Abstract
Objectives
This longitudinal study aimed to investigate the causal relationships between social support at work and mental health in terms of mental distress. Despite assuming social support at work to be associated with less mental distress, reversed and reciprocal relationships were investigated as well.
Methods
Self‐reports in questionnaires of social support and mental distress were collected longitudinally, with annual measurements over three consecutive years, among 301 office workers (57% women) in Sweden. Cross‐lagged structural equation modeling was used to test the hypotheses.
Results
The reciprocal causation model was considered the best‐fitting model. The results suggest that social support and mental distress influenced each other negatively, but with a delayed effect. Specifically, this involves Time 1 levels of social support being negatively associated with Time 2 levels of mental distress, while Time 2 levels of mental distress were negatively associated with Time 3 levels of support.
Conclusions
The findings partly align with the hypothesis that social support is related to lower levels of mental distress but also suggest that mental distress can reduce levels of social support. While the findings also suggest a mutual interrelation between social support and mental distress, this is not a consistent reciprocal causation. Rather, and due to the variation in reciprocity between time points, it appears to be a cyclical process, which needs further investigation.
Keywords: longitudinal mechanisms, occupational health, support
1. INTRODUCTION
Social support is considered a traditional factor of the work environment.1, 2 Specifically, social support from colleagues and supervisors may constitute a resource for workers to successfully carry out their work. Social support has been consistently linked to various mental health outcomes, including mental distress, which is common in working populations.1, 3, 4, 5 While much research assumes a one‐directional relationship, with social support influencing mental health outcomes, the detailed characteristics of the longitudinal relationship between work‐related social support and mental distress remain to be understood.6, 7, 8 Given the few empirical studies, this longitudinal study focused specifically on the associations between social support and mental distress.
1.1. Social support and mental distress
Within an occupational setting, social support can be conceptualized in different ways. For instance, conceptualizations can include various types of support, which, in turn, emanate from different sources, including coworkers and supervisors.1 While some studies have investigated social support from specific sources separately (eg, coworkers or supervisors only), others have merged different sources into a broader overall conceptualization.1, 2 While the conceptualizations of social support range from broad to specific, most research relies on self‐reports in questionnaires. The present study followed the broad and general approach1, 2 and, thus, investigated the overall perceptions of social support from various sources at work without differentiating between these.
Similar to social support, mental health is an umbrella term with many conceptualizations.9 Research regarding occupational health has traditionally investigated mental health in terms of ill‐health, dysfunction, and problems ranging from mental diseases and disorders to stress, discomfort, and anxiety.3 Some research has included physician ratings or objective registry data of diagnoses. Another common approach involves the use self‐reports in questionnaires to describe subjective health complaints including anxiety and mental distress that are prevalent among working adults.3, 7, 10 Operationalizations of mental distress vary9 and the present study used an established and commonly used self‐report measure, namely the General Health Questionnaire.11, 12
1.2. Relationships between social support at work and mental distress
Different theoretical models assume that social support is linked to favorable mental health outcomes.2, 13 Aligning with such assumptions are the abundant empirical findings showing positive effects of work‐related social support on mental health,1, 3, 4, 5 with social support reducing mental distress.3, 14, 15 This is referred to as the normal relationship.6, 7 Moreover, empirical findings have suggested a reversed relationship meaning that mental health problems, including mental distress, are associated with less social support.8, 16 An additional, third assumption suggests a reciprocal association between the two factors.7, 8
1.2.1. The normal relationship
Within occupational settings, the majority of studies has investigated the normal relationship between social support and different mental health outcomes.7, 8, 16, 17, 18 With work‐related social support being considered a resource, social support is typically expected to have positive effects on mental health outcomes for instance in terms of less mental distress. Instead, poor social support is expected to yield negative effects in terms of more mental distress.6, 7, 8 Accordingly, there is an assumed main effect of social support at one time point on mental health sometime later. Support for this normal causation is reflected in many studies6, 7, 8 showing an association between social support at one time point and better mental health outcomes, including less mental distress, later on.
