Abstract
Introduction: Dentinal hypersensitivity (DH) is an acute intensive tooth pain which can lead to dental annoyances during eating and drinking. Stimulating exposed dentinal tubules by either kind of thermal, tactile, chemical and/or osmotic stimuli is believed to be the cause of this pain. It is hypothesized that dentinal tubules’ orifice occlusion (DOO) can help relieve such dental irritations. Thus, this systematic review was conducted to evaluate the effectiveness of laser application as a prevention and treatment modality on DH reduction.
Methods: Electronic databases (MEDLINE, SCOPUS) were searched among randomized clinical trials from January 2007 to December 2016. The extraction of data and quality assessments were carried out by different independent observers.
Results: A total of 499 items were found of which3 9 relevant articles were extracted. The profound findings proved lasers’ effectiveness as a treatment of DH. Although some of the researches reported no significant difference between laser and other desensitizing agents, most of the studies suggested that better results (both rapid and long-lasting) were obtained in combined modalities. Furthermore, the preventive role of this new technology has been emphasized as well. Nd-YAG (neodymium-doped yttrium aluminum garnet) and diode lasers reduce DH after bleaching. Lasers can also protect cervical restorations from DH due to tubular occlusion. Moreover, it is suggested to apply lasers in relief of DH following scaling and root planning. Nevertheless, a few researchers dispute its beneficence as a result of placebo effect.
Conclusion: The results obtained from several studies in the present review revealed that the application of lasers is effective not only in terms of treatment of DH, but also in the prevention of this intensive tooth pain. Among various types of lasers, the application of Nd:YAG laser has shown the best results in DH treatment.
Keywords: Dentinal hypersensitivity, Laser, Treatment, Prevention
Introduction
Dentinal hypersensitivity (DH) is defined as a fairly specific acute intensive tooth pain which cannot be qualified as any other type of dental pathology. Stimulating exposed dentinal tubules by either kind of thermal, tactile, chemical and/or osmotic stimuli is believed to be the cause of this pain.1 Dentine hypersensitivity is a very common clinical symptom which has increased in prevalence through the past few years.2-6 Epidemiological researches have shown that the prevalence of DH varies from 2.8% in a cross-sectional study of patients visiting general dental practitioners7 to 98% in a population of patients referred to a specialist periodontology department.8,9 Meanwhile, different diagnostic criteria and selection bias in the enrollment of the study samples could be the potential explanations for this vast range of DH prevalence.8
DH may be initiated under several conditions. Attrition following excessive or parafunctional habits, abrasion subsequent to incorrect brushing technique, and microfractures or abfractures caused by heavy eccentric occlusal forces have been suggested as common predisposing factors. Moreover, erosion due to exposure to chemical products, medication and endogenous acids from reflux or regurgitation of stomach acid will make dentin prone to sensitivity.10-12 Even gingival recessions due to abrasion, dehiscences and fenestrations, frenum pulls and orthodontic movement, root exposure following age advances, postdental bleaching, and exposure of dentinal tubules following the removal of supra and/or subgingival calculi could predispose teeth to hypersensitivity.11,12 Most often, a combination of these conditions results in dentin hypersensitivity rather than one factor merely.13
Several theories have been introduced to explain the physiologic mechanisms occurring in DH.12 The most commonly accepted hypothesis is the classic hydrodynamic theory which was first developed by Brannstrom and Astrom in 1972. In this mechanism, basically, the stimulation of exposed dentinal tubules by certain stimuli leads to an increase in the fluid flow within dentinal tubules. Formerly, the movement of fluid creates a pressure change across the entire dentine which can stimulate individual intrapulpal nerves. Therefore, the ability to block dentinal tubules and reduce the movement of fluid in dentinal tubules or/and block pulpal nerve are considered among the necessities of the ideal treatment of DH.14-16 Moreover, the optimal treatment technique must have fast and long-lasting effects in the absence of any pulpal irritation and tooth pain.8,17
Many agents and treatment approaches have been used for prevention and treatment of dentine hypersensitivity. In this respect, the desensitizing methods are implemented either by the patient for home use, usually in the form of a dentifrice containing potassium salt, or professionally by a dentist using in-office topical desensitizing agents or very sophisticated equipment such as laser.17,18
Laser therapy was first applied for treating dentine hypersensitivity by Matsumoto et al in 1985.18 Since then, numerous studies investigating the effectiveness of lasers in the treatment of dentine hypersensitivity have been reported.12,19,20 Reviewing the literature, it was shown that low power lasers such as gallium/aluminum/arsenide (GaAlAs) diode laser reduce sensitivity following their effect on the nervous level, whereas the medium power lasers, including CO2, Nd:YAG, and Er:YAG lasers cause desensitization due to dentinal tubules’ orifice occlusion (DOO).13 A combination of laser therapy and desensitizing agents’ application has also been suggested to improve the treatment results.17
Furthermore, the preventive role of this sophisticated technology has been emphasized as well. For example, Nd-YAG and diode lasers are used to reduce DH subsequent to bleaching. Lasers can also protect cervical restorations from DH due to DOO. Moreover, it is suggested to apply lasers in relief of DH following scaling and root planning.21-23
Therefore, the objective of this article is to assess the efficiency of the various types of lasers used in dentistry for prevention and treatment of DH.
Methods
Search Strategies
The electronic databases (MEDLINE, SCOPUS) were searched by 2 independent researchers from January 2007 to December 2016 using the following keywords: “dentin sensitivity”[All Fields] OR “dentinal sensitivity”[All Fields] OR “dentin hypersensitivity”[All Fields] OR “dentinal hypersensitivity”[All Fields] AND (“laser”[All Fields] OR “lasers”[All Fields]).
All obtained papers were evaluated and selected based on the following inclusion criteria (Figure 1): RCTs and in vivo studies conducted in the recent 10 years.
Figure 1.
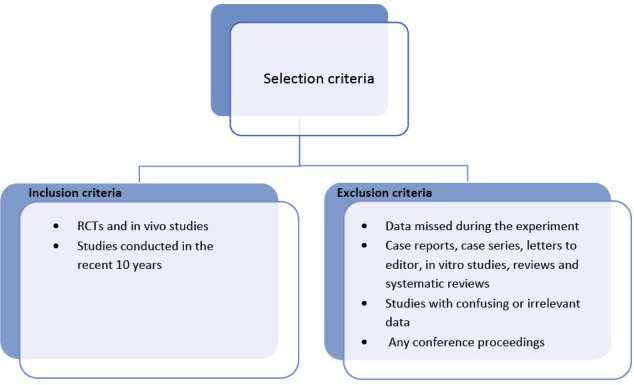
Selection Criteria.
In the next stage, the following exclusion criteria were applied: any data missed during the experiment, case reports, case series, letters to editor, in vitro studies, reviews and systematic reviews, studies with confusing or irrelevant data, and any conference proceedings.
Study Selection
Out of 499 results, 39 relevant literatures were selected (Figure 2). The abstracts were reviewed by two independent observers. After the screening and accomplishment of the admissibility criteria, the article was admitted if an agreement was reached. If any disparity was seen between the opinions, a third author was invited to discuss the article. Only those works that fulfilled all criteria were included in the study.
