Abstract
Background:
Fecal impaction (FI) is defined by a large mass of stool in the rectum and/or colon that is unable to be evacuated. No literature to date details demographics and outcomes in a sizeable sample of FI patients in the United States.
Aims:
The present study aims to develop knowledge of FI by reporting descriptive measures and outcomes of patients presenting to a U.S. emergency department (ED) with FI.
Methods:
Medical charts coded with FI at Beth Israel Deaconess Medical Center from 2016 or 2017 were identified retrospectively. Patients diagnosed with FI in the ED or subsequent to direct hospital admission from the ED were included. Patient-specific demographics, visit-specific details, medical and medication histories, and hospital treatment and outcome measures were included in a database and analyzed.
Results:
32 patients (mean age of 72.9 years, 62.5% female) had a total of 42 ED visits with FI. Patients had an average of 8.7 diagnoses and 11.2 medications listed in their charts. 54.8% of patients were taking at least one commonly prescribed constipating medication. The median total length of stay for admitted patients was 3 days, with nearly 90% of the ED visits with FI requiring hospital admission. 40.6% of patients experienced serious FI-related morbidities, and 21.9% of patients with FI died in the hospital.
Conclusion:
Patients presenting with FI had high risk of morbidity and mortality, complex medical histories, and large numbers of active treatment regimens. Patients with FI should receive immediate treatment and close monitoring for morbidities and complications.
Keywords: fecal impaction, constipation, morbidity, mortality, opioids, epidemiology
INTRODUCTION
Fecal impaction (FI) results from chronic or severe constipation and is defined by a large mass of stool in the rectum and/or colon which is unable to be evacuated (1,2). FIs are most common in the elderly population and become more prevalent with increasing age (3,4). In 2011, there were over 42,000 emergency department (ED) visits for FI, with 85+ and 65–84 year age groups having the highest and second highest visit rates, respectively, relative to all ED visits in each age group (5). FIs are particularly prevalent in the institutionalized elderly; prior studies report that up to half of institutionalized elderly experience FI each year (6–8). Patients with neurogenic bowel may also be at risk of developing FIs, along with patients who take constipating medications (3,9).
FIs often presents with symptoms such as abdominal pain, constipation, rectal discomfort, nausea, and vomiting, among other symptoms (3,10,11). FIs can be accompanied by more serious morbidities, including intestinal perforation, intestinal obstruction, stercoral colitis or ulceration, and megarectum or megacolon (3,4,10,12,13). A high rate of mortality has been linked with FI, often due to the complications occurring in elderly and chronically ill patients (11). A systematic review of FI reported that death occurred secondary to FI complications in 29% of cases (10).
Treatment for FI includes use of digital disimpaction, enemas, suppositories, and oral laxative regimens (3,11). For at-risk or refractory patients, preventative strategies like use of stool softeners or reduction in use of constipating medications are known to reduce FI incidence (11). Metabolic and endocrine screening is also suggested for at-risk patients, as endocrine and metabolic disorders can underlie FI development (14). Still, systematic research regarding management of FI is lacking.
While numerous clinical FI case reports have been published, no literature to date ties detailed demographic and medication profiles to sequelae and treatment outcomes in a sizeable sample of FI patients in the United States. To our knowledge, just one retrospective study from Lebanon reports aggregate statistics of treatments and demographics of FI patients (15), and one recent review details complications of FI by summarizing results from a number of case reports (10). However, because the case reports reviewed in the latter study typically included a single or small number of noteworthy cases, it is unclear whether the aggregate statistics translate to the clinical setting in U.S. hospitals.
The present study aims to develop knowledge of FI by reporting descriptive measures and outcomes of consecutive patients in the U.S. presenting to the ED with FI. Classifying FI patient demographics and treatment outcomes may help to improve management practices and reduce morbidity and mortality associated with FI.
METHODS
Medical charts coded with the ICD 10 code for FI (K56.41) in 2016 or 2017 were identified retrospectively using the ClinicalQuery2 tool in the Beth Israel Deaconess Medical Center Online Medical Records system. An ‘ED visit with FI’ was defined as a continuous visit in which a patient presented to the ED with FI and was diagnosed with FI either in the ED or during an inpatient stay subsequent to direct hospital admission from the ED. Charts were carefully reviewed to determine if an ED visit with FI occurred, and only visits which matched these criteria were evaluated further. Common reasons for exclusion included FI diagnosis in the outpatient setting and miscoded diagnosis. Instances of FI that developed in an inpatient setting subsequent to admission through the ED were also excluded.
