Abstract
Introduction: Gingival hyperpigmentation is excessive deposition of melanin pigments in the epithelium of gingiva which affects facial esthetics. Various surgical methods for gingival depigmentation have been used to treat the darkened color of pigmented gingiva. This study compared the use of 940 nm diode laser and liquid nitrogen cryosurgery in the treatment of gingival physiologic hyperpigmentation in terms of gingival depigmentation, postoperative pain, healing duration, pigmentation recurrence, and patients’ satisfaction.
Methods: Fifteen systemically healthy patients (11 females and 4 males; 17-35 years of age) with bilateral gingival physiologic hyperpigmentation were enrolled in this split-mouth randomized study. Maxillary anterior labial gingiva of each patient was divided into left and right halves, and each half was randomly depigmented by either laser or cryosurgery. Patients were given questionnaires to evaluate the procedures and were followed up in 3, 7, 10, 17 and 21 days postoperatively for the assessment of gingival healing and 1, 3, 6 and 12 months after the treatments to detect any sign of pigmentation recurrence.
Results: The severity of post-op pain measured by visual analogue scale (VAS) was mild to average and showed no significant difference between the 2 modalities (P>0.05). There was no considerable swelling or hemorrhage after the treatment procedures and the healing duration was significantly shorter in laser (P<0.05). The degree of pigmentation in all gingival sites treated by laser reached and remained at zero until the last follow up (1 year) and reached zero in 9 out of 15 cryosurgerytreated sites. All patients were completely satisfied with the laser, and 9 out of 15 were completely satisfied with cryosurgery. No pigmentation recurrence was observed during any follow-up periods.
Conclusion: Removal of gingival physiologic hyperpigmentation by laser therapy and cryotherapy was effective and safe. The efficiency of the laser was better than cryotherapy
Keywords: Hyperpigmentation, Gingiva, Cryosurgery, Diode laser
Introduction
Gingiva like skin can suffer from hyperpigmentation with internal or external origin. One of the most important types of internal pigmentation occurs due to the excessive deposition of brown melanin pigment, and gingiva is the most common site for pigmentation inside the oral cavity.1 Hyperpigmentation of gingiva is actually not due to the increased number of melanocytes but is due to the increased activity of these cells and that leads to the increased production of melanin pigments.2,3 Gingival pigmentation occurs as light to dark brown color with symmetric stripes with specific margins. The attached gingiva is the most common area inside the oral cavity that could suffer from gingival physiologic hyperpigmentation, but it can also be observed in buccal mucosa, hard palate, lips, and tongue.3 Although gingival pigmentation is mostly benign, it causes problems in esthetics and self-confidence of the patients who show a high smile line while smiling and speaking.1,2 Different treatment techniques such as scalpel surgery, abrasion with diamond burs, electrosurgery, cryosurgery, Nd: YAG laser, CO2 laser, semiconductor diode laser, and gingivectomy with free gingival autografting, acellular dermal matrix allograft (ADMA), chemical agents such as 90% phenol and 95% alcohol have been suggested.2,4 Cryosurgery means surgery with the help of freezing at a very low temperature which involves the use of different materials like liquid CO2, a mixture of ice and salt, liquid No2, and liquid nitrogen. Cryosurgery freezes the pigmented tissue quickly and destroys the pigmented cells.5 The diode laser is another common method for the treatment of gingival physiologic hyperpigmentation. Some studies reported that laser therapy is one of the most reliable methods for the treatment of gingival depigmentation2 and it has the highest level of absorbance in melanin and is also pleasant for patients. There are different opinions regarding which of the 2 methods, either 940 nm diode laser or cryosurgery with liquid nitrogen is more reliable and effective. Since the effects of using 940 nm diode laser and cryosurgery with liquid nitrogen have not been evaluated simultaneously, thus this study compared the 2 treatment methods and suggested the more appropriate technique for the treatment of gingival physiologic hyperpigmentation.
