Abstract
Introduction
This community-based participatory research, Growing Resilience, will be the first full-scale randomised controlled trial we have identified that is designed to evaluate impacts of home gardening on family health. It is based on observational studies suggesting home food gardening has myriad health benefits, Wind River Indian Reservation (WRIR) families’ interest in home gardening and the need to end Native American health disparities with empowering, appropriate and effective health interventions.
Methods and analysis
A total of 100 Native American families in WRIR who have not gardened recently but want to garden will be randomly allocated (1:1) to intervention (receiving 2 years of support designing, installing and maintaining a home food garden of at least 80 square feet (approximately 7 square meters) or to delayed-intervention control (receiving same gardening support after 2 years of data collection). Willing family members aged 5 and up will participate in data collection each February and August for 2 years, with blood, biometric and survey measures at each. The primary outcome is adult body mass index (BMI). Secondary outcomes include child BMI, and adult hand strength, self-reported physical and mental health, diabetes control and food security. Primary analysis will be intention to treat (ITT), using univariate and bivariate descriptive statistics followed by a mixed model to estimate the ITT effect of the intervention using analysis of covariance (ANCOVA) estimation. We will also examine treatment affects using a gardening fidelity measure, combined adult and child BMI outcomes using a lambda mu and sigma (LMS) Z-score reference data set and possible mechanisms of health impacts.
Ethics and dissemination
This protocol was approved by the University of Wyoming Institutional Review Board (IRB) and the project’s Community Advisory Board. De-identified data will be shared with each tribe, and results will be published in peer-reviewed journals, summarised for distribution in WRIR, and shared at a national event to be hosted in WRIR in 2020.
Trial registration number
NCT02672748; Pre-results.
Keywords: protocol, RCT, CBPR, home gardens, Native American, Wind River Reservation, LMS z-score, BMI
Strengths and limitations of this study.
This study leverages Wind River Indian Reservation assets of land, family, culture and community health organisations to learn how to reduce Native American health disparities with a family-based gardening intervention.
While home food gardening shows promise as a family-based health promotion intervention, this will be the first full-scale randomised controlled trial of the health impacts of home food gardens.
This study aims to provide the first internally consistent health outcome measure for interventions that may impact body mass index of both child and adult family members by generating and using an LMS Z-score reference data set from recent National Health and Nutritional Examination Survey (NHANES) data.
In any community, not all families will wish to garden which limits the reach of the proposed intervention.
Due to the nature of gardening and of working with a tightly knit community, this study cannot be blinded and some intervention benefits may ‘contaminate’ control families.
Introduction
As in all sovereign nations in the USA, the Northern Arapaho and Eastern Shoshone tribes that share the Wind River Indian Reservation (WRIR) in Fremont County, Wyoming are survivors of the historical trauma of colonialism. The average age of death for Native Americans in Fremont County is just over 53 years old, with immediate causes including murder, suicide, traffic accidents, chronic liver disease, cancer, diabetes and cardiovascular disease.1 2 Type II diabetes rates in WRIR are at least 11%, double the state-wide rate.3 4 Approximately 60% of middle-school-aged children are overweight or obese, also more than double the rates for children overall in Wyoming,5 and over 70% of adults in WRIR are obese, nearly triple the state-wide rate.4 Effective and appropriate health promotion interventions for tribal families, in WRIR specifically and among sovereign nations in the USA generally, are desperately needed.
Home food gardening shows promise as a family-based health promotion intervention. A growing body of observational research suggests that home and community gardens improve health in many ways, including increasing food security,6 7 fruit and vegetable intake,8–12 and physical activity8 13 14 while reducing stress.15 16 Since these outcomes would plausibly help reduce or prevent obesity, and because observational research has found positive associations between gardening and healthier body mass index (BMI),12 17 gardening shows promise as an obesity intervention. However, to date, no full-scale randomised controlled trials (RCTs) have been done to more conclusively identify health impacts of home gardening.
Specifically within WRIR, many families showed interest in receiving technical and financial help in establishing or expanding home gardens during a 5-year participatory action and research partnership called Food Dignity. In response, partners at University of Wyoming (UW) and WRIR tribal health and community-based organisations partnered in 2013 to co-design and implement a feasibility pilot study about health impacts of home gardens on the reservation.18 The Growing Resilience project, for which the protocol is described here, grew out of that pilot study. This appears to be the first full-scale RCT of the health impacts of home food gardens. Results from a pilot RCT with older cancer survivors was recently published, which found a trajectory toward positive outcomes. Also, an RCT of health impacts of community gardens is currently under way.19 In addition to being the first scaled RCT of home gardens, this research will contribute to a limited literature about effective and appropriate health promotion strategies for use in and by Native American communities.
Methods
Study design overview
About 100 Native American families in WRIR who are interested in starting a new home food garden have been or will be recruited over 3 years, starting in 2016. Participants will be randomly assigned by household to one of two arms: home gardening support for 2 years or control with delayed intervention after 2 years. This RCT was designed using the Consolidated Standards of Reporting Trials checklist and adhered to the Standard Protocol Items: Recommendations for Interventional Trials checklist. The first wave of participants will enrol in the study on 15 February 2016.
Participants will take part in four health data collection sessions, two per year. These sessions will be in February, prior to gardening activities each year, and again in August at the height of gardening season. Adult data collection will include biometric information (BMI, waist circumference, blood pressure and hand strength); blood serum analysis (including a standard blood chemistry panel, haemoglobin A1c (HbA1c), vitamin D and serum beta carotene); and survey-based measures including food security (US Department of Agriculture 6-question food security survey) and physical and mental wellness (SF-12v2 survey). Child (ages 5–17) measures collected will include BMI, waist circumference and HbA1c via finger-prick blood testing. Participants will be encouraged to fast for 12 hours prior to data collection, and we will record fast status prior to each data collection session. However, a failure to fast will not disqualify participants from a data collection session.
Adult BMI will be the primary health outcome. Primary analysis will be a mixed model that will be used to test for the effect of the garden intervention on adult BMI, controlling for baseline weight, gender, age and tribe and accounting for household clustering.
Secondary analyses will study the effects on a range of other biometric, blood and survey health outcome variables and on intrahousehold effects. Beyond BMI, health outcomes of particular interest are impacts on mental and physical health, hand strength, food security among food insecure households and diabetes control among those who are either diabetic or pre-diabetic.