Medical charts were reviewed by T.S. and T.P., and any inconsistencies were arbitrated by P.S. For each ED visit with FI, patient-specific demographics and medical histories were recorded, including age, gender, race, residence (institutionalized or non-institutionalized), ambulatory status (walking or wheelchair-bound), preexisting medical conditions, and use of laxatives (including bisacodyl, senna, milk of magnesia, magnesium oxide, docusate sodium, fleet enema, polyethylene glycol, lactulose, linaclotide, lubiprostone, and magnesium citrate) and constipating medications (opioids, anticholinergics, calcium-channel blockers, antidiarrheals, and iron). Medication information was obtained from preadmission lists or discharge paperwork, with over the counter and prescription medication being noted equally. Visit-specific details included date of ED visit; date of ED discharge or hospital admission; date of hospital discharge; time of FI diagnosis (in ED or as inpatient); reason(s) for ED visit; primary reason for hospital admission, if applicable; use of KUB, abdominal CT scan, or rectal exam in the ED; and use of follow-up KUB or abdominal CT scan. Hospital treatment and outcome measures included disimpaction method in the ED and/or hospital; use of opioids, antibiotics, or oral laxatives during a visit; discharge with oral laxatives or antibiotics; patient morbidities; and mortality.
Data were analyzed by determining the frequency of occurrence of a given factor for each categorical variable and by calculating the mean and standard error of the mean (SEM) for each discrete or continuous variable. Data related to any patient-specific demographic factors, outcomes, medications, or medical histories were evaluated once per patient, regardless of number of ED visits with FI. For patients with multiple ED visits with FI in 2016 and 2017, the first visit was included and subsequent visits were excluded when analyzing patient-specific measures. Data related to hospital-specific measures during the course of hospitalization were evaluated for all ED visits with FI, including all repeat visits.
RESULTS
Of the 53 patients identified in the BIDMC online medical record system with the ICD 10 code for FI in 2016 or 2017, 32 patients were confirmed upon detailed chart review to have ED visits with FI. These 32 patients had a total of 42 ED visits with FI (two patients had two ED visits with FI each; one patient had 9 ED visits with FI).
Patient Demographics and Medical Histories
The average age of patients presenting with FI was 72.9 years. The majority of patients were female (62.5%) and White (75.0%). On average, patients who presented with FI had 8.7 medical diagnoses listed in their medical chart. Of the patients whose records described residence, 46.7% were institutionalized. 42.1% of patients who had ambulatory status noted in their records were described as wheelchair-bound. 28.1% of patients had preexisting neurological disorders (stroke, Parkinson’s disease, multiple sclerosis, dementia, and diabetic neuropathy) (Table 1). Of the 16 patients presenting from non-institutional settings, 3 (18.8%) had neurological disorders, and 2 (20.0%) were wheelchair-bound (of the 10 which had documented ambulatory status). There were no patients who were both wheelchair-bound and had neurological disorders.
Table 1.
Demographic information for patients with ED visits with FI.