Methods
This study was carried out as a randomized clinical trial. It was performed on the patients with bilateral gingival physiologic hyperpigmentation who were referred to the dental clinic of Arak dentistry school from March 2015 to April 2016. The patients were first visited by a periodontist and their pigmentation type was diagnosed and categorized. By excluding other causes of gingival hyperpigmentation such as oral melanotic macule, malignant melanoma, drug-induced melanosis, smoker’s melanosis, melanosis associated with systemic and genetic diseases, hemochromatosis, amalgam tattoo, graphite tattoo, decorative tattoos, pigmentation due to pharmaceutical and heavy metals and pregnancy-related pigmentation, a total of 15 subjects were selected in this study which comprised of 11 females and 4 males, aged 17 to 35 years (mean age = 28.2±8.4) who signed a consent form. This study was performed in accordance with the Helsinki Declaration of 1975, as revised in 2000 and approved by ethics council of Arak University of Medical Sciences. Before any treatment, patients underwent full-mouth scaling, after which oral hygiene instructions were given. Then, the maxillary gingiva of each patient was split into right and left halves (split-mouth technique). One half was treated by 940 nm diode laser and the other half by cryosurgery. The divided areas were randomly allotted for depigmentation by the coin toss. According to the average of patients’ smile line, the decision was made to treat the gingiva of all patients at each quadrant from the central incisor to the distal of the first molar. The laser device was of EpicTM 10 diode type with wavelength of 940 ± 10 nm, operating maximum power output of 10 W, 0.01 ms to 20 seconds pulse duration, contact continuous mode, with 300 μm fiber tip diameter, spot size 30 mm diameter (= 7.1 cm2 area) and manufactured by Biolase Company, USA (Figure 1). Firstly, gingiva received topical anesthesia with 2% lidocaine gel and the tip of the laser was placed and moved on the entire pigmented area from the mucogingival line towards the free gingival margin, including the papillae until the pigmented area was deepithelialized and a normal pink color of gingiva was apparent. The carbonized gingiva was wiped with moist sterile gauze to ensure that no pigmented spots remained. In cryosurgery, a 10-L 3-chambered tank of liquid nitrogen (-196°C) was used. Some liquid nitrogen was poured inside a plastic cup and the tip of a cotton swab was dipped in the liquid and placed inside a small finger-like plastic and then placed on the pigmented gingiva for 3 to 5 seconds (Figure 2). The patients were followed up in 3, 7, 10, 17, 21 days, and 1, 3, 6, 12 months after the treatment. The 2 techniques, laser therapy, and cryotherapy were compared in terms of 5 parameters. These parameters are: (1) The amount of gingival pigmentation before and after the treatment; (2) The amount of pain after treatment; (3) The duration of gingival healing after the treatment; (4) The amount of pigmentation recurrence after the treatment; and (5) The amount of patients’ satisfaction with the treatment results. The extent of pigmentation was measured according to Gingival Pigmentation Index (GPI) and was graded from 0 to 3 (Table 1). All gingival sites were compared with each other and the color intensity of gingival pigmentation for each patient was graded from 0 to 3 in such a way that the darkest gingiva was given a score of 3 and the lightest gingiva had a score of 1. Digital pictures were taken before and after treatment within the same position and location of the light, using a calibrated Canon PowerShot A710 IS camera.
Figure 1.
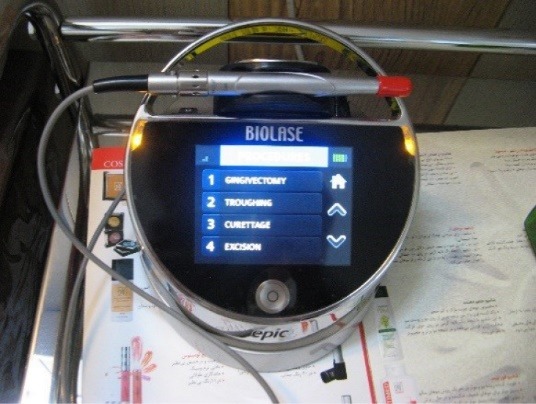
Biolase EpicTM 10 Diode Laser Device.
Figure 2.

(A) Liquid Nitrogen Delivery Device, (B) Placement of Dipped Cotton Swab On Patient’s Gingiva, (C) Liquid Nitrogen Stays on the Gingiva for a Few Seconds.
Table 1. GPI (Extent of Pigmentation) Scoring .
| Score | Criteria |
| 0 | Absence of pigmentation, pink color of the gingiva |
| 1 | Spots of brown to black pigmentation |
| 2 | Brown to black pigmentation, more than spots but not diffuse (patches of pigmentation) |
| 3 | Diffuse brown to black pigmentation |
Consistency, contour, and color of gingiva and the amount of gingival healing after surgery was assessed by 2 periodontists who were unaware of the treatment techniques received by each site (blind experts). Dentists calibrated the examiners. The amount of pain after the treatment was measured by VAS (Table 2). In a questionnaire, the patients were asked to mark the severity of pain on a line marked from 0 to 100 (Figure 3). Then, the score of the patients’ pain was matched with the VAS table. The satisfaction of patients with the surgery result was measured in a questionnaire (Figure 4). The data collected from the questionnaires were analyzed by SPSS 21 software. In the descriptive analysis, the mean, standard deviation, and frequency percent were used. Chi-square, Student t test, and two-way analysis of variance (ANOVA) repeated measures tests were used to analyze the results. Differences were considered as statistically significant at P<0.05.
