thinking about the contents of tasks, and thus at various times they may be simply staring into space without actually looking at the screen or using their eyes. We therefore devised a new method of resting just the eyes during VDT work and reducing eye strain by closing the eyes even for short periods at times when this does not interfere with the task at hand, which we named “blind working (BW).” In this study, a webcam was used to video record the anterior part of the eyes during regular VDT work, and BW time, the interblink interval (IBI), and subjective symptoms were investigated.
2. SUBJECTS AND METHODS
2.1. Subjects
The subjects who consented to participate in the study were 10 office staff in the General Affairs Department of our hospital who had never been examined in the hospital's Department of Ophthalmology. None of the subjects came into contact with the authors in the course of their work in the hospital, which involved at least 3 h a day of VDT work. They included 5 men and 5 women, with a mean age of 40.6 ± 8.6 years (range 28‐52 years). None of them suffered from any eye conditions other than ametropia, and all were systemically healthy. No subject had a history of refractive surgery or other ophthalmic surgery, and none was using eye drops. Subjects with a tear film breakup time (BUT) ≤ 5 seconds, those with chronic subjective ocular symptoms at times other than during VDT work, and those who wore contact lenses during VDT work were excluded.
2.2. Study design
To investigate BW time, the subjects were told before the experiment that its objective was to investigate the extent to which they were using their eyes, and that they should close their eyes as often as possible when their use was not required. They were asked to close their eyes when they were just staring vaguely at the screen while thinking or engaged in another activity that did not require the use of their eyes even for short periods, whenever closing their eyes did not interfere with their work, and they agreed to do so.
The computer used was the regular desktop computer with a 20‐inch monitor (Vostro®, Dell, TX, USA) that the subjects typically used for work. The positions of the monitor and keyboard were adjusted to the regular position used by each subject while working, with the screen fixed at a distance of 40‐50 cm from the subject's eyes. Room temperature was 23°C‐24°C, humidity was 51%‐55%, and room illumination was 485‐558 lux. The subjects engaged in their usual office tasks of text and number input, using the refractive correction method they typically used while working (the unaided eye for eight subjects and glasses for two) and using their regular keyboard.
2.3. Measurement
The anterior parts of the subjects’ eyes were each video recorded with a webcam (UCAM‐DLI500TNBK®, Elecom, Osaka, Japan) attached to the top of the monitor. The subjects were video recorded for two periods of 1 hour, the limit for continuous work according to Japanese guidelines: one while working normally and one while performing BW on the following day. On both days, the subjects worked according to their regular schedule from the morning, but they refrained from VDT work from 3 hours before the start of the experiment, took a full break before the start of the experiment, and confirmed that they were experiencing no subjective ocular symptoms whatsoever and that their VAS scores for fatigue, dry eye, and blurred vision were all zero. Video recording was started between 15:00 and 17:00 each day in line with the schedule of the individual concerned, in order to carry out all the day's VDT tasks in a single batch in the late afternoon. Video recordings of normal working and of the BW experiment were started at the same time of day for each subject. Although all subjects were engaged in the same type of work, the types of tasks they performed were the same when this video was taken, but the contents of the tasks were not identical to those carried out during the BW experiment.
To prevent subject awareness from affecting IBI measurement results, the subjects were video recorded without being informed that the IBI would be measured. Since previous studies have used 10‐ to 15‐minutes periods of VDT work to analyze the IBI and blink rate,12, 13, 14 and because the subjects may have been distracted at the start of video recording by having the camera immediately in front of their eyes, potentially making the data from this period unreliable,12 the 20‐minute period from 40 minutes to 60 minutes after the start of VDT work was used for the IBI study. The number of times subjects engaged in BW, the duration of each period of BW, and the total BW time were also measured during the final 20‐minute period. The IBI during normal working and that during the BW experiment were measured during the final 20‐minute period, and the two were compared. The mean of three IBIs immediately after each period of BW during the entire 20 minutes of the BW experiment was also calculated and compared with the mean IBI during normal working.