To investigate the intrahousehold effects, we will compare relative changes of individual-level BMI Z-scores for all children and adults in a survey household. These Z-scores will be constructed using NHANES survey data for people aged 5 to 74 as the reference population and following the statistical methodology developed in Naschold.20
We will also examine possible mechanisms that cause changes in health outcomes (eg, serum status of Vitamin D and/or beta-carotene). In this manuscript, we also briefly describe protocol development for analysing outcomes with adjustment for any reported changes in medication or supplement dosage.
In addition, we will extensively use qualitative methods for providing insights into project process, outcomes and mechanisms, including photo narratives, focus groups, participation and observation, and interviews with gardening families. Though this will not impact our primary quantitative analyses described here, these results may help with understanding of potential mechanisms and with interpreting any variations in results among gardening families. They will also inform both the gardening support strategies and the overall partnership process. These methods will be described elsewhere.
Project partners
Growing Resilience is a community-based participatory research project. It was co-designed by WRIR-based and UW partners, largely during the 2013 feasibility pilot and is overseen by a Community Advisory Board (CAB). Reservation-based partner organisations include native-run non-profit organisation Blue Mountain Associates (BMA), community health representatives (CHRs) from Eastern Shoshone Tribal Health and the Wind River Development Fund (whose CHR focuses primarily on Northern Arapaho family recruitment). Non-reservation-based partners include staff at UW’s Division of Kinesiology and Health, staff at the UW-based Wyoming Survey & Analysis Center (WYSAC), UW technicians who assist at the health data collection sessions and phlebotomists from the non-profit health organisation Wyoming Health Fairs (WHF).
BMA, and particularly their garden manager, will lead design and implementation of the gardening intervention, including development of a garden guide, overseeing an annual gardening workshop, assisting with garden installation and providing ongoing support and mentorship for all garden-intervention participants. CHRs will lead family recruitment and retention efforts. UW will lead collection of health metrics and data analysis efforts. The CAB will participate in policy decision-making in regard to ongoing project design and public representation; advocate for community interests in regard to research data collection, ownership and dissemination; serve as an additional contact point for all research participants seeking information or assistance with their involvement in the project; and consider how to maintain the capacity, infrastructure and momentum of the gardening programme beyond the life of the funded project. Seven members of the WRIR community make up the CAB.
Participants
To be eligible to participate, a family must meet the following requirements: (1) live within the boundaries of the Wind River Reservation (including Riverton, WY); (2) have at least one member enrolled in a federally-recognised tribe; (3) have at least two adults (or one adult for single-adult families) willing to participate in 2 years of gardening and four health data collection sessions over 2 years; and (4) have interest in starting and sustaining a home food garden, but don’t currently have a garden over 30 square feet. Though the gardening intervention will be at the household level, data collection and analysis will be at the individual level. Adults living in the household and children aged 5 or older can enrol in the study to participate in the data collection.
Even though adult BMI will be the primary outcome of this study, being overweight or obese will not be not part of the eligibility criteria. About 70% of adults in Wind River are obese,4 perhaps another 20% are overweight and at least two adults per participating household are expected to enrol in the study. Thus, the study team and the advisory board for the pilot study decided that the ethical and practical issues that screening for eligibility by BMI would raise were not worth surmounting.
Children will be included in the study because family health and participation was a priority set by the advisory group during the pilot phase, which had included only adult family members in data gathering. Children who are under 5 years old when the family enrols in the project may ‘age in’ to data collection procedures as long as they can participate in at least two data collection sessions. Similarly, youth who turn 18 during their family’s enrolment in the study may elect to participate in adult data measures (ie, blood draw, blood pressure, hand strength and survey). If a participant becomes pregnant or incarcerated while taking part in the study, he or she will not undergo data collection for the duration of pregnancy or incarceration.
The goal is to enrol 100 families in three waves over the first 3 years of Growing Resilience, with 20 in the first year and then 40 in each of the next 2 years. Eastern Shoshone Tribal Health and the Wind River Development Fund each will aim to recruit 50 households. They will primarily draw from the hundreds of families they already serve, though joint public events and media advertising will also be used.
Participant and public involvement
As discussed in the introduction, Growing Resilience was designed to meet the expressed needs of families in WRIR for more home gardens. Project partners from UW, tribal health programmes and BMA focused on home gardens based on families’ experience that food sovereignty depends on having food (including food gardens) close to their homes, given the large geographic size of WRIR and many families’ lack of access to reliable transportation.
Partners then collected feedback on the 2013 pilot from project participants. Changes resulting from this feedback included adding children aged 5–17 to the study (based on participants’ priorities for family-based interventions); providing financial compensation for participating in each health data collection session (based on participants’ assessment of the burden of participation); modifying survey questions and dramatically shortening the survey (attention and participation began dropping after 20 min, including because children were often present); adding multiple modes of survey administration (based on participants’ experience and preferences taking the pilot survey); removing the use of activity trackers (these were not well used nor received by participants); and setting the intervention duration to 2 years (based on project partners’ observation that most participants needed more than 1 year of gardening support to develop successful gardens.) We also will move data collection sessions to a central location on the reservation, providing transport as needed, instead of visiting participant homes (due to logistics of adding blood draws, which were not part of the pilot, and to both partner and participant preferences). One of the participants from the 2013 pilot project is now on the project’s CAB, but otherwise participants are not directly involved in ongoing study recruitment and conduct. However, new participants may join because they have heard of the project from current participants and wish to take part.
Participants will receive ongoing reports of their personal health information (including biometrics and blood chemistry panel) after each data collection session they attend. Additionally, results will be summarised for distribution in WRIR and shared at a national event to be hosted in WRIR in 2020.
Calculation of sample size
Sample size calculations were performed with adult BMI as the primary outcome. The feasibility pilot study data, combined with demographic data about WRIR, implies that the average participating family would have two adult and two child participants in the study. Thus, 100 families would include 200 adult participants.
The 80% power calculations below include a family-cluster design effect of 1.1 among adults in one household,21 an attrition rate of 16% and a difference in adult BMI change between control and intervention groups of 0.5 over the 2 years of intervention (0.75 vs 0.25; with a two-tailed test, α=0.05; σ=1.1).22 Assumptions are based on the literatures cited and on our pilot data.
Design effect of household adult clusters=1.1 = 1 + (m-1)*ICC=1 + (2 adults −1)*0.1.
Sample size needed (each group)=76 = 2[(1.96+0.842)2*σ 2]/(u1-u2)2=2[(1.96+0.842)2*(1.1)2]/(0.75–0.25)2.
Planned sample size (each group)=100 = 50 families * 2 adult participants per family on average.
