Abstract
Objectives
Human support can boost weight reduction in Internet‐based weight‐loss intervention. However, the most effective way to combine human support and the Internet for weight loss is unclear. This study aimed to examine the effects of two weight‐loss programs for male workers aged 18‐39 that combined different intensities of human support with website support compared to a delayed‐intervention group (control group; CG), in a randomized controlled trial.
Methods
Seventy‐one participants with overweight or obesity were allocated to one of three 12‐week treatment programs. The Standard Support Group (SSG) was provided support via website and two face‐to‐face group guidance sessions, at the beginning and at the end of the program along with monthly general emails throughout the program. The Enhanced Support Group (ESG) received four remote support sessions based on Supportive Accountability (SA) in addition to the SSG. The CG was provided the same program as SSG after the other two groups had completed the program. The primary outcome was body weight reduction.
Results
ESG participants reduced their weight significantly more than SSG and CG participants (P = 0.038, P < 0.001, respectively), and SSG participants reduced their weight significantly more than CG participants (P = 0.033).
Conclusions
The additional remote human support provided to the participants in the ESG was beneficial for weight loss in male workers. The low‐intensity program provided to the SSG was also effective. Further studies with more participants in diverse settings and with participants who are less interested in their health and weight management are needed.
Keywords: human support, randomized controlled trial, Supportive Accountability, Web‐based intervention, weight loss
1. INTRODUCTION
According to the World Health Organization (WHO), in 2016, 39% of adults were overweight, including 13% with obesity.1 In Japan, the incidence of men who were overweight or obese was 31%.2 Obesity and overweight cause lifestyle diseases, including cardiovascular disease and diabetes. In addition, a previous study revealed that workers with body mass index (BMI) more than 30 kg/m2 had higher sickness presenteeism than those with BMI less than 25 kg/m2, and there was a significant relationship between BMI and sickness presenteeism.3 By Japanese law, medical insurers including companies and health insurance associations are obligated to provide health checkup and guidance to people aged 40‐75 in order to prevent lifestyle diseases caused by metabolic syndrome. Another law requires employers to “make efforts” to provide health guidance to employees who need to improve their health behaviors after health checkup. Thus, people under 40 tend to have few opportunities to receive health guidance. Previous studies have shown that early adulthood adiposity and weight gain after age 20 contribute to the development of chronic diseases in middle and advanced age.4, 5, 6 It is important to support weight reduction among young people with obesity, as the rate of overweight and obesity increases with age.2 In particular, Japanese men's obesity rate is higher than that of women.2 Healthcare providers must foster lifestyle changes by providing clients with effective, user‐friendly health management tools that are reinforced with effective support.
Studies on Internet‐based weight‐loss interventions have increased in recent years. Internet‐based interventions are efficiently disseminated and produce significantly greater weight loss than traditional (offline) health guidance.7, 8, 9 Several studies report that Internet intervention produces significantly more weight loss with additional human support than without it.9, 10, 11, 12, 13, 14, 15 Studies have shown no significant differences in weight reduction between face‐to‐face and remote (eg, online) support.16, 17, 18, 19 Additionally, the frequency of human support has been inconsistent across studies, making the optimal frequency unclear.
Few studies have compared the effects of different aspects of human support.7, 20 One group who received additional nutrition psychoeducation and human support showed significantly reduced weight compared to the group participated in motivational interviews during a 12‐week Internet‐based intervention.7 Another 12‐week study reported that directive support (eg, prescriptive, protocol driven) was more beneficial to women and nondirective support (eg, collaborative, flexible) to men.20 Effective human support may differ by gender, but the optimal support to add to Internet‐based weight‐loss intervention remains unclear.
The theoretical model of Supportive Accountability (SA) was developed to enhance adherence to Internet‐based intervention21 and effectively boosts clients’ engagement in interventions.22, 23 However, few studies have assessed the effectiveness of SA in healthcare interventions.24, 25 One study assessed weight‐loss differences between an Internet‐only group and an intervention group that received Internet support plus two sessions of SA telephone support.25 No differences in weight reduction were found between the Internet‐only and intervention groups; however, within the intervention group, the participants who received telephone support reduced weight significantly more than those who did not. It is important to improve patients’ engagement in human support‐based intervention to enhance its effectiveness. Thus, we provided human support through face‐to‐face group sessions, along with telephone, and email support. This study assessed the effectiveness of SA‐based human support through different modalities and at different frequencies.
This study examines the effects of two weight‐loss programs for Japanese male workers between the ages of 18 and 39 in various occupations that combined different intensities of human support along with website support, compared to those in a delayed‐intervention group (control group; CG). We hypothesized that there would be significant differences among the three programs, particularly that CG participants would lose significantly less weight than the participants of the other groups.
2. SUBJECTS AND METHODS
We conducted a randomized controlled trial to assess the effectiveness of the 12‐week weight‐loss program, which combined the website with human support for male workers aged 18‐39 with obesity. The Standard Support Group (SSG) received website‐based support through two sessions of face‐to‐face group guidance, at the beginning and end of the program, and monthly emails that were sent to all participants. The Enhanced Support Group (ESG) received four sessions of individualized remote support in addition to the SSG program. The CG was asked to wait during the ESG and SSG programs and received the same program as SSG after completion of the ESG and SSG programs.