2.4. Subjective symptoms evaluation
A questionnaire was administered to investigate subjective symptoms using a visual analogue scale (VAS). Ocular fatigue, dry eye, and blurred vision immediately after 1 hour of normal working and immediately after the 1‐hour BW experiment were compared. Whether there was a dose‐response relationship between the VAS scores during the BW experiment and the total BW time was also investigated.
2.5. Ethics statement
This study complied with the Helsinki Declaration, and written, informed consent for voluntary participation was obtained from the subjects on the basis that every effort would be made to ensure that there was no external leakage of personal information, and that the results would be statistically analyzed and published. This study was approved by the Ethics Committee of Kuwano Kyoritsu Hospital (approval number 160201).
2.6. Statistical analysis
The results are expressed as means ± standard deviation. Wilcoxon's signed‐rank test was used to evaluate the IBI during BW and subjective symptoms after BW. Spearman's partial rank correlation coefficients controlling for the VAS scores during normal working were calculated to evaluate the correlations between the VAS scores during the BW experiment and total BW time. All statistical analyses were performed using SPSS version 22.0 for Windows (IBM Japan, Tokyo, Japan). P < 0.05 was considered significant.
3. RESULTS
Table 2 shows the data for each subject from the final 20 minutes of the BW experiment. They engaged in BW 7.4 ± 4.7 times (range 4‐19 times), and the duration of each BW was 8.6 ± 4.8 seconds (range 2.7‐17.3 seconds). The total BW time was 57.6 ± 36.5 seconds (range 20.6‐121.0 seconds), comprising 4.8% ± 3.0% (range 1.7%‐10.1%) of total working time.
Table 2.
Blind working time during a 20‐min period
| Subject number | Age (y) | Frequency | Mean duration (s) | Total duration (s) | Proportion of total time (%) |
|---|---|---|---|---|---|
| 1 | 40 | 9 | 12.3 ± 8.0 | 110.8 | 9.2 |
| 2 | 40 | 10 | 7.2 ± 8.1 | 71.9 | 6.0 |
| 3 | 28 | 6 | 3.6 ± 1.4 | 21.7 | 1.8 |
| 4 | 52 | 4 | 5.2 ± 2.4 | 20.6 | 1.7 |
| 5 | 51 | 5 | 11.8 ± 8.1 | 58.8 | 4.9 |
| 6 | 38 | 19 | 2.7 ± 0.9 | 51.1 | 4.3 |
| 7 | 30 | 4 | 17.3 ± 16.5 | 69.3 | 5.8 |
| 8 | 48 | 9 | 13.4 ± 5.2 | 121.0 | 10.1 |
| 9 | 33 | 4 | 7.4 ± 5.0 | 29.3 | 2.4 |
| 10 | 46 | 4 | 5.5 ± 1.0 | 22.0 | 1.8 |
The IBI was 6.2 ± 5.6 seconds during normal working and 5.5 ± 4.5 seconds during the BW experiment, a difference that was not significant (P = 0.245). However, the mean of three IBIs immediately after each BW during the 20‐minute BW experiment was 2.7 ± 1.0 seconds, significantly shorter than the IBI during normal working (P = 0.042) (Figure 1).
Figure 1.