Figure 2.
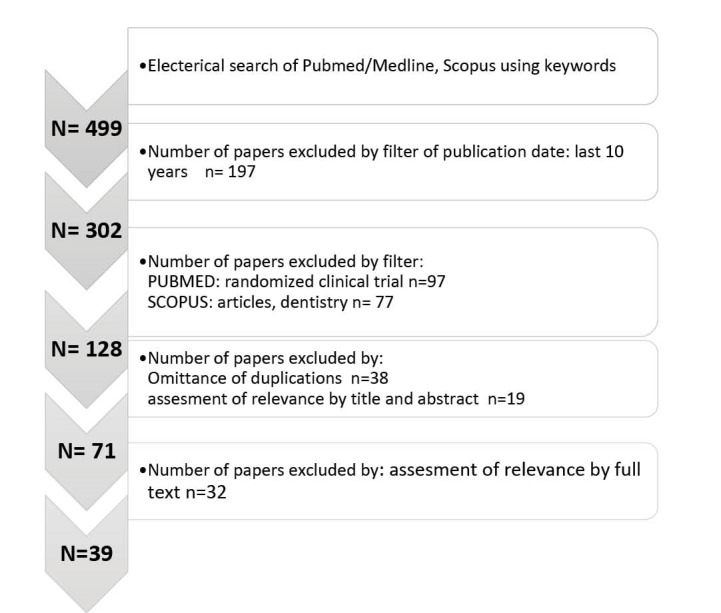
Flowchart for Literature Search and Study Selection.
Data Extraction
A standard chart form of the obtained data was prepared separately including authors’ names, publication date, objectives, number of patients and case selection, laser types as well as their parameters, desensitizing agent details, group tests, treatment procedures plus their intervals, measurement methods of DH, follow-up periods and the results (Table 1).
Table 1. Characteristics of 39 studies were involved for the final analysis .
| ID | Study, Year, Country | Sample Size | Treatment Groups and Specifications | TX. Interval | Pain Stimulation | DH Measurement | Follow-up Period | Results |
| 1 | Moosavi et al (2016), Iran | 66 patients |
Placebo LLRL Diode laser (660 nm InGaAlP, 200 mW, 15 s) LLIL Diode laser (810 nm GaAIAs, 200 mW, 15 s) |
1 | _ | VAS | 48 hours | 810-nm LLIL was significantly more effective than that of the 660-nm laser in DH reduction at 24 h after bleaching, although both laser groups experienced significantly lower pain level than the placebo after 48-h. |
| 2 | Soares et al (2016), UK |
23 patients (89 teeth) |
Placebo 2% neutral fluoride gel for 60 s. Nd:YAG laser (1, 10 Hz, 60 s) GaAlAs laser (40 mW; 4 J/cm2, 60 s) |
1 | _ | VAS | 1 week | All treatments provided adequate pain reduction immediately, but laser treatments resulted in significantly greater reductions in pain intensity. |
| 3 | Lee et al (2015), Korea | 102 patients |
Positive control: strontium chloride dentifrice (SC) 20% nano-carbonate apatite (n-CAP) Er,Cr:YSGG laser |
Tactile evaporative |
VAS ABS |
2 weeks | In spite of DH reduction in both treatment groups, laser had a superior desensitizing effect at the initial stage, whereas the n-CAP maintained its effect for a relatively longer time. | |
| 4 | Bal et al (2015), Turkey |
21 patients (156 teeth) |
Placebo Low-level laser (LLL) (685 nm diode laser, 25 mW, 100 s) Desensitizing paste (DP) 8% arginine-calcium carbonate Laser followed by DP (LLL+ DP) DP followed by laser (DP+ LLL) |
1 | Evaporative | VAS | 90 days | The application of either LLL or DP was effective in decreasing DH. However, their combined use did not improve the efficacy. |
| 5 | Suri et al (2016), India | 30 patients (20 teeth) |
5% NaF Diode laser (980 nm GaAlAs) Group I + group II Placebo |
1 |
Tactile evaporative |
VAS | 2 months |
In spite of DH reduction in all groups, 5% NaF varnish with DL showed the best results (P<0.001). G3>G2>G1 |
| 6 | Dantas et al (2016), Brazil | 86 teeth |
Fluoride varnish Diode laser (GaAlAs laser at a 4 J/cm2 dose) |
4 |
Tactile thermal |
VAS | 72 hours | In spite of DH reduction in both groups at last, the short term tx with Fluoride was more effective (P<0.001). |
| 7 | Yaghini et al (2015), Iran | 40 patients |
Laser toothbrush Non-laser toothbrush |
4 | Thermal | VAS | 2 months | In spite of DH reduction in both groups, laser toothbrush was more effective (P <0.05). |
| 8 | Moosavi et al (2015), Iran |
31 patients (62 teeth) |
Low-power red laser (630 nm, 28 mW, continuous wave, 60 s, 1.68 J) before resin composite restoration Placebo + resin composite restoration |
1 | Thermal | VAS | 30 days | Significantly greater DH reduction (P <0.05) in the laser than the placebo group was observed suggesting LLLT a suitable approach in class V restoration. |
| 9 | Lopes et al (2015), Brazil | 27 patients (55 teeth) |
Gluma Infrared Low-power laser (30 mW, 10 J/cm(2), 4 points, 9 s per point, 810 nm) Infrared Low-power laser (100 mW, 90 J/cm(2), 2 points, 11 s per point, 810 nm) Group I+ group II Group I + group III |
1 3 3 3 3 |
Evaporative tactile |
VAS | 2 months | All groups showed a reduction in DH (P<0.001). Gluma presented immediate effects. The combination of protocols is an interesting alternative in the treatment of cervical dentin hypersensitivity. |
| 10 | Yilmaz & Bayindir. (2014), Turkey |
20 patients (60 teeth) |
Er,Cr:YSGG laser at 0·25 W Er,Cr:YSGG laser at 0.5 W Placebo |
1 | Evaporative | VAS | Immediate | Both laser groups were effective for the tx of FH (P<0.001) according to VAS scores and tubuli occlusion in SEM; however, 0.5 W laser irradiation showed best results. |
| 11 | Ko et al (2014), South Korea | 96 patients |
635 nm per 6 mW laser-emitting toothbrush Placebo: 635 nm per 12·9 µW light-emitting diode (LED) toothbrush |
84 (3 times a day for 4 weeks) |
Evaporative | VAS | 4 weeks | In spite of DH reduction in both groups (P<0.05), this decrease was significantly greater in the test group with no noticeable side effects. |
| 12 | Hashim et al (2014), Sudan |
5 patients (14 teeth) |
Diode laser (810 nm) with exposure duration of 30 s Diode laser (810 nm) with exposure duration of 1 min |
2 | Tactile | VAS | 7 days | Diode laser was effective for the reduction of dentine hypersensitivity (P<0.001). |
| 13 | De Almeida Farhat et al (2014), Brazil | 16 patients |
LED LED-laser (300 mW/cm2) |
2 | _ | VRS | 6 months | LED-laser treatment was not able to prevent or reduce the sensitivity of teeth (P>0.05) and did not improve the efficacy of bleaching. |
| 14 | Raichur et al (2013), India | 45 patients |
Diode laser 0.4% stannous fluoride gel 5% potassium nitrate gel |
Evaporative | 6 months | All groups showed a reduction in DH (P= 0.0020). DL was not only the most effective, but also brought about improved immediate relief. | ||
| 15 | Lund et al (2013), Brazil |
13 patients (117 teeth) |
Placebo: carbomer 940 gel 2% sodium fluoride gel Low-level infrared diode laser |
4 4 3 |
Evaporative | VAS | 90 days | All groups were able to reduce DH (P<0.001), including placebo group, with no difference among them. |
| 16 | Lopes & Aranha (2013), Brazil |
24 patients (33 teeth) |
Gluma Nd:YAG Laser 1.5 W, 10 Hz, and 100 mJ, approximately 85 J/cm(2), 60 s Group I + group II |
1 |
Tactile Evaporative Thermal |