The research design was approved by the ethical review committee at Nagoya University. We obtained written informed consent from all participants. Participants received no financial incentive. The study protocol was registered on UMIN Clinical Trials Registry (UMIN‐CTR000023809).
2.1. Recruitment and participants
Participants were recruited from two urban areas in western Japan. We invited male workers in private companies and local government agencies that had approved the research. Those eligible interested applicants were identified by email or phone. Inclusion criteria were being between 18 and 39 years old, having a BMI ≧ 25, permission from a primary doctor if diagnosed with a lifestyle disease or orthopedic disorder, Internet access, and the ability to self‐weigh at home to monitor progress. Exclusion criteria were surgery within the past 6 months, severe psychiatric problems, and participation in other weight loss or other health‐related programs during this intervention.
Recruitment was conducted from April to June 2017 in one area and August to October 2017 in the other. We calculated sample size using G*Power 3.26, 27 We found that 158 participants were needed to detect an effect size of 0.25 (medium effect) with 0.8 power (α = 0.05).
2.2. Randomization, allocation concealment, and blinding
Eligible participants were randomized into the ESG, SSG, or CG groups. They were stratified by BMI (BMI < 30 kg/m2, BMI ≧ 30 kg/m2) and divided into three blocks through computer‐generated random numbers. Participants complete questionnaires to assess outcomes following treatment. Treatment was allocated by the first author; the process and methods of allocation were concealed from participants, who were blinded to differences among the programs. Participants in the CG were told they were assigned to the second round of the program and were asked to wait until that round started. It was impossible to blind the researchers to the treatment allocation, but the evaluators who measured weight, waist circumference, and body fat were blinded.
2.3. Interventions
2.3.1. Website components
The website developed for this study included information on lifestyle improvement methods, goal setting for weight loss and behavioral change, and self‐monitoring tools. Items included 13 on diet (eg, eating meals regularly every day), two on physical activities (eg, walking more than 8000 steps per day), and two on drinking behavior (eg, drinking less than 20 mg alcohol on average per day), based on current Japanese health guidelines. These items were meant to support male workers aged 18‐39 in goal setting. The website included graphing functionality to visualize participants’ weight change and progress toward goals, and provided tips regarding behavioral change for weight loss.
2.3.2. Standard Support Group
Figure 1 shows the construction of the treatment programs. At the beginning of the 12‐week program, SSG was provided with two hours’ group guidance. These participants received a one‐hour lesson on causes of obesity, methods of behavioral change for weight loss, benefits of self‐monitoring, and using self‐monitoring tools. Then, body weight, waist circumference, and body fat were measured, and they set weight‐loss goals based on the guideline of 3% weight loss from baseline weight recommended by the Japan Society for the Study of Obesity.28 Participants calculated the needed energy‐intake reduction over the course of the program to meet their weight‐loss goals and were given a calorie book. Next, the participants set goals for lifestyle improvement, with reference to the website, and considered their motivation for losing weight. Then, they were given 10 minutes’ of one‐on‐one advice to confirm whether they could properly set goals for weight loss and lifestyle improvement.
Figure 1.
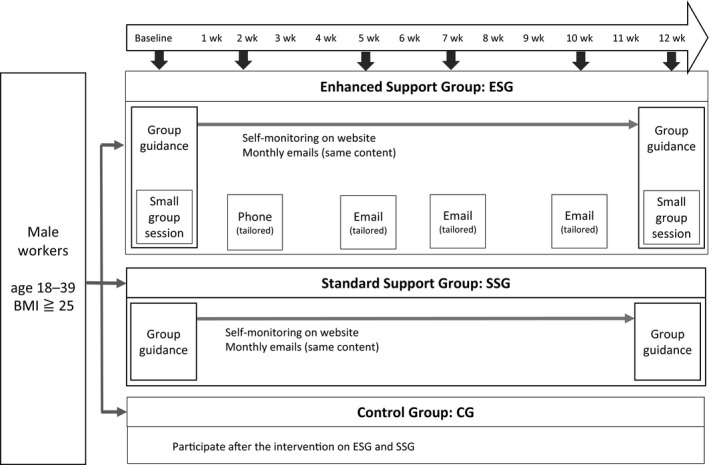
Construction of treatment programs
During the 12‐week program, the participants were encouraged to enter their body weight and degree of achievement of goal items for lifestyle improvement daily using the online self‐monitoring tools. The provider (see below) sent all participants an identical email once a month to encourage them to continue behavioral change and self‐monitoring to work toward their set goals.
At the program's conclusion, the participants received 90 minutes of group guidance. The lesson included 30‐minute on methods of preventing rebound weight gain. Their body weight, waist circumference, and body fat were again measured, and they received feedback about their degree of weight‐loss and behavioral change achievement. They also completed the questions from the baseline survey for outcome assessment. Finally, they set goals for further weight loss and lifestyle improvement after 6 months and were given individual advice on reaching those goals by the provider.
Some researchers, who were licensed nurses, provided ongoing support to the participants as providers.