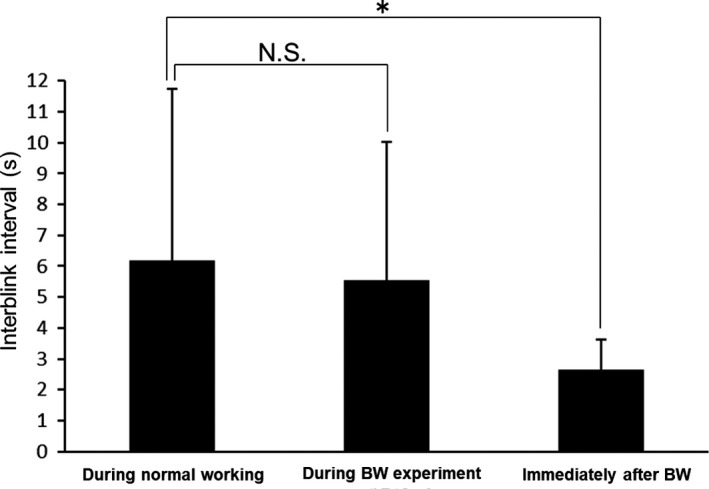
Interblink interval (IBI) during blind working (BW). There is no significant difference between the IBI during a 20‐min period of normal working and that during a 20‐min period of the BW experiment, but the mean of three IBIs immediately after BW during the BW experiment is significantly shorter than that during normal working. N.S.: Not significant. *P < 0.05
The VAS scores for dry eye, ocular fatigue, and blurred vision were 49.7 ± 27.8, 54.3 ± 25.9, and 39.6 ± 27.0, respectively, during normal working and 29.1 ± 20.7, 29.1 ± 24.1, and 26.5 ±2 0.6, respectively, during the BW experiment. The scores for all three symptoms were significantly lower during the BW experiment than during normal working (P = 0.003, 0.004, and 0.024, respectively) (Figure 2). The VAS scores for ocular fatigue were significantly correlated with total BW time (ρ = –0.694, P = 0.038), but there was no significant correlation with either dry eye (ρ = –0.512, P = 0.159) or blurred vision (ρ = –0.121, P = 0.757).
Figure 2.
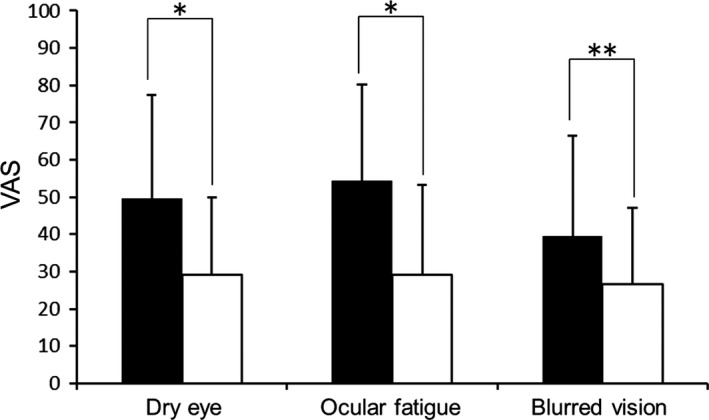
Subjective symptoms after blind working (BW). Dry eye, ocular fatigue, and blurred vision improve after the BW experiment. ■: Normal working. □: BW experiment. *P < 0.01. **P < 0.05
4. DISCUSSION
Guidelines on VDT work are inconsistent, varying from country to country.15 Measures for the management of breaks during VDT work (Table 1) also vary, with no actual figures stipulated by the United Kingdom, but included in the guidelines used in the United States and Japan. In the US, these figures are only recommendations, but in Japan, the Ministry of Health, Labour and Welfare has issued guidance that they are to be complied with. Breaks during VDT work are defined as follows: “Time in which VDT work is temporarily interrupted, exercises such as stretching different parts of the body are performed, or other tasks are carried out,” meaning that work is included in breaks as long as it is non‐VDT related. It is assumed that breaks need not be stipulated during non‐VDT work, as this does not involve looking at a screen, but they are required during VDT work because this entails continuously looking at a screen. This is because the various ophthalmic symptoms caused by VDT work are considered to result directly from the action of looking at the screen. Based on the above reasons, in this study, the Japanese guidelines were followed by defining “breaks during VDT work” as “breaks from looking at the screen.” It should be noted that VDT users in this study could engage in BW during VDT work. During BW, the subjects were not looking at the screen, and this therefore corresponded to a break. None of the countries mentioned above has formulated new measures for breaks in VDT work guidelines, but BW may provide a new method of taking breaks during VDT work. We therefore discuss the length, frequency, and timing of BW in a comparison of guidelines and studies of breaks during VDT work.