VAS | 6 months | All protocols were effective in reducing DH after 6 months (P<0.001); however, the association of Nd:YAG and Gluma Desensitizer is an effective treatment strategy that has immediate and long-lasting effects. |
| 17 | Flecha et al (2013), Brazil |
62 patients (434 teeth) |
(GaAlAs) infrared diode laser (795 nm,120 mW, 2.88 J/cm2, 8 s) Cyanoacrylate |
3 | Tactile | NRS | 180 days | Cyanoacrylate is as effective as low-intensity laser in reducing DH. In addition, it is a more accessible and low-cost procedure and can be safely used in the treatment of DH. |
| 18 | Femiano et al (2013), Italy |
24 patients (262 teeth) |
NaF Diode laser (808 nm-35 W) Group II + Group III Gluma desensitizer |
3 | Thermal | VAS | 6 months |
In spite of DH improvement in all groups, diode laser in association with NaF effectively reduced DH with a more immediate relief and longer lasting (P<0.001). |
| 19 | Mogharehabed et al (2012), Iran |
9 patients (60 teeth) |
Placebo 5% sodium fluoride varnish Nd: YAG laser (1 W, 20 Hz, 120 s) Group II + group III |
1 |
Evaporative Thermal |
VAS | 2 weeks | The use of 5% sodium fluoride varnish and laser for treatment of DH is accompanied by a placebo effect. The association of NaF and laser showed the best improvements. |
| 20 | Ehlers et al (2012), Germany | 22 patients |
Glutaraldehyde-based desensitizing system Er:YAG laser |
Evaporative | VAS | 6 months | Both laser and glutaraldehyde groups showed an effective and equal reduction of cervical dentin hypersensitivity (P<0.001). | |
| 21 | de Almeida et al(2012), Brazil | 40 patients |
Home bleaching with 10% carbamide peroxide, 4 h/d 35% hydrogen peroxide, 10 minutes Quartz−tungsten−halogen light irradiation, 10 min LED/laser light irradiation, 10 min |
3 weeks 3 sessions 3 sessions 3 sessions |
_ |
Analog scale (0-10) |
180 days | Although all groups led to tooth sensitivity, light irradiated techniques showed more sensitivity in terms of both duration and intensity. |
| 22 | Aranha & Eduardo Cde. (2012), Brazil | 28 patients |
Placebo Er:YAG laser (2 Hz/32.4 mJ/5.9 J/cm(2)) Er,Cr:YSGG laser treatment (0.25 W/4.4 J/cm(2)) Er,Cr:YSGG laser treatment (0.50 W/ 8.9 J/cm(2)) |
1 |
Evaporative Tactile |
VAS | 1 month | With the evaporative stimulus, group II was associated with the lowest level of pain. With the mechanical stimulus, group IV showed the most pronounced decrease in pain immediately after treatment; however, after 4 weeks, pain levels had increased. |
| 23 | Yilmaz et al (2011), Turkey |
51 patient (174 teeth) |
Diode laser (GaAlAs laser at 8.5 J/cm2, 60 s) Er,Cr:YSGG laser (0.25 W, 20 Hz, 0% water and 10% air, 30 s) No treatment |
1 | Evaporative | VAS | 3 months | Compared to the control group, both Er,Cr:YSGG and GaAlAs lasers were effective in DH reduction immediately after the treatment (P <0.05) with no significant difference (P < 0.05). |
| 24 | Yilmaz et al (2011), Turkey |
48 patients (244 teeth) |
GaAlAs laser (810 nm, 500 mW, 60 s, 8.5 J/cm(2)) Placebo laser NaF varnish Placebo NaF varnish |
1 | Evaporative | VAS | 6 months | GaAlAs laser and NaF varnish treatments resulted in a significant reduction in the VAS scores immediately after treatments that were maintained throughout the study when compared to the baseline and placebo treatments. |
| 25 | Yilmaz et al (2011), Turkey |
42 patients (146 teeth) |
Er,Cr:YSGG laser (0.25W, 20 kHz, 30 s) Placebo |
1 | Evaporative | VAS + plaque index | 3 months | Er,Cr:YSGG laser had a significantly higher desensitizing effect compared with the placebo immediately after treatment (P <0.05). |
| 26 | Orhan et al (2011), Turkey |
16 patients 64 teeth |
Glutaraldehyde containing dentin desensitizer Low-level Diode laser (25-mW, 655 nm, 4 J/cm(2), 160 s) Distilled water Placebo laser |
1 6 1 6 |
Thermal evaporative |
VAS | 7 days | Pain scores of placebo groups were significantly higher than those of the desensitizer's and diode lasers (P < 0.05). Significant DH reduction was observed in 7 days with the use of the desensitizer and low-level laser therapy with no statistically significant difference (P > 0.05). |
| 27 | Kossatz et al (2011), Brazil | 30 patients |
Light-activated (LA) (LEDs with wavelength of 470 nm and three infrared Laser diodes with 830 nm and light intensity of 200 mW/cm, 1 min for 3 times) Non-activated |
2 | _ | 0-4 scale | 48 hours | The intensity of sensitivity was similar for both groups immediately after bleaching but significantly higher for the LA group 24 hours after each bleaching session (P=0.001). |
| 28 | Pesevska et al (2010), Macedonia | (30 teeth) |
Low-level diode laser (630–670 nm; 100 mW/cm2, 20 s) Topical Fluoride Varnish (Fluor Protector) |
3 | _ | VRS | 5 days | DH reduction by Laser was superior to Fluoride Varnish. Complete resolution of pain was achieved in 26.67% of group I, compared to 0 % in group II after the second visit, and 86.67% in group I compared to 26.67% in group II after the third visit. |
| 29 | Gurgan et al (2010), Turkey | 40 patients |
Bleaching twice without light activation Bleaching with a diode laser (810 nm, 10 W) activation for 3 times Bleaching treatment with a plasma arc lamp (400-490 nm, 2800 mV/cm(2)) for 3 times Bleaching twice with a light emitting diode (LED) lamp (400–500 nm) |
1 | _ | VAS | Immediate | Group II showed significantly lower tooth and gingival sensitivity scores than did the other groups (P<0.001). |
| 30 | Genovesi et al (2010), Italy | 15 patients |
Er:YAG (2940 nm) & CO2 lasers (10600 nm) + fluoride gel Placebo Er:YAG & CO2 lasers Fluoride gel + Placebo |
1 | Evaporative | VAS | Immediate | There were statistically significant differences between groups I and II. There were no statistically significant differences between groups III and IV. Er:Yag and CO2 lasers together with fluoride gel are useful in the treatment of dentine hypersensitivity. |
| 31 | Dilsiz et al (2010), turkey |
13 patients (52 teeth) |