1.2.2. The reversed relationship
In contrast to normal causation, reversed relationships refer to associations being opposed to any assumed one‐directional effects.6, 7, 8 Regarding work‐related social support and mental health outcomes, a reversed relationship involves mental distress at one time point having an effect social support later on. Two main mechanisms have been suggested to explain such reversed relationships, namely (i) the health selection hypothesis, and (ii) the perception hypothesis.8 According to the health selection hypothesis, healthy employees are more likely to stay in or move to jobs with more favorable working conditions while the less healthy are more likely to have less favorable conditions. Thus, employees suffering from mental distress would be staying in situations involving poorer work‐related social support.8 The perception hypothesis, in turn, assumes that any changes in employees’ health and well‐being involve changes in employee evaluations of their occupational settings. Specifically, employees suffering from mental distress may, over time, evaluate their work situation more negatively in not perceiving any social support that they receive or in not adequately recalling situations involving social support.8
1.2.3. The reciprocal relationship
Besides the normal and reversed relationships,6, 7, 8 empirical findings also support reciprocal associations.6, 7, 8, 16, 17 Reciprocal relationships refer to any associations that influence each other mutually over time. For instance, this involves work‐related social support and mental distress continuously driving each other, thus propelling any positive or negative change over time. Reciprocal relationships have been found between different psychosocial job characteristics and mental health outcomes, including depression.6, 7, 8, 16, 17, 18
1.3. Present study
Taken together, most empirical studies have assumed and focused exclusively on investigating the one‐directional relationship between work‐related social support and mental health outcomes.6, 7, 8, 16, 17 However, existing longitudinal research investigating normal, reversed, and reciprocal associations, support all but also suggest that the normal relationship is the most prominent.6, 7, 8, 16
This study set out to add to the existing research of the associations between psychosocial factors at work and a common mental health outcome through investigating the longitudinal relationships between work‐related social support and mental distress among white‐collar workers using a three‐wave design and testing specifically the short‐term associations (ie, associations between each specific point in time). This design allows for testing different types of potential causal relationships between variables. With strong support for normal causation, this association was expected. Specifically, hypothesis 1 assumed social support to be positively associated with future mental distress in so that, over time, more social support would be associated with less mental distress (the normal relationship). However, given the support for the reversed and reciprocal relationships,6, 7, 8, 16, 17, 18 two additional hypotheses were formulated. Hypothesis 2 assumed mental distress to be negatively associated with future social support in so that, over time, more mental distress would be related to less social support (the reversed relationship). Hypothesis 3 assumed social support and mental distress to be mutually interrelated over time (the reciprocal relationship).
2. Materials and Methods
2.1. Participants and data collection
All employees of a Swedish accounting firm were invited to participate in a longitudinal survey study of working conditions and health‐related outcomes19, 20 which passed ethical vetting and was approved by the Regional Ethics Committee (Ref. No. 2007/932‐31). Data were collected annually (around September to late October/early November each year), at three time points, Time 1 (T1, 2007), Time 2 (T2, 2008), and Time 3 (T3, 2009). To avoid seasonal variation, which is prominent in accounting with deadlines set by national tax agencies, we chose a 1‐year time‐span. Questionnaires, along with information regarding the research project and research ethics, were mailed to the home address of each employee. At every time point, two reminders were mailed. First, a postcard was sent after approximately 2 weeks to remind those who were yet to return their questionnaires. A second reminder was mailed an additional 2 weeks later and also included a questionnaire. Participants returned their completed questionnaires to the research team in pre‐addressed postage‐paid envelopes.
Response rates varied over time. Of 725 individuals employed at T1, 571 (79%) responded. At T2, 782 employees received a questionnaire and 567 (72%) responded. At T3, 579 (75%) of the 776 employees receiving a questionnaire responded. Overall, 979 employees received a questionnaire, once, twice or three times. Of the 545 employees who received the questionnaire at all three time points, 310 (57%) participated in all waves.
A missing value analysis (MVA) revealed that 14 out of 310 participants had partial internal attrition. To be included in the final sample, participants had to fulfill the following inclusion criteria: having had completed at least half of the (i) social support items and (ii) mental distress items at each wave. Nine of the 14 respondents failed to meet these criteria and were excluded from further analysis. For the remaining five participants, missing values were imputed using the expectation‐maximization algorithm (EM) method, after Little's MCAR test were found to be found nonsignificant, with values missing completely at random.21, 22 The imputation was performed separately for each measure (ie, social support and mental distress) at each wave. This resulted in 17 (out of 25 284) imputed values. The effective sample thus included 301 cases with 17 imputed values. Participants’ mean age at Time 1 was 44 years (SD = 11), 57% were women, and the majority (71%) had a university degree.
2.2. Measures
The questionnaire covered, aside demographics, social support, and mental distress.
Social support was measured using six items asking about social support at work,23, 24 including social support from co‐workers (eg, “When I encounter problems at work, there is always a co‐worker to turn to”) and supervisors (eg, “I always receive help from my manager when difficulties in my work arise”). Response alternatives ranged from 1 (strongly disagree) to 5 (strongly agree), with higher scores indicating more social support. Internal consistency coefficients (Cronbach's alphas) across time points were good (T1 = 0.85; T2 = 0.86; T3 = 0.86).
Mental distress was measured using the 12‐item version of the General Health Questionnaire (GHQ‐12) that has been adapted to and widely used in occupational settings.12 Asking about experiences over the past 2 weeks, the items for instance cover ability to cope, depressive symptoms, and problems sleeping. Six of the items were positively framed (eg, “Have you over the past 2 weeks felt that you are playing a useful part in things?”), while six were negatively framed (eg, “Have you over the past 2 weeks felt unhappy and depressed?”). Responses were given along a 4‐point scale ranging from 1 (never; recoded to = 0) to 4 (always; recoded to 3). All items were coded with high scores indicating high‐mental distress. Internal consistency coefficients (Cronbach's alphas) across time points were good (T1 = 0.82; T2 = 0.84; T3 = 0.85).
Control variables included gender (1 = woman, 0 = man), age (in years), and education (1 = university education, 0 = no university education).