Table 2. VAS tabl .
| Marked Area on the VAS Line | Severity of Pain |
| 0-4 mm | None |
| 5-44 mm | Slight |
| 45-74 mm | Moderate |
| 75-100 mm | Severe |
Figure 3.
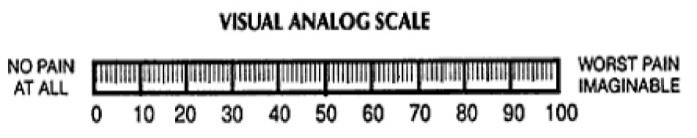
VAS Line.
Figure 4.
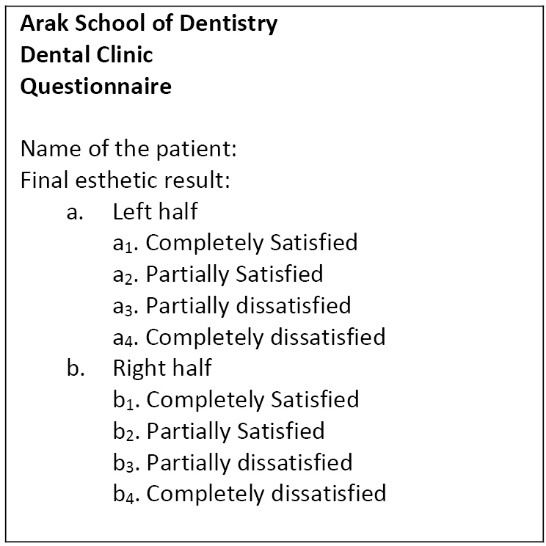
Questionnaire to Assess Patient Satisfaction.
Results
In the present study, none of the patients had any complications. Healing event and the results of the 2 methods were good (Figure 5).
Figure 5.
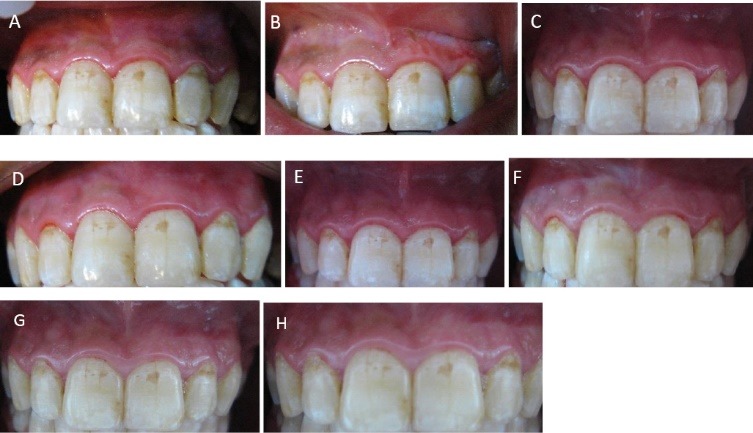
Follow Up Periods: (A) Pre-operative, (B) During the procedure (Laser on the left Quadrant; Cryosurgery on the Right Quadrant), (C) 1 week post-op (assessing wound healing), (D) 2 week post-op (assessing wound healing), (E) 1 month post-op, (F) 3 months post-op, (G) 6 months post-op, (H) 12 months post-op (No recurrence).
The Comparison of Pain Index
According to the results of Student’s t test, the amount of felt pain based on VAS scale on the day of treatment which varied from 0.5 to 6 for laser therapy and from 1 to 6 for cryotherapy, showed no significant difference with each other (P > 0.05; Table 3).
Table 3. Pain Perception for Laser and Cryosurgery .
| Group | Mean ± SD | P Value | F Value | |
| VAS score on day 1 | Laser | 2.36 ± 1.83 | 0.803 | 0.063 |
| Cryosurgery | 1.60 ± 1.68 | 0.803 | 0.063 |
The Duration of Gingival Healing
The duration of gingival healing varied from 3 to 14 days and 7 to 21 days in the treatment by laser and cryosurgery, respectively. Student’s t-test analysis showed a significant difference between the 2 groups in terms of gingival healing (P < 0.05; Table 4).
Table 4. Healing Duration After the Procedures .
| Group | Mean ± SD | P Value | F Value | |
| Healing time | Laser | 5.07 ± 3.13 | 0.004 | 0.981 |
| Cryosurgery | 9.47 ± 4.41 | 0.004 | 0.981 |
The Level of Individuals’ Satisfaction
There was a significant difference between the 2 groups, so that all patients were completely satisfied with the laser, while only 60% of patients were completely satisfied with cryosurgery (P < 0.05; Table 5).