2.3.3. Enhanced Support Group
ESG received the same content as SSG, along with a 20‐minute small‐group (4‐5 participant) session after the program, and two sessions of large‐group guidance. In addition, ESG received four sessions of remote support during the 12‐week program. The first remote support session was a 10‐minute telephone session in the second week, the time the participant preferred. The other three sessions were email support at the 5th, 7th, and 10th weeks. All the support sessions were conducted based on previous research and SA.18, 21 In the initial small‐group session, the provider explained her role monitoring participants’ achievement and providing support when solving obstacles. She also praised participants for setting their own goals. The participants talked about their goals, their motivation for trying to lose weight, what they wanted to do once they succeeded, and their concerns about achieving their goals and using the website. During telephone and email support, the provider praised participants for what they had changed and achieved, and encouraged them to think about the causes of their problems and strategies to address them. All human support in the ESG were provided by the first author to maintain consistency and foster trust.
2.3.4. Control Group
The participants in the CG received the same program as SSG, after the other groups had finished. The participants completed questionnaires for assessment at the same time as SSG and ESG.
2.4. Outcome measures
The study's primary outcome was change in absolute body weight. Secondary outcomes were BMI, percent weight loss, waist circumference, rate of body fat, physical activity, energy intake, self‐efficacy, and self‐monitoring. All outcomes were assessed at baseline and at the 12th week.
Body weight and body fat were measured on a calibrated scale (Tanita DC430). CG participants reported their home‐measured body weight; data on body fat and waist circumference were not collected for this group.
Energy intake was measured by a brief self‐administered Diet History Questionnaire (BDHQ),29, 30 which included 56‐items on energy and nutrient intake during the previous month. Reliability and validity were assessed in a validation study.29, 30
The self‐reported International Physical Activity Questionnaire (IPAQ) Long Form, Japanese Version measured physical activity.31 This scale includes 27 items which assess time, and amount of high‐intensity and moderate‐intensity physical activity during the week. Reliability and validity were assessed in validation studies.31, 32
Self‐efficacy was measured by the Modified Perceived Health Competence Scale (PHCS), Japanese Version,33 which measures domain‐specific self‐efficacy. This scale includes eight items, with a total score of 8‐40; a higher score means higher self‐efficacy.
Self‐monitoring was measured using the self‐monitoring tools on the website over the 12 weeks. The number of times body weight and achievement of goal items were entered was counted.
2.5. Statistical analyses
Differences in baseline data between groups were analyzed using a one‐way analysis of variance (ANOVA) for continuous variables and a chi‐squared test for nominal variables.
We compared the group (intervention) effects using the principle of intention‐to‐treat (ITT), carrying baseline data forward for missing data at the 12th week. The analysis set consisted of participants in ESG and SSG who received the allocated interventions and those in CG who completed the questionnaires. Differences in outcome variables between groups were analyzed using an Analysis of Covariance (ANCOVA), with baseline BMI as the covariate, treatment group as the independent variable, and outcome variables as the dependent variables. Post‐hoc analyses were performed using Bonferroni Adjustment. Partial eta‐squared (η2 p) was calculated for effect size. We also analyzed differences in outcome variables (except number of times self‐monitoring) between groups, using data of participants who completed the 12‐week assessment, with ANOVA. Post‐hoc analyses were performed using the Tukey HSD test. We compared the rate of participants achieving 3% weight loss from baseline weight between groups using a logistic regression analysis. Correlation analysis was used to assess the correlation between number of times self‐monitoring and weight change.
Statistical analyses were performed using SPSS 22.0. Statistical significant was set at P < 0.05.
3. RESULTS
3.1. Recruitment and attrition
Figure 2 shows a flow chart of participant attrition. Eighty participants were allocated across the three groups: 25 to ESG, 27 to SSG, and 28 to CG. We excluded one participant in ESG and two in SSG who did not receive the allocated intervention, as well as six in CG who did not complete the questionnaire. There were no differences in age or BMI at baseline between excluded and retained participants.
Figure 2.
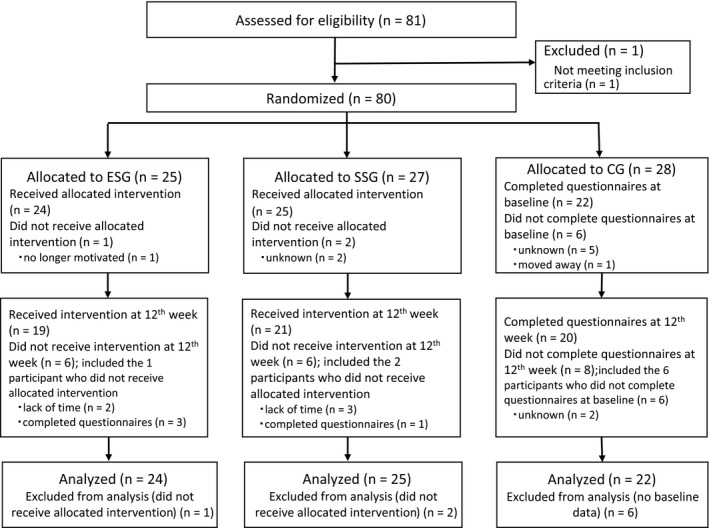
Flow chart of participants
3.2. Characteristics of participants
Table 1 shows characteristics of participants by treatment group. Of the 71 retained participants, average age was 34.2 (SD 4.2) years and average BMI was 28.7 (SD 4.2) kg/m2. In all, 81.5% of participants had at least an undergraduate education, 69.0% had jobs with low physical demands, 70.4% rated their health as good, and 95.8% used a smartphone for Internet media daily. There were no significant differences in characteristics at baseline between treatment groups.