Planned sample size (each group) including design effect of household clusters: 91=100/1.1.
Adult attrition rate this allows: 16%=1 - (76/91).
In sum, before attrition and adjustment for family cluster effects, this study requires 152 adults (76 per group) to power the study at 80%. ‘Discounting’ the planned sample of 100 adults per group for family cluster effects means reaching the recruitment goal statistically provides ‘91’ adults per group. Thus, this sample size adequately powers the study, allowing for 16% attrition, while attending to constraints of budget and institutional capacity. Additional families will be recruited in the fourth year if attrition or a smaller effect size necessitate that. Attrition rates are based on the relatively low mobility of families in this community, the strong existing relationships between the CHRs and many of the families in the community and previous research collaborations among this research team with participants from this community.
Randomisation and group assignment
A total of 100 families will be recruited and enrolled in the study in three waves. The first wave, recruited in the first year, will include 20 families. Wave 2 in year 2 of the project and wave 3 in year 3 of the project will include 40 families each. About half of the families in each wave will be recruited by CHRs from Eastern Shoshone Tribal Health (with a focus on Eastern Shoshone families) and the other half by Wind River Development Fund (with a focus on Northern Arapaho families).
Staff at UW’s WYSAC will oversee the randomisation process. Each wave will be randomised to control or intervention groups in a 1:1 ratio using stratified block randomisation. First, we will stratify by tribe to ensure each tribe has an equal number of participants. Second, we will use fixed-block randomisation within each tribe strata so that 50% of Northern Arapaho-recruited families and 50% of Eastern Shoshone-recruited families get gardens and half are assigned as controls/delayed intervention. Randomisation occurs by inputting both tribal groups into an IBM SPSS (version 24) datasheet and selecting the first 10 of each tribal group by using a continuous uniform distribution method to randomly select exactly 10 cases from the first n cases. The random cases selected are then input into a separate IBM SPSS datasheet where approximately 50% of the cases are randomly selected using IBM SPSS simple random sample without replacement. The randomly selected cases become the treatment groups and the cases not selected become the control/delayed intervention groups.
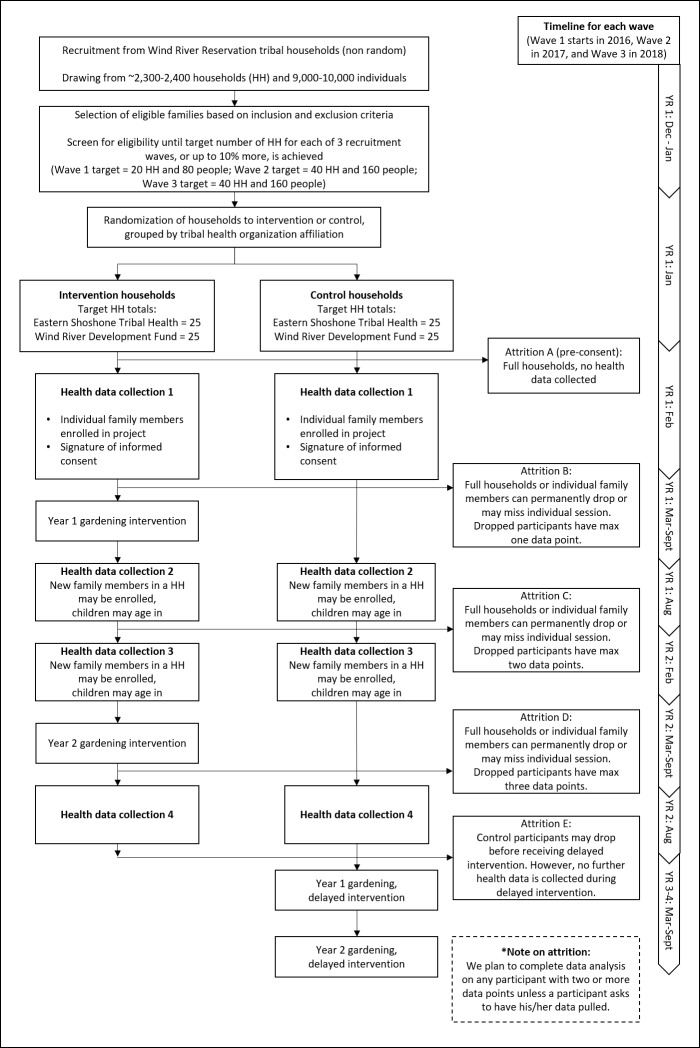
The rationale for stratified block (rather than simple) randomisation is practical and cultural. Practically, establishing the intervention gardens is so time and planning intensive that BMA needs managed and predictable numbers of families with whom they will work. Culturally and politically speaking, each tribe prefers to receive approximately equal services each year. The actual randomisation process will be blinded, that is, participants will be unable to manipulate the randomisation process itself. The flow chart in figure 1 summarises the randomisation, intervention and data gathering design.
Figure 1.
Flow chart of Growing Resilience study design.
Strategies for engaging families who are randomised to control will include issuing a project newsletter to all participants and the CHRs staying in touch with those families until they have completed the four data collection sessions and can begin planning their gardens with BMA.
Garden intervention
Families randomly assigned to intervention will receive a full gardening support package for 2 years from BMA. After the baseline data gathering session each February, the half-time, year-round garden manager will meet with each family to plan their garden. BMA’s garden manager is Northern Arapaho, a long-time gardener, and also was previously a Diabetes Navigator for Northern Arapaho Tribal Health, giving her particular insight and expertise in both gardening and health promotion. The first-year support package will include the following: (1) consultation (on location; whether in-ground, raised bed, container; and what they would like to grow), (2) garden bed installation, (3) purchase of materials (eg, tools, starts and seeds), (4) ongoing mentorship including garden visits and (5) gardening workshops. The planned average budget for this package will be $700 per family, excluding the manager’s time and the labour costs of seasonal hires. Garden-intervention participants will be in charge of maintaining their gardens through the season (eg, watering, weeding and harvesting). Because there will be no parameters regarding what a family chooses to grow, each garden will be different, based on the participants’ interests and needs, but will be a minimum of 80 square feet per family. Which family members participate in gardening will be at the household’s discretion.
During the second year of garden support, BMA will provide additional soil, soil amendments, seeds, seedlings and tools as needed, and ongoing mentorship and support for renewing the food garden. The planned average budget, per family, for the second year of support will be $200.