Table 5. Levels of Patients’ Satisfaction About the Procedures Outcome .
| Individual Count | Expected Count | Chi-Square Test | P Value | |||
| Completely Satisfied | Partially Satisfied | Completely Satisfied | Partially Satisfied | |||
| Laser | 15 | 0 | 12 | 3 | 7.50 | 0.006 |
| Cryosurgery | 9 | 6 | 12 | 3 | ||
Degree of Depigmentation
Differences between the 2 methods in terms of GPI (extent of pigmentation and color intensity) during the follow-up periods were significant (P < 0.05; Tables 6 and 7).
Table 6. Two-Way ANOVA Repeated Measures Analysis for the Comparison of Extent of Gingival Pigmentation Through Time Between Laser and Cryosurgery .
| Source | df | Mean Square | F Value | P Value |
| Treatment*Time | 6 | 0.376 | 8.778 | 0.000 |
| Error | 84 | 0.043 |
Table 7. Two-Way ANOVA Repeated Measures Analysis for the Comparison of Color Intensity of Pigmentation Through Time Between Laser and Cryosurgery .
| Source | df | Mean Square | F Value | P Value |
| Treatment*Time | 6 | 0.230 | 6.656 | 0.000 |
| Error | 84 | 0.035 |
The laser was a better treatment modality for depigmentation because GPI in all patients reached zero. At the first week of following-up the degree of GPI reached zero in the terms of the extent of pigmentation and color intensity in 14 laser-treated gingival sites, and at the second week upon completion of gingival healing it became zero in all patients and remained zero until the last follow-up. However, the degree of pigmentation became zero in 9 out of 15 patients who received cryosurgery; although it reduced in the remaining 6 patients but did not become zero with re-treatments. Figure 6 shows that GPI had a significant difference between the 2 treatments over time so that laser had lesser GPI as compared to cryosurgery and the relationship between treatment and time was a continuous line, indicating no pigmentation recurrence during 12 months.
Figure 6.
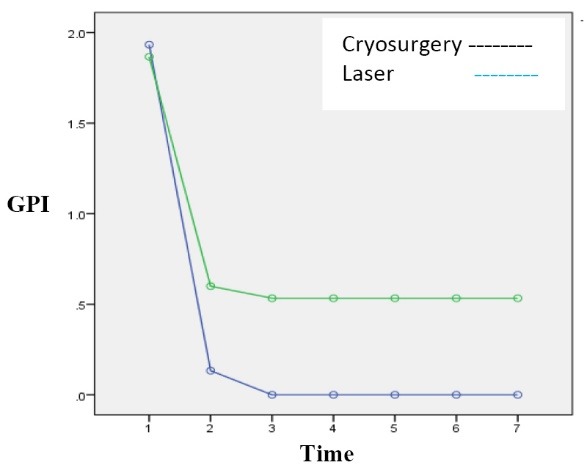
Variation of GPI Over Time.
Discussion
The present study is a one-year split-mouth clinical trial comparing diode laser ablation and liquid nitrogen cryosurgery for physiologic gingival pigmentation removal. The internal pigmentation of gingiva occurs due to the excessive deposition of brown melanin pigment, and gingiva is the most common site of pigmentation inside the oral mucosa. Gingival hyperpigmentation may cause unpleasant facial appearance which makes affected individuals seek for treatment. Various modalities are being used to treat gingival hyperpigmentation. Laser and cryotherapy are among the widely performed in research techniques for this treatment. Diode lasers (800-980 nm) is quickly absorbed by hemoglobin, melanin and other pigments. It penetrates into the tissue by one of the methods of absorption, propagation, radiation, and reflection. The penetration is done by laser energy and changes energy into heat which eventually causes physical changes.6 It seems that laser affects the production of melanin, pigment cells and melanocytes gene expression and reduces hyperpigmentation.7 Diode lasers are becoming popular in intraoral soft tissue procedures and in fact, a variety of scientific researches are being conducted to find their advantages or disadvantages over other gingival depigmentation treatment procedures.8 Laser surgery of gingival hyperpigmentation has several advantages over other modalities including less postoperative pain. Postoperative pain has been documented by some studies that used different types of laser, whereas other studies reported no pain. In fact, the observed different pain levels vary with regards to the type of used treatment techniques. There seems to be a lesser amount of post-op pain for cryosurgery and laser surgical procedures compared to other gingival depigmentation techniques.9-15 The lesser amount of post-op pain for the laser is due to the coagulation of protein on the wound surface that serves as a biological wound dressing. In addition, the laser has the ability to seal the sensory nerve endings.9,16 Rao et al10 reported slight pain after cryosurgery with NO2 and diode laser therapy with no statistically significant difference. Ribeiro et al11 and Lagdive et al12 also reported that the sites treated with laser had slight or no pain. Kaya et al11 compared diode and Er: YAG lasers in the treatment of gingival melanin pigmentation and showed mild postoperative pain for both treatment modalities. Rahmati et al17 recorded some pain reports by the patients, one to three days after cryosurgery with liquid nitrogen. The results of all mentioned studies are consistent with this study. However, Azzeh18 used Er: YAG laser for gingival depigmentation and reported no post-op pain. The absence of pain could be due to the unique characteristics of Er: YAG laser which involves the least tissue penetration and thermal damage of Er: YAG laser among all lasers which result in low tissue necrosis. Also, Shirazi et al19 reported no post-op pain for the patients who received liquid nitrogen cryosurgery, which is inconsistent with this study. The probable cause for the lack of post-op pain after cryosurgery in the study of Shirazi et al19 is the age range of participants (11 to 14 years) which is considered as adolescents and have a tendency to minimize or deny the perceived pain.20 Therefore, the provided reports of these patients are not considered reliable.