Table 1.
Baseline characteristics
| All participants (n = 71) | ESG (n = 24) | SSG (n = 25) | CG (n = 22) | P‐value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Age | 34.2 | 4.2 | 34.9 | 3.5 | 33.2 | 5.1 | 34.6 | 3.7 | 0.325a |
| Weight (kg) | 83.8 | 13.4 | 83.0 | 10.1 | 88.1 | 16.4 | 79.8 | 12.1 | 0.101a |
| BMI (kg/m2) | 28.7 | 4.2 | 28.4 | 2.8 | 29.7 | 4.8 | 28.0 | 4.7 | 0.350a |
| Waist circumference (cm) | 99.1 | 10.8 | 98.0 | 8.6 | 100.1 | 12.6 | 0.506a | ||
| Body fat (%) | 28.6 | 4.7 | 27.4 | 4.5 | 29.7 | 4.7 | 0.097a | ||
| Energy intake (kcal/day) | 1874.0 | 458.4 | 1839.6 | 566.2 | 1876.6 | 468.4 | 1908.7 | 309.9 | 0.807a |
| Energy expenditure (kcal/day) | 556.2 | 857.7 | 598.2 | 839.3 | 604.4 | 1067.7 | 455.5 | 602.0 | 0.546a |
| Self‐efficacy | 18.0 | 4.9 | 17.3 | 5.6 | 18.8 | 4.2 | 17.7 | 4.8 | 0.880a |
| n | % | n | % | n | % | n | % | ||
| Education | |||||||||
| High school | 7 | 10.8 | 2 | 9.1 | 2 | 9.1 | 3 | 14.3 | 0.486b |
| College, Special training college | 2 | 3.1 | 1 | 4.5 | 1 | 4.5 | 0 | 0.0 | |
| University, Graduate School | 53 | 81.5 | 16 | 72.7 | 19 | 86.4 | 18 | 85.7 | |
| Other | 3 | 4.6 | 2 | 13.6 | 0 | 0.0 | 0 | 0.0 | |
| Physical demands of job | |||||||||
| Heavy | 11 | 15.5% | 5 | 20.8 | 2 | 8.0 | 4 | 18.2 | 0.485b |
| Moderate | 11 | 15.5% | 2 | 8.3 | 6 | 24.0 | 3 | 13.6 | |
| Low | 49 | 69.0% | 17 | 70.8 | 17 | 68.0 | 15 | 68.2 | |
| Self‐rated health | |||||||||
| Very good | 2 | 2.8 | 0 | 0.0 | 1 | 4.0 | 1 | 4.5 | 0.183b |
| Good | 48 | 67.6 | 16 | 66.7 | 20 | 80.0 | 12 | 54.5 | |
| A little poor | 19 | 26.8 | 6 | 25.0 | 4 | 16.0 | 9 | 40.9 | |
| Poor | 2 | 2.8 | 2 | 8.3 | 0 | 0.0 | 0 | 0.0 | |
| Internet media on a daily basisc | |||||||||
| Smartphone | 68 | 95.8 | 23 | 95.8 | 24 | 96.0 | 21 | 95.5 | 0.996b |
| Cellphone | 2 | 2.8 | 1 | 4.2 | 1 | 4.0 | 0 | 0.0 | 0.630 |
| Personal computer | 45 | 63.4 | 15 | 62.5 | 14 | 56.0 | 16 | 72.7 | 0.491 |
| Tablet computer | 16 | 22.5 | 3 | 12.5 | 9 | 36.0 | 4 | 18.2 | 0.121 |
| Other: Video game system, television | 9 | 12.7 | 4 | 16.7 | 1 | 4.0 | 4 | 18.2 | 0.266 |
ESG: Enhanced Support Group, SSG: Standard Support Group, CG: Control Group, SD: Standard Deviation.
ANOVA;
Chi‐squared test;
Multiple answers allowed.
3.3. Change in body weight, percent weight loss, BMI change, waist circumference reduction, lowered body fat rate
Table 2 shows differences in changes from baseline to week 12 based on ITT analysis. Table 3 shows post‐hoc analysis of the ANCOVA. The group differences in weight loss were significant (P < 0.001, η2 p = 0.281). Post‐hoc analysis of ANCOVA showed that the average weight loss in ESG was significantly greater than that in SSG (P = 0.038) and CG (P < 0.001). The average weight loss in SSG was significantly greater than that in CG (P = 0.033). The group differences in percent weight loss were significant (P < 0.001, η2 p = 0.295). Post‐hoc analysis of ANCOVA showed that the average percent weight loss in ESG was significantly greater than that in SSG (P = 0.037) and CG (P < 0.001). The average percent weight loss in SSG was significantly greater than that in CG (P = 0.021). The group differences in BMI were significant (P < 0.001, η2 p = 0.281). Post‐hoc analysis of ANCOVA showed that the average BMI in ESG was significantly greater than that in SSG (P = 0.038) and CG (P < 0.001). The average BMI in SSG was significantly greater than that in CG (P = 0.033). The average waist circumference between ESG and SSG was not significant (P = 0.124, η2 p = 0.051). The average body fat in ESG tended to be greater than that in SSG (P = 0.063, η2 p = 0.073), but it was not significant.