In terms of the length of BW, this study showed that 4.8% ± 3.0% of working time could be occupied by BW, and the longer the duration of BW, the lower was the level of ocular fatigue. For example, if a shift of VDT work lasts 4 hours, Japanese guidelines state that breaks should account for 13.8%‐21.3% of total working time, and US guidelines state that they should account for 4.2%‐18.8%. For the subject in this study with the shortest total BW time, it accounted for 1.7% of total working time, which means that BW time was about the same length of time as a short break according to the Japanese guidelines. For the subject with the longest total BW time, it accounted for 10.1% of total working time. In terms of the US guidelines, the tasks undertaken by the subjects corresponded to “repetitive work tasks,”10 and BW time did not fully cover the entire break time required during VDT work. However, the present results suggest that BW may shorten the time spent looking at the screen and the required break time. According to the Japanese guidelines, VDT work may be divided into six different categories, comprising simple input, binding work, surveillance, writing/editorial work, technical work, and other types, and the subjects of this study were engaged in simple input type VDT tasks. It may be envisaged that variations in BW time will be even greater depending on the different professions, types of business, and individual abilities of VDT workers, as well as the nature of their work and the time when they perform it. For example, traffic monitoring and other surveillance type tasks that require constant watching of a screen will not offer much time for BW. Conversely, technical VDT workers engaged in tasks such as programming or technical drawing may be able to take more time for BW. We do not believe that BW time can fully cover the entire break time required for all VDT workers. We consider that once individuals have established the optimum frequency and duration of BW for themselves, they can combine BW with other break times in order to manage VDT working time appropriately.
With respect to the frequency of BW, subjects engaged in BW 7.4 ± 4.7 times (range 4‐19 times) in a 20‐minute period, which is a greater number of breaks than those stipulated in either the Japanese or US guidelines. The UK guidelines state that “Short, frequent breaks are more satisfactory than occasional, longer breaks,”11 and Balci et al16 reported that among the three work‐rest schedules (60‐minute work/10‐minute rest, 30‐minute work/5‐minute rest, and 15‐minute work/micro breaks), the 15/micro schedule resulted in the lowest eyestrain and blurred vision, and the highest speed, accuracy, and performance, suggesting that BW may also help improve work productivity.
The timing of BW is also extremely important. The UK guidelines state that “The timing of the break is more important than its length,” and that “Informal breaks appear from study evidence to be more effective in relieving ocular fatigue than formal rest breaks.”11 As VDT users may feel some resistance to taking the sort of enforced, passive breaks stipulated by the Japanese guidelines, they may also not be effective. Although the subjects in this study were able to use BW as many times as they liked while working, in reality, VDT users will probably not take every opportunity to engage in BW. Individual VDT users should choose to engage in BW appropriately when required and for as long as they are able to do so, and one advantage of BW is that the timing of actively taking informal breaks can be controlled.
As blinking is heavily influenced by external factors,17 the IBI should be measured under conditions as near to natural as possible. As an IBI method, we also investigated methods of regularly closing the eyes during a work‐rest schedule comprising a 15‐minute work period and micro breaks.16 In this method, however, even if blinking was not directly mentioned in the explanation prior to the experiment, subjects would still be aware that they were being video recorded when their eyes were open, and this would risk affecting the IBI. In the method used in this study, it was explained before the experiment that it concerned BW, so that the subjects primarily paid attention to closing their eyes, and they were unaware that their blinking while their eyes were open would be analyzed. In this study, the subjects were also faced with a camera immediately in front of their eyes, placing them under stress, and they were asked to close their eyes, something they did not usually do. To measure blinking under these circumstances, intervention involving eye closure should be minimized. Compared with the method of regularly closing the eyes mentioned above, which entails engaging in an unfamiliar task while compulsorily closing the eyes regularly in response to an external sound or words, the method used in this study enabled the subjects to work as usual in their regular workplace in an extremely relaxed environment, engaging irregularly in BW with no external elements, and thus enabled the IBI to be measured with greater accuracy.