Primary outcomes will be analysed as intention to treat (ITT), regardless of implementation fidelity. However, we will also consider fidelity in secondary analyses, running a mixed model of significant outcomes against a measure of garden success. This measure is in development based on a combination of two indicators. One is the percent of planted garden square footage in August out of the square footage planned and prepared in May (with prepared plot size provided by the BMA gardening manager and planted size estimated from photos taken by BMA staff and the participants themselves). The other is an assessment by the gardening manager of the extent to which each family planted and maintained their garden, using a 5-point scale. Implementation fidelity will also be compared with the records of intervention support to inform intervention design. Finally, the survey measures will ask each adult in an intervention family how many hours they spent gardening, and we will conduct a secondary analysis of individual health outcomes for adults versus self-reported hours spent in the garden.
After the two seasons of gardening support and four data collection sessions are over, families assigned to the control condition will receive the same first-year gardening support services from BMA as the intervention families do. In their second year they will receive $200 in credit at the gardening store of their choice to purchase what they need for renewing their gardens.
Quantitative data collection
Twice per year for 2 years, trained technicians will collect health indicator data from adult and child participants. The primary outcome after 2 years of gardening support is adult BMI. Secondary adult outcomes include physical and mental health (on the SF-12v2 survey), food security (USDA six-item), hand strength, waist circumference, blood pressure and fasting (when possible) blood-based measures including HbA1c. For children aged 5 and older, we are collecting BMI data, waist circumference and, via finger-prick tests, HbA1c. Table 1 summarises the quantitative data collected at each of the four sessions.
Table 1.
Health indicator data collected for adults and children, in February and August each year for 2 years
| Biometric | Blood-based | Survey-based | |
| Adults |
|
|
|
| Children |
|
|
Not Applicable |
BMI, body mass index.
Primary outcome measurement
Height will be measured using a Seca 213 Mobile Stadiometer. Participants will remove shoes and socks and stand with feet together, heels and back to the stadiometer. Technicians will ensure participant’s head is in the Frankfort plane, ask the participant to take and hold a deep breath, and then lower the sliding headboard until it is contact with the head, compressing hair if needed. Participant will then be asked to bend knees and step away from stadiometer. The technician will record height to the nearest half inch, written on a scrap piece of paper. The technician will measure height a minimum of three times, continuing to take measurements until they have a minimum of two height measures that match to the half inch.
Weight will be measured for most participants using a Tanita SC-331S Body Composition Analyzer. After verifying that the participant has no internal electronic devices (such as a pacemaker or diabetes pump), the technician will enter the participant’s measured height (to the half inch), age, self-identified gender, clothing weight (standardised at 3 lbs. [1.4 kg.] for adults and 2 lbs. [0.9 kg.] for children) and body type (standardised as ‘normal’ for all participants) into the Tanita. The participant will then step onto the unit, which measures weight to the 0.2 pound and also calculates BMI. Weight of participants who cannot use the Tanita will be weighed using a MyWeigh XL-High Capacity Scale.
Other outcome measurement
Waist circumference of adults and children will be measured using a Gulick II Tape Measure. The technician will request that the participant hold the zero of the tape measure on her navel and then ask the participant to turn in a circle. The technician will adjust the tape measure so that it lies parallel to the floor while remaining across the navel. The technician will then pull tension on the tape measure to 4 oz. (approximately 113 g.) as displayed on the tape’s tension indicator and then record waist circumference to the nearest half inch. Like other common methods for measuring waist circumference, this approach yields internally consistent and replicable results, while also being comparatively simple to use.23
Adult blood pressure will be taken using an Omron 10 Plus Series Upper Arm Blood Pressure Monitor with ComFit Cuff. The technician will wrap the cuff around a participant’s biceps, ask the participant to rest her arm on a table, then will initiate the automatic monitor process. If the cuff is too small to fit around a participant’s arm comfortably, technicians will read blood pressure by wrapping the cuff around the participant’s forearm instead of biceps.
Changes in hand strength provide a surprisingly strong nutrition indicator and disability and mortality predictor.24–26 Hand strength of adult participants will be measured with a Baseline 12–0240 Standard Hand Dynamometer. The technician will instruct the participant to hold the dynamometer facing away from themselves, elbow tight to waist and at a 90° angle from the upper arm. The participant will then squeeze the dynamometer and the technician will record hand strength to the nearest pound. The process will then be repeated for the other hand.
Adult participants will also complete a survey comprised of a maximum of 46 questions, depending on skip patterns. Survey questions will include physical and mental wellness (SF-12v2 Health Surveys),27 food security (USDA US Household Food Security Survey Module Six-Item Short Form,)28 confidence managing health, demographics and issues related to the Growing Resilience garden intervention. Questions also will ask participants to estimate their physical activity, vegetable consumption and (for the intervention group) how many hours they spent gardening each week. The need to limit overall survey length to a 20–30 min time burden on participants heavily constrained the number of questions that could be posed and answered with attention, or at all, by participants. Thus, for example, the survey includes the seven vegetable consumption questions from the National Cancer Institute’s Quick Food Scan,29 which shows reliability but little precision in measuring intake.30 Physical activity estimates are requested in just one question (‘Think about your level of physical activity in the past four weeks. How often have you done moderate or high levels of physical activity (for example, pushing a vacuum cleaner, gardening, playing horse shoes, walking, running, or playing basketball)?’), with examples derived from the pilot experience and the 11 response options modelled on the vegetable consumption questions. Medication and supplement data will be collected via interviews and, when consent is given, medication lists from the participants’ healthcare providers. Though the survey will not be administered to children, child gender and birth date data will be collected as part of intake procedures for use in BMI-for-age Z-score calculations.
For the blood-based measures, trained phlebotomists from Wyoming Health Fairs (WHF) will draw venous blood from adults for analysis by LabCorps. For adults 18 years and older, the chemistry panel includes measures of HbA1c, beta-carotene (as a proxy for vegetable consumption),31 vitamin D (as a proxy for sunlight exposure), cholesterol and triglycerides. HbA1c in youth aged 17 years and younger will be measured using A1c Now diagnostic kits that use a finger prick to obtain a small blood sample. Participants will be encouraged to fast for 12 hours prior to data collection, and we will record fast status prior to each data collection session.
Data collection and management procedures
The health data collection sessions will take place twice each year (February and August) in a public building that is relatively centrally located in WRIR. The CHRs will schedule appointments with each participating family and, if needed, assist with transportation. Families will move through six stations: check in, phlebotomy, biometrics, survey, medications and supplements interview and check out.