2.3. Statistical analyses
Statistical analyses were performed in LISREL 8,25 using the maximum likelihood (ML) estimation method based on the variance‐covariance matrix. To reduce the number of observed indicators, the observed items were combined into three parcels per construct at each time point.26, 27 For each measure, the assignment of items to parcels was based on the factor loadings from a one‐factor confirmatory factor analysis. The item with the highest loading and the item with the lowest loading were assigned to the first parcel. Then the item with the second highest loading and the item with the second lowest loading were assigned to the second parcel. This process continued until all items had been distributed. For each of the three parcels, the mean of the assigned items was computed at each time point and used as an indicator of the latent variable (social support and mental distress, respectively) in the subsequent analyses. Table 1 shows correlations, means, and standard deviations for all indicators of the structural equations models, and demographic control variables.
Table 1.
Correlations and descriptive statistics for the indicators and control variables at Time 1 (T1), Time 2 (T2), and Time 3 (T3)
| Variable |
Time 1 T1 |
Time 2 T2 |
Time 3 T3 |
Time 1 T1 |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SS1 | SS2 | SS3 | MD1 | MD2 | MD3 | SS1 | SS2 | SS3 | MD1 | MD2 | MD3 | SS1 | SS2 | SS3 | MD1 | MD2 | MD3 | Gender | Age | M | SD | |
| T1SS1 | 1 | 3.85 | 0.80 | |||||||||||||||||||
| T1SS2 | 0.77a | 1 | 3.55 | 0.85 | ||||||||||||||||||
| T1SS3 | 0.77a | 0.76a | 1 | 3.79 | 0.85 | |||||||||||||||||
| T1MD1 | −0.22a | −0.26a | −0.22a | 1 | 0.86 | 0.42 | ||||||||||||||||
| T1MD2 | −0.20a | −0.25a | −0.24a | 0.66a | 1 | 0.55 | 0.42 | |||||||||||||||
| T1MD3 | −0.18a | −0.19a | −0.18a | 0.68a | 0.61a | 1 | 0.54 | 0.38 | ||||||||||||||
| T2SS1 | 0.49a | 0.41a | 0.50a | −0.20a | −0.11 | −0.15a | 1 | 3.79 | 0.84 | |||||||||||||
| T2SS2 | 0.52a | 0.55a | 0.54a | −0.25a | −0.14a | −0.17a | 0.76a | 1 | 3.50 | 0.91 | ||||||||||||
| T2SS3 | 0.46a | 0.45a | 0.54a | −0.21a | −0.13a | −0.17a | 0.82a | 0.78a | 1 | 3.71 | 0.87 | |||||||||||
| T2MD1 | −0.27a | −0.30a | −0.23a | 0.56a | 0.46a | 0.44a | −0.32a | −0.37a | −0.32a | 1 | 0.92 | 0.45 | ||||||||||
| T2MD2 | −0.16a | −0.22a | −0.19a | 0.42a | 0.59a | 0.38a | −0.20a | −0.23a | −0.22a | 0.67a | 1 | 0.56 | 0.44 | |||||||||
| T2MD3 | −0.24a | −0.22a | −0.19a | 0.44a | 0.48a | 0.54a | −0.25a | −0.25a | −0.24a | 0.62a | 0.60a | 1 | 0.54 | 0.41 | ||||||||
| T3SS1 | 0.44a | 0.41a | 0.46a | −0.24a | −0.18a | −0.24a | 0.57a | 0.56a | 0.59a | −0.31a | −0.21a | −0.26a | 1 | 3.73 | 0.86 | |||||||
| T3SS2 | 0.38a | 0.44a | 0.43a | −0.26a | −0.21a | −0.20a | 0.48a | 0.62a | 0.53a | −0.35a | −0.28a | −0.24a | 0.80a | 1 | 3.54 | 0.86 | ||||||
| T3SS3 | 0.42a | 0.41a | 0.45a | −0.22a | −0.20a | −0.18a | 0.55a | 0.58a | 0.58a | −0.28a | −0.23a | −0.22a | 0.82a | 0.80a | 1 | 3.67 | 0.86 | |||||
| T3MD1 | −0.12a | −0.17a | −0.16a | 0.53a | 0.46a | 0.41a | −0.19a | −0.30a | −0.22a | 0.56a | 0.48a | 0.40a | −0.37a | −0.44a | −0.37a | 1 | 0.91 | 0.52 | ||||
| T3MD2 | −0.12a | −0.19a | −0.19a | 0.45a | 0.57a | 0.42a | −0.14a | −0.18a | −0.15a | 0.50a | 0.58a | 0.46a | −0.31a | −0.31a | −0.26a | 0.72a | 1 | 0.60 | 0.45 | |||
| T3MD3 | −0.17a | −0.16a | −0.19a | 0.47a | 0.41a | 0.53a | −0.17a | −0.19a | −0.18a | 0.45a | 0.40a | 0.56a | −0.34a | −0.30a | −0.31a | 0.68a | 0.67a | 1 | 0.56 | 0.43 | ||
| Gender (woman) | −0.03 | −0.07 | −0.06 | 0.00 | 0.15a | 0.00 | −0.01 | 0.01 | −0.06 | 0.07 | −0.13a | −0.05 | −0.08 | −0.17a | −0.14a | 0.18a | 0.14a | 0.11 | 1 | 0.57 | — | |
| Age | −0.04 | −0.05 | 0.03 | 0.02 | −0.00 | − 0.03 | −0.05 | −0.05 | 0.05 | 0.00 | −0.03 | −0.06 | 0.06 | 0.09 | 0.07 | −0.05 | −0.02 | −0.10 | −0.20a | 1 | 43.52 | 11.07 |
| Education (university) | −0.12a | −0.07 | −0.11 | −0.07 | −0.10 | −0.03 | −0.05 | 0.06 | 0.05 | −0.10 | −0.13a | −0.03 | −0.02 | 0.13a | 0.03 | −0.16a | −0.10 | −0.06 | −0.27a | −0.18a | 0.71 | — |
SS, social support; MD, mental distress; the numbers after these abbreviations refer to each of the three parcels/indicators for each construct at each time point.