| All Patients | Admitted to Hospital | ||
|---|---|---|---|
| Survived | Expired | ||
| Mean age (years) | (n = 32) | (n = 21) | (n = 7) |
| 72.9 (Range = 40.8 – 91.6; SEM = 2.4) | 70.8 (Range = 40.8 – 87.4; SEM = 2.8) | 73.9 (Range = 54.0 – 90.1; SEM = 5.7) | |
| Gender | (n = 32) | (n = 21) | (n = 7) |
| Female | 20 (62.5%) | 12 (57.1%) | 6 (85.7%) |
| Male | 12 (37.5%) | 9 (42.9%) | 1 (14.3%) |
| Race | (n = 32) | (n = 21) | (n = 7) |
| White | 24 (75.0%) | 15 (71.4%) | 5 (71.4%) |
| Black/African American | 6 (18.8%) | 4 (19.0%) | 2 (28.6%) |
| Asian | 2 (6.3%) | 2 (9.5%) | 0 (0.0%) |
| Residence | (n = 30) | (n = 21) | (n = 7) |
| Non-institutionalized | 16 (53.3%) | 12 (57.1%) | 3 (42.9%) |
| Institutionalized | 14 (46.7%) | 9 (42.9%) | 4 (57.1%) |
| -Nursing home | 13 (43.3%) | 8 (38.1%) | 4 (57.1%) |
| -Hospice | 1 (3.3%) | 1 (4.8%) | 0 (0.0%) |
| Ambulatory status | (n = 19) | (n = 12) | (n = 5) |
| Wheelchair-bound | 8 (42.1%) | 4 (33.3%) | 3 (60.0%) |
| Ambulatory | 11 (57.9%) | 8 (66.6%) | 2 (40.0%) |
| Neurological status | (n = 32) | (n = 21) | (n = 7) |
| No neurological disorder | 23 (71.9%) | 12 (57.1%) | 7 (100.0%) |
| Peripheral or central neurological disorder | 9 (28.1%) | 9 (42.9%) | 0 (0.0%) |
| -Diabetic neuropathy | 3 (9.4%)* | 3 (14.3%)* | 0 (0.0%) |
| -Dementia | 2 (6.2%)* | 2 (9.5%)* | 0 (0.0%) |
| -Stroke | 2 (6.2%) | 2 (9.5%) | 0 (0.0%) |
| -Multiple sclerosis | 2 (6.2%) | 2 (9.5%) | 0 (0.0%) |
| -Parkinson’s | 1 (3.1%) | 1 (4.8%) | 0 (0.0%) |
| Mean number of medical diagnoses | (n = 32) | (n = 21) | (n = 7) |
| 8.7 (SEM = 0.7) | 8.9 (SEM = 0.9) | 9.0 (SEM = 1.9) | |
| Mean number of medications | (n = 31) | (n = 21) | (n = 7) |
| 11.2 (SEM = 1.3) | 11.7 (SEM = 1.7) | 8.9 (SEM = 1.9) | |
| Previous medications | (n = 31)+ | (n = 21)+ | (n = 7)+ |
| Laxatives | 13 (41.9%) | 11 (52.4%) | 2 (28.6%) |
| Opioids | 8 (25.8%) | 5 (23.8%) | 3 (42.9%) |
| Non-opioid constipating medications | 14 (45.2%) | 10 (47.6%) | 3 (42.9%) |
| -Calcium channel blockers | 7 (22.6%) | 4 (19.0%) | 2 (28.6%) |
| -Anticholinergics | 7 (22.6%) | 7 (33.3%) | 1 (14.3%) |
| -Iron | 4 (12.9%) | 3 (14.3%) | 0 (0.0%) |
One patient had both dementia and diabetic neuropathy.
Some patients took multiple medications within each class or took multiple classes of medications.
Prior to their ED visits with FI, patients took an average of 11.2 medications. 25.8% of patients were reportedly taking at least one type of opioid, and 45.2% were taking at least one type of commonly prescribed non-opioid constipating medication (calcium channel blockers, anticholinergic agents, and iron). Overall, 54.8% were on at least one commonly prescribed constipating drug. 41.9% were taking laxatives prior to their FI visits (Table 1). For those patients on laxative regimens, 2.9 laxatives (SEM = 0.5) were used per individual, on average.
ED Visits
Upon ED presentation, the three most frequent complaints among the 42 visits were abdominal pain (20 visits; 47.6%), constipation (19 visits; 45.2%), and altered mental status (9 visits; 21.4%). Other common symptoms upon presentation were nausea, vomiting, per-oral (PO) difficulty, rectal pain or bleeding, and diarrhea (Figure 1).
Figure 1. Common complaints upon ED presentation.