The mechanism whereby the IBI became shorter immediately after BW might have involved reactive blinking due to light stimulation, the induction of voluntary blinking from the psychological perspective after the temporary cutoff in vision,17 or the stagnation of tear circulation as a result of BW, causing diminished tear stability that would be improved by blinking.18, 19 Concentrating on looking at a screen also reduces blinking,20, 21 and conversely, paying attention to the act of closing the eyes in BW may induce blinking, which is also the act of closing the eyes and increase its frequency.
In 2016, the diagnostic criteria for dry eye were revised to “BUT ≤ 5 seconds with subjective symptoms (eye discomfort or abnormal visual function),”22 and these two factors are viewed as clinically important in dry eye. In this study, subjective symptoms of dry eye and ocular fatigue were improved by BW. BUT has been reported to be ≤5 seconds in 78.6% of VDT users,23 and another study found that BUT is shortened in VDT users because of a decreased frequency of blinking and an increased rate of tear evaporation.1, 24 If the time spent looking at the screen could be reduced by BW, this would decrease the time during which the cornea was exposed, diminishing tear evaporation. The finding in this study that the IBI is shorter immediately after BW also suggests that improved tear exchange as a result of BW may help improve the reduction in BUT. These findings indicate that BW may contribute to decreasing dry eye among VDT users. Ocular fatigue and blurred vision were also improved by BW. The improvement in dry eye described above may also have improved these symptoms. Another reason may be that, although the sympathetic nervous system predominates under light stimulation, when the eyes are closed, 100% of external light is blocked, and the iris sphincter and ciliary muscle relax, reducing the strain on adjustment function.
Neither the US nor the UK guidelines mention closing the eyes during breaks in VDT work. The UK guidelines for breaks do state that “focusing eyes on distant objects can be helpful,”11 but this may not be possible in a small room or if sitting facing a wall. Not only does closing the eyes have the advantages of BW described above, but the accommodative resting position is also maintained,25 and blocking out information from the outside world may help improve concentration after the break, meaning that it may also be useful during breaks in VDT work.
The time spent on close work by not only the VDT users but also people in general has increased dramatically in recent years, and an advantage of the use of BW is that it is not limited to VDT users or dry‐eye patients. The use of BW is premised on ensuring both the safety of the individual concerned and the understanding in the workplace, and that it must be performed with caution goes without saying. In our contemporary world, it is hoped that, in this age of intense close work, people will soon be able to selectively receive visual information from the outside world through new ways of using the eyes, such as blind learning and blind listening, in addition to BW, and to benefit greatly from these methods.
This study had a number of limitations. The first was its nature as a short, small‐scale study with only 10 subjects. However, there was individual variation in BW between the subjects depending on their ability, judgment, and level of familiarization. It may also be envisaged that BW time will vary greatly among VDT users overall depending on their profession and the contents of the task involved. For this reason, measuring the BW time on a large scale would not be particularly meaningful. In relation to breaks while working, the UK guidelines also state “it is the nature and mix of demands made by the job which determine the length of break necessary to prevent fatigue,”11 and they do not indicate a specific optimum break length. Rather, the significant point in this study is the focus on the performance of several episodes of BW by all subjects in the short period of 20 minutes, which has not been attempted in previous studies, to the best of our knowledge. Second, IBI evaluation was performed for 10 subjects over a 20‐minute period. Previous studies of the IBI and blinking rate evaluated these parameters using 7,13 10,26 and 1214 subjects; thus, this study was not inferior to previous ones on this point. Third, in this study, it was shown in 1 hour using a VAS that BW improved subjective symptoms. In their study of 10 VDT users, Balci et al22 also reported that the work‐rest schedule consisting of a 15‐minute work period and micro breaks was useful for improving ocular fatigue, with the assessment performed over the short period of 1 hour. VAS evaluation is widely used in the ophthalmologic field,27, 28 and Ren et al27 also found that VAS scores of ocular fatigue improved with applications of a new warm moist air device to the eyes of the subjects, which was evaluated over a 1‐hour period as well. Fourth, as the subjects were not all performing the same task, the results may have been affected. The focus of this study was on BW and the IBI, and it was therefore carried out under conditions close to those of actual clinical situations. However, studies are also required to investigate the use of BW in standardized tasks under consistent conditions, particularly using a VAS to assess subjective symptoms. Because the study was carried out in an actual workplace, tests for dry eye, such as BUT and tear meniscus height, could not be carried out immediately after video recording. We intend to continue to carry out studies of the IBI when BW is performed for a specified time, of subjective symptoms, and of dry‐eye tests after the performance of BW, using more subjects and over a longer time period, and with the subjects performing standardized tasks under consistent conditions.