Gender (1 = woman), age (in years) and education (1 = university level) were measured at Time 1. Scale range: Social support (SS): 10‐5; mental distress (MD) indicators: 0‐3.
P < 0.05 (N = 301). —, Not applicable.
Before the structural analyses, and following previous recommendations,28 confirmatory factor analyses (CFA) were conducted to test the measurement models of the latent variables at each time point. The hypothesized six‐factor solution (social support and mental distress at T1, T2, and T3, respectively) was contrasted with a three‐factor solution reflecting the three time points (with all T1 indicators loading on one factor, all T2 indicators on a second factor, and all T3 indicators on a third factor) and a two‐factor model reflecting social support and mental distress regardless of time. The hypothesized model was also contrasted with a uni‐factor model (specifying all indicators to load on a single factor) and a structural null model (assuming no associations between indicators). Given that the measurement error of the same indicator is expected to correlate over time,29 error terms of the corresponding parcels were allowed to correlate over time, resulting in 18 correlated error terms.
Four structural models, based on the six latent factors, were analyzed to test the structural relationships between social support and mental distress over time. In all models, social support and mental distress were correlated within each time point. Initially, a baseline model (Model 0) was tested. This specified only the autoregressive effects within constructs over time. The normal causation model (Model 1) specified effects of social support on mental distress over time (ie, effects of T1 support on T2 distress; of T2 support on T3 distress). The reversed causation model (Model 2) tested the assumption of reversed relationships over time, by specifying effects of mental distress on social support over time (ie, effects of T1 distress on T2 support, and of T2 distress on T3 support). Finally, the reciprocal causation model (Model 3) was tested. Model 3 included the two pathways from the normal causation model (Model 1) and the two pathways from the reversed causation model (Model 2). Although aiming to study the short‐term effects, less parsimonious models including all lagged effects over time were tested as well. The cross‐lagged models were tested with and without the three control variables (gender, age, and education).
Following recommendations,30 the goodness‐of‐fit of the measurement and structural models were evaluated using several indicators. Besides the chi‐square statistic, the relative chi‐square was used. This divides the chi‐square with the degrees of freedom of the model,31 with a cut‐off <2 indicating satisfactory relative fit.22 Moreover, the following fit indices were used: the standardized root mean square residual (SRMR), the root mean square error of approximation (RMSEA), and the comparative fit index (CFI). Cut‐offs of SRMR < 0.09, RMSEA < 0.06, and CFI > 0.96 have been suggested to indicate satisfactory model fit32 and yield lower rates of Type I and Type II errors.33 For model comparisons, the chi‐square difference test, testing for significant differences between alternative models was used along with the akaike information criterion (AIC), for which the lowest value represents the best‐fitting model.32
3. RESULTS
3.1. Measurement models
Table 2 presents goodness‐of‐fit indices from the confirmatory factor analyses of the measurement models. The hypothesized six‐factor model, representing social support and mental distress at the three time points, respectively, provided a good fit. This model also provided a substantially better fit compared to the three‐factor solution specifying a general factor (including both social support and mental distress) at the three different time points, which, in turn, provided a substantially better fit compared to the two‐factor model (specifying a social support factor and a mental distress factor including all time points). The two‐factor model outperformed the uni‐factor model, which had a poor fit but clearly outperformed the structural null model. Based on these results, the six‐factor model was accepted and chosen for the structural analyses. The factor loadings for social support ranged between 0.86 and 0.91, while those for mental distress ranged between 0.75 and 0.87.
Table 2.