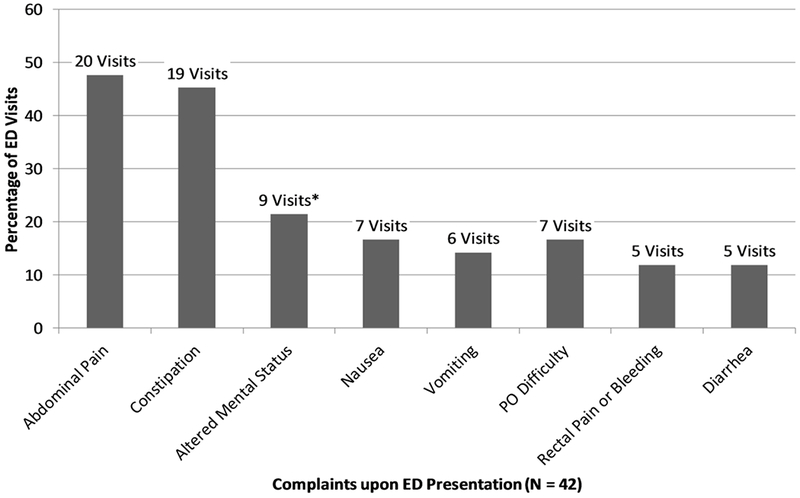
Bar graph displaying frequencies of commonly reported complaints upon ED presentation for all ED visits with FI. Multiple complaints were typically reported for each visit.
*Altered mental status resulted from respiratory complications (3 visits), lactic or metabolic acidosis (3 visits), urinary tract infection (UTI) or urosepsis (2 visits), and metabolic encephalopathy (1 visit)
FI was identified in 37 of 42 visits (88.1%) in the ED. FI was identified in the remaining 5 visits (11.9%) after hospital admission from the ED (Figure 2). In the ED, FIs were identified with abdominal CT scans in 29 patients (78.4%), KUBs in 3 patients (8.1%), and digital rectal exams in 5 patients (13.5%).
Figure 2. Efficacy of disimpaction in the ED.
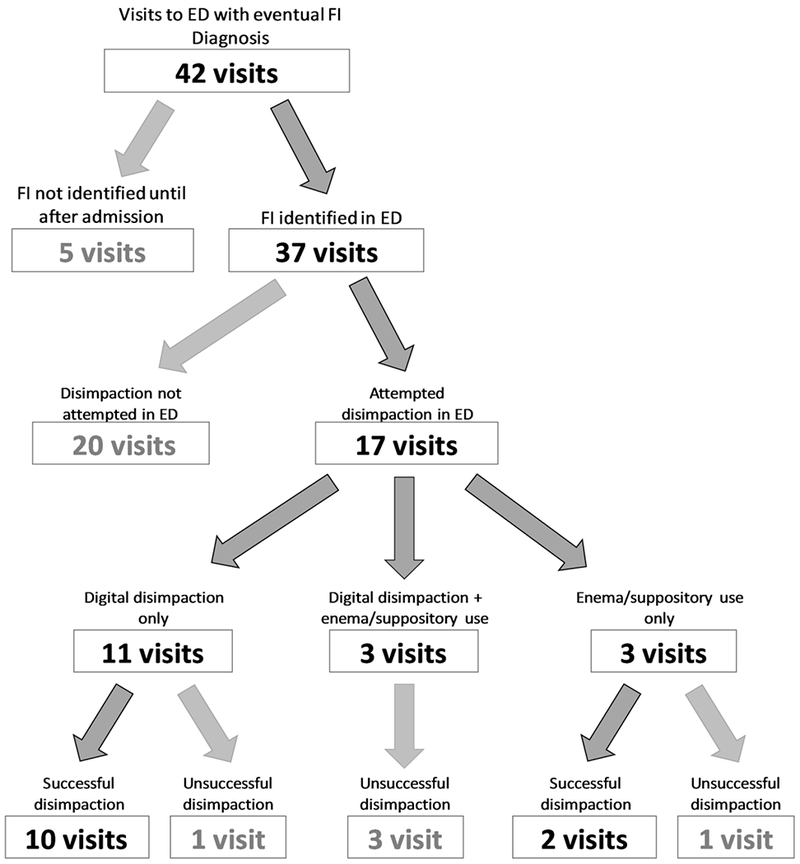
Flow chart of all ED visits with FI depicting whether or not patients were identified with FI in the ED, whether or not patients had disimpaction attempted in the ED, and whether or not patients were disimpacted successfully using digital maneuvers, enemas/suppositories, or both digital maneuvers and enemas/suppositories.
Disimpaction was attempted in the ED in 17 of the 37 visits (45.9%) in which FI was identified in the ED. 14 of the 17 attempts (82.4%) included digital maneuvers and three attempts (17.6%) exclusively used oral laxatives, enemas, and/or suppositories, without any attempted digital maneuvers. Only 12 out of the 37 visits (32.4%) that identified FI in the ED reported complete disimpaction of the stool burden in the ED (Figure 2).