GaAIAs Diode laser (100mw, 25 s, 808 nm) + desensitizer toothpaste Desensitizer toothpaste |
3 | Evaporative | VAS | 60 days | GaAIAs Diode laser plus desensitizer toothpaste group showed a higher degree of desensitization in teeth than did the control group (P<0.001). |
| 32 | Dilsiz et al (2010), turkey |
24 patients (96 teeth) |
Er:YAG laser (2,940 nm, 60 mJ/pulse, 2 Hz, 20 s) Nd:YAG laser (1,064 nm, 100 mJ/pulse, 15 Hz, 100 s) Diode laser (808 nm, 100 mW, 20 s) Placebo |
3 | Evaporative | VAS | 60 days | Significant reduction of DH occurred at all times for all groups. Nd:YAG laser was proved more effective in treatment of DH than the Er:YAG and diode lasers especially in 3-months results (P<0.001). |
| 33 | Sicilia et al (2009), Spain | 45 patients |
Diode laser (810 nm) + placebo gel Placebo laser + 10% potassium nitrate bio adhesive gel Placebo laser + placebo gel |
1 | Evaporative | VRS | 60 days | The DL and NK10% gel were proven effective in the treatment of DH. DL has shown efficacy in rapid and long-lasting DH reduction compared with placebo laser in periodontal patients. |
| 34 | Kara & Orbak. (2009), Turkey | 20 patients |
Nd:YAG laser (100 mJ, 20 Hz) Fluoride varnish |
1 | Evaporative | VAS | 4 weeks | Laser treatment resulted in significant improvements of discomfort immediately after treatment and after 1 week (P<0.001). However, the VAS scores at the 4-week examination were significantly lower in the fluoride group compared with those in the laser group (P<0.05). |
| 35 | Ipci et al (2009), Turkey |
50 patients (420 teeth) |
2% NaF CO(2) laser (1 W, 10 s) Er:YAG laser (30 Hz, 60 mJ,10 s) Group I + group II Group I + group III |
1 |
Thermal Evaporative |
VRS | 6 months | VRS scores were significantly lower for the other four treatments than for NaF gel alone (P +/- 0.001). No superiority was found for desensitization among the CO(2), Er:YAG, CO(2) + NaF, and Er:YAG + NaF groups. |
| 36 | Aranha et al (2009), Brazil | (101 teeth) |
Glumma Desensitizer Seal & Protect (SP) Oxa-gel (OG) Fluoride (F) Low intensity laser- LILT (660 nm/3.8 J/cm2/15 mW) |
1 1 1 1 3 |
Thermal Evaporative |
VAS | 6 months | OG and LILT showed significantly higher sensitivity immediately compared to Gluma Desensitizer and SP (P=0.0165). However, after 6 months, all therapies showed lower sensitivity compared with baseline presenting no statistically significant differences. |
| 37 | Tengrungsun & Sangkla. (2008), Thailand |
70 patients (140 teeth) |
GaAlAs laser (30 mW, 1 min) Dentin bonding agent |
1 | Tactile, thermal |
(0-4 degree scale) (Uchida criteria) |
30 days | A significant DH reduction after both treatments at all times was observed (P< 0.05). DH reduction by dentin bonding agent was significantly superior to GaAlAs laser (P< 0.05). |
| 38 | Marson et al (2008), Brazil | 40 patients |
35% Hydrogen Peroxide (HP) 35% HP + Halogen Curing Light XL 3000 (3M/ESPE) 35% HP + Demetron LED (Kerr) 35% HP + LED/LASER (Bio-art) |
2 | _ | VRS | 6 months | The recorded tooth sensitivity was similar in the number of patients and intensity. Tooth sensitivity occurred immediately following bleaching, but a higher degree of sensitivity was recorded after the second bleaching session, independent of the group evaluated. |
| 39 | Birang et al (2007), Iran |
9 patients (63 teeth) |
Nd:YAG laser (1 W, 15 Hz, 60 s, 2 times) Er:YAG laser (100 mJ, 3 Hz, 60 s, 2 times) Placebo |
1 | Tactile | VAS | 6 months | Both lasers, in spite of a placebo effect at short time, were so effective to decrease DH. Nd:YAG laser was more effective than Er:YAG laser in reduction of patients’ pain (P<0.0005). |
Results and Discussion
The present systematic review attempted to analyze all of the randomized clinical trials and comparative works to evaluate the effectiveness of laser therapy in prevention and treatment of dentine sensitivity. After final appraisals, 39 studies were involved for the final analysis (Table 1).
Previous researches evaluating the desensitizing effect of lasers have used different approaches which makes it difficult to compare their effectiveness.
In this systematic review, studies were divided into four groups; each group consists of those that:
Group 1: investigated laser application as a preventive procedure.
Group 2: compared laser with placebo.
Group 3: compared laser with desensitizing agents.
Group 4: examined different types of lasers.
In group 1, the preventive effect of laser therapy was assessed.21,22,24,25
The study by Pesevska et al21 compared the effect of low-level laser and topical fluoride treatment on DH following scaling and root planing. It was concluded that the reduction of DH by laser was superior to fluoride varnish. Therefore, laser can be successfully used for treatment of DH following scaling and root planing. Another study on different light-activated in-office bleaching systems concluded that bleaching with diode laser resulted in less tooth sensitivity than the other bleaching systems.22 Moosavi et al25 also evaluated the efficacy of low-level laser therapy on reducing DH after composite filling. Although both laser and placebo groups experienced a substantial improvement in pain reduction during the follow-up periods, VAS scores were significantly less in the laser group. However, the results obtained from some of the researches24,26-28 have discarded the potential protective role of lasers in DH prevention following bleaching as no significant decrease in tooth sensitivity has been shown after LED/laser treatment.
Most of the researches were conducted on the evaluation of the therapeutic effect of lasers in tooth sensitivity. Among these studies, many reported that laser therapy alone or in combination with different modalities was significantly more effective than the placebo treatment.
In group 2, eight articles directly compared laser treatment with placebo28-35; 6 of which reported significant reduction in tooth hypersensitivity.