Model fit for the different measurement models
| Model | df | χ2 | χ2/df | SRMR | RMSEA | CFI | Model comparisons | |||
|---|---|---|---|---|---|---|---|---|---|---|
| AIC | Models | Δdf | Δχ2 | |||||||
| 0 Independence model | 153 | 8097.56a | 52.93 | 8133.56 | ||||||
| 1 One‐latent factor | 117 | 1800.12a | 15.39 | 0.18 | 0.22 | 0.80 | 1908.12 | 1 vs 0 | 36 | 6297.44a |
| 2 Two‐latent factors (constructs) | 116 | 1386.72a | 11.95 | 0.08 | 0.19 | 0.85 | 1496.72 | 2 vs 1 | 1 | 413.40a |
| 3 Three‐latent factors (time points) | 114 | 963.10a | 8.45 | 0.19 | 0.16 | 0.89 | 1077.10 | 3 vs 2 | 2 | 423.62a |
| 6 Six‐latent factors | 102 | 124.54 | 1.22 | 0.03 | 0.03 | 1.00 | 262.54 | 6 vs 3 | 12 | 838.56a |
P < 0.05.
3.2. Cross‐lagged models
Table 3 shows fit indices for the four structural models analyzing the alternative causal relationships between social support and mental distress over time.1
Table 3.
Model fit for the four tested structural models (excluding control variables)
| Model | df | χ2 | χ2/df | SRMR | RMSEA | CFI | Model comparisons | |||
|---|---|---|---|---|---|---|---|---|---|---|
| AIC | Models | Δdf | Δχ2 | |||||||
| 0 Baseline model (auto‐regressions only) | 110 | 166.66a | 1.52 | 0.07 | 0.041 | 0.99 | 288.66 | |||
| 1 Normal causation | 108 | 161.08a | 1.49 | 0.06 | 0.040 | 0.99 | 287.08 | 1 vs 0 | 2 | 5.58 |
| 2 Reversed causation | 108 | 162.18a | 1.50 | 0.06 | 0.041 | 0.99 | 288.18 | 2 vs 1 | 0 | −1.10 |
| 3 Reciprocal causation | 106 | 153.71a | 1.45 | 0.04 | 0.039 | 0.99 | 283.71 | 3 vs 2 | 2 | 8.47a |
Models including control variables provided a similar fit to data. Models adding effects between Time 1 and Time 3 latent variables also provided a similar fit to data.
P < 0.05
All four models provided an acceptable fit to the data with no substantial differences in fit between these models. Although the CFI was identical across models and the differences in RMSEA were minor, the reciprocal causation model (Model 3) provided a significantly better fit to data as compared the reversed causation (Model 2; Δχ2 = 8.47, P < 0.05) and normal causation (Model 1; Δχ2 = 7.37, P < 0.05) models. Moreover, the reciprocal causation model had the lowest SRMR and the lowest AIC and was consequently accepted as the best‐fitting model.
Figure 1 shows the results of the reciprocal causation model (Model 3). The auto‐regression coefficients of the two constructs over time were strong (0.60‐0.64 for social support and 0.67‐0.71 for mental distress), with constructs being moderately associated within each time point (T1 = −0.30; T2 = −0.38; T3 = −0.45). Social support at Time 1 was associated with lower mental distress at Time 2 (−0.11, P < 0.05), while social support at Time 2 was unrelated to mental distress at Time 3. There was also a weak, but statistically significant negative effect of mental distress at Time 2 on social support at Time 3 (−0.13, P < 0.05), but no significant association between Time 1 mental distress and Time 2 social support. Thus, the results suggest that the two constructs influenced each other negatively, but with a delayed effect. Specifically, this is shown in Time 1 levels of social support being negatively associated with Time 2 levels of mental distress, while Time 2 levels of mental distress were negatively associated with Time 3 levels of support.2
Figure 1.
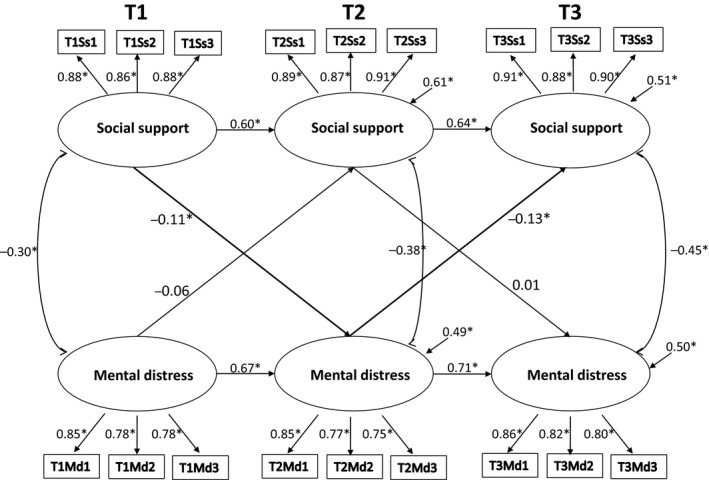
The results from the analysis of the reciprocal relationship between work‐related social support and mental distress over three time points. No covariates included, error terms and correlated measurement errors omitted
Partly, the results align with the proposition that social support is related to lower levels of mental distress (hypothesis 1) and the assumption that mental distress can reduce levels of social support (Hypothesis 2). Mainly, however, the findings suggest a mutual interrelationship between social support and mental distress. But this relationship includes no consistent reciprocal causation (Hypothesis 3). Rather, and due to the variation in reciprocity between time points, it seems as a cyclical process.