At their first check in, participants will review and sign consent (adults) and assent (children) forms along with protected health information sharing forms (to allow WHF and UW to share participant health information for reporting purposes). UW staff will oversee this process and will be on hand to assist (eg, reading aloud forms, as needed) and answer questions. After completing informed consents and assents, each family member will be assigned a unique identification number and will choose a code name. Both, along with date of birth and self-identified gender, will be written on the back of a hard-copy data collection booklet called ‘Your Health Data Passport’ (henceforth referred to only as a participant’s ‘health passport’) that participants take from station to station within each data gathering session. Real names will be linked with these numbers in a password-protected Excel sheet with a paper back-up copy stored in a locked cabinet on the UW campus. Template consent and data collection forms are available by request to the corresponding author.
The identification numbers will contain seven digits that signify the participant’s tribal health association (Eastern Shoshone or Northern Arapaho), recruitment wave (1–3), intervention status (garden or control), household and if she or he is head of that household. These identification numbers will help ensure participants are given the correct survey versions (eg, control participants will not answer questions about gardening and only heads of households will receive the food security questions). The code names, which are words chosen by the participant at enrolment, will enable both participants and staff to easily keep track of health passports and confirm identity at each data collection station. Participants also will be given the option to fill out paperwork to have a copy of blood lab results from the day sent to a specified healthcare provider. UW staff will keep health passports between data collection sessions.
Wyoming Health Fairs will staff the phlebotomy station and conduct blood draws for adults and HbA1c finger sticks for children. Participants will be invited to help themselves to the provided breakfast any time after completing the phlebotomy station.
The biometrics station, staffed by a combination of UW and Wyoming Health Fairs technicians, will include collection of height, weight, body composition (for people without pacemakers), blood pressure, waist circumference and hand strength. Generally, one technician will conduct the measurements while the other records measurements in the participants’ passport and in an online survey form (Qualtrics).
The survey station will be staffed by two UW technicians who will facilitate survey administration to adult participants. Participants may choose to complete the survey electronically (using Qualtrics), on paper or as an oral interview with a technician reading the questions and entering participant answers online.
At the medications and supplements interview station, adult participants will share current medications and supplements with a UW technician. When available, the technician will use a participant’s physician-provided medication list to guide the interview. The technician will enter all medications and supplements into a Microsoft Access database designed by WYSAC for this study.
Finally, at the check-out station, a UW technician will review participants’ passports to ensure completion of each station and will cross-check written information in passports to that in emailed Qualtrics reports and (if available) on the printout from the Tanita body composition monitor. She will log any inconsistencies in the designated error database for later correction and facilitate re-measurements if necessary. The technician will then conduct a short exit interview with participants to ask how the project is going and to ask for any feedback participants might have at that time. Finally, participants will receive cash stipends ($40 per adult, $15 per child and a $20 gas stipend per household). UW will keep one copy of each participant’s Tanita printout and will keep health passports until after a participant’s final data collection session, at which point each participant may keep his or her health passport. Participants keep one copy of their Tanita body composition print-out and adults will receive a copy of their blood test results in the mail.
To improve the chance that participants will arrive having fasted for 12 hours (unless they are diabetic or have another reason to avoid fasting), sessions will take place from 07:00 hours to no later than 13:00 hours. CHRs will use a scheduling software with automatic email and text reminders to set up times and dates for participants to attend sessions. CHRs and UW staff will also follow-up with any participants who are late for or miss a scheduled session. These contact procedures will be adapted as needed to meet participant preferences and most effectively reach them. Any participant who does not attend a main data collection session will have the option to attend a ‘sweep’ session for just biometric and survey data collection (no blood draw), scheduled around the participant’s calendar in the weeks following the full data gathering sessions.
In the fifth and final year of the project, in 2020, all participating families will be invited to return for a final data collection session. The design of this session will be constrained by funding, but otherwise shaped by the community advisory board, feedback from the families and the partner organisations.
In addition to the above-described check-out station data cross checks between participant health passports, emailed Qualtrics reports and printed Tanita receipts, we will be using several automated data checking approaches to ensure data integrity and avoid duplicate case entry. In particular, we will check for and review any inconsistencies in BMI-related variables. Also, UW has a Data and Safety Monitoring Board (DSMB) to which we report. All members of the data gathering team, including WHF, are responsible for reporting adverse events. CHRs and WHF will follow-up if needed with individual participants. In addition, the principal investigator (PI) will assign severity values to such events and report them annually to the DSMB and Institutional Review Board (IRB).
Outcomes and analysis methods
Primary outcome (BMI) analysis
The primary analysis will use an ITT analysis to examine the effect of gardening on changes in BMI. As the primary outcome, adult BMI data will be analysed separately from child BMI Z-score data. Z-scores will be constructed from CDC growth charts. To begin we will present univariate and bivariate descriptive statistics.
Then, we will use a mixed model to estimate the ITT effect of the intervention. Estimation will be via ANCOVA as this method has been shown to have more statistical power than traditional difference regressions.32 For exposition and comparison we will also present less efficient difference regressions that are traditionally reported. ANCOVA’s gain in efficiency is larger the smaller the degree of autocorrelation in the dependent variable. We will test for autocorrelation in all dependent variables as ANCOVA’s advantage is likely larger for some of the other health outcomes discussed under ‘Secondary Outcome Analysis’ below that may be (even) less correlated over time than BMI.
Change in adult BMI will be the dependent variable in primary outcome model. The fixed effects of interest in the model will be the indicator variable for ‘garden’ (treatment). As families will be recruited in three annual waves we will include an indicator variable for wave to control for recruitment year. Further, our estimations will control for baseline BMI, gender, age and tribe. Due to the longitudinal nature of our data we can also include individual- and household-level effects to control for unobserved, non-independence of observations. We include these as random effects, if possible, or as fixed effects if required by Hausman model specification tests. Analysis will be blind to participant control or intervention condition.
While the primary BMI analysis will examine adult outcomes separately from child outcomes, we will also use a novel technique that allows us to assess BMI outcomes for the entire sample (child and adult combined). Applying Naschold’s20 lambda mu sigma and tau (LMST)-based method we will first construct BMI Z-scores for all participants aged 5–74 using NHANES data as the reference population. These Z-scores will provide an internally consistent outcome measure for interventions expected to impact BMI of all family members. Biologically and statistically, this is as reasonable as the common practice of comparing Z-scores among children of varying ages. Using BMI Z-scores for all participants has two distinct advantages. First, combining children and adults in the same analysis will increase the number of observations and, thus, statistical precision. And second, it will allow us to look at the intrahousehold effects of the intervention, for instance, we can test whether gardens benefited children more or less than adults in the same household.