Another reported advantage of the laser is shorter healing duration of gingiva after depigmentation procedure. The reported duration of the gingival healing after depigmentation varies. Sharon et al21 and Esen et al22 reported 2 weeks and 6 weeks period for post-op healing after depigmentation with Co2 cryotherapy, respectively, and Atsawasuwan et al23 reported that complete healing was achieved in 1-3 weeks after Nd: YAG laser application. Those results are consistent with this study that recorded healing time of up to 2 weeks for laser treated areas and up to 3 weeks for cryosurgery treated gingival sites. In the studies of Berk et al,24 Thangavelu et al25 and Murthy et al,13 who used diode laser for the treatment of gingival physiologic hyperpigmentation, 1 week after operation gingiva healed and its color were pink. Govila et al26 used 940 nm diode laser for gingival depigmentation and patients completely recovered after 1 week. The results of these studies are in accordance with the present study. Regarding the effect of the laser on tissue healing, it is stated that the intensity of the laser has an important role in its effects.27 Laser radiation increases RNA and DNA synthesis and also stimulates the synthesis of proteins.28 Sing et al14 compared the 2 methods of diode laser therapy and cryosurgery in the treatment of gingival physiologic hyperpigmentation. The patients went under 3, 6, 12 and 18 months follow-up. They reported that both treatments were safe and satisfactory and the duration of healing for the gingival sites treated with laser was shorter than cryosurgery that is in accordance with the present study in which faster healing properties of the laser was observed. It has been stated that laser reduces bacteria, affects pigmentation and enhances wound healing by producing reactive oxygen species (ROS) due to its antibacterial effects and fibroblasts and collagen formation.29 Therefore, the faster healing of laser-treated gingival sites in the present study is probably due to the mentioned mechanism. Cryosurgery often causes considerable inflammation in the area under treatment which leads to the destruction of soft tissues on the first day.
Melanin hyperpigmentation score was assessed by GPI index 1 week, 2 weeks, 1 month, 3 months, 6 months and 12 months, postoperatively. Several studies have reported different rates of depigmentation and repigmentation with regards to different techniques used and follow up periods. In the present study, statistical significant difference existed in the melanin scores between the 2 techniques, laser showed a better efficiency in terms of pigmentation removal, and there were no signs of pigmentation recurrence for both modalities at the end of 1 year. The clinical reoccurrence of melanin pigmentation after a period of clinical depigmentation is known as “Repigmentation.” Postoperative gingival repigmentation has been documented in the literature and time of regimentation varies. Repigmentation occurs due to failure in complete removal of active melanocytic cells from the epithelial basal layer and it reoccurs as a result of melanocyte migration from surrounding gingival areas.9,16
According to the type of treatment techniques, the degree of depigmentation varied among studies. Darbandi et al30 used the nitrogen oxide cryoprobe for the treatment of gingival physiologic hyperpigmentation. Patients were treated in one session and their study results showed that 60% of the patients were healed 7 days after cryosurgery and in the other 40%, the areas of pigmentation remained pale. Two weeks after, only 10% of the lesions were pale and after 1 month all pigmented lesions were healed and there was no recurrence in 4 and 6 months follow-ups. This study showed a 100% effectiveness of cryotherapy in gingival pigmentation removal after one month. However, in the present study, the gingival sites did not achieve zero pigmentation after one session of N2 cryotherapy, even after re-cryotherapy sessions GPI index did not change. It seems that this difference might be due to the probable differences in the effectiveness of cryotherapy methods. Shirazi et al19 studied the treatment of gingival physiologic hyperpigmentation in teenagers with liquid nitrogen cryosurgery in a 12 month period. The patients’ gingiva was treated by cotton swab dipped in liquid nitrogen in the anterior area of the upper and lower jaws for 2 times with 2 weeks intervals. Statistical results showed a descending reduction in severity and color intensity of gingival pigmentation 3 months after the treatment. Although the severity of pigmentation gradually reduced but did not reach zero, which is in accordance with the present study. There was also the recurrence of pigmentation in 1–year follow-up which is inconsistent with the present study results. Govila et al26 used 940 nm diode laser for gingival depigmentation. The patients completely recovered after 1 week and were satisfied enough with the treatment results. No sign of recurrence of gingival pigmentation was reported after 3 years of follow-up. The