4. DISCUSSION
With previous studies showing that associations between work‐related social support and various mental health outcomes can be considered normal, reversed, or reciprocal,6, 7, 8, 16, 17, 18 this study investigated specifically the characteristics of the short‐term longitudinal associations between social support and mental distress in a specific group of workers, with associations being hypothesized to be normal (hypothesis 1), reversed (hypothesis 2), or reciprocal (hypothesis 3). In line with the first and second hypotheses, the present findings provided support for a normal association and for a reversed association. However, the most consistent support emerged for the assumption of mutual interrelationships between social support and mental distress. In line with the third hypothesis, this can be described as a reciprocal association.
In detail, our main hypothesis assumed a normal relationship between social support and mental distress with findings providing support for such a relationship. However, with social support at T1 being associated with less mental distress at T2, whereas no such association emerged between Times 2 and 3, the findings only provided partial support for hypothesis 1. Moreover, and following the second hypothesis assuming a reversed relationship, there was an association between less mental distress and less social support. Again, however, this association emerged between two time points only (T2‐T3), thus not fully supporting the hypothesis assuming a reversed relationship. Taken together, this provides support for the normal and the reversed relationships, but the associations were not repeated at the different time points. Thus, the associations between latent variables were inconsistent over time. As for the reciprocal relationship, the associations did not coincide at the different time points, meaning that there was no truly consistent reciprocity between work‐related social support and mental distress. Moreover, the lagged effects between Time 1 and Time 3 latent variables (results not shown) were not statistically significant, and produced no significant changes in the associations of the original model (Figure 1). Thus, the short‐term effects seem more important than the long‐term effects.
4.1. Normal, reversed, or reciprocal?
The empirical support for the normal relationship between work‐related social support and mental health outcomes is overwhelming,3, 6, 7, 8, 14 with the present empirical findings aligning with earlier results in showing that social support is associated with less mental distress. However, this association was inconsistent, not holding over all time points. Instead, and in line with other studies,6, 7, 8, 16, 18 a reversed effect with mental distress being associated with less social support (between T2 and T3) was observed. This inconsistency may relate to several issues. For instance, focusing exclusively on a specific occupation may reduce variance in study variables. This may be particularly prominent for health selection, over longer‐time periods but perhaps less of a problem during the 3‐year period investigated. Importantly, only employees staying with the organization over the 3‐year period were investigated. This means that the weak reversed relationship may reflect typical variations in mental distress among healthy workers wanting to stay in a job but also relate to employees with vulnerabilities of mental distress who stay for other reasons (eg, health selection). Also, the “gloomy perception mechanism”,8 which suggests that employees over time and especially when strained at work, readjust their subjective evaluation to focus on the negative regardless of their actual situation seems plausible here. Together, the normal and reversed relationships identified in the present study can be viewed as two one‐directional and simultaneous processes with different time‐spans, and perhaps also including subgroup differences. Yet, following previous research,6, 7, 8, 16, 17, 18 our most consistent finding was the reciprocal association. Considering the variation between time points (Figure 1), there was no perfect reciprocity. Instead, the mutual interrelationship, with the delayed effect of mental distress on social support perhaps indicates that changes in mental distress have to surface and be reported before having any influence on social support, which, in turn, can be conceptualized as a cyclical process. This seems reasonable with previous findings showing that no single mechanism clearly stands out and accounts for all effects between psychosocial factors and mental health.6
With longitudinal research of mechanisms having implications for causation, time‐lags become central. Yet, scientific guidance regarding choice of adequate time lags is limited34, 35 with studies using different time lags ranging from daily measurement, to weekly and monthly measurements to several years.8 Instead, and similar to this study, practical circumstances including the workload of organizations and their employees, may become decisive. This means that is unclear whether perceptions of social support at work, and experiences of mental distress, which are influenced by factors beyond work as well, develop similarly over time and whether the two should be measured with the same intervals and through self‐reports or other methods. This study relied on self‐reports only. Obviously, individuals can provide reliable details regarding their situation.36 While acknowledging the effects of any mono‐method bias, which may for instance be reflected in a gloomy perception of work and health, this bias has been exaggerated.37 Also, synchronized measurement is needed to detect effects.38 Here, this involved a 12‐month time lag, thus minimizing seasonal variation in workload and mental distress.
Many longitudinal occupational health studies mix occupations and organizational settings to increase sample size and generalizability and limit attrition effects.6, 7, 8, 16, 17 While this general approach is valuable to further the understanding of longitudinal interrelationships, it may overlook characteristics specific to occupations and organizations. Thus, the general approach needs to be complemented with research of specific occupations and organizational contexts, to allow an in‐depth understanding of whether and how findings from of general studies transfer to the specific contexts. Investigating specific occupations and settings also involves making an effort to minimize the influence of contextual factors of any occupational context (eg, organizational setting, and work‐tasks). Here, this involved focusing exclusively on accountants. This allowed minimizing variance depending on different job tasks. However, accounting work is similar across organizations and countries, thus allowing generalization to similar occupations but also to other contexts; given the EU legislation regarding accountant work, it adds uniformity. Moreover, accounting is comparable to much office‐work.