Secondary outcome analyses
Because this is the first full-scale RCT on health impact of home gardens, our secondary outcome analysis will replicate the ANCOVA analysis outlined above using the whole range of other biometric, blood serum and survey health outcomes (see table 1) as dependent variables. However, mental and physical health, hand strength, food security among food insecure households and diabetes control among those whose HbA1c and/or survey responses identify them as either diabetic or pre-diabetic will be the priority secondary outcome analyses. We will also examine child BMI outcomes (using BMI-for-age Z-score).
We will also use the gardening fidelity measures described above to analyse treatment effects on these primary and secondary outcomes, in addition to the primary ITT analysis.
Accounting for changes in medications and supplements
During focus groups in the pilot phase of this project, several participants reported that they reduced the dosage or discontinued medications for several chronic conditions including diabetes, blood pressure, depression and anxiety, and/or pain. Since changes in medication could either mask or amplify perceived health impacts of the gardening intervention, the protocol for this study includes gathering information about medication and supplement use and changes from participants. A pharmacist on the study team will then explore methods of accounting for any impacts of such changes on assessed health outcomes, especially for physical and mental health (on the SF-12v2 survey), blood pressure and HbA1c, as part of secondary analyses.
A review of the literature for a standardised way to accomplish this revealed no previous studies. When a participant reports medication or supplement changes that plausibly would impact a health outcome measured in this study, then a pharmacist on the research team will advise on development and use of two approaches for a secondary analysis of those health outcomes that accounts for those changes. One approach will be to quantify estimated impact of the medication change on a target outcome, if data are available to make such estimates. For example, if a participant is taking 1000 mg of metformin twice daily for treatment of diabetes at the start of the study and stops the medication during the intervention, this could be translated to a one percentage point reduction in HbA1c.33 Where such data are not available, such as for pain or antidepressant medications, the approach will be to develop an internally consistent scale for estimating impact of medication changes on outcome variables, and to report such outcomes qualitatively.
Missing data treatment
The CHRs at Wind River Development Fund and Eastern Shoshone Tribal Health, as well as BMA garden staff, will follow-up closely with the participants and make great efforts to obtain complete data for all the participants. Any participant with two or more data points (out of the four) will be included in analysis. Missing data patterns will be examined to identify and apply the appropriate method to deal with it (eg, multiple imputation, Full Information Maximum Likelihood, propensity scoring).
Insight into mechanisms
The mechanisms of any health changes attributable to the intervention are likely multifaceted. Each of the biometric and survey measures discussed above can potentially impact changes in BMI. For example, sunshine exposure alone might improve mental wellness and blood glucose regulation.34 The wide range of biometric, physical and mental health indicators collected will be used as explanatory variables in a panel data regression model. We will also test for potential complementarities between these indicators by including respective interaction terms. In addition to controlling for these observable characteristics, we will exploit the panel data structure to also control for sources of unobserved heterogeneity through the use of wave, household and individual dummy variables. This multivariate panel regression model will allow assessment of the effect each observable factor has on changes in participants’ BMI. Moreover, it helps to determine the relative importance of each of these factors, for example, whether a reduction in BMI is more strongly driven by increased vegetable consumption versus improved mental health. The point estimates from our regression will also be used to predict what changes in BMI are possible based on achievable ranges of changes in our biometric and survey measures. Qualitative data analysis will also inform quantitative estimation strategies for mechanism exploration. Overall, mechanism analyses will provide insight but not conclusions about how gardening may work to improve health, if indeed improvements are identified.
Expected outcomes
Better outcomes in nutritional, physical and emotional health are expected among family members in gardening households than in control households, measured per the above. Differences in adult BMI is the primary outcome. The pilot data and previous observational research indicate other significant outcomes may include improvements in emotional health, blood glucose levels and control, and hand strength.
Potential problems and alternative strategies
The incentives for participation are high enough that the team expects enough enrolment and retention to support this study. Yet, attrition and missed data gathering appointments are the most likely challenges, especially given the transportation issues many families face. However, the tribal health CHRs build and maintain strong relationships with the families they serve, and they will support families in making and keeping their data gathering appointments, including picking them up and bringing them if transportation is a problem. If families miss a main data collection time point, follow-up ‘sweep’ sessions for just biometrics and survey data collection (no blood draw) will be scheduled around those families’ schedules.
Contamination, that is, the spread of some benefits of gardening from intervention to control families, is possible. For example, intervention families may share their harvest or even just their excitement, and control families may help intervention families with their gardens. In addition, though control families will agree to wait to garden until data collection is complete, and will not receive gardening support until then, they are free to start a garden if they wish. These issues would reduce the ability of this study to detect any positive health impacts of gardening; yet, they also would suggest that such positive impacts are socially contagious. A question in the survey administered at each August data gathering will ask participants if they started or maintained a vegetable garden of any size that summer, which will help identify families who decide to garden during their period as controls. Additionally, the qualitative research accompanying these RCT methods will help provide insight into these issues, but will not change our primary ITT analysis.
If provisional data analysis indicates the study is impacting BMI but is not powered sufficiently to detect differences (eg, if attrition exceeds the maximum 16% assumed in the power calculations above or if the impact on BMI is smaller than estimated from pilot data), then the team will rerun power calculations based on observed attrition rates and BMI changes to inform how many additional families to recruit in a supplemental fourth wave.
The constraints on a feasible and appropriate length of the survey component in this context also limits the quality and quantity of data collected that might provide additional insight into mechanisms of any differential outcomes found between the two groups. For example, the beta-carotene blood measure only provides an indicator of consumption for vegetables rich in that vitamin, and though the brief vegetable consumption survey module will provide some indicator of vegetable consumption, responses will not provide precise intake information. However, the range of quantitative indicators combined with deep qualitative research with gardening and control families should provide a relatively rich data set to examine for potential mechanisms in any differential outcomes this study may find between the two groups. Also, this first full-scale RCT study into home garden impacts will provide foundations for future protocols that can be designed with greater focus into mechanisms and outcomes that this study’s results indicate are plausible or likely.
Discussion
This Growing Resilience research project leverages WRIR assets of land, family, culture and community health organisations to develop and evaluate home food gardens as a family-based health promotion intervention to reduce disparities suffered by Native Americans in nearly every measure of health. As a tribal health partner said during the pilot phase of this project, ‘We need to put health back into the hands of the people.’