Table 2.
Differences in outcome change from baseline to 12th week (ITT Analysis)
| ESG (n = 24) | SSG (n = 25) | CG (n = 22) | P‐value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | 95% CI | Mean | SE | 95% CI | Mean | SE | 95% CI | |||||
| Weight loss (kg) | −3.71 | 0.58 | −4.87 | −2.55 | −1.61 | 0.57 | −2.76 | −0.47 | 0.59 | 0.61 | −0.62 | 1.81 | <0.001a |
| Percent weight loss (%) | −4.30 | 0.68 | −5.65 | −2.95 | −1.85 | 0.67 | −3.19 | −0.52 | 0.87 | 0.71 | −0.55 | 2.28 | <0.001a |
| BMI (kg/m2) | −1.27 | 0.19 | −1.66 | −0.88 | −0.57 | 0.19 | −0.95 | −0.19 | 0.16 | 0.20 | −0.24 | 0.57 | <0.001a |
| Waist circumference (cm) | −3.51 | 0.84 | −5.20 | −1.81 | −1.65 | 0.82 | −3.31 | 0.01 | 0.124a | ||||
| Body fat (%) | −1.53 | 0.32 | −2.17 | −0.88 | −0.67 | 0.31 | −1.30 | −0.04 | 0.063a | ||||
| Energy intake (kcal/day) | −156.87 | 93.96 | −344.41 | 30.67 | −78.24 | 92.85 | −263.57 | 107.08 | −39.14 | 98.57 | −235.87 | 157.60 | 0.675a |
| Energy expenditure (kcal/day) | 81.54 | 128.07 | −174.10 | 337.17 | 162.58 | 126.56 | −90.03 | 415.19 | 135.69 | 124.55 | 134.36 | −143.62 | 0.904a |
| Self‐efficacy score | 4.63 | 1.21 | 2.22 | 7.04 | 3.14 | 1.19 | 0.76 | 5.52 | 0.88 | 1.27 | −1.65 | 3.41 | 0.106a |
| Self‐monitoring on website (days) | 53.26 | 6.28 | 40.62 | 65.9 | 40.79 | 6.15 | 28.41 | 53.17 | 0.165a | ||||
CG: Control Group, ESG: Enhanced Support Group, ITT: intention to treat, SE: Standard Error, SSG: Standard Support Group.
ANCOVA; means adjusted on baseline BMI.
Table 3.
Mean differences by treatment group (ITT analysis)
| Mean difference | SE | 95% CI | P‐value | ||
|---|---|---|---|---|---|
| Weight loss | |||||
| ESG vs. SSG | −2.10 | 0.82 | −4.11 | −0.09 | 0.038 |
| ESG vs. CG | −4.31 | 0.84 | −6.37 | −2.24 | <0.001 |
| SSG vs. CG | −2.21 | 0.84 | −4.28 | −0.14 | 0.033 |
| Percent weight loss | |||||
| ESG vs. SSG | −2.45 | 0.95 | −4.78 | −0.11 | 0.037 |
| ESG vs. CG | −5.17 | 0.98 | −7.57 | −2.77 | <0.001 |
| SSG vs. CG | −2.72 | 0.98 | −5.13 | −0.32 | 0.021 |
| BMI | |||||
| ESG vs. SSG | −0.70 | 0.27 | −1.37 | −0.03 | 0.038 |
| ESG vs. CG | −1.43 | 0.28 | −2.12 | −0.75 | <0.001 |
| SSG vs. CG | −0.73 | 0.28 | −1.42 | −0.04 | 0.033 |
ANCOVA Post‐hoc Analysis; Bonferroni Adjustment.
CG: Control Group, ESG: Enhanced Support Group, ITT: intention to treat, SE: Standard Error, SSG: Standard Support Group.
The results of ANOVA using data of participants who completed the 12‐week assessment revealed that group differences in weight loss were significant (P < 0.001) with those in the ESG and SSG groups showing significantly greater weight loss than those in the CG (P < 0.001, P = 0.010, respectively). There was a non‐significant trend between ESG and SSG (P = 0.074). Similarly, average percent weight loss in ESG and SSG was significantly greater than that in CG (P < 0.001, P = 0.007, respectively), and a non‐significant trend between ESG and SSG (P = 0.060) was noted. Similarly, average BMI in ESG and SSG was significantly greater than that in CG (P < 0.001, P = 0.009, respectively), and BMI showed a non‐significant trend between ESG and SSG (P = 0.078). Average waist circumference difference between ESG and SSG was not significant (P = 0.204). Similarly, average body fat difference between ESG and SSG was not significant (P = 0.063; Supplementary Tables 1 and 2).
The rate of participants achieving 3% weight loss from baseline weight was higher in ESG than in CG (54.2% vs 4.5%, OR = 25.06, P = 0.004, 95% CI [2.86‐219.55]) and the SSG (36.0%, OR = 11.07, P = 0.030, 95% CI [1.26‐97.34]).