result of this study is consistent with the present study in terms of recurrence of lesions. Although the duration of the present study was shorter, in order to evaluate pigmentation recurrence more accurately, more studies with a longer period of recalls are needed. Sing et al14 compared 2 methods of diode laser therapy and tetrafluoroethane cryosurgery in the treatment of gingival physiologic hyperpigmentation. The patients underwent 3, 6, 12 and 18 months follow-up. The pigmentation degree of all patients treated with laser and cryosurgery was zero in a 6-month follow-up. It seems that tetrafluoroethane is more effective than the use of liquid nitrogen with cotton swab which was used in the present study. Talebi et al31 in a case study treated the gingival hyperpigmentation of a 9-year-old boy using liquid nitrogen and a cotton swab. The patient was followed-up for 12 months. They concluded that cryosurgery is a simple method with no recurrence of gingival lesions, which is similar to the present study results. Soliman et al32 studied the treatment of gingival physiologic hyperpigmentation using 808 nm diode laser. Most patients needed 2 treatment sessions while in the present study all patients needed only one session for the complete depigmentation of gingiva using 980 nm diode lasers. There was no sign of recurrence after 9 months which is similar to the results of the present study. Lin et al8 conducted a systematic review study on 61 studies conducted between 1951 to 2013 regarding different methods of treatment for the removal of gingival melanin pigmentation. They concluded that cryosurgery and laser therapy are the best and most reliable treatment methods for melanin pigmentation removal and show less recurrence of hyperpigmentation. However, laser therapy especially diode laser seemed to be the best option. In the present study, the laser was also a better option compared to cryosurgery. Patil et al15 used 940 nm diode laser to treat an 18-year-old woman who suffered from gingival physiologic hyperpigmentation. After 1 week, the gingiva had no pigmentation, but after 6 months, pale patches appeared, and after 1 year the recurrent pigmentation was larger. While in the present study, no sign of recurrence was seen after 12 months. In the study of Doshi et al33 the treatment of gingival hyperpigmentation was done using 940 nm diode laser. The recurrence of pigmented lesions was reported after 1 year which is inconsistent with the results of the present study, but the regimentation could actually be the result of post-inflammatory hyperpigmentation caused by the high power of the laser used for depigmentation process.
All patients were completely satisfied with the results of laser because all laser-treated sites achieved zero GPI, while only 9 out of 15 patients, who reached zero pigmentation with cryotherapy, showed complete satisfaction about the results. In the study of Shirazi et al.19 although the severity of pigmentation after liquid nitrogen cryosurgery gradually reduced, but did not become zero and repigmentation was observed in one year follow-up and patients were satisfied with the results, while in the present study, those whose pigmentation degree reduced but did not reach zero showed a relative satisfaction. Govila et al26 used 940 nm diode laser for gingival depigmentation and all patients showed complete satisfaction with the results that are in accordance with our study results. In the present study, patients’ satisfaction was merely related to the results of depigmentation, and post-op pain had no effect on that. Thus, patients’ preference was a diode laser.
Jha et al34 treated gingival hyperpigmentation and stated that dental lasers are advanced modalities with enhanced precision of control compared to other depigmentation procedures. Laser procedures are safer, more comfortable and user-friendly to both patients and dentists and are expected to become more popular in time. All types of diode lasers from 810 nm to 1064 nm are becoming widely used in dentistry because of their small size, ease of manipulation in soft tissue surgery and lower cost compared to other lasers. The results of the present study show that both diode laser and liquid nitrogen cryosurgery can perform effective and satisfactory depigmentation of gingiva and are well-tolerated by the patients. However, the laser is a more optimal treatment.
Conclusion
The results of the present study indicate that 940 nm diode laser showed better effectiveness in comparison to cryosurgery with liquid nitrogen in the treatment of gingival physiologic hyperpigmentation using Split Mouth technique. Recurrence of pigmentation was not observed in any gingival sites treated by both laser and cryotherapy during the 12 months follow up.
Conflict of Interests
Authors have no conflict of interest to declare.
Ethical Considerations
This study registered in the Iranian Registry of Clinical Trials website (identifier: IRCT20160408027277N1; https://www.irct.ir/trial/28866).
Conflict of Interests
The authors declare no conflict of interest.