The central scientific hypothesis in this study is that, after 2 years of home gardening, the BMI and other objectively verifiable health indicators in members of intervention families will show positive and significant differences from those of control families. The long-term goal is to build tribal capacity to improve Native American health by identifying and evaluating suitable, scalable and sustainable health promotion interventions aimed at ending health disparities. If results from this study are positive, then supporting home gardens with tribal families will become a culturally relevant and empowering health promotion strategy for tackling health disparities.
Regardless of the RCT results, an immediate goal is to support WRIR organisations in establishing and sustaining home food gardening as an option for any family on the reservation who would like to start growing some of their own food. Benefits of such gardening likely extend beyond narrow measures of health such as those quantitatively assessed in this study.18
As the first full-scale RCT about health impacts of home gardening, which observational studies suggest improves health, results of this study may also be relevant for families in other settings and of other cultures. In addition, development of an LMS Z-score BMI curve might enable future studies to measure BMI outcomes in adults and children who are five or older as one population.
Ethics
This study was co-designed with tribal health organisations, gardeners from the WRIR community, garden-intervention participants from the project’s pilot study, UW-based researchers and a tribal community based organisation. A CAB is overseeing and advising the study implementation and dissemination. Additionally, all de-identified data will be shared with each tribe, and any major protocol modifications will be discussed with the CAB and shared with both tribes and the UW IRB. About half of the direct-cost budget for the project is allocated to WRIR-based partners and people and half to UW for data collection and analysis costs. Growing Resilience also responds to extensive interest in home gardening among WRIR families that emerged during an earlier UW-WRIR action-research collaboration.
However, the families who wait 2 years for their gardens—the controls—are bearing the costs of the rigour of an RCT design. Are the costs of this knowledge gain fair or right to ask anyone, especially in a Native American community, to bear?
Additional ethical questions are raised by widening the lens to examine the enormous political, institutional and financial power differences between a university, such as UW, and tribal organisations. For example, the National Institutes of Health (NIH) has awarded UW $570 856 in indirect costs for this project; the other partner organisations, together, will receive a total of $106 700 in funding for overhead. UW incurs substantial compliance and contract management costs that subawardees do not, but perhaps not costs that are more than five times those of community organisations.
Dissemination
Dissemination will include conference presentations, journal publications, ‘grey literature’ reports for practitioner and local use, Facebook and a project website, news media coverage and a national conference to be held in WRIR in 2020 to share our results with and learn from other Sovereign Nation efforts to promote health with food-related interventions. We will also produce gardening intervention guide tailored for reservation-based gardening programmes, drawing on BMA’s experience and on existing resources, such as existing family garden guides.35
Conclusion
This paper summarises the rationale and design for an RCT that will support development of a tribal-led home garden support programme, provide home food gardens to 100 Eastern Shoshone and Northern Arapaho families, and assess the health outcomes from this gardening intervention. This is the first RCT to evaluate the health impacts of home food gardening, to the knowledge of the authors. The goal is to identify and support desirable, empowering and effective family-based health promotion strategies that will help families in WRIR, and possibly in other communities, take control of and improve their health.
Supplementary Material
Footnotes
Contributors: CMP conceived the study and developed and designed it with AMW, Blue Mountain Associates, Eastern Shoshone Tribal Health, and Northern Arapaho Tribal Health. AMW led design of data gathering procedures with assistance from Wyoming Health Fairs and CMP. FN and SH designed data analysis methods and LF is designing approaches to secondary analyses that account for reported medication and supplement changes. CMP and AMW wrote the bulk of this protocol paper, with the other co-authors drafting the sections relevant to their design contributions. All authors, plus the Community Advisory Board, reviewed and approved this manuscript for submission.
Funding: The Growing Resilience study is funded by NHLBI and NIGMS National Institutes of Health, grant no. R01 HL126666-01. The 2013 pilot work was funded by NIGMS/NIH grant no. 8 P20 GM103432-12.
Competing interests: None declared.
Ethics approval: Protocol #20181001CP02135, University of Wyoming, USA, Institutional Review Board; the Northern Arapaho Business Council; and the Eastern Shoshone Business Council.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. Xu J, Murphy S, Kochanek K, et al. . Deaths: Final data for 2013. National Center for Health Statistics. Hyattsville, MD, 2016. [PubMed] [Google Scholar]
- 2. Reservation residents have much lower life expectancy and a higher incidence of disease, legislators told. (County 10 Community News Stream). 2014. Retrieved from http://4dc.b85.mwp.accessdomain.com/2014/01/08/reservation-residents-much-lower-life-expectancy-higher-incidence-disease-legislators-told/.
- 3. Sherard BD. The Burden of Diabetes in Wyoming: the Causes, Complications and Impact of Diabetes on Wyoming and Its Residents. Wyoming Department of Health, Cheyenne, WY. 2010. Retrieved from http://www.health.wyo.gov/Media.aspx?mediaId=8146.
- 4. Alliance to Reduce Disparities in Diabetes. Reducing Diabetes Disparities in American Indian Communities (Wind River Reservation) [Online]. http://ardd.sph.umich.edu/eastern_shoshone_tribe.html (accessed 21 Nov 2017).