The effect of 30 seconds application of Er,Cr:YSGG on DH in one session was examined in a clinical trial by Yilmaz et al.29 The authors concluded that the laser irradiation provided a significantly higher desensitizing effect compared with the placebo, immediately after treatment. Ko et al30 tested the efficacy of a low-level laser-emitting toothbrush (635 nm, 55 seconds) on the management of DH. In this double blind randomized clinical trial, VAS was significantly decreased in laser group than LED group. It was concluded that the application of laser emitting toothbrush is a safe and effective treatment option for the management of DH.
In another randomized controlled double-blind split mouth clinical study,32 the desensitizing effects of Er,Cr:YSGG and GaAlAs lasers have been compared with placebo on DH. The authors concluded that both Er,Cr:YSGG and GaAlAs lasers were effective in the treatment of DH following a single application.
Yimaz et al33 also reported that the Er,Cr:YSGG laser is effective in the treatment of DH compared with the placebo treatment.
Another study that compared the dentin desensitizing effect of 3 type of lasers (diode, Nd:YAG and Er:YAG) with placebo on teeth with gingival recessions concluded that lasers can be used for DH reduction.34
The effect of low-level laser toothbrushes in reduction of dentin hypersensitivity was evaluated by Yaghini et al,36 and concluded that laser toothbrushes reduce dentin hypersensitivity more than conventional toothbrushes.
However, studies conducted by Aranha et al37 (compared the effect of different types of erbium laser with placebo) and Kossatz et al28 (examined diode laser against placebo) did not show any significant effective results. Therefore, lasers might have shown a placebo effect but mostly limited to a short time.
Group 3: Based on our review, most of the researchers studied the treatment effect of lasers versus desensitizer chemical agents.
Some trials reported that laser was more effective than chemical agents. Sicilia et al38 evaluated the immediate efficacy of diode laser (810 nm) and potassium nitrate bioadhesive gel (10%) in the reduction of DH. A significant immediate response was observed in the laser group. Kara et al39 compared the effects of the Nd:YAG laser and fluoride varnish on DH in a similar study, and concluded that Nd:YAG laser is a suitable treatment for immediate reduction of DH and leads to a better patient satisfaction. The same results were concluded by Lee et al on the immediate effect of Er,Cr:YSGG laser in DH reduction.40 Raichur et al41 also examined the efficacy of diode laser versus stannous fluoride and potassium nitrate gels in the treatment of DH. There was a statistically significant decrease in all groups but the greatest difference in the DH scores was reported in the laser group which showed immediate relief as compared to the other methods. In a study by Yilmaz et al,42 GaAlAs laser was found more effective, faster and more comfortable than the traditional DH treatment approach (NaF). This result is concurrent with Soares’ findings on the superior effects of Nd:YAG and GaAIAs laser in comparison to neutral fluoride gel.43 Pesevska et al21 reported that low-power laser treatment was more effective than topical fluoride for relieving dental hypersensitivity following scaling and root planning.
In most of the researches, the combination of laser and desensitizer agents was more effective44-50 for example, Suri et al44 compared the effectiveness of GaAlAs laser alone and combined with the NaF varnish in treatment of DH. Even though both of them showed significant reduction in DH, the combination of fluoride varnish with diode laser led to the best results.44 In another study, Genovesi et al45 also reported that there were no significant differences among Er:Yag and CO2 laser groups as well as the fluoride gel and placebo group. However, Er:YAG and CO2 lasers together with fluoride gel were proved to be useful in the treatment of dentine hypersensitivity. Ipci et al46 in a similar study concluded that lasers (CO2 and Er:YAG) in combination with NaF gel showed a better efficacy for DH relief compared to each treatment alone. A significant effect of combined desensitizer toothpaste and diode laser therapy was also shown in the treatment of DH in gingival recessions.47 In a similar work that assessed different treatment protocols of Nd:YAG Laser, Gluma et al showed that all of the protocols were effective in reducing DH; however, the dual application of laser and Gluma Desensitizer was an effective treatment which had immediate and long-lasting effects.48
Femiano et al49 also evaluated the desensitizing efficacy of sodium fluoride solution, diode laser, and their association together with a solution of hydroxylethylmethacrylate and glutaraldehyde (HEMA-G: Gluma desensitizer) in cervical dentin hypersensitivity. The best result was reported for the combined treatment. Mogharehabed et al50 reported that the application of sodium fluoride varnish and Nd:YAG for the treatment of dentin hypersensitivity is accompanied by a placebo effect; however, this positive effect was more noticeable for the combined group (fluoride-laser) compared to the other groups. In spite of preceding conclusions, Bal et al51 reported that the combination of low-level laser and arginine-calcium carbonate desensitizing paste did not improve the efficacy of DH reduction beyond what was attainable with either treatment alone.
In contrast, as few researches have shown, chemical agents were more effective than laser. Tengrungsun et al52 made a comparison between the efficacy of the GaAlAs laser and dentin bonding agent in DH treatment and reported that the dentin bonding agent had more desensitizing efficacy compared to the GaAlAs laser. Dantas et al53 also showed that a short time treatment with fluoride was more effective than GaAlAs laser for DH reduction. Lopes et al54 compared low-power laser, Gluma (as a desensitizing agent), and their combination effect on dentin hypersensitivity treatment. The authors concluded that all of the methods were efficient in reducing pain but Gluma showed immediate effects. In another study,55 the effectiveness of cyanoacrylate and low-power laser in the treatment of DH was evaluated. It was suggested that cyanoacrylate is as effective as laser in reducing DH. This is to say that cyanoacrylate is a more accessible and low-cost procedure and can be safely used in DH treatment.
It is worth to note that some researchers have shown multifaceted results. For instance, Aranha et al31 compared the effect of different desensitizers (Gluma, fluoride) with low-level laser on DH for a period of 6 months. They concluded that both therapies demonstrated lower VAS compared with the baseline. However, LLLT (GaAlAs) presented a gradual reduction in DH while Gluma showed immediate effect on hypersensitivity.
Lund et al,56 in their study assessing the effectiveness of sodium fluoride gel and diode laser (infrared) for dentin hypersensitivity, proposed that there was no difference among the groups. In a similar study, Ehlers et al57 reported that both Gluma and Er:YAG laser have shown an equal effective reduction of cervical DH. Orhan et al58 also suggested that low-level laser therapy and desensitizer application have presented similar reduction in moderate DH.
Group 4: The lasers used for dental treatment are usually divided into 2 groups: low- power lasers (He-Ne and GaAlAs lasers), and high-power lasers (Nd:YAG , Er:YAG, Er,Cr:YSGG and CO2 lasers). Different studies have assessed various types of lasers for DH treatment.