3.4. Change in other outcomes
As shown in Table 2, analyses of observed data and ITT analyses on energy intake, energy expenditure, self‐efficacy, and number of times self‐monitoring indicated a similar pattern.
Group differences in energy intake were not significant (P = 0.675, η2 p = 0.012).Group differences in energy expenditure were not significant (P = 0.904, η2 p = 0.003). Group differences in self‐efficacy were not significant (P = 0.106, η2 p = 0.065). The number of self‐monitoring participants in ESG tend to be higher than in SSG; however, there were no significant differences in average number of times self‐monitoring between ESG and SSG (P = 0.165, η2 p = 0.041).
3.5. Correlation between self‐monitoring and weight loss
Correlation analysis revealed that frequency of times self‐monitoring was significantly associated with weight loss (r = −0.49, P < 0.001) in both intervention groups; significant (r = −0.56, P = 0.005) in ESG alone; and non‐significant (r = −0.40, P = 0.050) in SSG alone.
4. DISCUSSION
We examined the effects of two weight‐loss programs for male workers aged 18‐39 that combined different intensities of human support with a website, compared to a CG. SSG was provided website support with face‐to‐face group guidance at the beginning and end of the 12‐week program, and monthly emails. ESG was given two group sessions and four remote support sessions based on SA in addition to the SSG program. ITT analysis showed that participants lost weight: 3.71 kg (SE 0.59) in ESG, 1.61 kg (SE 0.58) in SSG. Previous studies with Japanese participants whose mean ages in their 50s reported similar weight loss in the intervention groups.34, 35, 36
In this study, ESG participants lost significantly more weight than the SSG and CG, and SSG participants lost significantly more than CG. The additional human support in the ESG program had the greatest effectiveness for weight loss for several possible reasons. First, this support was explicitly based on SA, which requires the (physical or remote, synchronous or asynchronous) “social presence” of another person.21 Accountability is also encouraged by relational factors: two‐way communication, trustworthiness, benevolence, and expertise; the former two are particular effectively for fostering engagement in Internet‐based professional health intervention.21, 22 Remote support is often effective but can complicate both rapport‐building and providers’ understanding of clients’ problems. Thus, clients may view the provider's trustworthiness and benevolence as low. These strategies in combination mutually reinforce one another to diminish barriers.21, 23 In the present study, group guidance at the beginning of the 12‐week program and the four remote support sessions were provided by one licensed nurse to create and sustain a trusting relationship. Also, the first remote session was conducted by telephone to provide greater social presence than by email. These strategies enabled participants to perceive the provider's trustworthiness and expertise, and improved the effectiveness of human support.
Second, human support based on SA may be especially beneficial to male workers. A previous study comparing directive and nondirective human support with Internet support found that nondirective support was more beneficial for men in a 12‐week weight‐loss program.20 Another study comparing coach‐led and self‐directed intervention revealed little difference.7 Together these results suggest that men may prefer nondirective support when losing weight. In SA‐based human support, the client is involved in determining goals and expectation21; however, limiting desired behavior and inducing perfunctory adherence should be minimized.21 In the present study, we supported participants to choose goals and strategies to address their problems, which appeared beneficial to them.
Third, the modality of human support provided was effective. Previous studies reveal that remote support by telephone is as effective as face‐to‐face support.15, 16 The telephone facilitates extemporaneous communication as participants can ask questions regarding methods of behavioral change for weight loss. However, telephone support must be convenient for participants, as was the case in this study. In contrast, although previous research has shown that a Web‐based self‐help program did not provide better weight‐loss outcomes with email support than without it,15 email has the advantage of being asynchronous, meaning it can be sent and received at any convenient time. In the present study, we did not ask participants to respond to the emails; therefore, the convenience of email may have reduced the pressure on participants but maintained their interest in achieving their goals. This combination of telephone and email support is also flexible and scalable.
SSG underwent a low‐intensity program in person, which also led to significant weight loss. However, there was a significant difference in weight loss between SSG and ESG but no significant difference in number of times self‐monitoring. Thus, the initial group guidance and the general monthly emails helped foster adherence to self‐monitoring. In group guidance, participants received information regarding weight‐loss strategies and support for goal setting. As for the emails, previous studies reveal that remainder emails facilitate engagement with health programs.22, 37 In the present study, group guidance and monthly emails were provided by the same provider who monitored participants’ achievement, thus personalizing the expectation of adherence and harnessing the trust relationship between participants and provider. Previous research has identified time constraints and increased workload as barriers to Internet‐based health intervention with in‐person support38; the low‐intensity program provided to SSG can address these issues.
The programs provided to ESG and SSG have possibilities of reducing the number of people needing health guidance after 40. Providing face‐to‐face health guidance to workers within the workplace can be challenging. Programs that combined website and in‐person remote support have the possibility of being accepted by workers. We suggest providing a program like SSG to workers with overweight who have high motivation to weight loss. In contrast, the ESG program can be provided to workers with obesity who may have difficulty improving their weight loss lifestyle alone.