- 5. Smith DT, Bartee RT, Dorozynski CM, et al. . Prevalence of overweight and influence of out-of-school seasonal periods on body mass index among American Indian schoolchildren. Prev Chronic Dis 2009;6:A20. [PMC free article] [PubMed] [Google Scholar]
- 6. Bushamuka VN, de Pee S, Talukder A, et al. . Impact of a homestead gardening program on household food security and empowerment of women in Bangladesh. Food Nutr Bull 2005;26:17–25. 10.1177/156482650502600102 [DOI] [PubMed] [Google Scholar]
- 7. Stroink ML, Nelson CH. Aboriginal health learning in the forest and cultivated gardens: building a nutritious and sustainable food system. J Agromedicine 2009;14:263–9. 10.1080/10599240902739737 [DOI] [PubMed] [Google Scholar]
- 8. Armstrong D. A survey of community gardens in upstate New York: implications for health promotion and community development. Health Place 2000;6:319–27. 10.1016/S1353-8292(00)00013-7 [DOI] [PubMed] [Google Scholar]
- 9. Twiss J, Dickinson J, Duma S, et al. . Community gardens: lessons learned from California Healthy Cities and Communities. Am J Public Health 2003;93:1435–8. 10.2105/AJPH.93.9.1435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alaimo K, Packnett E, Miles RA, et al. . Fruit and vegetable intake among urban community gardeners. J Nutr Educ Behav 2008;40:94–101. 10.1016/j.jneb.2006.12.003 [DOI] [PubMed] [Google Scholar]
- 11. Litt JS, Soobader MJ, Turbin MS, et al. . The influence of social involvement, neighborhood aesthetics, and community garden participation on fruit and vegetable consumption. Am J Public Health 2011;101:1466–73. 10.2105/AJPH.2010.300111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Castro DC, Samuels M, Harman AE. Growing healthy kids: a community garden-based obesity prevention program. Am J Prev Med 2013;44(3 Suppl 3):S193–S99. 10.1016/j.amepre.2012.11.024 [DOI] [PubMed] [Google Scholar]
- 13. Park S-A, Shoemaker CA, Haub MD. Physical and Psychological Health Conditions of Older Adults Classified as Gardeners or Nongardeners. HortScience 2009;44:206–10. 10.21273/HORTSCI.44.1.206 [DOI] [Google Scholar]
- 14. Draper C, Freedman D. Review and Analysis of the Benefits, Purposes, and Motivations Associated with Community Gardening in the United States. J Community Pract 2010;18:458–92. 10.1080/10705422.2010.519682 [DOI] [Google Scholar]
- 15. Hawkins JL, Thirlaway KJ, Backx K, et al. . Allotment Gardening and Other Leisure Activities for Stress Reduction and Healthy Aging. Horttechnology 2011;21:577–85. 10.21273/HORTTECH.21.5.577 [DOI] [Google Scholar]
- 16. Van Den Berg AE, Custers MH. Gardening promotes neuroendocrine and affective restoration from stress. J Health Psychol 2011;16:3–11. 10.1177/1359105310365577 [DOI] [PubMed] [Google Scholar]
- 17. Litt JS, Lambert JR, Glueck DH. Gardening and age-related weight gain: results from a cross-sectional survey of Denver residents. Prev Med Rep 2017;8:221–5. 10.1016/j.pmedr.2017.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Porter CM. What gardens grow: Outcomes from home and community gardens supported by community-based food justice organizations. J Agric Food Syst Community Dev 2018;8(Suppl 1):187–205. 10.5304/jafscd.2018.08A.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Community Activation for Prevention (CAPs): A Study of Community Gardening. 2017. http://clinicaltrials.gov/ct2
- 20. Naschold F. Constructing Internally Consistent BMI Z-Scores for Adults and Children to Examine Intra-Household Health Effects. Department of Economics, University of Wyoming, 2018. http://ageconsearch.umn.edu/record/258345/files/Abstracts_17_05_24_17_55_06_44__69_146_104_213_0.pdf. [Google Scholar]
- 21. Sund ER, Jones A, Midthjell K. Individual, family, and area predictors of BMI and BMI change in an adult Norwegian population: findings from the HUNT study. Soc Sci Med 2010;70:1194–202. 10.1016/j.socscimed.2010.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Block JP, Subramanian SV, Christakis NA, et al. . Population trends and variation in body mass index from 1971 to 2008 in the Framingham Heart Study Offspring Cohort. PLoS One 2013;8:e63217 10.1371/journal.pone.0063217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mason C, Katzmarzyk PT. Variability in waist circumference measurements according to anatomic measurement site. Obesity 2009;17:1789–95. 10.1038/oby.2009.87 [DOI] [PubMed] [Google Scholar]
- 24. Norman K, Stobäus N, Gonzalez MC, et al. . Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr 2011;30:135–42. 10.1016/j.clnu.2010.09.010 [DOI] [PubMed] [Google Scholar]
- 25. Rantanen T, Guralnik JM, Foley D, et al. . Midlife hand grip strength as a predictor of old age disability. JAMA 1999;281:558–60. 10.1001/jama.281.6.558 [DOI] [PubMed] [Google Scholar]
- 26. Rantanen T, Harris T, Leveille SG, et al. . Muscle strength and body mass index as long-term predictors of mortality in initially healthy men. J Gerontol A Biol Sci Med Sci 2000;55:M168–M173. 10.1093/gerona/55.3.M168 [DOI] [PubMed] [Google Scholar]
- 27. Ware JEJ, Kosinski M, Turner-Bowker DM, et al. . How to Score Version 2 of the SF-12 Healthy Survey (With a Supplement Document Version 1). Lincoln, RI, 2002. [Google Scholar]
- 28. Bickel G, Nord M, Price C, et al. . Guide to measuring household food security. U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. 2000. Retrieved from https://fns-prod.azureedge.net/sites/default/files/FSGuide.pdf
- 29. National Institutes of Health. Eating at America’s Table Study: Quick Food Scan. http://riskfactor.cancer.gov/diet/screeners/fruitveg/allday.pdf
- 30. Yaroch AL, Tooze J, Thompson FE, et al. . Evaluation of three short dietary instruments to assess fruit and vegetable intake: the National Cancer Institute’s food attitudes and behaviors survey. J Acad Nutr Diet 2012;112:1570–7. 10.1016/j.jand.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. John JH, Ziebland S, Yudkin P, et al. . Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: a randomised controlled trial. Lancet 2002;359:1969–74. 10.1016/S0140-6736(02)98858-6 [DOI] [PubMed] [Google Scholar]
- 32. McKenzie D. Beyond baseline and follow-up: the case for more T in experiments. J Dev Econ 2012;99:210–21. 10.1016/j.jdeveco.2012.01.002 [DOI] [Google Scholar]
- 33. Garber AJ, Duncan TG, Goodman AM, et al. . Efficacy of metformin in type II diabetes: results of a double-blind, placebo-controlled, dose-response trial. Am J Med 1997;103:491–7. [DOI] [PubMed] [Google Scholar]
- 34. Geldenhuys S, Hart PH, Endersby R, et al. . Ultraviolet radiation suppresses obesity and symptoms of metabolic syndrome independently of vitamin D in mice fed a high-fat diet. Diabetes 2014;63:3759–69. 10.2337/db13-1675 [DOI] [PubMed] [Google Scholar]
- 35. Center for American Indian Health, Johns Hopkins Bloomberg School of Public Health. Family Gardens How To Guide [Online]. http://caih.jhu.edu/programs/feastforthefuture/family-gardens/family-gardens-how-to-guide (accessed 15 Dec 2017).
- 36. Carney PA, Hamada JL, Rdesinski R, et al. . Impact of a community gardening project on vegetable intake, food security and family relationships: a community-based participatory research study. J Community Health 2012;37:874–81. 10.1007/s10900-011-9522-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.