Aranha et al37 compared two types of high-power laser (Er:YAG and Er,Cr:YSGG lasers) on DH and concluded that although none of the lasers could eliminate pain completely, both lasers were suitable for the treatment of DH. Another work reported that no significant difference was found between Er,Cr:YSGG and GaAlAs laser at follow-up sessions although both were effective after single application.32 Comparison of the desensitizing effect of Er:YAG, Nd:YAG, and GaAlAs (diode) lasers on DH has shown that Nd:YAG laser is more effective than Er:YAG and diode laser.34 A similar research on the effect of Nd:YAG and Er:YAG lasers on teeth sensitization, concluded that Nd:YAG laser is more effective than Er:YAG laser.35 Another study also reported that both CO2 and Er:YAG lasers are effective in the management of DH.46 Ladalardo et al18 conducted a research on the effectiveness of 2 types of low-power lasers (660 nm wavelength red, and 830 nm wavelength infrared) on DH. Their results showed that the red diode laser was more effective than the infrared laser and most of the desensitizing effects were observed within 15 and 30 minutes after irradiation. Moosavi et al59 in contrast reported opposing assumption that infrared laser was significantly more effective.
With respect to the increasing prevalence of DH, a comprehensive survey on the modern therapeutic methods such as laser therapy was demanding. Despite various treatment modalities, few valid studies are available in this area. Diagnostic criteria are less reliable and mostly count on patients’ report. Also, the use of different types of lasers, different methods and wavelengths, and conflicting findings were the restricting factors in terms of reaching a decisive conclusion. Furthermore, a great variation in types of desensitizing agents, the sample size and the number of patients in each group, follow-up periods, and assessment protocols were also among the limitations of this systematic review.
With regard to the results of the present review, it seems that laser is useful not only for the treatment, but also as prevention of DH. Furthermore, based on the experimental studies, laser application leads to tubuli orifice occlusion and decreases the dentine hydraulic conductance but has no effect on the mineral composition. High-power lasers (Nd:YAG and Er:YAG lasers) result in the reduction of dentine permeability mostly by sealing opened tubules; however, low- power lasers (diode lasers) affect DH probably by decreasing the dentinal fluid flow.
Finally, laser treatment could reduce DH but its efficacy may be the same as desensitizing agents. Nevertheless, a few researchers dispute its beneficence as a result of placebo effect. Irrespective of the fact that laser has several advantages such as long-lasting analgesic effects and seems to be safe, due to its high cost, it is not considered as a first choice of treatment.
The results attained in the present study are in consistent with Lin et al’s meta-analysis,60 which suggested that lasers were significantly more effective than placebo in reducing DH. However, this study did not consider the different types of lasers. The present results are in contrast with the systematic review of Sgolastra et al20 conducted in 2011. This difference could be related to the very few numbers of studies evaluated in their study.
Conclusion
Although the results obtained from 39 studies appraised in this systematic review were conflicting, most of them verified the clinical efficacy of laser in prevention and treatment of DH symptoms. Some of the researches have reported no significant difference between laser and other desensitizing agents, and most of the studies proposed better results (both rapid and long lasting) in combined modalities. Moreover, it was concluded that among various types of lasers, the application of Nd:YAG laser has shown the best results in DH treatment.
Ethical Considerations
Not applicable.
Conflict of Interests
The authors declare no conflict of interest.
Please cite this article as follows: Rezazadeh F, Dehghanian P, Jafarpour D. Laser effects on the prevention and treatment of dentinal hypersensitivity: a systematic review. J Lasers Med Sci. 2019;10(1):1-11. doi:10.15171/jlms.2019.01.
References
- 1. Burket LW, Greenberg MS, Glick M. Burket’s Oral Medicine: Diagnosis & Treatment. BC Decker; 2003.
- 2.Brisman R. Gamma knife surgery with a dose of 75 to 768 Gray for trigeminal neuralgia. J Neurosurg. 2004;100(5):848–854. doi: 10.3171/jns.2004.100.5.0848. [DOI] [PubMed] [Google Scholar]
- 3.Gronseth G, Cruccu G, Alksne J. et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology. 2008;71(15):1183–1190. doi: 10.1212/01.wnl.0000326598.83183.04. [DOI] [PubMed] [Google Scholar]
- 4.Walker J. Relief from chronic pain by low power laser irradiation. Neurosci Lett. 1983;43(2-3):339–344. doi: 10.1016/0304-3940(83)90211-2. [DOI] [PubMed] [Google Scholar]
- 5.Cruccu G, Finnerup NB, Jensen TS. et al. Trigeminal neuralgia: New classification and diagnostic grading for practice and research. Neurology. 2016;87(2):220–228. doi: 10.1212/wnl.0000000000002840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Falaki F, Nejat AH, Dalirsani Z. The Effect of Low-level Laser Therapy on Trigeminal Neuralgia: A Review of Literature. J Dent Res Dent Clin Dent Prospects. 2014;8(1):1–5. doi: 10.5681/joddd.2014.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zakrzewska JM, Akram H. Neurosurgical interventions for the treatment of classical trigeminal neuralgia. Cochrane Database Syst Rev. 2011;(9):Cd007312. doi: 10.1002/14651858.CD007312.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montano N, Papacci F, Cioni B, Di Bonaventura R, Meglio M. What is the best treatment of drug-resistant trigeminal neuralgia in patients affected by multiple sclerosis? A literature analysis of surgical procedures. Clin Neurol Neurosurg. 2013;115(5):567–572. doi: 10.1016/j.clineuro.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet. 2009;374(9705):1897–1908. doi: 10.1016/s0140-6736(09)61522-1. [DOI] [PubMed] [Google Scholar]
- 10.Jiang JA, Chang WD, Wu JH, Lai PT, Lin HY. Low-level laser treatment relieves pain and neurological symptoms in patients with carpal tunnel syndrome. J Phys Ther Sci. 2011;23(4):661–665. doi: 10.1589/jpts.23.661. [DOI] [Google Scholar]