A limitation of the present study was the number of participants, which fell short of the required sample size calculated. However, there were significant differences in weight loss, percent weight loss, and BMI, and other indicators in ESG compared to SSG. These findings support the effectiveness of ESG intervention. Our difficulty recruiting male workers aged 18 to 39 may have been because this group may not participate in weight‐loss programs and thus viewed our program as a low priority. They may prioritize other concerns—for example, spending time with family and pursuing career success—rather than their weight loss.39 In this study, 71% of participants rated their health as good. The reason for this may have been a self‐perception that they were well enough to work at present and did not imagine that overweight and obesity may be related to future serious disease. It is necessary to educate young male workers about the risks of overweight and obesity and the importance of weight control from an early age. Second, the participants were urban dwellers with high education, and jobs with low physical demands; therefore, the results may not generalize to other male workers with different characteristics. Third, we targeted only male workers, and a corresponding investigation using weight‐loss programs designed for women workers is needed. Fourth, we did not assess the intervention's long‐term effectiveness or to what degree participants maintained their lowered weight and healthier behavior. Such an assessment is needed. Finally, as the participants were those who were interested in the weight‐loss program, this may have biased the sample and enhanced the program's effects. Further research should involve participants without apparent interest in healthcare or weight management.
5. CONCLUSIONS
ESG participants lost significantly more weight than SSG and CG participants, while SSG participants lost significantly more weight than CG participants. The additional human support provided to ESG using SA was beneficial for participants. The low‐intensity program for SSG was less effective. Further studies with more participants from diverse settings with a wider range of interest in their health and weight management are needed.
DISCLOSURE
Approval of the research protocol: The name of IRB; Nagoya University Ethics Committee. The approval number; 15‐127. Informed consent: All participants provided informed consent prior to their inclusion in the study. Registry and the registration no. of the study/trial: UMIN Clinical Trials Registry (ID; 000023809). Animal studies: N/A.
CONFLICTS OF INTEREST
IO, IW, MN, and NS declare that there are no conflicts of interest.
AUTHOR CONTRIBUTIONS
IO, IW, and MN designed the study; IO, MN, and NS conducted the experiment; IO and IW analyzed the data; and all the authors were involved in writing the paper and had final approval of the submitted manuscript.
Supporting information
ACKNOWLEDGMENTS
We thank Drs. Eiji Shibata, Satoshi Osaga, and health nurse Naomi Iwanaga for their assistance to this study. This work was supported by JSPS KAKENHI Grant Number JP16K12303. We thank Editage (www.editage.jp) for English language editing.
Ozaki I, Watai I, Nishijima M, Saito N. Randomized controlled trial of Web‐based weight‐loss intervention with human support for male workers under 40. J Occup Health. 2019;61:110–120. 10.1002/1348-9585.12037
REFERENCES
- 1. World Health Organization . Fact sheet: Obesity and overweight [Web page]. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed April 7 2018.
- 2. Ministry of Health, Labour and Welfare (Japan). National Health and Nutrition Survey, 2016. Tokyo: MHLW; 2016.
- 3. Christensen JR, Kongstad MB, Sjogaard G, et al. Presenteeism among health care workers and the effect of BMI, cardiorespiratory fitness, and muscle strength. J Occup Environ Med. 2015;57(12):e146‐e152. [DOI] [PubMed] [Google Scholar]
- 4. de Mutsert R, Sun Qi, Willett WC, Hu FB, van Dam RM. Overweight in early adulthood, adult weight change, and risk of type 2 diabetes, cardiovascular diseases, and certain cancers in men: a cohort study. Am J Epidemiol. 2014;179(11):1353‐1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sogabe N, Sawada SS, Lee IM, et al. Weight change after 20 years of age and the incidence of dyslipidemia: a cohort study of Japanese male workers. J Public Health (Oxf). 2016;38(2):e77‐e83. [DOI] [PubMed] [Google Scholar]
- 6. Nanri A, Mizoue T, Takahashi Y, et al. Association of weight change in different periods of adulthood with risk of type 2 diabetes in Japanese men and women: the Japan Public Health Center‐Based Prospective Study. J Epidemiol Community Health. 2011;65(12):1104‐1110. [DOI] [PubMed] [Google Scholar]
- 7. Barnes RD, White MA, Martino S, Grilo CM. A randomized controlled trial comparing scalable weight loss treatments in primary care. Obesity. 2014;22(12):2508‐2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ma J, Yank V, Xiao L, et al. Translating the Diabetes Prevention Program lifestyle intervention for weight loss into primary care: a randomized trial. JAMA Intern Med. 2013;173(2):113‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yardley L, Ware LJ, Smith ER, et al. Randomised controlled feasibility trial of a Web‐based weight management intervention with nurse support for obese patients in primary care. Int J Behav Nutr Phys Act. 2014;11:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leahey TM, Thomas G, Fava JL, et al. Adding evidence‐based behavioral weight loss strategies to a statewide wellness campaign: a randomized clinical trial. Am J Public Health. 2014;104(7):1300‐1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pullen CH, Hageman PA, Boeckner L, Walker SN, Oberdorfer MK. Feasibility of Internet‐delivered weight loss interventions among rural women ages 50–69. J Geriatr Phys Ther. 2008;31(3):105‐112. [DOI] [PubMed] [Google Scholar]