Please cite this article as follows: Jokar L, Bayani M, Hamidi H, Keivan M, Azari-Marhabi A. A comparison of 940 nm diode laser and cryosurgery with liquid nitrogen in the treatment of gingival physiologic hyperpigmentation using split mouth technique: 12 months follow up. J Lasers Med Sci. 2019;10(2):131-138. doi:10.15171/jlms.2019.21.
References
- 1.Abdel Moneim RA, El Deeb M, Rabea AA. Gingival pigmentation (cause, treatment and histological preview) Fut Dent J. 2017;3(1):1–7. doi: 10.1016/j.fdj.2017.04.002. [DOI] [Google Scholar]
- 2. Glick M. Burket’s Oral Medicine. 12th ed. USA: People’s Medical Publishing House; 2015.
- 3.Sabrinath B, Sivapathasundharam B, Ghosh G, Dhivya Dhivya. Pigmentation. Indian J Dent Adv. 2009;1(1):38–45. [Google Scholar]
- 4.Farahmand AH, Moghareh Abed A, Mansouri Y. Clinical Application of ErYAG Laser and Cryosurgery in Gingival Depigmentation. World J Dent. 2014;5(2):102–8. [Google Scholar]
- 5.Özcan M, Işler SC, Bozkaya S, Özcan G. Complication after cryosurgery treatment for gingival melanin pigmentation: a case report. Clinic Adv Periodontics. 2015;5(1):56–60. doi: 10.1902/cap.2013.120124. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal N, Bhowmick D, Sinha A, Mishra A, Shukla S, Singh D. Depigmentation of gingiva using semiconductor diode laser: a clinical case report. J Pak Dent Assoc. 2014;23(3):126–30. [Google Scholar]
- 7.Azma E, Safavi N. Diode laser application in soft tissue oral surgery. J Lasers Med Sci. 2013;4(4):206–211. [PMC free article] [PubMed] [Google Scholar]
- 8.Lin YH, Tu YK, Lu C. et al. Systematic Review of treatment modalities for gingival depigmentation: a random-effects poisson regression analysis. J Esthet Restor Dent. 2014;26(3):162–178. doi: 10.1111/jerd.12087. [DOI] [PubMed] [Google Scholar]
- 9.Bakutra G, Shankarapillai R, Mathur L, Manohar B. Comparative evaluation of diode laser ablation and surgical stripping technique for gingival depigmentation: a clinical and immunohistochemical study. Int J Health Sci. 2017;11(2):51–58. [PMC free article] [PubMed] [Google Scholar]
- 10.Rao PVN, Penmetsa GS, Dwarakanath CD. Gingival depigmentation by cryosurgery and laser application - a comparative clinical study. Br J Med Med Res. 2015;5(11):1403–1412. doi: 10.9734/BJMMR/2015/12870. [DOI] [Google Scholar]
- 11.Ribeiro FV, Cavaller CP, Casarin RC. et al. Esthetic treatment of gingival hyperpigmentation with Nd:YAG laser or scalpel technique: a 6 month RCT of patient and professional assessment. Lasers Med Sci. 2014;29(2):537–544. doi: 10.1007/s10103-012-1254-5. [DOI] [PubMed] [Google Scholar]
- 12.Lagdive S, Doshi Y, Marawar PP. Management of gingival hyperpigmentation using surgical blade and diode laser therapy: a comparative study. J Oral Laser Appl. 2009;9(1):41–7. doi: 10.4103/0974-2077.91256. [DOI] [Google Scholar]
- 13.Murthy MB, Kaur J, Das R. Treatment of gingival hyperpigmentation with rotary abrasive, scalpel, and laser techniques: a case series. J Indian Soc Periodontol. 2012;16(4):614–619. doi: 10.4103/0972-124X.106933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh V, Giliyar SB, Kumar S, Bhat M. Comparative evaluation of gingival depigmentation by diode laser and cryosurgery using tetrafluoroethane:18-month follow-up. Clin Adv Periodontics. 2012;2(3):129–34. doi: 10.1902/cap.2012.110008. [DOI] [Google Scholar]
- 15.Patil KP, Joshi V, Waghmode V, Kanakdande V. Gingival depigmentation: A split mouth comparative study between scalpel and Cryosurgery. Contemp Clin Dent. 2015;6(1):97–101. doi: 10.4103/0976-237X.152964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaya GS, Yavuz GY, Sümbüllü MA, Dayı E. A comparison of diode laser and Er:YAG lasers in the treatment of gingival melanin pigmentation. Int J Health Sci. 2012;113(3):293–299. doi: 10.1016/j.tripleo.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Rahmati S, Darijani M, Nourelahi M. Comparison of surgical blade and cryosurgery with liquid nitrogen techniques in treatment of physiologic gingival pigmentation: short term results. J Dent Shiraz. 2014;15(4):161–166. [PMC free article] [PubMed] [Google Scholar]