- 11.Konstantinovic LM, Cutovic MR, Milovanovic AN. et al. Low-level laser therapy for acute neck pain with radiculopathy: a double-blind placebo-controlled randomized study. Pain Med. 2010;11(8):1169–1178. doi: 10.1111/j.1526-4637.2010.00907.x. [DOI] [PubMed] [Google Scholar]
- 12.Asnaashari M, Moeini M. Effectiveness of lasers in the treatment of dentin hypersensitivity. J Lasers Med Sci. 2013;4(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Biagi R, Cossellu G, Sarcina M, Pizzamiglio IT, Farronato G. Laser-assisted treatment of dentinal hypersensitivity: a literature review. Ann Stomatol (Roma) 2015;6(3-4):75–80. doi: 10.11138/ads/2015.6.3.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kingsley JD, Demchak T, Mathis R. Low-level laser therapy as a treatment for chronic pain. Front Physiol. 2014;5:306. doi: 10.3389/fphys.2014.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alfredo PP, Bjordal JM, Dreyer SH. et al. Efficacy of low level laser therapy associated with exercises in knee osteoarthritis: a randomized double-blind study. Clin Rehabil. 2012;26(6):523–533. doi: 10.1177/0269215511425962. [DOI] [PubMed] [Google Scholar]
- 16.Jang H, Lee H. Meta-analysis of pain relief effects by laser irradiation on joint areas. Photomed Laser Surg. 2012;30(8):405–417. doi: 10.1089/pho.2012.3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bamise CT, Esan TA. Mechanisms and treatment approaches of dentine hypersensitivity: a literature review. Oral Health Prev Dent. 2011;9(4):353–367. [PubMed] [Google Scholar]
- 18.Dehghani Nazhvani A, Haddadi P, Badiee P, Malekhoseini SA, Jafarian H. Antifungal Effects of Common Mouthwashes on Candida Strains Colonized in the Oral Cavities of Liver Transplant Recipients in South Iran in 2014. Hepat Mon. 2016;16(1):e31245. doi: 10.5812/hepatmon.31245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Lasers for the treatment of dentin hypersensitivity: a meta-analysis. J Dent Res. 2013;92(6):492–499. doi: 10.1177/0022034513487212. [DOI] [PubMed] [Google Scholar]
- 20.Sgolastra F, Petrucci A, Gatto R, Monaco A. Effectiveness of laser in dentinal hypersensitivity treatment: a systematic review. J Endod. 2011;37(3):297–303. doi: 10.1016/j.joen.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 21.Pesevska S, Nakova M, Ivanovski K. et al. Dentinal hypersensitivity following scaling and root planing: comparison of low-level laser and topical fluoride treatment. Lasers Med Sci. 2010;25(5):647–650. doi: 10.1007/s10103-009-0685-0. [DOI] [PubMed] [Google Scholar]
- 22.Gurgan S, Cakir FY, Yazici E. Different light-activated in-office bleaching systems: a clinical evaluation. Lasers Med Sci. 2010;25(6):817–822. doi: 10.1007/s10103-009-0688-x. [DOI] [PubMed] [Google Scholar]
- 23.Bakry AS, Takahashi H, Otsuki M, Sadr A, Yamashita K, Tagami J. CO2 laser improves 45S5 bioglass interaction with dentin. J Dent Res. 2011;90(2):246–250. doi: 10.1177/0022034510387793. [DOI] [PubMed] [Google Scholar]
- 24.de Almeida LC, Costa CA, Riehl H, dos Santos PH, Sundfeld RH, Briso AL. Occurrence of sensitivity during at-home and in-office tooth bleaching therapies with or without use of light sources. Acta Odontol Latinoam. 2012;25(1):3–8. [PubMed] [Google Scholar]
- 25.Moosavi H, Maleknejad F, Sharifi M, Ahrari F. A randomized clinical trial of the effect of low-level laser therapy before composite placement on postoperative sensitivity in class V restorations. Lasers Med Sci. 2015;30(4):1245–1249. doi: 10.1007/s10103-014-1565-9. [DOI] [PubMed] [Google Scholar]
- 26.de Almeida Farhat PB, Santos FA, Gomes JC, Gomes OM. Evaluation of the efficacy of LED-laser treatment and control of tooth sensitivity during in-office bleaching procedures. Photomed Laser Surg. 2014;32(7):422–426. doi: 10.1089/pho.2014.3729. [DOI] [PubMed] [Google Scholar]
- 27.Marson FC, Sensi LG, Vieira LC, Araujo E. Clinical evaluation of in-office dental bleaching treatments with and without the use of light-activation sources. Oper Dent. 2008;33(1):15–22. doi: 10.2341/07-57. [DOI] [PubMed] [Google Scholar]
- 28.Kossatz S, Dalanhol AP, Cunha T, Loguercio A, Reis A. Effect of light activation on tooth sensitivity after in-office bleaching. Oper Dent. 2011;36(3):251–257. doi: 10.2341/10-289-c. [DOI] [PubMed] [Google Scholar]
- 29.Yilmaz HG, Bayindir H. Clinical and scanning electron microscopy evaluation of the Er,Cr:YSGG laser therapy for treating dentine hypersensitivity: short-term, randomised, controlled study. J Oral Rehabil. 2014;41(5):392–398. doi: 10.1111/joor.12156. [DOI] [PubMed] [Google Scholar]
- 30.Ko Y, Park J, Kim C, Park J, Baek SH, Kook YA. Treatment of dentin hypersensitivity with a low-level laser-emitting toothbrush: double-blind randomised clinical trial of efficacy and safety. J Oral Rehabil. 2014;41(7):523–531. doi: 10.1111/joor.12170. [DOI] [PubMed] [Google Scholar]
- 31.Aranha AC, Pimenta LA, Marchi GM. Clinical evaluation of desensitizing treatments for cervical dentin hypersensitivity. Braz Oral Res. 2009;23(3):333–339. doi: 10.1590/s1806-83242009000300018. [DOI] [PubMed] [Google Scholar]
- 32.Yilmaz HG, Kurtulmus-Yilmaz S, Cengiz E, Bayindir H, Aykac Y. Clinical evaluation of Er,Cr:YSGG and GaAlAs laser therapy for treating dentine hypersensitivity: A randomized controlled clinical trial. J Dent. 2011;39(3):249–254. doi: 10.1016/j.jdent.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Yilmaz HG, Cengiz E, Kurtulmus-Yilmaz S, Leblebicioglu B. Effectiveness of Er,Cr:YSGG laser on dentine hypersensitivity: a controlled clinical trial. J Clin Periodontol. 2011;38(4):341–346. doi: 10.1111/j.1600-051X.2010.01694.x. [DOI] [PubMed] [Google Scholar]
- 34.Dilsiz A, Aydin T, Canakci V, Gungormus M. Clinical evaluation of Er:YAG, Nd:YAG, and diode laser therapy for desensitization of teeth with gingival recession. Photomed Laser Surg. 2010;28 Suppl 2:S11–17. doi: 10.1089/pho.2009.2593. [DOI] [PubMed] [Google Scholar]
- 35.Birang R, Poursamimi J, Gutknecht N, Lampert F, Mir M. Comparative evaluation of the effects of Nd:YAG and Er:YAG laser in dentin hypersensitivity treatment. Lasers Med Sci. 2007;22(1):21–24. doi: 10.1007/s10103-006-0412-z. [DOI] [PubMed] [Google Scholar]
- 36.Yaghini J, Mogharehabed A, Safavi N, Mohamadi M, Ashtiju F. Evaluation of the effect of low level laser therapy toothbrush in treatment of dentin hypersensitivity. J Lasers Med Sci. 2015;6(2):85–91. [PMC free article] [PubMed] [Google Scholar]