5. CONCLUSION
In this study, it was shown that, in VDT users engaged in BW during VDT work, the IBI was shorter immediately after BW, and BW improved subjective symptoms. These results suggest that BW may provide a more effective measure for the management of VDT working time, and that it may be possible to add BW as a new decision‐making criterion in VDT work guidelines.
DISCLOSURES
Approval of the research protocol: N/A. Informed consent: N/A. Registry and registration no. of the study/trial: N/A. Animal studies: N/A.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest.
ACKNOWLEDGMENTS
We are grateful to all the staff of Kuwano Kyoritsu Hospital (Fukushima, Japan) for their support in this study.
Fujita H, Sano K, Baba T, Tanaka T, Ohno‐Matsui K. Blind working time in visual display terminal users. J Occup Health. 2019;61:175–181. 10.1002/1348-9585.12027
REFERENCES
- 1. Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med. 1993;328(8):584. [DOI] [PubMed] [Google Scholar]
- 2. Uchino M, Schaumberg DA, Dogru M, et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology. 2008;115(11):1982‐1988. [DOI] [PubMed] [Google Scholar]
- 3. Thorud HM, Helland M, Aarås A, et al. Eye‐related pain induced by visually demanding computer work. Optom Vis Sci. 2012;89(4):E452‐464. [DOI] [PubMed] [Google Scholar]
- 4. Woods V. Musculoskeletal disorders and visual strain in intensive data processing workers. Occup Med (Lond). 2005;55(2):121‐127. [DOI] [PubMed] [Google Scholar]
- 5. Piccoli B. A critical appraisal of current knowledge and future directions of ergophthalmology: consensus document of the ICOH Committee on “Work and Vision”. Ergonomics. 2003;46(4):384‐406. [DOI] [PubMed] [Google Scholar]
- 6. Anshel JR. Visual ergonomics in the workplace. AAOHN J. 2007;55(10):414‐420. [DOI] [PubMed] [Google Scholar]
- 7. American Optometric Association: Computer Vision Syndrome. [Online]. 2018 [cited 2018 Aug 7]; Available from: URL: https://www.aoa.org/patients-and-public/caring-for-your-vision/protecting-your-vision/computer-vision-syndrome?sso=y
- 8. American Academy of Ophthalmology: Computers, Digital Devices and Eye Strain. [Online]. 2018 [cited 2018 Aug 7]; Available from: URL: https://www.aao.org/eye-health/tips-prevention/computer-usage
- 9. Ministry of Health, Labour and Welfare: Guidelines for Industrial Health Controls of VDT Operations. [Online]. 2002 [cited 2018 Aug 7]; Available from: URL: http://www.mhlw.go.jp/file/06-Seisakujouhou-11200000-Roudoukijunkyoku/0000184703.pdf (in Japanese).