Inpatient Stays
37 out of 42 ED visits (88.1%) with FI required hospital admission. The most frequent primary reasons for hospital admission were UTI (5 visits), FI (4 visits), constipation (3 visits), pneumonia (3 visits), and lactic acidosis (3 visits). For those patients who were admitted, inpatient stays lasted a median of 3 days (average: 6.4) prior to discharge (including death).
In the 5 visits in which FI was diagnosed during inpatient stay, FIs were identified with abdominal CTs (3 visits), KUBs (1 visit), or digital rectal exams (1 visit). Subsequent to diagnoses of FI, patients received follow-up KUBs in 14 of the 37 inpatient cases (37.8%) and follow-up abdominal CT scans in 8 cases (21.6%). During hospitalization, exclusive use of oral laxatives, enemas, and/or suppositories for disimpaction became much more common as the preferred disimpaction method, utilized in 16 of 27 recorded attempted disimpactions (59.3%). Digital maneuvers were utilized in just 11 of 27 attempted inpatient disimpactions (40.7%).
Overall, oral laxatives were given or continued in 32 of the 42 cases (76.2%) in the course of hospitalization (ED or inpatient). Antibiotics for GI symptoms were used in the course of hospitalization in 10 cases (23.8%), including treatment for suspected diverticulitis, colitis, and bowel perforation. Opioids were given or continued in 11 of the cases (26.2%).
Patient Outcomes
7 of the 32 patients (21.9%) with FI died while hospitalized. Two of these deaths were attributed directly to bowel-related complications, with the others due primarily to cardiorespiratory complications, multi-organ failure related to septic shock, and metastatic duodenal carcinoma. In total, 4 of the deaths were plausibly related to fecal impaction (Table 2). Additionally, one patient died 13 days after discharge due to esophageal cancer.
Table 2.
Causes of death for the 7 patients with ED visits with FI who died in the hospital.
| Gender | Age at visit | Reasons for admission | Description of cause of death | Length of stay prior to death |
|---|---|---|---|---|
| Female | 69 | Peritonitis, septic shock, febrile, lactic acidosis, and UTI | Ischemic small and large bowel with necrosis and resulting sepsis and multi-organ failure* | 2 |
| Female | 88 | Hypoxia, lethargy, and UTI | Sepsis (secondary to rectal ulcer, UTI, and possible aspiration pneumonia), respiratory failure, and heart failure* | 5 |
| Female | 54 | Lactic acidosis, sepsis, and failure to thrive | Metastatic duodenal carcinoma with resulting cholangitis and acute liver failure | 15 |
| Female | 71 | Distended colon, fecal impaction, hypokalemia, and abdominal pain | Pulseless electrical activity cardiac arrest | 2 |
| Female | 90 | Infectious diarrhea and sepsis | Mesenteric ischemia with necrosis of small bowel and right colon* | 6 |
| Male | 56 | Sepsis, tachycardia, respiratory distress, hyponatremia, metabolic acidosis, hypotension, anemia, and acute renal failure | Sepsis (secondary to skin and soft tissue infection and pyelonephritis) with resulting multi-organ failure* | 4 |
| Female | 87 | Acute hypercarbic respiratory failure, and possible pneumonia | Hypercarbic respiratory failure | 2 |
Cause of death plausibly related to/secondary to FI.
Italics indicates complications with possible etiologies secondary to fecal impaction.
Of the 7 patients with FI who died while hospitalized, 4 (57.1%) were given antibiotics for GI symptoms. After FI diagnosis, 5 (71.4%) had follow-up KUBs, and 3 (42.9%) had follow-up abdominal CT scans. 5 of the 7 (71.4%) were on common constipating medications, but only 2 (28.6%) were using laxatives. The median length of stay until death was 4 days.
13 of 32 patients (40.6%) had serious FI-related morbidities, defined as stercoral proctitis/colitis or bowel obstruction (Figure 3). 4 of the 32 patients (12.5%) were identified with bowel obstructions in the hospital, and stercoral proctitis or colitis was noted in 10 patients (31.3%). One patient (3.1%) experienced a bowel perforation. Two patients (6.3%) required abdominal surgery, both for bowel resections for ischemia/necrosis of the small bowel and colon. Both patients with bowel resections performed for ischemia/necrosis died in the hospital. Of the 25 patients who were alive when discharged from the ED or hospital, 17 (68.0%) were discharged with oral laxatives and 3 (12.0%) were discharged with antibiotics.