- 12. Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172‐1177. [DOI] [PubMed] [Google Scholar]
- 13. Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003;289(14):1833‐1836. [DOI] [PubMed] [Google Scholar]
- 14. Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e‐mail counseling, computer‐automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006;166(15):1620‐1625. [DOI] [PubMed] [Google Scholar]
- 15. Digenio AG, Mancuso JP, Gerber RA, Dvorak RV. Comparison of methods for delivering a lifestyle modification program for obese patients: a randomized trial. Ann Intern Med. 2009;150(4):255‐262. [DOI] [PubMed] [Google Scholar]
- 16. Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight‐loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959‐1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harvey‐Berino J, West D, Krukowski R, et al. Internet delivered behavioral obesity treatment. Prev Med. 2010;51(2):123‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Micco N, Gold B, Buzzell P, et al. Minimal in‐person support as an adjunct to internet obesity treatment. Ann Behav Med. 2007;33(1):49‐56. [DOI] [PubMed] [Google Scholar]
- 19. Pellegrini CA, Verba SD, Otto AD, et al. The comparison of a technology‐based system and an in‐person behavioral weight loss intervention. Obesity. 2012;20(2):356‐363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gabriele JM, Carpenter BD, Tate DF, Fisher EB. Directive and nondirective e‐coach support for weight loss in overweight adults. Ann Behav Med. 2011;41(2):252‐263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mohr DC, Cuijpers P, Lehman K. Supportive Accountability: a model for providing human support to enhance adherence to ehealth intervention. J Med Internet Res. 2011;13(1):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sigler BE. Investigating the perceptions of care coordinators on using behavior theory‐based mobile health technology with Medicaid populations: a grounded theory study. JMIR mHealth uHealth. 2017;5(3):e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Santarossa S, Kane D, Senn CY, et al. Exploring the role of in‐person components for online health behavior change interventions: can a digital person‐to‐person component suffice? J Med Internet Res. 2018;20(4):e144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dennison L, Morrison L, Lloyd S, et al. Does brief telephone support improve engagement with a Web‐based weight management intervention? Randomized controlled trial. J Med Internet Res. 2014;16(3):e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ho J, Corden ME, Caccamo L, et al. Design and evaluation of a peer network to support adherence to a Web‐based intervention for adolescents. Internet Interv. 2016;6:50‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Faul F, Erdfelder E, Buchner A, Lang A‐G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Meth. 2009;41(4):1149‐1160. [DOI] [PubMed] [Google Scholar]
- 27. Faul F, Erdfelder E, Lang, et al. *Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Meth. 2007;39(2):175‐191. [DOI] [PubMed] [Google Scholar]
- 28. Japan Society for the Study of Obesity (eds). Guidelines for the Management of Obesity Disease 2016. Tokyo: Life Science Publishing; 2016:38-70. [In Japanese.]. [Google Scholar]
- 29. Kobayashi S, Murakami K, Sasaki S, et al. Comparison of relative validity of food group intakes estimated by comprehensive and brief‐type self‐administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011;14:1200‐1211. [DOI] [PubMed] [Google Scholar]
- 30. Kobayashi S, Honda S, Murakami K, et al. Both comprehensive and brief self‐administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J Epidemiol. 2012;14(7):151‐159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Murase N, Katsumura T, Ueda C, et al. Validity and reliability of Japanese version of International Physical Activity Questionnaire. J Health Welf Stat. 2002;49(11):1‐9. [In Japanese.]. [Google Scholar]
- 32. Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12‐country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381‐1395. [DOI] [PubMed] [Google Scholar]
- 33. Togari T, Yamazaki Y, Koide S, et al. Reliability and validity of the modified perceived health competence scale (PHCS) Japanese version. Jpn J Public Health. 2008;53(1):51‐57. [PubMed] [Google Scholar]
- 34. Nanri A, Tomita K, Matsushita Y, et al. Effect of six months lifestyle intervention in Japanese men with metabolic syndrome: randomized controlled trial. J Occup Health. 2012;54(3):215‐222. [DOI] [PubMed] [Google Scholar]
- 35. Munakata M, Honma H, Akasi M, et al. Repeated counselling improves the antidiabetic effects of limited individualized lifestyle guidance in metabolic syndrome: J‐STOP‐METS final results. Hypertens Res. 2011;34(5):612‐616. [DOI] [PubMed] [Google Scholar]
- 36. Imanaka M, Ando M, Kitamura T, Kawamura T. Effectiveness of web‐based self‐disclosure peer‐to‐peer support for weight loss: randomized controlled trial. J Med Internet Res. 2013;15(7):e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Usher‐Smith JA, Winther LR, Shefer GS, Silarova B, Payne RA, Griffin SJ. Factors associated with engagement with a web‐based lifestyle intervention following provision of coronary heart disease risk: mixed methods study. J Med Internet Res. 2017;19(10):e351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Walthouwer M, Oenema A, Soetens K, Lechner L, de Vries H. Implementation of web‐based interventions by Dutch occupational health centers. Health Promot Int. 2017;32(5):818‐839. [DOI] [PubMed] [Google Scholar]
- 39. Lewis S, Thomas SL, Hyde J, et al. A qualitative investigation of obese men's experiences with their weight. Am J Health Behav. 2011;35(4):458‐469. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