- 18.Azzeh MM. Treatment of Gingival hyperpigmentation by erbium-doped:yttrium, aluminum, and garnet laser for esthetic purposes. J Periodontol. 2007;78(1):177–184. doi: 10.1902/jop.2007.060167. [DOI] [PubMed] [Google Scholar]
- 19.Shirazi ARS, Taghavi AM, Khorakian F. Treatment of gingival physiologic pigmentation in adolescent using cryosurgery technique with liquid nitrogen: one year follow up. J Mashhad Dent Sch. 2010;33(4):331–342. [Google Scholar]
- 20.Hagan JF Jr, Coleman WL, Foy JM. et al. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108(3):793–797. doi: 10.1542/peds.108.3.793. [DOI] [PubMed] [Google Scholar]
- 21.Sharon E, Azaz B, Ulmansky M. Vaporization of melanin in oral tissues and skin with a carbon dioxide laser: a canine study. J Oral Maxillofac Surg. 2000;58(12):1387–1393. doi: 10.1053/joms.2000.18272. [DOI] [PubMed] [Google Scholar]
- 22.Esen E, Haytac MC, Oz IA, Erdog˘an O, Karsli ED. Gingival melanin pigmentation and its treatment with the CO2 laser . Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(5):522–527. doi: 10.1016/j.tripleo.2004.02.059. [DOI] [PubMed] [Google Scholar]
- 23.Atsawasuwan P, Greethong K, Nimmanon V. Treatment of gingival hyperpigmentation for esthetic purposes by Nd:YAG laser: report of 4 cases. J Periodontol. 2000;71(2):315–21. doi: 10.1902/jop.2000.71.2.315. [DOI] [PubMed] [Google Scholar]
- 24.Berk G, Atici K, Berk N. Treatment of gingival pigmentation with Er, Cr:YSGG laser. J Oral Laser Appl. 2005;5(4):249–53. [Google Scholar]
- 25.Thangavelu A, Elavarasu S, Jayapalan P. Pink esthetics in periodontics - gingival depigmentation: a case series. J Pharm Bioallied Sci. 2012;4(2):186–190. doi: 10.4103/0975-7406.100267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Govila V, Gulati M, Govila S. Diode laser applications in periodontics. Indian J Dent Sci. 2011;3(5):64–67. [Google Scholar]
- 27.Saygun I, Karacay S, Serdar M, Ural AU, Sencimen M, Kurtis B. Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1 (IGFBP3) from gingival fibroblasts. Lasers Med Sci. 2008;23(2):211–5. doi: 10.1016/S107921040400160X. [DOI] [PubMed] [Google Scholar]
- 28.Yu W, Naim JO, Lanzafame RJ. The effect of laser irradiation on the release of bFGF from 3T3 fibroblasts. Photochem Photobiol. 1994;59(2):167–170. doi: 10.1111/j.1751-1097.1994.tb05017.x. [DOI] [PubMed] [Google Scholar]
- 29.Ozturan S, Ususmez A. Case report: asethetic treatment of gingival hyperpigmentation by Er:YAG laser. J Laser Health Acad. 2013;2013(1):1–3. [Google Scholar]
- 30.Darbandi A, Shahbaz NA. Effect of cryotherapy on physiologic pigmentation of oral mucosa: a preliminary study. J Dent Tehran Univ Med Sci. 2004;1(2):49–52. [Google Scholar]
- 31.Talebi M, Farmanbar N, Abolfazli S, Shirazi AS. Management of physiological hyperpigmentation of oral mucosa by cryosurgical treatment: a case report. J Dent Res Dent Clin Dent Prospects. 2012;6(4):148–151. doi: 10.5681/joddd.2012.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soliman MM, Al Thomali Y, Al Shammrani A, El Gazaerly H. The use of soft tissue diode laser in the treatment of oral hyper pigmentation. Int J Health Sci. 2014;8(2):133–140. doi: 10.12816/0006079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doshi Y, Khandge N, Byakod G, Patil P. Management of gingival pigmentation with diode laser: is it a predictive tool? Int J Laser Dent. 2012;2(1):29–32. [Google Scholar]
- 34.Jha N, Ryu JJ, Wahab R, Al-Khedhairy AA, Choi EH, Kaushik NK. Treatment of oral hyperpigmentation and gummy smile using lasers and role of plasma as a novel treatment technique in dentistry: an introductory review. Oncotarget. 2017;8(12):20496–20509. doi: 10.18632/oncotarget.14887. [DOI] [PMC free article] [PubMed] [Google Scholar]