Figure 3. Classification of serious FI-related morbidities.
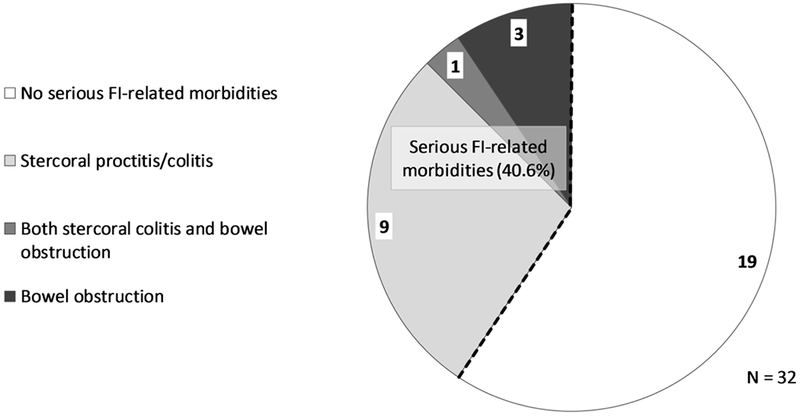
Pie chart revealing the breakdown of serious FI-related morbidities in all patients with ED visits with FI.
DISCUSSION
This study is the first to report descriptive measures and outcomes for ED visits with FI in consecutive patients in the United States. 21.9% of all patients who had ED visits with FI died in the hospital, and serious morbidity related to FI was identified in 40.6% of patients. The median total length of stay for admitted patients was 3 days, with nearly 90% of the visits to the ED requiring hospital admission. The mean age of patients with FI was 72.9 years. Patients presenting with FI had complex medical histories and active treatment regimens, with an average of 8.7 conditions and 11.2 medications per patient listed in medical charts. In this population, both opioid and non-opioid constipating medications were common, with 54.8% of patients taking at least one type of commonly prescribed constipating drug.
The patients captured in this study were similar to FI patients reported in past literature. Patients were primarily elderly individuals, with more than two-thirds (23 of 32) of patients age 65 years or older. A large portion (43.3%) of patients presented from nursing homes, which fits with previous studies that report high risk of FI in institutionalized elderly (6,8). Along with being elderly, patients who presented with FI had complicated medical histories and typically presented with other symptoms and comorbid conditions. The large mean numbers of medical diagnoses and medications indicate that FI typically develops in patients with multitudes of medical issues and active treatment regimens.
Less than half of patients were taking laxatives, suggesting that constipation was not diagnosed prior to presenting to the ED with FI. This finding is surprising, given that the majority of patients had at least one risk factor for constipation. For instance, we found a high percentage of patients who were taking at least one commonly prescribed constipating medication (54.8%). Likewise, approximately one-quarter of patients in this study had preexisting neurological disorders (multiple sclerosis, stroke, etc.) associated with constipation. A large portion of patients who developed FI were institutionalized (46.7%) or wheelchair-bound (42.1%), both of which also predispose constipation.
Surprisingly, the subset of patients who were on laxatives when they presented to the ED were prescribed an average of 2.9 laxatives. However, it is unclear whether the patients were compliant with the laxatives. Alternatively, these patients may have had severe or refractory constipation. Additionally, those patients with FI who died while hospitalized were less likely to take laxatives than those who did not die (28.6% vs. 52.4%). They also took fewer medications (mean of 8.9) when compared to those who did not die (mean of 11.7), despite having a similar number of medical diagnoses (9.0 vs. 8.9).
Hospital visits involving FI were often serious, and FI itself can serve as a marker for overall morbidity and mortality risk. A vast majority of patients who presented to the ED with FI were admitted, with inpatient stays lasting a median of 3 days. 21.9% of all patients who were admitted following an ED visit with FI died in the hospital, with one patient dying shortly after. A large number of patients experienced serious morbidities including bowel obstruction and perforation, stercoral colitis and proctitis, and acidosis and sepsis, among others. As such, patients presenting with FI should be considered to be at high risk for serious morbidities and mortality, and these patients should receive immediate attention and treatment.