Studying social support and mental distress and leaving out other central psychosocial factors, including job autonomy and various job demands, obviously limits conclusions regarding their effects. Similarly, and due to having to limit the length of the questionnaire, no data regarding other potential confounders, such as health behaviors, were included. Adding other factors would have increased the number of items in the self‐report questionnaire. This may, in turn, increase longitudinal attrition which jeopardizes assumptions of the cross‐lagged analysis. Yet, future studies should strive to include data on different psychosocial factors and different health‐related outcomes along with health behaviors to allow for further disentangling the associations between these factors among different occupational groups. Importantly, social support, in it covering possibilities for assistance, learning, and human interplay at work, is a key factor for long‐term health, thus making it essential to investigate how social support and mental distress change over time and the characteristics of their associations.
To conclude, this three‐wave study provided partial support for both normal and reversed associations between social support and mental distress. However, the strongest support emerged for a reciprocal association, but without perfect interrelatedness, which suggests a cyclical process. This has potential implications for the understanding of causal mechanisms of work‐related support and mental health.
DISCLOSURE
Approval of the research protocol: Ref. No. 2007/932‐31. Informed Consent: Ref. No. 2007/932‐31. Registry and the Registration No. of the study/Trial: N/A. Animal Studies: N/A.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
AUTHOR CONTRIBUTIONS
All authors were involved in developing the research question and the hypotheses. The first and the last authors analyzed the data and then discussed the findings with the other authors. The first author drafted the methods and results sections while the second author drafted the introduction and discussion. After all the authors provided the input on the draft, the second author finalized the manuscript.
ACKNOWLEDGMENTS
The authors thank all employees who volunteered participation. Financial support was given by a national funding agency to the last author (Ref. No. 2006‐1139). The research was carried out within Stockholm Stress Center, a FORTE center of excellence (Ref. No. 2009‐01758).
Sconfienza C, Lindfors P, Lantz Friedrich A, Sverke M. Social support at work and mental distress: A three‐wave study of normal, reversed, and reciprocal relationships. J Occup Health. 2019;61:91–100. 10.1002/1348-9585.12020
ENDNOTES
Table 3 shows findings without control variables and includes short‐term effects only. Controlling for gender, age, and education produced identical estimates of the associations in the structural model. Introducing long‐term lagged effects, between Time 1 and Time 3 latent variables, produced no changes in the estimates of the associations.
The cross‐lagged regression coefficients were identical when controlling for gender, age, and education. The lagged effects between Time 1 and Time 3 latent variables (not shown in the figure) were not statistically significant, and produced no significant changes in the associations of the original model (Figure 1).
REFERENCES
- 1. House JS. Work stress and social support. Reading, MA: Addison‐Wesley; 1981. [Google Scholar]
- 2. Karasek RA, Theorell T. Healthy work: stress, productivity, and the reconstruction of working life. New York, NY: Basic books; 1990. [Google Scholar]
- 3. Stansfeld S, Candy B. Psychosocial work environment and mental health–a meta‐analytic review. Scand J Work Environ Health. 2006;32(6):443‐462. [DOI] [PubMed] [Google Scholar]
- 4. Theorell T, Hammarström A, Aronsson G, et al. A systematic review including meta‐analysis of work environment and depressive symptoms. BMC Public Health. 2015;15:738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aronsson G, Theorell T, Grape T, et al. A systematic review including meta‐analysis of work environment and burnout symptoms. BMC Public Health. 2017;17:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Lange AH, Taris TW, Kompier M, et al. Different mechanisms to explain the reversed effects of mental health on work characteristics. Scand J Work Environ Health. 2005;31(1):3‐14. [DOI] [PubMed] [Google Scholar]
- 7. de Lange AH, Taris TW, Kompier M, et al. The relationship between work characteristics, and mental health: examining normal, reversed and reciprocal relationships in a 4‐wave study. Work Stress. 2004;18(2):149‐166. [Google Scholar]
- 8. Tang K. A reciprocal interplay between psychosocial job stressors and worker well‐being? A systematic review of the "reversed" effect. Scand J Work Environ Health. 2014;40(5):441‐456. [DOI] [PubMed] [Google Scholar]
- 9. McDowell I. Measuring mental health: a guide to rating scales and questionnaires, 3rd edn New York, NY: Oxford University Press; 2006. [Google Scholar]