- 10. Department of Labor, Working: Safely with Video Display Terminals. [Online]. 1997 [cited 2018 Aug 7]; Available from: URL: https://www.osha.gov/Publications/videoDisplay/videoDisplay.html
- 11. Health and Safety Executive. Work with display screen equipment. [Online]. 1992 [cited 2018 Apr 25]; Available from: URL: http://www.hse.gov.uk/pubns/priced/l26.pdf
- 12. Johnston PR, Rodriguez J, Lane KJ, et al. The interblink interval in normal and dry eye subjects. Clin Ophthalmol. 2013;7:253‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Miyake‐Kashima M, Dogru M, Nojima T, et al. The effect of antireflection film use on blink rate and asthenopic symptoms during visual display terminal work. Cornea. 2005;24(5):567‐570. [DOI] [PubMed] [Google Scholar]
- 14. Cardona G, Gómez M, Quevedo L, et al. Effects of transient blur and VDT screen luminance changes on eyeblink rate. Cont Lens Anterior Eye. 2014;37(5):363‐367. [DOI] [PubMed] [Google Scholar]
- 15. Mar Seguí MD, Ronda E, Wimpenny P. Inconsistencies in guidelines for visual health surveillance of VDT workers. J Occup Health. 2012;54(1):16‐24. [DOI] [PubMed] [Google Scholar]
- 16. Balci R, Aghazadeh F. The effect of work‐rest schedules and type of task on the discomfort and performance of VDT users. Ergonomics. 2003;46(5):455‐465. [DOI] [PubMed] [Google Scholar]
- 17. Stern JA, Walrath LC, Goldstein R. The endogenous eyeblink. Psychophysiology. 1984;21(1):22‐33. [DOI] [PubMed] [Google Scholar]
- 18. Palakuru JR, Wang J, Aquavella JV. Effect of blinking on tear dynamics. Invest Ophthalmol Vis Sci. 2007;48(7):3032‐3037. [DOI] [PubMed] [Google Scholar]
- 19. Nakamori K, Odawara M, Nakajima T, et al. Blinking is controlled primarily by ocular surface conditions. Am J Ophthalmol. 1997;124(1):24‐30. [DOI] [PubMed] [Google Scholar]
- 20. Tsubota K, Nakamori K. Effects of ocular surface area and blink rate on tear dynamics. Arch Ophthalmol. 1995;113(2):155‐158. [DOI] [PubMed] [Google Scholar]
- 21. Freudenthaler N, Neuf H, Kadner G, et al. Characteristics of spontaneous eyeblink activity during video display terminal use in healthy volunteers. Graefes Arch Clin Exp Ophthalmol. 2003;241(11):914‐920. [DOI] [PubMed] [Google Scholar]
- 22. Tsubota K, Yokoi N, Shimazaki J, et al. New perspectives on dry eye definition and diagnosis: a consensus report by the Asia dry eye society. Asia Dry Eye Society. Ocul Surf. 2017;15(1):65‐76. [DOI] [PubMed] [Google Scholar]
- 23. Uchino M, Yokoi N, Uchino Y, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol. 2013;156(4):759‐766. [DOI] [PubMed] [Google Scholar]
- 24. Yaginuma Y, Yamada H, Nagai H. Study of the relationship between lacrimation and blink in VDT work. Ergonomics. 1990;33(6):799‐808. [DOI] [PubMed] [Google Scholar]
- 25. Gilmartin B. A review of the role of sympathetic innervation of the ciliary muscle in ocular accommodation. Ophthalmic Physiol Opt. 1986;6(1):23‐37. [PubMed] [Google Scholar]
- 26. Wu Z, Begley CG, Port N, et al. The effects of increasing ocular surface stimulation on blinking and tear secretion. Invest Ophthalmol Vis Sci. 2015;56(8):4211‐4220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ren Y, Chen J, Zheng Q, et al. Short‐term effect of a developed warming moist chamber goggle for video display terminal‐associated dry eye. BMC Ophthalmol. 2018;18(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fujita H, Sano K, Ohno‐Matsui K, et al. Ocular discomfort at the initial wearing of rigid gas permeable contact lenses. Jpn J Ophthalmol. 2004;48(4):376‐379. [DOI] [PubMed] [Google Scholar]