The present study has several limitations. Because this study is retrospective, causality between FI and health outcomes or healthcare utilization cannot be determined. Charts were reviewed from a single urban tertiary care center, which limits the generalizability of the study population. The number of charts reviewed was relatively small due to the limited patient population with FI, the large number of variables reviewed per chart, and because 2016 was the first year with an ICD 10 code for FI. Due to this small sample size, a more in depth statistical analysis was not possible. When reviewing medication lists, it was not possible to determine durations or changes of medication regimens, and as such, medication-induced FI could not be directly inferred. Furthermore, FI severity and duration could not be determined in most cases.
In summary, this study is the first to report demographics and outcomes in consecutive patients presenting for an ED visit with FI in the U.S. This study found that FIs often occur in medically complicated patients with significant health histories and large numbers of active treatment regimens. FIs were also determined to be accompanied by significant morbidity and poor health outcomes, including death. Identifying patients at risk for developing FI and treating underlying constipation may reduce future complications.
Acknowledgments
Funding: This project was funded in part by RO1 AT008573–03 (AL) and T32DK007760 (SB and PS)
Footnotes
Conflicts of interests: None
REFERENCES
- 1.Zhao W, Ke M. Report of an Unusual Case With Severe Fecal Impaction Responding to Medication Therapy. J. Neurogastroenterol. Motil. 2010;16:199–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Obokhare I Fecal Impaction: A Cause for Concern? Clin. Colon Rectal Surg. 2012;25:53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Lillo AR, Rose S. Functional bowel disorders in the geriatric patient: constipation, fecal impaction, and fecal incontinence. Am. J. Gastroenterol. 2000;95:901–905. [DOI] [PubMed] [Google Scholar]
- 4.Araghizadeh F Fecal Impaction. Clin. Colon Rectal Surg. 2005;18:116–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corban C, Sommers T, Sengupta N, et al. Fecal Impaction in the Emergency Department: An Analysis of Frequency and Associated Charges in 2011. J. Clin. Gastroenterol. 2016;50:572–577. [DOI] [PubMed] [Google Scholar]
- 6.Read NW, Abouzekry L, Read MG, et al. Anorectal function in elderly patients with fecal impaction. Gastroenterology 1985;89:959–966. [DOI] [PubMed] [Google Scholar]
- 7.Barcelo M, Jimenez-Cebrian MJ, Diaz-Rubio M, et al. Validation of a questionnaire for assessing fecal impaction in the elderly: impact of cognitive impairment, and using a proxy. BMC Geriatr. 2013;13:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rey E, Barcelo M, Jiménez Cebrián MJ, et al. A nation-wide study of prevalence and risk factors for fecal impaction in nursing homes. PloS One 2014;9:e105281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downs J, Wolfe T, Walker H. Development of hydronephrosis secondary to poorly managed neurogenic bowel requiring surgical disimpaction in a patient with spinal cord injury: A case report. J. Spinal Cord Med. 2014;37:795–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serrano Falcón B, Barceló López M, Mateos Muñoz B, et al. Fecal impaction: a systematic review of its medical complications [Internet]. BMC Geriatr. 2016;16[cited 2018 Mar 29] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709889/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tracey J Fecal Impaction: Not Always a Benign Condition. J. Clin. Gastroenterol. 2000;30:228. [DOI] [PubMed] [Google Scholar]
- 12.Grinvalsky HT, Bowerman CI. Stercoraceous ulcers of the colon: relatively neglected medical and surgical problem. J. Am. Med. Assoc. 1959;171:1941–1946. [DOI] [PubMed] [Google Scholar]
- 13.Gau J- T, Acharya U, Marx T, et al. Megacolon and stercoral proctitis after frequent fecal impactions: report of an unusual case and review of the literature. J. Am. Med. Dir. Assoc. 2007;8:338–341. [DOI] [PubMed] [Google Scholar]
- 14.Wrenn K Fecal impaction. N. Engl. J. Med. 1989;321:658–662. [DOI] [PubMed] [Google Scholar]
- 15.Halawi HM, Maasri KA, Mourad FH, et al. Faecal impaction: in-hospital complications and their predictors in a retrospective study on 130 patients. Colorectal Dis. Off. J. Assoc. Coloproctology G. B. Irel. 2012;14:231–236. [DOI] [PubMed] [Google Scholar]