- 10. Ihlebaek C, Eriksen HR, Ursin H. Prevalence of subjective health complaints (SHC) in Norway. Scand J Public Health. 2002;30(1):20‐29. [PubMed] [Google Scholar]
- 11. Goldberg D. Manual of the General Health Questionnaire. London, UK: NFER Nelson; 1979. [Google Scholar]
- 12. Banks Mh, Clegg Cw, Jackson Pr, Kemp Nj, Stafford Em, Wall Td. The use of the General Health Questionnaire as an indicator of mental health in occupational studies. J Occup Psychology. 1980;53(3):187‐194. [Google Scholar]
- 13. Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands resources model of burnout. J Appl Psychology. 2001;86(3):499‐512. [PubMed] [Google Scholar]
- 14. van der Doef M, Maes S. The job demand‐control(‐support) model and psychological well‐being: a review of 20 years of empirical research. Work Stress. 1999;13(2):87‐114. [Google Scholar]
- 15. de Lange AH, Taris TW, Kompier M, Houtman I, Bongers PM. "The very best of the millennium": longitudinal research and the demand‐control‐(support) model. J Occup Health Psychol. 2003;8(4):282‐305. [DOI] [PubMed] [Google Scholar]
- 16. Zapf D, Dormann C, Frese M. Longitudinal studies in organizational stress research: A review of the literature with reference to methodological issues. J Occup Health Psychol. 1996;1(2):145‐169. [DOI] [PubMed] [Google Scholar]
- 17. Kompier M, Taris TW. Understanding the causal relations between psychosocial factors at work and health: a circular process. Scand J Work Environ Health. 2011;37(4):259‐261. [DOI] [PubMed] [Google Scholar]
- 18. Reis D, Hoppe A, Schröder A. Reciprocal relationships between resources, work and study engagement, and mental health: evidence for gain cycles. Europ J Work Org Psychol. 2015;24(1):59‐75. [Google Scholar]
- 19. Näsvall K, Baraldi S, Richter A, et al. The salaried employee in the modern working life: Threats and challenges. Technical report on the sample, a collection, and measurement properties of the instruments. SALTSA Report No 2006:3. Stockholm, Sweden: National Institute for Working Life. SALTSA; 2006. [Google Scholar]
- 20. Näswall K, Låstad L, Vetting T‐S, et al. Job insecurity from a gender perspective: data collection and psychometric properties. Stockholm, Sweden: Department of Psychology, Stockholm University; 2010. [Google Scholar]
- 21. Little R, Rubin DB. Statistical analysis with missing data. New York, NY: Wiley; 1987. [Google Scholar]
- 22. Tabachnick BG, Fidell LS. Using multivariate statistics, 5th edn New York, NY: Allyn and Bacon; 2007. [Google Scholar]
- 23. Näswall K, Sverke M, Hellgren J. Stand by me: The moderating effects of work‐based and family‐based support on the relation between job insecurity and subsequent strain. South African J Ind Psychol. 2005;31(4):57‐64. [Google Scholar]
- 24. Caplan RD, Cobb S, French J Jr, et al. Job demands and worker health: main effects and occupational differences. Washington, DC: US Government Printing Office; 1975. [Google Scholar]
- 25. Jöreskog K, Sörbom D. LISREL 8: User's reference guide. Chicago IL: Scientific Software International, Inc; 1996. [Google Scholar]
- 26. Brooke PP Jr, Russel DW, Price JL. Discriminant validation of measures of job satisfaction, job involvement, and organizational commitment. J Appl Psychol. 1988;73(2):139‐145. [Google Scholar]
- 27. Mathieu JE, Farr JL. Further evidence for the discriminant validity of measures of organizational commitment, job involvement, and job satisfaction. J Appl Psychol. 1991;76(1):127‐133. [Google Scholar]
- 28. Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two‐step approach. Psychol Bull. 1988;103(3):411‐423. [Google Scholar]
- 29. Bollen KA. Structural equations with latent variables. New York, NY: John Wiley; 1989. [Google Scholar]
- 30. Bentler PM. On tests and indices for evaluating structural models. Pers Ind Diff. 2007;42(5):825‐829. [Google Scholar]
- 31. Wheaton B, Muthen B, Alwin DF, Summers GF. Assessing reliability and stability in panel models. Sociol Methodol. 1977;8:84‐136. [Google Scholar]
- 32. Hooper D, Coughlan J, Mullen M. Structural equation modelling: Guidelines for determining model fit. Electronic J Bus Res Methods. 2008;6(1):53‐60. [Google Scholar]
- 33. L‐t Hu, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1‐55. [Google Scholar]
- 34. Dormann C, Griffin MA. Optimal time lags in panel studies. Psychol Methods. 2015;20(4):489‐505. [DOI] [PubMed] [Google Scholar]
- 35. Ford MT, Matthews RA, Wooldridge JD, Mishra V, Kakar UM, Strahan SR. How do occupational stressor‐strain effects vary with time? A review and meta‐analysis of the relevance of time lags in longitudinal studies. Work Stress. 2014;28(1):9‐30. [Google Scholar]
- 36. Podsakoff PM, MacKenzie SB, Lee J‐Y, Podsakoff NP. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879‐903. [DOI] [PubMed] [Google Scholar]
- 37. Spector PE. Method variance in organizational research: truth or urban legend? Org Res Methods. 2006;9(2):221‐232. [Google Scholar]
- 38. Collins LM. Analysis of longitudinal data: the integration of theoretical model, temporal design, and statistical model. Annual Rev Psychol. 2006;57:505‐528. [DOI] [PubMed] [Google Scholar]