- 37.Aranha AC, Eduardo Cde P. Effects of Er:YAG and Er,Cr:YSGG lasers on dentine hypersensitivity Short-term clinical evaluation. Lasers Med Sci. 2012;27(4):813–818. doi: 10.1007/s10103-011-0988-9. [DOI] [PubMed] [Google Scholar]
- 38.Sicilia A, Cuesta-Frechoso S, Suarez A, Angulo J, Pordomingo A, De Juan P. Immediate efficacy of diode laser application in the treatment of dentine hypersensitivity in periodontal maintenance patients: a randomized clinical trial. J Clin Periodontol. 2009;36(8):650–660. doi: 10.1111/j.1600-051X.2009.01433.x. [DOI] [PubMed] [Google Scholar]
- 39.Kara C, Orbak R. Comparative evaluation of Nd:YAG laser and fluoride varnish for the treatment of dentinal hypersensitivity. J Endod. 2009;35(7):971–974. doi: 10.1016/j.joen.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 40.Lee SY, Jung HI, Jung BY, Cho YS, Kwon HK, Kim BI. Desensitizing efficacy of nano-carbonate apatite dentifrice and Er,Cr:YSGG laser: a randomized clinical trial. Photomed Laser Surg. 2015;33(1):9–14. doi: 10.1089/pho.2014.3787. [DOI] [PubMed] [Google Scholar]
- 41.Raichur PS, Setty SB, Thakur SL. Comparative evaluation of diode laser, stannous fluoride gel, and potassium nitrate gel in the treatment of dentinal hypersensitivity. Gen Dent. 2013;61(3):66–71. [PubMed] [Google Scholar]
- 42.Yilmaz HG, Kurtulmus-Yilmaz S, Cengiz E. Long-term effect of diode laser irradiation compared to sodium fluoride varnish in the treatment of dentine hypersensitivity in periodontal maintenance patients: a randomized controlled clinical study. Photomed Laser Surg. 2011;29(11):721–725. doi: 10.1089/pho.2010.2974. [DOI] [PubMed] [Google Scholar]
- 43.Soares ML, Porciuncula GB, Lucena MI, Gueiros LA, Leao JC, Carvalho AA. Efficacy of Nd:YAG and GaAlAs lasers in comparison to 2% fluoride gel for the treatment of dentinal hypersensitivity. Gen Dent. 2016;64(6):66–70. [PubMed] [Google Scholar]
- 44.Suri I, Singh P, Shakir QJ, Shetty A, Bapat R, Thakur R. A comparative evaluation to assess the efficacy of 5% sodium fluoride varnish and diode laser and their combined application in the treatment of dentin hypersensitivity. J Indian Soc Periodontol. 2016;20(3):307–314. doi: 10.4103/0972-124x.181243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Genovesi A, Sachero E, Lorenzi C. The dental hygienist’s role in the laser treatment of the dentine hypersensitivity. Prev Assist Dent. 2010;36(1):32–35. doi: 10.1016/j.pad.2009.11.001. [DOI] [Google Scholar]
- 46.Ipci SD, Cakar G, Kuru B, Yilmaz S. Clinical evaluation of lasers and sodium fluoride gel in the treatment of dentine hypersensitivity. Photomed Laser Surg. 2009;27(1):85–91. doi: 10.1089/pho.2008.2263. [DOI] [PubMed] [Google Scholar]
- 47.Dilsiz A, Aydin T, Emrem G. Effects of the combined desensitizing dentifrice and diode laser therapy in the treatment of desensitization of teeth with gingival recession. Photomed Laser Surg. 2010;28 Suppl 2:S69–74. doi: 10.1089/pho.2009.2640. [DOI] [PubMed] [Google Scholar]
- 48.Lopes AO, Aranha AC. Comparative evaluation of the effects of Nd:YAG laser and a desensitizer agent on the treatment of dentin hypersensitivity: a clinical study. Photomed Laser Surg. 2013;31(3):132–138. doi: 10.1089/pho.2012.3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Femiano F, Femiano R, Lanza A, Festa MV, Rullo R, Perillo L. Efficacy of diode laser in association to sodium fluoride vs Gluma desensitizer on treatment of cervical dentin hypersensitivity A double blind controlled trial. Am J Dent. 2013;26(4):214–218. [PubMed] [Google Scholar]
- 50.Mogharehabed A, Khademi H, Abdi Zamharir Z, Ayoub Bouraima S, Yaghini J, Poormoradi B. Comparative evaluation of the effects of 5% sodium fluoride varnish and neodymium-doped yttrium aluminium garnet (Nd:YAG) laser and their combined application on dentin hypersensitivity treatment. J Lasers Med Sci. 2012;3(3):109–115. doi: 10.22037/2010.v3i3.3446. [DOI] [Google Scholar]
- 51.Bal MV, Keskiner I, Sezer U, Acikel C, Saygun I. Comparison of low level laser and arginine-calcium carbonate alone or combination in the treatment of dentin hypersensitivity: a randomized split-mouth clinical study. Photomed Laser Surg. 2015;33(4):200–205. doi: 10.1089/pho.2014.3873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tengrungsun T, Sangkla W. Comparative study in desensitizing efficacy using the GaAlAs laser and dentin bonding agent. J Dent. 2008;36(6):392–395. doi: 10.1016/j.jdent.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 53.Dantas EM, Amorim FK, Nobrega FJ, Dantas PM, Vasconcelos RG, Queiroz LM. Clinical Efficacy of Fluoride Varnish and Low-Level Laser Radiation in Treating Dentin Hypersensitivity. Braz Dent J. 2016;27(1):79–82. doi: 10.1590/0103-6440201602422. [DOI] [PubMed] [Google Scholar]
- 54.Lopes AO, Eduardo Cde P, Aranha AC. Clinical evaluation of low-power laser and a desensitizing agent on dentin hypersensitivity. Lasers Med Sci. 2015;30(2):823–829. doi: 10.1007/s10103-013-1441-z. [DOI] [PubMed] [Google Scholar]
- 55.Flecha OD, Azevedo CG, Matos FR. et al. Cyanoacrylate versus laser in the treatment of dentin hypersensitivity: a controlled, randomized, double-masked and non-inferiority clinical trial. J Periodontol. 2013;84(3):287–294. doi: 10.1902/jop.2012.120165. [DOI] [PubMed] [Google Scholar]
- 56.Lund RG, Silva AF, Piva E, Da Rosa WL, Heckmann SS, Demarco FF. Clinical evaluation of two desensitizing treatments in southern Brazil: A 3-month follow-up. Acta Odontol Scand. 2013;71(6):1469–1474. doi: 10.3109/00016357.2013.770919. [DOI] [PubMed] [Google Scholar]
- 57.Ehlers V, Ernst CP, Reich M, Kammerer P, Willershausen B. Clinical comparison of gluma and Er:YAG laser treatment of cervically exposed hypersensitive dentin. Am J Dent. 2012;25(3):131–135. [PubMed] [Google Scholar]
- 58.Orhan K, Aksoy U, Can-Karabulut DC, Kalender A. Low-level laser therapy of dentin hypersensitivity: a short-term clinical trial. Lasers Med Sci. 2011;26(5):591–598. doi: 10.1007/s10103-010-0794-9. [DOI] [PubMed] [Google Scholar]
- 59.Moosavi H, Arjmand N, Ahrari F, Zakeri M, Maleknejad F. Effect of low-level laser therapy on tooth sensitivity induced by in-office bleaching. Lasers Med Sci. 2016;31(4):713–719. doi: 10.1007/s10103-016-1913-z. [DOI] [PubMed] [Google Scholar]
- 60.Lin PY, Cheng YW, Chu CY, Chien KL, Lin CP, Tu YK. In-office treatment for dentin hypersensitivity: a systematic review and network meta-analysis. J Clin Periodontol. 2013;40(1):53–64. doi: 10.1111/jcpe.12011. [DOI] [PubMed] [Google Scholar]


